Abstract
Background
Because trends in the epidemiology and burden of gastroesophageal reflux disease (GERD) are changing, reinvestigating the geographical differences and trend changes is essential. Here we evaluated the latest epidemiologic patterns and trends for GERD, using data from Global Burden of Diseases, Injuries, and Risk Factors Study (GBD) 2019.
Methods
Annual case numbers, age-standardized rates of prevalence, incidence, and years of life lived with disability (YLDs), and their estimated annual percentage changes (EAPCs) for GERD between 1990 and 2019 were derived from the GBD 2019 study. Association between GERD burden and socio-demographic index (SDI) was also investigated.
Results
In 2019, there were 783.95 million cases of GERD globally. Between 1990 and 2019, the total number of prevalent cases, incident cases, and YLDs increased by 77.53%, 74.79%, and 77.19%, respectively. The global age-standardized incidence rate (ASIR) and age-standardized YLD rate (ASYR) increased during this period (EAPC = 0.06 and 0.05, respectively). Tropical Latin America and East Asia had the highest and lowest age-standardiZed prevalence rate (ASPR), ASIR, and ASYR in 2019, respectively. From 1990 to 2019, prevalent cases, incident cases, YLDs, and their corresponding age-standardized rates of GERD were higher in females than males in all years. Higher SDI was associated with lower ASPR, ASIR, and ASYR of GERD in 2019.
Conclusions
GERD will continue to be a major public health burden due to increasing numbers of prevalent cases, incident cases, and YLDs. In order to tackle this troublesome disease, it is crucial to understand the changes in both global and regional trends in epidemiology and the burden for policymakers and other stakeholders.
Key messages
This is the most updated estimate on GERD epidemiology globally, including 204 countries, some of which were not assessed before.
The overall burden of GERD continued to worsen with the prevalent cases increasing by 77.53% from 441.57 million in 1990 to 783.95 million in 2019.
GERD is likely to remain a common reason for consultation in primary care, and our data may allow for health service provision planning.
Keywords: Gastroesophageal reflux disease, global burden of disease, prevalence, epidemiology
Introduction
Gastroesophageal reflux disease (GERD) is a common condition in which the reflux of gastric contents into the oesophagus results in symptoms and/or complications [1]. Typical GERD symptoms include heartburn and acid reflux. Histological changes in the oesophageal mucosa can be categorized into non-erosive reflux disease, reflux esophagitis, and Barrett's oesophagus [2]. GERD can also cause a variety of extraesophageal manifestations including asthma, cough, sore throat, throat clearing, and unexplained chest pain [3]. Due to its recurrent and troublesome symptoms and complications (i.e. oesophageal inflammation, stricture, ulceration, perforation, metaplasia, and oesophageal adenocarcinoma) [4], GERD seriously lowers patients' health-related quality of life. Besides, due to its chronic nature and high prevalence, GERD has imposed a significant economic burden on patients and their families, health services, and society [5]. The clinical management of GERD influences the lives of many individuals and is responsible for the substantial consumption of health care and societal resources [2].
Previous systematic reviews have presented the prevalence and incidence of GERD in the past decade [4, 6]. Based on the Global Burden of Disease (GBD) 2017 Study, GBD 2017 Gastro-oesophageal Reflux Disease Collaborators comprehensively described the global burden of GERD [7]. However, the burden of GERD varies over time and between or within countries and territories. Clinical trial suggests similar remission rates with surgery or medication [8]. However, two-thirds to 100% of patients will relapse when PPIs are stopped [9]. The global prevalence of GERD is increasing [3]. And the incidence of GERD has been increasing yearly due to improvements in living standards and changes in lifestyle and dietary habits recently [10]. These significant changes highlight the need for a comparable, consistent and systematic analysis of disease burden and trends concerning GERD in different regions and countries, which is critical to creating strategies for global intervention.
The GBD 2019 Study, an extensive worldwide observational epidemiological study to date, assesses the incidence, prevalence, and disability of 369 diseases by age, sex, location, and year [11], which presents an opportunity to better understand the epidemiology of GERD. In this article, we aimed to describe the burden of GERD, by age, sex, and social-development index (SDI), in 204 countries and territories from 1990 to 2019. The availability of estimates of disease burden for GERD would provide a better understanding of the impact of GERD on population health and the need for appropriate preventive strategies and health resource allocations.
Methods
The detailed description of original data and general methodology of GBD 2019 study has been described in previous publications [11–14]. The study protocol and statistical codes of the estimated GERD can be obtained from the website: http://ghdx.healthdata.org/gbd-2019/code/cod-4. In brief, incidence and prevalence of disease were estimated using a wide range of data from representative population. These data were derived from literature reviews and identified through research collaborations, which included published scientific reports of registries and cohorts, data from cohort and registry studies, administrative health data and reports, and population surveys [12]. DisMod-MR 2.1, an epidemiologic state-transition disease modelling software, together with MR-BRT, a Bayesian meta-regression software, were used to produce consistent disease estimates [12]. Uncertainty intervals (UIs) were produced for every metric using the 25th and 975th ordered 1000 draw values of the posterior distribution [12].
Crude and age-standardized estimates of various measures of the burden of GERD in 204 countries and territories from 1990 to 2019 and the respective 95% UIs were extracted from the GBD database via http://ghdx.healthdata.org/gbd-results-tool and no specific permissions were required to access data. For the GBD 2019 assessment, GERD was claimed by the following codes according to the 10th revision of the International Classification of Diseases (ICD-10): K21-K21.9, K22.7, and R12 (Supplementary Table 1). The variables obtained from the database included incident cases, prevalent cases, YLDs numbers, and their corresponding age-standardized rates (ASRs) at the global, regional, and national levels. These data were stratified by age (5–9, every 5-year age group up to 95 years, and 95 years and older), calendar year (1990–2019), region, and country (or territory). Geographically, the world was divided into 21 GBD regions. Moreover, the 204 countries and territories were categorized into five groups in terms of their socio-demographic index (SDI): high, high-middle, middle, low-middle, and low SDI quintile [12].
Estimated average percentage change (EAPC) was computed to depict the secular trend in ASRs of GERD burden based on a regression model by fitting the natural logarithm of ASR with the calendar year, namely, y = α + βx+ɛ, where y = ln (rate), x = calendar year, and ε = error term. In this formula, β represents the positive or negative ASR trends. EAPC and its 95% confidence interval (CI) were calculated from the formula of 100 × (exp (β) −1) [15]. The age-standardized indicator was recognized to be in an increasing trend if the value of EAPC and the lower boundary of 95% CI were both greater than 0, to be a decreasing trend if EAPC value and the upper boundary of 95% CI were both less than 0, and to be a constant trend when 95% CI of EAPC included 0. All statistical analyses and visualizations were conducted using R statistical software program (version 4.1.0). P-value <.05 was considered statistically significant.
Because the study was based on publicly available dataset, this study was exempted by the ethics committee of the Third Xiangya Hospital of Central South University. Each step used to analyse the GBD database in the current study followed the guideline of cross-sectional study described in the Guidelines for Accurate and Transparent Health Estimates Reporting (GATHER) [16].
Results
Global burden and temporal trend in GERD
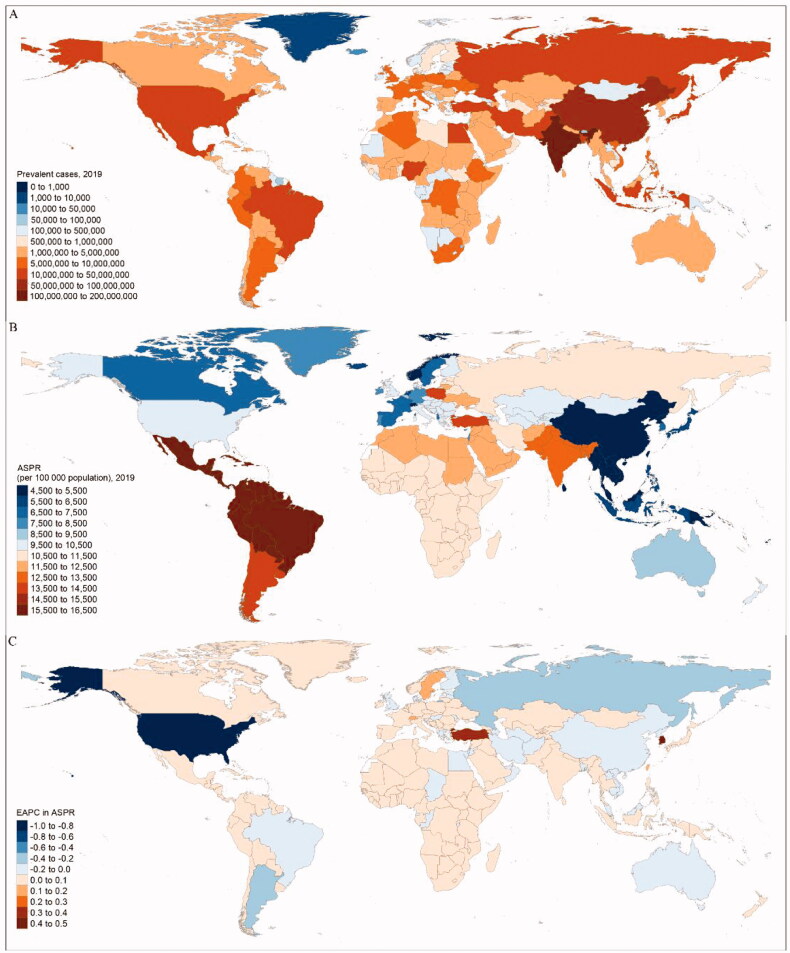
Globally, the number of prevalent cases of GERD increased by 77.53% from 441.57 million (95% UI 383.48– 496.84) in 1990 to 783.95 million (689.55–876.53) in 2019 (Supplementary Table 2 and Figure 1(a)). Besides, the age-standardized prevalence rate (ASPR) of GERD was 9344.52 (8213.69–10456.84) per 100,000 population in 1990 and 9574.45 (8416.42–10,698.38) per 100,000 population in 2019, with the EAPC being 0.04 (95% CI 0.00–0.08) (Table 1, Figure 1(b)). Meanwhile, the global incident cases of GERD were 309.38 million (272.53–349.51) in 2019, increasing from 177.00 million (154.83–201.15) in 1990, with an increasing EAPC in age-standardized incidence rate (ASIR) of 0.06 (0.02–0.10) from 3687.27 (3256.92–4165.86) in 1990–3792.79 (3341.66–4280.02) in 2019 per 100,000 population (Table 1 and Supplementary Table 2). Globally, there were 6.03 million (3.10–10.82) YLDs caused by GERD in 2019, which increased by 77.19% from 3.40 million (1.76–6.09) in 1990. The age-standardized YLD rate (ASYR) increased from 71.68 (36.95–128.64) in 1990 to 73.63 (38.03–132.08) in 2019 per 100,000 population with the EAPC being 0.05 (0.01–0.09) (Table 1 and Supplementary Table 2). Meanwhile, from 2015 to 2019, ASPR, ASIR, and ASYR all increased globally with the EAPC being 0.56 (0.30–0.82), 0.54 (0.30–0.79), and 0.56 (0.30–0.82), respectively (Supplementary Table 3).
Figure 1.
The global prevalence burden of GERD in 204 countries and territories. (a) The absolute number of GERD prevalent cases in 2019. (b) The ASPR (per 100,000 population) of GERD in 2019. (c) The EAPC of ASPR for GERD between 1990 and 2019. ASPR: age-standardized prevalence rate; EAPC: estimated annual percentage change; GERD: gastroesophageal reflux disease.
Table 1.
Age-standardized prevalence, incidence, and YLD rates for gastroesophageal reflux disease (GERD) in 1990 and 2019 and their temporal trends from 1990 to 2019.
| Characteristics | Age-standardized prevalence rate per 100,000 population |
Age-standardized incidence rate per 100,000 population |
Age-standardized YLD rate per 100,000 population |
||||||
|---|---|---|---|---|---|---|---|---|---|
| 1990 No. (95%UI) | 2019 No. (95%UI) | EAPC No. (95%CI) | 1990 No. (95%UI) | 2019 No. (95%UI) | EAPC No. (95%CI) | 1990 No. (95%UI) | 2019 No. (95%UI) | EAPC No. (95%CI) | |
| Global | 9344.52 (8213.69 to 10,456.84) | 9574.45 (8416.42 to 10,698.38) | 0.04 (0.00 to 0.08) | 3687.27 (3256.92 to 4165.86) | 3792.79 (3341.66 to 4280.02) | 0.06 (0.02 to 0.10) | 71.68 (36.95 to 128.64) | 73.63 (38.03 to 132.08) | 0.05 (0.01 to 0.09) |
| Sex | |||||||||
| Male | 8965.06 (7872.25 to 10,037.60) | 9202.85 (8087.69 to 10,290.43) | 0.06 (0.02 to 0.09) | 3548.43 (3129.86 to 4016.03) | 3655.00 (3218.54 to 4142.05) | 0.08 (0.04 to 0.11) | 69.08 (35.62 to 124.33) | 71.11 (36.71 to 127.76) | 0.07 (0.04 to 0.10) |
| Female | 9719.69 (8537.36 to 10,915.06) | 9941.90 (8717.74 to 11,155.47) | 0.02 (−0.03 to 0.06) | 3825.60 (3378.20 to 4311.11) | 3929.78 (3465.46 to 4430.41) | 0.05 (0.01 to 0.08) | 74.25 (38.28 to 132.56) | 76.13 (39.35 to 135.76) | 0.07 (0.04 to 0.10) |
| SDI quintile | |||||||||
| High | 8512.56 (7442.29 to 9594.13) | 8252.43 (7193.12 to 9291.2) | −0.24 (−0.32 to −0.15) | 3388.61 (2968.37 to 3866.89) | 3319.50 (2906.37 to 3810.77) | −0.17 (−0.24 to −0.11) | 65.37 (33.27 to 118.08) | 63.40 (32.17 to 114.26) | −0.23 (−0.32 to −0.15) |
| High-middle | 9014.77 (7927.55 to 10,110.23) | 8700.91 (7677.19 to 9701.44) | −0.21 (−0.27 to −0.14) | 3524.13 (3116.29 to 3994.07) | 3410.01 (3011.96 to 3854.01) | −0.19 (−0.24 to −0.13) | 69.26 (35.58 to 124.07) | 67.09 (34.59 to 120.40) | −0.19 (−0.25 to −0.13) |
| Middle | 8082.43 (7099.76 to 9064.77) | 8720.16 (7652.32 to 9769.90) | 0.24 (0.21 to 0.28) | 3203.91 (2827.63 to 3614.98) | 3461.20 (3052.34 to 3901.86) | 0.25 (0.22 to 0.28) | 62.16 (32.01 to 111.64) | 67.19 (34.68 to 120.62) | 0.25 (0.22 to 0.29) |
| Low-middle | 11,773.99 (10,401.16 to 13,164.30) | 11,887.87 (10,505.45 to 13,282.26) | 0.02 (0.01 to 0.03) | 4603.90 (4087.96 to 5177.94) | 4650.41 (4124.90 to 5226.35) | 0.03 (0.02 to 0.04) | 89.83 (46.6 to 161.42) | 90.99 (47.14 to 163.13) | 0.03 (0.02 to 0.05) |
| Low | 12,085.16 (10,597.10 to 13,536.65) | 12,054.64 (10,577.33 to 13,501.86) | 0.00 (−0.01 to 0.00) | 4758.96 (4219.43 to 5379.93) | 4741.79 (4202.29 to 5361.43) | −0.01 (−0.01 to −0.01) | 92.18 (47.98 to 165.24) | 92.25 (48.02 to 165.73) | 0.01 (0.01 to 0.02) |
| GBD region | |||||||||
| Andean Latin America | 15,934.38 (14,135.36 to 17,780.23) | 15,932.06 (14,135.41 to 17,774.71) | 0.00 (0.00 to 0.00) | 5976.14 (5315.06 to 6644.79) | 5974.25 (5312.88 to 6641.29) | 0.00 (0.00 to 0.00) | 123.03 (63.86 to 217.88) | 123.15 (64.00 to 218.31) | 0.00 (0.00 to 0.01) |
| Australasia | 8694.45 (7579.92 to 9896.39) | 8679.81 (7566.16 to 9881.92) | −0.02 (−0.16 to 0.12) | 3516.72 (3073.84 to 4048.01) | 3511.78 (3070.46 to 4043.23) | −0.01 (−0.12 to 0.09) | 66.71 (34.03 to 120.31) | 66.66 (34.06 to 121.04) | −0.02 (−0.16 to 0.13) |
| Caribbean | 15,937.21 (14,138.44 to 17,780.66) | 15,935.32 (14,137.14 to 17,777.84) | 0.00 (0.00 to 0.00) | 5976.80 (5315.24 to 6644.09) | 5975.49 (5313.40 to 6642.33) | 0.00 (0.00 to 0.00) | 122.99 (64.07 to 217.41) | 122.78 (64.04 to 216.84) | 0.00 (−0.01 to 0.00) |
| Central Asia | 10,482.56 (9135.45 to 11,801.76) | 10,471.50 (9125.15 to 11,787.88) | 0.00 (0.00 to 0.00) | 4171.74 (3663.06 to 4766.35) | 4168.45 (3658.11 to 4764.72) | 0.00 (0.00 to 0.00) | 80.89 (41.35 to 146.25) | 80.81 (41.30 to 145.70) | 0.00 (0.00 to 0.00) |
| Central Europe | 10,863.54 (9520.36 to 12,246.17) | 10,987.32 (9631.12 to 12,376.53) | 0.05 (0.04 to 0.05) | 4262.46 (3756.68 to 4830.14) | 4301.11 (3789.35 to 4872.82) | 0.04 (0.03 to 0.04) | 83.43 (42.78 to 148.19) | 84.64 (43.44 to 150.20) | 0.06 (0.05 to 0.06) |
| Central Latin America | 15,940.70 (14,148.00 to 17,600.10) | 15,949.53 (14,156.95 to 17,601.72) | 0.00 (0.00 to 0.00) | 6039.93 (5379.89 to 6694.89) | 6040.22 (5378.11 to 6691.82) | 0.00 (0.00 to 0.00) | 122.69 (63.80 to 218.43) | 122.92 (63.83 to 218.74) | 0.00 (0.00 to 0.01) |
| Central Sub-Saharan Africa | 11,036.02 (9606.30 to 12,450.75) | 11,035.93 (9621.69 to 12,451.49) | 0.00 (0.00 to 0.00) | 4388.20 (3855.17 to 5009.03) | 4388.34 (3853.19 to 5007.99) | 0.00 (0.00 to 0.00) | 84.13 (43.69 to 149.18) | 84.58 (43.95 to 151.08) | 0.02 (0.02 to 0.02) |
| East Asia | 4542.27 (3937.00 to 5164.94) | 4523.40 (3912.03 to 5149.59) | −0.14 (−0.29 to 0.00) | 1853.82 (1617.20 to 2149.28) | 1847.31 (1612.24 to 2139.60) | −0.13 (−0.26 to 0.01) | 35.12 (17.82 to 63.31) | 35.05 (17.78 to 63.23) | −0.13 (−0.28 to 0.01) |
| Eastern Europe | 11,356.33 (9995.84 to 12,756.35) | 11,331.34 (9974.89 to 12,728.49) | −0.21 (−0.33 to −0.10) | 4487.10 (3948.05 to 5093.00) | 4478.85 (3938.02 to 5080.20) | −0.17 (−0.26 to −0.08) | 86.98 (44.47 to 157.52) | 87.11 (44.45 to 157.69) | −0.20 (−0.31 to −0.08) |
| Eastern Sub-Saharan Africa | 11,191.12 (9742.00 to 12,561.77) | 11,199.13 (9750.44 to 12,572.49) | 0.00 (0.00 to 0.00) | 4451.93 (3906.53 to 5069.11) | 4454.59 (3909.59 to 5068.92) | 0.00 (0.00 to 0.00) | 85.62 (44.37 to 152.89) | 86.02 (44.60 to 154.04) | 0.02 (0.02 to 0.02) |
| High-income Asia Pacific | 6119.10 (5333.23 to 6997.03) | 6225.69 (5431.16 to 7113.27) | 0.25 (0.12 to 0.37) | 2532.38 (2208.26 to 2926.00) | 2572.68 (2244.20 to 2974.08) | 0.20 (0.10 to 0.30) | 47.29 (24.05 to 85.78) | 48.25 (24.60 to 87.46) | 0.25 (0.13 to 0.38) |
| High-income North America | 10614.30 (9254.75 to 11,985.62) | 9401.60 (8190.07 to 10,614.97) | −0.82 (−1.02 to −0.63) | 4095.69 (3560.93 to 4654.85) | 3727.97 (3253.14 to 4285.69) | −0.66 (−0.81 to −0.50) | 81.07 (41.69 to 145.33) | 71.62 (36.26 to 128.42) | −0.83 (−1.03 to −0.64) |
| North Africa and Middle East | 12,240.02 (10,688.33 to 13,786.42) | 12,341.45 (10,898.84 to 13,766.4) | 0.03 (0.01 to 0.05) | 4781.05 (4214.49 to 5396.43) | 4799.43 (4259.75 to 5391.27) | 0.01 (−0.01 to 0.03) | 94.30 (48.44 to 170.89) | 95.07 (48.91 to 170.82) | 0.03 (0.01 to 0.05) |
| Oceania | 5283.72 (4563.88 to 6047.55) | 5284.59 (4563.20 to 6048.44) | 0.00 (0.00 to 0.00) | 2164.68 (1891.94 to 2493.36) | 2165.05 (1892.06 to 2495.02) | 0.00 (0.00 to 0.00) | 40.54 (20.70 to 73.93) | 40.48 (20.57 to 73.75) | 0.00 (0.00 to 0.00) |
| South Asia | 13,377.44 (11,777.46 to 14,977.74) | 13,377.84 (11,769.10 to 14,984.49) | 0.00 (−0.01 to 0.01) | 5222.37 (4632.67 to 5883.96) | 5223.34 (4636.37 to 5882.55) | 0.00 (−0.01 to 0.01) | 101.66 (52.54 to 183.28) | 102.04 (52.78 to 183.85) | 0.01 (0.00 to 0.03) |
| Southeast Asia | 5432.59 (4716.44 to 6211.09) | 5427.51 (4711.75 to 6203.74) | 0.00 (0.00 to 0.00) | 2213.29 (1932.35 to 2562.26) | 2211.43 (1931.03 to 2560.16) | 0.00 (0.00 to 0.00) | 41.77 (21.23 to 75.63) | 41.85 (21.26 to 76.10) | 0.01 (0.01 to 0.01) |
| Southern Latin America | 13,628.01 (11,862.59 to 15,357.49) | 13,625.51 (11,860.68 to 15,353.48) | −0.15 (−0.21 to −0.09) | 5003.17 (4406.68 to 5687.32) | 5002.39 (4405.74 to 5686.77) | −0.09 (−0.13 to −0.06) | 105.21 (54.14 to 189.23) | 105.12 (54.12 to 187.46) | −0.15 (−0.21 to −0.09) |
| Southern Sub-Saharan Africa | 11,369.36 (9899.33 to 12,811.40) | 11,379.36 (9906.25 to 12,826.20) | 0.00 (0.00 to 0.00) | 4522.20 (3978.59 to 5137.46) | 4524.95 (3983.00 to 5139.59) | 0.00 (0.00 to 0.00) | 87.11 (45.02 to 155.84) | 86.82 (44.80 to 155.01) | −0.01 (−0.01 to −0.01) |
| Tropical Latin America | 16,335.09 (14,509.64 to 18,040.17) | 16,207.50 (14,319.22 to 17,944.65) | −0.12 (−0.16 to −0.08) | 6164.75 (5485.23 to 6806.08) | 6144.66 (5455.45 to 6787.85) | −0.07 (−0.09 to −0.04) | 125.29 (65.30 to 221.80) | 124.78 (64.60 to 222.07) | −0.11 (−0.15 to −0.07) |
| Western Europe | 8218.38 (7188.66 to 9247.73) | 8217.57 (7182.45 to 9250.17) | 0.02 (0.01 to 0.03) | 3304.06 (2909.15 to 3774.92) | 3303.30 (2898.46 to 3775.10) | 0.02 (0.00 to 0.03) | 63.26 (32.24 to 113.81) | 63.30 (32.30 to 114.14) | 0.02 (0.01 to 0.03) |
| Western Sub-Saharan Africa | 11,224.51 (9779.71 to 12,643.62) | 11,236.58 (9782.82 to 12,626.62) | 0.00 (0.00 to 0.01) | 4465.94 (3929.26 to 5079.05) | 4469.45 (3926.83 to 5086.96) | 0.00 (0.00 to 0.00) | 86.14 (44.53 to 154.02) | 86.45 (44.83 to 154.98) | 0.02 (0.01 to 0.02) |
Abbreviations: CI: confidence interval; EAPC, estimated annual percentage change; GBD: Global Burden of Disease; SDI: socio-demographic index; UI: uncertainty interval; YLD: years of life lived with disability.
Variation in GERD burden at regional level
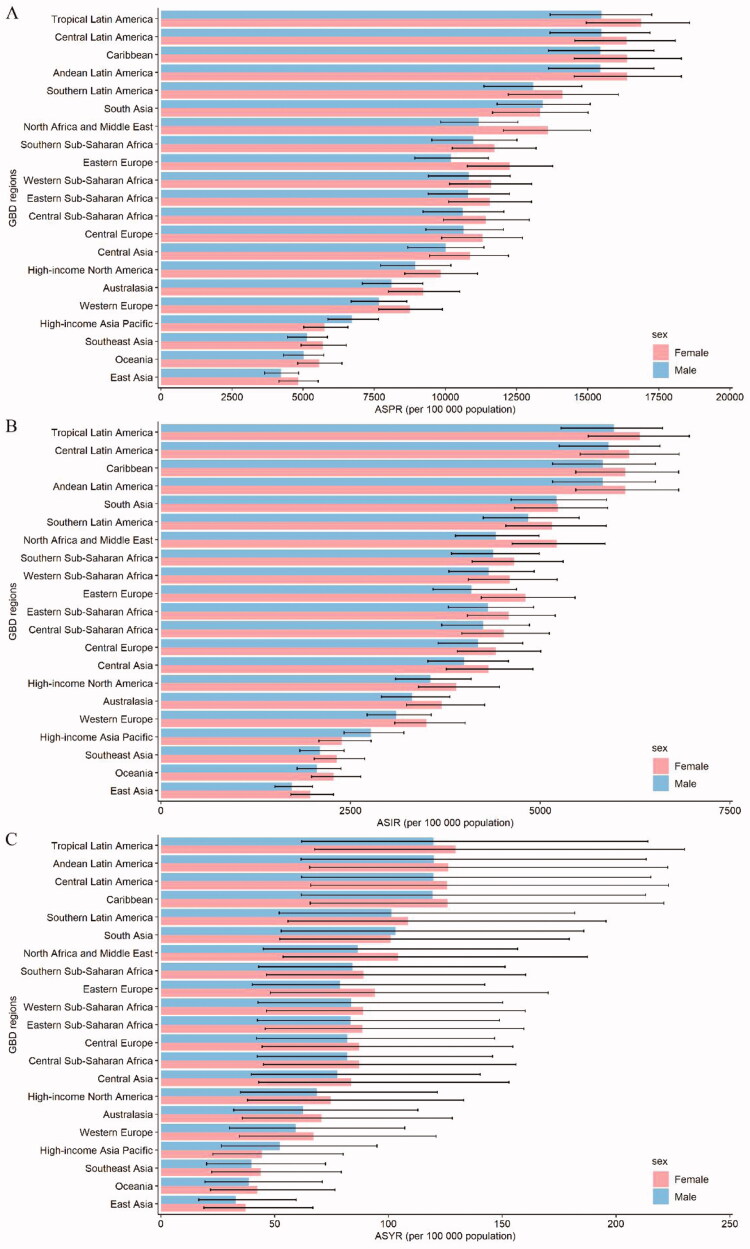
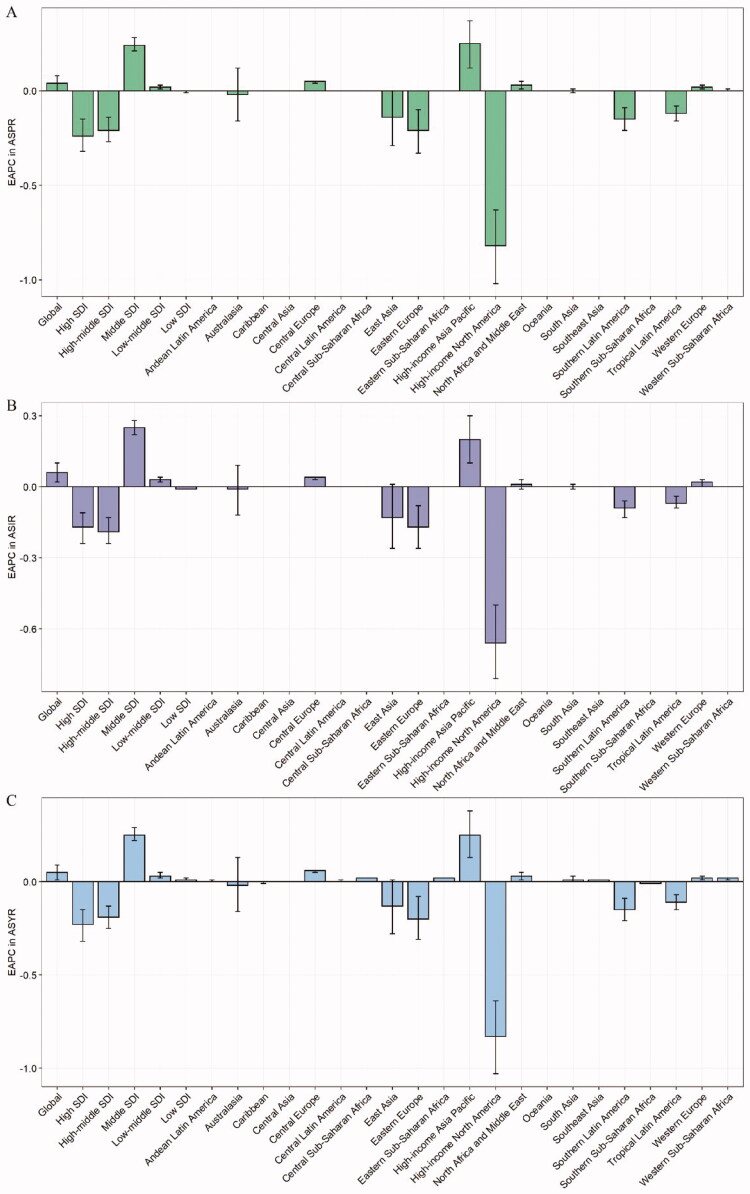
Regarding GBD regions, South Asia, East Asia, and North Africa and Middle East were among the top three regions for the largest numbers of prevalent cases, incident cases, and YLDs in 2019 (Supplementary Table 2). On the contrary, the lowest numbers of prevalent cases, incident cases, and YLDs in 2019 were observed in Oceania, Australasia, and Caribbean. Tropical Latin America was the region with the highest ASPR [16,207.50 (95% UI 14,319.22–17,944.65)], ASIR [6144.66 (5455.45–6787.85)], and ASYR [124.78 (64.60–222.07)] in 2019 (Table 1 and Figure 2). East Asia had the lowest ASPR [4523.40 (3912.03–5149.59)], ASIR [1847.31 (1612.24–2139.60)], and ASYR [35.05 (17.78–63.23)] among regions in 2019. Moreover, ASPR and ASIR remained stable over 30 years in almost half of all the regions. However, total prevalent cases, incident cases, and YLDs increased across all GBD regions during the observation period (Supplementary Figures 1–3). The EAPCs in ASPR, ASIR, and ASYR were highest in High-income Asia Pacific (EAPC = 0.25, 0.20, and 0.25, respectively) and lowest in High-income North America (EAPC = −0.82, −0.66, and −0.83, respectively) from 1990 to 2019 (Figure 3). However, from 2015 to 2019, the EAPCs in ASPR, ASIR, and ASYR were highest in Eastern Europe (EAPC = 1.74, 1.41, and 1.73, respectively), and the EAPC in ASPR was lowest in North Africa and Middle East (EAPC = −0.07), the EAPCs in ASIR and ASYR were lowest in Western Europe (EAPC = −0.08 and −0.13, respectively) (Supplementary Table 3).
Figure 2.
The ASPR (a), ASIR (b), and ASYR (c) due to GERD by sex, across 21 GBD regions, in 2019. Error bars indicate the 95% uncertainty interval (UI) for the age-standardized rates. ASIR: age-standardized incidence rate; ASPR: age-standardized prevalence rate; ASYR: age-standardized YLD rate; GBD: Global Burden of Disease; GERD: gastroesophageal reflux disease.
Figure 3.
The EAPCs in ASPR (a), ASIR (b), and ASYR (c) due to GERD from 1990 to 2019, both sexes, by GBD region, and by SDI quintile. Error bars indicate the 95% confidence interval (CI) for the rates. ASIR: age-standardized incidence rate; ASPR: age-standardized prevalence rate; ASYR: age-standardized YLD rate; EAPC: estimated annual percentage change; GBD: Global Burden of Disease; GERD: gastroesophageal reflux disease; SDI: socio-demographic index.
Variation in GERD burden at national and territorial level
At the national and territorial level in 2019, India and China had the highest number of prevalent cases [181.55 million (158.49–204.38), 81.64 million (70.73–93.51), respectively], the highest number of incident cases [71.84 million (95% UI 63.58–81.35), 32.71 million (28.44–38.21), respectively], and the highest number of YLD cases [1.39 million (0.72–2.49), 0.63 million (0.32–1.15), respectively] (Supplementary Table 4, Figure 1, and Supplementary Figures 4 and 5). In 2019, the highest ASIR of GERD was observed in Brazil [6146.60 (5457.64–6790.57) per 100,000 population], and the highest ASPR and ASYR were found in Paraguay [16,310.51 (14,395.46–18,167.8) per 100,000 population, 125.91 (65.11–223.26) per 100,000 population, respectively] (Supplementary Table 5 and Supplementary Figures 6 and 7). In contrast, the lowest ASPR, ASIR, and ASYR were found in China [4509.32 (3899.11–5133.17) per 100,000 population, 1841.66 (1607.09–2133.51) per 100,000 population, and 34.94 (17.73–63.02) per 100,000 population, respectively]. Between 1990 and 2019, ASPR and ASIR remained stable in more than 60% countries or territories. Republic of Korea, Turkey, and Taiwan (Province of China) ranked in the top three countries or territories experienced a significant increase in ASPR (EAPC = 0.48, 0.30, and 0.19, respectively), ASIR (EAPC = 0.35, 0.17, and 0.14, respectively), and ASYR (EAPC = 0.49, 0.29, and 0.19, respectively), while United States of America, Russian Federation, and Argentina ranked in the top three countries or territories experienced a significant decrease in ASPR (EAPC = −0.89, −0.31, and −0.22, respectively), ASIR (EAPC = −0.71, −0.25, and −0.14, respectively), and ASYR (EAPC = −0.90, −0.30, and −0.23, respectively) (Figure 1(c) and Supplementary Figures 8 and 9). Nevertheless, from 2015 to 2019, Russian Federation, Bangladesh, and Kuwait ranked in the top three countries or territories experienced a significant increase in ASPR (EAPC = 2.62, 1.32, and 0.10, respectively), ASIR (EAPC = 2.11, 0.88, and 0.09, respectively), and ASYR (EAPC = 2.61, 1.33, and 0.07, respectively) (Supplementary Table 6).
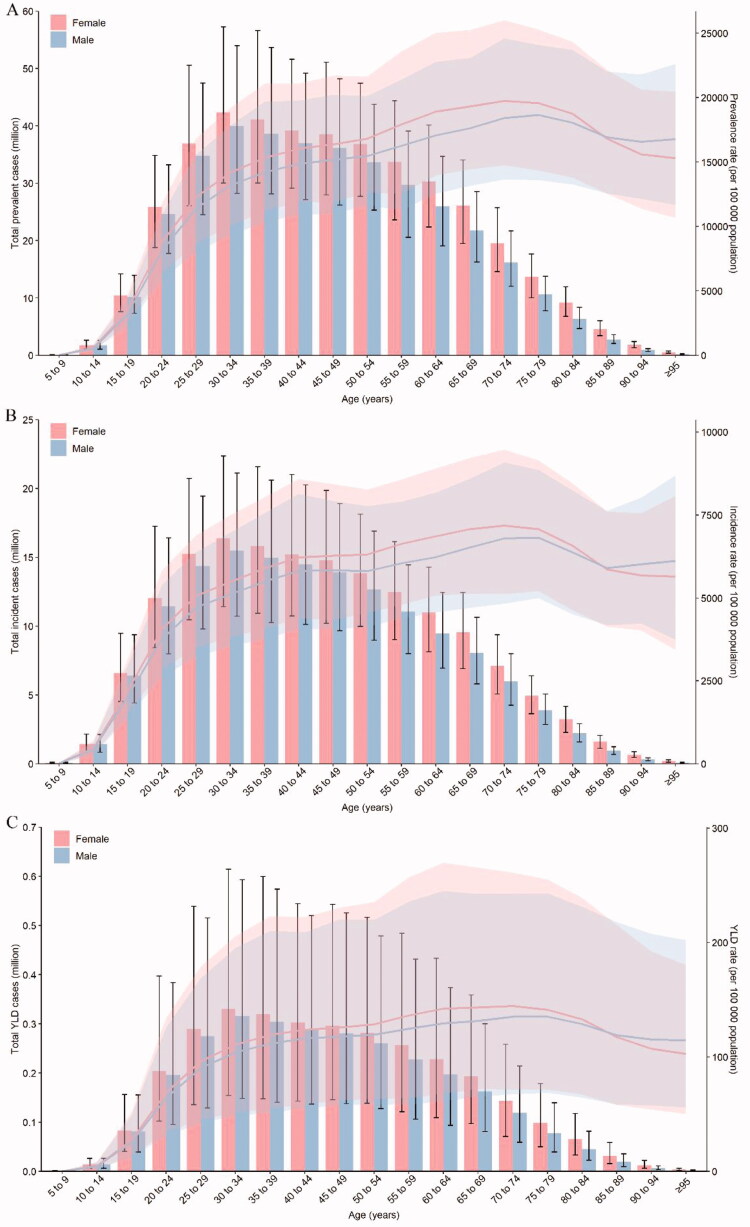
Variation in GERD burden in two sexes and five-year age groups
Overall, the global number of prevalent cases, incident cases, and YLDs was higher in females than males in 2019. The ASPR, ASIR, and ASYR were also higher in females than males (Supplementary Table 2). In 2019, the number of prevalent cases, incident cases, and YLDs peaked in the 30–34 years age group in both sexes (Figure 4). The highest peak of GERD ASPR and ASIR occurred at age 75–79 years in males and 70–74 years in females in 2019. And the highest ASYR was observed at age 70–74 years for both sexes. From 1990 to 2019, the number of prevalent cases, incident cases, and YLDs continued to increase in both sexes and was higher in females than males in all years. The ASIR and ASYR both increased in males [EAPC = 0.08 (95% CI 0.04–0.11), EAPC = 0.07 (0.04–0.10), respectively] and in females [EAPC = 0.05 (0.01–0.08), EAPC = 0.07 (0.04–0.10), respectively] (Table 1). However, the ASPR increased in males [EAPC = 0.06 (0.02–0.09)] and remained stable in females [EAPC = 0.02 (−0.03 – 0.06)]. Meanwhile, from 2015 to 2019, the EAPCs in ASPR, ASIR, and ASYR all increased in both males and females (Supplementary Table 3).
Figure 4.
Age patterns by sex of the total number and age-specific prevalence rate (a), age-specific incidence rate (b), and age-specific YLD rate (c) due to GERD at the global level in 2019. Error bars indicate the 95% uncertainty interval (UI) for the number of cases. Shading indicates the 95% UI for the rates. GERD: gastroesophageal reflux disease.
Variation in GERD burden by SDI
In 2019, higher SDI was associated with lower ASPR, ASIR, and ASYR of GERD, with values that were lower than the global rate in high, high-middle, and middle SDI quintiles, and higher than the global rate in the other two SDI quintiles (Table 1). High SDI quintile had the lowest ASPR, ASIR, and ASYR in 2019. Between 1990 and 2019, ASPR, ASIR, and ASYR decreased in high and high-middle quintiles, and increased in middle and low-middle SDI quintiles, whereas in low SDI quintile, ASIR decreased [EAPC = −0.01 (95% CI −0.01 – −0.01)], ASPR remained stable [EAPC = 0.00 (−0.01 – 0.00)], and ASYR increased [EAPC = 0.01 (0.01–0.02)]. Between 2015 and 2019, ASPR, ASIR, and ASYR decreased in low SDI quintile, but they all increased in the other four SDI quintiles (Supplementary Table 3).
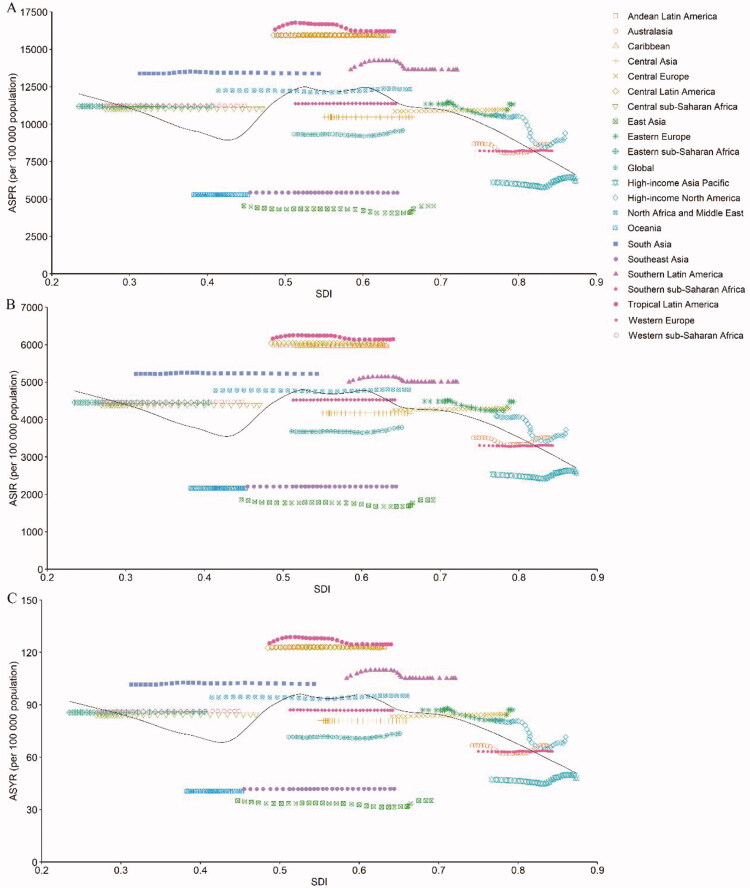
The observed global and regional ASPR, ASIR, and ASYR in relation to SDI, versus the expected level for each location on the basis of SDI, are shown in Figure 5, which are expressed in the annual time series from 1990 to 2019. Except for High-income North America, the ASPR, ASIR, and ASYR in most GBD regions presented little change with increasing SDI values. At the global level, the ASPR, ASIR, and ASYR climbed slightly with increasing SDI values but under the expected levels during the past 30 years.
Figure 5.
The ASPR (a), ASIR (b), and ASYR due to GERD globally and for 21 GBD regions by SDI from 1990 to 2019. The expected age-standardized rates in 2019 based solely on SDI were represented by the black line. For each region, points from left to right depict estimates from each year from 1990 to 2019. ASIR: age-standardized incidence rate; ASPR: age-standardized prevalence rate; ASYR: age-standardized YLD rate; GBD: Global Burden of Disease; GERD: gastroesophageal reflux disease; SDI: socio-demographic index.
Discussion
In this study, we comprehensively analysed the trend in gastroesophageal reflux disease (GERD) burden in 204 countries and territories for the past two decades, and compared the trend between the last 20 years and 5 years. GBD 2019 incorporated more studies, providing the most updated estimates on GERD epidemiology. Besides, GBD 2019 made adjustments for case ascertainment and updated data sources to further improve data reliability. After these adjustments, our study confirmed that the overall burden continued to worsen with the prevalent cases increasing by 77.53% from 441.57 million in 1990 to 783.95 million in 2019. Although the age-standardized prevalence (ASPR) rate was stabilized globally, it increased in certain countries and territories. This changing trend could make implications for researchers and policy-makers to prepare clinicians and health care systems to prioritize management strategies.
In GBD 2019, the highest ASPR was observed in Latin America, the Caribbean, South Asia, North Africa and the Middle East (>12,000 cases per 100,000 population). East Asia and China had the lowest ASPR below 5%. Estimated average percentage change (EAPC) was used to evaluate the changing trend. EAPCs in age-standardized rates were highest in High-income Asia Pacific and lowest in High-income North America between 1990 and 2019. However, from 2015 to 2019, the EAPCs were highest in Eastern Europe, and the EAPC in ASPR was lowest in North Africa and Middle East, the EAPCs in ASIR and ASYR were lowest in Western Europe. The increasing disease burden in these regions could be associated with risk factors, including obesity, alcohol, and smoking [6].
There are previous studies on GERD burden. At the global level, GBD 2017 also reported stabilized ASPR and ASYR, without estimating the trend in ASIR from 1990 to 2017 [7]. Our data reported stabilized ASPR, and increased ASYR and ASIR from 1990 to 2019. ASPR, ASIR and ASYR all increased globally between 2015 and 2019. These data demonstrated the increasing trend of GERD burden in recent years. It was likely related to the obesity epidemic, which increased the odds up to 3-fold [17], and the decreasing prevalence of Helicobacter pylori-associated gastritis [4]. Eusebi et al. [6] reported higher estimates in America and the Middle East and lower estimates in East Asia. The estimate of East Asia was substantially below 5% in our study and several other studies. A survey showed the prevalence in five regions in China ranged from 1.7% to 5.1%, and Shanghai at 6.4% [18,19]. Another study reported an increase in Korea [20]. The prevalence in the US previously reported ranged from 10% to 30% [21–23], which was generally higher than GBD 2019 reported. The estimates previously reported were largely based on the population in Olmsted County or employed polulation [21, 24,25], which was less representative of the current US demographics, or potential responders who have GI symptoms [22]. GBD 2019 has incorporated more studies after and is more generalized. Besides, the criteria in some previous studies [21] were relatively generous as heartburn or regurgitation for at least one day per week. The GERD definition used in our study is from expert recommendation [26] and is consistent with a previous study [6], at least once per week for 12 months, overcoming the potential overestimation. Overall, our data were largely in line with previous studies.
Our study showed that advancing age was associated with an increased risk of GERD, and women had slightly higher rates of GERD, which was consistent with a previous study [6]. Eusebi et al. reported an effect of the geographical region on the association between GERD and gender, and it is more likely to be observed in women from South America, Southeast Asia, and the Middle East. Advancing age was non-constantly associated with GERD symptoms [4].
There are several limitations and strengths. One of the limitations is significant heterogeneity between studies included. There are cultural, ethnic, and geographic differences in the same region between different studies [27]. High-quality studies well-matched in location and population should be performed in future rounds. Moreover, the variability in study design and data collection methods also affects the precision of the estimates. Prevalence could be higher when the survey focussed on gastrointestinal symptoms, or through a postal questionnaire [6, 22]. This is only partially compensated in our analysis model. Furthermore, diagnostic criteria have a significant impact like mentioned before [28]. Our study used criteria consistent with expert consensus recommendations and a previous meta-analysis. Our data are largely consistent with previous studies, suggesting the validation of our study. Additionally, the association between different risk factors and GERD should be included in the future.
To our knowledge, this is the most updated estimate on GERD epidemiology globally, including 204 countries some of which were not been assessed before. EAPC was used to describe the trend over time. YLDs were used to quantitatively describe the negative impact of GERD on patients’ life and potentially could be an indicator of disease control. It included more studies and compensated for the study heterogeneity. Hence, the data reported should be more representative of individuals.
GERD remains to have a significant impact on the economic burden as a result of increasing prevalent cases globally. ASPR was stabilized globally, and ASIR and ASYR were slightly increased. Due to the negative impact of GERD on patients’ life quality [29], the association between GERD and increased risk of oesophageal adenocarcinoma [2, 30] and potential side effects of PPIs usage in treatment[31], More research on exploring certain risk factors, pathophysiology, and novel therapeutic strategies of GERD should be performed in the future.
Supplementary Material
Acknowledgements
The authors thank all members of the IHME, and Bill & Melinda Gates Foundation which support the related GBD 2019 studies.
Glossary
Abbreviations
- EAPC
estimated annual percentage change
- GERD
gastroesophageal reflux disease
- SDI
socio-demographic index
- GBD
Global Burden of Disease, Injuries, and Risk Factors Study
- YLDs
years of life lived with disability
- IHME
Institute for Health Metrics and Evaluation
- GATHER
Guidelines for Accurate and Transparent Health Estimates Reporting
- ASR
age-standardized rate
- ASIR
age-standardized incidence rate
- ASPR
age-standardiZed prevalence rate
- ASYR
age-standardiZed YLD rate
- UI
uncertainty interval
- CI
confidence interval.
Funding Statement
This work was supported by the Natural Science Foundation of Changsha City [kq2014266].
Ethical approval and consent to participate
The institutional review board of the Third Xiangya Hospital of Central South University in Hunan Province, China, determined that the study did not need approval because it used publicly available data.
Author contributions
Study concept and design: Rui Wang and Decai Zhang. Acquisition of data: Shaojun Liu. Data analysis and interpretation: Decai Zhang, Zhaoqi Li, and Rui Wang. Drafting the manuscript: Rui Wang and Decai Zhang. Critical revision of manuscript: all authors. All authors had full access to all the data in the study and had final responsibility for the decisions to submit for publication.
Disclosure statement
The authors declare no conflict of interest.
Data availability statement
The data were obtained through an online query tool from the website of IHME (http://ghdx.healthdata.org/), and no permissions were required to access the data.
References
- 1.Katz PO, Dunbar KB, Schnoll-Sussman FH, et al. . ACG clinical guideline for the diagnosis and management of gastroesophageal reflux disease. Am J Gastroenterol. 2022;117(1):–. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Maret-Ouda J, Markar SR, Lagergren J.. Gastroesophageal reflux disease: a review. JAMA. 2020;324(24)–1384. [DOI] [PubMed] [Google Scholar]
- 3.Fass R, Boeckxstaens GE, El-Serag H, et al. . Gastro-oesophageal reflux disease. Nat Rev Dis Primers. 2021;7(1):1372. [DOI] [PubMed] [Google Scholar]
- 4.Richter JE, Rubenstein JH.. Presentation and epidemiology of gastroesophageal reflux disease. Gastroenterology. 2018;154(2):267–276. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Katzka DA, Kahrilas PJ.. Advances in the diagnosis and management of gastroesophageal reflux disease. BMJ. 2020;371:m3786. [DOI] [PubMed] [Google Scholar]
- 6.Eusebi LH, Ratnakumaran R, Yuan Y, et al. . Global prevalence of, and risk factors for, gastro-oesophageal reflux symptoms: a meta-analysis. Gut. 2018;67(3):430–440. [DOI] [PubMed] [Google Scholar]
- 7.Collaborators GBDG-oRD The global, regional, and national burden of gastro-oesophageal reflux disease in 195 countries and territories, 1990-2017: a systematic analysis for the global burden of disease study 2017. Lancet Gastroenterol Hepatol. 2020;5:561–581. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Galmiche JP, Hatlebakk J, Attwood S, et al. . Laparoscopic antireflux surgery vs esomeprazole treatment for chronic GERD: the LOTUS randomized clinical trial. JAMA. 2011;305(19):1969–1977. [DOI] [PubMed] [Google Scholar]
- 9.Schindlbeck NE, Klauser AG, Berghammer G, et al. . Three year follow up of patients with gastrooesophageal reflux disease. Gut. 1992;33(8):1016–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Zheng Z, Shang Y, Wang N, et al. . Current advancement on the dynamic mechanism of gastroesophageal reflux disease. Int J Biol Sci. 2021;17(15):4154–4164. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Collaborators GBDD Global age-sex-specific fertility, mortality, healthy life expectancy (HALE), and population estimates in 204 countries and territories, 1950-2019: a comprehensive demographic analysis for the global burden of disease study 2019. Lancet. 2020;396:1160–1203. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Vos T, Lim SS, Abbafati C, Diseases GBD, et al.. Global burden of 369 diseases and injuries in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396(10258):1204–1222. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Collaborators GBDUHC. Measuring universal health coverage based on an index of effective coverage of health services in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396:1250–1284. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Collaborators GBDRF. Global burden of 87 risk factors in 204 countries and territories, 1990-2019: a systematic analysis for the global burden of disease study 2019. Lancet. 2020;396:1223–1249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deng Y, Zhao P, Zhou L, et al. . Epidemiological trends of tracheal, bronchus, and lung cancer at the global, regional, and national levels: a population-based study. J Hematol Oncol. 2020;13(1):98. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Stevens GA, Alkema L, Black RE, (The GATHER Working Group), et al.. Guidelines for accurate and transparent health estimates reporting: the GATHER statement. Lancet. 2016;388(10062):e19–e23. [DOI] [PubMed] [Google Scholar]
- 17.Corley DA, Kubo A.. Body mass index and gastroesophageal reflux disease: a systematic review and meta-analysis. Am J Gastroenterol. 2006;101(11):2619–2628. [DOI] [PubMed] [Google Scholar]
- 18.He J, Ma X, Zhao Y, et al. . A population-based survey of the epidemiology of symptom-defined gastroesophageal reflux disease: the systematic investigation of gastrointestinal diseases in China. BMC Gastroenterol. 2010;10(1):94. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Zou D, He J, Ma X, et al. . Epidemiology of symptom-defined gastroesophageal reflux disease and reflux esophagitis: the systematic investigation of gastrointestinal diseases in China (SILC). Scand J Gastroenterol. 2011;46(2):133–141. [DOI] [PubMed] [Google Scholar]
- 20.Kim KM, Cho YK, Bae SJ, et al. . Prevalence of gastroesophageal reflux disease in korea and associated health-care utilization: a national population-based study. J Gastroenterol Hepatol. 2012;27(4):741–745. [DOI] [PubMed] [Google Scholar]
- 21.El-Serag HB, Sweet S, Winchester CC, et al. . Update on the epidemiology of gastro-oesophageal reflux disease: a systematic review. Gut. 2014;63(6):871–880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Delshad SD, Almario CV, Chey WD, et al. . Prevalence of gastroesophageal reflux disease and proton pump inhibitor-refractory symptoms. Gastroenterology. 2020;158(5):1250–1261 e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nirwan JS, Hasan SS, Babar ZU, et al. . Global prevalence and risk factors of gastro-oesophageal reflux disease (GORD): systematic review with Meta-analysis. Sci Rep. 2020;10(1):5814. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.El-Serag HB, Petersen NJ, Carter J, et al. . Gastroesophageal reflux among different racial groups in the United States. Gastroenterology. 2004;126(7):1692–1699. [DOI] [PubMed] [Google Scholar]
- 25.Locke GR, 3rd, Talley NJ, Fett SL, et al. . Prevalence and clinical spectrum of gastroesophageal reflux: a population-based study in Olmsted county, Minnesota. Gastroenterology. 1997;112(5):1448–1456. [DOI] [PubMed] [Google Scholar]
- 26.Vakil N, van Zanten SV, Kahrilas P, Global Consensus Group, et al.. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am J Gastroenterol. 2006;101(8):1900–1920; quiz 1943. [DOI] [PubMed] [Google Scholar]
- 27.Spechler SJ, Jain SK, Tendler DA, et al. . Racial differences in the frequency of symptoms and complications of gastro-oesophageal reflux disease. Aliment Pharmacol Ther. 2002;16(10):1795–1800. [DOI] [PubMed] [Google Scholar]
- 28.Camilleri M, Dubois D, Coulie B, et al. . Prevalence and socioeconomic impact of upper gastrointestinal disorders in the United States: results of the US upper gastrointestinal study. Clin Gastroenterol Hepatol. 2005;3(6):543–552. [DOI] [PubMed] [Google Scholar]
- 29.Liker H, Hungin P, Wiklund I.. Managing gastroesophageal reflux disease in primary care: the patient perspective. J Am Board Fam Pract. 2005;18(5):393–400. [DOI] [PubMed] [Google Scholar]
- 30.Lagergren J, Bergstrom R, Lindgren A, et al. . Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. N Engl J Med. 1999;340(11):825–831. [DOI] [PubMed] [Google Scholar]
- 31.Moayyedi P, Eikelboom JW, Bosch J, COMPASS Investigators, et al.. Safety of proton pump inhibitors based on a large, Multi-Year, randomized trial of patients receiving rivaroxaban or aspirin. Gastroenterology. 2019;157(3):682–691 e2. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
The data were obtained through an online query tool from the website of IHME (http://ghdx.healthdata.org/), and no permissions were required to access the data.