Abstract
Objectives
Increased likelihood of having step children among more recent cohorts of older adults, alongside lower levels of assistance from step children, has led to concerns about greater unmet needs for older parents in step families. However, few studies have directly examined family structure and unmet needs. We examined the associations between having step children (vs. only biological children) and receiving care from adult children, and unmet needs for assistance.
Methods
Using the 2015 National Health and Aging Trends Study, we investigated among older parents with care needs whether levels of care received from adult children and unmet needs differed between those with biological versus step families. We also explored whether a partner or paid care compensated for observed differences.
Results
Older parents in need of care were more than twice as likely to receive care from their adult children if they had biological instead of step families. Unmet needs among older parents did not differ by family structure, nor did levels of partner or paid care.
Discussion
Results illustrate that concerns about the implications of the rising prevalence of step families for care parents receive from their children may be warranted. However, there is a lack of evidence of greater unmet need for care for older parents in step families, as risks of unmet needs are high for older parents regardless of family type.
Keywords: Adult children, Caregiving, Family structure, Parents, Step families
In the United States, family members—particularly partners and adult children—have served as frontline caregivers for older adults who have activity limitations (Schulz & Eden, 2016). Yet, as the U.S. population continues to age, family systems also have been changing in size and composition, particularly with respect to children. Older parents today have fewer biological children and more step children than in prior decades (Agree, 2018; Seltzer, 2019; Wiemers et al., 2019). Roughly one in eight older adults with activity limitations has a step child (Lin, 2008a), and the number of older adults with both biological and step children is projected to grow (Wachter, 1997).
Disability and care needs of older adults increase with age (Freedman & Spillman, 2014) as does receipt of family care (Freedman & Wolff, 2020; Schulz & Eden, 2016). Increases in life expectancy, along with reduced family size, have already led to an increase in the proportion of adult children providing care to an aging parent (Metlife Mature Market Institute, 2011). Aging adults often expect spouses and biological children to care for them (Abrahamson et al., 2017), but filial obligations of step children are less clear, and their ties to stepparents may depend on whether their parent and stepparent remain married (Coleman et al., 2005; Ganong & Coleman, 1998; Noël-Miller, 2013a).
Consequently, recent and impending demographic shifts are likely to have important implications for assistance and care provided to older parents (Seltzer, 2019). Studies focused on intergenerational transfers have documented that among couples with children having a stepchild is associated with being less likely to receive time help from any children (Wiemers et al., 2019). Because studies find lower levels of transfers or care within step families, scholars and policymakers are concerned that a step family disadvantage—in terms of being less likely to receive care from children—will result in more unmet care needs. This assumption has yet to be examined empirically. In addition, adult children are only one potential source of care and parents may opt for care from a spouse or cohabiting partner or from a paid caregiver as an alternative for care from offspring.
Using the 2015 National Health and Aging Trends Study (NHATS), we examine family structure, care received, and unmet needs of older parents (aged 65 and older) who receive or need care because of their health or functioning. We consider both caregiving received as well as unmet care needs to assess gaps in care received by older Americans in biological, nonstepfamilies and those in step families. We focus on a sample of older parents for whom detailed physical and cognitive health needs are measured to take into account potential family structure differences in parents’ need for care. Additionally, we examine other sources of care (spouse/partner and paid nonfamily care) as alternative “care buffers” for older parents with step families.
Family Structure, Care, and Unmet Needs of Older Parents
Family systems theory is a useful framework for understanding older parents’ family composition and its association with the care they receive (Bronfenbrenner, 1986; Cox & Paley, 2003; Fingerman & Bermann, 2000). This theory emphasizes the family as an ecological setting within which the connections among all individuals in the family influence outcomes rather than focusing on individual dyads. Thus, by characterizing the family system available to older parents, one can better understand the balance of resources and obligations accessible to and expected from members (Bronfenbrenner, 1977, 1986). A family systems approach also sheds light on potential sources of diffusion of care responsibilities (Darley & Latané, 1968; Lin & Wu, 2019). An early application of family systems theory to caregiving was proposed by Cantor and Little (1985), who postulated that there is a hierarchy in the selection of caregivers, with close kin—notably spouses and children—favored over other relatives, friends, and neighbors. Empirical studies have provided evidence consistent with this theory, with spouses preferred over children among married older adults (Agree & Glaser, 2009), but extensions to more complex family configurations have been lacking.
Step families are a growing phenomenon among older adults with a substantial share of older couples with children in step families (40%; Lin et al., 2018). Step families are more common today because of increasing rates of gray divorce, whereby adults divorce at older ages (Brown & Lin, 2012), which can lead to repartnering later in life (Brown et al., 2019). Step family members may not share with each other the same understandings of obligations because some members are newer to the family constellation or because of competing obligations between biological children from previous unions or a child’s other biological parent and those in the step family. The overlapping of family boundaries creates ambiguity or conflict for some step family members (Cherlin, 1978; Seltzer, 2019). Consistent with this theoretical view, parents in step families feel less close with their biological children than parents who have no step children (Steinbach & Hank, 2016), and parents have less contact with their biological children if they are a part of a step family compared to a biological family (van der Pas & van Tilburg, 2010). This legacy of divorce within a family may alter ties with biological children and necessitate a greater need for care from step children.
The literature on intergenerational transfers, or family exchanges of time and money, provides insight into the role of family structure (Pezzin et al., 2008; Wiemers et al., 2019). Time transfers in this context include those related to the health and functioning of the older adult (i.e., caregiving) as well as other types of assistance (Freedman & Wolff, 2020). Intergenerational transfers are generally less likely within step families compared to biological families (Kalmijn et al., 2019; Wiemers et al., 2019). Pezzin et al. (2008), for example, find that family disruption, including divorce and remarriage, has a negative impact on child-to-parent time transfers for unpartnered older adults with limitations.
Studies focused on family care also provide relevant insights. Although many older adults report receiving care from only one adult child, the proportion of children helping their parents increases with parents’ frailty (Lin & Wolf, 2020). Among older parents with limitations, family size is positively associated with receiving care from children (Grundy & Read, 2012). Wolf (2014) finds among unpartnered older adults that having more children is associated with having more helpers (although not with having any helpers).
Studies of care differentials implicitly assume that when older adults receive less care from a particular source, there are more unmet care needs. Yet studies that directly test whether there are gaps in unmet needs between older parents in step families compared to biological families are needed. Unmet care needs, such as not being able to get out of bed or not having clean clothes to wear, are a negative consequence of receiving inadequate care (Allen & Mor, 1997). Measures of unmet need differ from care expectation gaps, in which an older adult expects one person to help but that person does not help (Abrahamson et al., 2017). Almost half (44.3%) of older adults in the U.S. report having at least one unmet need related to self-care, mobility, or household activities in the past month (Beach & Schulz, 2017). Having unmet care needs may lead to additional adverse consequences for older adults, including nursing home admission and mortality (Allen & Mor, 1997; He et al., 2015).
Alternative Sources of Support in Later Life
Because they recognize that step family members’ responsibilities for care may be weaker than in biological families, aging parents may prepare for less care by diversifying their care networks or calling upon their partner or paid caregivers for more support. Diffusion of responsibility theory would suggest that adult children will be less likely to care for parents who have access to a spouse or paid caregiver (Lin & Wu, 2019).
Older adults who are partnered and need care often receive care from their partner. Yet, it is unclear how these dynamics may play out in step families as studies often only examine unpartnered older adults (Pezzin et al., 2008; Wolf, 2014). Older parents with step families may be more likely to be partnered and therefore receive care from a partner caregiver. In Noel-Miller’s (2013a) analysis of stepparent–child dyads almost 88% of the parents were married or repartnered. Partners are more likely to provide assistance with self-care or mobility tasks than children and more likely to provide assistance with self-care, mobility, and/or household chores than even coresident children (McGarry, 1998). Because of the innate hierarchy in the selection of caregivers, patterns of care given by adult children may be distinct for partnered and unpartnered parents.
Some older parents may turn to paid sources for assistance. In 2011, about a third of older adults with one or more activity limitations received assistance from a paid caregiver, the vast majority in community settings (Freedman & Spillman, 2014). The research on paid care is mixed as to whether paid and unpaid care are substitutes or supplements (Hanley et al., 1991; Pickard, 2012; Pinquart & Sörensen, 2002). A recent study suggests that when residential care is more accessible, children are less likely to provide care (Van Den Broek & Dykstra, 2017), supporting diffusion theory interpretations of the association between paid care and care from children. Studies have not focused, however, on whether paid care is more likely to be used by older parents embedded in step families to alleviate unmet needs. Hence, it remains unclear as to whether paid care is instrumental in bridging any differences in care and unmet need for step and biological families.
The current study contrasts two common family compositions—having only biological children (henceforth, “biological family”) versus having any step children (i.e., “step family”)—to answer three questions: Do older parents who need care receive less care from children if the older parent has any step children? Are risks of unmet needs greater for older parents with any step children? Do spouses/partners and paid caregivers provide more assistance and buffer unmet care needs in families with any step children?
Data and Methods
We used the 2015 NHATS, an ongoing national panel study that is representative of the U.S. Medicare population aged 65 and older. NHATS was sponsored by the National Institute on Aging (grant number NIA U01AG32947) and was conducted by the Johns Hopkins University (NHATS, n.d.). The initial 2011 sample was drawn from Medicare enrollment files, and sample members have been interviewed annually since 2011. NHATS oversampled adults at older ages and Black older adults (Freedman & Kasper, 2019). The sample was refreshed in 2015, including the addition of a sample of beneficiaries who turned 65 since 2011, making the 2015 NHATS representative of the Medicare population aged 65 and older when sampling weights are used. The 2015 NHATS had an overall unweighted response rate of 76% (96% for continuing sample; 63% for replenishment) for a total sample of 8,334 older adults (DeMatteis et al., 2016).
We limited our sample to older adults who did not reside in a nursing home but were in need of care for health- or functioning-related reasons. We defined the need for care as living in a residential care setting (other than a nursing home) and receiving care from someone in the facility; receiving care from anyone with self-care or mobility or with household tasks for health or functioning-related reasons; or having at least one unmet care need for any of these tasks (N = 2,646). We further limited our main sample to older adults who reported having at least one living child (i.e., biological or step child), aged 18 or older, at the time of the survey (N = 2,424). For analyses of hours of care, we included only cases for which there was complete information about hours for all children (N = 1,088); sensitivity analyses with imputed hours showed similar results. Missing data for control variables were rare except for some adult child characteristics and the parent’s individual capacity measures. We performed chained multiple imputations on missing control variables for both the older parent and adult children (M = 25), including multiple auxiliary variables in our imputation models (e.g., region). All information used in the analyses was reported by the older adult or a proxy respondent (n = 380 proxies, of which 223 were biological children and one was a step child). Including an indicator for whether there was a child proxy does not alter our conclusions. All analyses were weighted and adjusted for survey design (Kasper & Freedman, 2020).
Primary Independent Variable
The key independent variable in this analysis distinguished between NHATS participants who had only biological children and those with any step children based on the rosters of all living children collected when a participant was first interviewed. Participants were asked to list their own (and if partnered, their partner’s) children, including any step children. Relationship for each child was recorded as daughter or stepdaughter, for instance. In each subsequent round, each child’s status was updated (e.g., marked deceased if no longer living), and new step children were added to the roster if the participant repartnered.
Dependent Variables
We analyzed four sets of dependent variables: care from adult children (any and hours), unmet needs, care from paid caregivers (any and hours), and care from a partner (any and hours).
Any care from adult children was defined as assistance in the last month with self-care, mobility, or household activities for health or functioning reasons. Self-care activities included bathing, dressing, eating, and toileting; mobility activities included getting out of bed, getting around inside, and getting outside; and household activities included laundry, shopping, making hot meals, managing money, and managing medications. For household tasks, a follow-up question asked if the reason that care was received was for health or functioning reasons or another reason; we only included care received for health or functioning reasons. For each activity, respondents were asked to report who helped and, if not already ascertained, that individual’s relationship to the NHATS respondent.
We define total hours of care from adult children, for those who received any, as the total for all adult children with positive hours. We use the NHATS-derived variable, which calculates hours of care in the last month for each caregiver based on a series of questions about each caregiver’s schedule, the number of days per week or month, and the number of hours per day on days when care was provided.
The second set of dependent variables captured unmet needs in the past month. NHATS asked respondents directly about experiencing consequences as the result of not having particular help (Kasper & Freedman, 2020). Respondents were asked, for example: “In the last month, did you ever go without [consequence] because it was too difficult to do by yourself/no one was there to help or do that for you?” Consequences included self-care (i.e., go without a shower/bath, not get dressed, go without eating, wet or soil clothing), mobility (i.e., have to stay in bed, or inside, did not go somewhere wanted to), or household (i.e., go without clean laundry, groceries/personal items, a hot meal, handling bills/banking, missed medicines).
To examine differential substitution between family and paid care by family type, we also explored whether the older parent received any paid care in the past month and total paid caregiver hours, if they received any. We included in the definition of any paid care: assistance from a paid aide, housekeeper, employee, or service/someone from the place that the respondent lives for any kind of care. Because numbers of hours were not collected for helpers from the place the respondent lives, analyses of total paid care hours were limited to the hours from other paid sources (paid aide, housekeeper, employee). Finally, we explored for older parents who were married or cohabiting whether they received any partner care in the last month for self-care, mobility, or household activities related to health or functioning, and total partner care hours received, if any, where care was defined as it was for adult children.
Control Variables
For family structure variables, we treated union status as a categorical variable (i.e., married/living with a partner, and among those unpartnered whether separated/divorced/never married, or widowed) and the number of children as a continuous variable. We logged total income (individual’s income if single, joint if partnered) using the income imputations provided by NHATS. Education was categorized as less than high school degree, high school degree, vocational degree/some college/associate’s degree, and bachelor’s degree or higher. We also controlled for a series of demographic characteristics. Race and ethnicity were specified as four mutually exclusive categories: White, non-Hispanic; Black, non-Hispanic; Hispanic; and Other, non-Hispanic. If the respondent indicated more than one race, we used their primary identification. We also controlled for whether the older parent was female and three age categories (65–74, 75–84, and 85 and older).
Given our focus on older parents with care needs, we also controlled for a series of health-related items. We included a positive self-rating of health (good/very good/excellent vs. fair/poor). We also controlled for the number of chronic health conditions the respondent had ever had (i.e., heart attack, heart disease, high blood pressure, arthritis, osteoporosis, diabetes, lung disease, stroke, cancer, or other illness not mentioned). To measure depression/anxiety, we used the Patient Health Questionnaire-4 (i.e., sum of little interest/pleasure, felt down/depressed/hopeless, felt nervous/anxious/on edge, unable to stop/control worry). Higher scores indicate worse mental health (Löwe et al., 2010). We also controlled for a summary measure of physical capacity where a higher score indicates greater physical ability, by combining scores for each of the five physical performance tests and six self-reported items into one total score (Freedman et al., 2011; Kasper et al., 2017; Kasper & Freedman, 2020). We classified individuals as having probable dementia or not, based on reports of diagnosis, an informant dementia screen, and a series of tests measuring memory, orientation, and executive functioning (Kasper et al., 2013).
Control variables also include characteristics of the older parent’s adult children, those 18 years or older. These controls include whether the older parent had any daughters, any children younger than 45 years, any children with a college degree, any unpartnered children, and any children with children of their own younger than 18.
Analytic Plan
First, we provided a description of the analytic sample characteristics, overall and by family type (biological vs. step families). Second, overall and by family type, we estimated the percentage receiving any care from a child, mean number of hours from children among those who received any care, percentage with any unmet needs, and percentage with any paid caregivers. Third, we estimated logistic regression models for any care received from children, ordinary least squares regression models for number of care hours received from children if any, and logistic regression models for any unmet needs and any paid care. Corresponding adjusted predicted percentages and average hours by family type based on the main regressions with controls held at their mean values were also calculated. Fourth, we estimated adjusted predicted values by family type of any care from children, hours from children, any unmet needs, and any paid care by parent’s partnership status. For those with partners, we also calculated the predicted percentage of any partner care and average care hours from partner if they received any partner care.
We conducted several supplemental analyses to assess the robustness of our findings about step–biological family differences. We disaggregated two outcomes—any care from children and any unmet needs—to predict separately self-care, mobility, and household activities. We also considered two additional control variables: whether any of the adult children were members of the older parent’s household and whether the parent lived in a residential care setting. Because decisions about proximity and care setting may reflect choices to facilitate contact and care, we omit these measures from our main analysis to avoid overcontrolling for differences between biological and step families.
Results
Among older parents in the United States who were in need of care, 14.2% had at least one step child, and 85.8% had only biological children (Table 1). Compared to older parents with only biological families, older parents with step families had more children, were more likely to have a spouse or cohabiting partner, were younger, had greater physical capacity scores, and were less likely to have dementia. A greater percentage of older parents with step families were men and their incomes were higher on average.
Table 1.
Weighted Descriptive Statistics, for Full Sample and by Family Type (Mean or Percentage)
| Full sample | Biological family | Step family | Difference p < .05 | |
|---|---|---|---|---|
| 100.0% | 85.8% | 14.2% | ||
| Older parent characteristics | ||||
| Number of children | 3.3 | 3.1 | 4.5 | * |
| Union status | ||||
| Married/living with partner | 48.7 | 44.8 | 71.7 | * |
| Separated/divorced/never married | 14.8 | 16.2 | 6.5 | * |
| Widowed | 36.5 | 39.0 | 21.8 | * |
| Race/ethnicity | ||||
| White, non-Hispanic | 74.7 | 74.0 | 78.9 | |
| Black, non-Hispanic | 10.9 | 11.5 | 7.4 | |
| Hispanic | 9.1 | 9.4 | 6.8 | |
| Other, non-Hispanic | 5.4 | 5.1 | 6.9 | |
| Female | 63.8 | 66.9 | 45.7 | * |
| Age | ||||
| 65–74 | 38.2 | 35.7 | 53.1 | * |
| 75–84 | 35.0 | 36.0 | 29.4 | |
| 85+ | 26.8 | 28.3 | 17.5 | * |
| Family income ($) | 44,934.4 | 43,124.9 | 55,852.1 | * |
| Education | ||||
| Less than high school | 24.8 | 24.9 | 24.3 | |
| High school degree | 31.2 | 32.3 | 25.5 | |
| Vocational/some college/AA/AS | 24.3 | 23.9 | 26.3 | |
| Bachelor’s degree or higher | 19.6 | 18.9 | 24.0 | |
| Positive self-rated health | 53.6 | 53.4 | 54.5 | |
| Depression/anxiety score | 7.1 | 7.1 | 7.3 | |
| Physical capacity score | 1.2 | 1.1 | 1.4 | * |
| Dementia status | ||||
| Probable dementia | 24.0 | 25.2 | 17.0 | * |
| Possible dementia | 13.0 | 13.0 | 13.3 | |
| No dementia | 63.0 | 61.8 | 70.0 | |
| Adult child (18+) characteristics | ||||
| Any daughters | 83.8 | 82.3 | 92.5 | * |
| Any children younger than 45 years | 40.7 | 38.3 | 54.8 | * |
| Any children with a college degree | 55.0 | 54.5 | 58.8 | |
| Any unpartnered children | 62.3 | 60.2 | 75.4 | * |
| Any children have children | 56.3 | 54.4 | 67.3 | * |
| N | 2,424 | 2,125 | 299 |
Notes: AA/AS = associate’s degree (Associate of Arts/Associate of Science). National Health and Aging Trends Study (NHATS) respondents who needed care for health or functioning reasons and had any children aged 18 or older. Weighted by NHATS analytic and clustering weights. Percentages may not sum to 100% due to rounding. *p <.05.
Among the full sample, less than half (44.9%) of older parents in need of care received care from their adult children in the prior month (Table 2). The average number of hours of care in the last month among those who reported receiving any care from children was 98.6 h, just under 25 h per week. About half (51.1%) of older parents in need had an unmet need, more than one third (38.7%) received care from a partner, and one quarter (25.3%) received paid care.
Table 2.
Weighted Unadjusted Descriptives of Receiving Care from Children, Hours of Care, Unmet Need, Receiving Care from Partner, and Receiving Paid Care in the Last Month by Family Type
| Received any care from adult children (%) | Average hours of care received from adult children, if any care from adult children (#) | Had any unmet needs (%) | Received any partner care (%) | Received any paid care (%) | |
|---|---|---|---|---|---|
| Full sample | 44.9 (1.3) | 98.6 (5.6) | 51.1 (1.2) | 38.7 (1.1) | 25.3 (1.3) |
| Family type | |||||
| Biological family | 48.6 (1.4) | 99.2 (6.0) | 50.9 (1.3) | 35.3 (1.3) | 26.7 (1.5) |
| Step family | 22.5a (2.9) | 91.5 (19.7) | 52.4 (2.9) | 59.7a (3.3) | 16.7a (2.4) |
| N | 2,424 | 1,088 | 2,424 | 2,424 | 2,424 |
Notes: National Health and Aging Trends Study (NHATS) respondents who needed care for health or functioning reasons and had any children aged 18 or older. Weighted by NHATS analytic and clustering weights. Standard errors in parentheses.
aSignificantly different from older parents with only biological children, p < .05.
The percentage receiving care from children was more than twice as high for older parents in families with only biological children compared to step families (48.6% vs. 22.5%; p < .05). Among those who received care from a child, parents with only biological children received slightly more hours per month than parents with a step child, but the difference was not statistically significant. Although older parents in step families were less likely to have received care from a child, unmet need was not significantly more common among them; about half of parents in both groups reported unmet needs. Older parents with step families were more likely than those with biological families to receive help from a partner (59.7% vs. 35.3%; p < .05); we explore differences among partnered older parents in Table 4. Older parents with biological families were more likely than those with step families to report receiving paid care (26.7% vs. 16.7%; p < .05), despite biological parents’ greater likelihood of receiving care from children.
Table 4.
Predicted Outcomes of Receiving Care From Children, Hours of Care, Unmet Need, Receiving Care From Partner, and Receiving Paid Care in the Last Month by Family Type, Stratified by Partnership Status
| Received any care from adult children (%) | Hours of care received from adult children, if any care from adult children (#) | Had any unmet needs (%) | Received any paid care (%) | Received any partner help (%) | |
|---|---|---|---|---|---|
| Unpartnered | |||||
| Family type | |||||
| Biological family | 71.0 (1.7) | 105.1 (5.9) | 55.4 (2.0) | 33.0 (2.1) | n.a. |
| Step family | 53.7a (6.7) | 100.2 (24.6) | 45.9 (7.3) | 33.0 (5.8) | n.a. |
| N | 1,455 | 861 | 1,455 | 1,455 | n.a. |
| Partnered | |||||
| Family type | |||||
| Biological family | 19.9 (2.1) | 82.4 (9.3) | 47.5 (2.3) | 9.9 (1.3) | 81.2 (1.9) |
| Step family | 6.0a (1.6) | 70.9 (21.2) | 49.2 (4.7) | 8.5 (2.2) | 86.4 (2.8) |
| N | 969 | 227 | 969 | 969 | 969 |
Notes: National Health and Aging Trends Study (NHATS) respondents who needed help for health or functioning reasons and had any children aged 18 or older. Weighted by NHATS analytic and clustering weights. Standard errors in parentheses. Models control for all control variables except union status. n.a., not applicable.
aSignificantly different from older parents with only biological children, p < .05.
Adjusting for characteristics of parents and their children, parents in biological families were more likely to have received care from a child than those with any step children (Table 3, Column 1). Among those receiving care from children, family type was not associated with the number of hours of care received from children (Table 3, Column 2). Stepparents and biological parents did not differ in the likelihood of having unmet needs (Table 3, Column 3). There also was no family type difference in the receipt of paid care once parent and family characteristics are taken into account (Table 3, Column 4). Findings with respect to family type for hours of paid care were similar to those for any care, that is, there is no step–biological family difference (Supplementary Appendix Table 1). Conclusions about family type differences were robust to the inclusion of an indicator of whether the parent lives with an adult child or in a residential care facility (Supplementary Appendix Tables 2 and 3).
Table 3.
Weighted Adjusted Regressions of Receiving Care From Children, Hours of Care, Unmet Need, and Paid Care in the Last Month
| Column 1 | Column 2 | Column 3 | Column 4 | |
|---|---|---|---|---|
| Logistic: received any care from adult children | OLS: hours of care received from adult children, if any care from adult children | Logistic: had any unmet needs | Logistic: received any paid care | |
| Family type | ||||
| Biological family | 1.110*** (0.224) | 3.953 (19.46) | −0.016 (0.165) | −0.009 (0.189) |
| Older parent characteristics | ||||
| Number of children | 0.172*** (0.045) | 7.007* (2.738) | 0.049 (0.036) | −0.065* (0.032) |
| Union status (married/living with partner omitted) | ||||
| Separated/divorced/never married | 1.157*** (0.193) | 18.520 (15.72) | 0.629** (0.203) | 1.454*** (0.207) |
| Widowed | 1.654*** (0.140) | 29.340* (13.49) | 0.308* (0.152) | 0.917*** (0.170) |
| Race/ethnicity (White, non-Hispanic omitted) | ||||
| Black, non-Hispanic | −0.005 (0.177) | 50.830*** (13.43) | −0.122 (0.164) | −0.406* (0.170) |
| Hispanic | −0.216 (0.266) | 35.580 (19.76) | 0.028 (0.235) | 0.038 (0.358) |
| Other, non-Hispanic | 0.443 (0.301) | 45.190 (23.17) | −0.083 (0.282) | −0.475 (0.374) |
| Female | 0.211 (0.166) | −12.630 (12.64) | −0.091 (0.164) | −0.355* (0.147) |
| Age (65–74 omitted) | ||||
| 75–84 | 0.177 (0.177) | −8.421 (16.95) | −0.031 (0.144) | 0.209 (0.167) |
| 85+ | 0.624** (0.199) | 9.622 (24.11) | −0.257 (0.165) | 0.690** (0.235) |
| Family income (logged $) | −0.117 (0.068) | 0.893 (1.680) | 0.050 (0.049) | 0.018 (0.065) |
| Education (less than high school omitted) | ||||
| High school degree | −0.087 (0.177) | 10.270 (14.88) | 0.078 (0.158) | 0.305 (0.196) |
| Vocational/some college/AA/AS | −0.312 (0.214) | 7.240 (17.69) | 0.278 (0.177) | 0.769*** (0.213) |
| Bachelor’s degree or higher | −0.355 (0.222) | −5.304 (16.67) | 0.536* (0.205) | 1.145*** (0.224) |
| Positive self-rated health | 0.017 (0.114) | −1.444 (11.11) | −0.375*** (0.106) | 0.126 (0.140) |
| Depression/anxiety score | −0.015 (0.025) | 0.732 (2.157) | 0.126*** (0.022) | −0.006 (0.021) |
| Physical capacity score | −1.103*** (0.125) | −30.61** (9.526) | −0.420*** (0.102) | −0.904*** (0.114) |
| Dementia status (probable omitted) | ||||
| Possible dementia | −0.695*** (0.152) | −94.29*** (15.50) | 0.127 (0.185) | −0.196 (0.162) |
| No dementia | −0.688*** (0.159) | −84.32*** (17.04) | 0.236 (0.144) | −0.647*** (0.128) |
| Adult child (18+) characteristics | ||||
| Any daughters | 0.478** (0.169) | 28.930* (13.31) | 0.0648 (0.159) | 0.062 (0.176) |
| Any children younger than 45 years | 0.141 (0.166) | −15.620 (13.65) | 0.259 (0.136) | −0.558** (0.189) |
| Any children with a college degree | −0.001 (0.123) | −7.126 (10.89) | 0.045 (0.126) | 0.309* (0.137) |
| Any unpartnered children | 0.557*** (0.158) | 14.230 (13.23) | −0.002 (0.132) | −0.244* (0.120) |
| Any children have children | −0.025 (0.129) | −2.822 (12.01) | 0.196 (0.105) | 0.146 (0.118) |
| Constant | −0.543 (0.917) | 84.360 (43.010) | −1.524* (0.614) | −0.874 (0.826) |
| N | 2,424 | 1,088 | 2,424 | 2,424 |
Notes: AA/AS = associate’s degree (Associate of Arts/Associate of Science); OLS = ordinary least squares. National Health and Aging Trends Study (NHATS) respondents who needed care for health or functioning reasons and had any children aged 18 or older. Weighted by NHATS analytic and clustering weights. Standard errors in parentheses.
***p < .001, **p < .01, *p < .05.
Several additional patterns with respect to covariates in Table 3 are noteworthy. First, number of children and whether any adult children were daughters were associated with receipt of any care from an adult child and hours of care received, but not unmet need. Second, only union status and physical capacity were associated with both care receipt and unmet need. Third, self-rated health and depression/anxiety scores were associated with unmet need, but not care receipt. Fourth, those with higher levels of schooling were more likely to receive paid care, but income was not associated with paid care.
Family type differences persisted in models that examined care from children and unmet needs separately by broad activity type (Supplementary Appendix Table 4). Specifically, older parents with biological families were more likely to receive help from adult children for each type of task, and the biological versus step family difference was substantial for each task, with adjusted coefficients in favor of biological versus step of 1.27 for self-care (p < .001), 0.68 for mobility assistance (p < .01), and 0.86 for household tasks (p < .001). As in the results given in Table 3, unmet needs did not differ significantly between those with biological only versus step families for any of the activity types.
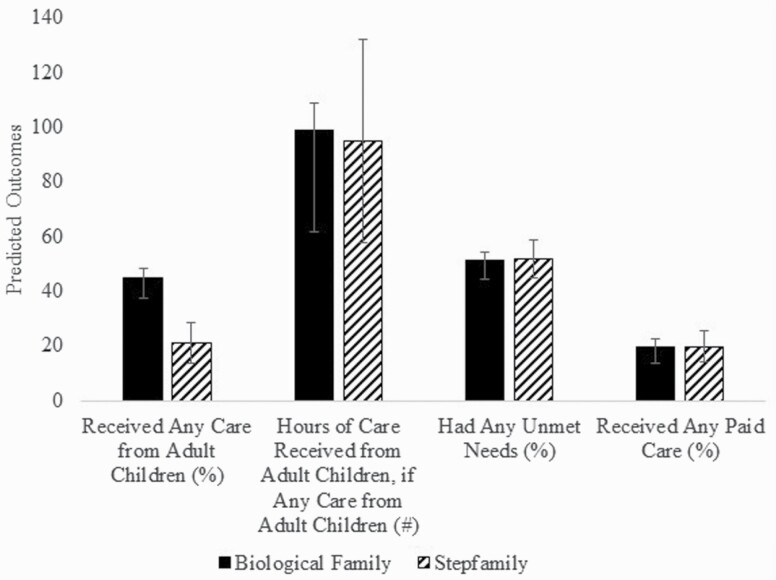
To facilitate interpretation, in Figure 1, we provide predicted adjusted outcomes by family type based on the multivariable models reported in Table 3. The predicted percentage of older parents with biological families receiving care was 45.1%, more than double that for older parents with step families (21.3%). Consistent with the model coefficients, among those receiving care from children, hours received from children were similar between the two family types. Additionally, there were no significant differences in unmet need or paid care after accounting for parent and child characteristics.
Figure 1.
Predicted outcomes by family type.
Finally, we reestimated the models in Table 3 stratified by whether the older parent was partnered or not (Supplementary Appendix Tables 5 and 6) to take into account that children may be more likely to assist their biological parent with caring for their other biological parent than with caring for their stepparent. We then used the results from the stratified models to calculate adjusted predicted percentages and hours (Table 4). Differences between biological and step families in receipt of care from children are substantial for both unpartnered and partnered parents. Among unpartnered parents, 71.0% received care from a child in biological families, whereas 53.7% did so in step families. Among partnered parents, 19.9% received care from a child in biological families compared to 6.0% in step families. In other words, consistent with estimates from the unstratified models, parents in biological families were more likely to have care from a child, regardless of partnership status. There were no significant differences between biological and step families in average hours, unmet need, or paid care among unpartnered parents or among partnered parents. Most parents who had a partner received care from that partner (81.2% biological and 86.4% step families), but even among those who were partnered, close to half had unmet needs. A comparison of the two panels of Table 4 shows that unpartnered parents are much more likely than partnered parents to receive care from a child within each family type. (Among those with a partner, there is no biological–step family difference in hours of care from a partner, if any partner care [Supplementary Appendix Table 1].)
Additional tests (Supplementary Appendix Table 7) show that the interaction between family type and whether the parent is partnered is not statistically significant in models of receiving any care from children, hours of care from children, unmet needs, or paid care. This suggests that the step family gap in receiving care from children is not altered by parents’ partnership status.
Discussion
The U.S. population continues to age and need care, and the likelihood of having stepkin also continues to increase across time (Agree, 2018). Changes in families of older adults have led to conclusions by scholars that older parents with step families may have greater risks of unmet needs due to weaker normative obligation and ties within these families. We test this hypothesis using a contemporary cohort of older parents with biological and step families.
We find a substantial “step gap” in care received from children. Older parents with biological families are more than twice as likely to get care from their adult children than older parents with step families. This finding holds true for each of the types of activities examined here (self-care, mobility, and household tasks). Parents in step families and biological families do not differ in the number of hours of care they receive from children, if they receive any care from children, unfortunately the data do not allow disaggregation of hours of care for the different types of tasks.
We also find that despite older adults in step families being much less likely to receive care from children, about half of older parents with care needs report unmet needs irrespective of family type. There is also no biological–step family difference in unmet need for particular types of tasks. Why there is no step family gap in unmet need is unclear. We found that despite the lower percentages receiving care from children, parents with step families were no more likely to receive paid care than parents with biological families, once other characteristics of parents and families were taken into account. We also explored whether older parents with step families were more likely to have partners providing care. We found that although older parents with a step family were more likely to be married or cohabiting, the step family gap in care persisted among those who were partnered. Although more family members may help if available, unmet needs remain high among all older parents regardless of family type.
Our estimates of unmet needs mirror other studies that have sampled high-need older adults, which found that about half of older adults experience negative consequences linked to unmet care needs (Beach et al., 2020). Those with more needs are likely to have more unmet needs (Dunatchik et al., 2019). Unmet needs may be high in our sample if older adults are hesitant to ask for more help even if needed (de São José et al., 2016). Also, some needs may be difficult to meet if there is no clear intervention (Curnow et al., 2021). Additional help from family caregivers might not be able to address an older parent’s unmet needs, especially if family caregivers do not have the training to perform needed tasks (Burgdorf et al., 2021). Future research should continue to investigate the association between unmet needs and care provided by family members.
Our findings regarding care received from children illustrate the enduring strength of biological ties between older parents and their children and echo previous research that shows that time transfers are less likely within step families (Wiemers et al., 2019). Filial obligation norms are stronger for biological parents compared to stepparents (Ganong & Coleman, 1998), and step children may be less inclined to care for aging stepparents due to weaker norms regarding roles within these families (Cherlin, 1978) or because of lack of reciprocity. For instance, step children are less likely than biological children to have received financial transfers from parents (Henretta et al., 2014). Our study takes a family systems approach to address larger concerns that older parents in step families may have greater unmet needs as a consequence of less assistance from children. Future research should investigate which children provide care by examining parent–child dyads within particular family systems (e.g., a biological child within a step family) to better understand the nuances of step family dynamics at older ages.
Our findings point to two other demographic phenomena that may affect care of aging parents. We found that parents in larger families are more likely to receive care from children and to receive more hours of care. Declining fertility may reduce the amount of care that parents receive. Parents who are married or cohabiting receive care from their partners, and when there is no spouse/partner, children provide more of the care their parents need. As education differences in the likelihood of forming and maintaining stable partnerships increase (McLanahan & Jacobsen, 2015; Perelli-Harris & Lyons-Amos, 2016), this may exacerbate existing inequalities in the receipt of needed care.
This study has limitations. First, we relied on the parent’s reports of care received. Reports on caregiving between parents and children sometimes diverge, with parents often underreporting how much they receive relative to children’s reports (Lin, 2008b; Lin & Wu, 2018). Therefore, our estimates of care received may be underestimated and unmet needs may be overestimated, although it is unclear if this bias would affect our findings about step versus biological families. Second, we relied on reports of family structure that may not fully capture step relationships from prior partnerships (i.e., “former step children”), and the data set used does not include historical information about the stepparent and step child ties (e.g., whether they ever lived together or age at which the step tie was established). Past research suggests that ties to a stepparent weaken substantially when the stepparent is no longer married or partnered with the child’s biological parent (Noël-Miller, 2013b), and the timing of the stepparent’s arrival in the child’s life may influence the quality of the relationship (Ganong & Coleman, 2018). As a result, our findings may not capture the full extent of step family differences in care from children. Third, due to the small number of step families in our analysis, we could not further distinguish among types of step families, for instance between families with only step children and those with a mix of biological and step children. Past research provides conflicting evidence on effects of variation in step family structure. Pezzin et al. (2008) found that the step–biological composition affects older parents’ receipt of care from children, but van der Pas and van Tilburg (2010) showed that contact between stepparents and step children does not differ between families in which both parents have children from a previous union and those in which only one parent has children from a previous union. Finally, our study shows that having a daughter is associated with increased care from adult children, but we were not able in this analysis to examine in detail the effects of parents’ and children’s gender. This is an important extension for future research.
Despite these limitations, our study has implications for both theoretical development and future research. Regarding family theory, we find support for thinking about the family as a system that responds to older parents’ care needs. Although step families may function differently from biological families, the effects of being in a step family may not be all negative. Our work supports other calls for more research on the variability of experiences for step families (Ganong & Coleman, 2018). Future research should examine differences among step families as the number of these families grows and survey sample sizes of different step family structures become larger. This research should also consider how step family structure affects which children in the family provide assistance to parents who need care. Lastly, the findings have important theoretical and empirical implications for older parents’ unmet needs. We find that there are few statistically significant differences in unmet needs when accounting for the full family system of the older parent. In particular, although older parents in step families compared to biological families are less likely to report receiving care from children, family type is not associated with older parents’ unmet needs. Future research should continue to tease apart important predictors of unmet needs, as results suggest they remain high among all older parents.
Supplementary Material
Contributor Information
Sarah E Patterson, Survey Research Center, University of Michigan, Ann Arbor, Michigan, USA.
Robert F Schoeni, Institute for Social Research, Ford School of Public Policy, Department of Economics, University of Michigan, Ann Arbor, Michigan, USA.
Vicki A Freedman, Institute for Social Research, University of Michigan, Ann Arbor, Michigan, USA.
Judith A Seltzer, Department of Sociology, California Center for Population Research, University of California, Los Angeles, Los Angeles, California, USA.
Funding
Funding was provided by the National Institute on Aging (R01AG054004; T32AG000221). The research was also supported, in part, by the California Center for Population Research at UCLA (CCPR), which receives core support (P2C- HD041022) from the Eunice Kennedy Shriver National Institute of Child Health and Human Development (NICHD). This paper was published as part of a supplement sponsored by the University of Michigan and the Johns Hopkins Bloomberg School of Public Health with support from the National Institute on Aging (U01AG032947 and P30AG012846).
Conflict of Interest
S. E. Patterson is the JGSS social media editor. All other authors declare no conflict of interest.
Acknowledgment
The views expressed are those of the authors alone and do not represent those of their employers or the funding agencies.
Author Contributions
S. E. Patterson, R. F. Schoeni, V. A. Freedman, and J. A. Seltzer planned the study, wrote and edited the paper; S. E. Patterson performed the statistical analyses.
References
- Abrahamson, K., Hass, Z., & Sands, L. (2017). Likelihood that expectations of informal care will be met at onset of caregiving need: A retrospective study of older adults in the USA. BMJ Open, 7(12), e017791. doi: 10.1136/bmjopen-2017-017791 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Agree, E. M. (2018). Demography of aging and the family. In Hayward M. D. & Majmundar M. K. (Eds.), Future directions for the demography of aging (pp. 159–186). The National Academies Press. [PubMed] [Google Scholar]
- Agree, E. M., & Glaser, K. (2009). Demography of informal caregiving. In Uhlenberg P. (Ed.), International handbook of population aging (pp. 705–728). Springer. doi: 10.1007/978-1-4020-835 [DOI] [Google Scholar]
- Allen, S. M., & Mor, V. (1997). The prevalence and consequences of unmet need. Contrasts between older and younger adults with disability. Medical Care, 35(11), 1132–1148. doi: 10.1097/00005650-199711000-00005 [DOI] [PubMed] [Google Scholar]
- Beach, S. R., & Schulz, R. (2017). Family caregiver factors associated with unmet needs for care of older adults. Journal of the American Geriatrics Society, 65(3), 560–566. doi: 10.1111/jgs.14547 [DOI] [PubMed] [Google Scholar]
- Beach, S. R., Schulz, R., Friedman, E. M., Rodakowski, J., Martsolf, R. G., & James, A. E. (2020). Adverse consequences of unmet needs for care in high-need/high-cost older adults. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 75(2), 459–470. doi: 10.1093/geronb/gby021 [DOI] [PubMed] [Google Scholar]
- Bronfenbrenner, U. (1977). Toward an experimental ecology of human development. American Psychologist, 32(7), 513–531. doi: 10.1037/0003-066X.32.7.513 [DOI] [Google Scholar]
- Bronfenbrenner, U. (1986). Ecology of the family as a context for human development: Research perspectives. Developmental Psychology, 22(6), 723–742. doi: 10.1037/0012-1649.22.6.723 [DOI] [Google Scholar]
- Brown, S. L., & Lin, I. (2012). The gray divorce revolution: Rising divorce among. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 67(6), 731–741. doi: 10.1093/geronb/gbs089 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brown, S. L., Lin, I. F., Hammersmith, A. M., & Wright, M. R. (2019). Repartnering following gray divorce: The roles of resources and constraints for women and men. Demography, 56(2), 503–523. doi: 10.1007/s13524-018-0752-x [DOI] [PMC free article] [PubMed] [Google Scholar]
- Burgdorf, J. G., Arbaje, A. I., Stuart, E. A., & Wolff, J. L. (2021). Unmet family caregiver training needs associated with acute care utilization during home health care. Journal of the American Geriatrics Society, 69(7), 1887–1895. doi: 10.1111/jgs.17138 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cantor, M., & Little, V. (1985). Aging and social care. In R. H. Binstock and E. Shanas (Eds.), Handbook of aging and the social sciences (pp. 745–781). [Google Scholar]
- Cherlin, A. J. (1978). Remarriage as an incomplete institution. American Journal of Sociology, 84(3), 634–650. doi: 10.1086/226830 [DOI] [Google Scholar]
- Coleman, M., Ganong, L. H., Hans, J. D., Sharp, E. A., & Rothrauff, T. C. (2005). Filial obligations in post-divorce stepfamilies. Journal of Divorce & Remarriage, 43(3–4), 1–27. doi: 10.1300/J087v43n03_01 [DOI] [Google Scholar]
- Cox, M. J., & Paley, B. (2003). Understanding families as systems. Current Directions in Psychological Science, 12(5), 193–196. doi: 10.1111/1467-8721.01259 [DOI] [Google Scholar]
- Curnow, E., Rush, R., Maciver, D., Górska, S., & Forsyth, K. (2021). Exploring the needs of people with dementia living at home reported by people with dementia and informal caregivers: A systematic review and meta-analysis. Aging & Mental Health, 25(3), 397–407. doi: 10.1080/13607863.2019.1695741 [DOI] [PubMed] [Google Scholar]
- Darley, J. M., & Latané, B. (1968). Bystander intervention in emergencies: Diffusion of responsibility. Journal of Personality and Social Psychology, 8(4), 377–383. doi: 10.1037/h0025589 [DOI] [PubMed] [Google Scholar]
- DeMatteis, J., Freedman, V. A., & Kasper, J. D. (2016). National Health and Aging Trends Study Round 5 sample design and selection. NHATS Technical Paper #16. [Google Scholar]
- de São José, J., Barros, R., Samitca, S., & Teixeira, A. (2016). Older persons’ experiences and perspectives of receiving social care: A systematic review of the qualitative literature. Health & Social Care in the Community, 24(1), 1–11. doi: 10.1111/hsc.12186 [DOI] [PubMed] [Google Scholar]
- Dunatchik, A., Icardi, R., & Blake, M. (2019). Predicting unmet need for social care. Journal of Long-Term Care, 0(2019), 194. doi: 10.31389/jltc.33 [DOI] [Google Scholar]
- Fingerman, K. L., & Bermann, E. (2000). Applications of family systems theory to the study of adulthood. International Journal of Aging & Human Development, 51(1), 5–29. doi: 10.2190/7TF8-WB3F-TMWG-TT3K [DOI] [PubMed] [Google Scholar]
- Freedman, V. A., & Kasper, J. D. (2019). Cohort profile: The National Health and Aging Trends Study (NHATS). International Journal of Epidemiology, 48(4), 1044–1045. doi: 10.1093/ije/dyz109 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman, V. A., Kasper, J. D., Cornman, J. C., Agree, E. M., Bandeen-Roche, K., Mor, V., Spillman, B. C., Wallace, R., & Wolf, D. A. (2011). Validation of new measures of disability and functioning in the National Health and Aging Trends Study. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 66(9), 1013–1021. doi: 10.1093/gerona/glr087 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman, V. A., & Spillman, B. C. (2014). Disability and care needs among older Americans. The Milbank Quarterly, 92(3), 509–541. doi: 10.1111/1468-0009.12121 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Freedman, V. A., & Wolff, J. L. (2020). The changing landscape of family caregiving in the United States. In Sawhill I. & Stevenson B. (Eds.), Caregiving leave. AEI/Brookings. [Google Scholar]
- Ganong, L. H., & Coleman, M. (1998). Attitudes regarding filial responsibilities to help elderly divorced parents and stepparents. Journal of Aging Studies, 12(3), 271–290. doi: 10.1016/S0890-4065(98)90004-4 [DOI] [Google Scholar]
- Ganong, L., & Coleman, M. (2018). Studying stepfamilies: Four eras of family scholarship. Family Process, 57(1), 7–24. doi: 10.1111/famp.12307 [DOI] [PubMed] [Google Scholar]
- Grundy, E., & Read, S. (2012). Social contacts and receipt of help among older people in England: Are there benefits of having more children? The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 67(6), 742–754. doi: 10.1093/geronb/gbs082 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanley, R. J., Wiener, J. M., & Harris, K. M. (1991). Will paid home care erode informal support? Journal of Health Politics, Policy and Law, 16(3), 507–521. doi: 10.1215/03616878-16-3-507a [DOI] [PubMed] [Google Scholar]
- He, S., Craig, B. A., Xu, H., Covinsky, K. E., Stallard, E., Thomas, J.3rd, Hass, Z., & Sands, L. P. (2015). Unmet need for ADL assistance is associated with mortality among older adults with mild disability. The Journals of Gerontology, Series A: Biological Sciences and Medical Sciences, 70(9), 1128–1132. doi: 10.1093/gerona/glv028 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Henretta, J. C., Van Voorhis, M. F., & Soldo, B. J. (2014). Parental money help to children and stepchildren. Journal of Family Issues, 35(9), 1131–1151. doi: 10.1177/0192513X13485077 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kalmijn, M., de Leeuw, S. G., Hornstra, M., Ivanova, K., van Gaalen, R., & van Houdt, K. (2019). Family complexity into adulthood: The central role of mothers in shaping intergenerational ties. American Sociological Review, 84(5), 876–904. doi: 10.1177/0003122419871959 [DOI] [Google Scholar]
- Kasper, J. D., Chan, K. S., & Freedman, V. A. (2017). Measuring physical capacity. Journal of Aging and Health, 29(2), 289–309. doi: 10.1177/0898264316635566 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kasper, J. D., & Freedman, V. A. (2020). National Health and Aging Trends Study (NHATS) user guide: Rounds 1–9 final release. www.NHATS.org [Google Scholar]
- Kasper, J. D., Freedman, V. A., & Spillman, B. (2013). Classification of persons by dementia status in the National Health and Aging Trends Study: Technical paper #5 (July Issue). Johns Hopkins University School of Public Health. www.NHATS.org. doi: 10.1007/s00129-002-1155-y [DOI] [Google Scholar]
- Lin, I.-F. (2008a). Consequences of parental divorce for adult children’s support of their frail parents. Journal of Marriage and Family, 70(1), 113–128. doi: 10.1111/j.1741-3737.2007.00465.x [DOI] [Google Scholar]
- Lin, I.-F. (2008b). Mother and daughter reports about upward transfers. Journal of Marriage and Family, 70(3), 815–827. doi: 10.1111/j.1741-3737.2008.00524.x [DOI] [Google Scholar]
- Lin, I. F., Brown, S. L., & Cupka, C. J. (2018). A national portrait of stepfamilies in later life. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 73(6), 1043–1054. doi: 10.1093/geronb/gbx150 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, I. F., & Wolf, D. A. (2020). Division of parent care among adult children. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 75(10), 2230–2239. doi: 10.1093/geronb/gbz162 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, I.-F., & Wu, H. S. (2018). Intergenerational transfer and reporting bias: An application of the mimic model. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 73(1), 19–29. doi: 10.1093/geronb/gbx080 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Lin, I. F., & Wu, H. S. (2019). Sibling influences, sibling similarities, and parent care in late life. EurAmerica, 49(1), 45–73. [PMC free article] [PubMed] [Google Scholar]
- Löwe, B., Wahl, I., Rose, M., Spitzer, C., Glaesmer, H., Wingenfeld, K., Schneider, A., & Brähler, E. (2010). A 4-item measure of depression and anxiety: Validation and standardization of the Patient Health Questionnaire-4 (PHQ-4) in the general population. Journal of Affective Disorders, 122(1–2), 86–95. doi: 10.1016/j.jad.2009.06.019 [DOI] [PubMed] [Google Scholar]
- McGarry, K. (1998). Caring for the elderly: The role of adult children. In D. A. Wise (Ed.), Inquiries in the economics of aging: Vol. I (pp. 133-166). University of Chicago Press. https://www.nber.org/system/files/chapters/c7084/c7084.pdf
- McLanahan, S., & Jacobsen, W. (2015). Diverging destinies revisited. In Amato P. R., Booth A., McHale S. M., & Van Hook J. (Eds.), Families in an era of increasing inequality (pp. 3–23). Springer. doi: 10.1007/978-3-319-08308-7_1 [DOI] [Google Scholar]
- Metlife Mature Market Institute . (2011). The MetLife study of caregiving costs to working caregivers: Double jeopardy for baby boomers caring for their parents (June Issue). https://www.caregiving.org/wp-content/uploads/2011/06/mmi-caregiving-costs-working-caregivers.pdf [Google Scholar]
- National Health and Aging Trends Study (NHATS) . (n.d.). Produced and distributed by www.nhats.orgwith funding from the National Institute on Aging (grant number NIA U01AG32947).
- Noël-Miller, C. M. (2013a). Repartnering following divorce: Implications for older fathers’ relations with their adult children. Journal of Marriage and Family, 75(3), 697–712. doi: 10.1111/jomf.12034 [DOI] [Google Scholar]
- Noël-Miller, C. M. (2013b). Former stepparents’ contact with their stepchildren after midlife. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 68(3), 409–419. doi: 10.1093/geronb/gbt021 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Perelli-Harris, B., & Lyons-Amos, M. (2016). Partnership patterns in the United States and across Europe: The role of education and country context. Social Forces, 95(1), 251–282. doi: 10.1093/sf/sow054 [DOI] [Google Scholar]
- Pezzin, L. E., Pollak, R. A., & Schone, B. S. (2008). Parental marital disruption, family type, and transfers to disabled elderly parents. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 63(6), 349–358. doi: 10.1093/geronb/63.6.s349 [DOI] [PubMed] [Google Scholar]
- Pickard, L. (2012). Substitution between formal and informal care: A natural experiment in social policy in Britain between 1985 and 2000. Ageing and Society, 32(7), 1147–1175. doi: 10.1017/S0144686X11000833 [DOI] [Google Scholar]
- Pinquart, M., & Sörensen, S. (2002). Older adults’ preferences for informal, formal, and mixed support for future care needs: A comparison of Germany and the United States. International Journal of Aging & Human Development, 54(4), 291–314. doi: 10.2190/1FVT-24T3-Y1V3-57A5 [DOI] [PubMed] [Google Scholar]
- Schulz, R., & Eden, J. (Eds.). (2016). Families caring for an aging America. National Academies Press. doi: 10.17226/23606 [DOI] [PubMed] [Google Scholar]
- Seltzer, J. A. (2019). Family change and changing family demography. Demography, 56(2), 405–426. doi: 10.1007/s13524-019-00766-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Steinbach, A., & Hank, K. (2016). Intergenerational relations in older stepfamilies: A comparison of France, Germany, and Russia. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 71(5), 880–888. doi: 10.1093/geronb/gbw046 [DOI] [PubMed] [Google Scholar]
- Van Den Broek, T., & Dykstra, P. A. (2017). Residential care and care to community-dwelling parents: Out-selection, in-selection and diffusion of responsibility. Ageing and Society, 37(8), 1609–1631. doi: 10.1017/S0144686X16000519 [DOI] [Google Scholar]
- van der Pas, S., & van Tilburg, T. G. (2010). The influence of family structure on the contact between older parents and their adult biological children and stepchildren in the Netherlands. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 65(2), 236–245. doi: 10.1093/geronb/gbp108 [DOI] [PubMed] [Google Scholar]
- Wachter, K. W. (1997). Kinship resources for the elderly. Philosophical Transactions of the Royal Society of London, Series B: Biological Sciences, 352(1363), 1811–1817. doi: 10.1098/rstb.1997.0166 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wiemers, E. E., Seltzer, J. A., Schoeni, R. F., Hotz, V. J., & Bianchi, S. M. (2019). Stepfamily structure and transfers between generations in U.S. families. Demography, 56(1), 229–260. doi: 10.1007/s13524-018-0740-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wolf, D. A. (2014). Getting help from others: The effects of demand and supply. The Journals of Gerontology, Series B: Psychological Sciences and Social Sciences, 69(Suppl. 1), 59–64. doi: 10.1093/geronb/gbu122 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.