Abstract
Bradykinin, a member of the kallikrein–kinin system (KKS), is a potent, short-lived vasoactive peptide that acts as a vasodilator and an inflammatory mediator in a number of signaling mechanisms. Bradykinin induced signaling is mediated through kinin B1 (BDKRB1) and B2 (BDKRB2) transmembrane receptors coupled with different subunits of G proteins (Gαi/Gα0, Gαq and Gβ1γ2). The bradykinin-mediated signaling mechanism activates excessive pro-inflammatory cytokines, including IL-6, IL-1β, IL-8 and IL-2. Upregulation of these cytokines has implications in a wide range of clinical conditions such as inflammation leading to fibrosis, cardiovascular diseases, and most recently, severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2). In SARS-CoV-2 infection, bradykinin is found to be at raised levels and is reported to trigger a diverse array of symptoms. All of this brings bradykinin to the core point as a molecule of immense therapeutic value. Our understanding of its involvement in various pathways has expanded with time. Therefore, there is a need to look at the overall picture that emerges from the developments made by deciphering the bradykinin mediated signaling mechanisms involved in the pathological conditions. It will help devise strategies for developing better treatment modalities in the implicated diseases. This review summarizes the current state of knowledge on bradykinin mediated signaling in the diverse conditions described above, with a marked emphasis on the therapeutic potential of targeting the bradykinin receptor.
Keywords: Bradykinin storm, Kinin receptors, Vasodilator, Inflammation, RAAS pathway, ARDS
Introduction
Bradykinin is a potent, transient vasoactive peptide that acts as a vasodilator and an inflammatory mediator in various signaling cascades. It is a member of the kallikrein–kinin system (KKS), associated with inflammatory response pathway mediating diverse functions in vascular permeability like thrombosis and blood coagulation [1]. Bradykinin induces vasodilation in peripheral circulation by decreasing the arterial tone of the smooth muscle and increasing blood flow [2]. Additionally, it initiates plasma extravasation by complying with capillary endothelium and vasoconstriction via the induction of venous smooth muscle fibers. During inflammatory conditions such as asthma, it promotes cellular movement from blood to tissues and activates mast cells, fibroblasts, macrophages and smooth muscles of organs [3, 4]. Bradykinin mediated signaling is also involved in chronic pain, vasculopathy, obesity, neuropathy, diabetes, and cancer [5–9].
Recently, it has been outlined that severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) disrupts KKS and renin–angiotensin–aldosterone system (RAAS), ushering in bradykinin storm, a process leading to heightened expression of bradykinin and consequent downstream signaling mediated effects. In such a state, bradykinin is at the core of many disparate symptoms of coronavirus disease (COVID-19), like loss of sense of smell and taste, leaky blood vessels, fluid accumulation in tissues and organs abnormal coagulation. The process impairs oxygen transfer from lungs to the blood, a common abnormality in COVID-19 patients [10]. Being a member of KKS, Bradykinin relies on other components for its synthesis and sustenance. Rightly so, the biochemistry of these components, namely bradykinin receptors, bradykinin-related peptides, receptor agonists and antagonists and various other aspects, has been outlined in far more detail than bradykinin [5, 11, 12]. The evidence above casts a spotlight on bradykinin as a molecule of immense therapeutic potential that deservingly needs its due share of focused discussion fulfilled.
Here, we attempt an excursion into the currently available knowledge on bradykinin under the broad landscape of KKS, its signaling cascades and role in disease pathophysiology, both protective and deleterious, and bradykinin receptor targeting that can carve the premise of the therapeutic utilization of bradykinin in various conditions.
Kallikrein–kinin system and bradykinin synthesis
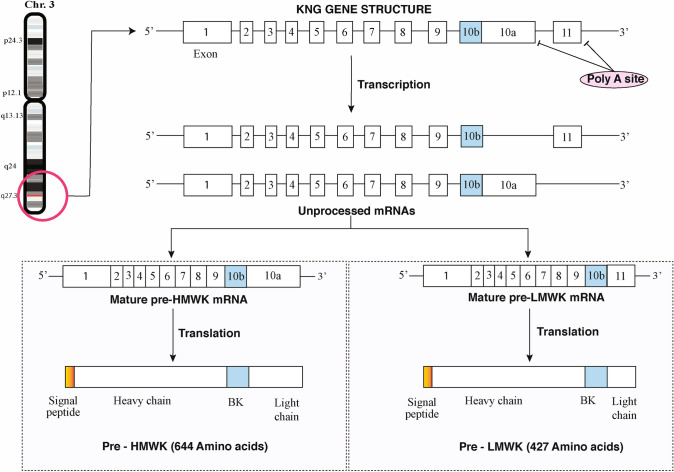
Kinins are low molecular weight peptides that get liberated from high molecular weight kininogens (HMWK) and low molecular weight kininogens (LMWK) by the action of plasma kallikrein (PK) or tissue kallikrein (TK), respectively, which makes up an integral part of KKS [13]. Distinct gene transcripts of plasma HMWK and tissue LMWK are derived from the kininogen gene (KNG1) located on chromosome 3q26 (in humans) by alternate splicing. This gene contains 11 exons, of which 9 and apart of exon 10 codes for the heavy chain of both kininogens. Full coding sequence of exon 10 makes 56 kDa light chain of HMWK and exon11 codes for 4 kDa light chain of LMWK [14, 15].
Plasma KKS are involved in constitutive anti-coagulant activity protecting endothelium, whereas the tissue system is essential in tissue repair and reaction to noxious or artificial stimuli [16]. HMWK is primarily expressed in the liver, whereas LMWK are widely distributed and expressed in endothelial cells of vasculature [17]. PK is produced as zymogen plasma pre-kallikrein, secreted primarily from hepatocytes into the blood. In the blood, it circulates as a complex with HMWK [18]. Normally, circulating PK is inactive but can be activated with a negatively charged surface like the basement membranes mediated blood clotting by factor XII (Hageman factor/FXII) and HMWK as co-factor]. PK then processes HMWK (120 kDa) to release the nonapeptide bradykinin [19, 20].
Meanwhile, TK differs from PK as it can be encoded by various genes and secreted by many organs, including the pancreas, salivary glands and kidney [21]. There are 15 known TKs encoded by the genes named it from KLK1 to KLK15, the most prominent protease family in the human genome, which are located on 19q13 chromosome [22]. TK produces decapeptide, kallidin or Lys-BK (LBK) mainly by its action on LMWK (70 kDa). In addition, TK can also act on HMWK to generate LBK [23] (Fig. 1). LBK can be converted into bradykinin in some circumstances by the action of plasma aminopeptidases upon removal of N-terminal lysine. These activated kinins can stimulate endothelial cells, increasing vasodilation, vascular permeability, nitric oxide (NO) production, and arachidonic acid mobilization [24]. Aminopeptidase B can act on LBK and release N-terminal lysine, thereby releasing bradykinin without further degradation [25].
Fig. 1.
The gene for KNG is present on q-arm of chromosome 3. Boxes 1–11 show the respective exons with intermittent introns. KNG gene undergoes alternative splicing to form HMWK and LMWK. Boxes 1–9 codes for signal peptide and heavy chain of HMWK and LMWK. Exon 10b encodes the bradykinin sequence. Exon 10b codes for the light chain of HMWK, whereas exon 11 contains sequences characteristic of the LMWK light chain
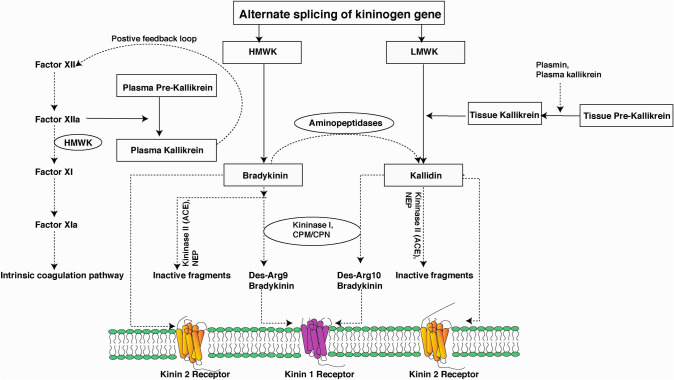
Kinins are altered by a number of enzymes, including Carboxypeptidase M (CPM), a kininase I-type enzyme that modifies bradykinin and LBK into des-Arg9-BK and des-Arg10-LBK, respectively [26]. Further, C-terminal arginine residues of the kinins can be removed by carboxypeptidase N (CPN), a plasma carboxypeptidase. Angiotensin I converting enzyme (ACE) is a key kininase II that cleaves C-terminal dipeptides from kinins, rendering them inactive. Kinins are cleaved at internal phenylalanine (Phe5 in BK) by membrane-bound Neutral endopeptidase (NEP) [27, 28]. Therefore, given these factors, the circulating lifespan of bradykinin corresponds to only a few seconds following its transient activity with this consortium of digesting enzymes [29] (Fig. 2).
Fig. 2.
KKS organisation. Following alternate splicing of KNG gene, LMWK and HMWK are synthesized. Various physiological insults such as tissue damage leads to proteolytic activations of TK, which converts LMWK into LBK. Factor XII (Hageman factor) activates PK, that transforms HMWK to bradykinin. LBK and bradykinin are agonists for BDKRB2, and upon the action of carboxypeptidases like CPM/CPN can result in the formation of Des-Arg9-Kallidin and Des-Arg9-BK, members BDKRB1 agonists. Bradykinin can be broken down into inactive fractions by ACE and NEP and LBK converted into bradykinin by an aminopeptidase. (Notations: LMWK-Low-molecular-weight kininogen, HMWK-High-molecular-weight kininogen, PK-Plasma kallikrein, ACE-Angiotensin-converting enzyme, NEP-Neutral endopeptidase)
Kinin receptors
Regoli et al. have characterized kinin receptors through pharmacological studies [30]. The cell surface receptors such as kinin B1 and B2 are transmembrane G-protein coupled receptors with seven domains that mediate the biological effects of kinins [31]. BDKRB2 is widely expressed in many healthy tissues and stimulated by the binding of unaltered kinins. Unlike BDKRB2, BDKRB1 is inducible and present minimally in healthy tissues but expressed rapidly during inflammation and responded to kinin lacking C-terminal arginine residues [6].
BDKRB1 is scarcely detectable in peripheral tissues under normal physiology, but its mRNA was present constitutively in different brain regions and spinal cord [32, 33]. BDKRB1 is rapidly induced in almost all inflammatory and stressful conditions at transcriptional and post-transcriptional levels in the whole body [8, 34]. Pro-inflammatory mediators like interleukin-1β, IFNγ, TNFα, soluble gC1qR and epidermal growth factor at inflammatory sites can upregulate de novo synthesis of BDKRB1 in various cells especially, endothelial [35–37]. CPM binds to the external loop 2 of BDKRB1 increasing conformational activation and generates BDKRB1 agonists from kinins [38]. BDKRB2 is localized constitutively in the majority of inflammatory relevant cells, including endothelial cells, osteoblasts, epithelial cells and neurons in the brain. It is also expressed in different types of tumor cells and immune cells [33, 39–41].
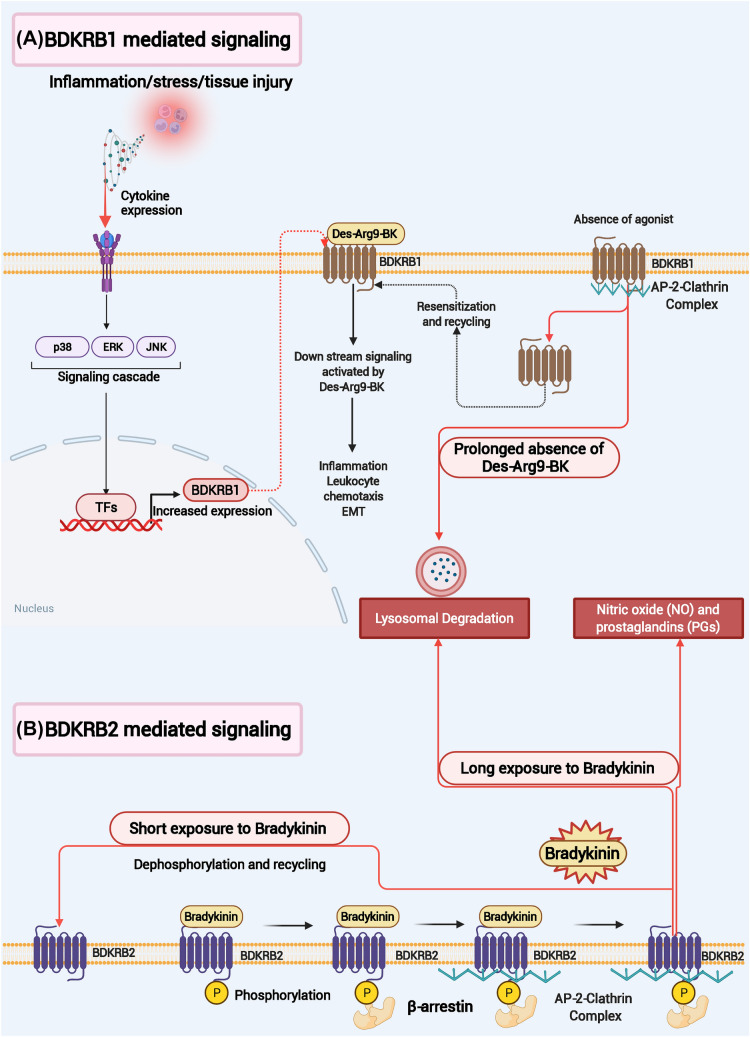
BDKRB2 is activated by phosphorylation at serine (S339, S346, S348) and threonine (T342, T345) residues on the C-terminal region when an agonist binds, which leads to arrestin mediated internalization through clathrin-coated vesicles [42, 43]. When exposed to kinin for an extended period of time, BDKRB2 is secluded into the lysosome for degradation, whereas short-term stimulation results in dephosphorylation and, as a result, the receptor is recycled back to the surface. In contrast, agonist-induced internalization is not seen in BDKRB1. Unless BDKRB1 binds to agonist, its internalization occurs independent of beta-arrestin and is broken down in lysosomes [44, 45]. However, if a ligand binds to BDKRB1, the available number of receptors is increased by redirecting sequestered clathrin-coated BDKRB1 vesicle into the cell membrane [44] (Fig. 3).
Fig. 3.
A schematic representation of BDKRB1 and BDKRB2 signaling mechanisms mediated by bradykinin. A Stress, inflammation and tissue injury lead to the expression of BDKRB1, which gets stimulated upon binding with Des-Arg9-BK and triggers downstream signaling cascades. In the absence of agonist stimulation, BDKRB1 gets internalized for breakdown by lysosomal degradation. B BDKRB2 receptor is activated upon the binding of Bradykinin and subsequent phosphorylation. Arrestin mediated internalization occurs through clathrin-coated vesicles. BDKRB2 is secluded into the lysosome for degradation if exposed to kinin for the long term. Short-term exposure with bradykinin results in dephosphorylation followed by receptor recycling back to the surface
In common, BDKRB1 and BDKRB2 receptors are involved in the progression and sustenance of chronic pain in complex regional pain syndrome type-I, vulvodynia and fibromyalgia-like pain symptoms [46–48]. Additionally, both receptors are activated in pathologies involving tissue damage due to oxidative stress, pro-inflammatory stimuli, vasoactive peptide stimuli such as those found in the renin-angiotensin system, lipopolysaccharides, and endotoxins. These receptors are also regulated by post-translational modifications (PTMs) [49–51]. Protective or pathological outcomes of receptors of kinin family (BDKRB1, BDKRB2) regulation and mediation by KKS in the events of both normal and pathophysiological states are discussed in multiple studies [52–54].
Bradykinin and its involvement in disease
Bradykinin-activated signaling pathways play a significant role in various pathological conditions such as cardiovascular complications, fibrosis and the most recent pandemic COVID-19.
COVID-19
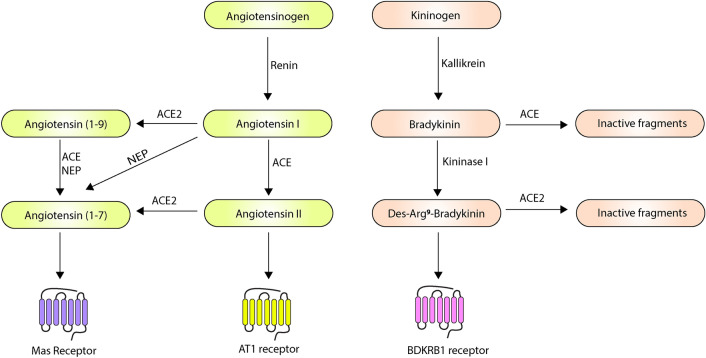
COVID-19 is a highly contagious viral infection caused by the SARS-CoV-2 virus. The infection was first reported from Wuhan, China in December 2019 and advanced rapidly due to onward transmission [8]. It is hypothesized that bradykinin pathway is dysregulated in COVID-19 patients leading to various complicated respiratory conditions. Garvin et al. have reported that bronchoalveolar lavage fluid (BALF) of COVID-19 patients have reduced ACE gene expression and raised ACE2, renin, angiotensin, AT1 and AT2, kininogen and kallikrein enzymes that activate BDKRB1 and BDKRB2 receptors [10] (Fig. 4). The expression of the BDKRB1 and BDKRB2 receptors was reported to be raised by 2945- and 207-folds, respectively. Kininogen and kallikreins expression was undetected in controls but expressed in COVID-19. Although ACE gene expression reduced eightfold, resulting in enhanced activity of bradykinin, downregulation of ACE2 culminated in reduced degradation of des‐Arg(9)‐bradykinin. All of this along with the increased expression BDKRB1 and BDKRB2 receptors can lead to the bradykinin storm [10, 55]. Such ‘Bradykinin storm’ leads to vasodilation, vascular permeability, and hypotension. It is possible that this bradykinin is produced by bronchiole and alveoli-resident mast cells. Tissue resident granulocytes and mast cells are known to generate bradykinin by synthesizing heparin, activating coagulation factor XII, and forming PK [56, 57]. Thus, the rise of bradykinin could be attributed to heightened mass cells density in the lungs of COVID-19 patients’ [58].
Fig. 4.
A schematic diagram of ACE2, ACE and Bradykinin regulation mechanisms. The enzyme ACE can act on Angiotensin I and Bradykinin to convert them into Angiotensin-(1–9) and inactive fragments, respectively, thus connecting the two pathways. The resulting products, Angiotensin-(1–7), Angiotensin II, and des-Arg9 bradykinin mediate their effects through Mas, AT1 and BDKRB1 receptors. (Notations: ACE- Angiotensin-converting enzyme, NEP- Neprilysin)
It is also hypothesized that bradykinin metabolite, des-Arg9-BK, could lead to inflammation, vasodilation, vascular permeability through bradykinin receptors [59]. This becomes important because des-Arg9-BK is cleaved by ACE2 [60] and is in contrary to the report by Garvin et al., it is established that SARS-CoV-2 infects target cells via its spike protein (S) antigen with ACE2 [61, 62]. The internalization of the resulting complex reduces the activity of ACE2. This increases its signaling via BDKRB1 leading to fluid extravasation and leukocyte movement to lungs [60, 63]. Raised BALF ACE2 levels in the study by Garvin et al. could be because it was either membrane shed form (via ADAM17-mediated proteolytic cleavage) or soluble form and that the type of ACE2 was not exactly determined [10]. Dry cough as a COVID-19 symptom could be explained by bradykinin-mediated sensory nerve activity as a cascade for ACE-inhibitor modulated dry cough [64]. Further, bradykinin may have a role in gustatory and olfactory dysfunctions [65]; also, ACE-inhibitors can lead to olfactory dysfunction [66].
The loss of ACE2 function and the resulting raised Ang-II levels can also lead to decreased ACE activity via a negative feedback loop (renal ACE and renin gene is downregulated by Ang-II). This decrease in ACE levels can lead to a rise in bradykinin levels. Further, it is reported that Ang-II is involved in the raised expression of prolyl-carboxypeptidase, resulting in PK-induced generation of bradykinin [67]. Reduced ACE2 level outcomes like vasoconstriction [68], pro-inflammatory cytokine levels [69], C-reactive protein [70], pulmonary fibrosis [71], coagulopathy with increased plasma D-dimer, pulmonary thrombosis and venous thromboembolism [72, 73], dispersed intravascular coagulation [74] and ARDS [69, 75] are reported in COVID-19 patients. Reduced eNOS activity and NO levels are involved in COVID-19 patients with endothelial dysfunction, resulting in thrombosis and organ dysfunctions [76, 77]. It supports the hypotheses of reduced BDKRB2 stimulation (which initiates eNOS) and NO generation. Besides ACE-2, a lysosomal cysteine endopeptidase, cathepsin L, also assists SARS-COV-2 cell entry via transmembrane protease serine-2 [61]. It forms kinins from LMWK and HMWK [78], and has kininogenase activity [79]. It can lead to bradykinin release and has hypotensive activities [80].
The rise in bradykinin, des-Arg9-BK, and Ang-II levels in the pulmonary vascular bed and peripheral vascular system by SARS-CoV-2 infection can lead to the onset of acute respiratory distress syndrome (ARDS) [81], a potentially fatal lung respiratory failure caused by inflammation and fluid build-up in the lungs, resulting in stiff lungs and hypoxemia [82]. It is proposed that BDKRB2 blockers and inhibition of PK might prevent the development of COVID-19 induced ARDS [59].
Cardiovascular complications
Prolonged hypertension is generally associated with renal dysfunction and tissue injury. Some studies suggest the protective function of bradykinin against hypertension-induced complications [83, 84]. For instance, salt-induced hypertensive and renal injured rats were infused subcutaneously with bradykinin showed protective effects against renal injury but not hypertension. In this way, bradykinin directly protects against salt-induced renal injury [84]. Bradykinin also has a proliferative effect on endothelial cells. Locally synthesised bradykinin takes part in neovascularization and helps repair vascular wall and remodeling after acute ischemia. It signals through BDKRB2/PI3K/eNOS mediated employment of circulating progenitor cells having the regenerating capacity to the injury site [83]. Bradykinin has a key function in all cardiac conditioning mechanisms [85, 86]. Bradykinin infusion in isolated rat hearts provides intermittent protection through a pathway involving BDKRB2, PKG, NOS and mitochondrial K(ATP) channel [86]. Bradykinin also inhibits myocardial apoptosis through Akt and GSK-3β phosphorylation, improves antiapoptotic protein profile and plays a role in ventricular remodeling [87, 88].
Similarly, a pharmacological study reports the myocardial protective role of BDKRB1 and BDKRB2 in diabetic and nondiabetic patients, respectively, in acute coronary syndrome [89]. Cardioprotective drug-mediated augmentation of kinins’ half-lives, including bradykinin, has protective roles in cardiac remodeling, apoptosis and fibrosis, via BDKRB2-NO [90, 91]. However, bradykinin can have anti-fibrotic effects in pathogenic remodeling that surrounds cardiomyocytes leading to left ventricular enlargement and dysfunction [92]. In addition, bradykinin is involved in infarction triggered chest pain (angina) mediated through 12-lipoxygenase products, IP3 and TRPV1 channels. Bradykinin also acts as a cardiac nociceptor which stimulates BDKRB2 in upper thoracic spinal (sympathetic) sensory neurons [93, 94]. Thromboxane A2, a lipid family member with prothrombotic properties, reciprocally interacts with bradykinin during myocardial ischemia stimulating cardiac spinal afferents [94, 95].Bradykinin agonists can be therapeutically used to counterbalance Bradykinin deficiency, which seems consistent with endogenous bradykinin-BDKRB2 mediated cardiac protection. However, deducing the right dosage, therapeutic window, and medication period will be significant determinants to control the balance.
Fibrosis
Fibrosis is the pathological wound healing condition in which connective tissue replaces normal parenchymal tissue to an extent that leads to substantial tissue remodeling and development of permanent scar tissue [96, 97]. Bradykinin has significant roles in diseases marked by tissue remodeling and chronic inflammation. In such states, bradykinin may have an anti-fibrogenic effect [98]. In cardiac and renal damage, stimulated BDKRB2 has protective effects. Overexpression of kallikrein gene reduces the onset of cardiac hypertrophy and renal fibrosis [98–100]. Bradykinin may induce such effects in heart and kidney via the beneficial role of RAAS inhibitors as the inhibition with pharmacologic agents of this system increases bradykinin levels [99, 101, 102]. Also, bradykinin has protective effects in models of ischemia–reperfusion, a condition characterised by the caused tissue damage owing to the return of the blood supply to tissue after a stretch of ischemia or anoxia (or hypoxia). This condition induces secretion of vasodilatory intermediaries like NO and prostaglandins [103]. Further, bradykinin activates signaling molecules that safeguards parenchymal cells from apoptosis by NF-kB and AKT pathway [104, 105].
Targeting the bradykinin receptor
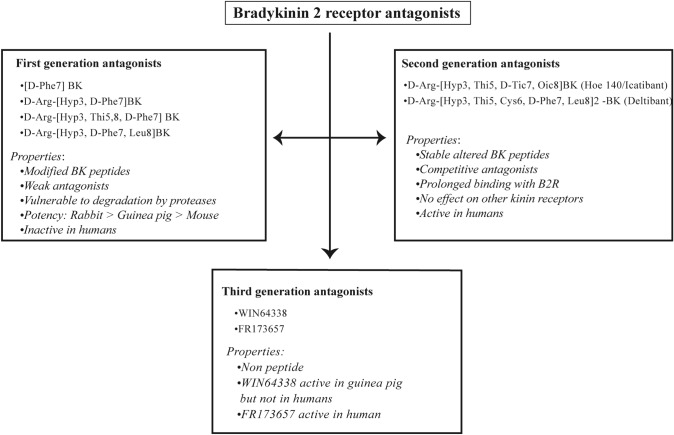
The proceeds in the cognizance of kinin roles, including BK and its receptors, stem from the progress made in chemically synthesized peptide and non-peptide selective receptor ligands [106–108]. Studies reporting compounds mediating their effects on B2R have been classified in three generations (Fig. 5). The first generation of B2R antagonists includes Vavrek and Stewart, who synthesized them by changing the C-terminal dipeptide Phe8-Arg9 of BK and substitution of Pro7 by D-Phe residue. This [D-Phe7] BK analogue is a weak antagonist and partial agonist of guinea pig and rabbit B2R [109]. Further, N-terminal addition of a D-Arg and the substitution of Pro3 by Hyp results in D-Arg- [Hyp3,D-Phe7] BK (NPC 567) with improved potency against degradation by proteases [110]. D-Arg- [Hyp3, Thi5,8, D-Phe7] BK is a homologue of NPC 567 with an unnatural amino acid. This replaces Phe at positions 5th and 8th, conceivably conferring resistance against degradation by proteases. In D-Arg- [Hyp3,D-Phe7, Leu8] BK, Phe8 is substituted by a Leu to eliminate aromaticity [109]. These antagonists are more potent in rabbit B2R than other study models (guinea pig, mouse) but inactive in humans because of rapid degradation by a battery of proteases [111, 112]. Additionally, they are converted to desArg9-metabolites (B1R agonists) by CPM, thereby making it non-selective [109].
Fig. 5.
B2R receptor antagonists. Members and properties of the three generations of B2R antagonists are depicted
The second generation of B2R antagonists was introduced by discovering HOE140 (Icatibant), which had rigidity, stability, increased binding, and potency without partial agonist activity [113]. In HOE140, D-Phe7 was substituted by the rigid analogue tetrahydroisoquinoline-3-carboxylic acid (D-Tic) and Thi8 by octa hydro indole-2-carboxylic acid (Oic) (D-Arg-[Hyp3, Thi5, D-Tic7, Oic8] BK) [111, 114]. It could resist endo and exopeptidase activity by its tertiary amides D-Tic and Oic, similar to proline and hydroxyproline, along with D-Arg at the amino terminus. These characteristics give this molecule extreme stability and prolong its interaction with B2R [114]. In addition, these two unnatural amino acids andthe beta-turn of the C-terminal region conferred extra rigidity, which marked the significance of the spatial orientation for optimal antagonist activity. Intra-arterial injection of HOE140 blocked the effect of exogenous bradykinin in rats and was found to be quite potent in humans as it competitively binds to B2R. HOE140 is very selective as it had almost no effect on other kinin receptors [115].
In addition, it is known as a non-equilibrium antagonist as it binds at the same site as BK but dissociates rather slowly, thereby preventing the complete occupation of agonist(s) [111, 116]. It has been employed in clinical trials to control acute rhinitis and asthma and gauge kinins' function in pain and hyperalgesia [117–119]. Even though it failed to manage pollen-induced seasonal allergic rhinitis, it antagonised house dust-mite triggered nasal obstruction in allergic rhinitis patients [118]. Subcutaneous injection of HOE140 leads to local skin reaction caused by interaction with a mast cell GPCR which releases histamine [120]. Further, it has been certified for HAE treatment with acute attacks [121]. In order to improve stability, duration of action and flexibility in comparison to the previously described antagonists, dimeric peptides were explored. One such example is Deltibant (CP-0127), a homodimer of D-Arg-[Hyp3,Thi5,Cys6,D-Phe7,Leu8] BK joined at Cys6 by bis-succinimidohexane (BSH) [122]. It has moderate potency as demonstrated in various assays and enhanced stability and efficacy in various in vivo models of trauma [4].
Later, non-peptide, orally active third-generation B2R antagonists including WIN64338 and FR173657 were synthesized. The former exerts moderate antagonism in the guinea pig but is inactive in humans [123–125]. However, later is highly potent on human B2R with pA2 value of 8.2 (pA2 value indicates the affinity of the antagonist to the receptor). FR173657 also inhibits bronchoconstriction in guinea pigs, reduces carrageenan-mediated paw edema, reduces caerulein-mediated pancreatitis in rats, and relieves kaolin-mediated pain in mice when administered orally [126, 127]. Anatibant (LF 16–0687; XY2405) is a synthetic non-peptide B2R antagonist with a characteristic pharmacological profile that meets essential criteria to be considered for clinical trials. Further, it is investigated in a clinical trial to brain edema after head injury [128–130].
Fasitibant (MEN16132) is also a nonpeptide selective antagonist for the B2R with high efficacy in several animal models of inflammation [131]. Based on the outcomes generated in various pharmacological investigations, it was taken up for phase II clinical trials for knee pain in osteoarthritis (NCT0109116) [132]. Lanadelumab (DX-2930) is a Human monoclonal antibody-containing κ-light-chain of immunoglobulin G1 against PK [133]. It binds to free soluble PK and HMWK bound PK. Further, it inhibits hydrolysis of HMWK by PK, without inhibiting other serine-proteases, like Factor XIa and the zymogen PPK [133] (Table 1). It was recently approved for the treatment of long-term prophylaxis for C1-INH-HAE attacks in patients aged 12 and above [134]. However, European Medicines Agency designated it as an orphan drug as it is not profitable to produce without government assistance [135].
Table 1.
List of drug targets (Bradykinin receptors) and therapeutics in clinical trials
| Drug | Target | Clinical phase | Indication | References |
|---|---|---|---|---|
| HOE-140 (Icatibant, Firazyr) | B2R antagonist | Approved |
Hereditary angioedema (HAE) |
[136, 137] |
| CP-0127 (deltibant) | B2R antagonist | Phase II | Severe traumatic brain injury sepsis | [138–140] |
| FR173657 | B2R antagonist | Reported | Bronchoconstriction, pancreatitis, kaolin-mediated pain | [125, 126] |
| LF16-0687 (anatibant) | B2R antagonist | Phase II | Severe traumatic brain injury | [129] |
| MEN16132 (fasitibant) | B2R antagonist | Phase II | Knee pain in osteoarthritis | [131] |
| DX-2930 (Lanadelumab) | Human monoclonal antibody- against PK | Approved | long-term prophylaxis for C1-INH-HAE attacks | [133] |
| PHA-022121 | B2R antagonist | Phase II |
Hereditary angioedema (HAE) |
[141] |
Future directions
The review summarizes pioneer research and recent updates on bradykinin-induced effects in various diseases. Along with bradykinin, we have also discussed distinctive role of BDKRB1 and BDKRB2 in various conditions, which are often involved in opposite and not always compensatory or synergistic manner. Albeit under the limelight of various KKS and RAAS components, the review showcases the important role of bradykinins in the pathophysiology of inflammatory conditions and recent COVID-19 burden. Due to this conjoined nature of bradykinin signaling with other mediators, the results of preclinical and clinical studies aiming to manage the above diseases by pharmacological exploration of kinin precursors, kinin receptors and related enzymes can be exploited in targeting bradykinin as a therapeutic molecule.
However, even with such open avenues, the approved drugs targeting bradykinin specifically are low in number. Furthermore, the challenge becomes formidable due to poor translational research outputs and, when considering infectious diseases, pathogen resistance, high toxicity states of most antimicrobial drugs, and unaddressed requirements, such as in severe COVID-19 cases. In conclusion, to counter the challenges mentioned above and cater for the need of improving treatment outcomes in the implicated diseases, a multi-pronged strategy that makes leverage of the current understanding of bradykinin mediated signaling aspects and undertakes pharmacological targeting of bradykinin associated KKS components; mainly kinin receptors need careful consideration to be devised.
Acknowledgements
We acknowledge a research grant from Olav Thon Foundation entitled "Discovering new therapeutic targets and drugs to combat AMR tuberculosis: proteomics characterization and drug screening of mycobacterium -infected macrophages". We also thank Karnataka Biotechnology and Information Technology Services (KBITS), Government of Karnataka, for the support to Center for Systems Biology and Molecular Medicine at Yenepoya (Deemed to be University) under the Biotechnology Skill Enhancement Programme in Multi-Omics Technology (BiSEP GO ITD 02 MDA 2017). D. A. B. Rex is a recipient of the Senior Research Fellowship from the Indian Council of Medical Research (ICMR), Government of India. Deepak and Neelanchal are recipients of BiSEP trainee fellowship from the Ministry of IT and BT, Government of Karnataka.
Author contributions
RDAB, NV and KD, drafted the manuscript. SD and TSKP, revised the manuscript. RDAB, NV and KD, prepared figures. TSKP reviewed the article and provided critical comments. All authors read, edited, and approved the final article.
Funding
Not Applicable.
Data availability
Not Applicable.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
Not Applicable.
Consent for publication
Not Applicable.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Devasahayam Arokiar Balaya Rex, Email: rexprem@yenepoya.edu.in.
Neelanchal Vaid, Email: vneelanchal@gmail.com.
K. Deepak, Email: newis27deepak@gmail.com
Shobha Dagamajalu, Email: shobha_d@yenepoya.edu.in.
T. S. Keshava Prasad, Email: keshav@yenepoya.edu.in.
References
- 1.Costa-Neto CM, et al. Participation of kallikrein-kinin system in different pathologies. Int Immunopharmacol. 2008;8(2):135–142. doi: 10.1016/j.intimp.2007.08.003. [DOI] [PubMed] [Google Scholar]
- 2.Mombouli JV, Vanhoutte PM. Kinins and endothelial control of vascular smooth muscle. Annu Rev Pharmacol Toxicol. 1995;35:679–705. doi: 10.1146/annurev.pa.35.040195.003335. [DOI] [PubMed] [Google Scholar]
- 3.Sharma JN. Basic and clinical aspects of bradykinin receptor antagonists. Prog Drug Res. 2014;69:1–14. doi: 10.1007/978-3-319-06683-7_1. [DOI] [PubMed] [Google Scholar]
- 4.Rodell TC. The kallikrein/kinin system and kinin antagonists in trauma. Immunopharmacology. 1996;33(1–3):279–283. doi: 10.1016/0162-3109(96)00071-9. [DOI] [PubMed] [Google Scholar]
- 5.Dagnino APA, Campos MM, Silva RBM. Kinins and their receptors in infectious diseases. Pharmaceuticals (Basel) 2020;13(9):215. doi: 10.3390/ph13090215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Lau J, et al. A Systematic Review of Molecular Imaging Agents Targeting Bradykinin B1 and B2 Receptors. Pharmaceuticals (Basel) 2020;13(8):199. doi: 10.3390/ph13080199. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang S, et al. Phospholipase C and protein kinase A mediate bradykinin sensitization of TRPA1: a molecular mechanism of inflammatory pain. Brain. 2008;131(Pt 5):1241–1251. doi: 10.1093/brain/awn060. [DOI] [PubMed] [Google Scholar]
- 8.Couture R, et al. Kinin receptors in pain and inflammation. Eur J Pharmacol. 2001;429(1–3):161–176. doi: 10.1016/S0014-2999(01)01318-8. [DOI] [PubMed] [Google Scholar]
- 9.Rex DAB, et al. A modular map of Bradykinin-mediated inflammatory signaling network. J Cell Commun Signal. 2022;16(2):301–310. doi: 10.1007/s12079-021-00652-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Garvin MR, et al. A mechanistic model and therapeutic interventions for COVID-19 involving a RAS-mediated bradykinin storm. Elife. 2020 doi: 10.7554/eLife.59177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Marceau F, et al. Bradykinin receptors: agonists, antagonists, expression, signaling, and adaptation to sustained stimulation. Int Immunopharmacol. 2020;82:106305. doi: 10.1016/j.intimp.2020.106305. [DOI] [PubMed] [Google Scholar]
- 12.Kashuba E, et al. The kinin-kallikrein system: physiological roles, pathophysiology and its relationship to cancer biomarkers. Biomarkers. 2013;18(4):279–296. doi: 10.3109/1354750X.2013.787544. [DOI] [PubMed] [Google Scholar]
- 13.Leeb-Lundberg LM, et al. International union of pharmacology XLV Classification of the kinin receptor family: from molecular mechanisms to pathophysiological consequences. Pharmacol Rev. 2005;57(1):27–77. doi: 10.1124/pr.57.1.2. [DOI] [PubMed] [Google Scholar]
- 14.Stewart JM, et al. Bradykinin-related compounds as new drugs for cancer and inflammation. Can J Physiol Pharmacol. 2002;80(4):275–280. doi: 10.1139/y02-030. [DOI] [PubMed] [Google Scholar]
- 15.Kitamura N, et al. Structural organization of the human kininogen gene and a model for its evolution. J Biol Chem. 1985;260(14):8610–8617. doi: 10.1016/S0021-9258(17)39516-9. [DOI] [PubMed] [Google Scholar]
- 16.Linz W, et al. Contribution of kinins to the cardiovascular actions of angiotensin-converting enzyme inhibitors. Pharmacol Rev. 1995;47(1):25–49. [PubMed] [Google Scholar]
- 17.From the American Association of Neurological Surgeons, ASoNC, et al., Multisociety Consensus Quality Improvement Revised Consensus Statement for Endovascular Therapy of Acute Ischemic Stroke. Int J Stroke, 2018. 13(6): 612–632. [DOI] [PubMed]
- 18.Bryant JW, Shariat-Madar Z. Human plasma kallikrein-kinin system: physiological and biochemical parameters. Cardiovasc Hematol Agents Med Chem. 2009;7(3):234–250. doi: 10.2174/187152509789105444. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Bjorkqvist J, Jamsa A, Renne T. Plasma kallikrein: the bradykinin-producing enzyme. Thromb Haemost. 2013;110(3):399–407. doi: 10.1160/TH13-03-0258. [DOI] [PubMed] [Google Scholar]
- 20.Pathak M, et al. Structure of plasma and tissue kallikreins. Thromb Haemost. 2013;110(3):423–433. doi: 10.1160/TH12-11-0840. [DOI] [PubMed] [Google Scholar]
- 21.Clements J, Mukhtar A. Tissue kallikrein and the bradykinin B2 receptor are expressed in endometrial and prostate cancers. Immunopharmacology. 1997;36(2–3):217–220. doi: 10.1016/S0162-3109(97)00024-6. [DOI] [PubMed] [Google Scholar]
- 22.Boyukozer FB, et al. Kallikrein gene family as biomarkers for recurrent prostate cancer. Croat Med J. 2020;61(5):450–456. doi: 10.3325/cmj.2020.61.450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Nokkari A, et al. Implication of the Kallikrein-Kinin system in neurological disorders: quest for potential biomarkers and mechanisms. Prog Neurobiol. 2018;165–167:26–50. doi: 10.1016/j.pneurobio.2018.01.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Golias C, et al. The kinin system–bradykinin biological effects and clinical implications. Multiple role of the kinin system–bradykinin. Hippokratia. 2007;11(3):124–128. [PMC free article] [PubMed] [Google Scholar]
- 25.Hopsu-Havu VK, Makinen KK, Glenner GG. Formation of bradykinin from kallidin-10 by aminopeptidase B. Nature. 1966;212(5067):1271–1272. doi: 10.1038/2121271a0. [DOI] [PubMed] [Google Scholar]
- 26.Zhang X, et al. Cross-talk between carboxypeptidase M and the kinin B1 receptor mediates a new mode of G protein-coupled receptor signaling. J Biol Chem. 2011;286(21):18547–18561. doi: 10.1074/jbc.M110.214940. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Scholzen TE, Luger TA. Neutral endopeptidase and angiotensin-converting enzyme—key enzymes terminating the action of neuroendocrine mediators. Exp Dermatol. 2004;13(Suppl 4):22–26. doi: 10.1111/j.1600-0625.2004.00260.x. [DOI] [PubMed] [Google Scholar]
- 28.Rex DAB, et al. Broadening COVID-19 Interventions to Drug innovation: neprilysin pathway as a friend, foe, or promising molecular target? OMICS. 2021;25(7):408–416. doi: 10.1089/omi.2021.0080. [DOI] [PubMed] [Google Scholar]
- 29.Kayashima K, Ueki M, Kinoshita Y. Ultrasonic analysis of the anatomical relationships between vertebral arteries and internal jugular veins in children. Paediatr Anaesth. 2012;22(9):854–858. doi: 10.1111/j.1460-9592.2012.03816.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Regoli DC, Marceau F, Lavigne J. Induction of beta 1-receptors for kinins in the rabbit by a bacterial lipopolysaccharide. Eur J Pharmacol. 1981;71(1):105–115. doi: 10.1016/0014-2999(81)90391-5. [DOI] [PubMed] [Google Scholar]
- 31.Hess JF, et al. Cloning and pharmacological characterization of a human bradykinin (BK-2) receptor. Biochem Biophys Res Commun. 1992;184(1):260–268. doi: 10.1016/0006-291X(92)91187-U. [DOI] [PubMed] [Google Scholar]
- 32.Shughrue PJ, Ky B, Austin CP. Localization of B1 bradykinin receptor mRNA in the primate brain and spinal cord: an in situ hybridization study. J Comp Neurol. 2003;465(3):372–384. doi: 10.1002/cne.10846. [DOI] [PubMed] [Google Scholar]
- 33.Raidoo DM, Bhoola KD. Kinin receptors on human neurones. J Neuroimmunol. 1997;77(1):39–44. doi: 10.1016/S0165-5728(97)00048-9. [DOI] [PubMed] [Google Scholar]
- 34.Marceau F, et al. Pharmacology of kinins: their relevance to tissue injury and inflammation. Gen Pharmacol. 1983;14(2):209–229. doi: 10.1016/0306-3623(83)90001-0. [DOI] [PubMed] [Google Scholar]
- 35.Ghebrehiwet B, et al. Soluble gC1qR is an autocrine signal that induces B1R expression on endothelial cells. J Immunol. 2014;192(1):377–384. doi: 10.4049/jimmunol.1302031. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Koumbadinga GA, et al. Effect of interferon-gamma on inflammatory cytokine-induced bradykinin B1 receptor expression in human vascular cells. Eur J Pharmacol. 2010;647(1–3):117–125. doi: 10.1016/j.ejphar.2010.08.008. [DOI] [PubMed] [Google Scholar]
- 37.Marceau F, Bachvarov DR. Kinin receptors. Clin Rev Allergy Immunol. 1998;16(4):385–401. doi: 10.1007/BF02737658. [DOI] [PubMed] [Google Scholar]
- 38.Zhang X, Tan F, Skidgel RA. Carboxypeptidase M is a positive allosteric modulator of the kinin B1 receptor. J Biol Chem. 2013;288(46):33226–33240. doi: 10.1074/jbc.M113.520791. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Wu J, et al. Identification of bradykinin receptors in clinical cancer specimens and murine tumor tissues. Int J Cancer. 2002;98(1):29–35. doi: 10.1002/ijc.10142. [DOI] [PubMed] [Google Scholar]
- 40.Bockmann S, Paegelow I. Kinins and kinin receptors: importance for the activation of leukocytes. J Leukoc Biol. 2000;68(5):587–592. [PubMed] [Google Scholar]
- 41.Walker K, Perkins M, Dray A. Kinins and kinin receptors in the nervous system. Neurochem Int. 1995;26(1):1–16. doi: 10.1016/0197-0186(94)00114-A. [DOI] [PubMed] [Google Scholar]
- 42.Blaukat A, et al. Determination of bradykinin B2 receptor in vivo phosphorylation sites and their role in receptor function. J Biol Chem. 2001;276(44):40431–40440. doi: 10.1074/jbc.M107024200. [DOI] [PubMed] [Google Scholar]
- 43.Pizard A, et al. Bradykinin-induced internalization of the human B2 receptor requires phosphorylation of three serine and two threonine residues at its carboxyl tail. J Biol Chem. 1999;274(18):12738–12747. doi: 10.1074/jbc.274.18.12738. [DOI] [PubMed] [Google Scholar]
- 44.Enquist J, et al. Kinins promote B2 receptor endocytosis and delay constitutive B1 receptor endocytosis. Mol Pharmacol. 2007;71(2):494–507. doi: 10.1124/mol.106.030858. [DOI] [PubMed] [Google Scholar]
- 45.Fortin JP, Bouthillier J, Marceau F. High agonist-independent clearance of rabbit kinin B1 receptors in cultured cells. Am J Physiol Heart Circ Physiol. 2003;284(5):H1647–H1654. doi: 10.1152/ajpheart.00884.2002. [DOI] [PubMed] [Google Scholar]
- 46.Brusco I, et al. Inhibitors of angiotensin I converting enzyme potentiate fibromyalgia-like pain symptoms via kinin receptors in mice. Eur J Pharmacol. 2021;895:173870. doi: 10.1016/j.ejphar.2021.173870. [DOI] [PubMed] [Google Scholar]
- 47.Goncalves ECD, et al. Bradykinin receptors play a critical role in the chronic post-ischaemia pain model. Cell Mol Neurobiol. 2021;41(1):63–78. doi: 10.1007/s10571-020-00832-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Falsetta ML, et al. A Role for bradykinin signaling in chronic vulvar pain. J Pain. 2016;17(11):1183–1197. doi: 10.1016/j.jpain.2016.07.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Naffah-Mazzacoratti Mda G, et al. What have we learned about the kallikrein-kinin and renin-angiotensin systems in neurological disorders? World J Biol Chem. 2014;5(2):130–140. doi: 10.4331/wjbc.v5.i2.130. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Bossi F, et al. Novel pathogenic mechanism and therapeutic approaches to angioedema associated with C1 inhibitor deficiency. J Allergy Clin Immunol. 2009;124(6):1303–1310. doi: 10.1016/j.jaci.2009.08.007. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Tschope C, Schultheiss HP, Walther T. Multiple interactions between the renin-angiotensin and the kallikrein-kinin systems: role of ACE inhibition and AT1 receptor blockade. J Cardiovasc Pharmacol. 2002;39(4):478–487. doi: 10.1097/00005344-200204000-00003. [DOI] [PubMed] [Google Scholar]
- 52.Albert-Weissenberger C, Siren AL, Kleinschnitz C. Ischemic stroke and traumatic brain injury: the role of the kallikrein-kinin system. Prog Neurobiol. 2013;101–102:65–82. doi: 10.1016/j.pneurobio.2012.11.004. [DOI] [PubMed] [Google Scholar]
- 53.Kayashima Y, Smithies O, Kakoki M. The kallikrein-kinin system and oxidative stress. Curr Opin Nephrol Hypertens. 2012;21(1):92–96. doi: 10.1097/MNH.0b013e32834d54b1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Kakoki M, Smithies O. The kallikrein-kinin system in health and in diseases of the kidney. Kidney Int. 2009;75(10):1019–1030. doi: 10.1038/ki.2008.647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Kaplan AP, Ghebrehiwet B. Pathways for bradykinin formation and interrelationship with complement as a cause of edematous lung in COVID-19 patients. J Allergy Clin Immunol. 2021;147(2):507–509. doi: 10.1016/j.jaci.2020.10.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Oschatz C, et al. Mast cells increase vascular permeability by heparin-initiated bradykinin formation in vivo. Immunity. 2011;34(2):258–268. doi: 10.1016/j.immuni.2011.02.008. [DOI] [PubMed] [Google Scholar]
- 57.Brunnee T, et al. Mast cell derived heparin activates the contact system: a link to kinin generation in allergic reactions. Clin Exp Allergy. 1997;27(6):653–663. doi: 10.1111/j.1365-2222.1997.tb01193.x. [DOI] [PubMed] [Google Scholar]
- 58.Motta Junior JDS, et al. Mast cells in alveolar septa of COVID-19 patients a pathogenic pathway that may link interstitial edema to immunothrombosis. Front Immunol. 2020;11:574862. doi: 10.3389/fimmu.2020.574862. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.van de Veerdonk FL, et al. Kallikrein-kinin blockade in patients with COVID-19 to prevent acute respiratory distress syndrome. Elife. 2020 doi: 10.7554/eLife.57555. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Sodhi CP, et al. Attenuation of pulmonary ACE2 activity impairs inactivation of des-Arg(9) bradykinin/BKB1R axis and facilitates LPS-induced neutrophil infiltration. Am J Physiol Lung Cell Mol Physiol. 2018;314(1):L17–L31. doi: 10.1152/ajplung.00498.2016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Hoffmann M, et al. SARS-CoV-2 cell entry depends on ACE2 and TMPRSS2 and is blocked by a clinically proven protease inhibitor. Cell. 2020;181(2):271–280. doi: 10.1016/j.cell.2020.02.052. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Xu X, et al. Evolution of the novel coronavirus from the ongoing Wuhan outbreak and modeling of its spike protein for risk of human transmission. Sci China Life Sci. 2020;63(3):457–460. doi: 10.1007/s11427-020-1637-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Vickers C, et al. Hydrolysis of biological peptides by human angiotensin-converting enzyme-related carboxypeptidase. J Biol Chem. 2002;277(17):14838–14843. doi: 10.1074/jbc.M200581200. [DOI] [PubMed] [Google Scholar]
- 64.Dicpinigaitis PV. Angiotensin-converting enzyme inhibitor-induced cough: ACCP evidence-based clinical practice guidelines. Chest. 2006;129(1 Suppl):169S–173S. doi: 10.1378/chest.129.1_suppl.169S. [DOI] [PubMed] [Google Scholar]
- 65.Meini S, et al. Olfactory and gustatory dysfunctions in 100 patients hospitalized for COVID-19: sex differences and recovery time in real-life. Eur Arch Otorhinolaryngol. 2020;277(12):3519–3523. doi: 10.1007/s00405-020-06102-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 66.Scangas GA, Bleier BS. Anosmia: Differential diagnosis, evaluation, and management. Am J Rhinol Allergy. 2017;31(1):3–7. doi: 10.2500/ajra.2017.31.4403. [DOI] [PubMed] [Google Scholar]
- 67.Zhu L, et al. Role of prolylcarboxypeptidase in angiotensin II type 2 receptor-mediated bradykinin release in mouse coronary artery endothelial cells. Hypertension. 2010;56(3):384–390. doi: 10.1161/HYPERTENSIONAHA.110.155051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Ruocco G, Feola M, Palazzuoli A. Hypertension prevalence in human coronavirus disease: the role of ACE system in infection spread and severity. Int J Infect Dis. 2020;95:373–375. doi: 10.1016/j.ijid.2020.04.058. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Jamilloux Y, et al. Should we stimulate or suppress immune responses in COVID-19? Cytokine and anti-cytokine interventions. Autoimmun Rev. 2020;19(7):102567. doi: 10.1016/j.autrev.2020.102567. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Liu Y, et al. Clinical and biochemical indexes from 2019-nCoV infected patients linked to viral loads and lung injury. Sci China Life Sci. 2020;63(3):364–374. doi: 10.1007/s11427-020-1643-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Spagnolo P, et al. Pulmonary fibrosis secondary to COVID-19: a call to arms? Lancet Respir Med. 2020;8(8):750–752. doi: 10.1016/S2213-2600(20)30222-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Frater JL, et al. COVID-19 and the clinical hematology laboratory. Int J Lab Hematol. 2020;42(Suppl 1):11–18. doi: 10.1111/ijlh.13229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Thachil J. The versatile heparin in COVID-19. J Thromb Haemost. 2020;18(5):1020–1022. doi: 10.1111/jth.14821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Lillicrap D. Disseminated intravascular coagulation in patients with 2019-nCoV pneumonia. J Thromb Haemost. 2020;18(4):786–787. doi: 10.1111/jth.14781. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Gattinoni L, Chiumello D, Rossi S. COVID-19 pneumonia: ARDS or not? Crit Care. 2020;24(1):154. doi: 10.1186/s13054-020-02880-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.Green SJ. Covid-19 accelerates endothelial dysfunction and nitric oxide deficiency. Microbes Infect. 2020;22(4–5):149–150. doi: 10.1016/j.micinf.2020.05.006. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Varga Z, et al. Endothelial cell infection and endotheliitis in COVID-19. Lancet. 2020;395(10234):1417–1418. doi: 10.1016/S0140-6736(20)30937-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Desmazes C, Gauthier F, Lalmanach G. Cathepsin L, but not cathepsin B, is a potential kininogenase. Biol Chem. 2001;382(5):811–815. doi: 10.1515/bchm.2001.382.5.811. [DOI] [PubMed] [Google Scholar]
- 79.Desmazes C, et al. Kininogen-derived peptides for investigating the putative vasoactive properties of human cathepsins K and L. Eur J Biochem. 2003;270(1):171–178. doi: 10.1046/j.1432-1033.2003.03382.x. [DOI] [PubMed] [Google Scholar]
- 80.Puzer L, et al. A possible alternative mechanism of kinin generation in vivo by cathepsin L. Biol Chem. 2005;386(7):699–704. doi: 10.1515/BC.2005.081. [DOI] [PubMed] [Google Scholar]
- 81.Cure E, Cumhur Cure M, Vatansev H. Central involvement of SARS-CoV-2 may aggravate ARDS and hypertension. J Renin Angiotensin Aldosterone Syst. 2020;21(4):14703203. doi: 10.1177/1470320320972015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.Fan E, Brodie D, Slutsky AS. Acute respiratory distress syndrome: advances in diagnosis and treatment. JAMA. 2018;319(7):698–710. doi: 10.1001/jama.2017.21907. [DOI] [PubMed] [Google Scholar]
- 83.Krankel N, et al. Role of kinin B2 receptor signaling in the recruitment of circulating progenitor cells with neovascularization potential. Circ Res. 2008;103(11):1335–1343. doi: 10.1161/CIRCRESAHA.108.179952. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Chao J, et al. Kinin infusion prevents renal inflammation, apoptosis, and fibrosis via inhibition of oxidative stress and mitogen-activated protein kinase activity. Hypertension. 2007;49(3):490–497. doi: 10.1161/01.HYP.0000255925.01707.eb. [DOI] [PubMed] [Google Scholar]
- 85.Gross GJ, et al. Abdominal surgical incision induces remote preconditioning of trauma (RPCT) via activation of bradykinin receptors (BK2R) and the cytochrome P450 epoxygenase pathway in canine hearts. Cardiovasc Drugs Ther. 2011;25(6):517–522. doi: 10.1007/s10557-011-6321-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Penna C, et al. Intermittent activation of bradykinin B2 receptors and mitochondrial KATP channels trigger cardiac postconditioning through redox signaling. Cardiovasc Res. 2007;75(1):168–177. doi: 10.1016/j.cardiores.2007.03.001. [DOI] [PubMed] [Google Scholar]
- 87.Yin H, et al. Differential role of kinin B1 and B2 receptors in ischemia-induced apoptosis and ventricular remodeling. Peptides. 2007;28(7):1383–1389. doi: 10.1016/j.peptides.2007.05.010. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Feng J, et al. Bradykinin preconditioning improves the profile of cell survival proteins and limits apoptosis after cardioplegic arrest. Circulation. 2005;112(9 Suppl):I190–I195. doi: 10.1161/CIRCULATIONAHA.104.524454. [DOI] [PubMed] [Google Scholar]
- 89.Potier L, et al. Selective kinin receptor agonists as cardioprotective agents in myocardial ischemia and diabetes. J Pharmacol Exp Ther. 2013;346(1):23–30. doi: 10.1124/jpet.113.203927. [DOI] [PubMed] [Google Scholar]
- 90.Blaes N, Girolami JP. Targeting the 'Janus face' of the B2-bradykinin receptor. Expert Opin Ther Targets. 2013;17(10):1145–1166. doi: 10.1517/14728222.2013.827664. [DOI] [PubMed] [Google Scholar]
- 91.Yao YY, et al. Tissue kallikrein and kinin infusion rescues failing myocardium after myocardial infarction. J Card Fail. 2007;13(7):588–596. doi: 10.1016/j.cardfail.2007.04.009. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Wei CC, et al. Cardiac kallikrein-kinin system is upregulated in chronic volume overload and mediates an inflammatory induced collagen loss. PLoS ONE. 2012;7(6):e40110. doi: 10.1371/journal.pone.0040110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Petho G, Reeh PW. Sensory and signaling mechanisms of bradykinin, eicosanoids, platelet-activating factor, and nitric oxide in peripheral nociceptors. Physiol Rev. 2012;92(4):1699–1775. doi: 10.1152/physrev.00048.2010. [DOI] [PubMed] [Google Scholar]
- 94.Qin C, et al. Bradykinin is involved in the mediation of cardiac nociception during ischemia through upper thoracic spinal neurons. Curr Neurovasc Res. 2009;6(2):89–94. doi: 10.2174/156720209788185623. [DOI] [PubMed] [Google Scholar]
- 95.Offermanns S. Activation of platelet function through G protein-coupled receptors. Circ Res. 2006;99(12):1293–1304. doi: 10.1161/01.RES.0000251742.71301.16. [DOI] [PubMed] [Google Scholar]
- 96.Birbrair A, et al. Type-1 pericytes accumulate after tissue injury and produce collagen in an organ-dependent manner. Stem Cell Res Ther. 2014;5(6):122. doi: 10.1186/scrt512. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 97.Wynn TA. Fibrotic disease and the T(H)1/T(H)2 paradigm. Nat Rev Immunol. 2004;4(8):583–594. doi: 10.1038/nri1412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Schanstra JP, et al. In vivo bradykinin B2 receptor activation reduces renal fibrosis. J Clin Invest. 2002;110(3):371–379. doi: 10.1172/JCI0215493. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99.Kakoki M, et al. Bradykinin B1 and B2 receptors both have protective roles in renal ischemia/reperfusion injury. Proc Natl Acad Sci U S A. 2007;104(18):7576–7581. doi: 10.1073/pnas.0701617104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 100.Zhang JJ, et al. Tissue kallikrein attenuates salt-induced renal fibrosis by inhibition of oxidative stress. Kidney Int. 2004;66(2):722–732. doi: 10.1111/j.1523-1755.2004.00794.x. [DOI] [PubMed] [Google Scholar]
- 101.Madeddu P, et al. Angiotensin II type 1 receptor blockade prevents cardiac remodeling in bradykinin B(2) receptor knockout mice. Hypertension. 2000;35(1 Pt 2):391–396. doi: 10.1161/01.HYP.35.1.391. [DOI] [PubMed] [Google Scholar]
- 102.Takemoto M, et al. Chronic angiotensin-converting enzyme inhibition and angiotensin II type 1 receptor blockade: effects on cardiovascular remodeling in rats induced by the long-term blockade of nitric oxide synthesis. Hypertension. 1997;30(6):1621–1627. doi: 10.1161/01.HYP.30.6.1621. [DOI] [PubMed] [Google Scholar]
- 103.Veeravalli KK, Akula A. Involvement of nitric oxide and prostaglandin pathways in the cardioprotective actions of bradykinin in rats with experimental myocardial infarction. Pharmacol Res. 2004;49(1):23–29. doi: 10.1016/j.phrs.2003.07.010. [DOI] [PubMed] [Google Scholar]
- 104.Yin H, Chao L, Chao J. Kallikrein/kinin protects against myocardial apoptosis after ischemia/reperfusion via Akt-glycogen synthase kinase-3 and Akt-Bad.14–3–3 signaling pathways. J Biol Chem. 2005;280(9):8022–8030. doi: 10.1074/jbc.M407179200. [DOI] [PubMed] [Google Scholar]
- 105.Xie P, et al. Activation of NF-kappa B by bradykinin through a Galpha(q)- and Gbeta gamma-dependent pathway that involves phosphoinositide 3-kinase and Akt. J Biol Chem. 2000;275(32):24907–24914. doi: 10.1074/jbc.M001051200. [DOI] [PubMed] [Google Scholar]
- 106.Lesage A, et al. In Vitro Pharmacological Profile of a New Small Molecule Bradykinin B2 Receptor Antagonist. Front Pharmacol. 2020;11:916. doi: 10.3389/fphar.2020.00916. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 107.Campos MM, et al. Non-peptide antagonists for kinin B1 receptors: new insights into their therapeutic potential for the management of inflammation and pain. Trends Pharmacol Sci. 2006;27(12):646–651. doi: 10.1016/j.tips.2006.10.007. [DOI] [PubMed] [Google Scholar]
- 108.Marceau F, Regoli D. Bradykinin receptor ligands: therapeutic perspectives. Nat Rev Drug Discov. 2004;3(10):845–852. doi: 10.1038/nrd1522. [DOI] [PubMed] [Google Scholar]
- 109.Rhaleb NE, et al. Structure-activity studies of bradykinin and related peptides B2-receptor antagonists. Hypertension. 1991;17(1):107–115. doi: 10.1161/01.HYP.17.1.107. [DOI] [PubMed] [Google Scholar]
- 110.Vavrek RJ, Stewart JM. Competitive antagonists of bradykinin. Peptides. 1985;6(2):161–164. doi: 10.1016/0196-9781(85)90033-6. [DOI] [PubMed] [Google Scholar]
- 111.Wirth K, et al. Hoe 140 a new potent and long acting bradykinin-antagonist: in vivo studies. Br J Pharmacol. 1991;102(3):774–777. doi: 10.1111/j.1476-5381.1991.tb12249.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112.Regoli D, et al. Kinin receptor subtypes. J Cardiovasc Pharmacol. 1990;15(Suppl 6):S30–S38. doi: 10.1097/00005344-199015061-00007. [DOI] [PubMed] [Google Scholar]
- 113.Whalley ET, et al. Discovery and therapeutic potential of kinin receptor antagonists. Expert Opin Drug Discov. 2012;7(12):1129–1148. doi: 10.1517/17460441.2012.729038. [DOI] [PubMed] [Google Scholar]
- 114.Hock FJ, et al. Hoe 140 a new potent and long acting bradykinin-antagonist: in vitro studies. Br J Pharmacol. 1991;102(3):769–773. doi: 10.1111/j.1476-5381.1991.tb12248.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 115.Gobeil F, Regoli D. Characterization of kinin receptors by bioassays. Braz J Med Biol Res. 1994;27(8):1781–1791. [PubMed] [Google Scholar]
- 116.Lembeck F, et al. New, long-acting, potent bradykinin antagonists. Br J Pharmacol. 1991;102(2):297–304. doi: 10.1111/j.1476-5381.1991.tb12169.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Akbary AM, Wirth KJ, Scholkens BA. Efficacy and tolerability of Icatibant (Hoe 140) in patients with moderately severe chronic bronchial asthma. Immunopharmacology. 1996;33(1–3):238–242. doi: 10.1016/0162-3109(96)00065-3. [DOI] [PubMed] [Google Scholar]
- 118.Austin CE, Foreman JC, Scadding GK. Reduction by Hoe 140, the B2 kinin receptor antagonist, of antigen-induced nasal blockage. Br J Pharmacol. 1994;111(4):969–971. doi: 10.1111/j.1476-5381.1994.tb14835.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.Dray A, Perkins M. Bradykinin and inflammatory pain. Trends Neurosci. 1993;16(3):99–104. doi: 10.1016/0166-2236(93)90133-7. [DOI] [PubMed] [Google Scholar]
- 120.McNeil BD, et al. Identification of a mast-cell-specific receptor crucial for pseudo-allergic drug reactions. Nature. 2015;519(7542):237–241. doi: 10.1038/nature14022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 121.Cicardi M, et al. Icatibant, a new bradykinin-receptor antagonist, in hereditary angioedema. N Engl J Med. 2010;363(6):532–541. doi: 10.1056/NEJMoa0906393. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Cheronis JC, et al. A new class of bradykinin antagonists: synthesis and in vitro activity of bissuccinimidoalkane peptide dimers. J Med Chem. 1992;35(9):1563–1572. doi: 10.1021/jm00087a010. [DOI] [PubMed] [Google Scholar]
- 123.Gessi S, et al. Human vascular kinin receptors of the B2 type characterized by radioligand binding. Br J Pharmacol. 1997;122(7):1450–1454. doi: 10.1038/sj.bjp.0701536. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124.Scherrer D, et al. Effects of WIN 64338, a nonpeptide bradykinin B2 receptor antagonist, on guinea-pig trachea. Br J Pharmacol. 1995;115(7):1127–1128. doi: 10.1111/j.1476-5381.1995.tb15013.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Farmer SG, DeSiato MA. Effects of a novel nonpeptide bradykinin B2 receptor antagonist on intestinal and airway smooth muscle: further evidence for the tracheal B3 receptor. Br J Pharmacol. 1994;112(2):461–464. doi: 10.1111/j.1476-5381.1994.tb13095.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Inamura N, et al. Characterization of FR173657, a novel nonpeptide B2 antagonist: in vitro and in vivo studies. Can J Physiol Pharmacol. 1997;75(6):622–628. doi: 10.1139/y97-021. [DOI] [PubMed] [Google Scholar]
- 127.Aramori I, et al. Novel subtype-selective nonpeptide bradykinin receptor antagonists FR167344 and FR173657. Mol Pharmacol. 1997;51(2):171–176. doi: 10.1124/mol.51.2.171. [DOI] [PubMed] [Google Scholar]
- 128.Simmon VF. Response to The BRAIN TRIAL a randomised, placebo controlled trial of a Bradykinin B2 receptor antagonist (Anatibant) in patients with traumatic brain injury. Trials. 2009;10:110. doi: 10.1186/1745-6215-10-110. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Shakur H, et al. The BRAIN TRIAL: a randomised, placebo controlled trial of a Bradykinin B2 receptor antagonist (Anatibant) in patients with traumatic brain injury. Trials. 2009;10:109. doi: 10.1186/1745-6215-10-109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Pruneau D, et al. Pharmacological profile of LF 16–0687, a new potent non-peptide bradykinin B2 receptor antagonist. Immunopharmacology. 1999;43(2–3):187–194. doi: 10.1016/S0162-3109(99)00128-9. [DOI] [PubMed] [Google Scholar]
- 131.Gomis A, et al. Blockade of nociceptive sensory afferent activity of the rat knee joint by the bradykinin B2 receptor antagonist fasitibant. Osteoarthritis Cartilage. 2013;21(9):1346–1354. doi: 10.1016/j.joca.2013.03.013. [DOI] [PubMed] [Google Scholar]
- 132.Valenti C, et al. MEN16132, a novel potent and selective nonpeptide kinin B2 receptor antagonist: in vivo activity on bradykinin-induced bronchoconstriction and nasal mucosa microvascular leakage in anesthetized guinea pigs. J Pharmacol Exp Ther. 2005;315(2):616–623. doi: 10.1124/jpet.105.088252. [DOI] [PubMed] [Google Scholar]
- 133.Kenniston JA, et al. Inhibition of plasma kallikrein by a highly specific active site blocking antibody. J Biol Chem. 2014;289(34):23596–23608. doi: 10.1074/jbc.M114.569061. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 134.Wu MA. Lanadelumab for the treatment of hereditary angioedema. Expert Opin Biol Ther. 2019;19(12):1233–1245. doi: 10.1080/14712598.2019.1685490. [DOI] [PubMed] [Google Scholar]
- 135.Kaplon H, Reichert JM. Antibodies to watch in 2019. MAbs. 2019;11(2):219–238. doi: 10.1080/19420862.2018.1556465. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136.Balaguer JM, et al. Contribution of endogenous bradykinin to fibrinolysis, inflammation, and blood product transfusion following cardiac surgery: a randomized clinical trial. Clin Pharmacol Ther. 2013;93(4):326–334. doi: 10.1038/clpt.2012.249. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Charignon D, et al. Icatibant, the bradykinin B2 receptor antagonist with target to the interconnected kinin systems. Expert Opin Pharmacother. 2012;13(15):2233–2247. doi: 10.1517/14656566.2012.723692. [DOI] [PubMed] [Google Scholar]
- 138.Marmarou A, et al. Effects of the bradykinin antagonist Bradycor (deltibant, CP-1027) in severe traumatic brain injury: results of a multi-center, randomized, placebo-controlled trial. American Brain Injury Consortium Study Group. J Neurotrauma. 1999;16(6):431–444. doi: 10.1089/neu.1999.16.431. [DOI] [PubMed] [Google Scholar]
- 139.Narotam PK, et al. Traumatic brain contusions: a clinical role for the kinin antagonist CP-0127. Acta Neurochir (Wien) 1998;140(8):793–802. doi: 10.1007/s007010050181. [DOI] [PubMed] [Google Scholar]
- 140.Fein AM, et al. Treatment of severe systemic inflammatory response syndrome and sepsis with a novel bradykinin antagonist, deltibant (CP-0127). Results of a randomized, double-blind, placebo-controlled trial CP-0127 SIRS and Sepsis Study Group. JAMA. 1997;277(6):482–487. doi: 10.1001/jama.1997.03540300050033. [DOI] [PubMed] [Google Scholar]
- 141.Lesage A, et al. In vitro pharmacological profile of PHA-022121, a small molecule bradykinin B2 receptor antagonist in clinical development. Int Immunopharmacol. 2022;105:108523. doi: 10.1016/j.intimp.2022.108523. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
Not Applicable.