Abstract
The healthcare system of Ukraine was already suffering from several shortfalls before February 2022, but the war of aggression started by the Russian leadership is poised to inflict a further severe blow that will have long-lasting consequences for the health of all Ukrainians. In pre-war Ukraine, noncommunicable diseases (NCDs) contributed to 91% of deaths, especially cardiovascular diseases (67%). Ukrainians have a high prevalence of risk factors for NCDs ranking among the highest levels reported by the World Health Organization (WHO) in the European (EU) Region. Cardiovascular disease is one of the key health risks for the conflict-affected Ukrainian population due to significant limitations in access to health care and interruptions in the supply of medicines and resources. The excess mortality observed during the COVID-19 pandemic, due to a combination of viral illness and chronic disease states, is bound to increase exponentially from poorly treated NCDs. In this report, we discuss the impact of the war on the public health of Ukraine and potential interventions to provide remote health assistance to the Ukrainian population.
Keywords: Ukraine, War, Healthcare systems, Cardiovascular disease, Remote monitoring
1. Introduction
Since time untold humankind has initiated wars under unclear or fake pretenses. None of them could ever be considered remotely acceptable by a humanity that should be striving to coexist as a unified community, fighting together for a mankind concerned with a world that is rapidly coming dangerously close to its limit of survival. While aiming to reap the spoils of war, the aggressors inevitably spoil the living conditions of entire nations, populations, or ethnicities for a very long time to come. On February 24, 2022 the Russian leadership unleashed an unprovoked military attack on Ukraine, on the wings of heightened tensions over the ongoing conflict in eastern Ukraine. Since Russian troops invaded Ukraine, innumerable attacks on civilians and civilian structures have been reported across the entire country with alarming numbers of civilian casualties. By the beginning of May 2022, over 5,8 million people had already fled Ukraine, seeking refuge in neighboring countries (3.2 million in Poland, 0.86 million in Romania, and 0.56 million in Hungary), with many more being internally displaced in search of protection and assistance [1]. The conflict escalation has devastated the infrastructure of Ukraine; by the end of April 2022, the World Health Organization (WHO) had already recorded 200 attacks on the healthcare system, impacting facilities, transport, and supplies, and 75 deaths and 54 injuries among patients and medical personnel [2]. These numbers are most likely much larger by now and growing. The healthcare system of Ukraine was already suffering from several shortfalls before February 2022, but the war is poised to inflict a further severe blow that will have long-lasting consequences for the health of all Ukrainians. Unfortunately, the long-term consequences of wars are paid most dearly by fragile members of society, such as the elderly, women, children, displaced refugees, and the sick and poor. As healthcare providers involved in a daily struggle to save a single life at the time, and health scientists we cannot stand by silently in front of atrocities that destroy the lives of thousands in a matter of days. The aim of this article is to provide a brief overview of the population health in pre-war Ukraine, and to put forward a proposal on what democratic nations can do to help mitigate the health crisis in Ukraine.
2. Pre-war in Ukraine
Communicable diseases, including tuberculosis (TB) and human immunodeficiency virus (HIV) infection, constitute a serious public health issue and priority in Ukraine [3]. The country has the fourth-highest TB incidence rate among WHO EU countries, and the second-highest prevalence of HIV/TB coinfection (26%), with drug-resistant TB representing 29% of new diagnoses [4]. Ukraine has an extremely high prevalence of HIV infection compared to other western countries in the WHO EU Region (37.5 vs 8.3 per 100,000 in 2020) [5], with a treatment coverage of 57%, lower than in the EU (82%) [3]. The COVID-19 epidemic is also concerning, with a significant increase (555%) in cases between January–February 2022, a fatality rate of 2.2%, and a very low vaccination rate (35%) [6]. Unfortunately, the vaccination rate against other infectious diseases, such as poliomyelitis, measles, rubella, was also relatively low (53%–85%) in the pre-war times [[7], [8], [9]].
Noncommunicable diseases (NCDs) in Ukraine contribute to 91% of deaths, especially cardiovascular diseases (67%), with an age-adjusted death rate for ischemic heart disease (IHD) more than six times higher than in other EU countries [10]. According to pre-war estimates issued by the European Society of Cardiology (ESC), the pre-war cardiovascular disease (CVD) mortality rate in Ukraine was nearly 800/100,000 for men and 1000/100,000 for women, compared to 328/100,000 and 311/100,000, respectively in European high-income countries, and 449/100,000 and 458/100,000, in European middle-income countries [11]. This accounted for more than two thirds of the total mortality in the country. Cardiovascular preventive care in Ukraine is delivered both by family doctors and by cardiologists, employed at state medical facilities (hospitals, outpatient clinics) and in private medical facilities [12]. The Ukrainian population has one of the highest rates of risk factors for cardiovascular disease in the WHO EU Region. The prevalence of overweightness in 2019 was 59% and nearly a quarter of Ukrainians were obese [10]. Diabetes prevalence in adults amounts to 7.1% [10]. A survey of children and teenagers in Ukraine in 2010–2013 showed a rate of obesity of 17.2% [12]. Over 40% of the population had elevated total blood cholesterol levels (defined as ≥ 5.0 mmol/L) or were taking hypolipemic medications. Overall, only 11% were at lipid target, and among very high-risk secondary prevention patients only 9% were at target [13]. Alcohol consumption and tobacco use are also very frequent. Nearly 35% of the Ukrainian population suffer from systemic hypertension or receive anti-hypertensive medications [10], with incomplete blood pressure control reported in 85% of cases [14]. The National program on prophylaxis and treatment of hypertension (1999–2005) (decree of president of Ukraine on February 04, 1999 No. 117/99) and the State Program of prevention and treatment of cardiovascular and cerebrovascular diseases (2006–2010) (resolution of cabinet of ministers May 31, 2006 No.761) have been implemented over the years to improve the overall cardiovascular health of the population. However, the prevalence of hypertension has not changed and over time the total risk factor burden in the male population has increased: the number of men with a single risk factor has decreased by 2.6 times, while the number of men with three and more risk factors has increased fivefold [12].
3. The Ukrainian healthcare system has been disrupted by war
Disruptions to the Ukrainian healthcare services pose a grave long-term risk for many patients but especially those with chronic cardiovascular conditions, cancer, and cardiometabolic disorders. An ongoing conflict triggers the flight of staff, leaving understaffed health systems to cope with growing patient loads caused by combat [15]. Healthcare workers have been injured, killed, or had to leave their homes, all of which has turned into shortages of medical personnel and medical supplies because of interruption of delivery patterns and supply chains.
Furthermore, the damaging of hospitals and clinics imposes additional risk for the health of all citizens. Attacks on healthcare facilities have been a prominent -- and shocking -- feature of the war in Ukraine. As of end of April 2022, the WHO confirmed that 200 attacks had already targeted healthcare facilities, workers, supplies, vehicles, and patients, with more than 300 healthcare facilities located in areas where there are active hostilities and therefore at risk of damage [2]. The number of hospitals rendered inactive is expected to rise with the escalation of the conflict. According to the former Ukrainian Deputy Minister of Health, who is working with a team evaluating the damage brought to Ukraine's health facilities, the healthcare infrastructure of whole cities has been devastated [16]. Damaged and mined roads further limit the access to healthcare facilities. Thus, the war will likely hurt the health of Ukrainian citizens for a long time to come, with profound socio-economic consequences.
Primary care, screening, and immunization programs have been disrupted. This means that people with chronic diseases such as coronary artery disease, heart failure, diabetes mellitus, chronic kidney disease etc., despite ongoing international medical aid, may not get optimal treatment –or no treatment at all [15]. No clinical monitoring can be provided to fragile patients outside of acute care facilities. Owing to a lack of access to medical care, such as insulin, antithrombotic and antiplatelet therapies, lipid lowering therapies, and antihypertensive agents, patients suffering from chronic disease states will require immediate medical attention when crossing a border into another nation [17]. For each direct war casualty, there might be many more indirect casualties because of the impact of war. Global action is urgently needed to provide immediate medical and humanitarian assistance to the people affected [18].
4. Cardiovascular health in times of war
Cardiovascular diseases have been identified as one of the key health risks for the conflict-stricken Ukrainian population due to significant limitations in access to healthcare and interruptions in the supply chains. Increasing rates of acute myocardial infarction and stroke may result in high excess mortality over the coming months; however, the highest mortality rate is expected for the immediate term obviously due to war casualties. The uninterrupted continuation of medical assistance is especially critical for people with uncontrolled blood pressure and at risk of cardiovascular events. A high risk of renal failure and other life-threatening conditions due to NCDs requiring continuity of care has been identified among the refugee population [14]. It is worth emphasizing that considerable numbers of patients with severe conditions and/or requiring special long-term treatments, e.g., hemodialysis, have been transported to neighboring countries to ensure continuation of medical care. However, cases of sudden death from arrhythmias, myocardial infarction, heart failure or worsening underlying conditions are increasingly being reported among refugees or hospitalized Ukrainians, often under-assisted due to shortage of personnel and resources [19]. The impact of mental disorders resulting from the stress of war (including post-traumatic stress disorders), will possibly be measured in an increase in substance abuse, obesity, and cardiometabolic disorders. There is an urgent need to act swiftly to reduce the impact of all of these societal stressors.
5. What the developed world can do to help
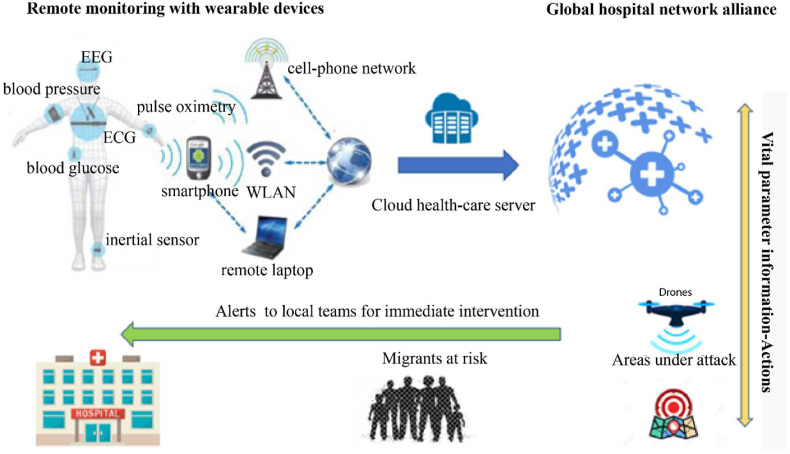
First and foremost, it is imperative for the benefit of all Ukrainians and the entire World, to immediately cease all hostilities with return of a lasting peace and restoration of normal trades and cooperation between nations. Ukraine supplies a very sizeable portion of the grains used around the globe, and without its contribution many nations will suffer from shortages that may spar new protests and even armed revolts. Meanwhile, several nations have come to the help of displaced Ukrainian refugees and have sent humanitarian aides and financial support to Ukraine. Non-governmental organizations such as the International Red Cross or Médecins Sans Frontières are providing lifesaving aid and medical care to the people caught up in the contested parts of Ukraine, as well as those who fled the fighting to safer parts of Ukraine or neighboring countries. They secure shelter, fresh water, and food, as well as equipment, and drugs for emergency care and acute treatments. They provide training of para-medical personnel in first aid, but also programs to combat tuberculosis, HIV, and COVID-19 [20,21]. Wealthy nations and each capable individual should consider supporting the efforts of these and other noble organizations. As a bridge to an auspicious end of the conflict, we propose to utilize modern technology to take a few more steps to attempt to save the lives of patients with cardiovascular conditions (Fig. 1 ).
Fig. 1.
Proposed remote health support for Ukraine.
Patient vital data are transferred through wearable devices to a network of hospitals and clinics, that can send alerts to local teams in Ukraine as well as those assisting migrants, when the values of these parameters are abnormal. Drones might be used to provide drug supplies, small diagnostic equipment and defibrillators to areas under attack. ECG = electrocardiography; EEG = electroencephalogram.
5.1. Remote clinical monitoring with wearable devices
A potentially life-saving project for the people of Ukraine could revolve around the provision of remote vital signs monitoring for individuals with known - or at risk of - cardiovascular disease. Wearable remote monitoring devices have been successfully used in the outpatient setting. This digital technology can help capture relevant data, such as heart rhythm, blood pressure, oxygen saturation, blood glucose, electrocardiographic tracings, and electronically transmit them to remote healthcare facilities [22]. Devices could be initially limited to track the health of patients at highest risk, admitted to Ukrainian medical facilities with limited assistance capabilities. To enhance the diagnostic yield, single devices could be worn in series by multiple subjects and tailored to individual risk. Selected hospitals in the European Union or worldwide, that have already agreed to provide other healthcare measures for Ukrainians, could remotely track the health status of people at risk or suffering from an acute event and intervene by informing local teams to provide specific and available therapies on site.
5.2. Medical supplies delivery via drones
Drones, also known as unmanned aerial vehicles (UAV), are aircrafts operated remotely by a human pilot (remotely-piloted aircraft: RPA), or with various degrees of autonomy, such as autopilot assistance [23]. The flight range can vary based on the model and reach over 200 km in the most advanced, long-endurance ones. Drones could therefore be used to deliver drug supplies and small diagnostic equipment within a wide range of kilometers. The most immediate need would be for essential drugs, such as antiseptics and antibiotics for the wounded, to be delivered near the front or to sites where first aid is provided. Prevention of cardiovascular events is not a high-ranking goal in the immediate, as limited resources and medical professionals make individualized risk factor control difficult or even impossible. However, it remains an important long-term goal to reduce the burden of cardiovascular disease. In this situation, a polypill approach combining fixed dosages of a statin and blood pressure lowering agents with or without aspirin may be the most effective approach. A recent meta-analysis of three large randomized and placebo-controlled trials (TIPS-3, HOPE-3, and PolyIran) encompassing 9038 women and 9124 men, with a mean age of 63 years and a mean follow-up of five years, showed the efficacy and safety of this strategy for primary prevention [24]. We are familiar with the importance of immediate defibrillation to improve survival following out-of-hospital cardiac arrest. Early defibrillation is crucial and has led to remarkable improvements in survival rates, reaching up to 90% in specific settings where it was optimally employed [25]. Drones could be used to deliver cardiac defibrillators in areas under attack without the need for in-person delivery, potentially improving survival [26]. Drones could be used to also transport small medical devices, blood products, vaccines, drugs and small diagnostic tools [27].
6. The spoils of war and the long-term spoiling of entire societies
The illusion that the spoils of war will make up for the suffering of the subjugated and their own people, has deluded many leaders and dictatorial regimes throughout the millennia of human history that preceded this day. It is distressing to observe that those responsible for war on foreign soil do not consider that, in addition to the casualties among their own soldiers, they will also damage the healthcare systems of entire nations for a very long time to follow. The interconnectedness of humankind is stronger today than ever before; a crack in a single link is and will be felt internationally for decades to come. The immediate consequences of a lack of health coverage are extreme, but the long-term consequences will be felt and span through several generations for millions of people. The ethical and financial costs are too high to not act now, and every effort must be made to contain the losses and stop the hemorrhage. The democratic nations of this world have a chance to come together to protect democracy and the lives of millions of people endangered by the spoiling of entire societies that is the natural outcome of any war.
Acknowledgements
No funding was received for this manuscript.
References
- 1.Ukraine refugee situation. Operational data portal. https://data2.unhcr.org/en/situations/ukraine
- 2.World Health Organization Surveillance system for attacks on health care (SSA) https://extranet.who.int/ssa/Index.aspx
- 3.European Centre for Disease Prevention and Control . 2022. Operational Considerations for the Prevention and Control of Infectious Diseases - Russia's Aggression towards Ukraine. [Google Scholar]
- 4.World Health Organization World Tuberculosis Day: supporting Ukraine in scaling up TB diagnosis and treatment. https://www.euro.who.int/en/countries/ukraine/news/news/2021/3/world-tuberculosis-day-supporting-ukraine-in-scaling-up-tb-diagnosis-and-treatment
- 5.European Centre for Disease Prevention and Control . 2019. HIV/AIDS Surveillance in Europe 2021 – 2020 Data. [Google Scholar]
- 6.Marchese V., Formenti B., Cocco N., et al. Examining the pre-war health burden of Ukraine for prioritisation by European countries receiving Ukrainian refugees. Lancet Reg Heal - Eur. 2022;15:100369. doi: 10.1016/j. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Immunization, measles The world bank data. https://data.worldbank.org/indicator/SH.IMM.MEAS?locations=UA
- 8.World Health Organization Ukraine: Immediate Steps Needed to Prevent a Measles Outbreak Due to the Ongoing War and Low Vaccination Rates. https://www.euro.who.int/en/media-centre/sections/press-releases/2022/ukraine-immediate-steps-needed-to-prevent-a-measles-outbreak-due-to-the-ongoing-war-and-low-vaccination-rates,-warns-who warns WHO.
- 9.Kluger J., Law T. Polio makes a comeback in Ukraine as war halts vaccination campaign. TIME. https://time.com/6155963/polio-ukraine-war/
- 10.World Health Organization . 2020. Risk Factors for Noncommunicable Diseases in Ukraine in 2019. Summary of Results from the WHO STEPS Survey and Comparison with Selected Countries. [Google Scholar]
- 11.Timmis A., Vardas P., Townsend N., et al. European Society of Cardiology: cardiovascular disease statistics 2021. Eur. Heart J. 2022;43(8):716–799. doi: 10.1093/EURHEARTJ/EHAB892. [DOI] [PubMed] [Google Scholar]
- 12.European Society of Cardiology EAPC Country of the Month – Ukraine. https://www.escardio.org/Sub-specialty-communities/European-Association-of-Preventive-Cardiology-(EAPC)/Advocacy/Prevention-in-your-country/country-of-the-month-ukraine
- 13.Vrablik M., Seifert B., Parkhomenko A., et al. Lipid-lowering therapy use in primary and secondary care in Central and Eastern Europe: DA VINCI observational study. Atherosclerosis. 2021;334:66–75. doi: 10.1016/J.ATHEROSCLEROSIS.2021.08.035. [DOI] [PubMed] [Google Scholar]
- 14.World Health Organization . 17 March 2022. Ukraine Crisis. Public Health Situation Analysis – Refugee-Hosting Countries; p. 2022. [Google Scholar]
- 15.Lee A. Ukraine: war has an impact on people's health beyond bullets and bombs. The Conversation. https://theconversation.com/ukraine-war-has-an-impact-on-peoples-health-beyond-bullets-and-bombs-178062
- 16.Attacks on Ukraine's Hospitals Will Cause Long-Term Harm to Health. https://reliefweb.int/report/ukraine/attacks-ukraine-s-hospitals-will-cause-long-term-harm-health ReliefWeb.
- 17.Jankowski M., Gujski M. The public health implications for the refugee population, particularly in Poland, due to the war in Ukraine. Med. Sci. Mon. Int. Med. J. Exp. Clin. Res. 2022;28 doi: 10.12659/MSM.936808. [DOI] [PubMed] [Google Scholar]
- 18.Southall D.P., MacDonald R., Kostiuk O., Shcherbakov V., Deierl A. The UN must provide secure medical and humanitarian assistance in Ukraine. Lancet. 2022;399(10332):1301–1302. doi: 10.1016/S0140-6736(22)00526-8. [DOI] [PubMed] [Google Scholar]
- 19.Health Cluster Ukraine . 3 March 2022. Ukraine Public Health Situation Analysis (PHSA) – Short-form; p. 2022. [Google Scholar]
- 20.Sans Frontières Médecins. Ukraine. https://www.msf.org/ukraine
- 21.International Committee of the Red Cross Where we work – Ukraine. https://www.icrc.org/en/where-we-work/europe-central-asia/ukraine
- 22.Soon S., Svavarsdottir H., Downey C., Jayne D.G. Wearable devices for remote vital signs monitoring in the outpatient setting: an overview of the field. BMJ Innov. 2020;6(2):55. doi: 10.1136/BMJINNOV-2019-000354. [DOI] [Google Scholar]
- 23.Cary L., Coyne J. 2011-2012 UAS Yearbook - UAS: the Global Perspective. ninth ed. Blyenburgh & Co; 2011. ICAO unmanned aircraft systems (UAS), circular 328; pp. 112–115. [Google Scholar]
- 24.Joseph P., Roshandel G., Gao P., et al. Fixed-dose combination therapies with and without aspirin for primary prevention of cardiovascular disease: an individual participant data meta-analysis. Lancet. 2021;398(10306):1133–1146. doi: 10.1016/S0140-6736(21)01827-4. [DOI] [PubMed] [Google Scholar]
- 25.Karam N., Jost D., Jouven X., Marijon E. Automated external defibrillator delivery by drones: are we ready for prime time? Eur. Heart J. 2022;43(15):1488–1490. doi: 10.1093/EURHEARTJ/EHAB565. [DOI] [PubMed] [Google Scholar]
- 26.Schierbeck S., Hollenberg J., Nord A., et al. Automated external defibrillators delivered by drones to patients with suspected out-of-hospital cardiac arrest. Eur. Heart J. 2022;43(15):1478–1487. doi: 10.1093/EURHEARTJ/EHAB498. [DOI] [PubMed] [Google Scholar]
- 27.Wimberley B. Drones in Healthcare: Blood Transportation and beyond. https://healthcaretransformers.com/healthcare-business/drones-healthcare/ HealthcareTransformers.