Abstract
Background
In this study, our aim was to present the 1-year results of the effect of thermal genicular nerve radiofrequency ablation (GNRFA) therapy on pain and functional outcomes in patients with advanced knee osteoarthritis.
Materials and Methods
After retrospectively examining the hospital records, 49 knees of 35 patients who had undergone thermal RFA of the superior medial, superior lateral, and inferior medial branches of the genicular nerve under fluoroscopic guidance between July 2019 and December 2020 were included in the study. The visual analog scale (VAS) scores of the patients were recorded before RFA, on the day of RFA, and at the first, sixth, and 12th months postoperatively, as well as their Western Ontario and McMaster Universities Arthritis Index (WOMAC) scores before RFA and at the 12th month postoperatively. Complications developed after the procedure and during the follow-up period were screened.
Results
Twenty-five of the patients were females and 10 males, with a mean age of 77.3 ± 7.9 years (range 61–92 years). The mean VAS score was 8.4 ± 0.9 before RFA, and as 1.7 ± 1.0 right after the procedure, 2.4 ± 1.7 at the first month, 3.4 ± 1.8 at the sixth month, and 4.4 ± 1.9 at the 12th month (p < 0.01). In terms of the WOMAC score, the average value was 69.7 ± 6.4 before the treatment and 36.1 ± 11.8 at the final follow-up at the 12th month (p < 0.01). No complications were observed in any patient during the treatment or the follow-up period.
Conclusion
Non-surgical thermal GNRFA therapy of knee osteoarthritis provides significant outcomes in terms of pain and functionality, with no significant systemic or local side effects. Therefore, the technique can be considered as an alternative to other methods when treating advanced osteoarthritis.
Keywords: Knee osteoarthritis, Pain, Radiofrequency ablation
Introduction
Non-surgical methods such as exercise, life modifications such as weight loss, use of non-steroidal anti-inflammatory drugs (NSAID), intraarticular corticosteroids (CS), viscosupplementation, and platelet-rich plasma (PRP) applications are usually preferred for the initial treatment of knee osteoarthritis. When these methods fail, surgical methods such as joint-sparing surgery and arthroplasty may be considered [1, 2]. Since total knee replacement (TKR) increases the morbidity and mortality in geriatric patients, the surgeons move towards more conservative methods in this patient group [3, 4]. Intraarticular CS, hyaluronic acid (HA), and PRP applications have become alternative treatment methods since the use of NSAIDs does not provide a significant improvement in pain and functional results, and its long-term use is associated with various side effects [5]. Recent studies and meta-analyses have shown that none of these three applications has superiority over another [6–8].
In recent years, it has been reported that thermal genicular nerve radiofrequency ablation (GNRFA) application has a positive effect on pain control and functional results in the elderly and morbid patients with advanced knee osteoarthritis, with which surgical treatment is not possible and significant results cannot be obtained with other conservative methods [9]. In RFA therapy, the aim is to block the pain afferents around the knee joint. The sensory innervation of the knee is provided by the so-called genicular nerve, which is formed by the articular branches of the femoral, common peroneal, saphenous, tibial, and obturator nerves. Because of their relatively reliable anatomical positions, RFA targets the superior lateral, superior medial, and inferior medial nerves [10–12]. The inferior lateral branch is not included in the application due to its proximity to the common peroneal nerve [12]. For this purpose, fluoroscopy or ultrasonography is used to determine the appropriate anatomical region during the application; then, the process is carried out at the appropriate time and temperature.
In this retrospective study, our aim was to determine the effectiveness of thermal GNRFA therapy as an alternative conservative treatment method in treating the pain, which is the most common complaint in advanced knee osteoarthritis patients who cannot undergo TKR due to comorbidity and patient rejection, and to share the 1-year follow-up results.
Materials and Methods
The hospital records and radiological images of the 49 knees of 35 patients (10 males, 25 females) who had undergone GNRFA therapy for knee osteoarthritis between July 2019 and December 2020 in our clinic were retrospectively evaluated. Patients who were over 60 years of age, were followed-up for knee osteoarthritis, those who did not respond to other conservative methods, and those who could not be operated on due to comorbidities were included in the study. Patients who were under the age of 60 and did not comply with the follow-up and treatments were excluded. The study was carried out in accordance with the 1964 Helsinki Declaration with the permission of the regional ethics committee. An informed consent form was obtained from all patients participating in the study. Ethics Committee approval number (08.04.2021, 2021/05-21).
Demographic characteristics of the patients were recorded. The level of osteoarthritis was determined using the patients’ images from the hospital archive and according to the Kellgren–Lawrence classification [13]. Accordingly, those in whom the mechanical axis passed through the center of the knee joint were considered to have ‘normal’ knees, while those in whom the axis passed 15 mm or more medially to the joint center to have ‘varus’ and those in whom the axis passed 10 mm or more laterally to have ‘valgus’ knees.
Genicular Nerve Radiofrequency Ablation Procedure
Thermal RFA treatment was performed by the same two senior surgeons. After the affected side knee joints of the patients were prepared and covered sterile, the knee was flexed to 30°, the popliteal fossa was supported with a pillow. Our RFA procedure targeted the superior lateral, superior medial, and inferior medial genicular nerves. Three of the genicular nerves were blocked. The inferior lateral branch is not included in the application due to its proximity to the common peroneal nerve. The procedure was performed identically in all patients. The concave region of the femoral condyles in the metadiaphysis of the femur is the anatomical trace of passage of the superomedial and superolateral genicular nerves. The inferomedial genicular nerve passes anatomically through the concave region between the tibial metadiaphysis and the shaft and the tibial plateau. Local anesthesia was administered with 2 mL of 1% lidocaine to each area to be treated. Then, a 10 mm cannulated needle was placed in the targeted areas under fluoroscopy (Fig. 1). The guide needle was removed and a 100-mm-long, 22-gauge RFA needle (JK2; NeuroTherm, Inc., Abbott Park, IL, USA) was inserted into the cannula (Fig. 2). The procedure was initiated in constant communication with the patient unsedated. No motor stimulation was observed upon giving 1.5 V of stimulating current to the patients. Then, RFA was applied at 60–80 °C for 120 s. The needle localization was checked under fluoroscopy and RFA was applied for another 60 s, bringing the total duration of application to 180 s. When pain was observed at 80 °C at the beginning of the procedure, the temperature was reduced to at least 60 °C. None of the patients were treated with ablation below 60 °C. Thus, the procedure was performed in the 60–80 °C range, providing a pain sensation the patients could tolerate. The patients were discharged the same day after the procedure.
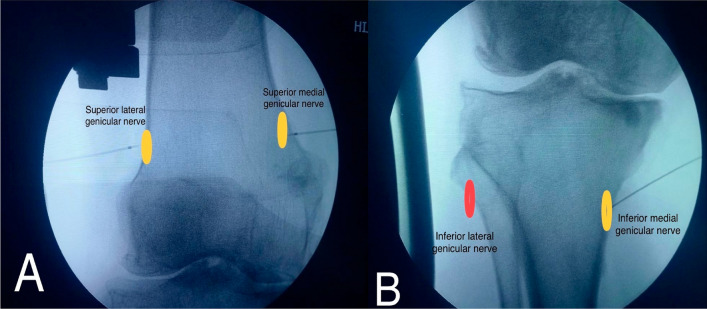
Fig. 1.
Anterior–posterior (A, B) fluoroscopic views of the electrode positions during three needle GNRFA procedure of the genicular nerves are shown. (The yellow rings indicate the superior medial, superior lateral, and inferior medial genicular nerves where ablation is performed. The red ring indicates the position of the inferior lateral genicular nerve, which is close to the common peroneal nerve, so ablation was not performed.)
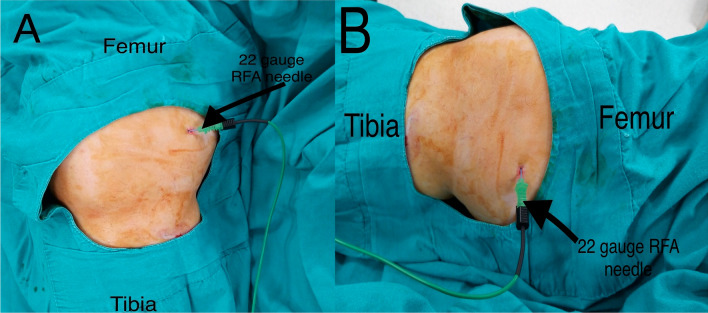
Fig. 2.
Clinical view of the anterior–posterior (A) and lateral (B) position of the radiofrequency ablation needle during the procedure
The visual analog scale (VAS) scores of the patients were recorded before RFA, on the day of RFA, and at the first, sixth, and 12th months postoperatively and their Western Ontario and McMaster Universities Arthritis Index (WOMAC) scores before RFA and at the 12th month postoperatively. Complications developed after the procedure and during the follow-up period were screened.
Statistical Analysis
The SPSS for Windows v.25.0 software (IBM Inc., Armonk, NY, USA) was used for statistical analyses. Descriptive statistics were expressed as mean, standard deviation, minimum and maximum for the numerical variables, and as numbers and percentages for the categorical variables. Differences between the normally distributed numerical variables in the dependent groups were tested with the paired t test and repeated measures ANOVA. The level of statistical significance was accepted as p < 0.05.
Results
The patients had a mean age of 77.3 ± 7.9 years (range 61–92 years) and were followed-up for an average period of 13.3 ± 1.7 months (range 12–18 months). Radiofrequency ablation therapy was applied to the right knee in 11 patients, left knee in 10 patients, and bilaterally in 14 patients. No complications were observed in any of the patients.
Radiologically, seven knees (14.3%) had Kellgren–Lawrence Stage 3 gonarthrosis and 42 were Stage 4 (85.7%). Two patients (4.1%) had valgus and 26 (53.1%) varus deformity, while 21 (42.9%) had a normal knee alignment. Demographic data and radiological findings of the patients are summarized in Table 1. No statistically significant relationship was detected between the osteoarthritis stages of the patients and the VAS scores obtained before and after the treatment (p = 0.086). In addition, there was no significant difference between males and females in terms of change in the VAS score (p = 0.456). The change in the VAS score was found statistically significant (p < 0.01). The VAS results are shown in Table 2.
Table 1.
Demographic data and radiological findings of the patients
| Age, mean ± SD | 77.3 ± 7.9 years (range:61–92 years) | |
| Gender, (%) | Female | 25 (71.4) |
| Male | 10 (28.6) | |
| Affected side, n (%) | Right | 25 (51.0) |
| Left | 24 (49.0) | |
| Gonarthrosis Kellgren–Lawrence stage, n (%) | Stage 3 | 7 (14.3) |
| Stage 4 | 42 (85.7) | |
| Alignment, n (%) | Normal knee alignment | 21 (42.9) |
| Varus | 26 (53.1) | |
| Valgus | 2 (4.1) | |
n = 49 (total number of knees for which the procedure was performed)
Table 2.
Change in the VAS score measured before and after RFA
| Pre-RFA | Post-RFA | First month | Sixth month | 12th month | p* | |
|---|---|---|---|---|---|---|
| VAS score, mean ± SD | 8.4 ± 0.9 | 1.7 ± 1.0 | 2.4 ± 1.7 | 3.4 ± 1.8 | 4.4 ± 1.9 | < 0.01 |
SD standard deviation
*Repeated measures ANOVA
In terms of the WOMAC score, the average value was 69.7 ± 6.4 before the treatment and 36.1 ± 11.8 at the final follow-up at the 12th month (p < 0.01). The decline in the WOMAC score was found statistically significant (p < 0.01).
The alignment in the lower extremities of the patients that underwent RFA was classified as varus, valgus, or normal. Mechanical alignments of knees were also employed to evaluate changes in VAS scores during follow-ups. Patients with normal alignment knees experienced a higher change in VAS score than those with varus alignment knees. The change in VAS scores was found to be greater in varus alignment knees than in valgus alignment knees. In other words, pain relief after RFA was more pronounced in patients with normal alignment, followed by those with varus and valgus knees, respectively. The difference among the groups was statistically significant (p = 0.007) (Table 3).
Table 3.
The relationship between the mechanical alignment of lower extremities and the changes in the VAS scores during the follow-up period
| The change in the VAS score during study period due to mechanical axis of lower extremity | ||||||
|---|---|---|---|---|---|---|
| Pre-RFA | Post-RFA | First month | Sixth month | 12th month | p | |
| Normal knee alignment (n: 21) (mean ± SD) | 8.3 ± 0.7 | 1.4 ± 1.0 | 2.0 ± 1.9 | 2.9 ± 1.9 | 3.6 ± 1.8 | 0.007* |
| Varus (n: 26) (mean ± SD) | 8.3 ± 0.9 | 1.9 ± 1.1 | 2.6 ± 1.4 | 3.6 ± 1.5 | 4.8 ± 1.5 | |
| Valgus (n: 2) (mean ± SD) | 10.0 ± 0.0 | 2.0 ± 0.0 | 4.0 ± 0.0 | 6.0 ± 0.0 | 8.0 ± 0.0 | |
n = 49 (total number of knees for which the procedure was performed)
SD standard deviation
*One-way analysis of variance (One-way ANOVA test) was performed
Discussion
Although the increase in average life expectancy also increases the number of patients in whom quality of life is affected due to osteoarthritis, it creates additional risks in surgical treatments. For this reason, many studies are currently conducted to examine the effectiveness of non-surgical treatment methods in osteoarthritis patients and to also find novel methods. With the thermal RFA procedure used in this study, significant results have been obtained in terms of both pain and functional results in advanced stage knee osteoarthritis.
Radiofrequency ablation can be applied via three different techniques: cooled, pulsed, or thermal RFA. Although it has been reported that thermal RFA may cause more damage to the surrounding tissue, some studies suggested that there is no significant difference among these methods [14, 15]. In this study where we preferred the thermal RFA method, the complications mentioned in the literature were not encountered.
Choi et al. applied RFA on patients who described 50% pain reduction after diagnostic block, and observed a 50% decline in the VAS scores of 59% of these patients 12 weeks after RFA [9]. In another study, in which RFA was applied to 31 knees with 80% pain reduction after diagnostic block, a 67% decline at the third month follow-up and a 64% decline at the sixth month follow-up were reported in the VAS scores [10]. McCormick et al. applied cooled RFA on 36 knees with 50% pain reduction after diagnostic block and on 35 knees without diagnostic block [16]. The authors observed 50% of improvement in 58.6% of the patients with diagnostic block and 64% of the patients without diagnostic block at the sixth month follow-up. If the pain does not decrease after RFA, it is not recommended to repeat the procedure [14]. However, the success rate was not increased in patients with diagnostic block compared to those without diagnostic block. In another study conducted on 49 patients, it was reported that the pre-procedure VAS score of 8.9 decreased to 4.73, 3.89 and 3.93 at the first, fourth, and 12th weeks, respectively [17]. In our study, and in compliance with the literature, the post-procedure VAS score has decreased by 80% compared to the pre-procedure score. The decrease was 71% at the first month, 59% at the sixth month, and 47% at the 12th month. The decrease between the VAS score before ablation therapy and the VAS scores right after the procedure and at the first, sixth, and 12th months was found statistically significant. During our study period, no re-apply of RFA was required in any of our patients. One of the limitations of our study is the 1-year follow-up period. In longer follow-ups, ultrastructural healing in the nerve and reduction in brain plasticity may cause higher levels of increases in patients' pain levels. However, as the studies conducted and the current study show, there is no reason why the procedure should not be reapplied in the long-term.
Increasing the quality of life and improving functional outcomes are the main goals in osteoarthritis treatment. On the other hand, minimizing the side effects of the treatments is another important issue, since knee osteoarthritis is mostly seen in the elderly population. A recent systematic review showed that although the use of NSAIDs or intraarticular injection of CSs in the treatment of osteoarthritis has positive effects on pain-related quality of life and functional outcomes, systemic side effects such as cardiovascular and gastrointestinal, or local side effects such as joint cartilage damage were reported. The fact that RFA, as a localized extraarticular method, has effective outcomes and no side effects has made it advantageous to be preferred as a non-surgical treatment method [18]. Similar results have also been reported in different comparative studies [19, 20]. When RFA application is performed with the right patient selection, it is a candidate to be an effective option among the many treatment options offered to patients with advanced osteoarthritis [21].
In studies evaluating the pain and functional results of RFA therapy, it was reported that the WOMAC score decreased from 64.26 before the procedure to 43.04 at the end of the 12th week [17]. In another study, the WOMAC score decreased by 15 points in 17 (55.2%) of the 29 patients in the group with prognostic block and in 15 (60%) of the 25 patients in the group with no block [16]. In our study, the WOMAC score was 69.7 ± 6.4 before the procedure and 36.1 ± 11.8 at the 12th month follow-up, exhibiting a decline of 33.6 points. Our findings support those from the literature.
In the evaluation of the mechanical alignment of the lower extremities of our patients, we found that varus alignment was the most frequent case (53.1%), followed by normal knees (42.9%) and valgus knees (4.1%). The greatest decrease in the VAS score at the end of the follow-up was observed in patients with a normal mechanical axis. Patients with varus and those with valgus alignment followed this group. We attribute the significant decrease in the VAS score in the normally aligned knees to the fact that knee pain is affected by the alignment biomechanically, therefore, rendering the effect of RFA treatment greater in patients with a normal mechanical alignment.
In a recent study, ultrasound-guided radiofrequency application has been reported to be a more popular method due to its advantages such as less exposure to radiation, real-time evaluation of the targeted anatomical region with the advancement of the needle, minimization of the possibility of damage to the surrounding tissues such as vascular structures, less cost, and easy transport of the ultrasound device [22]. In our study, all radiofrequency applications were performed with fluoroscopy using bone markers, and no complications or decreased effectiveness were encountered.
Significant reduction in pain after RFA is the main expected goal of this treatment. In our study, in which the thermal RFA method was applied, although the VAS scores increased throughout the 1-year follow-up period, they failed to reach the levels recorded prior the treatment. Similar to our study, Sarı et al. reported an increase in VAS scores over time during the follow-up [14, 19]. The authors associated this situation with brain plasticity and stated that even if the nerve heals, the decrease in perception of pain continues for a certain period of time. Ultrastructural changes, albeit transient, were detected in the A-delta and nociceptive fibers after RFA. However, the time required for recovery is unknown [23]. There is no further clear study on the recovery level and duration of nerve fibers, and further studies are needed on this subject. In addition, cooled RFA applications provide a wider neural tissue denervation thanks to their technical advantage. Therefore, it is believed that it provides longer term pain control than thermal RFA in the knee joint with a complex sensory innervation [24, 25].
Our study had some limitations. First, there was no control group in our study. Second, despite the follow-up period of 1 year, the number of patients included in the study was low. Conducting studies with larger patient groups will further support the generalizability of our results. Finally, although scoring systems were used in the study, the subjective nature of pain and the variability of the patients’ expectations from treatment may have affected the quality of the results. For this treatment method to become more popular or routine, further support to the literature with cost-effectiveness studies is required.
Conclusion
In conclusion, the treatment of knee osteoarthritis with non-surgical thermal GNRFA provides satisfactory results in terms of pain and functionality. The absence of obvious systemic and local side effects increases its popularity as a reliable treatment method. This treatment method as a reliable alternative for patients who refuse knee arthroplasty treatment or for whom arthroplasty is contraindicated, and for those who do not have a relevant indication for surgery yet.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
Declarations
Conflict of Interest
The authors declare no potential conflicts of interest.
Ethical Approval
The study protocol was approved by the Local Scientific Research Ethics Committee.
Informed Consent
All patients agreed to participate in the study.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Oğuz Kaya, Email: oguzkayamd@gmail.com.
Ahmet Şenel, Email: ahmetsenel23@gmail.com.
Ömer Cihan Batur, Email: istanbultip@gmail.com.
Nevzat Gönder, Email: n_gonder_02@hotmail.com.
Emre Ergen, Email: emreergen99@hotmail.com.
Barış Peker, Email: drbaris@yahoo.com.
References
- 1.Jevsevar DS. Treatment of osteoarthritis of the knee: Evidence-based guideline, 2nd edition. Journal of the American Academy of Orthopaedic Surgeons. 2013;21:571–576. doi: 10.5435/JAAOS-21-09-571. [DOI] [PubMed] [Google Scholar]
- 2.Bowman EN, Hallock JD, Throckmorton TW, Azar FM. Hyaluronic acid injections for osteoarthritis of the knee: Predictors of successful treatment. International Orthopaedics. 2018;42:733–740. doi: 10.1007/s00264-017-3731-8. [DOI] [PubMed] [Google Scholar]
- 3.Belmont PJ, Jr, Goodman GP, Waterman BR, Bader JO, Schoenfeld AJ. Thirty-day postoperative complications and mortality following total knee arthroplasty: Incidence and risk factors among a national sample of 15,321 patients. Journal of Bone and Joint Surgery. American Volume. 2014;96:20–26. doi: 10.2106/JBJS.M.00018. [DOI] [PubMed] [Google Scholar]
- 4.Adam RF, Noble J. Primary total knee arthroplasty in the elderly. Journal of Arthroplasty. 1994;9:495–497. doi: 10.1016/0883-5403(94)90095-7. [DOI] [PubMed] [Google Scholar]
- 5.Pelletier JP, Martel-Pelletier J, Rannou F, Cooper C. Efficacy and safety of oral NSAIDs and analgesics in the management of osteoarthritis: Evidence from real-life setting trials and surveys. Seminars in Arthritis and Rheumatism. 2016;45:S22–S27. doi: 10.1016/j.semarthrit.2015.11.009. [DOI] [PubMed] [Google Scholar]
- 6.He WW, Kuang MJ, Zhao J, Sun L, Lu B, Wang Y, Ma JX, Ma XL. Efficacy and safety of intraarticular hyaluronic acid and corticosteroid for knee osteoarthritis: A meta-analysis. International Journal of Surgery. 2017;39:95–103. doi: 10.1016/j.ijsu.2017.01.087. [DOI] [PubMed] [Google Scholar]
- 7.Di Y, Han C, Zhao L, Ren Y. Is local platelet-rich plasma injection clinically superior to hyaluronic acid for treatment of knee osteoarthritis? A systematic review of randomized controlled trials. Arthritis Research & Therapy. 2018;20:128. doi: 10.1186/s13075-018-1621-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Migliorini F, Driessen A, Quack V, Sippel N, Cooper B, Mansy YE, Tingart M, Eschweiler J. Comparison between intra-articular infiltrations of placebo, steroids, hyaluronic and PRP for knee osteoarthritis: A Bayesian network meta-analysis. Archives of Orthopaedic and Trauma Surgery. 2021;141:1473–1490. doi: 10.1007/s00402-020-03551-y. [DOI] [PubMed] [Google Scholar]
- 9.Choi WJ, Hwang SJ, Song JG, Leem JG, Kang YU, Park PH, Shin JW. Radiofrequency treatment relieves chronic knee osteoarthritis pain: A double-blind randomized controlled trial. Pain. 2011;152:481–487. doi: 10.1016/j.pain.2010.09.029. [DOI] [PubMed] [Google Scholar]
- 10.Iannaccone F, Dixon S, Kaufman A. A review of long-term pain relief after genicular nerve radiofrequency ablation in chronic knee osteoarthritis. Pain Physician. 2017;20:E437–E444. doi: 10.36076/ppj.2017.E444. [DOI] [PubMed] [Google Scholar]
- 11.Franco CD, Buvanendran A, Petersohn JD, Menzies RD, Menzies LP. Innervation of the anterior capsule of the human knee: Implications for radiofrequency ablation. Regional Anesthesia and Pain Medicine. 2015;40:363–368. doi: 10.1097/AAP.0000000000000269. [DOI] [PubMed] [Google Scholar]
- 12.Hirasawa Y, Okajima S, Ohta M, Tokioka T. Nerve distribution to the human knee joint: Anatomical and immunohistochemical study. International Orthopaedics. 2000;24:1–4. doi: 10.1007/s002640050001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kellgren JH, Lawrence JS. Radiological assessment of osteo-arthrosis. Annals of the Rheumatic Diseases. 1957;16:494–502. doi: 10.1136/ard.16.4.494. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kidd VD, Strum SR, Strum DS, Shah J. Genicular nerve radiofrequency ablation for painful knee arthritis: The why and the how. JBJS Essential Surgical Techniques. 2019;9:e10. doi: 10.2106/JBJS.ST.18.00016. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Gupta A, Huettner DP, Dukewich M. Comparative effectiveness review of cooled versus pulsed radiofrequency ablation for the treatment of knee osteoarthritis: A systematic review. Pain Physician. 2017;20:155–171. doi: 10.36076/ppj.2017.171. [DOI] [PubMed] [Google Scholar]
- 16.McCormick ZL, Korn M, Reddy R, Marcolina A, Dayanim D, Mattie R, Cushman D, Bhave M, McCarthy RJ, Khan D, Nagpal G, Walega DR. Cooled radiofrequency ablation of the genicular nerves for chronic pain due to knee osteoarthritis: Six-month outcomes. Pain Medicine. 2017;1(18):1631–1641. doi: 10.1093/pm/pnx069. [DOI] [PubMed] [Google Scholar]
- 17.Kirdemir P, Çatav S, Alkaya SF. The genicular nerve: Radiofrequency lesion application for chronic knee pain. Turkish Journal of Medical Sciences. 2017;47:268–272. doi: 10.3906/sag-1601-171. [DOI] [PubMed] [Google Scholar]
- 18.Chen AF, Mullen K, Casambre F, Visvabharathy V, Brown GA. Thermal nerve radiofrequency ablation for the nonsurgical treatment of knee osteoarthritis: A systematic literature review. Journal of American Academy of Orthopaedic Surgeons. 2021;29:387–396. doi: 10.5435/JAAOS-D-20-00522. [DOI] [PubMed] [Google Scholar]
- 19.Sarı S, Aydın ON, Turan Y, Özlülerden P, Efe U, Kurt Öİ. Which one is more effective for the clinical treatment of chronic pain in knee osteoarthritis: Radiofrequency neurotomy of the genicular nerves or intra-articular injection? International Journal of Rheumatic Diseases. 2018;21:1772–1778. doi: 10.1111/1756-185X.12925. [DOI] [PubMed] [Google Scholar]
- 20.El-Hakeim EH, Elawamy A, Kamel EZ, Goma SH, Gamal RM, Ghandour AM, Osman AM, Morsy KM. Fluoroscopic guided radiofrequency of genicular nerves for pain alleviation in chronic knee osteoarthritis: A single-blind randomized controlled trial. Pain Physician. 2018;21:169–177. [PubMed] [Google Scholar]
- 21.Carlone AG, Grothaus O, Jacobs C, Duncan ST. Is cooled radiofrequency genicular nerve block and ablation a viable option for the treatment of knee osteoarthritis? Arthroplast Today. 2021;7:220–224. doi: 10.1016/j.artd.2020.12.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Erdem Y, Sir E. The efficacy of ultrasound-guided pulsed radiofrequency of genicular nerves in the treatment of chronic knee pain due to severe degenerative disease or previous total knee arthroplasty. Medical Science Monitor. 2019;12:1857–1863. doi: 10.12659/MSM.915359. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Erdine, S., Bilir, A., Cosman, E. R., & Cosman, E. R. Jr. (2009). Ultrastructural changes in axons following exposure to pulsed radiofrequency fields. Pain Practice, 9, 407–417. 10.1111/j.1533-2500.2009.00317.x. Epub 2009 Sep 15. Erratum in: Pain Pract. 2010 May–Jun;10:264. [DOI] [PubMed]
- 24.Menzies RD, Hawkins JK. Analgesia and improved performance in a patient treated by cooled radiofrequency for pain and dysfunction postbilateral total knee replacement. Pain Practice. 2015;15:E54–E58. doi: 10.1111/papr.12292. [DOI] [PubMed] [Google Scholar]
- 25.Rojhani S, Qureshi Z, Chhatre A. Water-cooled radiofrequency provides pain relief, decreases disability, and improves quality of life in chronic knee osteoarthritis. American Journal of Physical Medicine and Rehabilitation. 2017;96:e5–e8. doi: 10.1097/PHM.0000000000000549. [DOI] [PubMed] [Google Scholar]