Abstract
Background
Over the past two decades, there has been a documented increase in paediatric ACL injuries because of a rise in younger age sports participation at the competitive level, awareness about sports-related injuries, and advanced imaging modalities.
Methods
A PubMed electronic database search was done, which revealed 1366 hits over the last five years (2016 – 2020). Finally, 37 articles that contributed to new findings were included. This review was conducted based on predefined research questions.
Results and conclusion
Early surgical reconstruction is recommended in children due to the increasing demand for early return to sports and to prevent the instability that can lead to progressive cartilage and meniscal damage. With the evolution of several “physeal sparing” ACL reconstruction (ACLR) techniques, a favorable clinical outcome with less growth disturbance is achievable. Although different autograft options are available, hamstring autografts are most commonly preferred. A specific pattern of a bone bruise not extending into the metaphysis, and lateral meniscus tears are the most common associated injuries. Following paediatric ACLR, complications like graft rupture and contralateral ACL injuries are two to three folds higher than with adult ACLR. Unprepared early return to sports is one of the reasons for increased complication rates in children; thus, clearance criteria for return to sports need to be standardized, and early return to sports (< 9 months post ACLR) should be avoided. Neuromuscular training protocols are recommended to minimize complications like graft ruptures.
Keywords: Adolescent, ACL, Autograft, Graft rupture, Hamstring, Pediatric, Quadriceps, Return to sports
Introduction
Paediatric ACL injuries have shown a progressive documented increase over the last 20 years due to multiple factors [1]. The current literature favors surgical management even in children, as it helps in reducing the risk of concomitant chondral damage and meniscus injuries [2–5]. However, the concern is the physeal injury during the surgical intervention [5, 6]. This problem has been minimized by improvised techniques of ACL reconstruction (ACLR) [7]. In 2018, Ardern et al. [8] published an article titled “2018 International Olympic Committee consensus statement on prevention, diagnosis, and management of paediatric anterior cruciate ligament (ACL) injuries”. A global expert group of Orthopaedic Surgeons and physiotherapists participated and made a consensus statement for six basic clinical questions about Paediatric ACL injuries. They published a comprehensive summary to aid clinicians, support the children with an ACL injury, and help their parents make the best possible decisions. Few original articles were published later in the literature focusing on complications following paediatric ACL reconstruction (ACLR) like graft rupture and contralateral ACL injuries and outcomes following quadriceps (QT) autograft reconstruction.
The present article aims to give a comprehensive literature review of the articles published in the past 5 years, focusing on the different subset of questions involving incidence rates, injury mechanisms, the evolution of treatment methods, associated intra-articular injuries, graft choice, and complications.
Methodology
A PubMed electronic database search (on 20th August 2020) in the English language with a pre-defined specific search strategy (Table 1) revealed 1366 hits over the last 5 years (2016–2020), which shows great interest in this topic among researchers recently. The articles obtained from the literature search were screened based on title and abstract by two authors independently (KR and RKR). Articles were excluded based on the pre-defined inclusion and exclusion criteria. Whenever there was any doubt regarding the eligibility of any article, the full text was obtained and reviewed. The Randomized controlled trials, meta-analysis, case–control and cohort studies, case series, and reports published during the period of database search, focused on the research questions mentioned in the following aims and objectives section, were included. Conference abstracts and studies published in a language other than English were excluded. Any conflict regarding the inclusion or exclusion of studies among the two authors was resolved by discussion with all the authors. Finally, 37 articles that contributed to new findings were included. Three independent authors (KR, MSD, and NRG) performed the data extraction from each included article and entered a pre-specified data collection excel sheet, and did the review based on the following research questions.
Table 1.
Search strategy used for article selection
| Database | Period -1st January 2016 to 20 th August 2020 with keywords | Results |
|---|---|---|
| PubMed | (((((("anterior cruciate ligament"[MeSH Terms] OR (("anterior"[All Fields] AND "cruciate"[All Fields]) AND "ligament"[All Fields])) OR "anterior cruciate ligament"[All Fields]) OR (("anterior cruciate ligament reconstruction"[MeSH Terms] OR ((("anterior"[All Fields] AND "cruciate"[All Fields]) AND "ligament"[All Fields]) AND "reconstruction"[All Fields])) OR "anterior cruciate ligament reconstruction"[All Fields])) AND (((((("tears"[MeSH Terms] OR "tears"[All Fields]) OR "tear"[All Fields]) OR "lacerations"[MeSH Terms]) OR "lacerations"[All Fields]) OR ((((((((("disrupt"[All Fields] OR "disrupted"[All Fields]) OR "disrupter"[All Fields]) OR "disrupters"[All Fields]) OR "disrupting"[All Fields]) OR "disruption"[All Fields]) OR "disruptions"[All Fields]) OR "disruptive"[All Fields]) OR "disruptiveness"[All Fields]) OR "disrupts"[All Fields])) OR ((((((((((("injurie"[All Fields] OR "injuried"[All Fields]) OR "injuries"[MeSH Subheading]) OR "injuries"[All Fields]) OR "wounds and injuries"[MeSH Terms]) OR ("wounds"[All Fields] AND "injuries"[All Fields])) OR "wounds and injuries"[All Fields]) OR "injurious"[All Fields]) OR "injury s"[All Fields]) OR "injuryed"[All Fields]) OR "injurys"[All Fields]) OR "injury"[All Fields]))) AND ((((((("paediatrics"[All Fields] OR "pediatrics"[MeSH Terms]) OR "pediatrics"[All Fields]) OR "paediatric"[All Fields]) OR "pediatric"[All Fields]) OR "pediatrics"[All Fields]) OR (((((("child"[MeSH Terms] OR "child"[All Fields]) OR "children"[All Fields]) OR "child s"[All Fields]) OR "children s"[All Fields]) OR "childrens"[All Fields]) OR "childs"[All Fields])) OR (((((("adolescences"[All Fields] OR "adolescency"[All Fields]) OR "adolescent"[MeSH Terms]) OR "adolescent"[All Fields]) OR "adolescence"[All Fields]) OR "adolescents"[All Fields]) OR "adolescent s"[All Fields]))) AND "English"[All Fields]) AND 2016/01/01:2020/08/20[Date—Publication] | 1366 |
Aims and Objectives
This review aimed to gather specific information on the following questions.
Has the incidence of paediatric ACL injury increased over time?
Have the surgical techniques and fixation methods evolved in the twenty-first century?
Are there significant re-injury rates in children?
What is the incidence of contralateral knee injury?
Is the associated chondral and meniscal injury rate similar to adults?
We also looked at injury mechanisms and patterns and evaluated factors affecting return to sports/activity.
Observations and Analysis
Has the Incidence of Paediatric ACL Injury Increased over Time?
Recent literature records a significant rise in paediatric ACL injury, at a rate significantly higher than in adults (12–47% of all paediatric traumatic knee effusions) [9–11]. In the past, ACL injury in the paediatric population was considered an uncommon occurrence [12], documented at 1–3.4% in the 1970s and early 1980s. [13–16] Increased awareness and improved imaging modalities have increased diagnostic rates [4, 16]. Weitz et al. demonstrated a twofold increase of ACL injury incidence in the adolescent Finnish population over 17 years, mostly related to increased competitive sports participation and better imaging modalities [17]. Beck et al. documented a similar trend of increased incidence of paediatric ACL injuries over the past 20 years, with a peak incidence noted in the time of high school years [1]. They reported that during younger age period (6–16 years), female gender had significantly higher rates of injury, but in the age group of 17 to 18 years, males had a significantly higher incidence. Shaw and Finch published the trend in Pediatric and Adolescent ACL Injuries in Victoria, Australia. They documented that the overall annual rate of ACL injuries had increased by 147.8%, from 2.74 per 100,000 population in the year 2005/2006 to 6.79 per 100,000 in the year 2014/2015 [18]. The past (historical) studies [12–15] were non-population-based, but the recent results were population-based [16, 18].
Mechanism of Injury and Injury Pattern—Is It the Same as an Adult?
The literature revealed the non-contact injury to be the most common mechanism of paediatric ACL injury (71%), probably due to a pivoting strain with the semi-flexed knee and foot placed on the ground [19, 20]. Current evidence shows non-contact ACL rupture due to neuromuscular and biomechanical events during dynamic movements; however, the movement patterns and the level of neuromuscular control among paediatric patients are not well understood [21, 22]. A hyperextension injury with a valgus or rotational force has also been documented to cause a paediatric ACL injury [19].
Children and adolescents show a more significant rate of partial ACL tears than complete tears as compared to adults [23]. ACL enthesis tears (distal > proximal) were also documented in the adolescent population [24]. The tibial eminence of the skeletally immature population is not fully ossified, making the cancellous bone underneath more susceptible to failure than the strong ACL [25]. This allows the more pliant tibial intercondylar eminence to be avulsed by traction forces at the chondro-osseous transition zone [26–28]. Nevertheless, a variable amount of plastic deformation of the ACL fibers may be associated, causing residual clinical laxity despite anatomic fracture reduction [29–31].
Treatment of Paediatric ACL Injuries
Paediatric ACL injuries can present as avulsions of the tibial spine or partial or full-thickness ACL tears. Conventionally, conservative options like bracing, casting, activity modification, and physical therapy had been advocated. However, current evidence [32–34] favors early surgical intervention, as many publications have documented poor outcomes in conservatively treated knees with the development of chronic instability and a greater risk of chondral and meniscal injury [35–37]. Fewer young athletes treated non-operatively could return to same or higher level sports than those who had surgical reconstruction [38, 39].
Injury prevention by implementing injury prevention programs for skeletally immature sports participants is advocated [22]. Non-operative treatment is currently limited to partial ACL tears with negative pivot shift test, type 1 tibial eminence fracture, and type 2 fractures with minimal displacement [38]. Non-operative treatment includes high-quality rehabilitation and usage of protective bracing during strenuous physical activities. It is a safe and viable option in children who do not have associated injuries or major instability problems. Surgical reconstruction in a paediatric patient is needed when a torn ACL is associated with a positive pivot shift test. Most surgeons currently agree that ACLR should only be done once the knee range of motion (ROM) has been improved (flexion more than 120°), unless in the scenario of a tibial eminence fracture or with an associated bucket-handle meniscus injury [8, 38, 40].
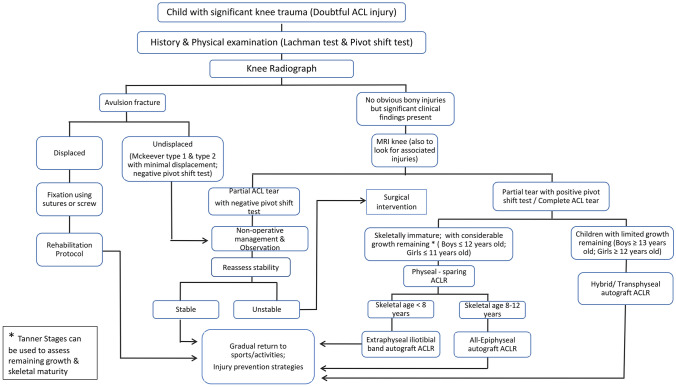
For ACLR in paediatric and adolescent populations, four primary approaches are currently used: a combined extra-articular/intra-articular iliotibial band reconstruction [41, 42], a transphyseal ACLR [34, 43], an all-epiphyseal ACLR [32], and a hybrid approach [44, 45] (all-epiphyseal tunnel in the femur and transphyseal tunnel in tibia). Factors like age, height, Tanner stage, and the surgeon’s experience and training should be taken into account primarily for deciding which approach to use. Age-wise treatment protocols [46] for ACL injuries are given in Table 2. A treatment algorithm for managing Paediatric ACL injuries is shown in Fig. 1.
Table 2.
Treatment options recommended in literature based on bone age
| S.No | Author/year | Age at which this procedure recommended | Techniques details | Comment |
|---|---|---|---|---|
| 1 | Micheli–Kocher/2005 | 6 years | Intra-articular and extra-articular iliotibial band reconstruction (Modified MacIntosh) with functionally control rotation | Avoid physeal tunnels; important consideration in younger patients |
| 2 | Anderson/2003 | 8 years | All-epiphyseal procedure; quadrupled hamstring graft tensioned across epiphyseal tunnels in the distal femur and proximal tibia. Femoral fixation with cortical button and tibial fixation with screw and post construct | Extra-physeal, but requires extra-osseous tensioning of the graft across the tibial physis |
| 3 | Ganley–Lawrence/2010 | 10 years | All-epiphyseal docking procedure; Fixation done using interference screws in epiphysis | Extra-physeal. Tunnels and fixation within both femur and tibial epiphysis |
| 4 | Willson/2018 | 12 years | Partial transphyseal (Hybrid)reconstruction; with an all-epiphyseal femoral tunnel and transphyseal tibial tunnel | Keep tibia tunnel in centre. Growth disturbance may occur as tibial physis is violated |
| 5 | Kocher/2007 | 14 years or more | Transphyseal reconstruction; tunnel placement and fixation across both femur and tibial physis | Like adult’s reconstruction using soft-tissue autografts |
Fig. 1.
Flow diagram for the management of Paediatric ACL Injuries
The anatomic trans-tibial technique can be single or double-bundle ACL reconstruction; the advantage is that it restores knee kinematics. In the all-epiphyseal technique described by Lawrence et al. [47] (a modification of the original description by Allen F Anderson [32]), a tunnel in the lateral femoral epiphysis and an oblique tunnel in tibial epiphysis are created by avoiding the physis; the graft is stabilized in the tunnels via bio-absorbable screws. Sparing the physis avoids growth disturbances, angular deformities, and limb length discrepancies, but the acute angle created by these tunnels increases strains on the graft, with a higher risk of graft rupture. Recently, Pennock et al. [48] modified the all-epiphyseal technique of ACLR in skeletally immature patients and stabilized the grafts using an interference screw on the femur and suspensory fixation in the tibia. This alteration avoids fixation or sutures across the physis as fixation devices are purely inside the epiphysis and avoiding iatrogenic “tethering” of the physis. Additionally, the fixation is truly anatomic; also, both the tunnels are placed on the ACL footprint’s centre. The stabilization attained with suspensory fixation and interference screw may be greater than a post-fixation or suture fixation to the periosteum. [48].
A tunnel created across proximal tibial physis disrupts the tibial growth plate in a hybrid ACLR. The graft is secured to the lateral aspect of the femur, sparing the distal femur physis (which contributes a greater proportion of growth in the lower limb). Willson et al. [49] published their early results in the skeletally immature athletes with an approximate bone age of 12 years (at least 2 years of growth leftover), using a transphyseal tibial tunnel and sparing the femoral physis (“hybrid” technique); 91.3% (21/23) cases had equal limb length at a mean 21 month follow-up. They used an adjustable loop cortical suspension device for femoral fixation, and either an interference screw, metaphyseal plate and screw, cortical button, or staple was used for tibial fixation. Mall and Paletta [38], in their modified transphyseal technique, fixed the femoral side with a suspensory device, and a staple (ligament) or screw and post was used for tibial stabilization or even a suspensory device.
For tibial eminence fractures, the fixation can be done either by open method or by arthroscopy. The fixation can be done using sutures, metal screws, bio-absorbable nails, Kirschner wires, or suture anchors. Suture fixation is recommended as the screws can cause comminution or may weaken the small fragment. Also, sutures have similar or improved strength profiles [50–52]. However, if the avulsed fragment is large and non-comminuted, screw fixation can be considered.
ACL Repair
In a systematic review, Van Eck et al. [53] documented that primary repair in proximal ACL fiber tears showed a better healing potential than distal or mid-substance tears. They concluded that ACL repair might be a useful option for patients with acute proximal ACL tears (specifically in the skeletally immature).
Internal Bracing
Smith et al. [54] did a direct repair and supplemented this with an internal brace in two cases of ACL tear with tibial spine fractures; at 3 months, second-look arthroscopy showed complete healing. Apart from suture, other augmentation methods have been suggested, including collagen scaffolds, patellar tendon, or iliotibial band, and may increase the success rate of repair. [52].
Graft Choice in Children
At the beginning of the twenty-first century, the graft choices for ACLR in children were bone–patellar–tendon–bone (BPTB) autograft, Hamstring tendon (HT) autograft, Quadriceps tendon (QT) autograft, iliotibial band (ITB), and various soft-tissue allografts. Although the graft choice has not changed much, HT autografts are currently the most preferred around the world. However, recent studies [55, 56] have favored the QT autograft over HT autograft due to reduced incidence of graft rupture. Pennock et al. [55] found that in transphyseal ACLR, the graft failure rate was 21% in the HT group and 4% in the QT group. Runer et al. [56] documented 5.5 times greater revision rates in children < 15 years of age compared to adults > 45 years, and these were 2.7 times greater in patients receiving HT autograft than QT autograft. The reason for reduced graft rupture of QT autograft is the larger size of the QT graft and the preservation of hamstring function by not harvesting it. Although the graft rupture rates of QT autograft are comparable with BPTB autograft, issues like anterior knee pain, high risk of patella fracture, and patellar tendon rupture slightly favor QT autograft over BPTB [56]. However, QT autograft is not without complications like initial extensor deficit, arthrofibrosis, and larger recovery time after surgery.
The current literature reveals no definitive higher level evidence favoring QT over HT autograft. In the future, higher level evidence, multicentric study with long-term follow-up comparing QT and HT autograft to find the right graft choice for Paediatric ACLR is the need of the hour.
Graft Rupture and Contralateral ACL Injury
Skeletally immature cases are reported to have 2.5-to-3.5 times greater risk of ACL graft ruptures when compared to the adult population [57–59]. In 2020, DeFrancesco et al. [60] published the largest series of ACLR in the paediatric population to date. They analyzed 996 patients who underwent ACLR over more than 7 years, in which 161 patients underwent all-epiphyseal ACLRs; 504 and 331 patients underwent transphyseal ACLRs at age less than 16 years and more than or equal to 16 years, respectively. Overall, the 4-year cumulative graft rupture rate was 19.7%, and contralateral ACL injury was 12%. The graft rupture rates and contralateral ACL injury rates were higher in children < 16 years who underwent transphyseal ACLRs (21.6% and 15.7%, respectively). Hamstring autograft was used in more than 87% of patients, but no statistically significant difference was found in graft rupture rates by graft type (autograft/ allograft/ hybrid). They also inferred that graft rupture rates are greater than contralateral ACL injuries.
In 2019, Astur et al. [61] analyzed 52 children < 16 years who underwent transphyseal ACLR using a quadruple hamstring tendon graft. 18/52 children (34.6%) had rupture of the graft, and 66.6% of this occurred after 24 months of surgery. They found no statistically significant correlation between the type of sport and graft rupture rates. Morgan et al. [62] published a 15-year survival rate of ACLR in children aged 18 years or younger. They used either autologous BPTB autograft or hamstring autograft, and found that the 15-year survival rates of ACL graft and contralateral ACL were 83% and 81%, respectively. They concluded that ACL grafts and contralateral ACLs were most vulnerable within the first 5 years after primary ACLR surgery.
Contralateral ACL injury following primary ACLR in children varies from 7 to 13%, whereas in adults, it is 3–4% [59, 63, 64]. Patel et al. [65] concluded that children less than 15 years of age had 3.1 times higher chance of contralateral ACL injury than children of age more than 15 years and female children had 3.5 times greater chance than male counterparts. They explained the reason for a contralateral ACL injury to be multifactorial, ranging from afferent signals loss from the injured ACL resulting in contralateral proprioceptive deficits to anatomic issues like narrow intercondylar (IC) notch, increased tibial posterior slope, etc. They suggest that younger children (age < 15 years), females, those with a narrow IC notch, increase in posterior tibial slope, and atypical knee kinematics should be identified as having a higher risk of contralateral injury. Injury prevention programs concerning strength, perception, and kinematics should be emphasized, and clearance for sports return should be given only after 9 months following ACLR, and that too only to patients who successfully passed multiple strength and functional tests.
A recent systematic review and meta-analysis by Zacharias et al. [66] analyzed 24 articles and found that ipsilateral graft failure occurred in 8.3% of patients; however, they could not note any statistically significant sex difference in terms of the prevalence of graft failure. They however, found that female children are at increased risk (odds ratio = 3.0) of contralateral ACL injury than male counterparts.
Perrone et al. [67] suggested that functional bracing while playing cutting and pivoting sports following 2 years of surgery reduces the risk of graft rupture, and there is no difference in the contralateral ACL injury rates.
The recent literature reveals significant graft rupture rates and contralateral ACL injury rates after paediatric ACLR in comparison to adults; females are predisposed to these injuries.
Growth Disturbances
The potential damage to the growth plate while drilling across the physis in the transphyseal technique can lead to physeal arrest. The tunnel size and tunnel drill angle are two important factors that determine the physeal injury, in addition to higher graft tensions. Small diameter tunnels with soft-tissue autografts are recommended, along with vertically oriented tunnel placement, less graft tensioning, and minimal hardware across lateral distal femoral physis [37]. Fauno et al. [68] analyzed 39 children with open physis at the time of transphyseal ACLR, and found that 24% of children had minor limb length growth disturbances at skeletal maturity. They concluded that the surgically (iatrogenic) induced valgus angulation deformity in the diastal femur is usually counterbalanced by a varus angulation in proximal tibia.
A meta-analysis by Wong et al. [69] included 45 studies with 1321 patients and 1392 knees; they found that 58 growth disturbances were documented, of which 16 required corrective surgery (27.6%). 3.7% had an angular deformity, mostly valgus, and 7.5% had at least 1 cm limb length discrepancy.
Associated Injuries
ACL injuries in skeletally immature patients are also associated with meniscal tears, bone contusions, and chondral injuries. In an MRI study by Bordoni et al. [70], there were 69% associated bone bruises, 43% meniscal injuries, 10% other ligament injuries, 3.7% cartilage lesions, and 3.7% associated patellar fractures in paediatric patients. They concluded that the pattern of distribution of the bone bruises and area affected are similar in both adults as well as children, but the bone bruises associated with ACL tears appear to be less common in paediatric patients when compared to adults.
In another MRI study, Novaretti et al. [71] found significantly lesser bone bruises that crossed the physis and extend into metaphysis in the skeletally immature (SI) group than in the skeletally mature (SM) group. They concluded that SI group patients with ACL injury had a unique pattern of bone bruise compared to individuals with closed physis, where the metaphysis involvement is more. The sub-regions most commonly involved in the SI group are medial/lateral and central regions of the tibia, without extension into metaphysis (42%) and lateral aspect of the femur without metaphyseal extension (59%).
Feucht et al. [72] did a multicentric study on the prevalence along with particulars of children who had surgery for the tibial eminence fractures and had arthroscopically documented meniscal injuries in 37% of children. 90% of these had lateral meniscal injury compared to 10% medial meniscal injury. The most commonly noted tear pattern was a longitudinal tear in the lateral meniscus’ posterior horn followed by root detachment in the anterior horn of lateral meniscus.
Vavken et al. [73] did a retrospective analysis from the records of 208 patients who underwent paediatric ACLR; they found that 35% had a lateral meniscal tear, 32% medial meniscal tear, and 5% had a chondral lesion. They documented an association with meniscal tears in relation to delay in the surgical intervention. They concluded that both the body mass index (BMI) and time period between the ACL injury and surgical reconstruction were significant indicators of chondral or meniscal damage.
Malatray et al. [74] concluded that the prevalence of ACL-associated ramp lesions in paediatric age group is same as adults. A systematic inspection via the intercondylar notch is recommended during an ACLR to make an accurate diagnosis. Rhodes et al. [75] made a comparison between MRI findings and surgical findings in tibial spine avulsion patients. They found that the incidence of meniscal entrapment identified during surgery was higher, whereas the incidence of positive findings noted by MRI is low. The most common unrecognized meniscal injury found was a vertical tear in the posterior horn. [76].
Kinsella et al. [77] evaluated associated posterolateral corner (PLC) injuries in children with the ACL injuries. They found that 52% had an associated PLC injury and 14% had a complete tear. There was correlation between PLC injury and age, with increased PLC injury by 1.8 times for every year increase in age. They found no correlation between the PLC injury and ACL graft failure.
Thus, the literature documents that the bone bruises not extending into the metaphysis and lateral meniscus injury are the most commonly associated injuries.
Return to Sports
Since there is a higher rate of graft rupture following primary ACLR in young, high-activity athletes compared to adult populations, the ideal time and criteria in getting clearance for return to sports (RTS) in children/adolescents are important. Paterno et al. [78] evaluated the clinical factors in predicting the risk of second ACL injury following primary ACLR and RTS among young athletes. One hundred and sixty-three participants who had primary ACLR and were allowed to RTS were followed for 2 years after primary reconstruction. High-risk people were identified based on age (age < 19 years), gender (female), performance on the triple hop to the distance, and knee-related confidence. The validation step found that the high-risk groups were five times (odds ratio) more likely to develop a second ACL injury, with sensitivity and specificity of 66.7% and 72.0%, respectively.
Cordasco et al. [79] assessed the clinical outcomes in three cohorts of athletes under the age of 20 years who received primary ACLR with follow-up of a minimum 2 years. Group 1 athletes included the youngest cohort from elementary and middle school who underwent all-epiphyseal ACL reconstruction with hamstring autograft. Group 2 athletes included those who received a partial or complete transphyseal reconstruction with hamstring autograft in the middle school age. Group 3 athletes included those who received bone–tendon–bone autograft among the skeletally mature high school age. They found that Group 2 middle school age athletes had significantly greater revision rates and lower RTS rates than group 1 and 3. They concluded that this age-associated risk profile could be used during counselling of players preoperatively about the surgical expectations concerning revision ACLR as well as RTS rates.
Beischer et al. [80] evaluated return to knee-strenuous sports, the function of muscle, and subjective knee function in the adolescents (15–20 years) and adult (21–30 years) patients at 8 and 12 months following primary ACLR. They concluded that most adolescent patients make an early return to sports compared to adults without recovering muscle function. They also recommend the clinicians ensure and inform the young athletes not to make an early return to sports until the muscle function is fully recovered, which might take more than 12 months.
Geffroy et al. [81] did a multicentric study by comparing paediatric groups with open physis with skeletally mature (closed physis) groups to determine RTS time after primary ACLR and what level of sports they engaged in. In the open physis group, the ACL re-injury and contralateral ACL injury rate was 9% and 6%, respectively. In the closed physis group, the ACL re-injury and contralateral ACL injury rate was 2.8% and 5%, respectively. The return to running in open and closed physis groups was 10.4 ± 4.7 and 8.8 ± 5.1 months, respectively. The return to pivoting/contact sports competition in open and closed physis groups was 13.8 ± 3.8 and 12.3 ± 4.2 months, respectively. 80% in the open physis group and 76.9% in the closed physis group returned to the same sport. In the open physis group, 19.4% had a poor outcome, 10.4% had an International Knee Documentation Committee (IKDC) score of C or D, and 9% had re-tears, whereas, in the closed physis group, 14.7% had a poor outcome, 11.9% had IKDC score C or D, and 2.8% had re-tears. They concluded that returning to pivoting/contact sports competitions should not be permitted until 14 months after primary ACLR in children with open physis.
Ithurburn et al. [82] concluded that athletes at the time of return to sports clearance in the paediatric age group after the all-epiphyseal physeal-sparing ACL reconstructive surgery showed higher quadriceps femoris strength symmetry, higher functional performance of knee, and also a higher level of self-reported knee function in comparison to adolescent and young adult groups after traditional ACLR.
After paediatric ACLR, RTS less than 9 months of surgery should be avoided due to higher re-injury rates.
Limitations The limitations of this review are that there were only a few level-1 evidence studies published on this topic and the lack of studies showing long-term outcomes (> 10 years) following Paediatric ACLR is evident. Conference abstracts and articles published in a language other than English were excluded from this review. A focused, systematic review and meta-analysis might give a more systematic insight into this topic with a higher level of evidence.
Inferences from the Literature Review
The incidence of paediatric ACL injury is rising due to increased competitive sports participation and better imaging modalities. A specific pattern of bone bruises and lateral meniscal injuries is commonly associated. The graft choice had not changed much; many centers are still using hamstring autografts, but graft fixation methods have evolved. In comparison to adults, paediatric ACL reconstruction is more prone to graft rupture and contralateral ACL injuries during the initial few years of surgery. The ideal time and clearance criteria for return to sports need to be standardized, and early return to sports less than 9 months of surgery should be avoided.
Current Concepts
Increased incidence of paediatric ACL injuries correlated with increased participation of children in competitive sports, increased awareness, and better imaging modalities.
Several “physeal-sparing” techniques have evolved. The fixation of the graft is done using interference screws and/or suspensory buttons. The tunnel placement into the center of ACL footprint and anatomic fixation allows for a better clinical outcome with minimal complications. Internal bracing using sutures augments the acute proximal ACL tear repair.
Skeletally immature cases have a 2.5–3.5 times increased risk of ACL graft ruptures and a threefold increase in contralateral ACL injury when compared to the adults.
A specific pattern of bone bruises and lateral meniscal injuries are the commonly associated injuries.
Neuromuscular conditioning helps prevent graft rupture rates, and early return to sports within 9 months of reconstruction is not advocated.
Future Perspectives
Multicentric, randomized control trials to find the ideal autograft for these high demand cohorts.
Strong, stable, and anatomic autograft fixation using “physeal-sparing” technique in skeletally immature children without causing much growth disturbances and other related complications.
Studies focusing on injury prevention strategies to reduce the graft rupture and contralateral ACL injury rates.
Standardizing the return to sports protocol with possible early return to same-level sports.
Acknowledgements
None.
Author Contributions
MSD: conceptualization, and critical revision of the manuscript. KR: manuscript drafting, article selection and review, data analysis, and interpretation. RKR: article selection and review, and manuscript drafting. NRG: manuscript revision, data curation, and supervision.
Funding
Nil. None of the authors received financial support for this study.
Declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Ethical approval
As this is a review of literature, approval by Institutional Ethics committee was deemed unnecessary. Departmental review board approval was obtained.
Informed consent
For this type of study the formal consent is not required.
Footnotes
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Contributor Information
Mandeep Singh Dhillon, Email: drdhillon@gmail.com.
Karthick Rangasamy, Email: drsrk05@gmail.com.
Rajesh Kumar Rajnish, Email: duktiraj@gmail.com.
Nirmal Raj Gopinathan, Email: dr.nirmalraj78@gmail.com.
References
- 1.Beck NA, Lawrence JTR, Nordin JD, DeFor TA, Tompkins M. ACL Tears in school-aged children and adolescents over 20 years. Pediatrics. 2017;139(3):e20161877. doi: 10.1542/peds.2016-1877. [DOI] [PubMed] [Google Scholar]
- 2.Aichroth PM, Patel DV, Zorrilla P. The natural history and treatment of rupture of the anterior cruciate ligament in children and adolescents. A prospective review. Journal of Bone and Joint Surgery. British Volume. 2002;84(1):38–41. doi: 10.1302/0301-620x.84b1.11773. [DOI] [PubMed] [Google Scholar]
- 3.Ramski DE, Kanj WW, Franklin CC, Baldwin KD, Ganley TJ. Anterior cruciate ligament tears in children and adolescents: A meta-analysis of non-operative versus operative treatment. American Journal of Sports Medicine. 2014;42(11):2769–2776. doi: 10.1177/0363546513510889. [DOI] [PubMed] [Google Scholar]
- 4.Werner BC, Yang S, Looney AM, Gwathmey FW., Jr Trends in pediatric and adolescent anterior cruciate ligament injury and reconstruction. Journal of Pediatric Orthopedics. 2016;36(5):447–452. doi: 10.1097/BPO.0000000000000482. [DOI] [PubMed] [Google Scholar]
- 5.Dumont GD, Hogue GD, Padalecki JR, et al. Meniscal and chondral injuries associated with pediatric anterior cruciate ligament tears: Relationship of treatment time and patient-specific factors. American Journal of Sports Medicine. 2012;40:2128–2133. doi: 10.1177/0363546512449994. [DOI] [PubMed] [Google Scholar]
- 6.Kocher MS, Saxon HS, Hovis WD, Hawkins RJ. Management and complications of anterior cruciate ligament injuries in skeletally immature patients: Survey of the Herodicus Society and The ACL Study Group. Journal of Pediatric Orthopedics. 2002;22(4):452–457. [PubMed] [Google Scholar]
- 7.Bonnard C, Fournier J, Babusiaux D, Planchenault M, Bergerault F, de Courtivron B. Physeal-sparing reconstruction of anterior cruciate ligament tears in children: Results of 57 cases using patellar tendon. Journal of Bone and Joint Surgery. British Volume. 2011;93(4):542–547. doi: 10.1302/0301-620X.93B4.25801. [DOI] [PubMed] [Google Scholar]
- 8.Ardern CL, Ekås G, Grindem H, Moksnes H, Anderson A, Chotel F, et al. 2018 International Olympic Committee consensus statement on prevention, diagnosis and management of paediatric anterior cruciate ligament (ACL) injuries. British Journal of Sports Medicine. 2018;52:422–438. doi: 10.1136/bjsports-2018-099060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Stanitski CL, Harvell JC, Fu F. Observations on acute knee hemarthrosis in children and adolescents. Journal of Pediatric Orthopedics. 1993;13:506–510. doi: 10.1097/01241398-199307000-00016. [DOI] [PubMed] [Google Scholar]
- 10.Luhmann SJ. Acute traumatic knee effusions in children and adolescents. Journal of Pediatric Orthopedics. 2003;23:199–202. [PubMed] [Google Scholar]
- 11.Askenberger M, Ekstrom W, Finnbogason T, et al. Occult intraarticular knee injuries in children with hemarthrosis. American Journal of Sports Medicine. 2014;42:1600–1606. doi: 10.1177/0363546514529639. [DOI] [PubMed] [Google Scholar]
- 12.Dodwell ER, LaMont LE, Green DW, Pan TJ, Marx RG, Lyman S. 20 Years of pediatric anterior cruciate ligament reconstruction in New York State. American Journal of Sports Medicine. 2014;42:675–680. doi: 10.1177/0363546513518412. [DOI] [PubMed] [Google Scholar]
- 13.Clanton T, DeLee J, Sanders B, Neidre A. Knee ligament injuries in children. J. Bone Jt. Surg. 1979;61:1195–1201. [PubMed] [Google Scholar]
- 14.DeLEE JC, Curtis R. Anterior cruciate ligament insufficiency in children. Clinical Orthopaedics and Related Research. 1983;172:112–118. [PubMed] [Google Scholar]
- 15.Lipscomb AB, Anderson A. Tears of the anterior cruciate ligament in adolescents. J. Bone Jt. Surg. Am. 1986;68:19–28. [PubMed] [Google Scholar]
- 16.Shea KG, Grimm NL, Ewing CK, Aoki SK. Youth sports anterior cruciate ligament and knee injury epidemiology: Who is getting injured? In what sports? When? Clinics in Sports Medicine. 2011;30:691–706. doi: 10.1016/j.csm.2011.07.004. [DOI] [PubMed] [Google Scholar]
- 17.Weitz FK, Sillanpää PJ, Mattila VM. The incidence of paediatric ACL injury is increasing in Finland. Knee Surgery, Sports Traumatology, Arthroscopy. 2020;28(2):363–368. doi: 10.1007/s00167-019-05553-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Shaw L, Finch CF. Trends in pediatric and adolescent anterior cruciate ligament injuries in Victoria, Australia 2005–2015. International Journal of Environmental Research and Public Health. 2017;14(6):599. doi: 10.3390/ijerph14060599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Domzalski M, Grzelak P, Gabos P. Risk factors for anterior cruciate ligament injury in skeletally immature patients: Analysis of intercondy- lar notch width using magnetic resonance imaging. International Orthopaedics. 2010;34(5):703–707. doi: 10.1007/s00264-010-0987-7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Tjoumakaris FP, Donegan DJ, Sekiya JK. Partial tears of the anterior cruciate ligament: Diagnosis and treatment. American Journal of Orthopedics. 2011;40:92–97. [PubMed] [Google Scholar]
- 21.Holden S, Boreham C, Delahunt E. Sex differences in landing biome- chanics and postural stability during adolescence: A systematic review with meta-analyses. Sports Medicine (Auckland, N. Z.) 2016;46(2):241–253. doi: 10.1007/s40279-015-0416-6. [DOI] [PubMed] [Google Scholar]
- 22.Moksnes H, Grindem H. Prevention and rehabilitation of paediatric ante- rior cruciate ligament injuries. Knee Surgery, Sports Traumatology, Arthroscopy. 2016;24(3):730–736. doi: 10.1007/s00167-015-3856-5. [DOI] [PubMed] [Google Scholar]
- 23.Stanitski CL, Harvell JC, Fu F. Observations on acute knee hemarthrosis in children and adoles-cents. Journal of Pediatric Orthopedics. 1993;13:506–510. doi: 10.1097/01241398-199307000-00016. [DOI] [PubMed] [Google Scholar]
- 24.Xavier PM, Fournier J, de Courtivron B, Bergerault F, Bonnard C. Rare ACL enthesis tears treated by suture in children. A report of 14 cases after a mean 15 years follow-up. Orthopaedics & Traumatology, Surgery & Research. 2016;102(5):619–623. doi: 10.1016/j.otsr.2016.06.006. [DOI] [PubMed] [Google Scholar]
- 25.Herring JA. Tachdijian’s pediatric orthopedics. 3. Saunders; 2002. p. 2354. [Google Scholar]
- 26.Stanitski CL, DeLee JC, Drez D. Orthopedic sports medicine. Saunders; 1994. p. 416. [Google Scholar]
- 27.Rinaldi E, Mazzarella F. Isolated fracture-avulsions of the tibial insertions of the cruciate ligaments of the knee. Ital J Othop Traumatol. 1980;6:77–83. [PubMed] [Google Scholar]
- 28.Ogden JA. Skeletal injury in the child. 3. Springer-Verlag; 2000. p. 948. [Google Scholar]
- 29.Kocher MS, Micheli LJ, Gerbino P, Hresko MT. Tibial eminence fractures in children: Prevalence of meniscal entrapment. American Journal of Sports Medicine. 2003;31:404–407. doi: 10.1177/03635465030310031301. [DOI] [PubMed] [Google Scholar]
- 30.Tudisco C, Giovarruscio R, Febo A, Savarese E, Bisicchia S. Intercondylar eminence avulsion fracture in children: Long-term follow-up of 14 cases at the end of skeletal growth. Journal of Pediatric Orthopedics. Part B. 2010;19:403–408. doi: 10.1097/BPB.0b013e32833a5f4d. [DOI] [PubMed] [Google Scholar]
- 31.Boden BP, Dean GS, Feagin JA, Jr, Garrett WE., Jr Mechanisms of anterior cruciate ligament injury. Orthopedics. 2000;23(6):573–578. doi: 10.3928/0147-7447-20000601-15. [DOI] [PubMed] [Google Scholar]
- 32.Anderson AF. Transepiphyseal replacement of the anterior cruciate ligament using quadruple hamstring grafts in skeletally immature patients. Journal of Bone and Joint Surgery. American Volume. 2004;86-A Suppl 1(Pt 2):201–209. doi: 10.2106/00004623-200409001-00010. [DOI] [PubMed] [Google Scholar]
- 33.Beynnon BD, Johnson RJ, Abate JA, Fleming BC, Nichols CE. Treatment of anterior cruciate ligament injuries, part I. American Journal of Sports Medicine. 2005;33(10):1579–1602. doi: 10.1177/0363546505279913. [DOI] [PubMed] [Google Scholar]
- 34.Kocher MS, Smith JT, Zoric BJ, Lee B, Micheli LJ. Transphyseal anterior cruciate ligament reconstruction in skeletally immature pubescent adolescents. Journal of Bone and Joint Surgery. American Volume. 2007;89(12):2632–2639. doi: 10.2106/JBJS.F.01560. [DOI] [PubMed] [Google Scholar]
- 35.Lawrence JT, Argawal N, Ganley TJ. Degeneration of the knee joint in skeletally immature patients with a diagnosis of an anterior cruciate ligament tear: Is there harm in delay of treatment? American Journal of Sports Medicine. 2011;39(12):2582–2587. doi: 10.1177/0363546511420818. [DOI] [PubMed] [Google Scholar]
- 36.Millett PJ, Willis AA, Warren RF. Associated injuries in pediatric and adolescent anterior cruciate ligament tears: Does a delay in treatment increase the risk of meniscal tear? Arthroscopy. 2002;18(9):955–959. doi: 10.1053/jars.2002.36114. [DOI] [PubMed] [Google Scholar]
- 37.Trivedi V, Mishra P, Verma D. Pediatric ACL Injuries: A Review of Current Concepts. Open Orthop J. 2017;28(11):378–388. doi: 10.2174/1874325001711010378. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Mall NA, Paletta GA. Pediatric ACL injuries: Evaluation and management. Current Reviews in Musculoskeletal Medicine. 2013;6(2):132–140. doi: 10.1007/s12178-013-9169-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Aronowitz ER, Ganley TJ, Goode JR, Gregg JR, Meyer JS. Anterior cruciate ligament reconstruction in adolescents with open physes. American Journal of Sports Medicine. 2000;28:168–175. doi: 10.1177/03635465000280020601. [DOI] [PubMed] [Google Scholar]
- 40.Shelbourne KD, Wilckens JH, Mollabashy A, DeCarlo M. Arthrofibrosis in acute anterior cruciate ligament reconstruction. The effect of timing of reconstruction and rehabilitation. American Journal of Sports Medicine. 1991;19(4):332–336. doi: 10.1177/036354659101900402. [DOI] [PubMed] [Google Scholar]
- 41.Kocher MS, Garg S, Micheli LJ. Physeal sparing reconstruction of the anterior cruciate ligament in skeletally immature prepubescent children and adolescents. Journal of Bone and Joint Surgery. American Volume. 2005;87(11):2371–2379. doi: 10.2106/JBJS.D.02802. [DOI] [PubMed] [Google Scholar]
- 42.Micheli LJ, Rask B, Gerberg L. Anterior cruciate ligament reconstruction in patients who are prepubescent. Clinical Orthopaedics and Related Research. 1999;364:40–47. doi: 10.1097/00003086-199907000-00006. [DOI] [PubMed] [Google Scholar]
- 43.Fabricant PD, Kocher MS. Management of ACL Injuries in Children and Adolescents. Journal of Bone and Joint Surgery. American Volume. 2017;99(7):600–612. doi: 10.2106/JBJS.16.00953. [DOI] [PubMed] [Google Scholar]
- 44.Lo IK, Kirkley A, Fowler PJ, Miniaci A. The outcome of operatively treated anterior cruciate ligament disruptions in the skeletally immature child. Arthroscopy. 1997;13(5):627–634. doi: 10.1016/s0749-8063(97)90191-2. [DOI] [PubMed] [Google Scholar]
- 45.Demange MK, Camanho GL. Nonanatomic anterior cruciate ligament reconstruction with double-stranded semitendinosus grafts in children with open physes: Minimum 15-year follow-up. American Journal of Sports Medicine. 2014;42(12):2926–2932. doi: 10.1177/0363546514550981. [DOI] [PubMed] [Google Scholar]
- 46.Milewski MD, Beck NA, Lawrence JT, Ganley TJ. Anterior cruciate ligament reconstruction in the young athlete: A treatment algorithm for the skeletally immature. Clinics in Sports Medicine. 2011;30:801–810. doi: 10.1016/j.csm.2011.08.001. [DOI] [PubMed] [Google Scholar]
- 47.Lawrence JTR, Bowers AL, Belding J, Cody SR, Ganley TJ. All epiphyseal anterior cruciate ligament reconstruction in skeletally immature patients. Clinical Orthopaedics and Related Research. 2010;468:1971–1977. doi: 10.1007/s11999-010-1255-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Pennock AT, Chambers HG, Turk RD, Parvanta KM, Dennis MM, Edmonds EW. Use of a modified all-epiphyseal technique for anterior cruciate ligament reconstruction in the skeletally immature patient. Orthopaedic Journal of Sports Medicine. 2018;6(7):2325967118781769. doi: 10.1177/2325967118781769. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Willson RG, Kostyun RO, Milewski MD, Nissen CW. Anterior cruciate ligament reconstruction in skeletally immature patients: Early results using a hybrid physeal-sparing technique. Orthopaedic Journal of Sports Medicine. 2018;6(2):2325967118755330. doi: 10.1177/2325967118755330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Berg EE. Comminuted tibial eminence anterior cruciate ligament avulsion fractures: Failure of arthroscopic treatment. Arthroscopy. 1993;9:446–450. doi: 10.1016/s0749-8063(05)80320-2. [DOI] [PubMed] [Google Scholar]
- 51.Mahar AT, Duncan D, Oka R, Lowry A, Gillingham B, Chambers H. Biomechanical comparison of four different fixation techniques for pediatric tibial eminence avulsion fractures. Journal of Pediatric Orthopedics. 2008;28:159–162. doi: 10.1097/BPO.0b013e318164ee43. [DOI] [PubMed] [Google Scholar]
- 52.Bong MR, Romero A, Kubiak E, Iesaka K, Heywood CS, Kummer F, et al. Suture vs screw fixation of displaced tibial eminence fractures: A biomechanical comparison. Arthroscopy. 2005;21:1172–1176. doi: 10.1016/j.arthro.2005.06.019. [DOI] [PubMed] [Google Scholar]
- 53.van Eck CF, Limpisvasti O, ElAttrache NS. Is there a role for internal bracing and repair of the anterior cruciate ligament? A systematic literature review. American Journal of Sports Medicine. 2018;46(9):2291–2298. doi: 10.1177/0363546517717956. [DOI] [PubMed] [Google Scholar]
- 54.Smith JO, Yasen SK, Palmer HC, Lord BR, Britton EM, Wilson AJ. Paediatric ACL repair reinforced with temporary internal bracing. Knee Surgery, Sports Traumatology, Arthroscopy. 2016;24(6):1845–1851. doi: 10.1007/s00167-016-4150-x. [DOI] [PubMed] [Google Scholar]
- 55.Pennock AT, Johnson KP, Turk RD, Bastrom TP, Chambers HG, Boutelle KE, Edmonds EW. Transphyseal anterior cruciate ligament reconstruction in the skeletally immature: Quadriceps tendon autograft versus hamstring tendon autograft. Orthopaedic Journal of Sports Medicine. 2019;7(9):2325967119872450. doi: 10.1177/2325967119872450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Runer A, Csapo R, Hepperger C, Herbort M, Hoser C, Fink C. Anterior cruciate ligament reconstructions with quadriceps tendon autograft result in lower graft rupture rates but similar patient-reported outcomes as compared with hamstring tendon autograft: A comparison of 875 patients. American Journal of Sports Medicine. 2020;48(9):2195–2204. doi: 10.1177/0363546520931829. [DOI] [PubMed] [Google Scholar]
- 57.Andernord D, Desai N, Bjornsson H, Ylander M, Karlsson J, Samuelsson K. Patient predictors of early revision surgery after anterior cruciate ligament reconstruction: A cohort study of 16,930 patients with 2-year follow-up. American Journal of Sports Medicine. 2015;43(1):121–127. doi: 10.1177/0363546514552788. [DOI] [PubMed] [Google Scholar]
- 58.Astur DC, Arliani GC, Debieux P, Kaleka CC, Amaro JT, Cohen M. Intraarticular hamstring graft diameter decreases with continuing knee growth after ACL reconstruction with open physes. Knee Surgery, Sports Traumatology, Arthroscopy. 2016;24(3):792–795. doi: 10.1007/s00167-016-4030-4. [DOI] [PubMed] [Google Scholar]
- 59.Dekker TJ, Godin JA, Dale KM, Garrett WE, Taylor DC, Riboh JC. Return to sport after pediatric anterior cruciate ligament reconstruction and its effect on subsequent anterior cruciate ligament injury. Journal of Bone and Joint Surgery. American Volume. 2017;99(11):897–904. doi: 10.2106/JBJS.16.00758. [DOI] [PubMed] [Google Scholar]
- 60.DeFrancesco CJ, Striano BM, Bram JT, Baldwin KD, Ganley TJ. An in-depth analysis of graft rupture and contralateral anterior cruciate ligament rupture rates after pediatric anterior cruciate ligament reconstruction. American Journal of Sports Medicine. 2020;48(10):2395–2400. doi: 10.1177/0363546520935437. [DOI] [PubMed] [Google Scholar]
- 61.Astur DC, Aretti JV, Cavalcante ELB, Goes A, Jr, Kaleka CC, Debieux P, et al. Pediatric anterior cruciate ligament reruptures are related to lower functional scores at the time of return to activity: A prospective, midterm follow-up study. Orthopaedic Journal of Sports Medicine. 2019;7(12):2325967119888888. doi: 10.1177/2325967119888888. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Morgan MD, Salmon LJ, Waller A, Roe JP, Pinczewski LA. Fifteen-year survival of endoscopic anterior cruciate ligament reconstruction in patients aged 18 years and younger. American Journal of Sports Medicine. 2016;44(2):384–392. doi: 10.1177/0363546515623032. [DOI] [PubMed] [Google Scholar]
- 63.Andernord D, Desai N, Bjornsson H, et al. Predictors of contralateral anterior cruciate ligament reconstruction: A cohort study of 9061 patients with 5-year follow-up. American Journal of Sports Medicine. 2015;43:295–302. doi: 10.1177/0363546514557245. [DOI] [PubMed] [Google Scholar]
- 64.DeFrancesco CJ, Storey EP, Flynn JM, et al. Pediatric ACL reconstruction and return to the operating room: revision is less than half of the story. J Pediatr Orthop. 2017. [Epub ahead of print]. [DOI] [PubMed]
- 65.Patel NM, Bram JT, Talathi NS, DeFrancesco CJ, Lawrence JTR, Ganley TJ. Which children are at risk for contralateral anterior cruciate ligament injury after ipsilateral reconstruction? Journal of Pediatric Orthopedics. 2020;40(4):162–167. doi: 10.1097/BPO.0000000000001364. [DOI] [PubMed] [Google Scholar]
- 66.Zacharias AJ, Whitaker JR, Collofello BS, Wilson BR, Unger RZ, Ireland ML, Johnson DL, Jacobs CA. Secondary injuries after pediatric anterior cruciate ligament reconstruction: A systematic review with quantitative analysis. American Journal of Sports Medicine. 2020;18:363546520934774. doi: 10.1177/0363546520934774. [DOI] [PubMed] [Google Scholar]
- 67.Perrone GS, Webster KE, Imbriaco C, Portilla GM, Vairagade A, Murray MM, Kiapour AM. Risk of secondary ACL injury in adolescents prescribed functional bracing after ACL reconstruction. Orthopaedic Journal of Sports Medicine. 2019;7(11):2325967119879880. doi: 10.1177/2325967119879880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Faunø P, Rømer L, Nielsen T, Lind M. The risk of transphyseal drilling in skeletally immature patients with anterior cruciate ligament injury. Orthopaedic Journal of Sports Medicine. 2016;4(9):2325967116664685. doi: 10.1177/2325967116664685. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69.Wong SE, Feeley BT, Pandya NK. Complications after pediatric acl reconstruction: A meta-analysis. Journal of Pediatric Orthopedics. 2019;39(8):e566–e571. doi: 10.1097/BPO.0000000000001075. [DOI] [PubMed] [Google Scholar]
- 70.Bordoni V, di Laura FG, Previtali D, Tamborini S, Candrian C, Cristallo Lacalamita M, Del Grande F, Filardo G. Bone bruise and anterior cruciate ligament tears: Presence, distribution pattern, and associated lesions in the pediatric population. American Journal of Sports Medicine. 2019;47(13):3181–3186. doi: 10.1177/0363546519872975. [DOI] [PubMed] [Google Scholar]
- 71.Aretti JV, Shin JJ, Albers M, Chambers MC, Cohen M, Musahl V, Fu FH. Bone bruise patterns in skeletally immature patients with anterior cruciate ligament injury: Shock-absorbing function of the physis. American Journal of Sports Medicine. 2018;46(9):2128–2132. doi: 10.1177/0363546518777247. [DOI] [PubMed] [Google Scholar]
- 72.Feucht MJ, Brucker PU, Camathias C, Frosch KH, Hirschmann MT, Lorenz S, Mayr HO, Minzlaff P, Petersen W, Saier T, Schneidmüller D, Stoehr A, Wagner D, Südkamp NP, Niemeyer P. Meniscal injuries in children and adolescents undergoing surgical treatment for tibial eminence fractures. Knee Surgery, Sports Traumatology, Arthroscopy. 2017;25(2):445–453. doi: 10.1007/s00167-016-4184-0. [DOI] [PubMed] [Google Scholar]
- 73.Vavken P, Tepolt FA, Kocher MS. Concurrent meniscal and chondral injuries in pediatric and adolescent patients undergoing ACL reconstruction. Journal of Pediatric Orthopedics. 2018;38(2):105–109. doi: 10.1097/BPO.0000000000000777. [DOI] [PubMed] [Google Scholar]
- 74.Malatray M, Raux S, Peltier A, Pfirrmann C, Seil R, Chotel F. Ramp lesions in ACL deficient knees in children and adolescent population: A high prevalence confirmed in intercondylar and posteromedial exploration. Knee Surgery, Sports Traumatology, Arthroscopy. 2018;26(4):1074–1079. doi: 10.1007/s00167-017-4471-4. [DOI] [PubMed] [Google Scholar]
- 75.Rhodes JT, Cannamela PC, Cruz AI, Mayo M, Styhl AC, Richmond CG, Ganley TJ, Shea KG. Incidence of Meniscal Entrapment and Associated Knee Injuries in Tibial Spine Avulsions. Journal of Pediatric Orthopedics. 2018;38(2):e38–e42. doi: 10.1097/BPO.0000000000001110. [DOI] [PubMed] [Google Scholar]
- 76.Munger AM, Gonsalves NR, Sarkisova N, Clarke E, VandenBerg CD, Pace JL. Confirming the Presence of Unrecognized Meniscal Injuries on Magnetic Resonance Imaging in Pediatric and Adolescent Patients With Anterior Cruciate Ligament Tears. Journal of Pediatric Orthopedics. 2019;39(9):e661–e667. doi: 10.1097/BPO.0000000000001331. [DOI] [PubMed] [Google Scholar]
- 77.Kinsella SD, Rider SM, Fury MS, Tepolt FA, Ecklund K, Kocher MS. Concomitant posterolateral corner injuries in skeletally immature patients with acute anterior cruciate ligament injuries. Journal of Pediatric Orthopedics. 2019 doi: 10.1097/BPO.0000000000001450. [DOI] [PubMed] [Google Scholar]
- 78.Paterno MV, Huang B, Thomas S, Hewett TE, Schmitt LC. Clinical factors that predict a second ACL injury after ACL reconstruction and return to sport: Preliminary development of a clinical decision algorithm. Orthopaedic Journal of Sports Medicine. 2017;5(12):2325967117745279. doi: 10.1177/2325967117745279. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Cordasco FA, Black SR, Price M, Wixted C, Heller M, Asaro LA, Nguyen J, Green DW. Return to Sport and Reoperation Rates in Patients Under the Age of 20 After Primary Anterior Cruciate Ligament Reconstruction: Risk Profile Comparing 3 Patient Groups Predicated Upon Skeletal Age. American Journal of Sports Medicine. 2019;47(3):628–639. doi: 10.1177/0363546518819217. [DOI] [PubMed] [Google Scholar]
- 80.Beischer S, Hamrin Senorski E, Thomeé C, Samuelsson K, Thomeé R. Young athletes return too early to knee-strenuous sport, without acceptable knee function after anterior cruciate ligament reconstruction. Knee Surgery, Sports Traumatology, Arthroscopy. 2018;26(7):1966–1974. doi: 10.1007/s00167-017-4747-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Geffroy L, Lefevre N, Thevenin-Lemoine C, Peyronnet A, Lakhal W, Fayard JM, Chotel F. French Arthroscopy Society. Return to sport and re-tears after anterior cruciate ligament reconstruction in children and adolescents. Orthopaedics & Traumatology, Surgery & Research. 2018;104(8S):183–188. doi: 10.1016/j.otsr.2018.09.006. [DOI] [PubMed] [Google Scholar]
- 82.Ithurburn MP, Paljieg A, Thomas S, Hewett TE, Paterno MV, Schmitt LC. Strength and function across maturational levels in young athletes at the time of return to sport after ACL reconstruction. Sports Health. 2019;11(4):324–331. doi: 10.1177/1941738119849070. [DOI] [PMC free article] [PubMed] [Google Scholar]