Key Teaching Points.
-
•
Early pacing was challenging and often resulted in multiple lead revisions and generator replacements.
-
•
Technological advancements in battery chemistry have dramatically improved the intervals between interventions required for patients with cardiac pacemakers.
-
•
Developments in cardiac pacing electronics now allow more sophisticated programming and predictable functionality.
Introduction
On October 8, 1958, the first rechargeable pacemaker, developed by Rune Elmquist, was implanted in Sweden by Ake Senning.1,2 The recipient of this device, Arne Larsson, was paced for the remaining 43years of his life, receiving 22 pulse generators and 5 lead revisions.2 In June 1960 the first self-powered implantable pacemaker was implanted by William Chardack in the United States; this lasted 2 years, until the patient died of natural causes.2,3 Pacemakers then became commercially available from 1961.4 The Guinness World Records state the longest single lifetime of a device to be 37 years, 281 days.5 We present a patient who was cardiac paced for 53 years, which we believe to be the longest in documented history. This patient’s story highlights the problems associated with early pacing systems, transvenous pacing from a young age, and the evolution of generator and lead technology.
Case report
On November 29, 1969, a previously well 36-year-old man presented following a syncopal episode. Initial investigations revealed second-degree heart block (Mobitz II) with a right bundle branch pattern and ventricular rate of 45 beats per minute (bpm) (Figure 1). Diagnosed with Stokes-Adam attack, the patient was admitted and commenced on long-acting isoprenaline and 40 mg prednisone.
Figure 1.
Electrocardiogram documenting presenting and subsequent heart rhythms with early interventions. Top line: Day 3 admission – lead II with isoprenaline infusion Mobitz II. Second line: Day 3 admission – V1 with isoprenaline infusion Mobitz II. Third line: Day 5 admission – lead II temporary pacemaker in situ at 78 beats/min. Bottom line: Day 5 admission – lead II with isoprenaline infusion Mobitz II rhythm.
The patient remained in heart block for a further 19 days while receiving both medical and temporary pacing therapy. On December 18, 1969, his first permanent system, a nonprogrammable mercury-zinc battery–powered Teletronics P6 (Figure 2) with a unipolar lead, was implanted via the right external jugular vein. A lead revision was required 3 days later for ongoing pectoral stimulation. Upon opening of the pocket, incomplete nylon set screw insertion was discovered, resulting in a battery short. The set holes were cleaned and filled with stopcock grease and the existing lead reinserted, then covered in silicone sealant, resolving pectoral stimulation.
Figure 2.
Examples of the pacemakers the patient received. From left to right, top to bottom: Teletronics P6 (1969), Teletronics P10 (1972 & 1974), Teletronics 120B (1976), Intermedics 223-01 (1980), Medtronic Mirel VL (1980), Medtronic Activatrax VVI+ (1986), Medtronic Legend 8416 (1995), St Jude Verity ADX 5156 (2008), Medtronic Azure SR (2021).
In February 1972 the patient presented with a ventricular rate of 43 bpm. The cause was attributed to pacemaker battery depletion, and an acute generator change to a Teletronics P10 (Figure 2) was performed. The patient again presented in September 1974 with a ventricular rate below 50 bpm and electrocardiogram (ECG) documented exit block. A manual lead extraction was attempted but failed owing to dense attachment on the tricuspid ring, requiring a new Teletronics P10 (Figure 2) generator and Teletronics PY3620/60 unipolar lead implantation via the right internal jugular. Two further presentations with ventricular rates below the fixed rate, in March 1976 and early May 1980, resulted in generator changes for battery depletion, first to a lithium-iodide battery–powered Teletronics 120B (Figure 2) and subsequently to an Intermedics 223-01 (Figure 2), with similar functionality.
Ten days after this generator change the patient experienced bradycardia in the community. Presenting ECG illustrated ventricular standstill, ventricular tachycardia, and ventricular fibrillation. A temporary pacemaker was acutely implanted as a bridge for 3 days until a programmable Medtronic Mirel VL generator (Figure 2) and Medtronic BP 6962-65 bipolar lead were implanted via the left external jugular. With dense myocardial attachment preventing manual extraction, the nonfunctioning right-sided Teletronics PY3620/60 lead was capped and buried.
An outpatient ECG in August 1986 showed loss of pacing, requiring acute lead replacement. A Medtronic target tip bipolar 4012 was implanted via the left cephalic vein and connected to a Medtronic Activatrax generator (Figure 2), the first commercially available rate-responsive pacemaker. In February 1989 one of the partially explanted right-sided leads eroded through the pectoral muscle region and required surgical intervention to trim the lead body. The patient then developed a chronic right-sided sinus infection requiring long-term drainage and medical treatment.
In June 1995 replacement indictors on the Activatrax were detected at a routine follow-up and the device was electively replaced with a Medtronic Legend 8416 (Figure 2). After 13 years, normal battery depletion triggered elective replacement to a St Jude Verity ADX 5156 (Figure 2). At this generator change a visible insulation breach was noted at the lead yoke and although the lead was alerted for polyurethane degradation, given that all parameters were within normal limits and a significant volume of hardware was already in situ, the breach was repaired with a splice kit. When scheduling elective box change for normal battery depletion in October 2021, it was decided replacement was necessary given the lead age of 36 years. With the right sinus now dry, a Medtronic 5076 was successfully implanted via right cephalic access and connected to a Medtronic Azure single-chamber pacemaker (Figures 2 and 3).
Figure 3.
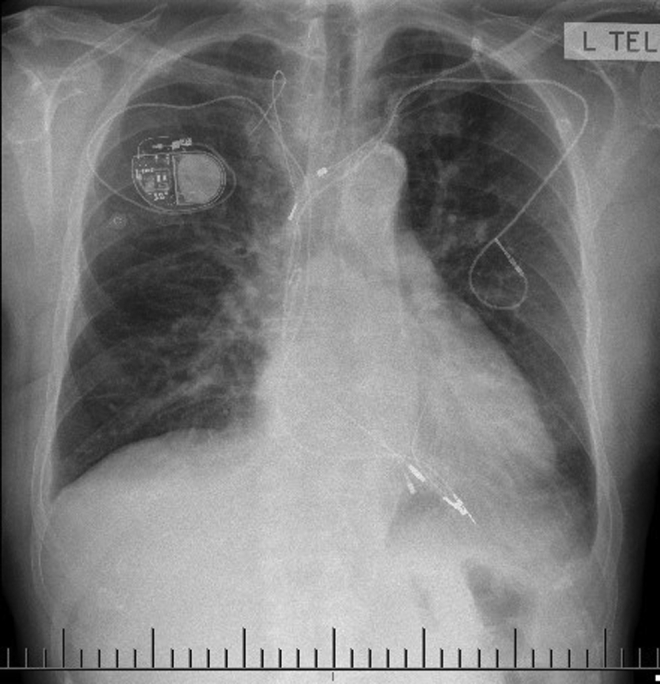
Chest radiograph October 2021 following tenth generator implant.
Discussion
We believe this patient with 53 years of pacing to be the longest reported example of cardiac pacing. While cardiac pacing is now regarded as routine with advancements in battery chemistry and software and hardware technology, this was not the case in the early days of cardiac pacing. The first fully implanted pacemaker in 1958 failed after 8 hours.1 Pacemakers were initially implanted with epicardial leads, requiring thoracotomy, and these patients typically had extreme bradycardia and were electrically unstable. The periprocedural mortality was up to 10%, device failure was common, and at best the mercury-zinc battery–powered devices lasted only 24 months before needing replacement.6 Long-term mortality remained high in paced patients, typically 20% at 1 year, and long-term survival was uncommon.7
Technical developments through the 1960s and 1970s improved these outcomes and presaged the modern era of permanent cardiac pacing. Placement of transvenous leads reduced the operative risk and provided more reliable long-term pacing. However, transvenous leads would and continue to still ultimately fail, requiring replacement. Transvenous leads also have long-term vascular risks, including venous obstruction and the risks associated with extraction.8 Improvements in pacing electronics allowed for ventricular sensing and demand pacing and the most important advance in this period was the introduction of the lithium battery, which improved device longevity and reliability.8,9
Having had 11 acute interventions for sudden battery depletion or acute lead failure in the first 20 years and only 3 elective interventions in the latter 33 years, this patient’s case demonstrates the risk and uncertainty of cardiac pacing prior to the modern era. These uncertain outcomes are now more routinely mitigated by follow-up with sophisticated software systems and developments in hardware manufacturing.
Conclusion
We believe this patient is the longest continuously paced patient in the world. He survives despite suffering the usual device failures commonly associated with early cardiac pacing systems, and his case illustrates the great advances in implantable cardiac pacemaker technology since the first implant in 1958.
Footnotes
Funding Sources: The authors have no funding sources to disclose.
Disclosures: All authors confirm no conflicts of interest to declare.
References
- 1.Elmqvist R. Review of early pacemaker development. Pacing Clin Electrophysiol. 1978;1:535–536. doi: 10.1111/j.1540-8159.1978.tb03518.x. [DOI] [PubMed] [Google Scholar]
- 2.Aquilina O. A brief history of cardiac pacing. Images Paediatr Cardiol. 2006;8:17–81. [PMC free article] [PubMed] [Google Scholar]
- 3.Chardack W.M., Gage A.A., Greatbach W. A transistorised, self-contained, implantable pacemaker for the long-term correction of complete heart block. Surgery. 1960;48:643–654. [PubMed] [Google Scholar]
- 4.Mond H.G., Hunt D., Vohra J., Sloman J.G. Cardiac pacing: memories of a bygone era. Pacing Clin Electrophysiol. 2008;31:1192–1201. doi: 10.1111/j.1540-8159.2008.01163.x. [DOI] [PubMed] [Google Scholar]
- 5.Guinness World Records https://www.guinnessworldrecords.com/world-records/longest-working-pacemaker-(present-day
- 6.Chardack W.M., Gage A.A., Federico A.J., Schimert G., Greatbatch W. Clinical experience with an implantable pacemaker. Sciences. 1964;3 doi: 10.1111/j.1749-6632.1964.tb53175.x. 813-112. [DOI] [PubMed] [Google Scholar]
- 7.Chardack W.M., Gage A.A., Federico A.J., Schimert G., Greatbatch W. Five years’ clinical experience with implantable pacemaker. An appraisal. Surgery. 1965;58:915. [PubMed] [Google Scholar]
- 8.Jeffrey K., Parsonnet V. Cardiac pacing, 1960-1985: a quarter century of medical and industrial innovation. Circulation. 1998;97:1978–1991. doi: 10.1161/01.cir.97.19.1978. [DOI] [PubMed] [Google Scholar]
- 9.Burr L.H. The lithium iodide-powered cardiac pacemaker. Clinical experience with 250 implantations. J Thorac Cardiovasc Surg. 1977;73:421–423. [PubMed] [Google Scholar]




