Abstract
The use of the electronic health record (EHR) system to identify and address social determinants of health (SDOH) in vulnerable patients is still lacking, and examples for customizing the EHR to meet the workflows of clinical and administrative professionals are missing. We custom designed and built into the Epic EHR a SDOH screening tool integrated with a community resource network management (CRNM) software-as-a-service (SaaS) platform to systematically identify and address SDOH in Medicare and Medicaid beneficiaries across multiple clinical care settings. We further describe our workflow redesign and EHR implementation process to maximize SDOH screening and referral efficiency. The SDOH EHR solution has been operationally used over three years by staff to screen 111,486 Medicare and Medicaid beneficiaries, identify 7,878 SDOH, and refer 6,103 high-risk beneficiaries to community resources. Transforming an EHR into a catalyst software to support SDOH screening and referral in a clinical setting is an interdisciplinary process that benefits from various technical, administrative, and clinical experts that provide subject matter knowledge into all phases of the build.
Keywords: community referral summary, electronic health records, health information technology, social determinants of health, social needs
Introduction
Social determinants of health (SDOH) continue to be both undetected and unaddressed despite research demonstrating that social, economic, and physical environment factors have an estimated relative contribution of 55 percent to health outcomes that include measures of mortality and morbidity.1, 2 Recent healthcare delivery system reforms have spurred health policy innovations that have placed increasing emphasis on healthcare systems to respond to SDOH and improve population health through systematic strategies that improve patient access to social resources that may address their unmet social needs.
One such healthcare delivery innovation is the Centers for Medicare & Medicaid Services (CMS) Center for Medicare and Medicaid Innovation's (CMMI) Accountable Health Communities (AHC) Model. The goal of the AHC Model is to assess whether systematically identifying and addressing SDOH in community-dwelling Medicare and Medicaid beneficiaries through building effective social services, medical care, public health, and community-based partnerships can improve health outcomes and lower healthcare costs and utilization.3 Participating clinical delivery sites use the CMS CMMI's 10-item Health-Related Social Needs (HRSNs) Screening Tool, the AHC screening tool, to identify non-medical needs across five social risk domains: housing instability, food insecurity, transportation problems, utilities, and interpersonal safety.4
Furthermore, there has been a rise in recent research underscoring the importance of incorporating SDOH screening and referral in the electronic health record (EHR).5-7 Few studies, however, have described their design and implementation approach to integrating an EHR with a community resource network management (CRNM) software-as-a-service (SaaS) platform to systematically identify and address SDOH in community-dwelling Medicare and Medicaid beneficiaries across multiple care settings. In addition, an Institute of Medicine committee8 has highlighted the importance of standardization of data collection on SDOH into patient EHRs as a critical factor that influences treatment care and improves health outcomes.
The purpose of this paper is to describe the design, integration, and implementation of a systematic strategy to identify and screen inpatient, outpatient, and emergency department Medicare and Medicaid beneficiaries for SDOH utilizing EHR decisional support clinical workflows integrated with a CRNM SaaS platform, and upon patient's response, to congruently refer beneficiaries with identified social needs to social service resources in their community. Although this paper is specific to design and integration into Epic EHR (Epic Systems, Verona, Wisconsin), the intent behind the design elements can be generalized to the field and other EHRs.
Methods
Setting
This prospective study is being implemented at Hackensack University Medical Center (HUMC), a suburban research and academic hospital, part of Hackensack Meridian Health Network and the largest provider of inpatient and outpatient services in New Jersey, which includes the Hackensack University Medical Group Accountable Care Organization (ACO). We utilize an enterprise-wide EHR (Epic Systems) integrated with Healthify (2019), a CRNM SaaS platform, to screen and refer Medicare and Medicaid beneficiaries across inpatient, outpatient, and emergency department settings since the implementation of the AHC Model at HUMC in 2018. The description of the available CRNM platforms on the market has been published elsewhere.9 Institutional review board approval was obtained before implementation of the AHC Model at HUMC. HUMC is one of 28 organizations participating in the AHC Model.10
EHR SDOH Screening and Referral Key Design Elements
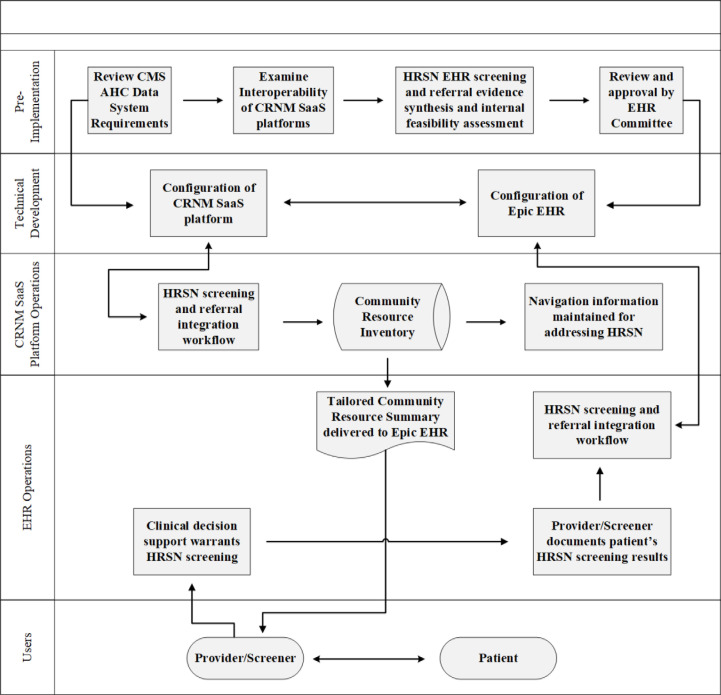
In this section, we describe the EHR SDOH screening and referral design, operational elements, and related clinical workflow functions in ambulatory, inpatient, and emergency department settings (Figure 1). Our EHR design goal was to build on familiar processes by modeling our approach after existing clinical workflows. For example, some of our clinics had an established falls risk screening workflow similar to what we intended to develop for SDOH screening. Therefore, we built upon the existing workflow in the EHR to support the screening process. It is important to note that the SDOH screening is administered to all Medicare and Medicaid beneficiaries regardless of language, literacy level, or whether the patient has a disability.
Figure 1.
EHR SDOH Screening and Referral Design, Integration and Operational Elements
Prior to implementation, we undertook several tasks. First, we reviewed the AHC Model data system logic to guide the modification and configuration of the EHR and the CRNM SaaS platform. While the AHC Model data system logic and the design of the CRNM SaaS platform are beyond the scope of this paper, the data system is required to support activities related to systematic SDOH screenings, providing social service referrals to beneficiaries with identified HRSNs, randomizing high-risk navigation-eligible beneficiaries, and conducting community service navigation.
Concurrently we met with stakeholders across all clinical departments conducting SDOH screening and referral to identify workflows that could be integrated into their existing workflows as to ensure that operations run effectively and efficiently as possible. We focused on automation to decrease the human factor in initiating screening, to minimize burden on screening staff, and to align with current workflows, thereby making this a standard of care. Stakeholders included physician-leaders (e.g., department chairs), administrators, nursing leaders, managers and supervisors, and front-line staff (front desk staff, medical assistants, unit clerks, nurses). Workflow topics ranged from but not limited to: job tasks and system requirements, key processes, EHR applications, implementation barriers, quality improvement plan, and resources required. To support pre-implementation workflow meetings, we created flowcharts of key processes, mapped proposed workflows, and drafted standard operating procedures. The EHR Committee comprised an information technologist, health information management staff, information systems staff, vendors, and trainers, and worked closely with project, clinical, and administrative staff to define workflow requirements, business rules, and other processes. During the implementation phase, customized support and training materials were distributed to clinical departments. Involving people who were affected by the workflow changes strengthened acceptability, effectiveness, and efficiency during testing and rollout. Careful monitoring ensued to track adherence to workflows, end user satisfaction, and EHR design elements. Refinements were made to the workflows and the EHR design throughout testing and implementation to ensure clinical staff needs and internal productivity standards were met.
Ambulatory SDOH Screening
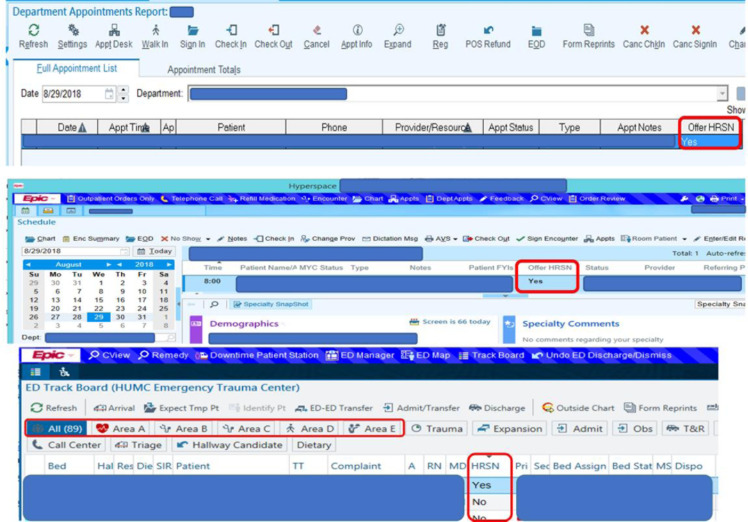
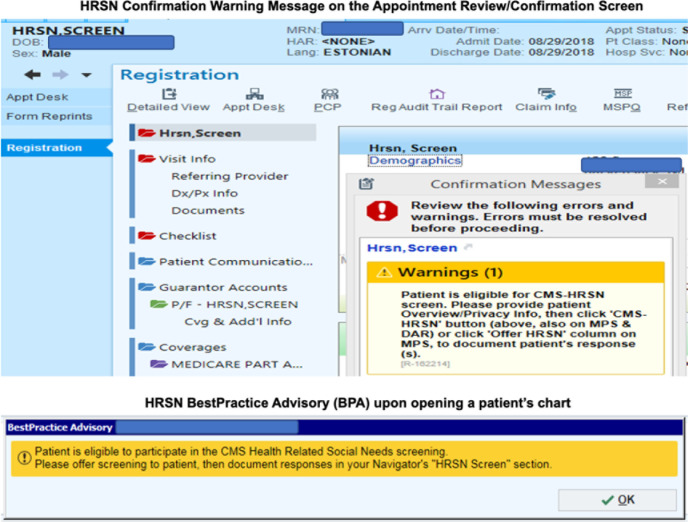
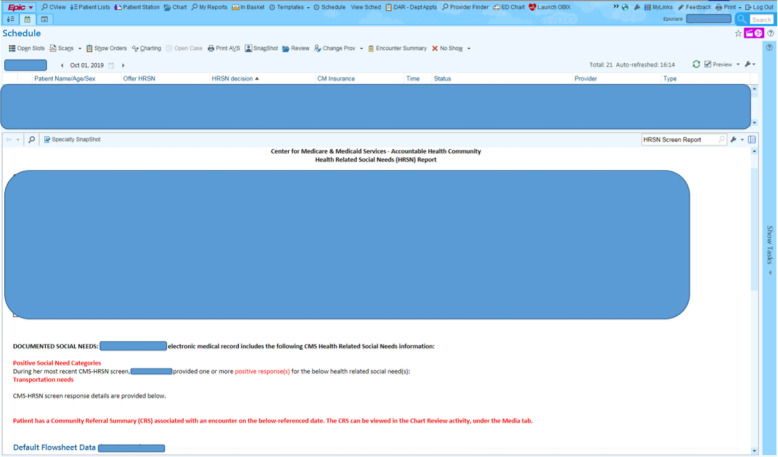
The Epic EHR was configured to allow staff at the clinical delivery sites to conduct the SDOH screening and referral workflow as part of their routine clinical workflow. The EHR was modified in several ways to identify eligible beneficiaries who require SDOH screening. First, we modified EpicCare Ambulatory's Departments Appointments Report (DAR), Multi-Provider Schedule (MPS), and Technologist Work List (TWL) to display an “Offer SDOH screening /Health Related Social Needs (HRSN)” column to staff that indicates by a “Yes” or “No” if the patient meets certain eligibility criteria, namely that the patient is a community-dwelling Medicare and/or Medicaid beneficiary and resides in our catchment area (Figure 2). If the “Offer HRSN” indicates a “Yes,” staff have been trained to screen the patient for SDOH. Additionally, to ensure all Medicare and Medicaid beneficiaries are screened for SDOH, we incorporated into the EHR an alert when a patient meets the eligibility criteria. During the registration and check-in workflows, we added a warning message to the “Confirmation Messages” box on the Appointment Review/Confirmation screen to remind the front desk receptionist to offer the HRSNs screening to the patient (Figure 3). Also, when a medical assistant, sleep technologist, or nurse rooms a patient, or a community health worker engages a patient, and the patient's chart is opened, Epic will display a Best Practice Advisory (BPA) to remind these staff to screen the patient for HRSNs (Figure 3). Upon identifying an eligible patient, staff administer the HRSNs screening tool in one of three ways, or a combination thereof, depending on the method most conducive to the office and patient: 1) self-administered screening where the patient completes the HRSNs screening tool themselves by using a tablet or hard copy version; 2) proxy-administered screening where the parent, guardian, or caregiver is completing the HRSNs screening tool on behalf of the patient by using a tablet or hard copy version; or 3) interviewer-administered screening by using a desktop or laptop where the staff member (e.g., medical assistant, sleep technologist, nurse, community health worker, front desk receptionist) administers the HRSNs screening tool by reading the questions aloud to the patient or proxy. Based on the user role and/or menu settings, staff can access the HRSNs screening tool on any of the following: DAR, MPS, TWL, registration interactive face sheet, or rooming tab, by clicking the “CMS-HRSN” activity button found in the menu toolbar of each of these activities. The staff member who administers the HRSNs screening tool or an office colleague records the patient's responses in the Epic flowsheet. The Epic flowsheet is reflective of the AHC Screening Tool. Screenings completed using a tablet are automatically stored in the patient's EHR as a flowsheet. If the patient screens positive for a SDOH social risk domain, the patient will receive a tailored CRS with their After Visit Summary (AVS). Providers can run a quick report within the patient's EHR to see which SDOH the patient screened positive for (Figure 4).
Figure 2.
HRSN Column to Identify Medicare or Medicaid Patients Requiring Screening
Figure 3.
HRSN Confirmation Warning Message and Best Practice Advisory (BPA)
Figure 4.
HRSN Screen Report Displaying Positive Social Needs
Emergency Department SDOH Screening
In the emergency department (ED), we identified research assistants and unit clerks as the most appropriate roles to conduct SDOH screening based on pre-implementation meetings with leadership. We modified Epic ASAP's ED Track Board to display an “Offer HRSN” column to staff that indicates by a “Yes” or “No” if the patient meets AHC eligibility criteria (Figure 2). Primarily, select research assistants and unit clerks are assigned areas of the ED to screen. Using the ED Track Board as a guide to view patients' requiring screening, if the “Offer HRSN” indicates a “Yes” the staff followed up with eligible patients in the ED to offer the screening. The staff use EHR carts (“workstations on wheels”) to administer the HRSNs screening tool by reading the questions aloud to the patient or proxy. Staff document the patient's SDOH screening results in the Epic flowsheet by clicking the “Yes” button found on the ED Track Board of each “Area” tab (Figure 2). We added the HRSNs Screening report to the ED Track Board report pane to allow clinicians to see which SDOH the patient screened positive for. If the patient screened positive for a SDOH, the discharge nurse will give the patient a tailored CRS with their AVS.
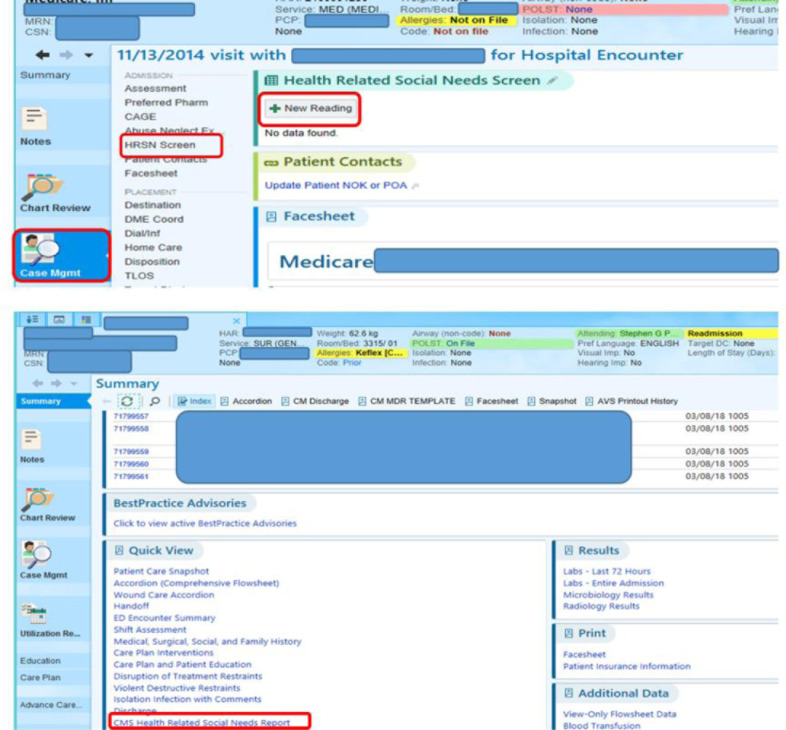
Inpatient SDOH Screening
In the inpatient setting, we identified case managers and social workers as the most appropriate roles to conduct SDOH screening based on pre-implementation meetings with leadership. We modified EpicCare Inpatient's Clinical Case Management platform to display a BPA (Figure 3) upon staff opening the medical record of an eligible patient. This clinical decision support tool provides the staff with an alert to screen eligible patients during the hospital stay. Upon receiving the BPA, the case manager or social worker will navigate to the “Case Mgmt” activity, select the “HRSN Screen” section, then select “New Reading” to open the Epic flowsheet and document the patient's SDOH screening results (Figure 5). Clinicians can run a quick report in the patient's EHR to see identified SDOH. Patients screening positive for a SDOH domain will receive a tailored CRS with their discharge instructions.
Figure 5.
Inpatient Case Management HRSN Screen Section to Document Patient Screening Responses
Other EHR Environments
We also maximized the use of MyChart patient portal to allow patients to complete the SDOH screening prior to their appointment. Within the Medicare and Medicaid beneficiaries' MyChart portal, the SDOH screening is available in the Questionnaires section under the Health tab. Additionally, the SDOH screening is listed as a To Do task to remind the patient to complete the questionnaire. Patients also receive an inbox message within their MyChart portal that alerts them to complete the SDOH screening questions. After completing the SDOH screening questions in MyChart, the patient's responses are filed within their EHR until they present to the clinic for their appointment. If the patient screens positive for a SDOH, the patient will receive a tailored CRS with their AVS.
We added the patient's SDOH screening results to Epic's SnapShot tool so healthcare providers can see a quick overview of the identified health-related social needs. Incorporating the patient's social needs data into the SnapShot allows clinicians to have a comprehensive, yet quick overview of this information in light of other important data for population healthcare planning, such as a problem list, medications, history, and follow-up on unmet social needs.
Results
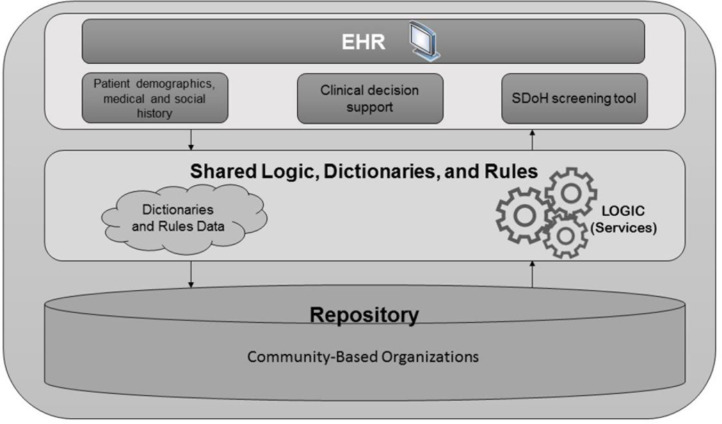
Figure 6 provides a schematic of the HUMC Epic and CRNM SaaS platform integration workflow. Shared dictionaries and rules between Epic EHR and the CRNM SaaS platform make it possible for the two software to extract, transform, and load Health Level Seven (HL7) SDOH data to create a logic workflow that is triggered whenever a new HL7 message (e.g., patient screening) is added to the queue of Epic EHR. The resulting integration workflow is as follows: 1) systematic screening for SDOH; 2) capture responses in the EHR as flowsheet values; 3) securely transmit screening (i.e., flowsheet) values from the EHR to the CRNM SaaS platform as HL7 messages; 4) CRNM software's algorithm reviews screening values for the patient's demographics (i.e., age, gender, and ZIP code) and positive SDOH responses; 5) CRNM SaaS platform generates tailored CRS from the CBO repository and in real-time returns the tailored CRS (PDF) to the patient's EHR as HL7 messages; and 6) staff prints the tailored CRS from the EHR and gives it to the patient with their discharge summary or AVS.
Figure 6.
Schematic of the HUMC Epic-CRNM SaaS Platform Integration Workflow
All Medicare and Medicaid beneficiaries who screen positive for at least one SDOH receive a tailored CRS upon discharge or checkout. The tailored CRS lists community service providers (CSPs) across community-based organizations in the beneficiary's ZIP code (or nearest ZIP code) that may be able to assist with resolving each one of the SDOHs identified through the screening. The CRS includes the name, contact information (i.e., addresses, phone numbers, website, and email, as applicable), type of SDOH resource (e.g., housing), and hours of operation for each CSP. We also modified Epic's Chart Review tool to store the CRS so healthcare providers can review the CSPs the patient was referred to. Upon the patient being discharged from the ED, inpatient, or ambulatory location, Community health workers conduct outreach to randomized and navigation eligible high-risk patients in order to coordinate and connect them to community resources through community service navigation.
The CRNM SaaS platform has three primary roles: 1) storage of the community resource inventory, 2) real-time generation of the CRS, and 3) ability of CHWs to document and track whether patients have accessed a CSP via the referral platform and, if not, identify additional CSPs that may help with resolving social needs. The community resource inventory includes the information for each CSP in the defined geographical region that provides services and supports that might be able to assist with resolving at least one of the five core social risk domains.
This custom-built SDOH EHR solution has been in operational use for over three years by clinical and administrative staff to screen 111,486 Medicare and Medicaid beneficiaries, identify 7,878 SDOH, and refer 6,103 beneficiaries to community services to address their identified needs.
Discussion
Key elements of our project have been 1) to begin with stakeholder engagement (informatics professionals, health information management professionals, organizational and departmental leadership, clinicians, front-line staff) to understand preferences about social needs screening and referral workflows at the point of care and to gain buy-in; 2) to design the EHR using clinical decision support features to enhance decision-making in the SDOH clinical workflows; and 3) to automate the multiple steps of the SDOH screening and referral workflow to optimize staff engagement and buy-in at all of the clinical delivery sites.
Organizations that collect and store SDOH patient data within their EHR are well suited for population health management because they have the data to evaluate and deploy value-based models that take actionable steps to achieve health equity and reduce health disparities in healthcare. Collating SDOH data with clinical data helps organizations to know where and how to invest resources to keep their populations healthier. By building SDOH data into the patient data capture process, clinicians have a complete picture of their patients' needs. This allows clinicians to co-create a person-centered care plan that tracks individuals along the care continuum, thus improving the likelihood of care plan success.
In addition, collecting and storing SDOH data within the EHR has the advantage of access to an engaged user base with whom the screening and referral design elements can be co-created with. Including care team members in screening and referral workflow design can optimize usability and improve the end user experience. Through this process, clinicians, developers, and other key stakeholders communicate openly and share specific usability and safety challenges associated with EHR technology.
Depending solely on clinical data to advance value-based care often provides a disparate picture of the patient and the determinants of their health. Population health transformation requires healthcare organizations to reach across the care continuum to share and integrate SDOH data and applications to drive awareness into innovative care models that prevents disease, enhances treatment and management care, and improves patient outcomes. Enterprise integration encourages key stakeholders involved in the design and implementation process to consider not just clinical data, but how SDOH data can be collected throughout the healthcare enterprise, including at different points of care within and outside the organization, and all the different data standards that facilitate or impede this process. While national data standards for capturing and integrating SDOH data across care continuums are in early stages, an EHR that offers full integration support coupled with a CRNM SaaS platform using HL7's Fast Healthcare Interoperability Resources (FHIR) standards, ensures the standardization, reuse, and integration of the SDOH data across applications throughout the healthcare enterprise is extremely important to advancing value-based care.
Conclusion
Addressing SDOH is an essential component of person-centered medical care. EHR SDOH screening and referral design and integration is an interdisciplinary process that benefits from various technical, administrative, and clinical experts that provide subject matter knowledge in the planning, analysis, design, development, implementation, integration and testing, and operations and maintenance phases of the project. Including the SDOH screening questions in multiple Epic EHR environments ensures comprehensive screening and referral across multiple care settings. Incorporating electronic clinical notifications such as BPAs into the EHR to alert providers to screen and refer for SDOH has multiple advantages, such as ensuring every patient every time is screened for these vital determinants of health. Additionally, we designed the EHR so that the personalized CRS automatically prints with the patient's AVS or discharge summary at the point of care. This helps overcome literacy barriers to care by ensuring the patient understands how to use the information for the social services resources listed.
Continued monitoring and quality improvement efforts are needed to ensure the EHR design supports the SDOH screening and referral workflow of clinical staff members and providers. For example, the project staff conducted repeated Plan-Do-Study-Act (PDSA) method cycles in a number of provider practices and clinical departments to optimize usability of the SDOH customized build EHR, screening and referral workflows, and training procedures.
Institutional support was crucial for garnering together resources and momentum for SDOH screening and referral. It has become increasingly clear that optimizing and using EHRs as an effective tool to screen and refer for SDOH minimizes burden on screening staff and allows access to large data that are needed to map and improve effective population health.
Support
This project is supported by the Centers for Medicare & Medicaid Services (CMS) of the US Department of Health and Human Services (HHS) as part of a financial assistance award totaling $2,500,000 with 100 percent funded by CMS and HHS. The contents are those of the author(s) and do not necessarily represent the official views of, nor an endorsement by CMS or HHS, or the US government.
Conflict of Interest Statement
None declared.
Author Biographies
Christopher K. Rogers was the project/program manager for the Accountable Health Communities Program at Hackensack University Medical Center.
Manisha Parulekar currently serves as the director in the Division of Geriatrics and the program director for the Accountable Health Communities Program at Hackensack University Medical Center.
Fareeha Malik was the Master of Public Health graduate intern for the Accountable Health Communities Program at Hackensack University Medical Center.
Ciara A. Torres currently serves as the program manager for the Accountable Health Communities Program at Hackensack University Medical Center.
Acknowledgments
Hackensack University Medical Center clinical and administrative teams involved in planning and implementing the AHC program.
Hackensack University Medical Center EHR applications team.
Notes
- 1.Alley DE, Asomugha CN, Conway PH, Sanghavi DM. “Accountable Health Communities–Addressing Social Needs through Medicare and Medicaid.”. N Engl J Med. 2016;374((1)):p. 8–11. doi: 10.1056/NEJMp1512532. [DOI] [PubMed] [Google Scholar]
- 2.Park H, Roubal AM, Jovaag A, Gennuso KP, Catlin BB. “Relative contributions of a set of health factors to selected health outcomes.”. Am J Prev Med. 2015;49((6)):p. 961–9. doi: 10.1016/j.amepre.2015.07.016. [DOI] [PubMed] [Google Scholar]
- 3.Alley DE, et al. 2016 [Google Scholar]
- 4.Centers for Medicare & Medicaid Services The Accountable Health Communities Health-Related Social Needs Screening Tool. 2018 Available at https://innovation.cms.gov/files/worksheets/ahcm-screeningtool.pdf. [Google Scholar]
- 5.Gottlieb LM, Tirozzi KJ, Manchanda R, et al. “Moving electronic medical records upstream incorporating social determinants of health.”. Am J Prev Med. 2015;48:p. 215–218. doi: 10.1016/j.amepre.2014.07.009. [DOI] [PubMed] [Google Scholar]
- 6.Adler NE, Stead WW. “Patients in context—EHR capture of social and behavioral determinants of health.”. N Engl J Med. 2015;372((8)):p. 698–701. doi: 10.1056/NEJMp1413945. [DOI] [PubMed] [Google Scholar]
- 7.Chen M, Tan X, Padman R. “Social determinants of health in electronic health records and their impact on analysis and risk prediction: A systematic review.”. J Am Med Inform Assoc. 2020;27((11)):p. 1764–1773. doi: 10.1093/jamia/ocaa143. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Institute of Medicine . Washington, DC: The National Academies Press; 2014. Capturing Social and Behavioral Domains and Measures in Electronic Health Records: Phase 2. Available at . [DOI] [PubMed] [Google Scholar]
- 9.Cartier Y, Fichtenberg C, Gottlieb L. Community Resource Referral Platforms: A Guide for Health Care Organizations. San Francisco, CA: SIREN. 2019 Available at https://sirenetwork.ucsf.edu/tools-resources/resources/community-resource-referral-platforms-guide-health-care-organizations. [Google Scholar]
- 10.Centers for Medicare & Medicaid Services (CMS) Accountable Health Communities (AHC) Model Assistance and Alignment Tracks Participant Selection. 2017 Available ate https://www.cms.gov/newsroom/fact-sheets/accountable-health-communities-ahc-model-assistance-and-alignment-tracks-participant-selection. [Google Scholar]