Abstract
Acute and chronic wound infection has become a major worldwide healthcare burden leading to significantly high morbidity and mortality. The underlying mechanism of infections has been widely investigated by scientist, while standard wound management is routinely been used in general practice. However, strategies for the diagnosis and treatment of wound infections remain a great challenge due to the occurrence of biofilm colonization, delayed healing and drug resistance. In the present review, we summarize the common microorganisms found in acute and chronic wound infections and discuss the challenges from the aspects of clinical diagnosis, non-surgical methods and surgical methods. Moreover, we highlight emerging innovations in the development of antimicrobial peptides, phages, controlled drug delivery, wound dressing materials and herbal medicine, and find that sensitive diagnostics, combined treatment and skin microbiome regulation could be future directions in the treatment of wound infection.
Keywords: Wound infections, Skin microbiome, Diagnosis, Antimicrobial wound dressings, Herbal medicine, Hydrogels, Antimicrobial peptides, Phages, Drug delivery
Highlights.
Both acute and chronic wound infection and associated microorganisms are reviewed.
Current advances and challenges in treating wound infections, particularly diagnosis, non-surgical and surgical approaches are described.
Innovations in wound infection control, including antimicrobial peptides, wound dressing materials and herbal medicine are discussed.
Background
Acute and chronic wounds affect >6 million people every year in the USA States with a cost of $25 billion (USD) [1]. Uncomplicated, acute wounds can heal within a predictable period depending on the nature of the injury, with clinical signs of erythema, swelling, warmth and purulent discharges for infection. Chronic wounds, for instance diabetic ulcers, display delayed wound healing due to confounding factors such as aging, stage of diabetic disease, medication (or treatment) compliance, associated peripheral neuropathy, immunocompromised status and/or arterial and venous insufficiency. Despite significant advances in wound management over the last decades, scientists and clinicians continue to develop novel therapeutic approaches aimed at preventing and controlling infections for both acute and chronic wounds [2]. Intravenous injection or oral administration of antibiotics are widely used in general practice for acute wounds [3], while in treating chronic wound infections, antimicrobial creams, ointments or gels are accepted to eliminate the deep infections caused by the migration of bacteria or fungi to the subcutaneous tissues [4]. However, biofilm colonization, delayed healing and drug resistance remain as challenges in the management of wound infections. In this review, we outline acute and chronic wound infections with associated micro-organisms and discuss the challenges, innovations and future directions in treating wound infections, with focuses on diagnostics, therapeutic approaches and the regulation of the skin microbiome.
Review
Acute wound infection
Acute wounds normally heal within 14 days, depending on the type, severity and size of the injury as well as the patient’s age, co-morbidities and post-injury care. Due to the damage of the skin barrier and local microbial colonization (moisture, temperature and nutrient conditions), infections occur in ~5.6–26% of wounds [5]. Burn, surgical site and traumatic wounds are the top three wounds that are prone to infection [6].
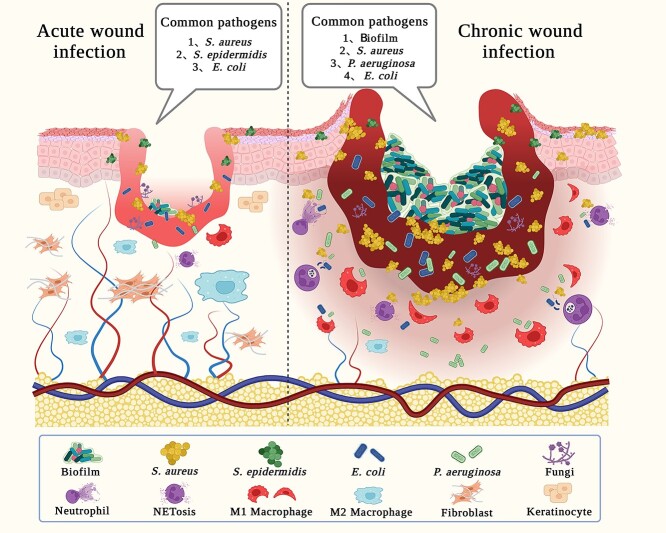
Burn injury caused by heat, flame, chemicals, electricity or radiation [7] is a major public health problem with high morbidity and mortality worldwide and ~180,000 deaths per year [8]. Moreover, burn wound infections are responsible for >75% of burn mortality worldwide [9,10]. Various pathogens have been identified in the acute phase post burn injury [11], including Staphylococcus aureus (S. aureus), Escherichia coli (E. coli), Pseudomonas aeruginosa (P. aeruginosa), coagulase-negative Staphylococci [10] and many other aerobic and anaerobic microorganisms (Figure 1 and Table 1). Fetal methicillin-resistant S. aureus (MRSA) and vancomycin-resistant enterococci in burn injuries are found to be increasing every year, particularly in patients with full-thickness injury [11,12].
Figure 1.
Differences between acute and chronic wound infection together with common pathogens. S. aureus Staphylococcus aureus, S. epidermidis Staphylococcus epidermidis, E. coli Escherichia coli, P. aeruginosa Psuedomonas aeruginosa
Table 1.
Common pathogens causing acute wound infection
| Group | Species |
|---|---|
| Gram negative | Psuedomonas aeruginosa, Actinetobacter baumanni, Enterobacteriaceae, Escherichia coli, Klebsiella pneumoniae, Serratia marcescens, Enterobacter spp., Proteus spp., Bacteroides spp. |
| Gram positive | Staphylococcus aureus, Streptococcus, Enterococcus, Micrococcus, Corynebacterium, Streptococcus pyogens, Corynebacterium diphtheria, Coagulase-negative staphylococci |
| Fungi | Candida spp., Non-albicans Candida, Aspergillus, Blastomycosis, Mucor circinelloides, Candida spp., Aspergillus spp., Fusarium spp., Alternaria spp., Rhizopus spp. Mucor spp. |
| Viruses | Herpes simplex, Varicella-zoster |
| Drug-resistant strains | Methicillin-resistant Staphylococcus aureus, vancomycin-resistant enterococci, extended-spectrum beta-lactamases, MDR Psuedomonas aeruginosa |
Acute surgical site wound infections (SSWIs) occur in many surgical wounds ranging from elective to traumatic non-elective procedures. During surgery, microorganisms on sutures or prostheses can induce both superficial and deep infection [13,14]. Studies have shown that acute SSWIs increase morbidity and mortality, while patients with acute SSWIs are 2–11 times more likely to succumb to complications than uninfected patients [14–16]. The most common pathogenic microorganisms for acute SSWIs are Staphylococcus epidermidis and S. aureus. As cutaneous commensal bacteria, Staphylococcus can form biofilms on the epidermis, which is the main virulence factor, and S. aureus is often found in medical device related infections [17]. Other microorganisms have also been isolated from acute SSWIs, including E. coli, Clostridium difficile, coagulase-negative Staphylococci [11], Legionella pneumophila, Mycobacterium chelonae, Clostridium perfringens, Mycobacterium fortuitum, P. aeruginosa and Acinetobacter baumanii [18].
Traumatic wounds include abrasions or laceration wounds with extensive tissue, bone and internal organ damage [19]. The common pathogens of traumatic wound infections are Gram-positive S. aureus and Gram-negative P. aeruginosa [20]. Infections in skin laceration wounds were noted mostly in elderly patients with chronic use of corticosteroids [20], while 2–10% of infections are reported to be of plantar puncture wounds, mainly caused by Staphylococcus or Streptococcus [21]. High mortality and septic complications, including abdominal infections, necrotizing fasciitis and diffuse septic peritonitis, can often be attributed to sepsis induced by wound infection [22]. Invasive fungal infection is also known as a serious complication for traumatic wounds, usually caused by agricultural accidents, war bombings and natural disasters, resulting in deep tissue wounds [23]. As fungi can survive in both acidic and iron-rich environments, they can stimulate severe pelvic injuries or limb amputations [24,25]. Although fungal infections are less reported compared to bacterial infections they lead to high amputation and mortality rates of 31 and 38%, respectively [25].
Chronic wound infection
In contrast to acute wounds, chronic wounds are complicated by having a delayed wound healing capacity. Chronic wounds occur more often in elderly people, patients with diabetes, vascular disease, obesity, malnutrition and chronic mechanical stress, or a combination of these factors [26]. Most chronic wounds are colonized by polymicrobial communities that can form biofilms, resulting in excessive inflammation and infection susceptibility which significantly delay wound repair [27] (Figure 1). Generally, Gram-negative bacteria are common colonizing organisms in chronic wounds, accounting for 61% of all microbial isolates. S. aureus is the most commonly found pathogen in chronic infections, followed by P. aeruginosa. Other pathogenic microorganisms are Proteus mirabilis, E. coli, A. baumanni and Klebsiella pneumoniae [28]. Anaerobic bacteria in chronic wounds include Prevotella, Peptonipihlus, Peptostreptococc, and Anaerococcus [29].
Biofilm is one of the major challenges in the treatment of chronic wound infections. It occurs for >60% of chronic wound infections and only 6% of acute wound infections [30,31]. Biofilms are complex microbial communities of bacteria and fungi that exist as unicellular, planktonic or multicellular communities and aggregates, surrounded by a polymeric matrix of polysaccharides, lipids, proteins and nucleic acids. The matrix facilitates signaling among micro-organisms by producing population-sensing molecules. This cross-communication can further aid microbial proliferation, optimize nutrient uptake and regulate virulence, leading to a persistent impairment of wound healing [29,30,32]. Bacterial endotoxin- and exotoxin-associated wound infections are found to induce non-specific and specific immune responses [33], while excessive inflammation can further trigger adverse outcomes, where inflammatory cells recruited at the wound site produce large amounts of proteases that degrade the extracellular matrix and delay wound healing [34].
Diabetic foot ulcer is a type of wound associated with chronic infection, and is a complication of diabetes mellitus, particularly in advanced disease including diabetic neuropathy [35]. S. aureus is known to be the most common infecting species (accounting for >50% of all wounds) [36,37], with other causative organisms including coagulase-negative Staphylococcus, Streptococcus streptococci spp., MRSA, Enterococcus spp., Corynebacterium spp., Enterobacteriaceae and P. aeruginosa [38]. Up to 90% of the bacteria found in diabetic ulcer wounds are pathogenic or exclusively anaerobic, including Gram-positive cocci, Prevotella spp., Poryphyromonas spp. and Bacteroids fragilis [38], whilst >75% of diabetic foot wounds are found to be colonized with fungi [39].
Pressure ulcers are defined as ‘a localized injury to the skin and underlying tissue usually over a bony prominence in combination with shear’ [40], particularly when wounds are exposed to a fecal environment. A study by Norman et al., showed that among 145 patients with pressure ulcers, S. aureus and Gram-negative bacilli were detectable in 112 wounds [40]. Lower extremity venous ulcers are normally caused by venous hypertension [41] in aging and obese people with severe leg trauma or vascular surgery [42]. Wound sites having high moisture are ideal for microbial growth, therefore, all lower extremity venous ulcers are colonized by microorganisms, resulting in serious infections. The most common microorganisms at the ulcer site are S. aureus and P. aeruginosa, with Streptococcus haemolyticus and MRSA also being identified [42].
Current advances and challenges in treating wound infections
Clinical diagnosis
Clinical diagnosis is the first step to prevent further complications (Figure 2). However, classification of wound infections remains a challenge in practice. In general, almost all wounds contain microorganisms, but not all wounds develop infections. A clinical report by Leaper et al. showed that ~50% of patients who have a local wound infection do not show any sign of systemic infection [43], making diagnosis difficult [44]. Currently, there is a lack of objective clinical diagnostic criteria for wound infection, and clinicians usually make subjective judgments based on experience. Diagnostic criteria (e.g. foul odor, friable or discolored granular tissue) are highly subjective [44,45], resulting in high rates of misdiagnosis or overtreatment with antibiotics. As a result, patients can be at risk of developing multi-resistance bacterial strains [46].
Figure 2.
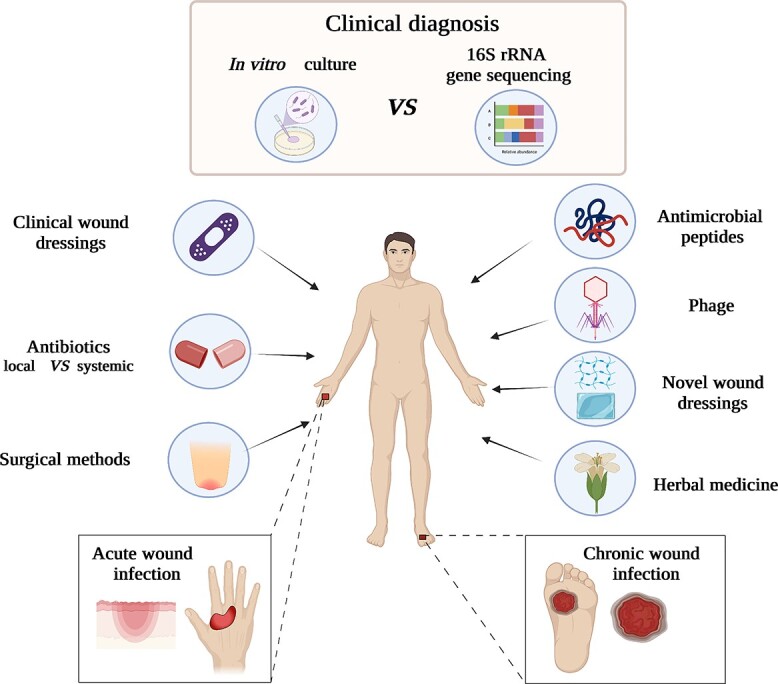
Therapeutical approaches and innovations in managing acute and chronic wound infection
In vitro culture has been used as the golden standard for clinical identification of microorganisms since the 19th century [26]. However, it is only applicable for 1% of known microorganisms that can be cultured in vitro under laboratory conditions [47]. In contrast, most microorganisms, such as fungi and anaerobes, are yet to be identified using in vitro culture [26]. It takes ~24–48 h to obtain results by this method. Alternatively, 16S rRNA gene sequencing is a state-of-the art technology that is widely used in basic science for identifying bacteria in various types of wounds. The limitations of this technique are that it cannot distinguish alive or dead microorganism, it can only be used for the identification of bacteria but not fungi or viruses, while the cost is high and it is time-consuming [48,49].
Clinical wound dressing materials
Wound dressings are used to temporarily cover wounds and to prevent or manage wound infections. However, wound dressing may become a favorable place for microorganisms and biofilm formation, resulting in increased microbial load and delayed wound healing [18]. The ideal wound dressing should be flexible and immune-compatible, forming a physical defensive barrier but allowing oxygen exchange [50]. Many novel clinical wound dressings have been developed and are utilized, including sponges, hydrofibers, hydrocolloids, fucoidan, collagen, hydrogels and films. Antimicrobial wound dressings can be categorized as antiseptic, ionic/nanocrystalline silver and antibiotic. An antiseptic wound dressing is a treatment that releases antiseptics to eliminate microorganisms within the tolerance limits of living tissue [51]. Products can contain either silver (e.g. Aquacel AG), nano-crystalline silver (e.g. ACTICOAT) or cadexomer iodine (e.g. Iodosorb™) as antimicrobials. Applications of silver compounds on acute wounds was a major milestone in topical therapy, which remarkably reduced the incidence of acute wound-induced sepsis and death. Bactigras™ are cotton roving fabrics containing 0.5% w/w chlorhexidine acetate for preventing wound infection by Gram-positive and Gram-negative bacteria, but not by spores, fungi and viruses [52]. Iandine is a low-adhesive knitted viscose fabric impregnated with a polyethylene glycol matrix containing 10% povidone iodine, which is the broadest spectrum antiseptic in human use, while Iodosorb™ is a unique antiseptic dressing composite of cadexomer microbeads with 0.9% elemental iodine. Iodosorb™ is effective against biofilm formation due to its high release rate of antimicrobials [53]. Ionic or nanocrystalline silver-containing dressings are also widely accepted in the control and treatment of wound infections because of their broad-spectrum antimicrobial activity [33].
Antibiotics
The first antibiotics were discovered in the late 19th century, and over the past hundred years, various antibiotics such as sulfonamides, penicillin, streptomycin, tetracycline and vancomycin have been clinically used for infection control. At present, the extensive use and overuse (long-term or for uninfected wounds) of topical or systemic antibiotics has led to a global antibiotic resistance crisis [48]. It is estimated that ~70% of bacteria causing wound infections are now resistant to one antibiotic [33]. The spread of resistant strains has become a pandemic threat to human health with >700,000 deaths per year, and the number of deaths is expected to rise to 10 million annually by 2050 [54]. The International Committee of the Red Cross recommends that the best type of ‘antibiotic’ is the appropriate surgical treatment [55], and the Infectious Diseases Society of America recommends that antibiotics should be avoided for diabetic foot ulcers if there are no signs of infection [56]. Antiseptics with antimicrobial effects are being utilized more frequently to overcome drug resistance of antibiotics. Octenidine hydrochloride , polyhexamethylene biguanide, povidone-iodine and sodium hypochlorite are currently utilized in clinics as topical treatments for wound infections because of their high bactericidal and anti-biofilm forming activity [30].
Surgical methods
The standard surgical approach to treating wound infection is debridement, and if the infection is deep into muscle or the adipose layer, amputation is required to prevent systemic infection or sepsis. Debridement is a common surgical approach for the treatment of acute wounds, such as burn injury. It can help to reduce bacterial diversity and promote wound epithelialization, while it can also reduce the blood load on the wound via removing necrotic infected tissue, apoptotic cells and biofilms from the wound [30,57,58]. High microbial loads can lead to wound deterioration, osteomyelitis and ultimately amputation [35]. Patients with severe limb ischemia usually require below-knee amputation, and postoperative wound closure is effective in reducing reinfection [59]. First pioneered in 1920, radiographic amputation was utilized in salvage surgery for proximal phalangeal dysfunction. It can also control wound infection, vascular insufficiency and congenital anomalies of the hand [60]. However, reinfection after amputation remains a risk as patients with diabetic foot ulcers have a fairly high risk (40%) of mortality after amputation [61].
Animal models
Animal models aimed at studying the complex biochemical processes in the treatment of wound infections and evaluating the biosafety and efficacy of medical treatments have been well developed. Currently, animal models of wound infection vary between animal species, different modeling drugs and equipment, microbial species and inoculation amount, size and depth of the wound. For studying acute wound infection, large or small animals with burn infection, surgical site infection, skin abrasion infection or laceration wound infection are commonly utilized (Table 2) [20], while animal models of chronic wound infection are described for diabetic wound infection only (Table 3) [62,63]. Additionally, the model pathogenic microorganisms are S. aureus and P. aeruginosa [20]. Rodents such as mice have been found to be the most popular model due to the similarity of their immune systems to that of humans and the ability to create gene knockout varieties. However, FDA guidance recommends that all new drugs need to be assessed on two animal models involving a non-rodent large animal [62]. In such case, porcine models are commonly used to investigate new approaches for the treatment of wound infection. The skin structure of the pig is similar to human skin, and both pig and human wounds heal via re-epithelialization not by contractile healing [64]. However, limitations in using different animal models still exist as none of the models can completely mimic wound infection in humans [65]. Moreover, current animal studies mainly focus on local wounds, but the systemic conditions, including systemic inflammatory response and changes in metabolism, should also be considered [63].
Table 2.
Representative animal models of acute wound infection
| Infection model | Animal species | Modeling methods | Microorganisms |
|---|---|---|---|
| Burn infections | Rodents and pig | Heat source used: boiling water, burning ethanol bath, gas flame, pre-heated double brass blocks, pre-heated single metal plate/bar, etc. | Psuedomonas aeruginosa, Staphylococcus aureus, Klebsiella pneumoniae, Acinetobacter baumannii and Candida albicans. |
| Surgical site infections | Mouse, rat and pig | Incisional wounds with foreign bodies, subcutaneous injection of foreign bodies and microorganisms into pocket wounds with or without foreign bodies. | Staphylococcus aureus, Psuedomonas aeruginosa and methicillin-resistant Staphylococcus aureus. |
| Skin abrasion wound infections | Mouse, rat and rabbit | Needle scratch model, blade scrape model, tap striping model, sand paper model and dermatome model. | Staphylococcus aureus, Psuedomonas aeruginosa and Candida albicans. |
| Excisional wound infections | Mouse, rat, rabbit and pig | Removing the full-thickness skin. | Staphylococcus aureus, Psuedomonas aeruginosa, Escherichia coli and methicillin-resistant Staphylococcus aureus. |
| Lacerated wound infections | Guinea pig and rat | Non-crushed lacerated wounds and crushed lacerated wounds. | Staphylococcus aureus, Streptococcus pyogenes, Psuedomonas aeruginosa, Klebsiella pneumoniae and Proteus mirabilis. |
Table 3.
Representative animal model of diabetic wound infection
| Animal species | Induction of diabetes mellitus in animals | Induction of wound in diabetic animals | Microorganism |
|---|---|---|---|
| Mouse, rat, rabbit, dog, guinea pig, pig | 1. Chemically-induced diabetes mellitus: streptozotocin, alloxan, dithizone, gold thioglucose, monosodium glutamate. 2. Genetic manipulation: db/db mouse, KK-Ay mouse, ob/ob mice, Goto–Kakizaki rat, Otsuka Long Evans Tokushima fatty rat, Spontaneous diabetic Torii rat, Zucker diabetic fatty rat, Watanabe heritable hyperlipidemic rabbit and Postprandial hyper- triglyceridemia rabbit. 3. Virus-induced diabetes mellitus: D-variant encephalomyocarditis, coxsackie B4 virus. 4. Hormone-induced diabetes mellitus: growth hormone, corticosteroid. |
Excision wound model, incision wound model, burn wound model, ear wound model, dead space wound model, tape stripping wound model, pressure ulcer model, parabiosis wound model, denervated wound model, skinfold chamber model, xenograft wound model. | Psuedomonas aeruginosa and Staphylococcus aureus. |
Innovations in wound infection control
Antimicrobial peptides (AMPS)
AMPs are an emerging class of drugs for the treatment of traumatic infections [57,66] and have tremendous research value in the treatment of severe chronic infections (Figure 2). To date, >2000 natural or synthetic AMPs have been developed with broad-spectrum antimicrobial properties that are less likely to develop drug resistance. AMPs that can be extracted from insects, animals or plants, including tylotoin, plant defensins and LL-37, have been investigated for their novel antimicrobial properties [67]. Peptides induce cell death by interacting electrostatically with microbial cell membranes, inducing porous membrane formation and inhibiting cell wall formation and protein synthesis, resulting in an inhibition of micro-organism proliferation [68]. Current investigations of AMPs are focussed on increasing their activity. Based on studying human thrombocidin-1-derived peptide L3 (a protein isolated from human blood platelets that has the ability to destroy microorganism) [69], a new AMPs named TC-19 was synthesized, with promising results against S. aureus and A. baumannii. Compared to rifampicin and ciprofloxacin, TC-19 exhibited minimal drug resistance [70]. In a full-thickness wound model, TC-19-containing hypromellose ointment was capable of suppressing S. aureus infection significantly [69]. In a study of a novel synthetic cationic peptide, AMC-19, effective antimicrobial results were reported in a MRSA-induced wound infection [71]. Results also showed high stability of AMC-19 with a 7-fold reduced bacterial load in 3 days, demonstrating its potential against MRSA via topical administration [72]. Because of their low activity, nonspecific cytotoxicity and susceptibility to proteolysis, ongoing studies aim to further develop a second generation of AMPs. In the second generation, a modified peptide, DGL13K, proved to have enhanced antimicrobial activity [73]. Topical administration of DGL13K ointment on a burn infection model showed a significantly decreased bacterial load post treatment [73]. Unfortunately, no topical AMP drugs are commercially available [57] and the clinical effects, long-term safety and side effects in patients are yet to be studied.
In order to avoid inactivation of AMPs caused by their degradation by various proteases secreted by human pathogens, such as P. aeruginosa elastase, P. mirabilis proteinase, Enterococcus faecalis gelatinase and Streptococcus pyogenes cysteine proteinase, researchers improved their antibacterial activity by enhancing their stability to proteases and their stability under high salt conditions. Methods include using terminal modifications such as N-terminal acetylation and/or C-terminal amidation, replacing amino acids in AMPs with non-encoded α-amino acid derivatives which can reduce the susceptibility of AMPs to microbial proteases, particularly the complete substitution of D-amino acids, and AMP multimerization. Moreover, the antibacterial ability can be improved by varying the hydrophobicity and amphiphilic affinity of AMPs or via stabilizing the structure through dimerization or cyclization of disulfide bonds. At present, novel therapeutics also include utilizing carriers and scaffolds such as liposomes and polymers to achieve controlled delivery of AMPS that can further increase the antimicrobial activity and stability and reduce toxicity and protease degradation [74–76].
Controlled drug delivery systems
Drug delivery systems are widely used to deliver antibiotics, growth factors, genes and cells for preventing or curing wound infections. Microcarriers are designed and developed to incorporate unstable antibiotics for controlled drug release with significantly reduced risk of bacterial infection. However, due to the size of microcarriers, in the range of 10–50 μm, they are not suitable for intracellular delivery. Nanoparticles, such as polymer nanocarriers, lipid nanoparticles, and metal and metal oxide nanoparticles, can be precisely tailored to have specific drug properties or to target specific cell types. For instance, cationic polymers are reported as carriers for releasing anionic drugs [77]. Lipid-based nanoparticles normally exhibit sustained drug release based on smaller particle size and lipid composition, ensuring better interaction on the wound site with a prolonged release time [78]. Metal and metal oxide nanoparticles, such as silver, copper oxide, zinc oxide and titanium dioxide nanoparticles, have also been used as alternatives for the treatment of drug-resistant bacterial infections due to their high antibacterial activity. Because of the high surface area of metal nanoparticles, after binding with antibacterial agent, the area of the antimicrobial agent contact with bacteria is increased resulting in the destruction of bacterial membrane permeability and respiratory function [79]. The minimum inhibitory concentration value of gold nanoparticles immobilized with antimicrobial peptide surfactin is 80 times lower compared to that of free surfactin [80], and these nanoparticles were found to promote wound healing in a rat model of MRSA-infected wounds. Additionally, metal oxides (vanadium pentoxide, iron oxide and graphene) can be utilized as artificial enzyme catalysts to enhance the efficiency of H2O2 conversion to hydroxyl radicals (•OH), improving the antibacterial activity against E. coli and Vitis vinifera [81]. Innovative approaches such as ex vivo loading of neutrophils with antibacterial agents and use of cells as delivery vehicles have been reported previously [82].
Other advances and innovations in treating wound infection
Phages are natural antibacterial agents that are highly abundant in the environment. Phages are capable of regulating bacterial populations via inducing bacterial lysis and disrupting bacterial metabolism, leading to self-destruction (Figure 2) [83]. Lytic tailed phages are increasingly subject to investigation for use in a clinical setting [84]. Lytic tailed phages consist of an icosahedral capsid head that contains double-stranded DNA (15–500 Kbp) and a tail covered by surface receptor proteins that interact with surface features of the host bacterium. Phages can adsorb to the host bacterium and inject phage DNA, delivering multiple phage virions which aim to kill the bacteria [85]. They are known to be highly specific to their bacterial host, targeting only one or a couple of different bacterial strains [86]. Cocktail therapy using various phages in a single treatment has been studied in a clinical setting [87]. A phase I clinical trial using phage therapy showed that injection with P. aeruginosa, S. aureus and E. coli phages is safe and has high efficacy in treating chronic venous leg ulcers [88]. Topical administration of Staphylococcal phage S applied once a week was also found to heal small ulcers in 7 weeks and large ulcers in 18 weeks [89,90]. Despite advances in phage therapy research, there is no commercial phage product available yet [91].
Innovations in wound dressing materials
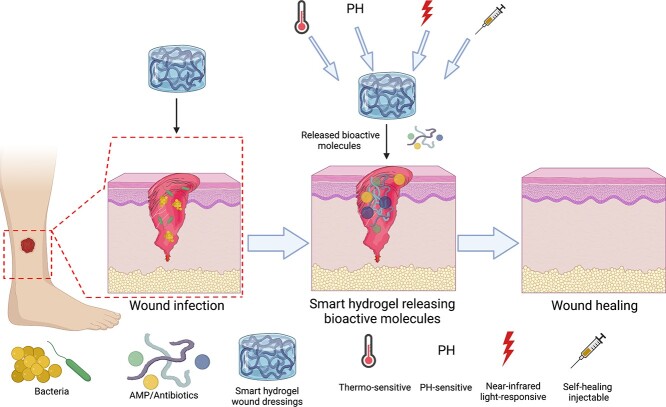
Advances have been made in the structure and properties of wound dressing materials, developing the ability for controlled release of antimicrobial drugs. Advanced wound dressings normally have the dual function of treating infections as well as promoting wound healing [68]. Recent advances in wound dressing materials can be sub-categorized into thermos-sensitive, pH-sensitive and light-responsive (Figure 3). These hydrogels have shifted the focus from traditional wound dressings to smart hydrogel wound dressings [92].
Figure 3.
Smart hydrogel wound dressings in the treatment of wound infection. AMP antimicrobial peptide
Thermo-sensitive hydrogels
Thermo-sensitive hydrogels can change their characteristics in the context of temperature. With gelation time and temperature regulation being adjustable, thermo-responsive hydrogels can transform from the liquid state into a hydrogel, aiming for controlled delivery of active molecules or drugs [93,94]. Thermo-sensitive hydrogels have great clinical potential, particularly in the treatment of deep tissue damage or in the context of irregular wounds [95], allowing drugs to be precisely delivered to a target area. Natural and synthetic polysaccharides and proteins, such as chitosan and collagen [96], have been used in the production of thermos-sensitive hydrogels due to their biocompatibility with the wound environment. A thermo-sensitive hydrogel using chitosan cross-linked with β-glycerol phosphate was investigated in the treatment of a full-thickness surgical wound infected with A. baumanni and the results showed that the number of bacteria significantly decreased over 28 days [97].
pH-sensitive hydrogels
The pH of wounds is different compared to healthy skin. Normally, the pH of healthy skin is 4.5–6.5, while the pH of a wound alkalizes to a value of 7.4. Due to alkaline byproducts of proliferating bacterial colonies, the pH of the wound can reach up to 9 [98–100]. Relying on pH variations between healthy and damaged tissue, a novel pH-sensitive hydrogel composed of red cabbage extract and methacrylate chitosan was successfully fabricated [101]. Results showed that red cabbage extract can be used to indicate the pH of the wound bed as well as accelerate wound healing [101]. This study indicates a new research avenue involving the synthesis of smart materials with ‘diagnosis and curing’ effects. pH-sensitive hydrogels can control the delivery of drugs in treating wound infections. A recent study showed that a nano-chitosan-enriched poly (ɛ-caprolactone) pH-sensitive nanofibrous membrane was used to release curcumin at a controlled rate according to changes in pH [102]. Under both acidic conditions of pH 1.2 and alkaline conditions of pH 7.4, ~48% of curcumin was released on day 15, but under neutral conditions, release of curcumin reached 71% on day 15 [102]. Similarly, a study by Ren et al. investigated a multi-functional hydrogel with a combination of tannic acid and keratin cross-linked with graphene oxide quantum dots. It could swell by >80% in alkaline conditions, which is better for wound healing. The high swelling rate, which allows the drug to be dispersed evenly, thus achieving a sustained-release, long term treatment of wound infection [103]. This multifunctional hydrogel promotes wound healing and is effective against E. coli and S. aureus. These findings suggest that pH-sensitive hydrogel should be further investigated as a new anti-infection wound dressing.
Near-infrared light-responsive hydrogels
Light-responsive hydrogel is a smart hydrogel proportionally responsive to light wavelengths, allowing for controlled drug release. Among light-responsive hydrogels, near-infrared (NIR) light-responsive hydrogels have promising advantages in converting light into heat, utilized to destroy bacteria with no risk of drug resistance. Polydopamine nanoparticles (PDA-NPs) have also been used for their photothermal effects in biomedical applications due to their biocompatibility and biodegradability [68,104,105]. A study by Gao et al. investigated the photothermal effect of a PDA NIR-responsive hydrogel on wound infections in a S. aureus infected mouse wound model, showing encouraging anti-bacterial activity. An enhanced release of ciprofloxacin, a potent antibiotic that has the capability to destroy bacteria, was also instigated via local hyperthermia [106]. However, the uncertain biosafety of light-responsive hydrogel limits its translational research in clinical practice.
Other innovative hydrogels
Self-healing injectable hydrogels are receiving more attention from researchers due to their multifunctionality. Self-healing injectable hydrogels can be prepared by two principles: dynamic covalent chemistry or weak interactions of supramolecular chemistry. Hydrogels prepared based on dynamic covalent chemistry are capable of achieving self-healing after the covalent bond is broken via introducing special covalent bonds, such as hydrazone bonds, imine bonds, disulfide bonds and Diels–Alder reversible covalent bonds. In contrast, hydrogels prepared based on supramolecular chemistry can fuse molecules or molecular chains through weak and reversible intermolecular forces to form cross-linked networks, such as hydrogen bond interactions, metal coordination bonds, ionic interactions and π–π interactions [107]. Self-healing injectable hydrogels with antibacterial activity, antioxidant, responsive, biocompatibility and electrical conductivity are all beneficial for the treatment of wound infection. A report showed that injectable self-healing carbon dot hydrogels with strong antibacterial activity using ε-poly(L-lysine) carbon dots and oxidized dextran can completely kill 107 CFU ml−1 S. aureus in 10 min [108].
Polypeptide hydrogels have optimized mechanical strength and can resist shear stress to the wound and selectively inhibit specific bacteria when incorporated with antibacterials to reduce drug resistance. In the past decade, peptide hydrogels with antibacterial effects have been effective in the treatment of all stages of infection, mainly for the treatment of S. aureus, MRSA, S. epidermidis, E. coli, P. aeruginosa and K. pneumoniae, and future research will be focused on designing species-specific hydrogels [109]. Scientists found that when multi-domain peptide hydrogels have different charges, they can produce various regulatory effects on the host immune response. For instance, the multi-domain peptide hydrogels containing deprotonated carboxylic acids can trigger mild inflammation with minimal macrophage infiltration into the wound area and less secretion of inflammatory cytokines. However, multi-domain peptide hydrogels containing protonated amines normally induce severe inflammation, which diminishes over time, increase acute immune cells and promote host vascularization and tissue remodeling. Additionally, multi-domain peptide hydrogels containing guanidine ions trigger a long-term, highly pro-inflammatory response that is difficult to resolve [110]. These data showed that specific peptide hydrogels can be designed for different purposes in the treatment of wound infection [111].
Innovative herbal medicine
Herbal medicine has been used clinically since 5000 BC. Herbal medicine has minimal side effects and a low risk of drug resistance in treating wound infections (Figure 2). Natural products derived from insects such as periplaneta Americana extract [112], manuka honey [113] and the natural product chitin [114] have been clinically used in the treatment of various types of wound infection. A list of herbal medicines with antibacterial effects including herbal monomer and herbal compound is given in Table 4.
Table 4.
Some herbal medicines for infection wound healing
| Herb | Sources of materials | Agent | Target microbes | Reference |
|---|---|---|---|---|
| Tannins | Extract of Entada phaseoloides (L.) Merr | Ointment | Staphylococcus aureus (S. aureus) | [116] |
| Tannic acid | Chemical reagent | Hydrogels | Escherichia coli (E. coli), S. aureus | [124] |
| Epigallocatechin gallate | Green tea | Cationic nanoliposomes | E. coli, methicillin-resistant S. aureus | [125] |
| Aloe vera | Extract of Aloe vera leaf | Nanofibers | E. coli | [126] |
| Aloe vera | Chemical reagent | Dressing | E. coli, S. aureus | [127] |
| Curcumin and Aloe vera | Chemical reagent | Dressing | E. coli, S. aureus | [128] |
| Trans-cinnamaldehyde and eugenol | Chemical reagent | Solution | Acinetobacter baumannii | [129] |
| Gentiana macrophylla | Extract of Gentiana macrophylla Roots | Solution | E. coli, S. aureus, Staphylococcus epidermidis, Psuedomonas aeruginosa (P. aeruginosa) , Klebsiella pneumoniae, Micrococcus luteus, Enterococcus faecalis, Streptococcus uberis | [130] |
| Allium sativum and Cleome droserifolia | Extracts of bulbs of fresh A. sativum and dried leaves of Cleome droserifolia | Nanofibers | E. coli, S. aureus, methicillin-resistant S. aureus | [131] |
| Rutin and quercetin | Chemical reagent | Nanofibers | E. coli, S. aureus | [132] |
| Extract of Chamaecyparis obtusa plant | Chamaecyparis obtusa | Solution | S. aureus, Streptococcus pyogenes | [133] |
| Salvia officinalis essential oil | The dried leaves of Salvia officinalis | Ointment | S. aureus, P. aeruginosa | [134] |
| Zataria multiflora essential oil | Chemical reagent | Ointment | S. aureus, P. aeruginosa | [135] |
| Rosemary essential oil | Rosmarinus officinalis L | Oil nanostructured lipid carriers (NLCs) in gel | E. coli, S. aureus, S. epidermidis, Listeria monocytogenes, P. aeruginosa | [136] |
| Olive oil and eucalyptus oil | Chemical reagent | NLCs | S. aureus, Staphylococcus pyogenes | [137] |
| Clove oil and sandalwood oil | Chemical reagent | Dressing | E. coli, S. aureus | [120] |
| Moringa oleifera seed polysaccharide | Extract of Moringa oleifera seed | Nanocomposite with silver | E. coli, S. aureus, P. aeruginosa | [122] |
The therapeutic effect of herbal medicine is attributed to certain chemical components. Among them, natural tannins have shown remarkable antibacterial and antioxidant activities [115]. Tannins are polyphenolic compounds that are widely distributed in plants. A study showed that the total tannin content in phaseoloides (L.) Merr extract was found to be ~76.18% [116]. Transmission electron microscopy observations demonstrated that tannins could interfere with S. aureus and destroy the cell membranes, releasing their intracellular cytoplasm. This study showed that tannin promoted wound healing in rats infected with S. aureus. Subsequent to these investigations, tannic acid has been approved by the US FDA and clinically used for skin ulcers and burns due to its favorable antioxidant, hemostatic and antibacterial properties [117].
Essential oils extracted from herbals are also known to have antibacterial effects. Phenolic components are capable of fighting drug-resistant strains through their anti-biofilm activity [118,119]. The antibacterial clove oil contains eugenol, β-caryophyllene, oleic acid, lipids and small amounts of other ingredients [120]. According to Singh et al., eugenol, together with other phenolic compounds, denatures proteins and reacts with bacterial cell membrane phospholipids, affecting permeability, and subsequently causes cell lysis. The antibacterial activity of sandalwood oil is due to the destruction of cell wall and cell plasma membrane, leading to lysis and leakage of intracellular compounds. The combination of clove oil and sandalwood oil enhances antibacterial activity against S. aureus and E. coli by 98% [120]. In addition to its direct bactericidal effect, it can also mediate the secretion of antimicrobial peptides from HBD-3 and LL-37 through the olfactory receptor OR2AT4 to methicillin-sensitive S. aureus, MRSA and purulent [120]. In summary, it is expected that herbal derivatives are a group from which strong candidates for future treatment of chronic wound infections and biofilms will be selected.
One limitation of herbal medicine is its low activity compared to metals or synthetic drugs. At present, research has shifted to combining biomaterials or natural products, including silver (Ag+), gold (Au) and other known antibacterial agents. A study has shown that 87.1% of δ-trienol and 12.9% of γ-trienol extracts obtained from Bixa Orellana L. (Bixaceae) seeds are isomers of vitamin E, which can be used as an immune adjuvant to increase the effectiveness of the antibiotic daptomycin in treating MRSA-infected wounds. This study suggests that the activity of antibiotics can be increased by boosting systemic immune responses against drug-resistant pathogens [121]. Another study demonstrated that polysaccharides isolated from Moringa oleifera seeds can be used to stabilize silver nanoparticles (AgNPs) [122]. Moringa oleifera seed polysaccharides have strong antimicrobial activity against pathogens collected from wounds, with minimal cytotoxicity toward mouse fibroblasts cells, and promote the migration of cells. In recent years, the multi-functionality and plasticity of herbal medicine and their derivatives are being investigated for their use as novel antimicrobial biomaterials. Cellulose microfibers (CM) extracted from Gleditsia triacanthos have been developed into a wound dressing via freeze-drying CM [123]. Controlled release of phenolic compounds from CM was found to be effective against Gram-negative and Gram-positive bacteria. A study showed pro-anthocyanidins and carrageenan conducting chemical reactions under various pH conditions and can be used as a visual system to monitor skin wound infections [100]. This finding also suggests that herbal medicines and their derivatives can serve not only in the treatment of infected wounds but can also have a role in the design of methods of detection and diagnosis.
Future directions
Early diagnosis
An accurate diagnosis of wound infections is crucial to prescribe appropriate wound treatment. However, current approaches are speculative and time-consuming, with varying specificity and sensitivity. Novel diagnostic methods have been developed using the methods of PCR and auto-fluorescent imaging. A PCR kit, DxWound, has been developed to detect anaerobic bacteria, aerobic bacteria and fungi, allowing on-time monitoring for wound infections [138], while a portable autofluorescence imaging devices (e.g. MolecuLight™) has been utilized clinically for diagnosing wound infections [139]. Future directions may involve denaturing gradient-gel electrophoresis, fluorescence in situ hybridization, metabolomics and genomics, techniques currently demonstrating great potential for the development of accurate, rapid, simple, noninvasive, inexpensive and specific diagnosis in wound infections [140,141].
Combined therapies for wound infection
For the treatment of acute or chronic wound infection, monotherapies, such as using antimicrobials, still have a high risk of antimicrobial resistance. Moreover, the spatial distributions of the microorganisms in the wound are complicated, the community behaviours of the bacteria are dynamic and the interactions between the polymicrobial and human immunity are undefined [142]. In response to these, dual therapies are expected to potentiate development of effective therapies for wound infections. For instance, silver-impregnated foam and topical negative pressure have been shown to have a synergistic effect in destroying bacterial biofilms in the wound [143]. Moreover, silver nanoparticles and neomycin have shown strong synergistic efficacy against MDR P. aeruginosa with faster wound contraction in a mouse model [144]. Some combination therapies like ultrasound-assisted debridement and vacuum pump therapy have also been studied to treat deep sternal wound infections in clinical trials [145]. All these pioneering studies demonstrated significant potential in wound treatment and prevention of infections. Other combinations include antimicrobial agents (antibiotics, herbal medicines and synthetics), immune-based antimicrobial molecules (antimicrobial peptides), therapeutic microorganisms (probiotics and bacteriophages) and cell therapy. These combinations are expected to lead to future developments in the treatment of wound infection, while external stimuli such as antimicrobial phototherapy (NIR based therapies), laser therapy, light-emitting diode, high-frequency ultrasound and microcurrent electrical stimulation may also be utilized in wound infection therapy.
Targeting skin microbiome as a new direction
Skin microbiome is vital in maintaining the epithelial barrier function of skin and preventing the invasion of pathogenic microorganisms. Loss of microbial diversity in wound sites is known to stimulate prolonged inflammation. Clinical applications have demonstrated the efficacy of targeting the skin microbiome in the healing of atopic dermatitis by reintroduction of antimicrobial Lactobacillus johnsonii or Vitreoscilla filiformis [29]. Interestingly, Lactobacillus plantarum can inhibit Pseudomonas colonization, reduce collagen accumulation and accelerate wound repair with minimal scarring post burn injury [146,147]. Probiotics have also been observed to significantly reduce the length and depth of chronic wounds, suggesting their great potential in conjugating with antibiotics to treat wound infections. Ongoing studies of the skin microbiome are focusing on isolation and engineering of functional probiotics or microbiota, and studying the interactions between wound microbiome and regulation of host skin microbiome [148]. However, pioneering research findings suggest that pathogenic bacteria could play a beneficial role in wound healing by mediating the inflammatory response and tissue regeneration [149,150]. Therefore, future research may shift from killing or preventing the wound microbiome to controlling skin microbiome-mediated inflammatory responses.
Conclusions
Infection remains a challenge in both acute and chronic wounds, leading to increased morbidity, mortality and healthcare-associated costs. Gram-positive bacteria, such as E. coli and P. aeruginosa, and Gram-negative bacteria, like S, aureus, are found to be the most predominant pathogens, with multi-resistant strains continuing to increase in incidence. Promising findings in novel antimicrobial peptides, phages, cell therapy, development of pH- or NIR-responsive hydrogels together with herbal medicine will address current issues in wound infection and translate to general practice eventually. Early detection of wound infections, combination therapies and understanding the skin microbiome can also aid in the treatment and prevention of wound infections.
Abbreviations
AMP: Antimicrobial peptide; CM: Cellulose microfibers; CFU: Colony forming unit; FDA: Food and drug adminisration; MDR: Multiple drug resistence; NETosis: NETosis is a programme for formation of neutrophil extracellular traps; NIR: Near-infrared; PCR: Polymerase chain reaction; PDA-NP: Polydopamine nanoparticles; SSWIs: Surgical site wound infections.
Acknowledgments
This work was supported by National Science Foundation of China (82172217), Fundamental Science (Natural Science) Research Project of the Jiangsu Higher Education Institutions of China (No. 21KJB360016) and Natural Science Foundation of Nanjing University of Chinese Medicine (No. XZR2020069).
Conflicts of interest
None declared.
Contributor Information
Xiaotong Ding, School of Pharmacy, Jiangsu Provincial Engineering Research Center of Traditional Chinese Medicine External Medication Development and Application, Nanjing University of Chinese Medicine, Nanjing 210023, People’s Republic of China.
Qinghan Tang, School of Pharmacy, Jiangsu Provincial Engineering Research Center of Traditional Chinese Medicine External Medication Development and Application, Nanjing University of Chinese Medicine, Nanjing 210023, People’s Republic of China.
Zeyu Xu, School of Pharmacy, Jiangsu Provincial Engineering Research Center of Traditional Chinese Medicine External Medication Development and Application, Nanjing University of Chinese Medicine, Nanjing 210023, People’s Republic of China.
Ye Xu, Department of Burns and Plastic Surgery, The affiliated Drum Tow Hospital of Nanjing University of Chinese Medicine, Nanjing 210008, People’s Republic of China.
Hao Zhang, Department of Burns and Plastic Surgery, The affiliated Drum Tow Hospital of Nanjing University of Chinese Medicine, Nanjing 210008, People’s Republic of China.
Dongfeng Zheng, Department of Burns and Plastic Surgery, The affiliated Drum Tow Hospital of Nanjing University of Chinese Medicine, Nanjing 210008, People’s Republic of China.
Shuqin Wang, Department of Burns and Plastic Surgery, The affiliated Drum Tow Hospital of Nanjing University of Chinese Medicine, Nanjing 210008, People’s Republic of China.
Qian Tan, Department of Burns and Plastic Surgery, The affiliated Drum Tow Hospital of Nanjing University of Chinese Medicine, Nanjing 210008, People’s Republic of China.
Joanneke Maitz, Burns Injury and Reconstructive Surgery Research, ANZAC Research Institute, University of Sydney, Sydney, Australia, 2137; Burns Unit, Concord Repatriation General Hospital, Concord, Australia 2137.
Peter K Maitz, Burns Injury and Reconstructive Surgery Research, ANZAC Research Institute, University of Sydney, Sydney, Australia, 2137; Burns Unit, Concord Repatriation General Hospital, Concord, Australia 2137.
Shaoping Yin, School of Pharmacy, Jiangsu Provincial Engineering Research Center of Traditional Chinese Medicine External Medication Development and Application, Nanjing University of Chinese Medicine, Nanjing 210023, People’s Republic of China.
Yiwei Wang, School of Pharmacy, Jiangsu Provincial Engineering Research Center of Traditional Chinese Medicine External Medication Development and Application, Nanjing University of Chinese Medicine, Nanjing 210023, People’s Republic of China; Burns Injury and Reconstructive Surgery Research, ANZAC Research Institute, University of Sydney, Sydney, Australia, 2137.
Jun Chen, School of Pharmacy, Jiangsu Provincial Engineering Research Center of Traditional Chinese Medicine External Medication Development and Application, Nanjing University of Chinese Medicine, Nanjing 210023, People’s Republic of China.
References
- 1. Parani M, Lokhande G, Singh A, Gaharwar AK. Engineered nanomaterials for infection control and healing acute and chronic wounds. ACS Appl Mater Interfaces. 2016;8:10049–69. [DOI] [PubMed] [Google Scholar]
- 2. Fan Z, Yao B, Ding Y, Xu D, Zhao J, Zhang K. Rational engineering the DNA tetrahedrons of dual wavelength ratiometric electrochemiluminescence biosensor for high efficient detection of SARS-CoV-2 RdRp gene by using entropy-driven and bipedal DNA walker amplification strategy. Chem Eng J. 2022;427:131686. 10.1016/j.cej.2021.131686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. Bassetti M, Peghin M, Castaldo N, Giacobbe DR. The safety of treatment options for acute bacterial skin and skin structure infections. Expert Opin Drug Saf. 2019;18:635–50. [DOI] [PubMed] [Google Scholar]
- 4. Jamaledin R, Yiu CKY, Zare EN, Niu LN, Vecchione R, Chen G, et al. Advances in antimicrobial microneedle patches for combating infections. Adv Mater. 2020;32:e2002129. 10.1002/adma.202002129. [DOI] [PubMed] [Google Scholar]
- 5. Rahim K, Saleha S, Zhu X, Huo L, Basit A, Franco OL. Bacterial contribution in chronicity of wounds. Microb Ecol. 2017;73:710–21. [DOI] [PubMed] [Google Scholar]
- 6. Turner KH, Everett J, Trivedi U, Rumbaugh KP, Whiteley M. Requirements for Pseudomonas aeruginosa acute burn and chronic surgical wound infection. PLoS Genet. 2014;10:e1004518. 10.1371/journal.pgen.1004518. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Norman G, Christie J, Liu Z, Westby MJ, Jefferies JM, Hudson T, et al. Antiseptics for burns. Cochrane Database Syst Rev. 2017;7:CD011821. 10.1002/14651858.CD011821.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Wang Y, Beekman J, Hew J, Jackson S, Issler-Fisher AC, Parungao R, et al. Burn injury: challenges and advances in burn wound healing, infection, pain and scarring. Adv Drug Deliv Rev. 2018;123:3–17. [DOI] [PubMed] [Google Scholar]
- 9. Sganga G, Pea F, Aloj D, Corcione S, Pierangeli M, Stefani S, et al. Acute wound infections management: the 'Don'ts' from a multidisciplinary expert panel. Expert Rev Anti-Infect Ther. 2020;18:231–40. [DOI] [PubMed] [Google Scholar]
- 10. Reid G, Younes JA, Van der Mei HC, Gloor GB, Knight R, Busscher HJ. Microbiota restoration: natural and supplemented recovery of human microbial communities. Nat Rev Microbiol. 2011;9:27–38. [DOI] [PubMed] [Google Scholar]
- 11. Branch-Elliman W, Ripollone JE, O'Brien WJ, Itani KMF, Schweizer ML, Perencevich E, et al. Risk of surgical site infection, acute kidney injury, and Clostridium difficile infection following antibiotic prophylaxis with vancomycin plus a beta-lactam versus either drug alone: a national propensity-score-adjusted retrospective cohort study. PLoS Med. 2017;14:e1002340. 10.1371/journal.pmed.1002340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Altoparlak U, Koca O, Ozkurt Z, Akcay MN. Incidence and risk factors of vancomycin-resistant enterococcus colonization in burn unit patients. Burns. 2011;37:49–53. [DOI] [PubMed] [Google Scholar]
- 13. Costa ML, Achten J, Knight R, Bruce J, Dutton SJ, Madan J, et al. Effect of incisional negative pressure wound therapy vs standard wound dressing on deep surgical site infection after surgery for lower limb fractures associated with major trauma: the WHIST randomized clinical trial. JAMA. 2020;323:519–26. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Heal CF, Banks JL, Lepper PD, Kontopantelis E, van Driel ML. Topical antibiotics for preventing surgical site infection in wounds healing by primary intention. Cochrane Database Syst Rev. 2016;11:CD011426. 10.1002/14651858.CD011426.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. O'Neal PB, Itani KM. Antimicrobial formulation and delivery in the prevention of surgical site infection. Surg Infect. 2016;17:275–85. [DOI] [PubMed] [Google Scholar]
- 16. Cooper C, Horner C, Barlow G, Stryja J, Sandy-Hodgetts K, Guise T, et al. A survey of practice and opinions on the use of topical antibiotics to prevent surgical site infection: more confusion than consensus. J Antimicrob Chemother. 2018;73:1978–83. [DOI] [PubMed] [Google Scholar]
- 17. Mihai MM, Holban AM, Giurcaneanu C, Popa LG, Oanea RM, Lazar V, et al. Microbial biofilms: impact on the pathogenesis of periodontitis, cystic fibrosis, chronic wounds and medical device-related infections. Curr Top Med Chem. 2015;15:1552–76. [DOI] [PubMed] [Google Scholar]
- 18. Percival SL. Importance of biofilm formation in surgical infection. Br J Surg. 2017;104:e85–94. [DOI] [PubMed] [Google Scholar]
- 19. Iheozor-Ejiofor Z, Newton K, Dumville JC, Costa ML, Norman G, Bruce J, et al. Negative pressure wound therapy for open traumatic wounds. Cochrane Database Syst Rev. 2018;2018:CD012522. 10.1002/14651858.CD012522.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Dai T, Kharkwal GB, Tanaka M, Huang YY, Bil de Arce VJ, Hamblin MR. Animal models of external traumatic wound infections. Virulence. 2011;2:296–315. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Singer AJ, Dagum AB. Current management of acute cutaneous wounds. N Engl J Med. 2008;359:1037–46. [DOI] [PubMed] [Google Scholar]
- 22. Herrod PJ, Boyd-Carson H, Doleman B, Blackwell J, Williams JP, Bhalla A, et al. Prophylactic antibiotics for penetrating abdominal trauma: duration of use and antibiotic choice. Cochrane Database Syst Rev. 2019;12:CD010808. 10.1002/14651858.CD010808.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Ganesan A, Shaikh F, Bradley W, Blyth DM, Bennett D, Petfield JL, et al. Classification of trauma-associated invasive fungal infections to support wound treatment decisions. Emerg Infect Dis. 2019;25. 10.3201/eid2509.190168. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Kronen R, Liang SY, Bochicchio G, Bochicchio K, Powderly WG, Spec A. Invasive fungal infections secondary to traumatic injury. Int J Infect Dis. 2017;62:102–11. [DOI] [PubMed] [Google Scholar]
- 25. Warkentien T, Rodriguez C, Lloyd B, Wells J, Weintrob A, Dunne JR, et al. Invasive mold infections following combat-related injuries. Clin Infect Dis. 2012;55:1441–9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Tomic-Canic M, Burgess JL, O'Neill KE, Strbo N, Pastar I. Skin microbiota and its interplay with wound healing. Am J Clin Dermatol. 2020;21:36–43. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kalan L, Loesche M, Hodkinson BP, Heilmann K, Ruthel G, Gardner SE, et al. Redefining the chronic-wound microbiome: fungal communities are prevalent, dynamic, and associated with delayed healing. M bio. 2016;7. 10.1128/mBio.01058-16. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Di Domenico EG, Farulla I, Prignano G, Gallo MT, Vespaziani M, Cavallo I, et al. Biofilm is a major virulence determinant in bacterial colonization of chronic skin ulcers independently from the multidrug resistant phenotype. Int J Mol Sci. 2017;18:1077. 10.3390/ijms18051077. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Johnson TR, Gomez BI, McIntyre MK, Dubick MA, Christy RJ, Nicholson SE, et al. The cutaneous microbiome and wounds: new molecular targets to promote wound healing. Int J Mol Sci. 2018;19:2699. 10.3390/ijms19092699. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Versey Z, da Cruz Nizer WS, Russell E, Zigic S, DeZeeuw KG, Marek JE, et al. Biofilm-innate immune Interface: contribution to chronic wound formation. Front Immunol. 2021;12:648554. 10.3389/fimmu.2021.648554. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Wu YK, Cheng NC, Cheng CM. Biofilms in chronic wounds: pathogenesis and diagnosis. Trends Biotechnol. 2019;37:505–17. [DOI] [PubMed] [Google Scholar]
- 32. Xuan Q, Jiang F, Dong H, Zhang W, Zhang F, Ma T, et al. Bioinspired intrinsic versatile hydrogel fabricated by amyloidal toxin simulant-based Nanofibrous assemblies for accelerated diabetic wound healing. Adv Funct Mater. 2021;31:2106705. 10.1002/adfm.202106705. [DOI] [Google Scholar]
- 33. Liu YF, Ni PW, Huang Y, Xie T. Therapeutic strategies for chronic wound infection. Chin J Traumatol. 2021;25:11–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34. Bertesteanu S, Triaridis S, Stankovic M, Lazar V, Chifiriuc MC, Vlad M, et al. Polymicrobial wound infections: pathophysiology and current therapeutic approaches. Int J Pharm. 2014;463:119–26. [DOI] [PubMed] [Google Scholar]
- 35. Uçkay I, Gariani K, Pataky Z, Lipsky BA. Diabetic foot infections: state-of-the-art. Diabetes Obes Metab. 2014;16:305–16. [DOI] [PubMed] [Google Scholar]
- 36. Kalan LR, Brennan MB. The role of the microbiome in nonhealing diabetic wounds. Ann N Y Acad Sci. 2019;1435:79–92. [DOI] [PubMed] [Google Scholar]
- 37. Wei S, Xu P, Yao Z, Cui X, Lei X, Li L, et al. A composite hydrogel with co-delivery of antimicrobial peptides and platelet-rich plasma to enhance healing of infected wounds in diabetes. Acta Biomater. 2021;124:205–18. [DOI] [PubMed] [Google Scholar]
- 38. Trivedi U, Madsen JS, Rumbaugh KP, Wolcott RD, Burmolle M, Sorensen SJ. A post-planktonic era of in vitro infectious models: issues and changes addressed by a clinically relevant wound like media. Crit Rev Microbiol. 2017;43:453–65. [DOI] [PubMed] [Google Scholar]
- 39. Zhou J, Yao D, Qian Z, Hou S, Li L, Jenkins ATA, et al. Bacteria-responsive intelligent wound dressing: simultaneous in situ detection and inhibition of bacterial infection for accelerated wound healing. Biomaterials. 2018;161:11–23. [DOI] [PubMed] [Google Scholar]
- 40. Norman G, Dumville JC, Moore ZE, Tanner J, Christie J, Goto S. Antibiotics and antiseptics for pressure ulcers. Cochrane Database Syst Rev. 2016;4:CD011586. 10.1002/14651858.CD011586.pub2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. O'Meara S, Al-Kurdi D, Ologun Y, Ovington LG, Martyn-St James M, Richardson R. Antibiotics and antiseptics for venous leg ulcers. Cochrane Database Syst Rev. 2014;1:CD003557. 10.1002/14651858.CD003557.pub5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42. Pugliese DJ. Infection in venous leg ulcers: considerations for optimal Management in the Elderly. Drugs Aging. 2016;33:87–96. [DOI] [PubMed] [Google Scholar]
- 43. Leaper D, Assadian O, Edmiston CE. Approach to chronic wound infections. Br J Dermatol. 2015;173:351–8. [DOI] [PubMed] [Google Scholar]
- 44. Thet NT, Mercer-Chalmers J, Greenwood RJ, Young AER, Coy K, Booth S, et al. SPaCE swab: point-of-care sensor for simple and rapid detection of acute wound infection. ACS Sens. 2020;5:2652–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45. Reddy M, Gill SS, Wu W, Kalkar SR, Rochon PA. Does this patient have an infection of a chronic wound? JAMA. 2012;307:605–11. [DOI] [PubMed] [Google Scholar]
- 46. Bystritsky R, Chambers H. Cellulitis and soft tissue infections. Ann Intern Med. 2018;168:ITC17–32. [DOI] [PubMed] [Google Scholar]
- 47. Jnana A, Muthuraman V, Varghese VK, Chakrabarty S, Murali TS, Ramachandra L, et al. Microbial community distribution and Core microbiome in successive wound grades of individuals with diabetic foot ulcers. Appl Environ Microbiol. 2020;86. 10.1128/AEM.02608-19. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48. Liu C, Ponsero AJ, Armstrong DG, Lipsky BA, Hurwitz BL. The dynamic wound microbiome. BMC Med. 2020;18:358. 10.1186/s12916-020-01820-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49. Wolcott R, Costerton JW, Raoult D, Cutler SJ. The polymicrobial nature of biofilm infection. Clin Microbiol Infect. 2013;19:107–12. [DOI] [PubMed] [Google Scholar]
- 50. Chin JS, Madden L, Chew SY, Becker DL. Drug therapies and delivery mechanisms to treat perturbed skin wound healing. Adv Drug Deliv Rev. 2019;149-150:2–18. [DOI] [PubMed] [Google Scholar]
- 51. Daeschlein G. Antimicrobial and antiseptic strategies in wound management. Int Wound J. 2013;10:9–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52. Szweda P, Gorczyca G, Tylingo R. Comparison of antimicrobial activity of selected, commercially available wound dressing materials. J Wound Care. 2018;27:320–6. [DOI] [PubMed] [Google Scholar]
- 53. Schwarzer S, James GA, Goeres D, Bjarnsholt T, Vickery K, Percival SL, et al. The efficacy of topical agents used in wounds for managing chronic biofilm infections: a systematic review. J Inf Secur. 2020;80:261–70. [DOI] [PubMed] [Google Scholar]
- 54. Chen Z, Wang Z, Ren J, Qu X. Enzyme mimicry for combating bacteria and biofilms. Acc Chem Res. 2018;51:789–99. [DOI] [PubMed] [Google Scholar]
- 55. Eardley WG, Brown KV, Bonner TJ, Green AD, Clasper JC. Infection in conflict wounded. Philos Trans R Soc Lond Ser B Biol Sci. 2011;366:204–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56. Gardner SE, Haleem A, Jao YL, Hillis SL, Femino JE, Phisitkul P, et al. Cultures of diabetic foot ulcers without clinical signs of infection do not predict outcomes. Diabetes Care. 2014;37:2693–701. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57. Falcone M, De Angelis B, Pea F, Scalise A, Stefani S, Tasinato R, et al. Challenges in the management of chronic wound infections. J Glob Antimicrob Resist. 2021;26:140–7. [DOI] [PubMed] [Google Scholar]
- 58. Verbanic S, Shen Y, Lee J, Deacon JM, Chen IA. Microbial predictors of healing and short-term effect of debridement on the microbiome of chronic wounds. NPJ Biofilms Microbiomes. 2020;6:21. 10.1038/s41522-020-0130-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59. Tisi PV, Than MM, Cochrane Vascular Group . Type of incision for below knee amputation. Cochrane Database Syst Rev. 2014;4:CD003749. 10.1002/14651858.CD003749.pub3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60. Blazar PE, Garon MT. Ray resections of the fingers: indications, techniques, and outcomes. J Am Acad Orthop Surg. 2015;23:476–84. [DOI] [PubMed] [Google Scholar]
- 61. Chang M, Nguyen TT. Strategy for treatment of infected diabetic foot ulcers. Acc Chem Res. 2021;54:1080–93. [DOI] [PubMed] [Google Scholar]
- 62. Grada A, Mervis J, Falanga V. Research techniques made simple: animal models of wound healing. J Invest Dermatol. 2018;138:2095–2105.e1. 10.1016/j.jid.2019.03.1134. [DOI] [PubMed] [Google Scholar]
- 63. Kathawala MH, Ng WL, Liu D, Naing MW, Yeong WY, Spiller KL, et al. Healing of chronic wounds: An update of recent developments and future possibilities. Tissue Eng Part B Rev. 2019;25:429–44. [DOI] [PubMed] [Google Scholar]
- 64. Sanapalli BKR, Yele V, Singh MK, Thaggikuppe Krishnamurthy P, Karri V. Preclinical models of diabetic wound healing: a critical review. Biomed Pharmacother. 2021;142:111946. 10.1016/j.biopha.2021.111946. [DOI] [PubMed] [Google Scholar]
- 65. Zindle JK, Wolinsky E, Bogie KM. A review of animal models from 2015 to 2020 for preclinical chronic wounds relevant to human health. J Tissue Viability. 2021;30:291–300. [DOI] [PubMed] [Google Scholar]
- 66. Suo H, Hussain M, Wang H, Zhou N, Tao J, Jiang H, et al. Correction to “injectable and pH-sensitive hyaluronic acid-based hydrogels with on-demand release of antimicrobial peptides for infected wound healing”. Biomacromolecules. 2021;22:5400. 10.1021/acs.biomac.1c01487. [DOI] [PubMed] [Google Scholar]
- 67. Thapa RK, Diep DB, Tonnesen HH. Topical antimicrobial peptide formulations for wound healing: current developments and future prospects. Acta Biomater. 2020;103:52–67. [DOI] [PubMed] [Google Scholar]
- 68. Mofazzal Jahromi MA, Sahandi Zangabad P, Moosavi Basri SM, Sahandi Zangabad K, Ghamarypour A, Aref AR, et al. Nanomedicine and advanced technologies for burns: preventing infection and facilitating wound healing. Adv Drug Deliv Rev. 2018;123:33–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 69. Kwakman PH, Krijgsveld J, de Boer L, Nguyen LT, Boszhard L, Vreede J, et al. Native thrombocidin-1 and unfolded thrombocidin-1 exert antimicrobial activity via distinct structural elements. J Biol Chem. 2011;286:43506–14. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70. Riool M, de Breij A, Kwakman PHS, Schonkeren-Ravensbergen E, de Boer L, Cordfunke RA, et al. Thrombocidin-1-derived antimicrobial peptide TC19 combats superficial multi-drug resistant bacterial wound infections. Biochim Biophys Acta Biomembr. 2020;1862:183282. 10.1016/j.bbamem.2020.183282. [DOI] [PubMed] [Google Scholar]
- 71. Diaz E, Fernandez IM, Jimenez L, Rodriguez M, Surani S. Is methicillin-resistant Staphylococcus aureus pneumonia epidemiology and sensitivity changing? Am J Med Sci. 2012;343:196–8. [DOI] [PubMed] [Google Scholar]
- 72. Hakansson J, Cavanagh JP, Stensen W, Mortensen B, Svendsen JS, Svenson J. In vitro and in vivo antibacterial properties of peptide AMC-109 impregnated wound dressings and gels. J Antibiot (Tokyo). 2021;74:337–45. [DOI] [PubMed] [Google Scholar]
- 73. Gorr SU, Flory CM, Schumacher RJ. In vivo activity and low toxicity of the second-generation antimicrobial peptide DGL13K. PLoS One. 2019;14:e0216669. 10.1371/journal.pone.0216669. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74. Gan BH, Gaynord J, Rowe SM, Deingruber T, Spring DR. The multifaceted nature of antimicrobial peptides: current synthetic chemistry approaches and future directions. Chem Soc Rev. 2021;50:7820–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75. Li W, Separovic F, O'Brien-Simpson NM, Wade JD. Chemically modified and conjugated antimicrobial peptides against superbugs. Chem Soc Rev. 2021;50:4932–73. [DOI] [PubMed] [Google Scholar]
- 76. Ong ZY, Wiradharma N, Yang YY. Strategies employed in the design and optimization of synthetic antimicrobial peptide amphiphiles with enhanced therapeutic potentials. Adv Drug Deliv Rev. 2014;78:28–45. [DOI] [PubMed] [Google Scholar]
- 77. Liu S, Fukushima K, Venkataraman S, Hedrick JL, Yang YY. Supramolecular nanofibers self-assembled from cationic small molecules derived from repurposed poly(ethylene teraphthalate) for antibiotic delivery. Nanomedicine. 2018;14:165–72. [DOI] [PubMed] [Google Scholar]
- 78. Fumakia M, Ho EA. Nanoparticles encapsulated with LL37 and serpin A1 promotes wound healing and synergistically enhances antibacterial activity. Mol Pharm. 2016;13:2318–31. [DOI] [PubMed] [Google Scholar]
- 79. Comune M, Rai A, Chereddy KK, Pinto S, Aday S, Ferreira AF, et al. Antimicrobial peptide-gold nanoscale therapeutic formulation with high skin regenerative potential. J Control Release. 2017;262:58–71. [DOI] [PubMed] [Google Scholar]
- 80. Chen WY, Chang HY, Lu JK, Huang YC, Harroun SG, Tseng YT, et al. Self-assembly of antimicrobial peptides on gold Nanodots: against multidrug-resistant bacteria and wound-healing application. Adv Funct Mater. 2016;25:7189–99. [Google Scholar]
- 81. Gao L, Giglio KM, Nelson JL, Sondermann H, Travis AJ. Ferromagnetic nanoparticles with peroxidase-like activity enhance the cleavage of biological macromolecules for biofilm elimination. Nanoscale. 2014;6:2588–93. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82. Baistrocchi SR, Lee MJ, Lehoux M, Ralph B, Snarr BD, Robitaille R, et al. Posaconazole-loaded leukocytes as a novel treatment strategy targeting invasive pulmonary aspergillosis. J Infect Dis. 2017;215:1734–41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83. Matsuzaki S, Yasuda M, Nishikawa H, Kuroda M, Ujihara T, Shuin T, et al. Experimental protection of mice against lethal Staphylococcus aureus infection by novel bacteriophage phi MR11. J Infect Dis. 2003;187:613–24. [DOI] [PubMed] [Google Scholar]
- 84. Wittebole X, De Roock S, Opal SM. A historical overview of bacteriophage therapy as an alternative to antibiotics for the treatment of bacterial pathogens. Virulence. 2014;5:226–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85. Bull JJ, Gill JJ. The habits of highly effective phages: population dynamics as a framework for identifying therapeutic phages. Front Microbiol. 2014;5:618. 10.3389/fmicb.2014.00618. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86. Pinto AM, Cerqueira MA, Banobre-Lopes M, Pastrana LM, Sillankorva S. Bacteriophages for chronic wound treatment: from traditional to novel delivery systems. Viruses. 2020;12:235. 10.3390/v12020235. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87. Kering KK, Kibii BJ, Wei H. Biocontrol of phytobacteria with bacteriophage cocktails. Pest Manag Sci. 2019;75:1775–81. [DOI] [PubMed] [Google Scholar]
- 88. Rhoads DD, Wolcott RD, Kuskowski MA, Wolcott BM, Ward LS, Sulakvelidze A. Bacteriophage therapy of venous leg ulcers in humans: results of a phase I safety trial. J Wound Care. 2013;18:237–8 240-3. [DOI] [PubMed] [Google Scholar]
- 89. Fish R, Kutter E, Wheat G, Blasdel B, Kutateladze M, Kuhl S. Compassionate use of bacteriophage therapy for foot ulcer treatment as an effective step for moving toward clinical trials. Methods Mol Biol. 2018;1693:159–70. [DOI] [PubMed] [Google Scholar]
- 90. Fish R, Kutter E, Wheat G, Blasdel B, Kutateladze M, Kuhl S. Bacteriophage treatment of intransigent diabetic toe ulcers: a case series. J Wound Care. 2016;25:S27–33.26949862 [Google Scholar]
- 91. Huh H, Wong S, St. Jean J, Slavcev R. Bacteriophage interactions with mammalian tissue: therapeutic applications. Adv Drug Deliv Rev. 2019;145:4–17. [DOI] [PubMed] [Google Scholar]
- 92. Kharaziha M, Baidya A, Annabi N. Rational Design of Immunomodulatory Hydrogels for chronic wound healing. Adv Mater. 2021;33:2100176. 10.1002/adma.202100176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93. Fathi A, Mithieux SM, Wei H, Chrzanowski W, Valtchev P, Weiss AS, et al. Elastin based cell-laden injectable hydrogels with tunable gelation, mechanical and biodegradation properties. Biomaterials. 2014;35:5425–35. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 94. Zheng Z, Bian S, Li Z, Zhang Z, Liu Y, Zhai X, et al. Catechol modified quaternized chitosan enhanced wet adhesive and antibacterial properties of injectable thermo-sensitive hydrogel for wound healing. Carbohydr Polym. 2020;249:116826. 10.1016/j.carbpol.2020.116826. [DOI] [PubMed] [Google Scholar]
- 95. Yun EJ, Yon B, Joo MK, Jeong B. Cell therapy for skin wound using fibroblast encapsulated poly(ethylene glycol)-poly(L-alanine) thermogel. Biomacromolecules. 2012;13:1106–11. [DOI] [PubMed] [Google Scholar]
- 96. Dang Q, Liu K, Zhang Z, Liu C, Liu X, Xin Y, et al. Fabrication and evaluation of thermosensitive chitosan/collagen/α, β-glycerophosphate hydrogels for tissue regeneration. Carbohydr Polym. 2017;167:145–57. [DOI] [PubMed] [Google Scholar]
- 97. Aliakbar Ahovan Z, Khosravimelal S, Eftekhari BS, Mehrabi S, Hashemi A, Eftekhari S, et al. Thermo-responsive chitosan hydrogel for healing of full-thickness wounds infected with XDR bacteria isolated from burn patients: in vitro and in vivo animal model. Int J Biol Macromol. 2020;164:4475–86. [DOI] [PubMed] [Google Scholar]
- 98. Schaude C, Fröhlich E, Meindl C, Attard J, Binder B, Mohr GJ. The development of indicator cotton swabs for the detection of pH in wounds. Sensors (Basel). 2017;17:1365. 10.3390/s17061365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 99. Ono S, Imai R, Ida Y, Shibata D, Komiya T, Matsumura H. Increased wound pH as an indicator of local wound infection in second degree burns. Burns. 2015;41:820–4. [DOI] [PubMed] [Google Scholar]
- 100. Zepon KM, Martins MM, Marques MS, Heckler JM, Dal Pont Morisso F, Moreira MG, et al. Smart wound dressing based on κ–carrageenan/locust bean gum/cranberry extract for monitoring bacterial infections. Carbohydr Polym. 2019;206:362–70. [DOI] [PubMed] [Google Scholar]
- 101. Arafa AA, Nada AA, Ibrahim AY, Sajkiewicz P, Zahran MK, Hakeim OA. Preparation and characterization of smart therapeutic pH-sensitive wound dressing from red cabbage extract and chitosan hydrogel. Int J Biol Macromol. 2021;182:1820–31. [DOI] [PubMed] [Google Scholar]
- 102. Reshmi CR, Suja PS, Manaf O, Sanu PP, Sujith A. Nanochitosan enriched poly epsilon-caprolactone electrospun wound dressing membranes: a fine tuning of physicochemical properties, hemocompatibility and curcumin release profile. Int J Biol Macromol. 2018;108:1261–72. [DOI] [PubMed] [Google Scholar]
- 103. Ren Y, Yu X, Li Z, Liu D, Xue X. Fabrication of pH-responsive TA-keratin bio-composited hydrogels encapsulated with photoluminescent GO quantum dots for improved bacterial inhibition and healing efficacy in wound care management: in vivo wound evaluations. J Photochem Photobiol B. 2020;202:111676. 10.1016/j.jphotobiol.2019.111676. [DOI] [PubMed] [Google Scholar]
- 104. Liu X, Cao J, Li H, Li J, Jin Q, Ren K, et al. Mussel-inspired polydopamine: a biocompatible and ultrastable coating for nanoparticles in vivo. ACS Nano. 2013;7:9384–95. [DOI] [PubMed] [Google Scholar]
- 105. Liu Y, Ai K, Liu J, Deng M, He Y, Lu L. Dopamine-melanin colloidal nanospheres: an efficient near-infrared photothermal therapeutic agent for in vivo cancer therapy. Adv Mater. 2013;25:1353–9. [DOI] [PubMed] [Google Scholar]
- 106. Gao G, Jiang YW, Jia HR, Wu FG. Near-infrared light-controllable on-demand antibiotics release using thermo-sensitive hydrogel-based drug reservoir for combating bacterial infection. Biomaterials. 2019;188:83–95. [DOI] [PubMed] [Google Scholar]
- 107. Zheng BD, Ye J, Yang YC, Huang YY, Xiao MT. Self-healing polysaccharide-based injectable hydrogels with antibacterial activity for wound healing. Carbohydr Polym. 2022;275:118770. 10.1016/j.carbpol.2021.118770. [DOI] [PubMed] [Google Scholar]
- 108. Yang X, Li P, Tang W, Du S, Yu M, Lu H, et al. A facile injectable carbon dot/oxidative polysaccharide hydrogel with potent self-healing and high antibacterial activity. Carbohydr Polym. 2021;251:117040. 10.1016/j.carbpol.2020.117040. [DOI] [PubMed] [Google Scholar]
- 109. Cross ER, Coulter SM, Pentlavalli S, Laverty G. Unravelling the antimicrobial activity of peptide hydrogel systems: current and future perspectives. Soft Matter. 2021;17:81–821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 110. Lopez-Silva TL, Leach DG, Azares A, Li IC, Woodside DG, Hartgerink JD. Chemical functionality of multidomain peptide hydrogels governs early host immune response. Biomaterials. 2020;231:119667. 10.1016/j.biomaterials.2019.119667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111. Carrejo NC, Moore AN, Lopez Silva TL, Leach DG, Li IC, Walker DR, et al. Multidomain peptide hydrogel accelerates healing of full-thickness wounds in diabetic mice. ACS Biomater Sci Eng. 2018;4:1386–96. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 112. He Y, Zhao W, Dong Z, Ji Y, Li M, Hao Y, et al. A biodegradable antibacterial alginate/carboxymethyl chitosan/Kangfuxin sponges for promoting blood coagulation and full-thickness wound healing. Int J Biol Macromol. 2021;167:182–92. [DOI] [PubMed] [Google Scholar]
- 113. Roberts AE, Maddocks SE, Cooper RA. Manuka honey reduces the motility of Pseudomonas aeruginosa by suppression of flagella-associated genes. J Antimicrob Chemother. 2015;70:716–25. [DOI] [PubMed] [Google Scholar]
- 114. Xia T, Xie F, Bian X, Chen Z, Zhang S, Fang Z, et al. Ultrabroad-spectrum, multidrug resistant bacteria-killing, and biocompatible quaternized chitin derivative for infected wound healing. Mater Sci Eng C Mater Biol Appl. 2021;126:112177. 10.1016/j.msec.2021.112177. [DOI] [PubMed] [Google Scholar]
- 115. Widsten P, Cruz CD, Fletcher GC, Pajak MA, McGhie TK. Tannins and extracts of fruit byproducts: antibacterial activity against foodborne bacteria and antioxidant capacity. J Agric Food Chem. 2014;62:11146–56. [DOI] [PubMed] [Google Scholar]
- 116. Su X, Liu X, Wang S, Li B, Pan T, Liu D, et al. Wound-healing promoting effect of total tannins from Entada phaseoloides (L.) Merr. In rats. Burns. 2017;43:830–8. [DOI] [PubMed] [Google Scholar]
- 117. Xu F, Weng B, Gilkerson R, Materon LA, Lozano K. Development of tannic acid/chitosan/pullulan composite nanofibers from aqueous solution for potential applications as wound dressing. Carbohydr Polym. 2015;115:16–24. [DOI] [PubMed] [Google Scholar]
- 118. Low WL, Kenward K, Britland ST, Amin MC, Martin C. Essential oils and metal ions as alternative antimicrobial agents: a focus on tea tree oil and silver. Int Wound J. 2017;14:369–84. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119. Perez-Recalde M, Ruiz Arias IE, Hermida EB. Could essential oils enhance biopolymers performance for wound healing? A systematic review. Phytomedicine. 2018;38:57–65. [DOI] [PubMed] [Google Scholar]
- 120. Singh S, Gupta A, Sharma D, Gupta B. Dextran based herbal nanobiocomposite membranes for scar free wound healing. Int J Biol Macromol. 2018;113:227–39. [DOI] [PubMed] [Google Scholar]
- 121. Pierpaoli E, Orlando F, Cirioni O, Simonetti O, Giacometti A, Provinciali M. Supplementation with tocotrienols from Bixa orellana improves the in vivo efficacy of daptomycin against methicillin-resistant Staphylococcus aureus in a mouse model of infected wound. Phytomedicine. 2017;36:50–3. [DOI] [PubMed] [Google Scholar]
- 122. Mehwish HM, Liu G, Rajoka MSR, Cai H, Zhong J, Song X, et al. Therapeutic potential of Moringa oleifera seed polysaccharide embedded silver nanoparticles in wound healing. Int J Biol Macromol. 2021;184:144–58. [DOI] [PubMed] [Google Scholar]
- 123. Marinas IC, Oprea E, Geana EI, Tutunaru O, Pircalabioru GG, Zgura I, et al. Valorization of Gleditsia triacanthos invasive plant cellulose microfibers and phenolic compounds for obtaining multi-functional wound dressings with antimicrobial and antioxidant properties. Int J Mol Sci. 2020;22. 10.3390/ijms22010033. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 124. Ma M, Zhong Y, Jiang X. Thermosensitive and pH-responsive tannin-containing hydroxypropyl chitin hydrogel with long-lasting antibacterial activity for wound healing. Carbohydr Polym. 2020;236:116096. 10.1016/j.carbpol.2020.116096. [DOI] [PubMed] [Google Scholar]
- 125. Gharib A, Faezizadeh Z, Godarzee M. Therapeutic efficacy of epigallocatechin gallate-loaded nanoliposomes against burn wound infection by methicillin-resistant Staphylococcus aureus. Skin Pharmacol Physiol. 2013;26:68–75. [DOI] [PubMed] [Google Scholar]
- 126. Barbosa R, Villarreal A, Rodriguez C, De Leon H, Gilkerson R, Lozano K. Aloe Vera extract-based composite nanofibers for wound dressing applications. Mater Sci Eng C Mater Biol Appl. 2021;124:112061. 10.1016/j.msec.2021.112061. [DOI] [PubMed] [Google Scholar]
- 127. Anjum S, Gupta A, Sharma D, Gautam D, Bhan S, Sharma A, et al. Development of novel wound care systems based on nanosilver nanohydrogels of polymethacrylic acid with Aloe vera and curcumin. Mater Sci Eng C Mater Biol Appl. 2016;64:157–66. [DOI] [PubMed] [Google Scholar]
- 128. Gupta B, Agarwal R, Sarwar Alam M. Antimicrobial and release study of drug loaded PVA/PEO/CMC wound dressings. J Mater Sci Mater Med. 2014;25:1613–22. [DOI] [PubMed] [Google Scholar]
- 129. Karumathil DP, Surendran-Nair M, Venkitanarayanan K. Efficacy of trans-cinnamaldehyde and eugenol in reducing Acinetobacter baumannii adhesion to and invasion of human keratinocytes and controlling wound infection in vitro. Phytother Res. 2016;30:2053–9. [DOI] [PubMed] [Google Scholar]
- 130. Yin C, Xie L, Guo Y. Phytochemical analysis and antibacterial activity of Gentiana macrophylla extract against bacteria isolated from burn wound infections. Microb Pathog. 2018;114:25–8. [DOI] [PubMed] [Google Scholar]
- 131. Sarhan WA, Azzazy HM, El-Sherbiny IM. Honey/chitosan nanofiber wound dressing enriched with Allium sativum and cleome droserifolia: enhanced antimicrobial and wound healing activity. ACS Appl Mater Interfaces. 2016;8:6379–90. [DOI] [PubMed] [Google Scholar]
- 132. Zhou L, Cai L, Ruan H, Zhang L, Wang J, Jiang H, et al. Electrospun chitosan oligosaccharide/polycaprolactone nanofibers loaded with wound-healing compounds of Rutin and quercetin as antibacterial dressings. Int J Biol Macromol. 2021;183:1145–54. [DOI] [PubMed] [Google Scholar]
- 133. Kim BE, Goleva E, Hall CF, Park SH, Lee UH, Brauweiler AM, et al. Skin wound healing is accelerated by a lipid mixture representing major lipid components of Chamaecyparis obtusa plant extract. J Invest Dermatol. 2018;138:1176–86. [DOI] [PubMed] [Google Scholar]
- 134. Farahpour MR, Pirkhezr E, Ashrafian A, Sonboli A. Accelerated healing by topical administration of Salvia officinalis essential oil on Pseudomonas aeruginosa and Staphylococcus aureus infected wound model. Biomed Pharmacother. 2020;128:110120. 10.1016/j.biopha.2020.110120. [DOI] [PubMed] [Google Scholar]
- 135. Farahpour MR, Sheikh S, Kafshdooz E, Sonboli A. Accelerative effect of topical Zataria multiflora essential oil against infected wound model by modulating inflammation, angiogenesis, and collagen biosynthesis. Pharm Biol. 2021;59:1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 136. Khezri K, Farahpour MR, Mounesi Rad S. Accelerated infected wound healing by topical application of encapsulated rosemary essential oil into nanostructured lipid carriers. Artif Cells Nanomed Biotechnol. 2019;47:980–8. [DOI] [PubMed] [Google Scholar]
- 137. Saporito F, Sandri G, Bonferoni MC, Rossi S, Boselli C, Icaro Cornaglia A, et al. Essential oil-loaded lipid nanoparticles for wound healing. Int J Nanomedicine. 2018;13:175–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 138. Melendez JH, Frankel YM, An AT, Williams L, Price LB, Wang NY, et al. Real-time PCR assays compared to culture-based approaches for identification of aerobic bacteria in chronic wounds. Clin Microbiol Infect. 2010;16:1762–9. [DOI] [PubMed] [Google Scholar]
- 139. Rennie MY, Dunham D, Lindvere-Teene L, Raizman R, Hill R, Linden R. Understanding real-time fluorescence signals from bacteria and wound tissues observed with the MolecuLight i:X(TM). Diagnostics (Basel). 2019;9. 10.3390/diagnostics9010022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 140. Vyas KS, Wong LK. Detection of biofilm in wounds as an early indicator for risk for tissue infection and wound chronicity. Ann Plast Surg. 2016;76:127–31. [DOI] [PubMed] [Google Scholar]
- 141. Wei D, Zhu X-M, Chen Y-Y, Li X-Y, Chen Y-P, Liu H-Y, et al. Chronic wound biofilms: diagnosis and therapeutic strategies. Chin Med J. 2019;132:2737–44. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 142. Watters C, Everett JA, Haley C, Clinton A, Rumbaugh KP. Insulin treatment modulates the host immune system to enhance Pseudomonas aeruginosa wound biofilms. Infect Immun. 2014;82:92–100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 143. Valente PMDS, Deva A, Ngo Q, Vickery K. The increased killing of biofilms in vitro by combining topical silver dressings with topical negative pressure in chronic wounds. Int Wound J. 2016;13:130–6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 144. Khalil MA, El Maghraby GM, Sonbol FI, Allam NG, Ateya PS, Ali SS. Enhanced efficacy of some antibiotics in presence of silver nanoparticles against multidrug resistant Pseudomonas aeruginosa recovered from burn wound infections. Front Microbiol. 2021;12:648560. 10.3389/fmicb.2021.648560. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 145. Tewarie L, Chernigov N, Goetzenich A, Moza A, Autschbach R, Zayat R. The effect of ultrasound-assisted debridement combined with vacuum pump therapy in deep sternal wound infections. Ann Thorac Cardiovasc Surg. 2018;24:139–46. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 146. Satish L, Gallo PH, Johnson S, Yates CC, Kathju S. Local probiotic therapy with lactobacillus plantarum mitigates scar formation in rabbits after burn injury and infection. Surg Infect. 2017;18:119–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 147. Valdez JC, Peral MC, Rachid M, Santana M, Perdigon G. Interference of lactobacillus plantarum with Pseudomonas aeruginosa in vitro and in infected burns: the potential use of probiotics in wound treatment. Clin Microbiol Infect. 2005;11:472–9. [DOI] [PubMed] [Google Scholar]
- 148. Lu Y, Li H, Wang J, Yao M, Peng Y, Liu T, et al. Engineering bacteria-activated multifunctionalized hydrogel for promoting diabetic wound healing. Adv Funct Mater. 2021;31:2105749. 10.1002/adfm.202105749. [DOI] [Google Scholar]
- 149. Wang G, Sweren E, Liu H, Wier E, Alphonse MP, Chen R, et al. Bacteria induce skin regeneration via IL-1β signaling. Cell Host Microbe. 2021;29:777–91.e6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 150. Kalan LR, Meisel JS, Loesche MA, Horwinski J, Soaita I, Chen X, et al. Strain- and species-level variation in the microbiome of diabetic wounds is associated with clinical outcomes and therapeutic efficacy. Cell Host Microbe. 2019;25:641–55.e5. [DOI] [PMC free article] [PubMed] [Google Scholar]