Abstract
Introduction
Telemedicine is the delivery of healthcare across a distance using some form of communication technology. The COVID-19 pandemic has led to increased adoption of telemedicine with national orthopaedic governing bodies advocating its use, as evidence suggests that social distancing maybe necessary until 2022. This systematic review aims to explore evidence for telemedicine in orthopaedics to determine its advantages, validity, effectiveness and utilisation.
Methods
Databases of PubMed, Web of Science, Scopus and CINAHL were systematically searched and articles were included if they involved any form of telephone or video consultation in an orthopaedic population. Findings were synthesised into four themes: patient/clinician satisfaction, accuracy and validity of examination, safety and patient outcomes and cost effectiveness. Quality assessment was undertaken using Cochrane and Joanna Briggs Institute appraisal tools.
Results
Twenty-one studies were included consisting of nine randomised controlled trials (RCTs). Studies revealed high patient satisfaction with telemedicine for convenience, less waiting and travelling time. Telemedicine was cost effective particularly if patients had to travel long distances, required hospital transport or time off work. No clinically significant differences were found in patient examination nor measurement of patient-reported outcome measures. Telemedicine was reported to be a safe method of consultation.
Discussion
Evidence suggests that telemedicine in orthopaedics can be safe, cost effective, valid in clinical assessment and with high patient/clinician satisfaction. However, more high-quality RCTs are required to elucidate long-term outcomes. This systematic review presents up-to-date evidence on the use of telemedicine and provides data for organisations considering its use during the COVID-19 pandemic and beyond.
Keywords: Teleconsulting, telemedicine, telehealth, remote consultation
Introduction
Telemedicine is the delivery of healthcare across a distance using some form of communications technology.1 With continued development of technology, telemedicine has become cheaper and easier to access, enabling a more widespread use.2 Reviews of telemedicine in other surgical specialties such as urology,3 vascular surgery4 and plastic surgery5 have found telemedicine to be cost effective, convenient and valid in its application. Although telerehabilitation of musculoskeletal conditions has been well investigated,6 evidence of telemedicine and its application within orthopaedic consultations remains to be more clearly defined.
On March 11, the World Health Organization declared a COVID-19 pandemic,7 and evidence suggests that ‘prolonged or intermittent social distancing’ may be necessary until 2022.8 National orthopaedic associations such as the British Orthopaedic Association (BOA) and the American Academy of Orthopaedic Surgeons (AAOS)9 have already issued pragmatic guidance advocating the use of telemedicine during COVID-19 in the interest of public health.10
Access to traditional F2F orthopaedic care is likely to be reduced in capacity, and therefore there is an urgent need to employ alternative methods such as telemedicine during current COVID-19 circumstances. This systematic review aims to explore current evidence for telemedicine in orthopaedic consultations to determine its advantages, validity and effectiveness, particularly during an era of limited physical patient contact and social distancing.
Method
Search strategy
A systematic literature search was conducted in May 2020 in compliance with the Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA) guidelines.11 The databases of MEDLINE (PubMed), Web of Science, Scopus and CINAHL were searched and all references of eligible articles were also manually reviewed. The search strategy involved searching study titles, abstracts and keywords by combining the terms orthopaedics AND telemedicine. Several synonyms and different spelling variations for each search term were used in order to capture as many articles as possible. Table 1 shows all 37 synonyms/variations searched and Table 3 (Supplementary materials) reveals the full search strategy for each database. The search was not limited by years (all articles up to May 2020 were included) and only English articles were reviewed.
Table 1.
Search terms, synonyms and variations used in search strategy.
| Term | Synonyms/variations searched |
|---|---|
| Orthopaedic | Orthopaedic, orthopedic, orthopaedics, orthopedics |
| Telemedicine | Telemedicine, tele medicine, tele-medicine |
| Teleconferencing | Teleconferencing, tele conferencing, tele-conferencing |
| Videoconferencing | Videoconferencing, video conferencing, video-conferencing |
| Video consultation | Video consultation, video-consultation |
| Remote consultation | Remote consultation, remote-consultation |
| Telehealth | Telehealth, tele health, tele-health |
| Telephone consultation | Telephone consultation, telephone-consultation |
| Teleconsultation | Teleconsultation, Tele consultation, Tele-consultation |
| Mobile health | Mobile health, mhealth, m-health |
| Teleorthopaedic | Teleorthopaedic, tele orthopaedic, tele-orthopaedic, teleorthopedic, teleorthopedic, tele-orthopedic |
| Telecare | Telecare, Tele care, Tele-care |
Eligibility criteria
A PICO framework (Population, Intervention, Control, Outcome) was used for our selection criteria. Articles were eligible for inclusion if they involved an orthopaedic patient population, using any form of video or telephone consultation and a measurable outcome assessing telemedicine.
Articles were excluded if they involved any of the following: combined speciality patient populations, telerehabilitation studies, military or rural medicine studies involving remote patient transfers, descriptive author experiences with no comparable outcomes, asynchronous consultations and web-based telemedicine not involving telephone or video consultations. Conference papers and letters were excluded as authors felt these did not provide enough detail to allow adequate quality/bias assessment of results and evaluate strength of conclusions.
Study selection and data extraction
Two reviewers (ZH and BA) independently screened the titles and abstracts of all studies. The full texts of potential articles were then assessed for eligibility by both reviewers with a third reviewer (FI) available to assist for consensus on inclusion. Study data were extracted using a framework including: author, year of publication, study type, intervention type, study population, themes assessed and findings. Discrepancies in data extraction were adjudicated by a third assessor (FI).
Quality assessment
Included randomised controlled trials (RCTs) were assessed for methodological quality and risk of bias using the revised Cochrane risk-of-bias tool (RoB 2).12 This tool allows assessment of bias across several domains with overall study quality graded as ‘high’, ‘low’ or ‘some concerns’. Remaining cohort studies, cross-sectional studies and case series were assessed for methodological quality using critical appraisal tools from the Joanna Briggs Institute.13 These tools allow assessment of quality over several domains with rating scales of ‘yes’, ‘no’ and ‘unclear’. Our criteria for a non-RCT study to be considered low quality was if more than two domains were graded as ‘no’ or two domains ‘no’ with one or more domains graded as ‘unclear’. Articles were assessed by two authors (ZH and BA) and any discrepancies decided by a third author (FI).
Results
Study characteristics
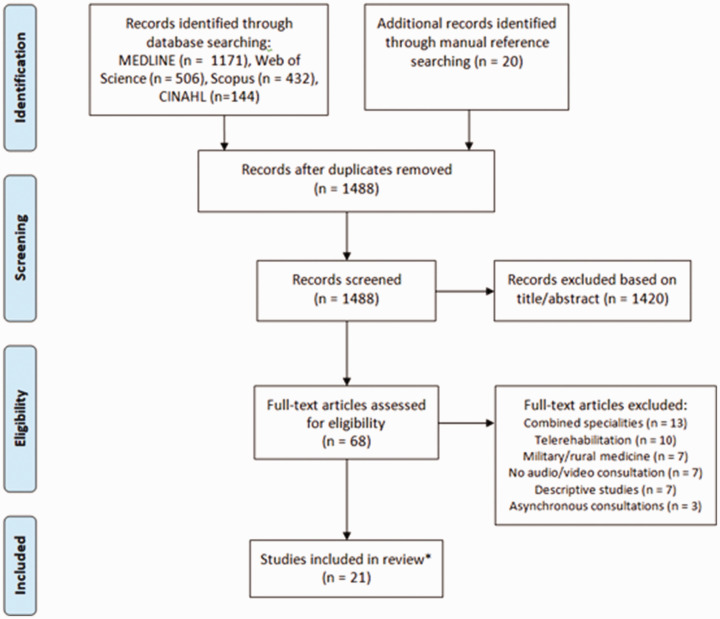
Electronic searches revealed 2273 records, of which 21 studies met the inclusion criteria. The search process is depicted in a PRISMA flow chart (Figure 1). Included studies consisted of nine RCTs,14–22 three cohort studies,23–25 seven cross-sectional studies26–32 and two case series.33,34 Studies covered a variety of orthopaedic care including paediatric and adult fracture care, elective orthopaedics, post-operative follow-up and oncology. Twelve studies utilised telemedicine at a remote clinical for a specialist consult, with the remaining nine studies performing telemedicine consults in the patient’s own home. Extracted data are summarised in Table 2 with study outcomes synthesised into four main themes: Clinician and patient satisfaction, accuracy and validity of clinical examination, patient safety and outcomes, cost effectiveness.
Figure 1.
PRISMA flow chart showing search process.*no articles were included from manual reference searching as inclusion criteria were not met.
Table 2.
Summary of study characteristics and extracted data.
| Author/ year | Type of study | Telemedicine setting | Number of patients | Patient population | Themes assessed | Findings |
|---|---|---|---|---|---|---|
| Kane et al., 202014 | RCT | Home telemedicine vs. F2F | 58 | Post-operative arthroscopic rotator cuff repair patients | Patient safety & outcomes | No significant difference in post-operative pain scores (p = 0.95) or ROM (p≥0.37). No significant difference in post-operative complications. |
| Clinician & patient satisfaction | No significant difference in patient satisfaction scores (p = 0.30). Significantly less time spent with telemedicine appointments (21.4 vs. 37.8 minutes). Telemedicine patients reported less time off work, less time waiting and preferred further follow-up using telemedicine. No significant difference in clinician satisfaction with entire telemedicine consult (p = 0.71). | |||||
| Sultan et al., 202026 | Cross-sectional | Home telemedicine | 189 | Paediatric spinal deformity vs. general paediatric patients | Patient satisfaction | Patients reported high satisfaction scores in both paediatric spinal deformity and general paediatric patients (5.0 ±0 vs. 4.8±0.1 points, p = 0.08). Patients had significantly shorter waiting times with telemedicine compared with F2F (13 vs. 41mins, p<0.001). |
| Silva et al., 201915 | RCT | Home telemedicine (at 4-week follow-up) vs. F2F (all follow-ups) | 57 | Paediatric humerus supracondylar fractures | Patient satisfaction | No significant difference in patient satisfaction scores (p = 0.12). |
| Patient safety & outcomes | No evidence of fracture displacement in either group or significant difference in Baumann’s angle (p = 0.09), ROM (p = 0.5), carrying angle (p = 0.11) or pain scores at 8-week follow-up (p = 0.1). | |||||
| Buvik et al., 201916 | RCT | Remote hospital joint telemedicine (nurse assisted) vs. F2F | 389 | General orthopaedic pathology | Patient satisfaction | No significant difference in patient satisfaction between two groups (p = 0.57). Those preferring telemedicine preferred the shorter travel time. Those preferring face to face wanted to see their specialist in person. Telemedicine patients had significantly shorter appointment waiting times. |
| Patient safety & outcomes | No significant difference in EQ-5D (p = 0.42) and EQ-VAS (p = 0.053) scores at 12-month follow-up. | |||||
| Goldstein et al., 201927 | Cross-sectional | Smart phone telemedicine at hospital site (researcher assisted) vs. F2F | 47 | Adult shoulder pathology | Accuracy & validity of clinical examination | No clinically significant difference in mean measurement of Constant Shoulder scores (0.53, 95%CI –2.6 to 1.6) between two methods. Telemedicine can obtain reliable estimate of shoulder function. |
| Sinha et al., 201923 | Cohort | Remote hospital joint telemedicine (PA assisted) vs. F2F | 167 | Paediatric fractures | Patient satisfaction | No significant difference in patient satisfaction between telemedicine and F2F (p = 0.07). More patients preferred to continue with telemedicine following an initial telemedicine consultation. |
| Cost effectiveness | Statistically significant less direct and indirect costs reported by patients using telemedicine (p≤ 0.03). | |||||
| Aponte-Tinao et al., 201928 | Cross-sectional | Home telemedicine vs. F2F | 207 | New orthopaedic oncology referrals | Cost effectiveness | Telemedicine would reduce healthcare costs by 12.2%. For 36 patients who had to travel more than 400 km costs reduced by 72%. |
| Buvik et al., 201917 | RCT | Remote hospital joint telemedicine (nurse assisted) vs. F2F | 389 | General orthopaedic pathology | Cost effectiveness | €18,616 saved using telemedicine with a workload of 300 consultations per year. Minimum 151 and 183 telemedicine consultations required per year to be cost effective from societal and health care perspectives, respectively. |
| Abel et al., 201729 | Cross-sectional | Home telemedicine vs. F2F | 34 | 10–20yr olds post-knee arthroscopic surgery | Accuracy & validity of clinical examination | No clinically significant difference in assessment of ROM (p = 0.07), effusion, incision colour between two methods. |
| Patient satisfaction | 96% of patients were satisfied with telemedicine. Two-thirds of telemedicine patients wanted future telemedicine consultations. | |||||
| Buvik et al., 201618 | RCT | Remote hospital joint telemedicine (nurse assisted) vs. F2F | 389 | General orthopaedic pathology | Clinician satisfaction | 98 % of consultations with telemedicine and 99% F2F were rated as ‘good’ or ‘very good’.Three patients needed consultation F2F as physician was not satisfied with examination. No significant difference in mean consultation time (p = 0.6). |
| Patient safety & outcomes | No significant difference in planned clinic outcomes; referral to surgery (p = 0.07), number of follow-ups (p = 0.06). No difference in serious events between two groups at 12-month follow-up (p = 0.26). | |||||
| Sathiyakumar et al., 201519 | RCT | Home telemedicine using Skype vs. F2F | 17 | Adult fracture follow-up | Patient satisfaction | No significant difference in patient satisfaction (p = 0.7). 75% of telemedicine patients preferred to continue with telemedicine follow-up. |
| Patient safety & outcomes | One patient in each group had a complication. Pyelonephritis in the control group and a DVT in the telemedicine group. | |||||
| Sharareh and Schwarzkopf, 201424 | Cohort study | Home telemedicine using Skype vs. F2F | 78 | Post-operative hip and knee arthroplasty patients | Patient safety & outcomes | One patient in the telemedicine group suffered a femoral head dislocation during follow-up. No significant difference in HOOS (p = 0.21), KOOS (p = 0.37), EQ-5D (p = 0.41), SF-12 (p≥0.29) and UCLA activity score (p = 0.25) between two groups. |
| Patient satisfaction | Higher average satisfaction rating with telemedicine (9.88 out of 10) compared with F2F consultations (average rating of 8.1 out of 10). | |||||
| Good et al., 201130 | Cross-sectional | Home telemedicine using Skype vs. F2F | 29 | Post-acromio-clavicular joint hook plate surgery for fractures | Accuracy & validity of clinical examination | No significant difference in measurement of Oxford Shoulder Score (–0.48, 95% CI –0.84 to –0.12) and Constant Shoulder scores (–0.68, 95% CI –1.08 to –0.29) between the two methods. |
| Williams et al., 200833 | Case series | Telephone consultation | 630 | Post-operative carpal tunnel decompression | Patient satisfaction | 93% of patients were satisfied with telephone follow-up. Patients commented on convenience and less time off work with telemedicine. |
| Cost effectiveness | Cost saving of £45,958 over 2 years using telemedicine. | |||||
| Vuolio et al., 200320 | RCT | Remote primary care joint telemedicine (nurse and GP assisted) vs. F2F | 145 | General orthopaedic pathology including trauma | Patient safety & outcomes | No significant difference in planned clinic outcomes between two groups (referral for surgery, follow-up). |
| Ohinmaa et al., 200221 | RCT | Remote primary care joint telemedicine (GP assisted) vs. F2F | 145 | General orthopaedic pathology | Cost effectiveness | Telemedicine cost effective, saved €2620 at a workload of 100 patients. Minimum 80 patients needed for societal cost saving. |
| Harno et al, 2001 [25] | Cohort | Remote primary care joint telemedicine (GP assisted) vs. F2F | 194 | General orthopaedic pathology | Clinician satisfaction | Feasibility of telemedicine as rated by clinicians was ‘excellent’ or ‘good’ in 49% of consultations. Confidence of specialists in telemedicine replacing F2F was low in 89% of specialists. |
| Cost effectiveness | 45% greater cost for F2F appointments compared with telemedicine. Higher cost due to hospital service charges. | |||||
| Haukipuro et al., 200022 | RCT | Primary care joint telemedicine (GP assisted) vs. F2F | 145 | General orthopaedic pathology including trauma | Clinician & patient satisfaction | Clinicians rated overall success of teleconsultation as ‘good’ or ‘very good’ in 80% compared with 99% in F2F (p<0.001). No significant difference in patient satisfaction (p>0.05); 97% of teleconsultation patients wanted to use this method for their next visit (with reasons including ease of visit, time saving and no travel). |
| Tachakra et al., 200031 | Cross-sectional | Minor injuries unit joint telemedicine (nurse assisted) vs. F2F at same location | 200 | Minor injuries | Accuracy & validity of clinical examination | Telemedicine accuracy in assessment of colour change 97%, swelling or deformity 98%, ROM 95%, tenderness 97%, weight bearing 99% compared with F2F assessment. Treatment over prescribed in one case and under prescribed in three cases. |
| Aarnio et al., 199932 | Cross-sectional | Remote hospital joint telemedicine (surgeon assisted) vs. F2F | 29 | General orthopaedic pathology | Clinician & patient satisfaction | 87% of patients rated the teleconsultation as ‘good’ or ‘very good’. Consultants felt teleconsultation showed the exam ‘well’ or ‘very well’ 84% of cases. The ability to make decisions was ‘good’ or ‘very good’ in 93%. |
| Lambrecht et al., 199834 | Case series | Remote hospital telemedicine | 91 | General trauma | Clinician satisfaction | All consultations were rated as ‘satisfactory’ or ‘excellent’. |
| Patient safety & outcomes | No adverse patient outcomes during monitoring but unclear follow-up time. |
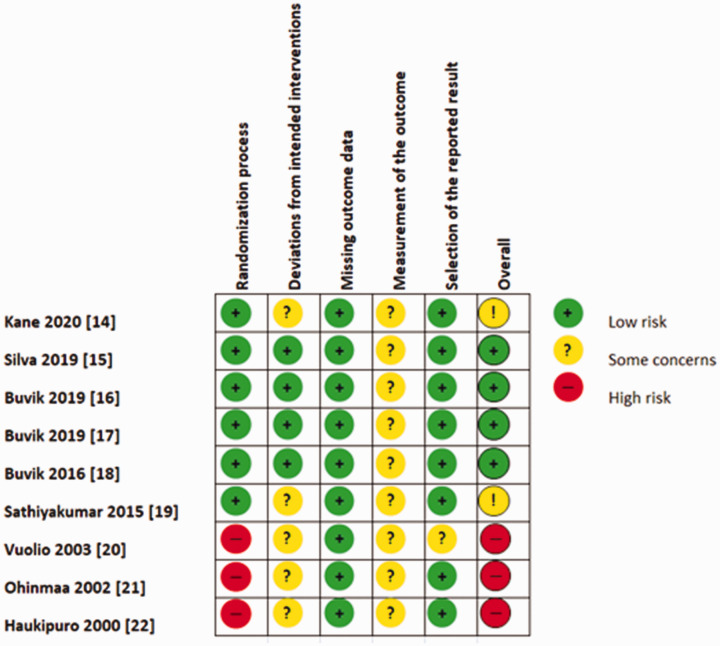
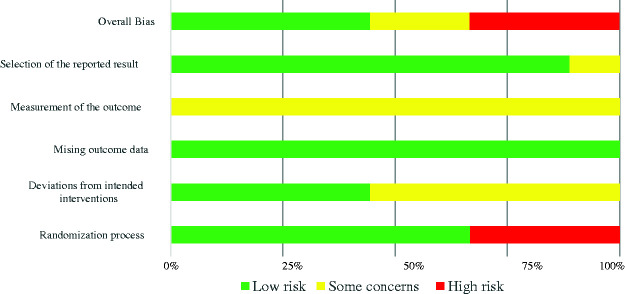
The overall risk of bias was deemed low for four out of the nine (44%) RCTs (Figure 2). All RCTs were graded ‘some concern’ for the ‘measurement of the outcome’ domain, predominantly due to no blinding in the studies, whilst the ‘missing outcome data’ domain was low risk of bias for all trials (Figure 3). Out of the remaining 12 non-RCT studies, three studies (25%) were found to be of high quality. The rest were graded overall as ‘some concern’ or ‘low quality’ due to deficiencies in valid measurement of outcomes and exploration of confounding factors. Quality assessment results for non-RCT studies can be found in Supplementary material.
Figure 2.
Results of risk of bias assessment using Cochrane RoB2 tool.
Figure 3.
Summary for risk of bias assessment using Cochrane RoB2 tool.
Clinician and patient satisfaction
Fourteen studies assessed clinician/patient satisfaction including six RCTs, three of which involved joint telemedicine with the patient, GP and specialist16,18,22 and three with telemedicine from home.14,15,19 All RCTs revealed no statistically significant difference in patient satisfaction between the two consultation methods.14–16,19,22 In terms of clinician satisfaction, Buvik et al.16 reported 98% of telemedicine versus 99% of F2F were evaluated as ‘good’ or ‘very good’. However, Haukipuro et al.22 found clinician ratings of ‘good’ or ‘very good’ in 80% of telemedicine consultations compared with 99% with F2F (p<0.001).
The remaining studies showed similar patient satisfaction rates as the RCTs, ranging from no statistically significant difference (p = 0.071)23 to ‘satisfactory’ and above in 96%,29 93% in another study,33 and ‘good’ or ‘very good’ in 87%.32 Sultan et al.26 also showed high satisfaction rates with telemedicine in paediatric patients with spinal deformity and general orthopaedic conditions (5.0±0 points vs. 4.8±0.1 points, p = 0.08). Sharareh and Schwarzkopf24 studied hip/knee arthroplasty follow-up and found higher satisfaction rates (average of 9.88 out of 10) with additional telemedicine consults compared with F2F (average of 8.1 out of 10, p = 0.05). Harno et al.25 found clinicians were satisfied with the image/sound quality and history taking ability in at least 84% and 91% of the consultations, respectively. However, feasibility of telemedicine was rated as ‘good’ or ‘excellent’ in 49% and the confidence of surgeons in telemedicine replacing F2F was low in 89%.
Patients who underwent telemedicine consultations wanted to continue with this method of consultation, with multiple studies reporting high preference rates of 66–97%.16,19,22,29 Reasons for this included time saving,22 shorter travel time,16,22 less time spent during consultation15 and more convenient appointment times.29 In addition, six studies demonstrated that total consultation time (including waiting time) was significantly less (p<0.05)14,15,25,26,28 or not significantly different (p = 0.50)23 compared with F2F.
Accuracy and validity of telemedicine examination
Four studies sought to determine the validity of telemedicine examination for use in diagnosis and patient-reported outcome measures (PROMs).27,29–31 Tachakra et al.31 evaluated 200 patients with minor trauma and compared accuracy of injury examination using telemedicine vs. a F2F review. Authors found a high accuracy of specific examination features using telemedicine with colour change accuracy of 97%, swelling or deformity of 98%, range of movement (ROM) of 95%, tenderness of 97% and weight bearing of 99%. Overtreatment of one injury and under-treatment of three injuries were reported using telemedicine. Another study comparing examination by home telemedicine vs. F2F consultation in 34 post- operative knee arthroscopy adolescents found no clinically significant difference in ROM, incision colour and effusion size examinations between the two methods of examination.29
Two studies also assessed the validity of PROMs using telemedicine.27,30 Goldstein et al.27 evaluated the shoulder Constant Score (CS) and compared scores using a smart phone (within a clinic setting) vs. F2F consultation in 47 patients. The mean difference in CS was a non-significant 0.53 points (95%CI –2.6 to 1.6) between the two methods, and authors concluded that telemedicine was valid and reliable in estimating shoulder function using CS scores. Another study evaluated the accuracy of the Oxford Shoulder Score and CS in 29 patients with surgically treated clavicle fractures and compared home Skype vs. clinic visit scores.30 Authors also reported a non-clinically significant mean difference in scores of 0.48 (95%CI –0.84 to –0.12) and 0.68 (95%CI –1.08 to –0.29), respectively, between the two methods. Other studies assessing clinician satisfaction have also reported high levels of satisfaction with physical examination of patients using telemedicine.14,18,22,32
Safety and patient outcomes
Eight studies assessed the safety of telemedicine or patient outcomes.14–16,18–20,24,34 Buvik et al.18 found no difference in self-reported serious events or complications between telemedicine and F2F (p = 0.26), similar to Lambrecht et al.34 Sathiyakumar et al.19 evaluated fracture management and reported one complication in each group; this included pyelonephritis in the F2F group and deep vein thrombosis (DVT) in the telemedicine group. It is unclear with regards to the association this had to their initial presentation.
Buvik et al.18 assessed planned clinic outcomes and found no significant difference in follow-up appointments (p = 0.06) or listing for surgery (p = 0.07) between telemedicine and F2F. They also reported that 27 out of 389 patients required specific F2F follow-up; three of these were due to physician dissatisfaction with telemedicine examination (11%), and the remainder due to the need for removal of osteosynthesis implants (48%), diagnostic injections (11%), CT scans (19%) and ‘other’ causes not specified (11%). Vuolio et al.20 similarly reported no difference in follow-up appointments, and found management plans were followed equally well in both groups with no observed difference in emergency department or unscheduled clinic visits.
A further study by Buvik et al.16 found no significant difference in F2F vs. telemedicine scores for European quality of life five-dimension index (EQ-5D) and European quality of life visual analogue scale (EQ-VAS) at baseline and 12-month follow-up of general orthopaedic patients. Sharareh and Schwarzkopf24 also found no significant difference in hip/knee disability and osteoarthritis outcome scores (HOOS p = 0.21; KOOS p = 0.37), EQ-5D (p = 0.41), Short Form survey (p≥0.29) or UCLA activity scores (p = 0.25) in their follow-up of hip/knee arthroplasty patients. Silva et al.15 assessed objective outcomes in children with non-displaced supracondylar fractures. They found no evidence of fracture displacement and no significant difference in changes of Baumann’s angle (p = 0.09), carrying angle (p = 0.11) or pain scores (p = 0.12) at 8-week follow-up between the two consultation methods. Kane et al.14 also assessed ROM and pain scores following rotator cuff repair and found no difference between telemedicine and F2F follow-up either.
Cost effectiveness
Five studies primarily assessed cost effectiveness of telemedicine versus traditional F2F consultations.17,21,25,28,33 Buvik et al.17 performed a prospective RCT with a detailed cost analysis of 389 patients comparing telemedicine vs. F2F consultations in Norway. Quality-adjusted life years (QALYs) and resource use were measured at baseline and 12-month follow-up, and no statistical significant difference was found in the QALYs gained between the two methods (p = 0.29). Authors found telemedicine cost €65 less per F2F consultation and concluded that telemedicine was cost effective from both a societal and health sector perspective if consults exceeded 151 and 183 consultations, respectively.
Another RCT performed a cost minimisation analysis of 145 patients and found with a workload of a hundred patients, telemedicine reduced both healthcare and patient costs by 23%.21 Greater distances travelled by patients to attend F2F appointments were noted to provide the most cost saving to patients utilising telemedicine. This was also supported by a simulated study for 207 bone oncology patients who calculated a healthcare and travel cost saving of 12.2% using telemedicine.28 In patients who had to travel from more than 400 km to visit the hospital in person, a cost reduction of 72% was calculated. Similar large cost savings of 45% were reported in primary care referrals to orthopaedics using telemedicine25 and a saving of £45,958 across 2 years for 630 post carpal tunnel decompression patients using telephone follow-up.33 Studies assessing patient satisfaction with telemedicine also support the finding of reduced patient and societal cost, with patients reporting reduced cost of travelling and less time off work to be motivating high satisfaction with telemedicine.16,19,22,23
Discussion
This systematic review aimed to determine current evidence for telemedicine in orthopaedic consultations. Results reveal that telemedicine can be an accurate, valid, cost effective, safe and acceptable if not a preferable method of consultation for patients and clinicians compared with F2F consultations. These findings have been demonstrated across a broad application of orthopaedic subspecialties within this literature review including paediatric and adult fracture care, elective orthopaedics, post-operative follow-up and orthopaedic oncology patients. This is in keeping with a recent mapping study of teleorthopaedic trends which also found that the most common utilisation of telemedicine was in joint arthroplasty, general post-operative care and fracture management.35
Patients revealed particularly high satisfaction with telemedicine for reasons of convenience, reduced appointment delays, travelling times, travel costs and time off work, findings which support existing literature on high patient satisfaction with telemedicine.36 Recent evidence also suggests that employing a regional telemedicine strategy by utilising telemedicine consultations with GPs, patients and orthopaedic specialists can significantly reduce referral wait time (reduced from 201.4 to 40 days in a region of Chile).37 Furthermore, studies within this review found cost savings were particularly magnified if patients had to travel significant distances to seek specialist opinion, required hospital transport, required a significant time away from work or another individual to accompany the patient to their appointment. Evidence also suggests that once patients had been exposed to telemedicine, the majority preferred further follow-up using this technology. High patient satisfaction may lead to increased patient compliance and reduced missed appointments, enabling further saving. Missed appointments cost the UK NHS £1 billion annually.38
Orthopaedic assessment relies heavily on patient examination, and thus accuracy and validity of patient examination when using telemedicine is vital. Existing literature has shown that that ROM in hips,39 knee,39,40 shoulder,41 elbow,41 wrist42 and hand43 can be reliably and accurately measured using telemedicine technology. Studies within this review have demonstrated no clinically significant differences in patient examination or PROMs using telemedicine. However, in a study which concluded telemedicine has good accuracy of examination, three injuries were found to be undertreated including a base of fifth metatarsal fracture and mallet injury, both of which have high a propensity of non-union.31 No authors reported significant differences in adverse events or reduced outcomes in patients using telemedicine vs. F2F consultations, although studies addressing this subject are minimal and lacking long-term follow-up.
The methodological quality of studies included in this review was variable. Studies included were likely to have an inherent selection bias, given that patients who agreed to participate in telemedicine studies were more likely to be more familiar with technology and more open to newer methods of consultation. In addition, patients who were unable to access telemedicine technology, had poor English proficiency or preferred not to undertake telemedicine consults were excluded from numerous studies, thus omitting a cohort of patients who perhaps were likely to be less satisfied with telemedicine.14,16,18,19 Given the unblinded nature of the studies, assessors’ or patients’ motivations to undertake telemedicine consultations may have affected the outcome of results.
Three RCTs, based upon the same study protocol, were found to have high risk of bias in the randomisation process. At the request of staff, some patients who required ambulance transport to attend for a F2F consultation were excluded from randomisation and examined using telemedicine.20–22 Furthermore, studies assessing patient/clinician satisfaction used their own non-validated questionnaires, as no universal and tested satisfaction measure exists, therefore affecting validity of results. Other studies assessed to be of low quality, using JBI appraisal tools, failed to address confounding factors such as dissimilar patient follow-up between telemedicine and F2F consultations24 or lengthy time periods (up to 2 weeks) between the two methods where patient condition could change.32
Further work exploring long-term outcomes of patients utilising telemedicine, validity of various patient examinations and PROMs is required with large, high-quality RCTs and longer follow-up. Moreover, a validated measure to assess clinician and patient satisfaction is needed for reliability and comparability of study results. Many of our included studies involved remote joint consultations whereby a primary care physician and/or specialist nurse with the patient would perform a telemedicine consultation with the specialist. Further studies are needed to determine whether telemedicine consultations from the patient’s own home are truly reliable and achievable.
There are some limitations within our systematic review. Although nine out of 21 studies were RCTs, we also included cohort studies, cross-sectional studies and case series, providing lower quality evidence. Nevertheless our findings were supported equally from all levels of evidence, and including these studies allowed us to provide a greater breadth of findings. Given that there is no agreed definition of telemedicine, with at least 104 definitions in peer-reviewed literature,44 it is possible we may have missed some search terms, limiting the number of articles included. In addition, heterogeneity of patient populations and orthopaedic pathology within the included studies means direct comparison of results is difficult and therefore challenging to determine the true scope of telemedicine within orthopaedics. However, including a variety of orthopaedic pathology provides a current insight into the broad application of telemedicine within orthopaedic subspecialties.
Several issues with orthopaedic related telemedicine still remain to be addressed. A qualitative study by Caffery et al.45 interviewed staff from nine teleorthopaedic services across Australia, identifying barriers and enablers to the implementation and running of teleorthopaedic services. Barriers included initial disruption and redesigning of care processes, cost of implementation, difficulty in obtaining imaging from multiple imaging providers and staff resistance.45 Furthermore, multiple medico-legal and ethical concerns still persist such as the liability of clinicians performing remote examinations/diagnoses, responsibility of privacy and confidentiality and the potential requirement of chaperones during telemedicine consultations.46 This has prompted the General Medical Council to produce ethical guidance for clinicians to manage patient risk safely during the current pandemic.47 Nonetheless, there are already reports in the literature of the rapid adoption of telemedicine within orthopaedics because of the present circumstances,48,49 a move supported by large reputable national associations such as the BOA and AAOS.9,10 Given the current necessity of telemedicine, the orthopaedic community will have to adapt to an era of increased digital consultation, expanding our understanding of telemedicine capabilities and providing further evidence on the performance of telemedicine. Shared experiences from colleagues will help us to maximise telemedicine effectiveness, such as Tanaka et al.50 who have produced virtual orthopaedic examination protocols for the major body joints during their COVID-19 experience of telemedicine consultation.
Conclusion
There is variable evidence to suggest that telemedicine within orthopaedic consultations can be safe, cost effective, valid in clinical assessment, and with high patient and clinician satisfaction. However, more high-quality evidence is required, with stricter methodology to elucidate long-term outcomes. This systematic review presents up-to-date evidence on the use of telemedicine in orthopaedics and provides objective data for organisations considering the utilisation of telemedicine within the current COVID-19 pandemic and in the future.
Supplemental Material
Supplemental material, sj-pdf-1-jtt-10.1177_1357633X20938241 for Telemedicine in orthopaedics and its potential applications during COVID-19 and beyond: A systematic review by Zakir Haider, Bashaar Aweid, Padmanabhan Subramanian and Farhad Iranpour in Journal of Telemedicine and Telecare
Declaration of conflicting interests
The authors declare no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding
The authors received no financial support for the research, authorship, and/or publication of this article.
ORCID iD
Zakir Haider https://orcid.org/0000-0002-4049-8363
Supplemental material
Supplemental material for this article is available online.
References
- 1.Bashshur RL.On the definition and evaluation of telemedicine. Telemed J 1995; 1(1): 19–30. [DOI] [PubMed] [Google Scholar]
- 2.Boxer R.Telemedicine in a global context. MHealth 2015; 1: 12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Castaneda P, Ellimoottil C.Current use of telehealth in urology: A review. World J Urol 2019. [DOI] [PubMed] [Google Scholar]
- 4.Minion DJ, Sprang R, Endean ED.A review of telemedicine in vascular surgery. Minerva Chir 2002; 57(2): 237–244. [PubMed] [Google Scholar]
- 5.Vyas KS, Hambrick HR, Shakir A, et al. A systematic review of the use of telemedicine in plastic and reconstructive surgery and dermatology. Ann Plast Surg 2017; 78(6): 736–768. [DOI] [PubMed] [Google Scholar]
- 6.Cottrell MA, Galea OA, O’Leary SP, et al. Real-time telerehabilitation for the treatment of musculoskeletal conditions is effective and comparable to standard practice: A systematic review and meta-analysis. Clin Rehabil 2017; 31(5): 625–638. [DOI] [PubMed] [Google Scholar]
- 7.WHO. Coronavirus disease 2019, Situation Report – 51. 2020. Available at: https://www.who.int/docs/default-source/coronaviruse/situation-reports/20200311-sitrep-51-covid-19.pdf?sfvrsn=1ba62e57_10.
- 8.Kissler SM, Tedijanto C, Goldstein E, et al. Projecting the transmission of dynamic of SARS-COV-2 through the postpandemic period. J Sci 2020. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.BOA. COVID -19 British Orthopaedic Association Standards for Trauma. Management of patients with traumatic injuries and urgent orthopaedic conditions treated as outpatients during the coronavirus pandemic. 2020. Available at: https://www.boa.ac.uk/uploads/assets/ee39d8a8-9457-4533-9774e973c835246d/4e3170c2-d85f-4162-a32500f54b1e3b1f/COVID-19-BOASTs-Combined-FINAL.pdf
- 10.Bracy C, Willer J. AAOS. Stay updated on COVID-19- related telemedicine guidelines. 2020. Available at: https://aaos.org/aaosnow/2020/apr/covid19/covid-19–telemedicine-tips/
- 11.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. PloS Med 2009; 6(7): e1000097. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Sterne JAC, Savović J, Page MJ, et al. RoB 2: A revised tool for assessing risk of bias in randomised trials. BMJ 2019; 366: l4898. [DOI] [PubMed] [Google Scholar]
- 13.Moola S, Munn Z, Tufanaru C, et al. Systematic reviews of aetiology and risk. In: Aromataris E, Munn Z (eds) Joanna Briggs Institute Reviewer’s Manual. The Joanna Briggs Institute, 2017, Ch. 7. Available from https://reviewersmanual.joannabriggs.org/
- 14.Kane LT, Thakar O, Jamgochian G, et al. The role of telehealth as a platform for postoperative visits following rotator cuff repair: A prospective, randomized controlled trial. J Shoulder Elbow Surg 2020; 29(4): 775–783. [DOI] [PubMed] [Google Scholar]
- 15.Silva M, Delfosse EM, Aceves-Martin B, et al. Telehealth: A novel approach for the treatment of nondisplaced pediatric elbow fractures. J Pediatr Orthop B 2019; 28(6): 542–548. [DOI] [PubMed] [Google Scholar]
- 16.Buvik A, Bugge E, Knutsen G, et al. Patient reported outcomes with remote orthopaedic consultations by telemedicine: A randomised controlled trial. J Telemed Telecare 2019; 25(8): 451–459. [DOI] [PubMed] [Google Scholar]
- 17.Buvik A, Bergmo TS, Bugge E, et al. Cost-effectiveness of telemedicine in remote orthopaedic consultations: randomised controlled trial. J Med Internet Res 2019; 21(2): e11330. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Buvik A, Bugge E, Knutsen G, et al. Quality of care for remote orthopaedic consultations using telemedicine: A randomised controlled trial. BMC Health Serv Res 2016; 16: 483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Sathiyakumar V, Apfeld JC, Obremskey WT, et al. Prospective randomized controlled trial using telemedicine for follow-ups in an orthopaedic trauma population: A pilot study. J Orthop Trauma 2015; 29(3): e139–e145. [DOI] [PubMed] [Google Scholar]
- 20.Vuolio S, Winblad I, Ohinmaa A, et al. Videoconferencing for orthopaedic outpatients: One-year follow-up. J Telemed Telecare 2003; 9(1): 8–11. [DOI] [PubMed] [Google Scholar]
- 21.Ohinmaa A, Vuolio S, Haukipuro K, et al. A cost-minimization analysis of orthopaedic consultations using videoconferencing in comparison with conventional consulting. J Telemed Telecare 2002; 8(5): 283–289. [DOI] [PubMed] [Google Scholar]
- 22.Haukipuro K, Ohinmaa A, Winblad I, et al. The feasibility of telemedicine for orthopaedic outpatient clinics – a randomised controlled trial J Telemed Telecare 2000; 6(4): 193–198. [DOI] [PubMed] [Google Scholar]
- 23.Sinha N, Cornell M, Wheatley B, et al. Looking through a different lens: Patient satisfaction with telemedicine in delivering paediatric fracture care. J Am Acad Orthop Surg Glob Res Rev 2019; 3(9): e100. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Sharareh B, Schwarzkopf R.Effectiveness of telemedical applications in postoperative follow-up after total joint arthroplasty. J Arthroplasty 2014; 29(5): 918–922. [DOI] [PubMed] [Google Scholar]
- 25.Harno K, Arajarvi E, Paavola T, et al. Clinical effectiveness and cost analysis of patient referral by videoconferencing in orthopaedics. J Telemed Telecare 2001; 7(4): 219–225. [DOI] [PubMed] [Google Scholar]
- 26.Sultan A, Acuna A, Samuel L, et al. Utilization of telemedicine virtual visits in pediatric spinal defomory patients: A comparison of feasibility and patient satisfaction at a large academic center. J Pediatr Orthop 2020. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 27.Goldstein Y, Schermann H, Dolkart O, et al. Video examination via the smartphone: A reliable tool for shoulder function assessment using the constant score. J Orthop Sci 2019; 24(5): 812–816. [DOI] [PubMed] [Google Scholar]
- 28.Aponte-Tinao LA, Farfalli GL, Albergo JI, et al. Face to face appointment vs telemedicine in first time appointment orthopedic oncology patients: A cost analysis. Stud Health Technol Inform 2019; 264: 512–515. [DOI] [PubMed] [Google Scholar]
- 29.Abel K, Baldwin K, Chuo J, et al. Can telemedicine be used for adolescent postoperative knee arthroscopy follow-up? JBJS JOPA 2017; 5(4): e26. [Google Scholar]
- 30.Good DW, Lui DF, Leonard M, et al. Skype: A tool for functional assessment in orthopaedic research. J Telemed Telecare 2012; 18(2): 94–98. [DOI] [PubMed] [Google Scholar]
- 31.Tachakra S, Lynch M, Newson R, et al. A comparison of telemedicine with face-to-face consultations for trauma management. J Telemed Telecare 2000; 6: 178–181. [DOI] [PubMed] [Google Scholar]
- 32.Aarnio P, Lamminen H, Lepisto J, et al. A prospective study of teleconferencing for orthopaedic consultations. J Telemed Telecare 1999; 5(1): 62–66. [DOI] [PubMed] [Google Scholar]
- 33.Williams M, Amin A, Getgood A, et al. Telephone clinic follow-up following carpal tunnel decompression. J Hand Surg Eur Vol 2008; 33(5): 641–644. [DOI] [PubMed] [Google Scholar]
- 34.Lambrecht CJ, Canham WD, Gattey PH, et al. Telemedicine and orthopaedic care. A review of 2 years of experience. Clin Orthop Relat Res 1998; 348: 228–232. [PubMed] [Google Scholar]
- 35.Behmanesh A, Sadoughi F, Mazhar F, et al. Tele-orthopaedics: A systematic mapping study. J Telemed Telecare 2020; [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 36.Kruse CS, Krowski N, Rodriguez B, et al. Telehealth and patient satisfaction: A systematic review and narrative analysis. BMJ Open 2017; 7: e016242. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Prada C, Izquierdo N, Traipe R, et al. Results of a new telemedicine strategy in traumatology and orthopedics. Telemed J E Health 2020; 26(5); 665–670. [DOI] [PubMed] [Google Scholar]
- 38.NHS Benchmarking Network. 2019 Outpatients project- results published. 2019. Available at: https://www.nhsbenchmarking.nhs.uk/news/2019-outpatients-project-results-published.
- 39.Russo RR, Burn MB, Ismaily SK, et al. Is digital photography an accurate and precise method for measuring range of motion of the hip and knee? J Exp Orthop 2017; 4(1): 29. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Mica MC, Wagner ER, Shin AY.Smartphone photography as a tool to measure knee range of motion. J Surg Orthop Adv 2018; 27(1): 52–57. [PubMed] [Google Scholar]
- 41.Russo RR, Burn MB, Ismaily SK, et al. Is digital photography an accurate and precise method for measuring range of motion of the shoulder and elbow? J Orthop Sci 2018; 23(2): 310–315. [DOI] [PubMed] [Google Scholar]
- 42.Wagner ER, Mica MC, Shin AY.Smartphone photography utilized to measure wrist range of motion. J Hand Surg Eur Vol 2018; 43(2): 187–192. [DOI] [PubMed] [Google Scholar]
- 43.Zhao JZ, Blazar PE, Mora AN, et al. Range of motion measurements of the fingers via Smartphone photography. Hand NY 2019; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Sood S, Mbarika V, Jugoo S, et al. What is telemedicine? A collection of 104 peer-reviewed perspectives and theoretical underpinnings. Telemed J E Health 2007; 13(5): 573–590. [DOI] [PubMed] [Google Scholar]
- 45.Caffery L, Taylor M, North J, et al. Tele-orthopaedics: A snapshot of services in Australia. J Telemed Telecare 2017; 23(10): 835–841. [DOI] [PubMed] [Google Scholar]
- 46.Stanberry B.Legal and ethical aspects of telemedicine. J Telemed Telecare 2006; 12(4): 166–175. [DOI] [PubMed] [Google Scholar]
- 47.General Medical Council. Ethical Hub- Remote consultations. 2020. Available at: https://www.gmc-uk.org/ethical-guidance/ethical-hub/remote-consultations
- 48.Rao SS, Loeb AE, Amin RM, et al. Establishing telemedicine in an academic total joint arthroplasty practice: Needs and opportunities highlighted by the COVID-19 pandemic. Arthroplast Today 2020; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Stinner D, Lebrun C, Joseph R, et al. The orthopaedic trauma service and COVID-19: Practice considerations to optimize outcomes and limit exposure . J Orthop Trauma 2020; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Tanaka MJ, Oh LS, Martin SD, et al. Telemedicine in the era of COVID-10: The virtual orthopaedic examination. J Bone Joint Surg AM 2020; [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-pdf-1-jtt-10.1177_1357633X20938241 for Telemedicine in orthopaedics and its potential applications during COVID-19 and beyond: A systematic review by Zakir Haider, Bashaar Aweid, Padmanabhan Subramanian and Farhad Iranpour in Journal of Telemedicine and Telecare