Abstract
Objective:
A large body of research has shown that alcohol use, drug use, aggression, and self-harm often co-occur within the same individuals, suggesting the possibility of shared etiologies. Research has yet to determine the factor structure of these dysregulated behaviors.
Method:
Participants (Mage = 40.33; 74% women) completed self-report and interview-based measures of dysregulated behaviors (alcohol use, drug use, aggression, and self-harm), emotion dysregulation, maladaptive personality traits, and symptoms of DSM disorders (e.g., borderline personality disorder, depression).
Results:
Results showed support for a bifactor model (i.e., all indicators load on a common dysregulated behavior factor and on unique alcohol, drug, aggression, and self-harm factors), which provided a better fit to the data than other models. In line with our hypotheses, the general dysregulated behavior factor was positively associated with emotion regulation difficulties, negative affect, and BPD symptoms.
Conclusions:
These results have implications for several areas of psychopathology and intervention research.
Keywords: Self-injury, Binge Drinking, Violence, Emotional Dysregulation
A large body of research has shown that behaviors such as alcohol use, drug use, aggression, and self-harm often co-occur within the same individuals (Kingston et al., 2011; Guo et al., 2017; Sadeh & Baskin-Sommers, 2017). Research also shows that engagement in one behavior (e.g., alcohol intoxication) increases the likelihood of other behaviors (self-harm, aggression; Bresin & Mekawi, 2020; Duke et al., 2017). These findings combined with overlap in theories of drug and alcohol use, aggression, and self-harm (e.g., negative reinforcement; Baker et al., 2004; Conger, 1956, Chapman, Gratz, & Brown, 2006; Hokanson, 1974) suggests the possibility of common etiological factors. These dysregulated behaviors have serious consequences for both the individual engaging in the behaviors, those around them, and society as a whole. Thus, understanding the points of convergence and divergence across these behaviors has the potential to improve etiological models of psychopathology and inform the development of transdiagnostic interventions designed to reduce the frequency of these behaviors. Determining an empirical taxonomy of these dysregulated behaviors is necessary to guide etiological research elucidating their unique and shared functions. Therefore, the goal of this study was to test competing factor structures of a subset of dysregulated behaviors and establish the nomological network of these factors in relation to emotion dysregulation, maladaptive personality traits, and symptoms of psychopathology.
Bresin (2020; also see Selby & Joiner, 2009) defines dysregulated behaviors as active behaviors that have benefits (e.g., reduction in negative affect) in the short-term (seconds to hours) but cause serious distress or impairment to the individual and/or those around them in the long-term (days, weeks, years). Dysregulated behaviors are proposed to be a subset of avoidance behaviors and impulsive behaviors and can be distinguished from compulsive behaviors (e.g., Guo et al., 2017) and thrill-seeking behaviors (Bresin, 2020). Although the term dysregulated behavior comes from research on borderline personality disorder (BPD; Selby & Joiner, 2009), these behaviors occur in a broader population of individuals and, therefore, represent a transdiagnostic phenomenon (Bresin, 2020).
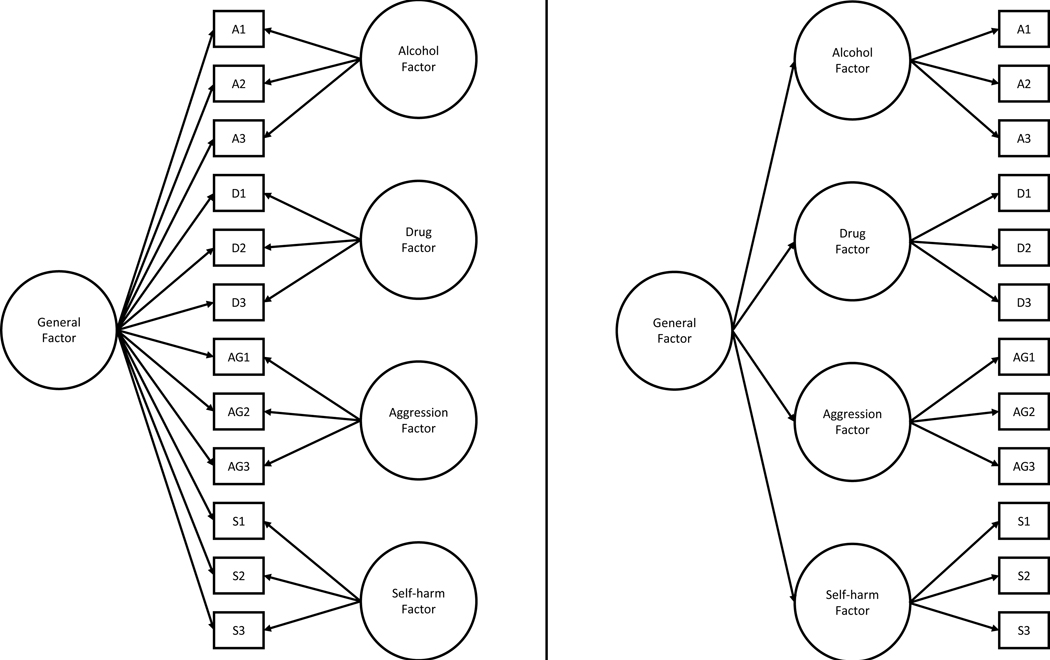
Although it has been established that these behaviors co-occur, the specific factor structure is yet to be determined (Kingston et al. 2011; Sadeh & Baskin-Sommers, 2017). One possibility is that there is one common vulnerability (or vulnerabilities) that underlie all dysregulated behaviors, and there are no unique vulnerabilities for specific behaviors. This would be consistent with a higher-order factor model (see Figure 1 right panel), where the covariance among factors is explained by a higher-order factor (Markon, 2019). Kingston et al. (2011) found evidence for a higher-order model of dysregulated behaviors, where a general dysregulated behavior factor was indicated by eight lower-order factors (e.g., self-harm, drug use, excessive alcohol use, and aggression). Another possibility is that there is one common vulnerability that applies to all dysregulated behaviors and separate unique vulnerabilities that apply to specific behaviors. This would be consistent with a symmetrical bifactor model (Markon, 2019), where all indicators load on a common factor and on unique factors (see Figure 1, left panel). Sadeh and Baskin-Sommers (2017) found support for a bifactor model of their 38-item Risk, Impulsive, and Self-destructive Behavior Questionnaire, where all items loaded on a general factor with eight specific factors (e.g., drug-related behavior, self-harm, aggression, and heavy alcohol use).
Figure 1.
Conceptual Models for the Symmetric Bifactor Model (left panel) and Higher-order Model (right panel)
Note. A1-A3 = Alcohol Indicator 1–3; D1-D3 = Drug Indicator 1–3; AG1-AG3 = Aggression Indicator 1–3; S1-S3 = Self-harm Indicator 1–3.
These preliminary factor structure studies provide some clues to the underlying nature of dysregulated behaviors; however, several questions remain. First, because one study supports each model (e.g., Kingston et al., 2011; Sadeh & Baskin-Sommers, 2017), there is no clear evidence to support one model over the other. Second, neither study compared a higher-order factor to a bifactor model (Kingston et al., 2011; Sadeh & Baskin-Sommers, 2017), which could provide support for one model over another. Given that the correlations between dysregulated behaviors are moderate and individuals who engage in one do not necessarily engage in all dysregulated behaviors (e.g., Kingston et al., 2011), it could be assumed that there would be common and unique factors that contributed to dysregulated behaviors. This may suggest a that a bifactor model would best fit the data. Third, these studies used primarily White samples with high educational attainment, which can limit generalizability. Finally, there has been limited work elucidating the nomological network (i.e., the pattern of relations among antecedent, mediator, and outcome variables; Hagger et al., 2017) of the shared variance of dysregulated behaviors (see Sadeh & Baskin-Sommers, 2017 for an example).
Nomological Network of Dysregulated Behaviors
Establishing the correlates of common and unique factors of dysregulated behaviors (i.e., the nomological network) can inform theory development. For example, identifying the nomological network of the common factor would aid in the development of an etiological model common to all dysregulated behaviors. Similarly, identifying correlates of unique factors, if identified, could lead to the development of etiological theories unique to specific behaviors that could be used to develop more effective interventions for dysregulated behaviors. Although there are several candidate correlates, we focused on emotion dysregulation, personality, and symptoms of psychopathology because of their inclusion in theories of substance use, self-harm, and aggression (e.g., Chapman et al., 2006; Selby & Joiner, 2009).
Emotion Dysregulation
Emotion dysregulation is a factor common to theories of dysregulated behaviors (e.g., Bresin, 2020; Selby & Joiner, 2009). For example, Selby and Joiner (2009) posit that individuals engage in dysregulated behaviors to deal with uncontrollable unpleasant emotions. This suggests that emotion dysregulation may contribute to several dysregulated behaviors. Along these lines, self-reported difficulties in regulating emotions have been found to correlate positively to individual dysregulated behaviors in separate studies (e.g., alcohol use, aggression: Grigorian et al., 2020; self-harm: Wolff et al., 2019) and within the same study (Buckholdt et al., 2015; Miller & Racine, 2020). Moreover, there is some evidence that, at least when ignoring overlap among behaviors, self-harm and alcohol use are more strongly related to different aspects of emotion dysregulation (e.g., difficulties engaging in goal-directed behaviors when upset) than drug use (Buckholdt et al., 2015; Miller & Racine, 2020). It is currently unclear whether these unique associations would be maintained when common variance across dysregulated behaviors is accounted for.
Maladaptive Personality Traits
Research using several instruments in clinical (e.g., Samuel et al., 2010) and normal range of personality (e.g., Goldberg, 1999) has coalesced on a five-factor model of personality traits. The traits range from normal to maladaptive, with the maladaptive extremes being negative affectivity, disinhibition, antagonism, detachment, and psychoticism. Maladaptive personality traits can be linked to symptoms of psychopathology (Widiger et al., 2019). For example, the Hierarchical Taxonomy of Psychopathology (Hi-TOP; Kotov et al., 2017), a recently proposed alternative to the 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5; American Psychiatric Association, 2013), explains co-occurring symptoms (e.g., depression and post-traumatic stress disorder [PTSD]) by identifying higher-order factors (or spectra) that map on to the maladaptive personality traits (e.g., negative affectivity; Kotov et al., 2017).
The Hi-TOP may be used to develop several predictions about how common and unique variance in dysregulated behaviors may be associated with maladaptive personality traits. First, given that negative affectivity has been shown to positively relate to the common variance across many forms of psychopathology (e.g., Caspi et al., 2014), it could be assumed that the shared variance in dysregulated behaviors would have a positive relation with negative affectivity. Second, the Hi-TOP places substance use disorders underneath the disinhibited externalizing spectra, suggesting that substance use may be uniquely related to disinhibition. Third, the Hi-TOP predicts that disorders characterized by aggression (e.g., intermittent explosive disorder, antisocial personality disorder) are a function of the antagonistic externalizing spectra. This suggests that aggression may be uniquely related to antagonism. Finally, although self-harm is not directly modeled in the Hi-TOP, given the strong positive relation between self-harm and BPD, depression, PTSD, and eating disorders (e.g., Bentley et al., 2015; Cucchi et al. 2016), it could be posited that self-harm may be uniquely related to negative affectivity. This fits with studies showing that negative affectivity is positively related to self-harm (e.g., Brown, 2009).
Symptoms of Psychopathology
Within the DSM-5, dysregulated behaviors are most prominently represented in the symptoms of BPD. Specifically, alcohol and drug use, aggression, and self-harm are included in the symptoms of BPD. Thus, it is likely that the general dysregulated behavior factor would be strongly positively associated with symptoms of BPD. In line with this prediction, Sadeh and Baskin-Sommers (2017) found that their general factor and unique factors were positively correlated with self-reported BPD symptoms. Several other DSM diagnoses (e.g., major depression, PTSD, and panic disorder) have been found to have positive relations with alcohol and drug use (e.g., Cosci et al., 2007; Lai et al., 2015; Mills et al., 2006), aggression (e.g., Dutton & Karakanta, 2013; Jakupack et al., 2007), and self-harm (e.g., Bentley et al., 2015; Fox et al., 2015; Kimbrel et al., 2016). Currently, it is unknown whether these correlations may be explained by a common dysregulated behavior factor or whether there may be unique associations between some dysregulated behaviors and symptoms of psychopathology.
Current Study
Previous research has shown that there is significant co-occurrence of dysregulated behaviors such as problematic drug and alcohol use, aggression, and self-harm (Kingston et al., 2011; Sadeh & Baskin-Sommers, 2017); however, very few studies have examined the factor structure of dysregulated behaviors and established the common and unique correlates. Moreover, the studies that have examined the factor structure have not directly compared higher-order and bifactor models. The goal of this study was to examine the factor structure of a subset of dysregulated behaviors (i.e., those with the highest societal impact; Bresin, 2020) in a sample with a high likelihood for endorsement of dysregulated behaviors (i.e., a large urban-dwelling, trauma-exposed sample). The sample was also more racially diverse than those used in previous studies. Based on previous research showing that the correlations between dysregulated behaviors are moderate and individuals who engage in one do not necessarily engage in all dysregulated behaviors (e.g., Kingston et al., 2011), we tentatively predicted that a bifactor model would be the better fit to the data than a higher-order or correlated factor model. After determining the best fitting solution, we extracted factor scores and examined their relations with several correlates (i.e., emotion dysregulation, maladaptive personality traits, symptoms of BPD, depression, PTSD, and panic disorder) to establish construct validity. We predicted that the general dysregulated behaviors factor would be positively correlated with emotion dysregulation, BPD symptoms, and negative emotionality (Kotov et al., 2017; Selby & Joiner, 2009). We explored the relation between the general factor and symptoms of depression, PTSD, and anxiety sensitivity. In terms of unique factors, we predicted that the unique drug and alcohol use factor would be positively correlated with disinhibition, the unique aggression factor would be positively correlated with antagonism, and the unique self-harm factor would be positively correlated with negative emotionality (Kotov et al., 2017).
Method
Procedure
The current study focuses on a secondary analysis of data collected from January 2006 through February 2020 as part of a larger NIH-funded study on the risk factors for the development of PTSD in a urban population with low socioeconomic resources. Participants were recruited from waiting rooms in the gynecology and primary care medical clinics at a publicly-funded hospital and the emergency department waiting room of a pediatric, non-profit hospital in Atlanta, Georgia. We did not narrow recruitment to specific criteria but approached any individual in the waiting room. To be eligible for participation, participants had to be at least 18 years old and able to give informed consent. After signing the informed consent approved by the university and hospital ethics review boards, an interview was administered with questionnaires regarding trauma history and psychological variables. Trained research assistants administered this interview (approximately 45–75 min). More comprehensive assessments of psychological functioning were conducted in a separate associated study drawn from the pool of participants who completed the initial assessment. Participants were compensated for their time.
Participants
Although the n’s varied from measure to measure, the current sample included 3,707 adults who ranged from 18 to 65 years old (M = 40.33; SD = 13.17). The majority of the sample identified as female (74%) and non-Hispanic/Latinx (98%). The racial breakdown of the sample was as follows: 93% African American, 3% Caucasian/White, 2% mixed race, 1% Latinx, and 1% other. In terms of highest level of education achieved, 21% reported not completing a high school degree, 40% reported completing high school or GED, and 39% reported completing at least some college or technical school. Approximately 68% of the sample indicated they were currently unemployed, and the majority reported a monthly household income of less than $2,000/month (83%). The full battery of measures was changed periodically during the 14 years of data collection; therefore, the number of participants for each measure varies.
Measures
Dysregulated Behaviors
Alcohol Use Disorders Identification Test (AUDIT; de Meneses-Gaya et al., 2009).
The AUDIT is a 10-item self-report screening instrument for problematic alcohol use occurring in the last year. Items on the AUDIT assess both consumption (e.g., “How often did you have a drink containing alcohol?”) and consequences (e.g., “How often have you failed to do what was normally expected of you because of drinking?”), and responses are coded on a 0 (never) to 4 (daily or almost daily) scale. The total score (M = 9.81, SD = 9.72) was used in the current study (α = .88), and data were available for N = 3,707 participants.
Drug Abuse Screening Test (DAST; Yudko et al., 2007).
The DAST is a 10-item self-report measure of current and lifetime substance use (excluding alcohol) and associated problems (e.g., “Have you had blackouts as a result of drug use?”) which participants responded on a dichotomous scale of 0 (no) and 1 (yes). Items were summed to create a total score (M = 3.32, SD = 2.82, α = .77) for lifetime use, and data were available for N = 3,621 participants.
Behavior Questionnaire-Short (BQ-S; Gillikin et al., 2016).
The BQ-S is an internally constructed 5-item scale designed to assess aggressive behavior frequency. This measure was based on the Conflicts Tactics Scale (Straus et al., 1996), a measure commonly used to assess aggressive behavior. Items from the BQ-S ask participants how often in their lifetime they have perpetrated violent acts (e.g., punched, hit, pulled a knife or gun, stabbed, or shot at someone) using a scale of 0 (never) to 4 (more times than I can count). The sum was computed to obtain the total score (M = 4.49, SD = 3.72, α = .76), and data were available for N = 2,968 participants.
Suicide and Self-Harm (SSH).
The SSH is an internally constructed, face valid 4-item scale designed to assess the frequency of suicidal behaviors. Items from the SSH ask participants how often they have engaged in various self-harm behaviors (e.g., intentionally putting oneself in harm’s way, intentionally hurting oneself without suicidal intent, being hospitalized for suicidal ideation, and attempting suicide) using a scale of 0 (never) to 4 (more times than I can count). We focused on the two items more directly tied to self-harm (intentionally hurting oneself without suicidal intent and attempting suicide). The items were summed to obtain the total score (M = 0.36, SD = 0.98, α = .60), and data were available for N = 1,889 participants.
Measures: Construct Validity
Emotion Dysregulation
Difficulties in Emotion Regulation Scale (DERS; Gratz & Roemer, 2003).
The DERS is a psychometrically valid 36-item self-report measure that assesses problems with emotion regulation. Participants rated items on a scale of 1 (almost never, 0–10%) to 5 (almost always, 91–100%). The DERS includes six subscales, including attention to and awareness of emotions (e.g., “I pay attention to how I feel;” reverse-scored; α = .74), acceptance of one’s emotions (e.g., “When I’m upset, I become angry with myself for feeling that way; α = .89), the ability to execute goal-directed behavior (e.g., “When I’m upset, I have difficulty focusing on other things; α = .83), the ability to inhibit impulsive behavioral urges (e.g., “I experience my emotions as overwhelming and out of control,” α = .86), access to contextually appropriate emotion regulation strategies (e.g., “When I’m upset, it takes me a long time to feel better;” α = .88) and clarity into one’s emotional state (e.g., “I have no idea how I am feeling;” α = .79). Items were summed to create each subscale data were collected for N = 599–600 participants.
Maladaptive Personality Traits/(Hi -TOP Spectra)
Personality Inventory for DSM-5-Brief Form (PID-5-BF; Anderson et al., 2018).
The PID-5-BF is a 25-item self-report measure of pathological personality traits included in the DSM-5 Alternative Model of personality disorder. Participants indicated how much each item described themselves on a scale of 1 (very false or often false) to 4 (very true or often true). All five subscales of the PID-5-BF were included as follows: negative affect (e.g., “I get emotional easily, often for very little reason;” α = .82), detachment (e.g., “I often feel like nothing I do really matters;” α = .76), antagonism (e.g., “I use people to get what I want;” α = .52), disinhibition (e.g., “I’m not good at planning ahead;” α = .52) and psychoticism (e.g., “I have seen things that weren’t really there;” α = .69). The items were summed to obtain each subscale score and data were available for N = 384 participants.
Symptoms of Psychopathology
Structured Clinical Interview for DSM-IV (e.g., SCID-IV; First & Gibbon, 2004).
The SCID-IV was used to assess BPD symptoms (e.g., “Inappropriate, intense anger or difficulty controlling anger) using a semi-structured interview. Participants received a symptom score (i.e., = no evidence of symptom, 2 = sub-threshold, 3 = symptom present) based on the extent to which they were able to provide examples of each symptom from on their personal experiences. The items were summed to obtain the total score (α = .87), and data were available for N = 326 participants.
Beck Depression Inventory-II (BDI-II; Beck et al., 1996).
The BDI-II is a reliable and well-validated 21-item measure used to assess depressive symptoms. For each item, participants indicated which of four statements best described the way they had been feeling over the past two weeks. Each statement had a corresponding score, ranging from 0 (e.g., “I do not feel sad”) to 3 (e.g., “I am so sad or unhappy that I can’t stand it”). The scores were summed to create a total depressive symptom severity score (α = .93), and data were available for N = 3,246 participants.
MINI International Neuropsychiatric Interview (MINI; Sheehan et al., 1998).
The MINI for DSM-IV-TR is a validated and reliable structured diagnostic interview that assesses mood, anxiety, substance use, and psychotic disorders). In this study, we used the depressive disorders module, which assesses symptoms of a major depressive episode (e.g., appetite changes, changes in sleep). Participants received a symptom score (i.e., 0 = symptom absent, 1 = symptom present) based on the extent to which they were able to provide examples of each symptom occurring within a two-week period and confirm that this experience deviated from typical behavior. Data were collected from N = 411 for current and N = 383 for past.
Modified Posttraumatic Stress Disorder Symptom Scale (mPSS; Falsetti et al., 1993).
The mPSS is a reliable and well-validated 17-item measure used to assess current PTSD symptoms based on DSM–IV–TR (American Psychiatric Association, 2000) criteria. Participants indicated the degree to which they experienced symptoms (e.g., “persistently been making efforts to avoid thoughts or feelings associated…?”) regarding traumatic experiences on a scale of 0 (not at all) to 3 (five or more times a week). Scores were summed to create a total score (α = .92), and data were collected from N = 3,168 participants.
Clinician-Administered PTSD Scale (CAPS; Blake et al., 1995; Weathers et al., 2001).
The CAPS is a psychometrically valid, standardized interviewer-administered diagnostic instrument for current PTSD based on DSM criteria. The CAPS for DSM-IV and DSM-5 were both used in this study (the adoption of CAPS-5 occurred upon its release). A sum of PTSD symptoms based on CAPS items was used as the measure of PTSD symptoms. In order to combine CAPS-IV and CAPS-5, all scores were weighted to balance 1) differences in the number of items (17 for CAPS-IV and 20 for CAPS-5), and 2) differences in scoring (for CAPS-IV frequency and intensity scores were separated while for CAPS-5 scoring frequency and intensity scores were combined into one severity rating on a scale of 0 (absent) to 4 (extreme/incapacitating)). The severity rating is derived based on the scores for frequency and intensity for each item, which are still scored separately for each item, and thus represents the same components of the ratings as CAPS-IV (Weathers et al., 2018). Interrater reliability (IRR) in this sample has been previously reported and has shown good IRR for current diagnosis of PTSD (k = 0.83). Data were collected from N = 839 participants.
Anxiety Sensitivity Inventory (ASI; Peterson & Heilbronner, 1987).
The ASI is a 16-item self-report inventory of sensitivity to symptoms of anxiety. The ASI is thought to measure the fear of internal body sensations central to panic disorder (e.g., McNally, 2002). Participants indicated the degree to which they experienced anxiety sensitivity (e.g., “When I notice that my heart is beating rapidly, I worry that I might have had a heart attack”) on a scale of 0 (very little) to 4 (very much). Scores were summed to create a total score (α = .89), and data were collected from N = 3,003 participants.
Results
Data Analytic Plan
Data analysis proceeded in two stages. In the first stage, we fit four factor analytic structural equation models: 1) a four-factor model where alcohol use, drug use, aggression, and self-harm were separate correlated factors, 2) a three-factor model where alcohol and drug use, aggression, and self-harm, were separate correlated factors, 3) a higher-order model, where alcohol use, drug use, aggression, and self-harm were indicators of a higher-order dysregulated behavior factor, and 4) a fully symmetric bifactor model where all items indicated a general dysregulated behavior factor and four unique factors (alcohol use, drug use, aggression, and self-harm). Models were compared on their fit statistics (CFI, TFI, SRMR, RMSEA) to determine the best fitting model. We used threshold values recommended by Hu and Bentler (1999) as indicators of fit: CFI & TFI >.95, SRMR <.10, RMSEA < .06.
Because simulation studies show that fit indices are biased toward bifactor models (e.g., Greene et al., 2019), we also calculated two additional indices that have been recommended to address biases in traditional fit indices (Greene et al., 2019). The expected value of cross-validation index (ECVI; Browne & Cudeck, 1992) is a single sample index of the expected discrepancy between the calibration sample and validation sample, with smaller values indicating a better fitting model. The Vuong test for non-nested models tests which model is a closer fit to the underlying data (Merkle et al., 2016). Structural equation models were fit in the lavaan package in R (Rosseel, 2012). Missing data were addressed using Full-information Maximum Likelihood estimation. We chose Full-information Maximum Likelihood estimation over listwise deletion because listwise deletion have been shown to lead to biased results (e.g., Enders & Bandalos, 2001). We chose Full-information Maximum Likelihood estimation over multiple imputation due to several reasons (cf. Allison, 2012). Most importantly, multiple imputation introduces several choices (e.g., estimation method, number of datasets to impute) that can affect the results. Moreover, full-information Maximum Likelihood estimation has been shown to be robust to missing data that are missing completely at random or missing at random (e.g., Enders & Bandalos, 2001).1 In our data, Little’s test for missing completely at random was significant, χ2(3359) = 6394.92, p < .001. Therefore, we assumed the data were missing at random.
In the second stage of the analysis, the factor scores from the best fitting factor model were correlated with the construct validity measures (e.g., maladaptive personality traits). To adjust for multiple tests, we adjusted our p-values to maintain a false discovery rate of .05% (Benjamini & Hochberg, 1995). Supplemental Tables 3–5 also show unadjusted 99% confidence intervals for correlations, which are helpful for interpretation because the false-discovery rate adjustment only applies to the set of tests we conducted. We interpreted the size of the correlations based on Cohen’s (1992) recommendations (0.1 = small, 0.3 = medium, 0.5 = large). In addition to the main results, the Supplemental Material includes exploratory correlations between the factor scores and traumatic and stressful events.
Stage 1: Factor analytic structural equation models
Preliminary analyses indicated high levels of endorsement for lifetime alcohol use (92% endorsement), drug use (96% endorsement), and aggression (85% endorsement) in the sample. Self-harm was less common (17% lifetime endorsement). Model fit statistics for the factor models are shown in Table 1. All fit statistics favored the bifactor model as the best fitting model. The Vuong test comparing the bifactor to the higher-order model, Z = 9.70, p <.001, and four-factor model, Z = 9.49, p <.001, showed that the bifactor model was a significantly better fit to the data. Considering all this evidence together, we interpreted the bifactor model as the best fitting model. The Supplemental Material contains additional analyses with bifactor (S-1) models (Eid et al. 2017), which provide additional evidence that the fully symmetrical bifactor model was the best fitting model.
Table 1.
Model Fit Statistics for Factor Analytic Structural Equation Models
| Model | χ2 | df | CFI | TFI | SRMR | RMSEA [90% CI] | ECVI |
|---|---|---|---|---|---|---|---|
| One-Factor | 3601.28 | 324 | .62 | .66 | .10 | .112 [.109, .115] | 4.614 |
| Three-Factor | 5920.38 | 311 | .78 | .76 | .08 | .069 [.067, .070] | 1.642 |
| Four-Factor | 3520.86 | 318 | .87 | .85 | .05 | .052 [.051, .054] | 0.997 |
| Higher-Order | 3538.96 | 320 | .87 | .86 | .05 | .052 [.051, .054] | 1.001 |
| Bifactor | 2505.46 | 297 | .91 | .90 | .05 | .045 [.043, .046] | 0.734 |
Note. CFI = Comparative Fit Index; TFI = Tucker Lewis Index; SRMR = Standardized Root Mean-square Residual; RMSEA = Root Mean Square Error of Approximation; ECVI = Expected Value of Cross-Validation Index
The standardized loadings (see Supplemental Table 8) on the dysregulated behavior factor were generally modest (M =.37, SD = .18). The loadings for the unique factors were much stronger: alcohol use (M = .54, SD = .16), drug use (M = .21, SD = .33), aggression (M = .61, SD = .10), self-harm (M = .66, SD = .20). All loadings were significant at p < .001 Together, these results may suggest that there is meaningful shared variance across dysregulated behaviors; however, there is more variance shared within specific dysregulated behaviors than across different dysregulated behaviors.
Stage 2: Construct Validity
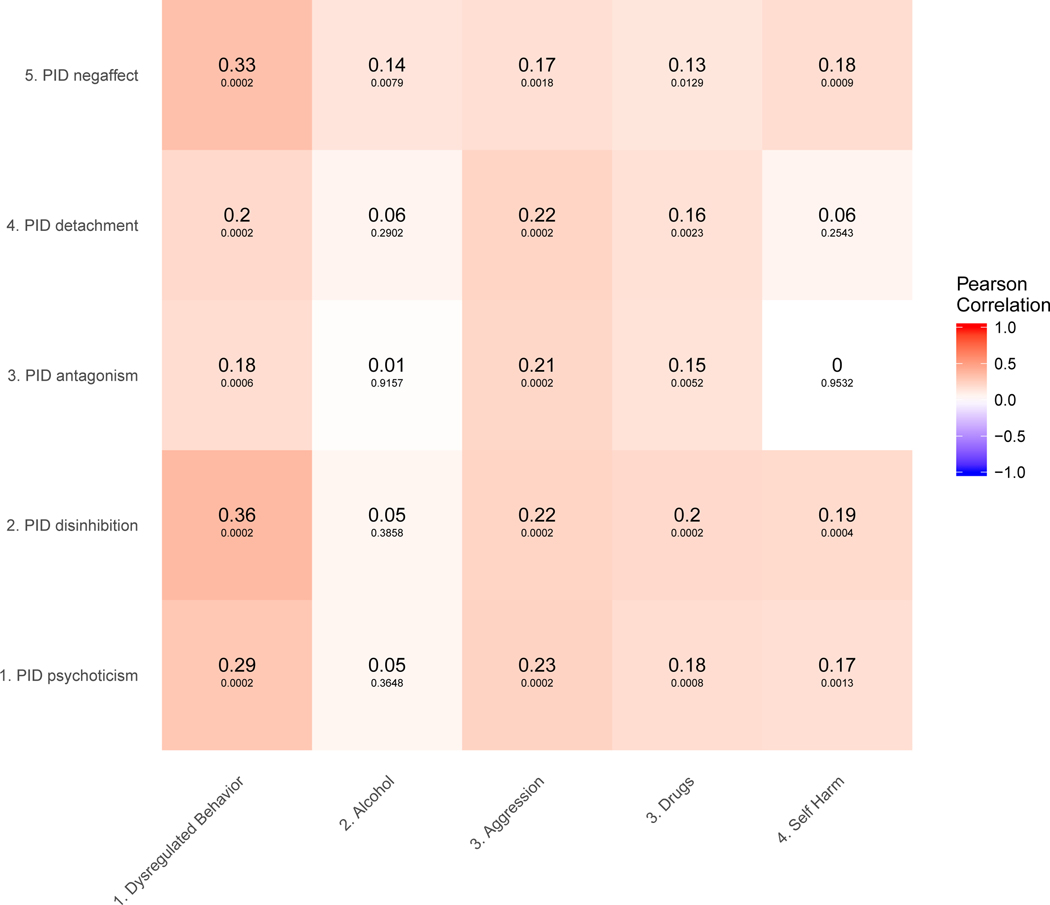
Figure 2 displays the correlation heatmap between the factor scores and measures of emotion dysregulation. The general dysregulated behaviors factor had significant positive correlations with all the subscales of the DERS that were medium in size. Thus, the general dysregulated behaviors factor is associated with high levels of emotion dysregulation. The unique alcohol use factor was not significantly correlated to any of the subscales of the DERS. The unique drug use factor was significantly positively related to all DERS subscales, aside from lack of awareness with small effect sizes. The unique aggression factor was significantly positively related to all DERS subscales, aside from lack of awareness with medium effect sizes for goals and impulse, and small effect sizes for strategies, nonacceptance, and clarity. The unique self-harm factor was significantly positively related to the goals, impulse, strategy, and nonacceptance DERS subscales.
Figure 2.
Correlations (and Adjusted P-Values) Among the Factor Scores and Emotion Dysregulation (Left Panel; N = 600) and Pathological Personality Traits (Right Panel; N = 384)
Note. DERS = Difficulty Regulating Emotions Scale.
Taken together, there are some similarities across the unique factors. None of the unique factors were related to the lack of awareness subscale of the DERS. The effect sizes were smaller for the unique factors compared to the common factor. The one exception was the unique aggression factor had a medium-sized positive relation with the DERS impulsive control subscale. There were also some notable differences. The unique alcohol use factor was not related to difficulties regulating emotions. Aside from the unique alcohol use factor, the unique self-harm factor was the only unique factor not related to lack of emotional clarity.
The Figure 3 displays the correlation heatmap among the extracted factor scores and maladaptive personality traits. The general dysregulated behaviors factor was significantly positively related to all the subscales of the PID-5-BF with small-to-medium effect sizes. This was predicted for negative affect, but not disinhibition, antagonism, detachment, or psychoticism. As predicted, the unique self-harm factor was significantly positively correlated with the negative affect scale of the PID-5-BF. The other unique factors also had small positive correlations with negative affectivity. Inconsistent with our prediction, disinhibition was not significantly related to alcohol use but was positively related to drug use. Consistent with our prediction, antagonism was related to the unique aggression factor. All unique factors aside from alcohol use were positively correlated with the detachment, disinhibition, and psychoticism scales of the PID-5-BF with small-to-medium effect sizes. Drug use was also significantly positively related to antagonism with the small-to-medium effect size.
Figure 3.
Correlations (and Adjusted P-Values) Among the Factor Scores and Pathological Personality Traits (Right Panel; N = 384)
Note. PID = Personality Inventory for DSM-5; Negaffect = Negative Affectivity
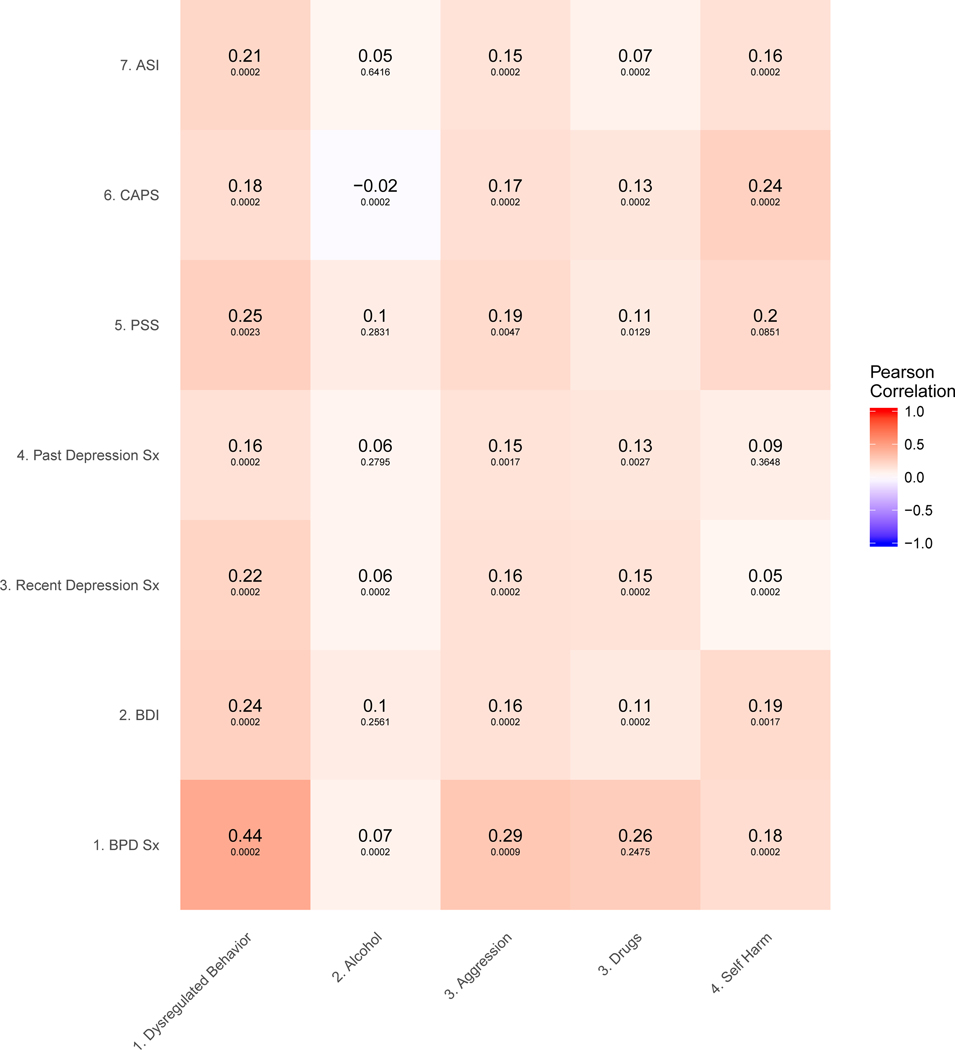
Figure 4 displays the correlations between the factor scores and symptoms of BPD, depression, PTSD, and anxiety sensitivity. As predicted, the general factor had a medium-sized positive correlation with symptoms of BPD. The general dysregulated behaviors factor was also significantly positively related to measures of depression, PTSD, and ASI with small-to-medium effect sizes.
Figure 4.
Correlations (and Adjusted P-Values) Among the Factor Scores and Symptoms of Psychopathology
Note. BPD Sx = Borderline Personality Disorder Symptoms (N= 326); BDI = Beck Depression Inventory (N = 3246); Recent Depression Sx = Current Depression Symptoms (N = 411); Past Depression Sx = Past Depression Symptoms (N = 383); PSS = Post-traumatic Symptom Scale (N = 3168); CAPS = Clinician Administered Posttraumatic Disorder Scale (N = 839); ASI = Anxiety Sensitivity Index (N = 3003).
The unique alcohol factor had small positive significant correlations with the BDI, PSS, and ASI. All the correlations with the interview-based measures were not significant. The unique drug use factor and aggression factor shared a similar pattern of correlations. They both had significant medium-sized correlations with BPD symptoms and small correlations with depression and PTSD symptoms. The one difference is that the unique aggression factor was significantly positively related to anxiety sensitivity with a small effect size, whereas the unique drug factor was not. The unique self-harm factor had significant positive correlations with BPD symptoms and BDI, but not interview-measures of depression. Interestingly, the unique self-harm factor was significantly positively related to PTSD symptoms assessed via self-report and interview with small-to-medium effect sizes. The unique self-harm factor was also significantly positively correlated with anxiety sensitivity with a small effect size. These results show that both the general and unique factors are generally positively related to symptoms of the DSM disorders included in our study.
Discussion
The goal of this paper was to address two limitations of the dysregulated behavior literature to advance etiological models of commonly co-occurring behaviors. First, we furthered research on the factor structure of dysregulated behaviors by comparing bifactor and higher-order models. In line with our prediction, our results showed support for a bifactor model, with a general dysregulated behavior factor and unique alcohol, drug, aggression, and self-harm factors. Second, we expanded research on the nomological network of the general and unique factors by examining their relations with emotion regulation difficulties, personality traits, and symptoms of psychopathology. In line with our hypotheses, the general dysregulated behavior factor was positively associated with emotion regulation difficulties, negative affectivity, and BPD symptoms. Many of our hypotheses for the unique factors were also supported. These results add to the growing literature on dysregulated behaviors and have implications for several areas of psychopathology and intervention research.
Our results suggest that a bifactor model provides the best fit to the data. This is in line with Sadeh and Baskin-Sommers (2017), who found evidence for a bifactor model over a correlated factor model, and are different from Kingston et al. (2011), who found evidence for a higher-order model but did not test a bifactor model. Our results add to the literature in that we directly compared the fit of a higher-order and bifactor model in a large sample of individuals at high risk for stress-related psychopathology. Thus, our results provide more direct evidence for a bifactor model where there are shared and unique vulnerabilities for dysregulated behaviors. Some caution is warranted in interpreting these results as many fit indices are biased to favor the bifactor model (Greene et al., 2019); however, we used additional measures to compare models, which are less biased and found the same results. Our results also show that these results generalize to a more racial and socioeconomically diverse sample compared to previous studies.
In line with our predictions, the general dysregulated behavior factor was positively correlated with all facets of emotion dysregulation. This indicates that part of what is shared across dysregulated behaviors is difficulty regulating emotions. This fits with Selby & Joiner (2009), who posited that individuals engage in dysregulated behaviors to regulate unpleasant emotions. Also, in line with our prediction, the general dysregulated behavior factor was positively correlated with negative affectivity. Together, this suggests that individuals who engage in dysregulated behaviors tend to experience negative affect and have difficulty regulating that affect. This is directly in line with the emotional cascade theory, which suggest that the reason people turn to dysregulated behaviors, as opposed to other methods of emotion regulation, is that they lack effective strategies to regulate their intense emotions (Selby & Joiner, 2009). We also found that the general dysregulated behavior factor was positively correlated with symptoms of BPD, which is in line with theory the emotional cascade theory of BPD (e.g., Selby & Joiner, 2009). This is also in line with Bresin’s (2020) suggestion that BPD is the DSM diagnosis most directly related to dysregulated behaviors. Together, these results could indicate that negative emotionality and the inability to regulate negative emotions are critical to the development of dysregulated behaviors.
We also found several significant correlations that were not predicted. The general dysregulated behavior factor was strongly correlated with the personality trait of disinhibition. In hindsight, this makes sense because dysregulated behaviors are a subset of impulsive behaviors (Bresin, 2020), and disinhibition is an important aspect of impulsivity (e.g., Whiteside & Lynam, 2001). When combined with our a priori predictions, this suggests that high negative affect and disinhibition combined with a lack of ability to regulate emotions may be a general risk profile for dysregulated behaviors. The general dysregulated behavior factor was positively correlated with the personality traits of antagonism, detachment, and psychoticism and the symptoms of depression, PTSD, and anxiety sensitivity. The correlations between the general dysregulated behavior factor and other personality traits are somewhat surprising as psychoticism (the pathological form of openness) and detachment (the pathological form of introversion; Widiger et al., 2019) are not necessarily associated with dysregulated behaviors (e.g., Barlett & Anderson, 2012; Brown, 2009; Malouff et al., 2007). It is not surprising that the general factor was positively related to symptoms of depression, PTSD, and anxiety sensitivity because symptoms of these disorders are correlated with high levels of negative affect (Kotov et al., 2017). Regardless, given that these correlations were not predicted a priori, replication is necessary.
We had three predictions for the unique factors, all of which were generally supported. First, we found that the unique drug factor was positively correlated with disinhibition. Counter to our prediction, however, the unique alcohol factor was not significantly related to disinhibition. Second, we found that the unique aggression factor was positively correlated with antagonism. Finally, we found that the unique self-harm factor was positively correlated with negative emotionality. The finding that the common general dysregulated behavior factor and unique dysregulated behavior factors were related to the same maladaptive personality traits may be interpreted to suggest that there are common and unique pathways to specific dysregulated behaviors via the same personality traits. Specifically, it may be that the broad personality dimensions are general risk factors for all dysregulated behaviors, whereas specific facets of personality traits may be uniquely related to some dysregulated behaviors and not others. For example, some research has found that specific facets of antagonism have stronger correlations with aggression than other facets (Crowe et al., 2018). Similarly, it may be that specific negative affect states may be more strongly related to some dysregulated behaviors than others (cf. Bresin, 2020). Thus, these results represent an opportunity for future research and theory development.
Beyond our a priori predictions, there were several patterns of correlations that emerged with the unique factors. First, aside from a few small significant correlations, the unique alcohol factor was largely unrelated to the variables examined in our study, which differed from the other unique factors. Research on externalizing psychopathology suggests that the unique variance in alcohol use when accounting for overlap between alcohol and antisocial psychopathology represents sensation seeking (e.g., Patrick et al., 2013). It is also possible that when the variance shared with other dysregulated behaviors is removed, the leftover variance in alcohol use is normative social drinking. The unique drug use, aggression, and self-harm factors shared similar patterns of correlations with emotion dysregulation, personality, and symptoms of psychopathology. It is worth noting that there were no correlations with unique factors that were not also shared by the general factor. Moreover, the correlations with the general factor tended to be stronger. This may suggest that most of the vulnerability for dysregulated behaviors is shared, and thus, theories of dysregulated behaviors may have the most predictive value at the general level. Still, given the size of the correlations, there are yet to be identified sources of variance in the unique factors.
In terms of psychopathology models, our results highlight some of the limitations of examining dysregulated behaviors with the DSM-5. For instance, we found that the general dysregulated behavior factor was positively correlated with symptoms of several DSM-5 disorders that are proposed to be distinct. We also found evidence for a common dysregulated behavior factor with symptoms that are part of distinct disorders (e.g., substance use, self-harm). Shared variance suggests that there may be common etiological factors across disorders. These results are in line with theory suggesting that the DSM-5 taxonomy creates artificial distinctions between dysregulated behaviors (Bresin, 2020). Our results provide some support that the Hi-TOP model may be more effective for classifying and identified etiological factors for dysregulated behaviors. For example, we found that the unique alcohol and substance use factors had significant positive associations with disinhibition, which is consistent with the Hi-TOP model’s placement of substance use disorders under the disinhibited externalizing spectra. Similarly, we found that the unique aggression factor was correlated with antagonism, which is in line with the Hi-TOP conceptualization. Despite these results, more research on the association between dysregulated behaviors and Hi-TOP is necessary.
These results have important implications for intervention development. Our results suggest that negative affect and emotion dysregulation would be ideal treatment targets to address several dysregulated behaviors. This is consistent with interventions for dysregulated behaviors that target emotion dysregulation. For instance, Dialectical Behavior Therapy (DBT; Linehan, 1991) is a multi-modal intervention that attempts to help clients replacing unskillful behavior, which includes but is not exclusively dysregulated behaviors, with more effective behavior. DBT has empirical support for treating self-harm (DeCou et al., 2019), aggression (Frazier & Vela, 2014), and substance use (Linehan et al., 2002). There is also some preliminary evidence that improvements in emotion regulation may be a mechanism of change in DBT (Maffei et al., 2018; Neacsiu et al., 2018). Given the modest correlations between the general dysregulated behavior factor and negative affect and emotion dysregulation (as much as 90% of the variance is not shared), our results also suggest that other treatment targets are needed. For instance, increasing the ability to inhibit responding to urges (i.e., decreasing disinhibition) may be helpful. Because we found associations between the unique factors and emotion dysregulation and maladaptive personality traits, it may suggest that more specific targeted interventions may help in reducing specific dysregulated behaviors (e.g., decreasing antagonism for aggression).
Limitations and Strengths
The results of this study should be considered in light of the limitations. First, these data are cross-sectional, which preclude the ability to draw causal conclusions from these associations. Second, we had high levels of missing data for the dysregulated behaviors. Specifically, 95% of participants had data for drug use, 73% had data for aggression, and 50% of participants had data for self-harm. We assumed that these were missing at random and used statistical techniques that have been shown to be robust to missing data. Still, replication in another sample with less missing data is necessary. Moreover, some of our model fit statistics (e.g., CFI) were below recommended thresholds, indicating that another model may fit the data better. We interpreted the best fitting model among those hypothesized. Still, a better fitting, theoretically interesting model may exist. Further replication is needed. Third, we only included a subset of dysregulated behaviors. It is possible that including other dysregulated behaviors (e.g., gambling, risky sex) would have led to a different factor structure, although Sadeh and Baskin-Sommers (2017) found support for a bifactor model with a larger set of dysregulated behaviors.
This study also has a number of strengths worth noting. First, we used a sample with a high rate of endorsement of dysregulated behaviors (a large urban-dwelling, trauma-exposed sample), whereas the two previous studies relied heavily on student and community samples (Kingston et al., 2011; Sadeh and Baskin-Sommers, 2017). Using an at-risk sample (i.e., a sample with a high rate of endorsement of dysregulated behaviors) advanced our understanding of the etiology of dysregulated behaviors in those most likely to seek and benefit from interventions. Our sample also contained a high percentage of Black participants with lower income than prior studies. This aids in generalizing the results from previous studies to other, often understudied, groups. Second, our sample size was much larger than the two previous studies, which enhances generalizability. Finally, although there are issues comparing higher-order and bifactor models (e.g., Greene et al., 2019), we used the current best methods to compare models. Together our results provide support for a bifactor model of dysregulated behaviors, and identify possible common and unique correlates, which could be used for further theory and intervention development.
Supplementary Material
Acknowledgments
Grant Funding and Acknowledgements
This work was supported by the National Institute of Mental Health (MH071537; MH100122; MH102890; MH115174; MH101380), the National Institute of Child Health and Human Development (HD071982), the National Center for Complementary and Integrative Health (K23AT009713), and the National Institute of Aging (AG062334).
We would like to thank the entire Grady Trauma Project team for their assistance in data collection and management for this project and the Grady Trauma Project participants for their willingness to be involved in our research.
Footnotes
Disclaimer: The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Institutes of Health. Additionally, the contents of this report do not represent the views of the Department of Veterans Affairs or the United States Government.
See the Supplemental Material for models with listwise deletion, which show similar results for the best fitting model with missing data
References
- Allison PD (2012, April). Handling missing data by maximum likelihood. In SAS global forum (Vol. 2012, No. 312, pp. 1038–21). [Google Scholar]
- American Psychiatric Association (2000). Diagnostic and statistical manual of mental disorders (4th ed. TR). Washington, DC: Author. [Google Scholar]
- American Psychiatric Association (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, DC: Author. [Google Scholar]
- Anderson JL, Sellbom M, & Salekin RT (2018). Utility of the Personality Inventory for DSM-5-Brief Form (PID-5-BF) in the measurement of maladaptive personality and psychopathology. Assessment, 25, 596–607. 10.1177/1073191116676889 [DOI] [PubMed] [Google Scholar]
- Baker TB, Piper ME, McCarthy DE, Majeskie MR, & Fiore MC (2004). Addiction motivation reformulated: An affective processing model of negative reinforcement. Psychological Review, 111, 33–51. 10.1037/0033-295X.111.1.33 [DOI] [PubMed] [Google Scholar]
- Barlett CP, & Anderson CA (2012). Direct and indirect relations between the Big 5 personality traits and aggressive and violent behavior. Personality and Individual Differences, 52, 870–875. 10.1016/j.paid.2012.01.029 [DOI] [Google Scholar]
- Beck AT, Steer RA, & Brown GK (1996). Manual for the Beck Depression Inventory-II. Psychological Corporation. [Google Scholar]
- Benjamini Y, & Hochberg Y. (1995). Controlling the false discovery rate: A practical and powerful approach to multiple testing. Journal of the Royal Statistical Society, 57, 289–300. http://www.jstor.com/stable/2346101 [Google Scholar]
- Bentley KH, Cassiello-Robbins CF, Vittorio L, Sauer-Zavala S, & Barlow DH (2015). The association between nonsuicidal self-injury and the emotional disorders: A meta-analytic review. Clinical Psychology Review, 37, 72–88. 10.1016/j.cpr.2015.02.006 [DOI] [PubMed] [Google Scholar]
- Blake DD, Weathers FW, Nagy LM, Kaloupek DG, Gusman FD, Charney DS, & Keane TM (1995). The development of a Clinician-Administered PTSD Scale. Journal of Traumatic Stress, 8, 75–90. 10.1007/BF02105408 [DOI] [PubMed] [Google Scholar]
- Bresin K. (2020). Toward a unifying theory of dysregulated behaviors. Clinical Psychology Review, 101885. 10.1016/j.cpr.2020.101885 [DOI] [PubMed] [Google Scholar]
- Bresin K. & Mekawi Y. (2020). Different ways to drown out the pain: A meta-analysis of the association between nonsuicidal self-injury and alcohol use. Archives of Suicide Research. DOI: 10.1080/13811118.2020.1802378 [DOI] [PubMed] [Google Scholar]
- Brown SA (2009). Personality and non-suicidal deliberate self-harm: Trait differences among a non-clinical population. Psychiatry Research, 169, 28–32. 10.1016/j.psychres.2008.06.005 [DOI] [PubMed] [Google Scholar]
- Browne MW, & Cudeck R. (1992). Alternative ways of assessing model fit. Sociological Methods & Research, 21, 230–258. [Google Scholar]
- Buckholdt KE, Parra GR, Anestis MD, Lavender JM, Jobe-Shields LE, Tull MT, & Gratz KL (2015). Emotion regulation difficulties and maladaptive behaviors: Examination of deliberate self-harm, disordered eating, and substance misuse in two samples. Cognitive Therapy and Research, 39(2), 140–152. 10.1007/s10608-014-9655-3 [DOI] [Google Scholar]
- Caspi A, Houts RM, Belsky DW, Goldman-Mellor CJ, Harrington H, Israel S, . . . Moffitt TE (2014). The p factor: One general psychopathology factor in the structure of psychiatric disorders? Clinical Psychological Science, 2, 119–137. DOI: 10.1177/2167702613497473 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Chapman AL, Gratz KL, & Brown MZ (2006). Solving the puzzle of deliberate self-harm: The experiential avoidance model. Behaviour Research and Therapy, 44, 371–394. 10.1016/j.brat.2005.03.005 [DOI] [PubMed] [Google Scholar]
- Cohen JA, (1992) power primer. Psychological Bulletin, 112, 155–159. doi: 10.1037/0033-2909.112.1.155. [DOI] [PubMed] [Google Scholar]
- Conger J. (1956). Reinforcement theory and the dynamics of alcoholism. Quarterly Journal of Studies on Alcohol, 17, 296–305. [PubMed] [Google Scholar]
- Cosci F, Schruers KRJ, Abrams K, & Griez EJL (2007). Alcohol use disorders and panic disorder: A review of the evidence of a direct relationship. The Journal of Clinical Psychiatry, 68, 874–880. 10.4088/JCP.v68n0608 [DOI] [PubMed] [Google Scholar]
- Crowe ML, Lynam DR, & Miller JD (2018). Uncovering the structure of agreeableness from self-report measures. Journal of Personality, 86, 771–787. 10.1111/jopy.12358 [DOI] [PubMed] [Google Scholar]
- Cucchi A, Ryan D, Konstantakopoulos G, Stroumpa S, Kaçar AŞ, Renshaw, … Kravariti E. (2016). Lifetime prevalence of non-suicidal self-injury in patients with eating disorders: A systematic review and meta-analysis. Psychological Medicine, 46, 1345–1358. 10.1017/S0033291716000027 [DOI] [PubMed] [Google Scholar]
- DeCou CR, Comtois KA, & Landes SJ (2019). Dialectical behavior therapy is effective for the treatment of suicidal behavior: A meta-analysis. Behavior Therapy, 50, 60–72. 10.1016/j.beth.2018.03.009 [DOI] [PubMed] [Google Scholar]
- de Meneses-Gaya C, Zuardi AW, Loureiro SR, & Crippa JAS (2009). Alcohol Use Disorders Identification Test (AUDIT): An updated systematic review of psychometric properties. Psychology & Neuroscience, 2, 83–97. 10.3922/j.psns.2009.1.12 [DOI] [Google Scholar]
- Duke AA, Smith KM, Oberleitner L, Westphal A, & McKee SA (2018). Alcohol, drugs, and violence: A meta-meta-analysis. Psychology of Violence, 8, 238–249. 10.1037/vio0000106 [DOI] [Google Scholar]
- Dutton DG, & Karakanta C. (2013). Depression as a risk marker for aggression: A critical review. Aggression and Violent Behavior, 18, 310–319. 10.1016/j.avb.2012.12.002 [DOI] [Google Scholar]
- Eid M, Geiser C, Koch T, & Heene M. (2017). Anomalous results in G-factor models: Explanations and alternatives. Psychological Methods, 22, 541–562. 10.1037/met0000083 [DOI] [PubMed] [Google Scholar]
- Enders CK, & Bandalos DL (2001). The relative performance of full information maximum likelihood estimation for missing data in structural equation models. Structural Equation Modeling, 8(3), 430–457. 10.1207/S15328007SEM0803_5 [DOI] [Google Scholar]
- Falsetti SA, Resnick HS, Resick PA, & Kilpatrick DG (1993). The Modified PTSD Symptom Scale: A brief self-report measure of posttraumatic stress disorder. The Behavior Therapist, 16, 161–162. [Google Scholar]
- First MB, & Gibbon M. (2004). The Structured Clinical Interview for DSM-IV Axis I Disorders (SCID-I) and the Structured Clinical Interview for DSM-IV Axis II Disorders (SCID-II). In Comprehensive handbook of psychological assessment, Vol. 2: Personality assessment (pp. 134–143). John Wiley & Sons Inc. [Google Scholar]
- Fox KR, Franklin JC, Ribeiro JD, Kleiman EM, Bentley KH, Nock MK (2015). Meta-analysis of risk factors for nonsuicidal self-injury. Clinical Psychology Review, 42,156–167. doi: 10.1016/j.cpr.2015.09.002. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Frazier SN, & Vela J. (2014). Dialectical behavior therapy for the treatment of anger and aggressive behavior: A review. Aggression and Violent Behavior, 19, 156–163. 10.1016/j.avb.2014.02.001 [DOI] [Google Scholar]
- Gillikin C, Habib L, Evces M, Bradley B, Ressler KJ, & Sanders J. (2016). Trauma exposure and PTSD symptoms associate with violence in inner city civilians. Journal of Psychiatric Research, 83, 1–7. 10.1016/j.jpsychires.2016.07.027 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Goldberg LR (1999). A broad-bandwidth, public domain, personality inventory measuring the lower-level facets of several five factor models. In Mervielde I, Deary I, De Fruyt F, & Ostendorf F. (Eds.), Personality psychology in Europe (Vol. 7, pp. 7–28). Tilburg, The Netherlands: Tilburg University Press. [Google Scholar]
- Gratz KL, & Roemer L. (2003). Multidimensional Assessment of Emotion Regulation and Dysregulation: Development, Factor Structure, and Initial Validation of the Difficulties in Emotion Regulation Scale. Journal of Psychopathology and Behavioral Assessment, 15. doi: 10.1023/B:JOBA.0000007455.08539.94. [DOI] [Google Scholar]
- Greene AL, Eaton NR, Li K, Forbes MK, Krueger RF, Markon KE, …. Kotov R. (2019). Are fit indices used to test psychopathology structure biased? A simulation study. Journal of Abnormal Psychology, 128, 740–764. 10.1037/abn0000434.supp [DOI] [PubMed] [Google Scholar]
- Grigorian HL, Brem MJ, Garner A, Florimbio AR, Wolford-Clevenger C, & Stuart GL (2020). Alcohol use and problems as a potential mediator of the relationship between emotion dysregulation and intimate partner violence perpetration. Psychology of Violence, 10, 91–99. 10.1037/vio0000237 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Guo K, Youssef GJ, Dawson A, Parkes L, Oostermeijer S, López-Solà C, Lorenzetti V, Greenwood C, Fontenelle LF, & Yücel M. (2017). A psychometric validation study of the impulsive-compulsive behaviours checklist: A transdiagnostic tool for addictive and compulsive behaviours. Addictive Behaviors, 67, 26–33. [DOI] [PubMed] [Google Scholar]
- Hagger MS, Gucciardi DF, & Chatzisarantis NL (2017). On nomological validity and auxiliary assumptions: The importance of simultaneously testing effects in social cognitive theories applied to health behavior and some guidelines. Frontiers in psychology, 8, 1933. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hokanson JE (1974). An escape-avoidance view of catharsis. Criminal Justice & Behavior, 1, 195–223. [Google Scholar]
- Hu LT, & Bentler PM (1999). Cutoff criteria for fit indexes in covariance structure analysis: Conventional criteria versus new alternatives. Structural Equation Modeling, 6, 1–55. 10.1080/10705519909540118 [DOI] [Google Scholar]
- Jakupcak M, Conybeare D, Phelps L, Hunt S, Holmes HA, Felker B, & Mcfall ME, (2007). Anger, hostility, and aggression among Iraq and Afghanistan war veterans reporting PTSD and subthreshold PTSD. Journal of Traumatic Stress, 20, 945–954. 10.1002/jts.20258 [DOI] [PubMed] [Google Scholar]
- Kimbrel NA, DeBeer BB, Meyer EC, Gulliver SB, & Morissette SB (2016). Nonsuicidal self-injury and suicide attempts in Iraq/Afghanistan war veterans. Psychiatry Research, 243, 232–237. 10.1016/j.psychres.2016.06.039 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kingston J, Clarke S, Ritchie T, & Remington B. (2011). Developing and validating the “Composite Measure of Problem Behaviors.” Journal of Clinical Psychology, 67(7), 736–751. 10.1002/jclp.20802 [DOI] [PubMed] [Google Scholar]
- Kotov R, Krueger RF, Watson D, Achenbach TM, Althoff RR, Bagby RM, ... Zimmerman M. (2017). The hierarchical taxonomy of psychopathology (HiTOP): A dimensional alternative to traditional nosologies. Journal of Abnormal Psychology, 126, 454–477. 10.1037/abn0000258.supp [DOI] [PubMed] [Google Scholar]
- Lai HMX, Cleary M, Sitharthan T, & Hunt GE (2015). Prevalence of comorbid substance use, anxiety and mood disorders in epidemiological surveys, 1990–2014: A systematic review and meta-analysis. Drug and Alcohol Dependence, 154, 1–13. 10.1016/j.drugalcdep.2015.05.031 [DOI] [PubMed] [Google Scholar]
- Linehan MM, Dimeff LA, Reynolds SK, Comtois KA, Welch SS, Heagerty P, & Kivlahan DR (2002). Dialectical behavior therapy versus comprehensive validation therapy plus 12-step for the treatment of opioid dependent women meeting criteria for borderline personality disorder. Drug and Alcohol Dependence, 67, 13–26. 10.1016/S0376-8716(02)00011-X [DOI] [PubMed] [Google Scholar]
- Linehan MM (1991). Cognitive-behavioral treatment of borderline personality disorder. Guilford Publications. [Google Scholar]
- Maffei C, Cavicchioli M, Movalli M, Cavallaro R, & Fossati A. (2018). Dialectical behavior therapy skills training in alcohol dependence treatment: Findings based on an open trial. Substance Use & Misuse, 53, 2368–2385. 10.1080/10826084.2018.1480035 [DOI] [PubMed] [Google Scholar]
- Malouff JM, Thorsteinsson EB, Rooke SE, & Schutte NS (2007). Alcohol involvement and the Five-Factor Model of personality: A meta-analysis. Journal of Drug Education, 37, 277–294. 10.2190/DE.37.3.d [DOI] [PubMed] [Google Scholar]
- Markon KE (2019). Bifactor and hierarchical models: Specification, inference, and interpretation. Annual Review of Clinical Psychology, 15, 51–69. 10.1146/annurev-clinpsy-050718-095522 [DOI] [PubMed] [Google Scholar]
- McNally RJ (2002). Anxiety sensitivity and panic disorder. Biological Psychiatry, 52(10), 938–946. 10.1016/S0006-3223(02)01475-0 [DOI] [PubMed] [Google Scholar]
- Merkle EC, You D, & Preacher KJ (2016). Testing nonnested structural equation models. Psychological Methods, 21, 151–163. 10.1037/met0000038 [DOI] [PubMed] [Google Scholar]
- Miller AE, & Racine SE (2020). Emotion regulation difficulties as common and unique predictors of impulsive behaviors in university students. Journal of American College Health. 10.1080/07448481.2020.1799804 [DOI] [PubMed] [Google Scholar]
- Mills KL, Teesson M, Ross J, & Peters L. (2006). Trauma, PTSD, and substance use disorders: Findings from the Australian National Survey of Mental Health and Well-Being. The American Journal of Psychiatry, 163, 651–658. 10.1176/appi.ajp.163.4.652 [DOI] [PubMed] [Google Scholar]
- Neacsiu AD, Rompogren J, Eberle JW, & McMahon K. (2018). Changes in problematic anger, shame, and disgust in anxious and depressed adults undergoing treatment for emotion dysregulation. Behavior Therapy, 49, 344–359. 10.1016/j.beth.2017.10.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Patrick CJ, Kramer MD, Krueger RF, & Markon KE (2013). Optimizing efficiency of psychopathology assessment through quantitative modeling: Development of a brief form of the Externalizing Spectrum Inventory. Psychological Assessment, 25, 1332–1348. 10.1037/a0034864.supp [DOI] [PMC free article] [PubMed] [Google Scholar]
- Peterson RA, & Heilbronner RL (1987). The anxiety sensitivity index: Construct validity and factor analytic structure. Journal of Anxiety Disorders, 1, 117–121. 10.1016/0887-6185(87)90002-8 [DOI] [Google Scholar]
- Rosseel Y. (2012). Lavaan: An R package for structural equation modeling and more. Version 0.5–12 (BETA). Journal of Statistical Software, 48(2), 1–36. [Google Scholar]
- Samuel DB, Simms LJ, Clark LA, Livesley WJ, & Widiger TA (2010). An item response theory integration of normal and abnormal personality scales. Personality Disorders: Theory, Research, and Treatment, 1(1), 5–21. 10.1037/a0018136 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sadeh N, & Baskin-Sommers A. (2017). Risky, Impulsive, and Self-Destructive Behavior Questionnaire (RISQ): A validation study. Assessment, 24, 1080–1094. 10.1177/1073191116640356 [DOI] [PubMed] [Google Scholar]
- Selby EA, & Joiner TE Jr. (2009). Cascades of emotion: The emergence of borderline personality disorder from emotional and behavioral dysregulation. Review of General Psychology, 13, 219–229. doi: 10.1037/a0015687 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sheehan DV, Lecrubier Y, Sheehan KH, Amorim P, Janavs J, Weiller E, Hergueta T,Baker R, & Dunbar GC (1998). The Mini-International Neuropsychiatric Interview (M.I.N.I): The development and validation of a structured diagnostic psychiatric interview for DSM-IV and ICD-10. The Journal of Clinical Psychiatry, 59(Suppl 20), 2233. [PubMed] [Google Scholar]
- Straus MA, Hamby SL, Boney-McCoy S, & Sugarman DB (1996). The revised Conflict Tactics Scales (CTS2): Development and preliminary psychometric data. Journal of Family Issues, 17, 283–316. 10.1177/019251396017003001 [DOI] [Google Scholar]
- Weathers FW, Keane TM, & Davidson JR (2001). Clinician-administered PTSD scale: A review of the first ten years of research. Depression and Anxiety, 13, 132–156. 10.1002/da.1029 [DOI] [PubMed] [Google Scholar]
- Whiteside SP, & Lynam DR (2001). The Five Factor Model and impulsivity: Using a structural model of personality to understand impulsivity. Personality and Individual Differences, 30, 669–689. 10.1016/S0191-8869(00)00064-7 [DOI] [Google Scholar]
- Widiger TA, Sellbom M, Chmielewski M, Clark LA, DeYoung CG, Kotov R, ... & Samuel DB (2019). Personality in a hierarchical model of psychopathology. Clinical Psychological Science, 7, 77–92. 10.1177/216770261879710 [DOI] [Google Scholar]
- Wolff JC, Thompson E, Thomas SA, Nesi J, Bettis AH, Ransford B, … Liu RT (2019). Emotion dysregulation and non-suicidal self-injury: A systematic review and meta-analysis. European Psychiatry, 59, 25–36. 10.1016/j.eurpsy.2019.03.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Yudko E, Lozhkina O, & Fouts A. (2007). A comprehensive review of the psychometric properties of the Drug Abuse Screening Test. Journal of Substance Abuse Treatment, 32(2), 189–198. 10.1016/j.jsat.2006.08.002 [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.