Abstract
Objective:
To describe prevalence, trends, and risk factors for catastrophic health expenditures in the year of delivery among birth parents (delivering people).
Methods:
We conducted a retrospective, cross-sectional study of the Medical Expenditure Panel Survey 2008-2016. We identified newborn birth parents, and a 2:1 nearest-neighbor propensity-matched cohort of non-pregnant reproductive-age controls, then assessed for catastrophic health expenditures (spending >10% family income) in the delivery year. We applied survey weights to extrapolate to the non-institutionalized US population and used the Adjusted Wald test for significance testing. We compared risk of catastrophic health expenditures between birth parents and controls, and described time trends and risk factors for catastrophic spending with subgroup comparisons.
Results:
We analyzed 4,056 birth parents and 7,996 reproductive-age females without pregnancy in a given year. Birth parents reported higher rates of unemployment (52.6% vs. 46.6%, p<0.001), and high rates of gaining (22.4%) and losing (25.6%) Medicaid in the delivery year. Birth parents were at higher risk of catastrophic health expenditures (excluding premiums: 9.2% vs. 6.8%, OR=1.95, 95%CI 1.61-2.34; including premiums: 21.3% vs. 18.4%, OR=1.53, 95%CI 1.32-1.82). Birth parents living on low incomes had the highest risk of catastrophic health expenditures (18.8% vs. 0.7% excluding premiums for ≤138% vs. >400% federal poverty level [FPL], RR=26.9; 29.8% vs 5.9% including premiums, RR=5.1). For birth parents living at low incomes, public insurance was associated with lower risks of catastrophic health expenditures than private insurance, particularly when including premium spending (incomes ≤138% FPL: 18.8% public vs. 67.9% private, RR=0.28; incomes 139-250% FPL: 6.5% public vs. 41.1% private, RR=0.16). The risk of catastrophic spending for birth parents did not change significantly over time from before to after ACA implementation.
Conclusion:
Pregnancy and delivery are associated with increased risk of catastrophic health expenditures in the delivery year. Medicaid and public coverage were more protective from high out-of-pocket costs than private insurance, particularly among low-income families.
Précis:
Pregnancy and delivery increases the risk of catastrophic health care expenditures for reproductive-age females, and among low-income parents, Medicaid is more financially protective than private insurance.
Introduction
Pregnancy, delivery, and the postpartum period represent a time of high health care utilization for reproductive-age females.1 Pregnant people must adjust to shifts in medical needs, employment, and coverage eligibility as well as navigate the complex United States (US) health care and insurance markets,2,3 leading to high rates of insurance churn (gain and loss of coverage).4 Socioeconomic status, family structure, and maternal comorbidities further complicate health care needs and can contribute to the financial burden on a parent and their family following the birth of a newborn.5
The Patient Protection and Affordable Care Act (ACA), passed into law in March 2010,6 contained provisions impacting pregnancy care, including prohibition of coverage denials based on pregnancy, sex, or other medical conditions as well as coverage eligibility expansions for dependents, and regulations on annual out-of-pocket spending.7 Additionally, effective in January 2014, coverage expansions via Medicaid expansion and state insurance exchanges with low-income subsidies launched as the last major ACA program.
While the ACA has decreased uninsurance,8–10 the incidence of excessive out-of-pocket cost burden associated with pregnancy and delivery has not been well described. Chua, et al. examined out-of-pocket costs for privately insured families for the delivery hospitalization, finding mean cost $3000.11 Taylor et al. assessed the financial stress of labor and delivery, noting 24% of peripartum individuals endorsed an unmet health care need secondary to cost.12 However, McMorrow et al. noted that new parents were less likely to report unmet health care needs or concerns about medical bills after ACA implementation.13
According to the Commonwealth Fund, a family faces catastrophic health expenditures when out-of-pocket health spending exceeds 10% of income in a given year.14 Our objectives of this study were (1) to compare employment, insurance coverage, and prevalence of catastrophic health expenditures among birth parents (delivering people) in the delivery year in the US to matched non-pregnant, reproductive-aged controls, and (2) to assess for risk factors for catastrophic health expenditures in the delivery year among birth parents, including changes over time during the implementation of the Affordable Care Act.
Methods
This study used the Medical Expenditure Panel Survey (MEPS), an annual cross-sectional survey of families, individuals, medical practitioners, and employers in the US executed since 1996 by the Agency for Healthcare Research and Quality.15,16 The survey assesses a subsample of households that participated in the prior year’s National Health Interview Survey, and is designed to be representative of the civilian, non-institutionalized US population. We merged data from multiple MEPS files to the level of the person-year for analysis. MEPS is de-identified and this study was not considered Human Subject research by the IRB.
We included the years 2008-2016 to encompass the passage and implementation of the Affordable Care Act.17 From the full MEPS sample, we first identified newborns, defined as individuals with age <1 on December 31st of the given year.18 Newborns were then mapped to the indicated mother (referred to henceforth as “birth parent”) in MEPS. We excluded newborns with no listed birth parent (children adopted into MEPS families), and if newborn or birth parent was ineligible for survey inclusion in the birth month.
MEPS uses an overlapping panel design that samples individuals for two consecutive years. We excluded birth parents with multiple deliveries in the same year. For birth parents with deliveries in both survey years, we randomly selected one year and /delivery for inclusion to avoid including two observations from the same individual, in order to maintain independence of observations.4 To assess the impact of pregnancy and delivery on outcomes, we created a control cohort of reproductive-age female respondents, without pregnancy or delivery in a given year. We first selected non-birth parent female respondents in the age range corresponding to the birth parent cohort age range. We then excluded those reporting pregnancy, those in a family where a newborn was born to a different female, and those who died. Again, to maintain independence of observations, we randomly selected one of two survey years for each respondent to be eligible for inclusion in the matched cohort.
MEPS surveys individuals on a number of demographic characteristics, including age, race (White, Black, Native American, Asian, multiple or none of these categories; used for propensity matching, described in more detail below, to avoid out differences related to racially imbalanced groups given concerns for systemic disparities in healthcare access and economic opportunity), ethnicity (Hispanic vs. Non-Hispanic), primary language in the home (English vs. Non-English), marital status, family size (count of people), education (no high school equivalent, high school degree or equivalent, college degree), and family income as a percent of the federal poverty level (FPL; ≤138%, 139-250%, 251-400%, >400%), and self-reported perceived health status (excellent, very good, good, fair, poor). We calculated Elixhauser comorbidity scores19 from Medical Condition files for each respondent in a given year (0, 1, 2, ≥3). Obstetrics specific comorbidity scores, such as the Bateman score, could not be used due to limitations in reporting of pregnancy-specific comorbidities in MEPS.20
We also sought to report on important contextual characteristics for catastrophic health expenditures associated with pregnancy and delivery. MEPS surveys employment status (non-employed versus employed or job to return to). MEPS also reports detailed month-to-month insurance status, which we used to summarize birth month coverage and measures of insurance churn in the delivery year. We assessed for coverage gain (uninsurance to insurance), loss (insurance to uninsurance), and change (any switch coverage type).4,21 Data quantifying annual health care utilization is reported for individuals for each year by self-report in MEPS. We extracted reported counts of annual office visits, emergency department visits, inpatient stays, and total days spent hospitalized in the given year. These counts included visits related to the pregnancy and delivery. Lastly, we merged data on delivery hospitalizations from Hospital Inpatient Stays files. Delivery hospitalization data was not identified in 13% of newborn and birth parent pairs. This is consistent with under-reporting identified in prior comparisons of MEPS to national hospitalization data, thought to be secondary to partial reliance on recall from individuals, or individuals not recognizing the delivery as an inpatient hospitalization in the survey.22 Hospitalization data assessed included vaginal delivery vs cesarean section, length of hospital stay, singleton vs multiple delivery, total and out-of-pocket visit expenditures, and extended newborn hospitalizations (newborn hospitalization is only reported separate from the delivery hospitalization in MEPS if the newborn stay extended after the parent’s discharge). Extended newborn stays were assumed to be inclusive of and have high overlap with neonatal intensive care admissions, though there was no way of confirming this, given the limited clinical information available from the MEPS data.
To ensure comparability of birth parents and the control cohort of female respondents without pregnancy or delivery, we used propensity-score matching. We performed 2:1 nearest neighbor matching without replacement, using a maximum caliper of 0.02 (approximately 20% of the standard deviation of the propensity-score).23 Matching variables included age, race, ethnicity, non-English home language, marital status, family size, education, income category, Elixhauser comorbidity, self-perceived health status, survey year, and the respondent’s survey weight.24 Respondents were considered married in the delivery year if they reported being married during any of three annual assessments. We selected self-perceived health status as the first reported value in the delivery year. All other variables were static or only assessed once each survey year. We chose not to match on insurance coverage or employment status, as insurance eligibility is explicitly impacted by pregnancy, and pregnancy may strongly impact choices around employment. While there is not exact consensus on variable selection for propensity matching, variables that may be influenced or modified by the matching treatment of interest (pregnancy) should not be included in the model.25
MEPS collects data on self-reported income as well as out-of-pocket spending on health care services, pharmaceuticals, and private insurance premiums.16,26 Premiums for Medicare coverage were imputed from published rates,27,28 and premiums for Medicaid and other public coverage were assumed to be $0.29 All expenses and incomes were adjusted for inflation to 2018 US$.30 We calculated catastrophic health expenditures according to the Commonwealth Fund definition: annual family health expenditures, excluding premium spending, in excess of 10% of family income, or 5% of family income for families at or near poverty (<250% federal poverty level).14 This definition is based on spending and income of the family, rather than the individual, as the burden of health spending is typically shared at the family level, and is consistent with other MEPS studies.21,27,31,32
In MEPS, family income and individual out-of-pocket health expenditures are reported as annual totals. As monthly spending and income data are not reported in MEPS, all analyses describe the 12 months of the year of delivery, rather than the specific months of pregnancy and postpartum period. While this represents a limitation, the vast majority of peripartum health spending occurs at the time of delivery.33 Health expenditures were summed across family members, including and excluding out-of-pocket spending on insurance premiums. The ratio of family health expenditures/family income was then calculated for each individual.
For our primary specification, we assessed family out-of-pocket health care expenses (excluding premiums) exceeding 10% of family income in the birth year. As secondary outcomes, we assessed (1) expenses plus out-of-pocket premium spending exceeding 10% of income, and (2) expenses (excluding premiums) exceeding 5% of income among families with incomes ≤250% FPL.
We applied the survey weights for all analyses to make estimates applicable to the civilian, non-institutionalized US population. To improve estimate precision, we pooled data across years, in most cases across the entire cohort (2008-2016). Group comparisons were tested for statistical significance with the Adjusted Wald test. We assessed for risk factors for catastrophic health expenditures among birth parents by comparisons of prespecified subpopulations of interest, including by income, marital status, employment, insurance coverage, and extended newborn stay.
While we hoped to explore the impacts of the ACA, we lacked data on individual utilization of specific ACA policies or programs, and therefore we were limited to an exploratory assessment of changes over time. The ACA was signed into law in March 2010 and the first legal changes were implemented late that year. Between 2011 and the end of 2013, various legal rules changed, but some of the most important coverage expanding programs including state insurance exchanges and Medicaid expansion did not launch until January 2014.17,34 Thus, we compared insurance and catastrophic health expenditure outcomes among birth parents and the pooled control cohort from before (2008-2010) to after (2014-2016) ACA implementation, with statistical comparisons similarly by the Adjusted Wald test.
We considered p<0.05 to be statistically significant. We followed STROBE reporting guidelines for observational studies.35 We used STATA v15.1 (Statacorp, College Station, TX, USA) for all analyses, including the ‘SVYSET’ package to account for the complex survey design. We created figures with Microsoft PowerPoint/Excel v14.7.7 (Microsoft Corporation, Redmond, WA, USA).
Results
We identified 4,452 newborns in MEPS from 2008-2016, corresponding to an estimated 3.98 million annual births (95%CI 3.72-4.23 million) in the US over that time, which closely corresponds to published US population data reporting 3.95 million births in 2016.36 From this cohort of newborns, we included 4,153 newborns (4,039 singletons, 108 twins, 6 triplets) with 4,095 corresponding birth parents. After 2:1 propensity-score matching to non-pregnant reproductive-age female controls, we analyzed 4,056 birth parents in comparison to 7,996 matched controls (see Figure 1).
Figure 1.
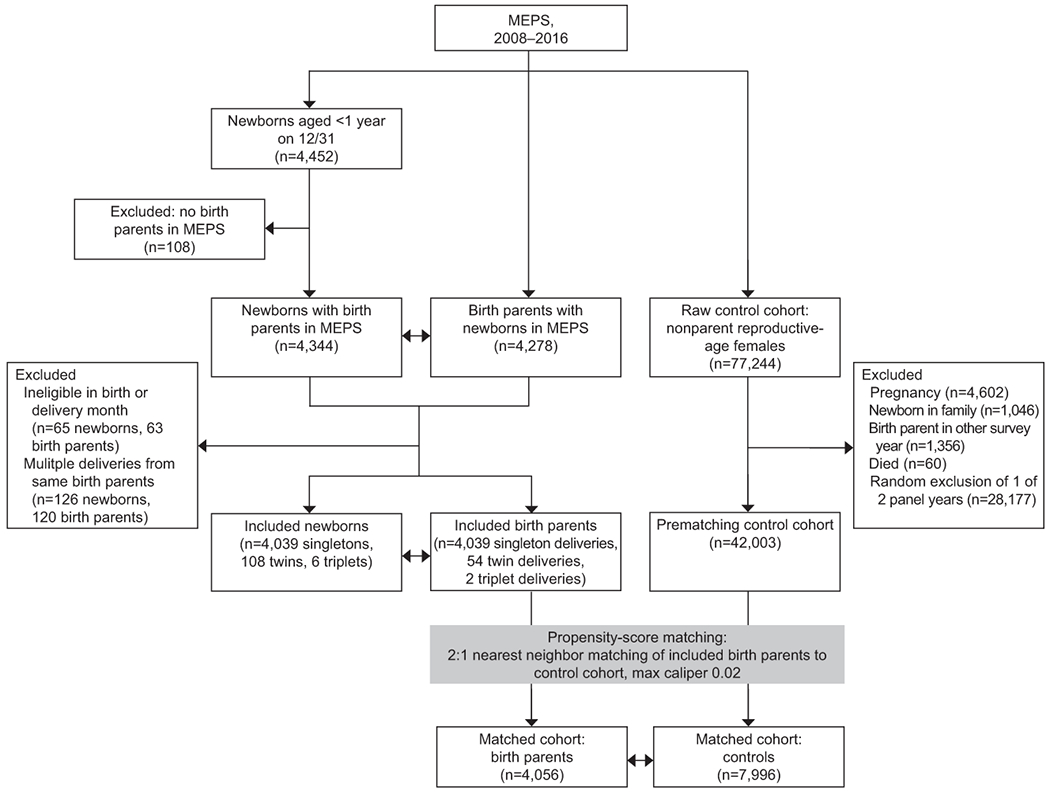
Cohort selection flow diagram for study sample of newborns, birth parents, and the propensity-matched control cohort from the Medical Expenditure Panel Survey (MEPS), 2008–2016.
Demographic characteristics of the birth parents and matched controls are presented in Table 1. Matching characteristics of age, race, ethnicity, language, education, comorbidity, and self-reported health status were well balanced between the two cohorts. Birth parents were slightly more likely to be married (67.8% vs. 60.5%, p<0.001), in larger families (4.1 people vs. 4.0, p<0.001), and less likely to be in families with income ≤138% FPL (35.7% vs. 38.8%, p=0.01). These few differences between groups were small and unlikely to be clinically significant or to introduce significant bias in our matched comparisons.
Table 1:
Population demographic characteristics of annual population of birth parents in the United States versus propensity-matched controls, Medical Expenditure Panel Survey, 2008-2016.
| Birth Parents Estimate (95%CI) |
Matched controls Estimate (95%CI) |
P value | |
|---|---|---|---|
|
|
|||
| Sample n (unweighted) | 4,056 | 7,996 | |
|
|
|||
| Annual Pop. Estimate (millions) | 3.5 (3.3–3.7) | 6.7 (6.4–7.0) | |
| Age (years) | 28.0 (27.3-28.3) | 27.8 (27.6-28.0) | 0.17 |
| Race (%) | |||
| Asian | 6.1% (4.9-7.2) | 6.4% (5.2-7.6) | 0.61 |
| Black | 14.2% (12.3-16.1) | 14.5% (12.7–16.3) | 0.73 |
| Native American | 0.85% (0.3-1.4) | 1.2% (0.60-1.8) | 0.09 |
| White | 77.1% (74.8-79.4) | 76.1% (73.7–78.4) | 0.32 |
| None of the above/mixed | 1.8% (1.4-2.2) | 1.90% (1.5-2.4) | 0.69 |
| Hispanic ethnicity (%) | 22.5% (19.6-25.4) | 21.8% (19.2-24.4) | 0.47 |
| Non-English home* (%) | 20.6% (18.4-22.7) | 20.7% (18.7-22.7) | 0.91 |
| Low Education† (%) | 11.4% (10.1-12.6) | 11.8% (10.8-12.9) | 0.44 |
| Married (%) | 67.8% (65.8-69.9) | 60.5% (58.7-62.2) | <0.001 |
| Family Size (n) | 4.1 (4.1-4.2) | 4.0 (3.9-4.01) | <0.001 |
| Family Income (%) | |||
| ≤138% FPL | 35.7% (33.4-37.9) | 38.8% (36.8-40.8) | 0.01 |
| 139-250% FPL | 20.7% (19.0-22.5) | 20.8% (19.4–22.2) | 0.96 |
| 251-400% FPL | 17.8% (15.9-19.8) | 16.1% (14.8-17.4) | 0.11 |
| >400% FPL | 25.7% (23.4-28.1) | 24.3% (22.4-26.2) | 0.30 |
| Elixhauser Comorbidity ≥2 (%) | 13.9% (12.0-15.7) | 13.1% (11.8-14.4) | 0.43 |
| Self-reported health status (%) | |||
| Excellent | 33.1% (30.8-35.4) | 32.2% (30.7-33.6) | 0.45 |
| Very Good | 35.6% (33.7-37.6) | 36.0% (34.5-37.5) | 0.75 |
| Good | 24.7% (22.8-26.6) | 25.2% (23.8-26.6) | 0.64 |
| Fair | 5.8% (4.8-6.8) | 5.6% (4.9%-6.2) | 0.65 |
| Poor | 0.8% (0.5-1.0) | 1.1% (0.7-1.4) | 0.21 |
FPL=Federal poverty line; CI = confidence interval; Pop. = population; All estimates applicable to extrapolated civilian, non-institutionalized US population, p value by Adjusted Wald test. Matched control cohort was 2:1 nearest-neighbor propensity matched on all variables included in this table, in addition to survey year and weight.
Language other than English is primary language spoken in family home
Low education indicates age >18 and no high school or equivalent degree
Out-of-pocket health spending depends on insurance status, and insurance status is frequently tied to employment in the US, thus these characteristics give important context to spending outcomes (see Table 2). Relative to matched controls, birth parents were significantly more likely to report non-employment during the delivery year: with 52.6% reporting being unemployed for at least part of the year (versus 46.6% of matched controls, p <0.001) and 32.1% reporting being unemployed for an entire year (versus 26.0% of matched controls, p<0.001). For the delivery month, birth parents had high enrollment in Medicaid (32.1% vs. 16.4%, p<0.001), and were significantly less likely to be uninsured versus matched controls (9.9% vs. 27.8%, p<0.001). Though only 9.9% of birth parents were uninsured in the delivery month, 27.6% reported uninsurance in at least one month during the delivery year. Consistent with this finding, we observed high risk of insurance churn in the delivery year for birth parents relative to matched controls. Birth parents were more likely to have any change in insurance type (28.1% vs. 18.8%, p<0.001) and were more likely for this change to be a loss of insurance (14.9% vs. 12.0%, p=0.007). This churn was concentrated among Medicaid recipients, with birth parents more likely to gain (22.4% vs. 17.9%, p=0.01) and lose (25.6% vs. 17.0%, p<0.001) Medicaid coverage, but less likely to gain (6.3% vs. 9.9%, p<0.001) or lose (6.0% vs. 9.6%, p=0.002) private insurance, versus matched controls.
Table 2.
Employment and insurance coverage characteristics for annual population of newborn mothers in the United States versus propensity-matched controls, Medical Expenditure Panel Survey, 2008-2016.
| Birth Parents Estimate (95%CI) n = 4,056 |
Matched controls Estimate (95%CI) n = 7,996 |
P value | |
|---|---|---|---|
| Employment* (%) | |||
| Part-year non-employment | 52.6% (50.5-54.8) | 46.6% (45.0-48.3) | <0.001 |
| Full-year non-employment | 32.1% (30.2-34.0) | 26.0% (24.5-27.6) | <0.001 |
| Birth-month Insurance† (%) | |||
| Private coverage | 56.3% (53.7-59.0) | 54.1% (52.1-56.2) | 0.09 |
| Medicaid coverage | 32.1% (29.5-34.7) | 16.4% (14.8-18.0) | <0.001 |
| Other public coverage | 1.7% (1.1-2.4) | 1.7% (1.2-2.2) | 0.95 |
| Uninsured | 9.9% (8.5-11.3) | 27.8% (25.8-29.7) | <0.001 |
| Uninsurance | |||
| Never insured (%) | 6.2% (5.1-7.3) | 20.1% (19.0-22.7) | <0.001 |
| Any period (%) | 27.6% (25.2-29.9) | 35.9% (34.0-37.8) | <0.001 |
| Months uninsured (n) | 1.7 (1.5-1.9) | 3.2 (3.0-3.4) | <0.001 |
| Insurance Churn‡ (%) | |||
| All coverage | |||
| Any change | 28.1% (26.1-30.2) | 18.8% (17.6-20.0) | <0.001 |
| Any loss | 14.9% (13.0-16.8) | 12.0% (10.9-13.0) | 0.007 |
| Any gain | 13.8% (12.4-15.3) | 12.5% (11.4-13.7) | 0.18 |
| Medicaid | |||
| Gain | 22.4% (19.7-25.0) | 17.9% (15.4-20.3) | 0.01 |
| Loss | 25.6% (22.3-29.0) | 17.0% (14.7-19.2) | <0.001 |
| Disruption | 33.5% (30.0-37.0) | 23.2% (20.4-26.0) | <0.001 |
| Private | |||
| Gain | 6.3% (4.7-7.9) | 9.9% (8.7-11.1) | <0.001 |
| Loss | 6.0% (4.7-7.3) | 9.6% (8.3-10.9) | 0.002 |
| Disruption | 9.8% (9.4-12.1) | 9.8% (8.2-11.4) | 0.33 |
CI = confidence interval; Matched control cohort was 2:1 nearest-neighbor propensity matched on age, race, ethnicity, home language, marital status, family size, education, income, comorbidity, health status, year, and survey weight.
Employment status assessed at 3 interview points in each calendar year, non-employment defined as reporting no job at present or to return to for non-retirees >18 years of age
Coverage in birth month for mothers, and first eligible month for matched controls
Insurance churn in year of delivery: change (any change in coverage type), loss (insurance to uninsurance), gain (uninsurance to insurance), disruption (insurance type to uninsurance or other coverage).
Among the 4,056 birth parents, we identified hospitalization data for 3,531 deliveries, with delivery type specified in 3,301 cases (68.2% vaginal, 30.8% cesarean, see Table 3). Although mean total expenditures were significantly higher for cesarean versus vaginal deliveries ($11,500 vs. $8,000, p<0.001), out-of-pocket costs were similar ($470 vs. $560, p=0.12). Out-of-pocket delivery costs were far higher with private coverage ($781, 95%CI $699-$863) or uninsurance ($776, 95%CI $540-$1,013) versus Medicaid coverage ($65, 95%CI $25-$106). We identified 524 newborns with hospitalization beyond birth parent discharge. Among these extended stays, male newborns (55.6%) and newborns from multiple deliveries (5.7%) were slightly overrepresented, and mean length of stay was 10.3 days. Total expenditures for these extended stays, averaged $19,500, though only 2.4% of this total ($470) was paid by the patient out-of-pocket on average. Birth parents with newborn extended stays were more likely to have catastrophic health expenditures by expenses alone in the delivery year (12.1%, 95%CI 8.2-15.9%) versus other parents (8.8%, 95%CI 7.5-10.0%).
Table 3.
Delivery hospitalization characteristics and associated catastrophic health expenditures for mothers and newborns in the United States, Medical Expenditure Panel Survey, 2008-2016.
| Delivery Hospitalizations* |
Extended Newborn Hospitalizations† Estimate (95%CI) n = 524 |
|||
|---|---|---|---|---|
| Vaginal Delivery Estimate (95%CI) n = 2,252 |
Cesarean section Estimate (95%CI) n = 1,049 |
P value | ||
| Hospitalization Characteristics | ||||
|
| ||||
| Female (%) | 100% (-) | 100% (-) | 1.0 | 44.4% (38.4-50.5) |
|
| ||||
| Multiple delivery (%) | 1.0% (0.4-1.6) | 3.0% (1.7-4.2) | 0.006 | 5.7% (2.4-9.1) |
|
| ||||
| Length of stay (days) | 2.4 (2.3-2.4) | 3.5 (3.3-3.7) | <0.001 | 10.3 (8.1-12.4) |
| Visit Expenditures | ||||
| Total ($) | $8,000 (7,500-8,500) | $11,500 (10,700-12,300) | <0.001 | $19,500 (10,700-28,200) |
| Out-of-pocket ($) | $560 (470-650) | $470 (400-540) | 0.12 | $470 (360-580) |
| Risk of Catastrophic Health Expenditures‡ in birth year | ||||
| Expenses >10% income (%) | 10.2% (8.5-11.9) | 7.5% (5.7-9.3) | 0.03 | 12.1% (8.2-15.9) |
| Expenses >5% income among those <250% FPL (%) | 25.8% (22.3-29.3) | 22.8 (18.2-27.5) | 0.30 | 25.3% (18.0-32.7) |
| Expenses + Premiums >10% income (%) | 21.0% (18.3-23.6) | 23.4% (20.2-26.6) | 0.22 | 26.5% (20.8-32.3) |
FPL = Federal Poverty Level; CI = Confidence Interval
Hospitalization data missing for n = 525, and present but unknown delivery type for n = 230, these observations are not represented in this table
Hospitalization data for newborns only reported in cases where newborn stay extended beyond maternal stay, all costs are additional costs on top of maternal hospitalization
Catastrophic health expenditures defined at family level, annual family out-of-pocket health expenses (with or without premiums) as a percent of annual family income
Annual health care utilization and risk of catastrophic health care expenditures in the delivery year for birth parents and matched controls are presented in Table 4. Relative to matched controls, birth parents reported more annual office visits (10.9 vs. 3.3), emergency department visits (0.4 vs 0.2), and inpatient stays (0.98 vs 0.04). Birth parents also faced higher risks of catastrophic health expenditures. Family health expenses, excluding premiums, exceeded 10% of family income for 9.2% of birth parents in the delivery year (vs. 6.8% of controls OR=1.95, 95%CI 1.61-2.34; including premiums: 21.3% vs. 18.4%, OR=1.53, 95%CI 1.32-1.82 ).For parents in families ≤250% FPL, expenses alone exceeded 5% of income for 24.7% of birth parents (vs. 18.4% of controls, p<0.001). When including out-of-pocket spending on premiums, 21.3% of all birth parents had catastrophic spending over 10% of family income (vs. 19.6% of controls, p=0.008).
Table 4.
Annual health care utilization and Catastrophic Health Expenditures* in delivery year for birth parents versus matched controls in the United States, Medical Expenditure Panel Survey, 2008-2016.
| Outcome | Birth Parents Estimate (95%CI) n = 4,056 |
Matched controls Estimate (95%CI) n = 7,996 |
P Value |
|---|---|---|---|
| Annual utilization | |||
| Mean office visits (n) | 10.9 (10.4 to 11.3) | 3.3 (3.1 to 3.6) | <0.001 |
| Mean Emergency Department visits (n) | 0.40 (0.37 to 0.44) | 0.20 (0.20 to 0.21) | <0.001 |
| Mean inpatient stays (n) | 0.98 (0.96 to 1.00) | 0.04 (0.03 to 0.05) | <0.001 |
| Mean total inpatient length of stay (days) | 2.73 (2.61 to 2.87) | 0.16 (0.11 to 0.22) | <0.001 |
| Annual Risk of Catastrophic Health Expenditures * | |||
| Expenses >10% income (%) | 9.2% (8.0 to 10.4) | 6.8% (6.1 to 7.6) | <0.001 |
| Expenses >5% income for those <250% FPL (%) | 24.7% (22.1 to 27.2) | 19.6% (18.1 to 21.2) | <0.001 |
| Expenses + premiums >10% income (%) | 21.3% (19.3 to 23.3) | 18.4% (17.2 to 19.5) | 0.008 |
CI = confidence interval
Catastrophic health expenditures defined at family level, annual family out-of-pocket health expenses (with or without premiums) as a percent of annual family income
We used subgroup comparisons to explore risk factors for catastrophic health expenditures among birth parents (see Table 5). Income level was the strongest driver of risk of catastrophic health spending for birth parents in the year of delivery. The risk was highest for those in families living on income <138% FPL, with catastrophic spending risk of 18.8% by expenses alone, or 29.8% including premium spending, for respective relative risks (RR) of 26.9 and 5.1 vs birth parents living on incomes >400% FPL. Unemployment and being unmarried were associated with some increased risk of catastrophic spending among birth parents living on the lowest incomes, but not for those at higher incomes. With the exception of birth parents living on incomes >400% FPL (92% of whom reported private insurance), having public insurance was associated with lower risk of catastrophic health expenditures when compared to those with private insurance in the same income level, particularly when including spending on insurance premiums. For birth parents living on incomes <138% FPL, those with Medicaid and public insurance had 14.7% and 18.8% risk of catastrophic spending in the delivery year, excluding or including premium spending. These risks rose to 23.6% and 67.9% for these lowest income birth parents with private insurance coverage (RR=0.62 and 0.28 for public vs private coverage). Newborn extended stay was associated with significantly increased risk of catastrophic health expenditure only for those at 250-400% FPL (14.8% vs. 3.0%, RR=4.9 excluding premiums; 41.5% vs. 17.0%, RR=2.4 including premiums).
Table 5.
Risks and relative risks of catastrophic health expenditures in the delivery year among birth parents in the United States, Medical Expenditure Panel Survey, 2008-2016.
| n | Expenses >10% Income† | Expenses + Premiums >10% Income† | |||
|---|---|---|---|---|---|
| Risk (95% CI) | RR | Risk (95% CI) | RR | ||
| <138% FPL | 2,114 | 18.8% (16.4-21.3) | 26.9* | 29.8% (26.6-33.1) | 5.1* |
| Unmarried | 1,444 | 21.3% (18.0-24.6) | 1.5* | 30.7% (26.9-34.6) | 1.1 |
| Any Employment | 1,670 | 20.8% (17.8-23.8) | 1.7* | 30.3% (26.6-34.0) | 1.1 |
| Full-Year Employment | 1,061 | 25.7% (21.7-29.8) | 2.1* | 33.5% (28.9-38.1) | 1.3* |
| Insurance | |||||
| Uninsured | 369 | 32.3% (25.4-39.3) | 1.4 | 34.7% (27.8-41.7) | 0.51* |
| Public | 1,487 | 14.7% (11.8-17.5) | 0.62* | 18.8% (15.5-22.2) | 0.28* |
| Private | 258 | 23.6% (17.0-30.1) | Ref. | 67.9% (60.9-74.8) | Ref. |
| Newborn Extended Stay | 261 | 21.4% (13.6-29.2) | 1.2 | 36.0% (27.3-44.7) | 1.2 |
| 139-250% FPL | 795 | 7.2% (4.8-9.5) | 10.2* | 26.6% (21.6-31.6) | 4.5* |
| Unmarried | 255 | 8.8% (2.9-14.7) | 1.4 | 24.5% (17.4-31.8) | 0.90 |
| Any Employment | 377 | 7.5% (3.8-11.1) | 1.1 | 24.6% (18.3-30.9) | 0.84 |
| Full-Year Employment | 263 | 7.2% (2.7-11.7) | 1.0 | 24.7% (16.6-32.7) | 0.90 |
| Insurance | |||||
| Uninsured | 116 | 12.5% (5.1-20.0) | 1.3 | 18.8% (9.6-27.9) | 0.46* |
| Medicaid | 311 | 1.5% (0-3.5) | 0.16* | 6.5% (2.8-10.2) | 0.16* |
| Private | 368 | 9.6% (5.7-13.6) | Ref. | 41.1% (33.9-48.2) | Ref. |
| Newborn Extended Stay | 86 | 10.0% (2.4-17.6) | 1.5 | 25.8% (13.3-38.2) | 0.96 |
| 250-400% FPL | 529 | 4.6% (2.1-7.0) | 6.6* | 20.2% (15.6-24.8) | 3.4* |
| Unmarried | 98 | 1.3% (0-4.0) | 0.26 | 10.3% (3.3-17.2) | 0.47* |
| Any Employment | 232 | 5.7% (1.5-9.8) | 1.5 | 18.7% (12.5-24.9) | 0.90 |
| Full-Year Employment | 124 | 7.2% (0.7-13.8) | 1.9 | 22.9% (13.5-32.2) | 1.2 |
| Insurance | |||||
| Uninsured | 41 | 7.8% (0-20.1) | 1.6 | 11.1% (0-24.7) | 0.47* |
| Public | 82 | 0.9% (0-2.7) | 0.19* | 1.3% (0-3.3) | 0.06* |
| Private | 406 | 4.8% (2.1-7.5) | Ref. | 23.5% (18.1-28.9) | Ref. |
| Newborn Extended Stay | 65 | 14.8% (3.8-25.7) | 4.9* | 41.5% (24.9-58.1) | 2.4* |
| >400% FPL | 618 | 0.7% (0.1-1.4) | Ref. | 5.9% (3.6-8.1) | Ref. |
| Unmarried | 41 | 1.5% (0-4.6) | 2.1 | 2.7% (0-6.9) | 0.45 |
| Any Employment | 171 | 0.7% (0-2.0) | 0.88 | 11.9% (4.7-19.1) | 3.4* |
| Full-Year Employment | 90 | 0 (0-0) | 0* | 18.7% (6.9-30.6) | 4.9* |
| Insurance | |||||
| Uninsured | 23 | 1.4% (0-4.1) | 2.0 | 1.4% (0-4.1) | 0.23* |
| Public | 26 | 2.9% (0-8.7) | 4.1 | 3.0% (0-8.7) | 0.49 |
| Private | 569 | 0.7% (0-1.3) | Ref. | 6.1% (3.8-8.5) | Ref. |
| Newborn Extended Stay | 86 | 0.8% (0-2.0) | 1.1 | 6.6% (0.4-12.7) | 1.1 |
RR = risk ratio by dividing risk in subgroup vs inverse or referent group, for overall population for income, and witihin income sub-populations for other characteristics; CI = confidence interval;
p<0.05 by Adjusted Wald test comparison to inverse or referent group
Catastrophic health expenditures defined at family level, annual family out-of-pocket health expenses (with or without premiums) as a percent of annual family income
In assessing trends in catastrophic health expenditures over time (see Figure 2), birth parents had significantly higher annual risk compared with matched controls at all studied time points. After full implementation of the ACA in 2014, the matched controls had significantly lower risk of catastrophic health expenditures by expenses alone from before passage (5.7% in 2014-2016 vs. 7.9% in 2008-2010, p=0.019). The estimated risk was also lower in 2014-2016 for birth parents but did not reach statistical significance (10.7% vs. 8.7%; p=0.13). When including premium out-of-pocket spending, there were no reductions in risk of catastrophic spending over time. When limiting to birth parents and controls living on low incomes, overall risks of catastrophic spending were higher, but time trends were similar for both <138% FPL and <250% FPL. Full implementation of the ACA was associated with reductions in uninsurance (29% to 24%) and gains in Medicaid coverage (15% to 19%) for matched controls relative to pre-ACA years, but no significant changes among birth parents.
Figure 2.
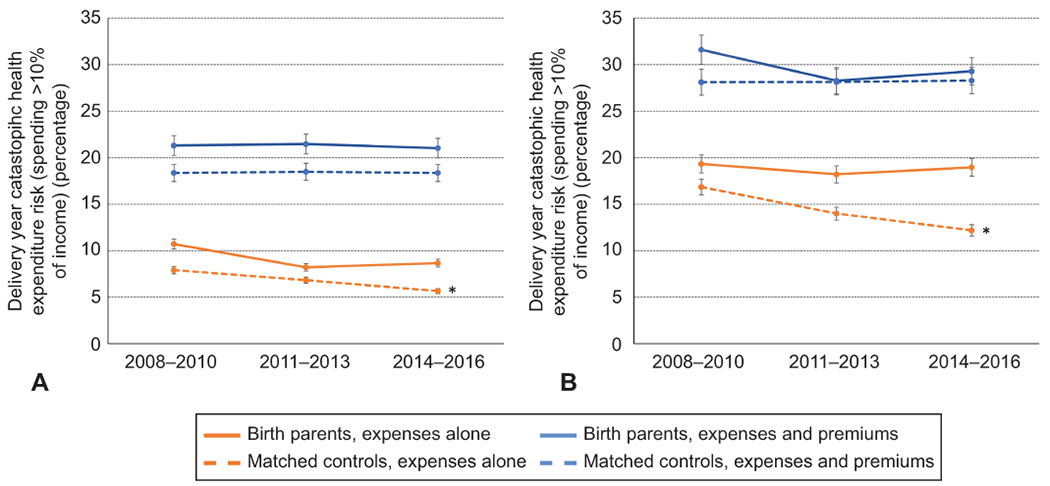
Trends over time in annual risk of catastrophic health expenditure for birth parents and the matched control cohort in the United States, relative to implementation of the Affordable Care Act, Medical Expenditure Panel Survey, 2008–2016. All incomes (A) and income lower than 138% of the federal poverty level (B). *P,.05 for 2014–2016 vs 2008–2010.
Discussion
In this study of a nationally representative survey of the US population, pregnancy and delivery were associated with higher risk of catastrophic health expenditures in the delivery year relative to matched non-pregnant controls. Birth parents in low-income families had the highest risks of catastrophic health expenditure, especially among those living on low incomes and with private insurance. Unemployment and being unmarried during the delivery year were associated with slightly increased risk of catastrophic expenditure for those living on the lowest incomes (≤138% FPL), but not for those in higher income brackets. Extended stay by the newborn beyond the birth parent hospitalization was an independent predictor of catastrophic spending for those living at 250-400% of FPL. Birth parents showed high rates of uptake and loss of Medicaid coverage in the delivery year and public coverage was associated with a lower risk of catastrophic health expenditure at all but the highest income levels. We found no reductions in risks of catastrophic health spending among birth parents with full implementation of the ACA in 2014 relative to pre-ACA years.
Previous studies have sought to determine how pregnancy affects insurance acquisition and retention. Daw, et al first described insurance churn in pregnancy and the postpartum period using MEPS.4 They noted approximately half of women in their cohort who were uninsured prior to pregnancy gained Medicaid or CHIP during pregnancy, but many lost coverage after delivery. More recent research has shown that the ACA has benefited coverage access and continuity in pregnancy. 3,37
Studies of out-of-pocket spending in pregnancy have been fewer. Another recent study examined the effect of ACA implementation on cost for maternity care among privately insured, finding that out-of-pocket costs went up, though mostly among the high-income.38 We similarly found that birth parents did not have lower risk of catastrophic health expenditures after ACA implementation, regardless of income level, and that the privately insured were at relatively high risk for catastrophic spending.
This study demonstrates that birth parents have higher rates of unemployment and insurance churn in the year of a delivery as well as higher risk of catastrophic health expenditures when compared to non-pregnant reproductive-aged controls. While we cannot show causality in our analysis, the interplay of employment, insurance, and health care spending is clearly important. From MEPS, we cannot delineate the reason for unemployment in the delivery year, but possibilities include disability as a result of pregnancy, unaccommodating employers, and new childcare responsibilities. Unemployment was associated with increased risk of catastrophic health expenditure for those living at the lowest income levels only. Given that we considered income at the family level, birth parents with low family incomes likely have less family support, increasing the impact of personal employment on risk of catastrophic health spending. While employment often leads to eligibility for employer-based private insurance, we found that these plans were associated with higher risk of catastrophic spending compared with Medicaid, possibly dampening the benefits of employment in this population.
We found that public insurance (94% of which was Medicaid) was associated with reduced risk of catastrophic health care expenditures for incomes <400% FPL, corresponding to 85% of all birth parents. To qualify for Medicaid, in states that have expanded Medicaid coverage, an individual’s income must be ≤138% FPL. However, in pregnancy many people become eligible for Medicaid given the higher income threshold for eligibility in most states.39 Previously, birth parents lost Medicaid eligibility after 60 days postpartum if they were previously ineligible based on immigration status or income level. The recent American Rescue Plan Act allows states to extend coverage to 12 months postpartum.2,40 However, states are allowed to opt out of this extension and Medicaid expansion, which has been shown to decrease insurance churn in the pregnant population,10 has yet to be adopted by 12 states.41
One interesting finding was that the risk of catastrophic health expenditures only went up with extended newborn admission for birth parents 250-400% FPL, but not at other income levels. This may be in part due to CHIP coverage, which, in most states, allows for newborn care costs to be covered for more of those earning <250% of FPL, but not for many above that threshold.42 This puts those who are >250% of FPL but still not high income (>400% of FPL) under the most financial stress from this situation. Additionally, some commercial insurance cost benefit designs can leave those who are low-income but privately insured vulnerable to catastrophic spending due to annual limits or high deductibles or cost sharing.
While our study provides a national view of catastrophic spending in pregnancy, institutional studies with direct patient assessment could better assess how particular maternal or neonatal complications contribute to health expenditures as well as patient perceived financial toxicity. There is limited data on perceived financial toxicity in the peripartum period. Taylor, et al noted that 60% of peripartum women reported health care unaffordability which was defined as worrying about paying for a medical bill or incurring medical debt and 54.0% reported financial stress defined as worrying about paying their monthly bills.12 In oncology, there is more research about financial toxicity related to treatment, including a standardized patient questionnaire that has been validated to assess for financial burden related to care.43,44,38 However, a recent systematic review noted that current methods used to quantify financial toxicity fail to comprehensively assess financial toxicity, especially in third party payer systems.45 Direct surveys may better identify indirect costs such as parking and childcare for health care visits.46
The strengths of this study include the data source, as MEPS has been used extensively to study health spending with results applicable to the civilian, institutionalized US population. We used an extensive matching algorithm to identify a comparable cohort and maintained independence of observations in the final cohort. This study is limited somewhat by the relatively small sample of respondents with a pregnancy and delivery as a subset of the full cohort of MEPS respondents, limiting the precision of some estimates. Delivery hospitalization information was missing for 13% of the sample, and we lacked detailed clinical data on particular maternal complications or details of neonatal stays to assess the impact of these factors on health spending. We focus our analysis on the delivery year, and thereby include a variable number of months of prenatal and postpartum care, so some of the included health care expenditures were for non-pregnancy related care. Insurance churn with pregnancy affects coverage in non-pregnant months. However, prior research assessing spending in pregnancy and delivery has shown that the vast majority of expenditures are tied to the delivery.39 Lastly, we acknowledge that racial and ethnic disparities play a crucial role in employment status, income, and health. Given that these complex interactions were not the intended focus of this study, the decision was made to defer limited or speculative analysis so that it could be more fully explored in a future study.
Pregnancy, delivery, and the postpartum period are times of high health care utilization and expenditure for birth parents, who are relatively young, healthy, and living on lower incomes compared to the overall US population. Significant reform is necessary to mitigate the risk of catastrophic health expenditures associated with maternal and neonatal care. Further expansion of Medicaid access, and increased subsidization, as well as cost-sharing and benefit design regulation of private insurance plans are potential strategies to reduce financial burdens on parents, particularly for those who are both low-income and privately insured.
Supplementary Material
Acknowledgments
Haley A. Moss is supported by early career funding from the National Institutes of Health (BIRCWH K12HD043446).
Footnotes
Financial Disclosure
The authors did not report any potential conflicts of interest.
Each author has confirmed compliance with the journal’s requirements for authorship.
REFERENCES
- 1.Law A, McCoy M, Lynen R, et al. The prevalence of complications and health care costs during pregnancy. J Med Econ. 2015;18(7):533–541. doi: 10.3111/13696998.2015.1016229 [DOI] [PubMed] [Google Scholar]
- 2.Ranji U, Gomez I, Salganicoff A. Expanding Postpartum Medicaid Coverage. Kaiser Family Foundation. Published 2021. Accessed May 10, 2021. https://www.kff.org/womens-health-policy/issue-brief/expanding-postpartum-medicaid-coverage/ [Google Scholar]
- 3.Daw JR, Sommers BD. The Affordable Care Act and Access to Care for Reproductive-Aged and Pregnant Women in the United States, 2010-2016. Am J Public Health. 2019;109(4):565–571. doi: 10.2105/AJPH.2018.304928 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Daw JR, Hatfield LA, Swartz K, Sommers BD. Women In The United States Experience High Rates Of Coverage ‘Churn’ In Months Before And After Childbirth. Health Aff. 2017;36(4):598–606. doi: 10.1377/hlthaff.2016.1241 [DOI] [PubMed] [Google Scholar]
- 5.Chatterjee S, Kotelchuck M, Sambamoorthi U. Prevalence of Chronic Illness in Pregnancy, Access to Care, and Health Care Costs. Implications for Interconception Care. Women’s Heal Issues. 2008;18(6 SUPPL.):S107–S116. doi: 10.1016/j.whi.2008.06.003 [DOI] [PubMed] [Google Scholar]
- 6.U.S. Department of Health and Human Servicies. Compliation of Patient Protection and Affordable Care Act. Accessed June 14, 2021. https://www.hhs.gov/sites/default/files/ppacacon.pdf
- 7.Lee LK, Chien A, Stewart A, et al. Women’s Coverage, Utilization, Affordability, And Health After The ACA: A Review Of The Literature. Health Aff. 2020;39(3):387–394. doi: 10.1377/hlthaff.2019.01361 [DOI] [PubMed] [Google Scholar]
- 8.Johnston EM, McMorrow S, Thomas TW, Kenney GM. ACA medicaid expansion and insurance coverage among new mothers living in poverty. Pediatrics. 2020;145(5). doi: 10.1542/PEDS.2019-3178 [DOI] [PubMed] [Google Scholar]
- 9.Margerison CE, MacCallum CL, Chen J, Zamani-Hank Y, Kaestner R. Impacts of Medicaid Expansion on Health Among Women of Reproductive Age. Am J Prev Med. 2020;58(1):1–11. doi: 10.1016/j.amepre.2019.08.019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Daw JR, Winkelman TNA, Dalton VK, Kozhimannil KB, Admon LK. Medicaid expansion improved perinatal insurance continuity for low-income women. Health Aff. 2020;39(9):1531–1539. doi: 10.1377/hlthaff.2019.01835 [DOI] [PubMed] [Google Scholar]
- 11.Chua KP, Fendrick AM, Conti RM, Moniz MH. Out-of-pocket spending for deliveries and newborn hospitalizations among the privately insured. Pediatrics. 2021;148(1). doi: 10.1542/PEDS.2021-050552/179972 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Taylor K, Compton S, Kolenic GE, et al. Financial Hardship Among Pregnant and Postpartum Women in the United States, 2013 to 2018. JAMA Netw Open. 2021;4(10):e2132103–e2132103. doi: 10.1001/JAMANETWORKOPEN.2021.32103 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.McMorrow S, Johnston EM, Thomas T, Kenney GM. Changes in New Mothers’ Health Care Access and Affordability under the Affordable Care Act; 2020. Accessed June 1, 2021. https://www.urban.org/research/publication/changes-new-mothers-health-care-access-and-affordability-under-affordable-care-act
- 14.Collins SR, Gunja MZ, Aboulafia GN. U.S. Health Insurance Coverage in 2020: A Looming Crisis in Affordability — Findings from the Commonwealth Fund Biennial Health Insurance Survey, 2020. Published 2020. Accessed September 4, 2020. https://www.commonwealthfund.org/sites/default/files/2020-08/Collins_looming_crisis_affordability_biennial_2020_sb.pdf
- 15.[Dataset]* Medical Expenditure Panel Survey (MEPS). Agency for Healthcare Research and Quality https://www.meps.ahrq.gov/mepsweb/data_stats/download_data_files.jsp [PubMed]
- 16.Cohen JW, Cohen SB, Banthin JS. The medical expenditure panel survey: a national information resource to support health care cost research and inform policy and practice. Med Care. 2009;47(7 Suppl 1). doi: 10.1097/MLR.0b013e3181a23e3a [DOI] [PubMed] [Google Scholar]
- 17.Blumenthal D, Collins SR, Fowler EJ. The Affordable Care Act at 10 Years - Its Coverage and Access Provisions. N Engl J Med. 2020;382(10):963–969. doi: 10.1056/NEJMhpr1916091 [DOI] [PubMed] [Google Scholar]
- 18.Agency for Healthcare Research and Quality. MEPS HC-192 2016 Full Year Consolidated Data File Documentation.; 2018. [Google Scholar]
- 19.Quan H, Sundararajan V, Halfon P, et al. Coding algorithms for defining comorbidities in ICD-9-CM and ICD-10 administrative data. Med Care. 2005;43(11):1130–1139. doi: 10.1097/01.mlr.0000182534.19832.83 [DOI] [PubMed] [Google Scholar]
- 20.Bateman BT, Mhyre JM, Hernandez-Diaz S, et al. Development of a comorbidity index for use in obstetric patients. Obstet Gynecol. 2013;122(5):957–965. doi: 10.1097/AOG.0B013E3182A603BB [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Goldman AL, Woolhandler S, Himmelstein DU, Bor DH, McCormick D. Out-of-pocket spending and premium contributions after implementation of the affordable care act. JAMA Intern Med. 2018;178(3):347–355. doi: 10.1001/jamainternmed.2017.8060 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Bigelow JH, Fonkych K. Interpreting MEPS-Based Estimates. In: Analysis of Healthcare Interventions That Change Patient Trajectories. RAND Corporation; 2005:57–86. [Google Scholar]
- 23.Austin PC. Optimal caliper widths for propensity-score matching when estimating differences in means and differences in proportions in observational studies. Pharm Stat. 2011;10(2):150–161. doi: 10.1002/pst.433 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Austin PC, Jembere N, Chiu M. Propensity score matching and complex surveys. Stat Methods Med Res. 2018;27(4):1240–1257. doi: 10.1177/0962280216658920 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Austin PC. An Introduction to Propensity Score Methods for Reducing the Effects of Confounding in Observational Studies. Multivariate Behav Res. 2011;46(3):399–424. doi: 10.1080/00273171.2011.568786 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Medical Expenditure Panel Survey (MEPS). Published online 2020. https://www.meps.ahrq.gov/mepsweb/data_stats/download_data_files.jsp
- 27.Bernard DSM, Farr SL, Fang Z. National estimates of out-of-pocket health care expenditure burdens among nonelderly adults with cancer: 2001 to 2008. J Clin Oncol. 2011;29(20):2821–2826. doi: 10.1200/JCO.2010.33.0522 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Anspach D. Current and Past Medicare Part B Premiums. The Balance. Published 2021. Accessed January 8, 2020. https://www.thebalance.com/current-and-historical-medicare-part-b-premiums-2388483
- 29.Brooks T, Miskell S, Artiga S, Cornachione E, Gates A. Medicaid and CHIP Eligibility, Enrollment, Renewal, and Cost-Sharing Policies as of January 2016: Findings from a 50-State Survey.; 2016. Accessed August 25, 2020. http://files.kff.org/attachment/report-medicaid-and-chip-eligibility-enrollment-renewal-and-cost-sharing-policies-as-of-january-2016-findings-from-a-50-state-survey
- 30.CPI Inflation Calculator. Published online 2020. Accessed August 25, 2020. https://www.bls.gov/data/inflation_calculator.htm
- 31.Banthin JS, Bernard DM. Changes in financial burdens for health care: National estimates for the population younger than 65 years, 1996 to 2003. J Am Med Assoc. 2006;296(22):2712–2719. doi: 10.1001/jama.296.22.2712 [DOI] [PubMed] [Google Scholar]
- 32.Khera R, Valero-Elizondo J, Okunrintemi V, et al. Association of out-of-pocket annual health expenditures with financial hardship in low-income adults with atherosclerotic cardiovascular disease in the United States. JAMA Cardiol. 2018;3(8):729–738. doi: 10.1001/jamacardio.2018.1813 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Research Findings #27: Health Care Expenditures for Uncomplicated Pregnancies. August 2007. Agency for Healthcare Research and Quality,. Rockville, MD. http://www.meps.ahrq.gov/data_files/publications/rf27/rf27.shtml [Google Scholar]
- 34.Blumenthal D, Abrams M. The Affordable Care Act at 10 Years - Payment and Delivery System Reforms. N Engl J Med. 2020;382(11):1057–1063. doi: 10.1056/NEJMhpr1916092 [DOI] [PubMed] [Google Scholar]
- 35.Von Elm E, Altman DG, Egger M, Pocock SJ, Gøtzsche PC, Vandenbroucke JP. The Strengthening the Reporting of Observational Studies in Epidemiology (STROBE) statement: Guidelines for reporting observational studies. Ann Intern Med. 2007;147(8):573–577. doi: 10.7326/0003-4819-147-8-200710160-00010 [DOI] [PubMed] [Google Scholar]
- 36.Martin JA, Hamilton BE, Osterman MJ, Driscoll AK, Drake P. Births: Final Data for 2016. Natl Vital Stat Reports. 2018;67(1):1–55. https://pubmed.ncbi.nlm.nih.gov/29775434/ [PubMed] [Google Scholar]
- 37.Clapp MA, James KE, Kaimal AJ, Sommers BD, Daw JR. Association of Medicaid Expansion With Coverage and Access to Care for Pregnant Women. Obstet Gynecol. 2019;134(5):1066–1074. doi: 10.1097/AOG.0000000000003501 [DOI] [PubMed] [Google Scholar]
- 38.Moniz MH, Fendrick AM, Kolenic GE, Tilea A, Admon LK, Dalton VK. Out-of-pocket spending for maternity care among women with employer-based insurance, 2008–15. Health Aff. 2020;39(1):18–23. doi: 10.1377/hlthaff.2019.00296 [DOI] [PubMed] [Google Scholar]
- 39.Centers for Medicare and Medicaid Services. Medicaid, Children’s Health Insurance Program, & Basic Health Program Eligibility Levels. Accessed December 12, 2021. https://www.medicaid.gov/medicaid/national-medicaid-chip-program-information/medicaid-childrens-health-insurance-program-basic-health-program-eligibility-levels/index.html
- 40.117th Congress. H.R.1319 - American Rescue Plan Act of 2021. Accessed June 14, 2021. https://www.congress.gov/bill/117th-congress/house-bill/1319/text?q=%7B%22search%22%3A%5B%22hr+1319%22%5D%7D&r=1&s=1 .
- 41.Status of State Medicaid Expansion Decisions: Interactive Map. Kaiser Family Foundation. Published 2020. Accessed February 2, 2020. https://www.kff.org/medicaid/issue-brief/status-of-state-medicaid-expansion-decisions-interactive-map/ [Google Scholar]
- 42.Medicaid and CHIP Eligibility, Enrollment, Renewal, and Cost-Sharing Policies as of January 2016: Findings from a 50-State Survey. Published 2016. Accessed August 25, 2020. https://www.kff.org/report-section/medicaid-and-chip-eligibility-enrollment-renewal-and-cost-sharing-policies-as-of-january-2016-premiums-and-cost-sharing/
- 43.de Souza JA, Yap BJ, Hlubocky FJ, et al. The development of a financial toxicity patient-reported outcome in cancer: The COST measure. Cancer. 2014;120(20):3245–3253. doi: 10.1002/cncr.28814 [DOI] [PubMed] [Google Scholar]
- 44.de Souza JA, Yap BJ, Wroblewski K, et al. Measuring financial toxicity as a clinically relevant patient-reported outcome: The validation of the COmprehensive Score for financial Toxicity (COST). Cancer. 2017;123(3):476–484. doi: 10.1002/cncr.30369 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Witte J, Mehlis K, Surmann B, et al. Methods for measuring financial toxicity after cancer diagnosis and treatment: a systematic review and its implications. Ann Oncol. 2019;30(7):1061–1070. doi: 10.1093/ANNONC/MDZ140 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Lee A, Shah K, Chino F. Assessment of Parking Fees at National Cancer Institute-Designated Cancer Treatment Centers. JAMA Oncol. 2020;6(8):1295–1297. doi: 10.1001/jamaoncol.2020.1475 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


