Abstract
Significance:
Cannabis use is increasing among cigarette smokers. If cannabis use is associated with cigarette dependence, a barrier to smoking cessation, this could have public health implications for tobacco control. The current study estimated the prevalence of cigarette dependence among United States (US) individuals who smoke cigarettes by cannabis use status, and investigated trends in cigarette dependence from 2002 to 2019 among cigarette smokers by cannabis use status and cigarette consumption (i.e., cigarettes per day, CPD).
Methods:
Data were drawn from the 2002–2019 annual National Survey on Drug Use and Health (NSDUH) and included US individuals ages 12+ who used cigarettes at least once in the past month (n=231,572). Logistic regression was used to estimate the prevalence of cigarette dependence, measured as Time to First Cigarette (TTFC) <30 minutes, by past-month cannabis use (no use, non-daily use, daily use), and to estimate trends in cigarette dependence from 2002 to 2019 overall, and stratified by cannabis use and smoking level (light, 1–5 CPD; moderate, 6–15 CPD; heavy, 16+ CPD).
Results:
Across all levels of cigarette use, cigarette dependence was significantly more common among individuals with daily cannabis use compared with those with non-daily or no cannabis use. From 2002 to 2019, cigarette dependence increased among cigarette smokers with non-daily cannabis use, and among light and moderate cigarette smokers with no cannabis use.
Conclusions:
US individuals who use both cigarettes and cannabis report a higher prevalence of cigarette dependence relative to individuals who use cigarettes and do not use cannabis at virtually all levels of cigarette consumption. Further, cigarette dependence is increasing in the US both among those who use and do not use cannabis. Given the increase in cannabis use among those using cigarettes, efforts to elucidate the nature of the association of cannabis and cigarette dependence are needed.
Keywords: co-substance use, nicotine, cigarettes, addiction, public policy
INTRODUCTION
Despite declines in cigarette use, tobacco-related disease remains the leading cause of preventable disease and premature mortality in the United States (US) and a leading cause globally [1–3]. While cigarette use continues to decrease in many countries [2, 4], including the US (e.g., decrease from 22.5% in 2002 to 14.0% in 2019 [5, 6]), cannabis use is increasing globally [7] and in the US (e.g., increase in use from 10.4% in 2002 to 15.3% in 2017 and daily use from 1.9% in 2002 to 4.2% in 2017 [8]). Cigarette use is associated with increased likelihood of cannabis use and more frequent cannabis use [9–11]. Conversely, cannabis use is associated with greater likelihood of cigarette use [12–14] and heavier cigarette use [15], and cannabis use is associated with increased risk of cigarette initiation, lower cigarette quit rates, and increased risk of cigarette relapse [16–18]. The well-documented health risks associated with cigarette use [1, 19] appear to be intensified with use of both cigarettes and cannabis compared to use of cigarettes alone [20, 21].
Recent findings indicate that cigarette quit rates are lower among US individuals who use versus do not use cannabis [17]. The reasons underlying the lower quitting among those using cigarettes and cannabis are not yet clear. One possibility is that there is a link between cannabis use and smoking-related factors such as cigarette dependence which occurs among a subgroup of those using cigarettes and is often characterized by intense cravings and withdrawal symptoms [22]. Cigarette dependence is widely considered to be the primary barrier to smoking cessation [23, 24]. The use of cannabis may contribute to cigarette dependence through any number of direct (e.g., endocannabinoid system) or indirect (e.g., greater use of tobacco products leading to increased nicotine exposure) pathways among persons who use both cannabis and cigarettes, compared with those using cigarettes alone. As such, it is conceivable that cigarettes and cannabis co-use may increase levels of cigarette dependence relative to those who use cigarettes and not cannabis.
Few studies have directly investigated the relationship between cannabis use and cigarette dependence. Available evidence has been inconsistent with several, but not all [15], studies suggesting cannabis use is associated with higher levels of cigarette dependence [25–27]. Time to First Cigarette (TTFC), an item from the Fagerström Test for Nicotine Dependence (FTND)[28], later renamed the Fagerström Test for Cigarette Dependence (FTCD)[29], assesses how long an individual goes before having the first cigarette of the day [28]. Shorter TTFC (i.e., a shorter number of minutes to the first cigarette) is associated with greater cigarette exposure and poorer smoking cessation outcomes [30, 31] as well as smoking-related health consequences [31–35]. The TTFC demonstrated the strongest predictive validity related to cessation outcomes among the items of the FTCD suggesting that it is a useful one-item measure of cigarette dependence [36].
To date, prior studies have not examined the relationship between cannabis use and cigarette dependence by level of cigarette consumption (i.e., cigarettes per day (CPD)). Since level of nicotine exposure is directly related to likelihood of cigarette dependence, if people who use cannabis also have greater cigarette consumption, then the association between cannabis use and cigarette dependence may be attributable to a higher level of nicotine use, not with cannabis specifically. Examining differences in the relationship between cannabis use and cigarette dependence by smoking level can help clarify whether a relationship between cannabis use and cigarette dependence is driven by heavier smoking levels, or whether cannabis use is associated with elevated cigarette dependence across levels of low and high cigarette use.
The overall goal of this study was to investigate whether cannabis use is associated with cigarette dependence overall and further to estimate the degree to which these relationships are modified by level of cigarette consumption (assessed with CPD) and cannabis use frequency (assessed by days/month of use). The first aim was to examine, among US individuals ages 12 and older who smoke cigarettes, whether cigarette dependence (assessed as <30 minutes TTFC) was more common among those who use cannabis versus do not use cannabis, and whether this relationship varies by cannabis use frequency (daily vs. non-daily vs. none) and/or level of smoking (i.e., CPD), using combined data from 2002 to 2019. The second aim of the study was to estimate, among US individuals ages 12 or older who smoke cigarettes, whether the prevalence of cigarette dependence changed differentially over time from 2002 to 2019 by cannabis use status, and whether these trends varied by level of cigarette smoking (i.e., CPD) or cannabis use frequency (daily vs. non-daily vs. none).
METHODS
Data source and study population
Data came from the National Survey on Drug Use and Health (NSDUH; [37, 38]). The NSDUH collects yearly cross-sectional data from non-institutionalized civilians ages 12 and older in each of the 50 US states and the District of Columbia. The current analyses were conducted on data from 2002 to 2019 extracted from the public data portal (http://datafiles.samhsa.gov/). The analytic sample included respondents who reported cigarette use in the past month (combined sample 2002–2019, n=231,572). This study used de-identified epidemiologic data that were available in a public, open access repository and was not subject to IRB review.
Measures
Cannabis use.
Respondents were asked how long it had been since their last cannabis use. Individuals reporting using cannabis “within the past 30 days” were categorized as having past-month cannabis use while individuals who did not report using cannabis “within the past 30 days” were classified has having no past-month cannabis use. Respondents with past-month cannabis use were further classified into two mutually exclusive groups: daily cannabis use (reported using cannabis 30 days out of the past 30 days) and non-daily cannabis use (reported using cannabis 29 or fewer days out of the past 30 days).
Cigarette use.
All respondents in the analytic sample had to report past-month cigarette use (i.e., using cigarettes “within the past 30 days”). Respondents were asked how many CPD they consumed on average and were classified into three mutually exclusive groups based on their level of daily cigarette consumption: 1–5 CPD (light), 6–15 CPD (moderate), 16 or more CPD (heavy), consistent with other research.[39]
TTFC.
Cigarette dependence was assessed using the TTFC, an item from the FTCD, that assesses how long, in minutes, an individual goes before having the first cigarette of the day [28]. For this study, cigarette dependence was indicated by report of having the first cigarette of the day in less than 30 minutes (TTFC <30 minutes) similar to past research.[35, 39, 40]
Sociodemographics.
Sociodemographics included age (12–17, 18–25, 26–34, 35 and older), gender (male, female), race/ethnicity (non-Hispanic (NH) White, NH Black, Hispanic, NH Other (i.e., all other races, more than one race)), and total annual family income (<$20,000, $20,000-$74,999, ≥$75,000).
Statistical analysis
To examine the first aim of our study, descriptive statistics were generated showing the prevalence of cigarette dependence by cannabis use status overall and stratified by level of cigarette smoking for the combined 2002–2019 data. Logistic regression models were used to estimate odds ratios and 95% confidence intervals comparing the prevalence of cigarette dependence based on cannabis use status (daily cannabis use vs. non-daily use; daily cannabis use vs. no use; and non-daily cannabis use vs. no use), unadjusted and adjusted for sociodemographic covariates (i.e., age, gender, race/ethnicity, income) and survey year.
To examine the second aim of our study, the prevalence of cigarette dependence among those using cigarettes by CPD from 2002 and 2019 were calculated and linear trends of cigarette dependence by CPD were tested by crude and adjusted logistic regressions with year included as a continuous predictor. To determine the differential time trend between different cannabis use groups, logistic regression models with continuous year as predictor were used to test for the interactions and F-test results were generated. Next, the prevalence of cigarette dependence among those using cigarettes by CPD stratified by current cannabis use status over time were generated and the rate of change in the cigarette dependence among smokers by CPD stratified by current cannabis use status were examined through crude and adjusted logistic regressions with year included as a continuous predictor. To determine the differential time trend between different CPD groups stratified by cannabis use status, logistic regression models with continuous year as predictor were used to test for the interactions and F-test results were generated. The rate of change in cigarette dependence prevalence among those with current cannabis use and current cigarette use were examined by multivariable logistic regression. Analyses were run unadjusted and adjusted for sociodemographic covariates (i.e., age, gender, race/ethnicity, income). All analyses used appropriate sample weights to correct for the differences in the probability of selection and adjusted for survey design effects to obtain accurate standard errors via SAS (Version 9.4) survey procedures.
RESULTS
Sample characteristics
Just over half of the analytic sample identified as male (54.0%) while over two-thirds identified their race/ethnicity as NH White (70.5%; NH Black, 12.0%; Hispanic, 12.1%; NH Other, 5.4%). Over half of the sample were ages 35 or older (57.4%; 12–17 years old, 3.4%; 18–25 years old, 19.0%; 26–34 years old, 20.3%) and over half of the sample reported a total annual family income of $20,000 to $74,999 (53.0%; <$20,000, 25.5%; ≥$75,000, 21.5%). Regarding past-month cannabis use, 80.7% of respondents reported no cannabis use, 15.0% reported non-daily cannabis use, and 4.3% reported daily cannabis use. A total of 40.8% of respondents reported using 1–5 CPD, 27.7% reported 6–15 CPD, and 31.6% reported 16 or more CPD.
Cigarette dependence by cannabis use (combined 2002–2019 data)
Table 1 presents the association between past-month cannabis use status and cigarette dependence overall and by cigarettes smoked per day. Those with current cigarette smoking and cannabis use were significantly more likely to report cigarette dependence compared with those with current cigarette smoking and no cannabis use or non-daily cannabis use. In unadjusted analyses, cigarette dependence was significantly more common among current cigarette smokers with no current cannabis use compared with current cigarette smokers with non-daily cannabis use. In adjusted analyses, this effect was reversed whereby the prevalence of cigarette dependence was higher among those with cigarette smoking and non-daily cannabis use than among those with cigarette smoking and no cannabis use. When the association between cannabis use and cigarette dependence was stratified by CPD, daily cannabis users reported higher rates of cigarette dependence at every level of smoking, compared with non-daily cannabis users and those not using cannabis. Further, non-daily cannabis users showed higher rates of cigarette dependence than those not using cannabis for those with moderate (6–15 CPD) and heavy (16+ CPD) cigarette smoking, but not light (1–5 CPD) smoking.
Table 1.
Prevalence of cigarette dependence by past-month cannabis use status and by cigarettes smoked per day (combined 2002–2019 NSDUH data; n=231,572, ages 12+)
| No Cannabis Use | Non-daily Cannabis Use | Daily Cannabis Use | Non-Daily Cannabis Use vs. No Cannabis Use OR/aOR (95% CI) | Daily Cannabis Use vs. No Cannabis Use OR/aOR (95% CI) | Daily Cannabis Use vs. Non-Daily Cannabis Use OR/aOR (95% CI) | |
|---|---|---|---|---|---|---|
| Full sample | 49.6% (se=0.22) | 44.9% (se=0.40) | 58.5% (se=0.66) | OR=0.8 (0.80–0.86) aOR=1.1 (1.03–1.11) | OR=1.4 (1.35–1.52) aOR=1.9 (1.81–2.06) | OR=1.7 (1.64–1.83) aOR=1.8 (1.72–1.94) |
| Cigarettes per day | ||||||
| 1–5 CPD | 20.3% (se=0.23) | 18.7% (se=0.47) | 29.2% (se=0.98) | OR=0.9 (0.84–0.96) aOR=0.9 (0.89–1.03) | OR=1.6 (1.45–1.79) aOR=1.7 (1.50–1.86) | OR=1.8 (1.60–1.99) aOR=1.7 (1.55–1.93) |
| 6–15 CPD | 54.2% (se=0.39) | 56.8% (se=0.84) | 62.2% (se=1.22) | OR=1.1 (1.03–1.20) aOR=1.1 (1.06–1.23) | OR=1.4 (1.25–1.54) aOR=1.4 (1.29–1.59) | OR=1.3 (1.11–1.41) aOR=1.2 (1.07–1.39) |
| 16+ CPD | 79.7% (se=0.34) | 81.0% (se=0.57) | 83.8% (se=0.97) | OR=1.1 (1.01–1.18) aOR=1.2 (1.22–1.31) | OR=1.3 (1.14–1.53) aOR=1.5 (1.32–1.79) | OR=1.2 (1.03–1.42) aOR=1.2 (1.05–1.46) |
Key: aOR, adjusted odds ratio; CI, confidence intervals; CPD, cigarettes per day; NSDUH, National Survey on Drug Use and Health; OR, odds ratio; se, standard error
Notes: Sample included respondents who reported past-month cigarette use. Cigarette dependence was defined as the time to the first cigarette of <30 minutes. Multivariable models adjusted for age (12–17, 18–25, 26–34, 35 and older), gender (male, female), race/ethnicity (non-Hispanic (NH) White, NH Black, Hispanic, NH Other), family income (<$20.000, $20,000–$74.999, >$75,000), and survey year.
Trends in cigarette dependence by cannabis use, 2002 to 2019
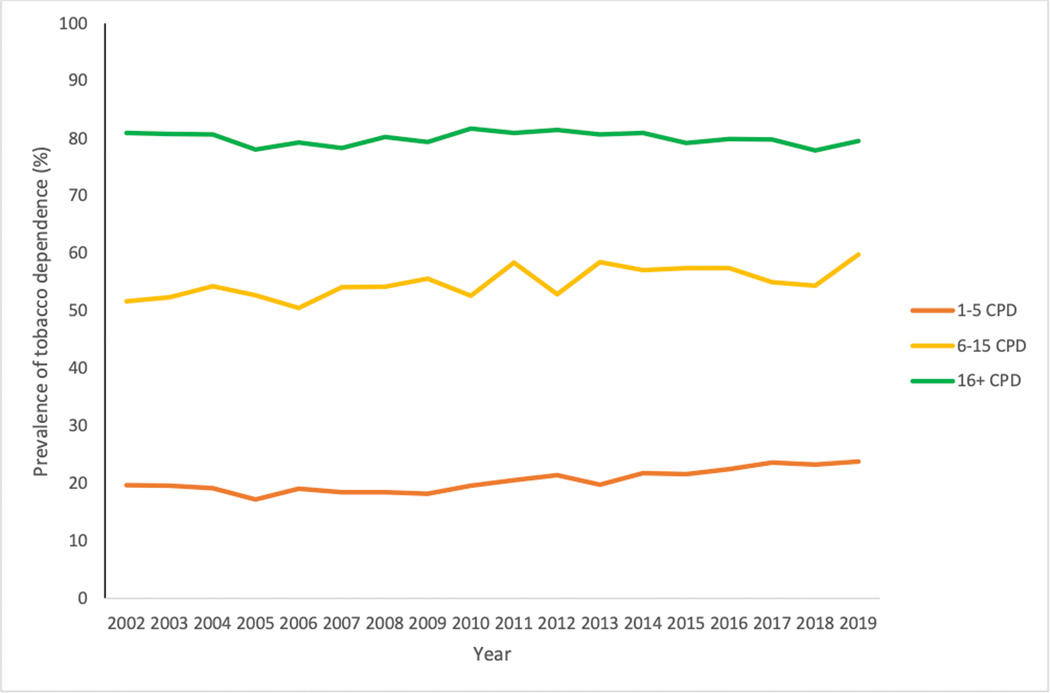
Figure 1 and Supplemental Table 1 present the prevalence of cigarette dependence among those with current cigarette smoking stratified by CPD from 2002 to 2019. Cigarette dependence increased from 2002 to 2019 among those with light and moderate smoking (1–5 and 6–15 CPD), with no change among those with heavier smoking (16+ CPD).
Figure 1. Prevalence of cigarette dependence stratified by cigarettes per day (CPD), NSDUH 2002–2019.
Notes. Adjusted for age (12–17, 18–25, 26–34, 35 and older), gender (male, female) and race (non-Hispanic (NH) White, NH Black, Hispanic, NH Other) and family income (<$20,000, $20,000–$74.999, >$75,000). Cigarette dependence was defined as self-report of having the first cigarette of the day in less than 30 minutes.
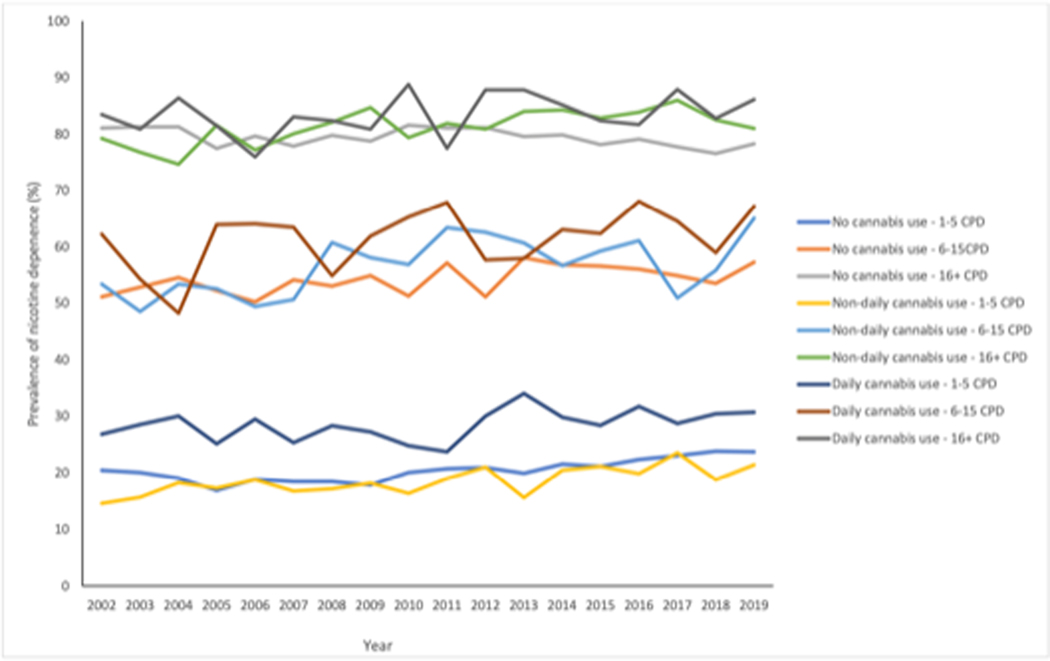
Figure 2 and Supplemental Table 2 present the prevalence of cigarette dependence among those with current cigarette smoking stratified by both CPD and cannabis use status from 2002 to 2019. Among daily cannabis users, the linear trend over time for cigarette dependence was not significant for any level of CPD. Among non-daily cannabis users, cigarette dependence increased among those with light (1–5 CPD), moderate (6–15 CPD) and heavy (16+CPD) smoking, with no significant differences in the rate of increase among CPD groups. The prevalence of cigarette dependence increased among those with no cannabis use and light (1–5 CPD) or moderate (6–15 CPD) smoking, and the rate of increase did not differ for these two groups, while there was no significant change in cigarette dependence over time for those with no cannabis use and heavy (16+CPD) smoking.
Figure 2. Prevalence of cigarette dependence stralified by cigarette per day (CPD) and cannabis use status, NSDUH 2002–2019.
Notes. Adjusted for age (12–17, 18–25, 26–34, 35 and older), gender (male, female) and race (non-Hispanic (NH) White, NH Black, Hispanic, NH Other) and family income (<$20,000, $20,000-$74,999, >$75,000), Cigarette dependence was defined as self-report of having the first cigarette of the day in less than 30 minutes.
DISCUSSION
The study has a number of important findings. First, among US individuals, cigarette dependence was significantly more common among cigarette smokers who use cannabis daily (58.5%), compared with non-daily cannabis use (44.9%) and no cannabis use (49.6%). The elevated prevalence was consistent across light, moderate, and heavy cigarette consumption levels. Second, a dose-response relationship was evident whereby at each CPD level, cigarette dependence was higher among those who use cannabis compared with those who do not use cannabis. Third, over time, the prevalence of cigarette dependence did not change among those with daily cannabis use across all cigarette consumption levels. Fourth, over time, cigarette dependence increased among those with non-daily cannabis use across cigarette consumption levels. Fifth, cigarette dependence also increased among those who did not use cannabis across all cigarette consumption levels over time, except among the heaviest smokers among whom cigarette dependence remained stable. The increase in cigarette dependence among those with light and moderate smoking is consistent with previous findings through 2015 [39] and extends those findings by showing this trend through 2019.
While cannabis was associated with a higher prevalence of cigarette dependence, the increase in cigarette dependence over time among those both with and without cannabis use raises questions about whether there could be other factors, beyond cannabis, contributing to this rise in cigarette dependence in the population. These may be factors that are related to cannabis use or factors that are unrelated to cannabis use directly (i.e., impact those who both do and do not use cannabis) but occur more frequently among those who use cannabis (e.g., use of alternative, newer tobacco products; smoking-related behaviors such as frequency of smoking; mental health problems such as depression) [41–44]. For example, the measure of cigarette smoking included both daily and non-daily cigarette use. Non-daily cigarette smokers are becoming a larger proportion of the smoking population, demonstrate different patterns of cigarette dependence (e.g., past daily smoking versus no past daily smoking [45]), and are more likely to report use of non-cigarette tobacco products (e.g., hookah, cigars [46]). Future research can work to identify these factors and examine their role in the increases seen in cigarette dependence. In addition, it may be useful examine cigarette dependence and cigarette consumption separately among those who use fewer cigarettes per day (e.g., concurrent use of other tobacco products; cutting down to a small number of CPD and then augmenting with other tobacco products; using cannabis to try to decrease CPD) [39], and among those at higher levels of cigarette consumption.
Though it is not possible to identify the reasons that cigarette dependence would be increasing over time from these data alone, there are several potential biological/genetic, environmental/social, and drug-related factors that may underlie the relationship between cannabis use and cigarette dependence (see [47–50] for reviews). With regard to biological factors, preclinical research [48] has demonstrated that the endocannabinoid system is involved in nicotine-related reward so that cannabis use may be linked with experiencing greater reward and reinforcement for nicotine use. Perkins and colleagues [51] found that young adults with a self-reported lifetime history of cannabis use reported greater reward from nicotine nasal spray compared to those without lifetime cannabis use in a laboratory study of 131 US adults age 21 to 39, but more human research is needed. Common genetic factors related to both disinhibition and sensation seeking have been identified; and cannabis and cigarette use are both strongly predicted by these behaviors as well as by drug-related positive reinforcement. Environmental/social factors may include peer influences (e.g., peer use of both cannabis and cigarettes, living with those using cigarettes and/or cannabis) and availability of drugs (e.g., greater accessibility to cannabis).
Drug-related factors, where exposure to cannabis may increase exposure to nicotine, may also play a role in the relationship of cannabis and cigarette use. Exposure to nicotine for those using cannabis can happen in a number of intentional or unintentional ways. The most common route of administration is smoking for both cannabis and cigarettes. Cannabis administration can occur through joints that only include cannabis, by mixing tobacco in with cannabis to create spliffs (also known as mulled cigarettes), or by adding cannabis to a hollowed out cigar to create blunts.[52] In several studies, the majority of participants reporting cannabis use reported spliff/mulled cigarette or blunt use (e.g., 81.7% of 881 Swiss adolescents [53]; 64.4% of 340 US adults in substance use disorder treatment in California [54]). While those who use blunts likely have lower exposure to nicotine [55] than those who mix tobacco and cannabis together directly, the nicotine content of cigar wrappers is 1.2–6.0mg [56] and so those using blunts are exposed to some level of nicotine and more than if they used cannabis alone.
Little is known about the relationship between modes of tobacco and cannabis co-use (e.g., blunts, spliffs) and cigarette dependence, but one study found that higher interrelatedness of cigarette and cannabis use (assessed using an author-developed scale that examined factors such as the concurrent or sequential use of both substances and use of one substance to increase effects of the other substance) was associated with higher cigarette dependence, measured by the FTCD, compared with lower interrelatedness [57]. Notably, this sample included US individuals and fewer individuals who use cannabis in American countries report using tobacco and cannabis together such as through blunts or spliffs (e.g., 4.4% in the US, 6.9% in Mexico, 16.0% in Canada) compared to individuals who use cannabis in other countries (e.g., 51.6% in Australia, 77.0–77.2% in the United Kingdom, 94% in Italy, see [58, 59]). More research is needed to understand the relationship between cigarette dependence among those who co-administer tobacco and cannabis simultaneously versus other types of tobacco-cannabis co-use (e.g., not co-administered).
The relationship between cannabis use and cigarette dependence could have critical clinical and public health implications. First, dependence is the primary barrier to quitting cigarettes [23], so an increase in cigarette dependence among smokers may suggest that a larger proportion of smokers will have a difficult time quitting smoking. Cessation of both tobacco and cannabis may lead to the best outcomes for both substances and there is evidence for the feasibility and acceptability of treatments that target both cigarettes and cannabis [60–64] and preliminary evidence for resulting decreases in tobacco use or cigarette dependence [60, 61, 63, 65]. Second, as cannabis use continues to increase and increasingly legalized, it may be beneficial to consider cannabis in tobacco control efforts. For instance, Quitlines, available in every US state, could assess for cannabis use and incorporate information about cannabis use when working with callers to quit cigarette use. Similarly, public service announcements related to tobacco could include information for community members about higher levels of cigarette dependence associated with cannabis use. It may also be useful for cannabis-related policy to consider the relationship between cannabis and cigarette dependence (e.g., policies to prohibit sales of tobacco and cannabis in the same location).
While the current study was conducted in the US, cannabis use is increasing globally [7], so the relationship between cannabis and cigarette dependence may be an important consideration in a range of countries trying to reduce the burden and consequences of cigarette use. There are differences among countries in the prevalence of cigarette smoking (e.g., 13.1% in the US versus 20.9%−24.2% in Europe and 4.7–13.6% in Africa [66]) and cannabis use (e.g., 12.4% in North America versus 5.2% in Europe and 7.5% in Africa [66]) as well as differences in norms/attitudes about and legalization of cannabis (e.g., [67, 68]). Future research should examine both the relationships between cannabis use and cigarette dependence and the role of cannabis-related attitudes and legalization [69] in the relationship of cannabis use and cigarette dependence across a range of countries.
Limitations should be noted. First, these results may not generalize to those outside of the US or US individuals not eligible for the NSDUH study (e.g., institutionalized individuals). Relatedly, this study focused on cigarette dependence and results may not apply to dependence on other nicotine/tobacco products. A number of recently emerging tobacco products have seen rapid increases in popularity (e.g., e-cigarettes, heated tobacco products; e.g., [41–44]) and provide new methods for cannabis use (e.g., vaping, [70, 71]). Future research should examine the relationship of cannabis use to dependence on a range of tobacco products and consider a range of methods for using tobacco and cannabis. Further, cigarette dependence and cannabis use were self-reported and self-report may be vulnerable to responding biases, memory errors, and underreporting especially related to illegal behaviors (e.g., adolescent use of cannabis).
A number of cannabis-related variables should be examined more closely in future research. For example, “nondaily cannabis use” included individuals with more and less frequent use and future analyses should more closely examine the frequency of cannabis use (e.g., more frequent non-daily use versus less frequent non-daily use, amount of cannabis used per day, frequency of use during the day) in relation to cigarette dependence. Further, co-use of cannabis and cigarettes is more prevalent in states with versus without legalization of cannabis for medical use [27]. As more US states and countries legalize cannabis for medical and/or recreational use, the reasons for cannabis use may multiply and must be carefully measured and taken into account in the context of the relationship between cannabis use and cigarette dependence.
Finally, the waves of data in the NSDUH were cross-sectional and so we could not follow patterns of cigarette dependence and cannabis use longitudinally over time (e.g., to examine changes in cannabis use in relation to changes in cigarette dependence). In addition, past studies of cannabis use and smoking transitions (e.g., smoking initiation, smoking relapse; [16, 18, 72, 73]) did not examine the role of cigarette dependence in these relationships and this would be another important area for future research with longitudinal data.
Conclusions
US individuals with cigarette-cannabis co-use reported a higher prevalence of cigarette dependence relative to those who use cigarettes and do not use cannabis at virtually all levels of cigarette use. Next steps are needed to understand the multiple pathways that may underlie or impact this association including the factors described above such as biological/genetic factors, other individual-level factors (e.g., other substance use, mental health), use of other nicotine-containing products (e.g., e-cigarettes), and aspects of other products (e.g., e-cigarette flavors) due to the rapidly changing tobacco marketplace.
Supplementary Material
WHAT THIS PAPER ADDS.
It is not known whether and to what degree cannabis use may be linked with increased cigarette dependence nationally among adolescents and adults who use cigarettes.
US adolescents and adults who use both cigarettes and cannabis have higher levels of cigarette dependence, relative to those who use cigarettes and do not use cannabis.
The prevalence of cigarette dependence increased from 2002 to 2019 both among those with non-daily cannabis use and those with no cannabis use across nearly all cigarette consumption levels.
The prevalence of cigarette dependence did not change appreciably from 2002 to 2019 among those who use cannabis daily across all cigarette consumption levels.
Acknowledgments
Funding:
This work was supported by the National Institute on Drug Abuse (grant R01-DA20892 to Goodwin) and the National Cancer Institute (grant R21-CA226300 to Dierker). The funders had no role in the design, management, analysis, or interpretation of the data; and preparation, review, or approval of the manuscript.
Footnotes
Conflicts of Interest:
The authors have no conflicts of interest to report.
Authorship:
Dr. Goodwin conceived of the study and data analysis plan and contributed to the interpretation of the data and drafting of the manuscript. Dr. Weinberger contributed to the data analysis plan, interpretation of the data, and wrote the first draft of the manuscript. Dr. Dierker and Ms. Gbedemah conducted the statistical analysis. Dr. Dierker also contributed to the drafting of the manuscript. Mr. Levin contributed to the literature review and manuscript preparation. All authors have contributed to and approved the final draft of the manuscript.
All authors included on the manuscript fulfil the criteria of authorship and there is no one else who fulfils the criteria of authorship that has been excluded as an author.
REFERENCES
- [1].USDHHS. The Health Consequences of Smoking—50 years of progress: A report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health 2014. [Google Scholar]
- [2].GBD 2015 Tobacco Collaborators. Smoking prevalence and attributable disease burden in 195 countries and territories, 1990–2015: a systematic analysis from the Global Burden of Disease Study 2015. Lancet 2017;389(10082):1885–1906. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Creamer MR, Wang TW, Babb S, et al. Tobacco product use and cessation indicators among adults - United States, 2018. MMWR Morb Mortal Wkly Rep 2019;68(45):1013–1019. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [4].Ng M, Freeman MK, Fleming TD, et al. Smoking prevalence and cigarette consumption in 187 countries, 1980–2012. JAMA 2014;311(2):183–192. [DOI] [PubMed] [Google Scholar]
- [5].Cornelius ME, Wang TW, Jamal A, et al. Tobacco product use among adults - United States, 2019. MMWR Morb Mortal Wkly Rep 2020;69(46):1736–1742. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [6].CDC. Cigarette smoking among adults -- United States, 2002. MMWR Morb Mortal Wkly Rep 2004;53(20):427–431. [PubMed] [Google Scholar]
- [7].Gorelick DA, Saxon AJ, Friedman M. Cannabis use and disorder: Epidemiology, comorbidity, health consequences, and medico-legal status. UpToDate 2021; Retrieved August 4, 2021 from https://www-uptodatecom.elibrary.einsteinmed.org/contents/cannabis-use-and-disorder-epidemiology-comorbidity-health-consequences-and-medico-legal-status/. [Google Scholar]
- [8].Compton WM, Han B, Jones CM,et al. Cannabis use disorders among adults in the United States during a time of increasing use of cannabis. Drug Alcohol Depend 2019;204:107468. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [9].Goodwin RD, Pacek LR, Copeland J, et al. Trends in Daily Cannabis Use Among Cigarette Smokers: United States, 2002–2014. Am J Public Health 2018;108(1):137–142. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [10].Weinberger AH, Pacek LR, Wall MM, et al. Trends in cannabis use disorder by cigarette smoking status in the United States, 2002–2016. Drug Alcohol Depend 2018;191:45–51. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [11].Dierker L, Braymiller J, Rose J, et al. Nicotine dependence predicts cannabis use disorder symptoms among adolescents and young adults. Drug Alcohol Depend 2018;187:212–220. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [12].Fix BV, Smith D, O’Connor R, et al. Cannabis use among a nationally representative cross-sectional sample of smokers and non-smokers in the Netherlands: results from the 2015 ITC Netherlands Gold Magic Survey. BMJ Open 2019;9(3):E024497. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [13].Weinberger AH, Funk AP, Goodwin RD. A review of epidemiologic research on smoking behavior among persons with alcohol and illicit substance use disorders. Prev Med 2016;92:148–159. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [14].Okoli CT, Richardson CG, Ratner PA, et al. Adolescents’ self-defined tobacco use status, marijuana use, and tobacco dependence. Addict Behav 2008;33(11):1491–1499. [DOI] [PubMed] [Google Scholar]
- [15].Ramo DE, Delucchi KL, Hall SM, et al. Marijuana and tobacco co-use in young adults: patterns and thoughts about use. J Stud Alcohol Drugs 2013;74(2):301–310. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Weinberger AH, Platt J, Copeland J, et al. Is cannabis use associated with increased risk of cigarette smoking initiation, persistence, and relapse? Longitudinal data from a representative sample of US Adults. J Clin Psychiatry 2018;79(2). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [17].Weinberger AH, Pacek LR, Wall MM, et al. Cigarette smoking quit ratios among adults in the USA with cannabis use and cannabis use disorders, 2002–2016. Tob Control 2020;29(1):74–80. [DOI] [PubMed] [Google Scholar]
- [18].Weinberger AH, Delnevo CD, Wyka K, et al. Cannabis use is associated with increased risk of cigarette smoking initiation, persistence, and relapse among adults in the United States. Nicotine Tob Res 2020;22(8):1404–1408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [19].USDHHS. How Tobacco Smoke Causes Disease: The Biology and Behavioral Basis for Smoking-Attributable Disease: A Report of the Surgeon General. Atlanta,GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health 2010. [PubMed] [Google Scholar]
- [20].Peters EN, Schwartz RP, Wang S, et al. Psychiatric, psychosocial, and physical health correlates of co-occurring cannabis use disorders and nicotine dependence. Drug Alcohol Depend 2014;134:228–234. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [21].Tucker JS, Rodriguez A, Dunbar MS, et al. Cannabis and tobacco use and co-use: Trajectories and correlates from early adolescence to emerging adulthood. Drug Alcohol Depend 2019;204:107499. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [22].APA . Diagnostic and Statistical Manual of Mental Disorders, 5th ed. (DSM-5). Washington DC: American Psychiatric Association 2013. [Google Scholar]
- [23].Breslau N, Johnson EO, Hiripi E, Kessler R. Nicotine dependence in the United States: Prevalence, trends and smoking persistence. Arch Gen Psychiatry 2001;58:810–816. [DOI] [PubMed] [Google Scholar]
- [24].Hyland A, Li Q, Bauer JE, et al. Predictors of cessation in a cohort of current and former smokers followed over 13 years. Nicotine Tob Res 2004;6(Suppl 3):S363–S369. [DOI] [PubMed] [Google Scholar]
- [25].McClure EA, Baker NL, Sonne SC, et al. Tobacco use during cannabis cessation: Use patterns and impact on abstinence in a National Drug Abuse Treatment Clinical Trials Network study. Drug Alcohol Depend 2018;192:59–66. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [26].Timberlake DS, Haberstick BC, Hopfer CJ, et al. Progression from marijuana use to daily smoking and nicotine dependence in a national sample of U.S. adolescents. Drug Alcohol Depend 2007;88(2–3):272–281. [DOI] [PubMed] [Google Scholar]
- [27].Wang JB, Ramo DE, Lisha NE, Cataldo JK. Medical marijuana legalization and cigarette and marijuana co-use in adolescents and adults. Drug Alcohol Depend 2016;166:32–38. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [28].Heatherton TF, Kozlowski LT, Frecker RC, Fagerström KO. The Fagerström Test for Nicotine Dependence: a revision of the Fagerström Tolerance Questionnaire. Br J Addict 1991;86:1119–1127. [DOI] [PubMed] [Google Scholar]
- [29].Fagerström K. Determinants of tobacco use and renaming the FTND to the Fagerström Test for Cigarette Dependence. Nicotine Tob Res 2012;14(1):75–78. [DOI] [PubMed] [Google Scholar]
- [30].Branstetter SA, Muscat JE, Mercincavage M. Time to first cigarette: A potential clinical screening tool for nicotine dependence. J Addict Med 2020. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].Rojewski AM, Tanner NT, Dai L, et al. Tobacco dependence predicts higher lung Cancer and mortality rates and lower rates of smoking cessation in the National Lung Screening Trial. Chest 2018;154(1):110–118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [32].Gu F, Wacholder S, Kovalchik S, et al. Time to smoke first morning cigarette and lung cancer in a case-control study. J Natl Cancer Inst 2014;106(6):dju118. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [33].Guertin KA, Gu F, Wacholder S, et al. Time to first morning cigarette and risk of chronic obstructive pulmonary disease: Smokers in the PLCO Cancer Screening Trial. PLoS One 2015;10(5):e0125973. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [34].Selya AS, Oancea SC, Thapa S. Time to first cigarette, a proxy of nicotine dependence, increases the risk of pulmonary impairment, independently of current and lifetime smoking behavior. Nicotine Tob Res 2016;18(6):1431–1439. [DOI] [PubMed] [Google Scholar]
- [35].Fagerström K. Time to first cigarette; the best single indicator of tobacco dependence? Monaldi archives for chest disease = Archivio Monaldi per le malattie del torace 2003;59(1):91–94. [PubMed] [Google Scholar]
- [36].Baker TB, Piper ME, McCarthy DE, et al. Time to first cigarette in the morning as an index of ability to quit smoking: implications for nicotine dependence. Nicotine Tob Res 2007;9 Suppl 4:S555–570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [37].Center for Behavioral Health Statistics and Quality. 2016. National Survey on Drug Use and Health: Methodological Summary and Definitions. Rockville, MD: Substance Abuse and Mental Health Services Administration 2017. [Google Scholar]
- [38].Substance Abuse and Mental Health Services Administration. Data from: National Survey on Drug Use and Health, January 5, 2021. https://www.datafiles.samhsa.gov/dataset/national-survey-drug-use-and-health-2019-nsduh-2019-ds0001. [PubMed]
- [39].Goodwin RD, Wall MM, Gbedemah M, et al. Trends in cigarette consumption and time to first cigarette on awakening from 2002 to 2015 in the USA: new insights into the ongoing tobacco epidemic. Tob Control 2018;27(4):379–384. [DOI] [PubMed] [Google Scholar]
- [40].Schnoll RA, Goren A, Annunziata K, et al. The prevalence, predictors and associated health outcomes of high nicotine dependence using three measures among US smokers. Addiction 2013;108(11):1989–2000. [DOI] [PubMed] [Google Scholar]
- [41].Czoli CD, White CM, Reid JL, et al. Awareness and interest in IQOS heated tobacco products among youth in Canada, England and the USA. Tob Control 2020;29(1):89–95. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [42].Ho LLK, Li WHC, Cheung AT, et al. Awareness and use of heated tobacco products among youth smokers in Hong Kong: A cross-sectional study. Int J Environ Res Public Health 2020;17(22). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [43].Nyman AL, Weaver SR, Popova L, et al. Awareness and use of heated tobacco products among US adults, 2016–2017. Tob Control 2018;27(Suppl 1):s55–s61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [44].USDHHS. E-Cigarette Use Among Youth and Young Adults: A Report of the Surgeon General. Atlanta, GA: U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health 2016. [Google Scholar]
- [45].Shiffman S, Ferguson SG, Dunbar MS, et al. Tobacco dependence among intermittent smokers. Nicotine Tob Res 2012;14(11):1372–1381. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Dunbar MS, Shadel WG, Tucker JS, et al. Use of and reasons for using multiple other tobacco products in daily and nondaily smokers: Associations with cigarette consumption and nicotine dependence. Drug Alcohol Depend 2016;168:156–163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [47].Agrawal A, Budney AJ, Lynskey MT. The co-occurring use and misuse of cannabis and tobacco: A review. Addiction 2012;107(7):1221–1233. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [48].Rabin RA, George TP. A review of co-morbid tobacco and cannabis use disorders: Possible mechanisms to explain high rates of co-use. Am J Addict 2015;24:105–116. [DOI] [PubMed] [Google Scholar]
- [49].Subramaniam P, McGlade E, Yurgelun-Todd D. Cormobid cannabis and tobacco use in adolescents and adults. Curr Addict Rep 2016;3:182–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [50].Lemyre A, Poliakova N, Bélanger RE. The relationship between tobacco and cannabis use: A review. Subst Use Misuse 2019;54(1):130–145. [DOI] [PubMed] [Google Scholar]
- [51].Perkins KA, Coddington SB, Karelitz JL, Jetton C, Scott JA, Wilson AS, Lerman C. Variability in initial nicotine sensitivity due to sex, history of other drug use, and parental smoking. Drug Alcohol Depend 2009;99(1–3):47–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [52].Schauer GL, Rosenberry ZR, Peters EN. Marijuana and tobacco co-administration in blunts, spliffs, and mulled cigarettes: A systematic literature review. Addict Behav 2017;64:200–211. [DOI] [PubMed] [Google Scholar]
- [53].Bélanger RE, Akre C, Kuntsche E, et al. Adding tobacco to cannabis--its frequency and likely implications. Nicotine Tob Res 2011;13(8):746–750. [DOI] [PubMed] [Google Scholar]
- [54].Campbell BK, Le T, Kapiteni K, et al. Correlates of lifetime blunt/spliff use among cigarette smokers in substance use disorders treatment. J Subst Abuse Treat 2020;116:108064. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [55].Cooper ZD, Haney M. Comparison of subjective, pharmacokinetic, and physiological effects of marijuana smoked as joints and blunts. Drug Alcohol Depend 2009;103(3):107–113. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [56].Peters EN, Schauer GL, Rosenberry ZR, et al. Does marijuana “blunt” smoking contribute to nicotine exposure?: Preliminary product testing of nicotine content in wrappers of cigars commonly used for blunt smoking. Drug Alcohol Depend 2016;168:119–122. [DOI] [PubMed] [Google Scholar]
- [57].Akbar SA, Tomko RL, Salazar CA, et al. Tobacco and cannabis co-use and interrelatedness among adults. Addict Behav 2019;90:354–361. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [58].GDS Core Research Team. Global Drug Survey 2017: Global overview and highlights. Retrieved from https://www.globaldrugsurvey.com on July 19, 2021. 2017. [Google Scholar]
- [59].Hindocha C, Freeman TP, Ferris JA, et al. No smoke without tobacco: A global overview of cannabis and tobacco routes of administration and their association with intention to quit. Front Psychiatry 2016;7:104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [60].Adams TR, Arnsten JH, Ning Y, et al. Feasibility and preliminary effectiveness of varenicline for treating co-occurring cannabis and tobacco use. J Psychoactive Drugs 2018;50(1):12–18. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [61].Becker J, Haug S, Kraemer T, et al. Feasibility of a group cessation program for co-smokers of cannabis and tobacco. Drug Alcohol Rev 2015;34(4):418–426. [DOI] [PubMed] [Google Scholar]
- [62].Beckham JC, Adkisson KA, Hertzberg J, et al. Mobile contingency management as an adjunctive treatment for co-morbid cannabis use disorder and cigarette smoking. Addict Behav 2018;79:86–92. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [63].Hill KP, Toto LH, Lukas SE, et al. Cognitive behavioral therapy and the nicotine transdermal patch for dual nicotine and cannabis dependence: a pilot study. Am J Addict 2013;22(3):233–238. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [64].Lee DC, Budney AJ, Brunette MF, et al. Outcomes from a computer-assisted intervention simultaneously targeting cannabis and tobacco use. Drug Alcohol Depend 2015;155:134–140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [65].Herrmann ES, Cooper ZD, Bedi G, et al. Varenicline and nabilone in tobacco and cannabis co-users: effects on tobacco abstinence, withdrawal and a laboratory model of cannabis relapse. Addict Biol 2019;24(4):765–776. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [66].Peacock A, Leung J, Larney S, et al. Global statistics on alcohol, tobacco and illicit drug use: 2017 status report. Addiction 2018;113(10):1905–1926. [DOI] [PubMed] [Google Scholar]
- [67].Wadsworth E, Hammond D. International differences in patterns of cannabis use among youth: Prevalence, perceptions of harm, and driving under the influence in Canada, England & United States. Addict Behav 2019;90:171–175. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [68].European Monitoring Centre for Drugs and Drug Addiction. Medical use of cannabis and cannabinoids: questions and answers for policymaking. Luxembourg: Publications Office of the European Union 2018. [Google Scholar]
- [69].Pacula RL, Smart R. Medical Marijuana and Marijuana Legalization. Annu Rev Clin Psychol 2017;13:397–419. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [70].Chadi N, Minato C, Stanwick R. Cannabis vaping: Understanding the health risks of a rapidly emerging trend. Paediatr Child Health 2020;25(Suppl 1):S16–s20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [71].Fataar F, Hammond D. The prevalence of vaping and smoking as modes of delivery for nicotine and cannabis among youth in Canada, England and the United States. Int J Environ Res Public Health 2019;16(21). [DOI] [PMC free article] [PubMed] [Google Scholar]
- [72].Ford DE, Vu HT, Anthony JC. Marijuana use and cessation of tobacco smoking in adults from a community sample. Drug Alcohol Depend 2002;67:243–248. [DOI] [PubMed] [Google Scholar]
- [73].Abrantes AM, Lee CS, MacPherson L, et al. Health risk behaviors in relation to making a smoking quit attempt among adolescents. J Behav Med 2009;32(2):142–149. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.