Abstract
Background
E-learning has found its way into dental teaching in general and endodontic teaching in particular. The present study aimed to implement a newly developed multimedia learning application and assess its effect on students’ first root canal treatment on real patients. With the COVID-19 outbreak, the application’s performance was investigated during the pandemic.
Methods
A total of 138 students in the initial clinical endodontic course participated in this study. The control group (n = 49) followed the traditional curriculum, including practice on artificial teeth and face-to-face teaching events. In addition to the traditional curriculum, test group 1 (n = 54) had access to an endodontic e-learning application containing videos demonstrating artificial teeth and patient cases. With the COVID-19 outbreak, test group 2 (n = 35) had no face-to-face teaching; however, endodontic patient treatments were included. The quality of students’ first root canal treatment on real patients was compared using performance and radiographic assessment items. Statistical analysis was done using Kruskal–Wallis and chi-squared tests. Test groups received a questionnaire to assess the learning application. Test group 2 also completed a COVID-19-specific survey to measure students’ perceptions of how the pandemic affected their endodontic education.
Results
The results of endodontic treatments were significantly better for test group 1 (P < 0.001) and 2 (P < 0.001) than for the control group. Likewise, there were significantly fewer treatment errors in test group 1 (P < 0.001) and 2 (P < 0.001). No significant differences were found between test groups 1 and 2. Students of the test groups positively evaluated the e-learning application. Students of test group 2 expressed their fear of negative impacts on their course performance.
Conclusion
The e-learning application was well-received and seemed to improve endodontic education. The results imply that the quality of education may be maintained by implementing e-learning to compensate for face-to-face teaching. As no difference was found between online and face-to-face teaching, students’ and lecturers’ concerns that endodontic education is suffering because of the pandemic may be eased.
Supplementary Information
The online version contains supplementary material available at 10.1186/s12909-022-03463-y.
Keywords: Artificial teeth, Blended learning, COVID-19, E-learning, Endodontic teaching
Background
Performing root canal treatments requires appropriate expertise and, therefore, a certain amount of practice. Although students can perform root canal treatments in most cases with acceptable quality and adequacy [1], the error rate increases with more complex root canal systems [2]. University education can only provide theoretical and practical skills to a limited extent, but the question arises as to how education can be improved; therefore, standards of university education in endodontics have been established [3–5]. However, teachers are aware that practice is the most important factor in developing endodontic skills. One major innovation of endodontic teaching has been introducing endodontic tooth models created using cone-beam computed tomography and manufactured using 3D printing [6–9]. Based on treatment errors observed in the last five years, our department developed the DRSK RCT® endodontic tooth model, optimized due to extensive evaluations by students and instructors and proofed to contribute to endodontic teaching [10]. Attempts have been made to incorporate media into teaching effectively to enhance dental education. In blended learning, content is prepared using media, resulting in a mixed digital and analog teaching form. For example, the format of face-to-face instruction has been successfully replaced by the use of video instruction [11]. Although other studies have demonstrated that the sole use of videos instead of lectures has its limitations, the method is preferred by students and thus should play a permanent role in dental teaching [12, 13].
Flipped classroom designs are part of blended learning and provide learners with content prior to attending the lectures or seminars. These designs are another innovation in teaching that seems to be advantageous over traditional teaching methods [14, 15]. A considerable advantage is the great acceptance of this method among students [16]. Recent studies have indicated that students’ achievements can be effectively enhanced through the flipped classroom approach [14, 17].
In December 2019, the coronavirus disease (COVID-19) appeared in China and was declared a pandemic by the World Health Organization (WHO) shortly thereafter [18]. The COVID-19 pandemic brought dental education to a standstill, forcing educators to find new approaches to continue student education [19]. Due to infection control measures such as social distancing and the prescription of lockdowns, universities worldwide responded with distance learning, implementing online courses and lectures [20–22]. Medical teaching has faced the challenge of maintaining teaching events, and virtual tutor groups have constituted a promising approach to substitute for face-to-face teaching until it can happen again safely [23]. Incorporating virtual learning applications can supplant traditional teaching methods in times of the pandemic [24–26].
Dentists have an extremely high risk of infection due to aerosol-producing procedures. Moreover, most dental education consists of lectures, simulated learning, and teaching practical skills that require a significant amount of practice. Hence, dental education has significantly suffered from COVID-19 restrictions [27]. Most dental schools initially suspended practical courses, shifted to online courses, and introduced alternative performance assessments [20, 22, 28–30]. Other adaptations have included designing virtual curricula, simulation labs, distance learning, and postponing training [19]. Moreover, portable mannequins for preclinical teaching have been advocated [31].
Given the persistence of the pandemic, it is necessary to implement a long-term strategy to sustain dental education, including endodontic education [32], while improving education for the post-pandemic world [33].
Our study aimed to measure the effect of a new endodontic e-learning application associated with using an endodontic tooth model [10] to measure its effectiveness in overcoming disruptions in endodontic teaching due to the current COVID-19 pandemic. The first null hypothesis was that the newly developed e-learning application would not enhance students’ endodontic performance in their first clinical course. Secondly, it was hypothesized that during the COVID-19 pandemic, the new teaching method would not maintain the quality of endodontic teaching when face-to-face teaching was replaced entirely by distance teaching.
Methods
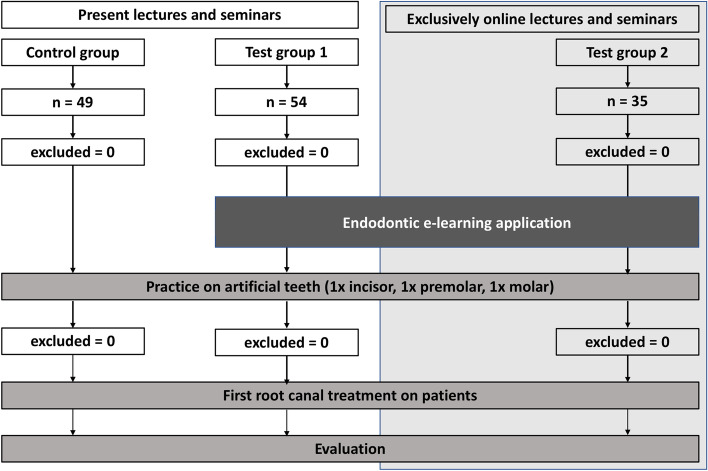
The present study was conducted at the Department for Operative Dentistry, Periodontology, and Preventive Dentistry of RWTH Aachen University in Germany. After independently reviewing, the local ethics committee waived the need for ethical approval as the survey data was collected during the context of teaching. The study was initially intended to occur over four semesters. A total of 138 students were screened for participation: a control group with 49 students, test group 1 with 54 students, and test group 2 (during the pandemic) with 35 students. The number of students in each group was determined by the number of students assigned to the respective groups each semester. The authors aimed to recruit as many subjects as possible for this pilot study. The endodontic patient treatment is an examination performance of the initial clinical course. All data were collected anonymously and not included in the course evaluation. All students were examined by separate demonstrators who had no connection to the present study and no knowledge of the collected data. Participating students were assigned semester-wise into their groups for ethical reasons (Fig. 1).
Fig. 1.
Flow diagram displaying the study design for an immediate understanding. The number of participating students and exclusions are portrayed, and the difference in received treatments is shown
Informed written consent was obtained from every participant. All participants successfully passed the preclinical endodontic course, so they already had a theoretical and practical knowledge of performing root canal treatments on extracted teeth and recently developed artificial teeth [10]. Students in the control group entered the first endodontic course without interventions other than the traditional curriculum, which contained theoretical lectures in endodontics, theoretical courses explaining the procedure of root canal treatments, exercises on extracted teeth, and an objective structured clinical examination. Before entering the clinical endodontic course, students performed practical exercises on three artificial teeth (i.e., incisor, premolar, molar). Endodontic teaching at this department was performed according to the current status [3, 4, 34]. The root canal treatment protocol contained the trepanation following primary and secondary access cavities. The negotiation of the root canal system was performed by using C-Pilot-files® (VDW®, Munich, Germany) and K-files (VDW®, Munich, Germany). After length measurement was carried out endometrically and radiographically, the root canals were enlarged with K-files up to ISO-size 25 and continued with rotary mechanical files (F 360®, Komet®, Lemgo, Germany) depending on the root canals’ initial sizes. Irrigation was performed with 3% sodium hypochlorite and 17% ethylenediaminetetraacetic acid. Eventually, the root canal system was obturated with gutta-percha points with a taper of 0.2 (Antaeos®, VDW®, Munich, Germany) using cold lateral compaction.
Test group 1 had access to educational videos incorporated in a multimedia e-learning application (AVMZ, RWTH Aachen University®) with the traditional curriculum, comprised of 48 h of practical hands-on training on extracted teeth, 7 h of theoretical seminars, and 16 h of lectures. Students could voluntarily practice further hands-on training on their own. Thus, together with the established use of artificial teeth, students could learn at their own pace and practice as often as necessary [35].
Like test group 1, the COVID-19 test group 2 experienced the traditional curriculum (exercises on extracted teeth, theoretical lectures, hands-on training on artificial teeth) and used the e-learning application. However, the lectures and seminars appeared online. Only patient treatments remained in person, performed under strict hygiene regulations.
The multimedia learning application
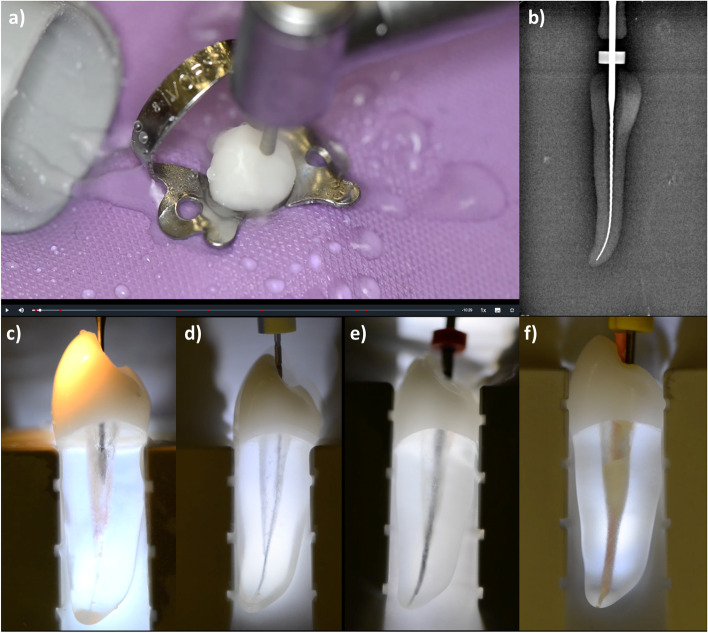
The multimedia application was launched by the Audiovisual Media Centre of the Department of Medicine, RWTH Aachen University® (AVMZ), available only to the participating students of the test groups. A total of 6 educational videos were produced, showing root canal treatments according to the clinical standards of our department. An instructional video was produced for every type of tooth represented by the DRSK® RCT models (i.e., incisor, premolar, molar). Root canal treatments were demonstrated according to the American Association of Endodontists® guidelines and the current literature [3, 5, 36–38]. Through the tooth models’ translucent roots, the performed procedures were visible to the students, helping them understand the impact of each step in the process (Fig. 2).
Fig. 2.
Screenshots from the endodontic e-learning application showing several steps of the routine root canal treatment on a premolar endodontic tooth model (RCT, DRSK® AB Group, Sweden): a) preparation of the access cavity under rubber dam isolation; b) radiographic length measurement using an ISO 15 K-file; c) enlarging the coronal third of the root canal system; d) sounding of the root canal system using an ISO 06 C-Pilot file®; e) flaring of the root canal walls with a mechanical file system (Reciproc®, VDW, Germany); f) obturation using the cold lateral compaction technique
Additionally, three videos containing a representative patient case were made available with the same procedures on real patients. The videos were filmed using a dental camera with autofocus (Elio® HD60, EKLER®, Fr) and an action camera (Hero7® Black, GoPro® Inc., US). Ambient sound was recorded with an MP3/Wave Handy Recorder (H1n, Zoom® North America, US). The videos were shortened to a maximum length of 10 min. Playability was optimized using jump tags to select specific sections of the videos. Explanatory commentary for each video was separately recorded by a tutor in the recording studio and later added to the videos. Eventually, the videos were incorporated into an online multimedia learning application accessible to students in test groups 1 and 2 via the internet and password authorization. An internet platform (https://emedia-medizin.rwth-aachen.de) widely used in medical teaching at RWTH Aachen University® was utilized. The platform is run by the AVMZ and contains various multimedia applications for several medical and dental departments. All participating students of both test groups confirmed their use of the endodontic e-learning application. The evaluation of the e-learning application assured that students had attended the online course and watched the videos.
Endodontic teaching during the COVID-19 pandemic
At the beginning of the pandemic, our faculty, similar to almost all dental schools globally, discontinued in-person teaching and switched to online courses [28]. Instead of continuing dental teaching solely virtually and using mannequins [27, 39], a hygiene protocol was developed that made it possible to restart clinical teaching. Thus, any student could perform an endodontic treatment on a real patient.
Hygiene, distancing regulations, and drastically increased infection protection measures affected clinical teaching during the pandemic [27, 32]. Lectures and seminars were held entirely online using video communication software (Zoom®, Zoom Video Communication ®, US) to prevent unnecessary contact between individuals.
Evaluation of students’ first root canal treatment on real patients
As the present study aimed to analyze the performance of the students’ first root canal treatment on patients, the endodontic performance during the seventh semester endodontic course was evaluated by independent demonstrators of our department. For all groups, the same demonstrators were involved. All were general practitioners with a minimum of two years of experience in endodontics. The evaluation of the treatment performance for this study was performed independently from the course assessment. The demonstrators associated with this study were not part of the first clinical course so that the result of the evaluation for this study would not conflict with the students passing the course. The evaluation sheet used in this study was designed similar to a study that examined students’ endodontic performances through items [40], resembling the evaluation sheets used in our department ‘s preclinical endodontic courses. The evaluation sheet in this study contained 21 items ranging from assessing performing straight-line access to evaluating a completed root canal filling. Notably, a maximum of 20 error points could be registered. All steps performed on the patient and the radiographs taken were evaluated because the independent demonstrators were present during treatments.
Criteria for the teeth considered for the study were freedom from pain and difficulty level suitable for the first clinical course. Molars with a moderate root canal curvature were included due to organizational reasons. For example, teeth with pronounced curvature and complex molars were excluded before the patient pool was allocated to the first clinical endodontic course since these teeth were unsuitable for students in the seventh semester performing their first root canal treatment on real patients [41]. A dentist assessed all teeth at the department before being assigned to the endodontic course.
Evaluation of the multimedia learning application
The students in test groups 1 and 2 evaluated the learning application anonymously online using a 5-point Likert scale (1 = fully disagree, 5 = fully agree), as routinely used in medical questionnaires [42–44]. An incorporated system usability scale (SUS) was used to assess the learning application. The tooth models were rated using the same questionnaire based on a 7-point Likert scale similar to a previous study.
Finally, the COVID-19 test group answered an additional 5-point Likert scale questionnaire with 10 questions regarding their perceptions and concerns about the COVID-19 pandemic. There was no evaluation of the traditional curriculum in any of the three groups.
Statistical analysis
All collected data were recorded in Excel® using version 16.43. Statistical analysis was performed using SPSS® (IBM® 27.0). Statistical graphics were created with either Excel® or SPSS®. The performances of the three cohorts – control group, test group 1, and test group 2 (COVID-19) – including their success and error rates were statistically analyzed using a Kruskal–Wallis test after a Shapiro–Wilk test indicated a non-normal distribution. Bonferroni correction was used as a post-hoc test. The individual items and errors between groups (dichotomous data) were statistically compared using a chi-squared and Fisher’s exact test as appropriate. For all statistical analyses, P ≤ 0.05 was considered significant.
The results of the Likert-scale questionnaires of test groups 1 and 2 were analyzed descriptively. A score was estimated for each participant, and an overall mean with the standard deviation was calculated. The reliability of the Likert scale was confirmed using Cronbach’s alpha.
Results
Treatment performance
Altogether, 138 students participated in this study. There were no dropouts regarding the evaluation of root canal treatments registered. In total, 138 teeth with 217 root canals were treated (Table 1).
Table 1.
Number of teeth and root canals treated by students during their first real patient treatments in the first clinical endodontic course (n = 138)
| Incisors | Premolars | Molars | |
|---|---|---|---|
| Number of teeth (root canals) percentage | Number of teeth (root canals) percentage | Number of teeth (root canals) percentage | |
| Control group (n = 49) | 16 (16) 32% | 23 (33) 47% | 10 (34) 20% |
| Test group 1 (n = 54) | 19 (19) 35% | 25 (30) 46% | 10 (32) 18% |
| Test group 2 (n = 35) | 11 (11) 31% | 17 (22) 49% | 7 (20) 20% |
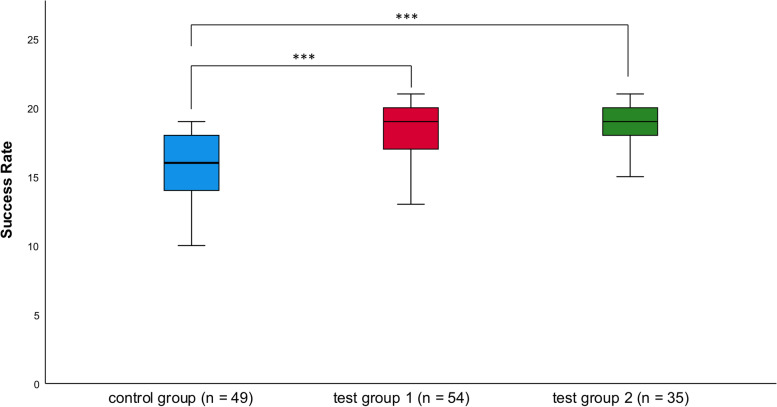
After implementing the endodontic multimedia application combined with additional exercises on endodontic tooth models before the first clinical endodontic course, the score of the treatment performance of the control group was 15.0 ± 3.7 (mean ± SD). The scores of test groups 1 and 2 were significantly higher (18.2 ± 2.2 and 19.0 ± 1.7, respectively; P < 0.001). There was no significant difference in treatment success in real patients between test group 1 (who experienced face-to-face teaching with access to the e-learning application) and test group 2 (who experienced exclusively digital teaching; Fig. 3).
Fig. 3.
Graphic of the results of the students’ first root canal treatments on real patients during their first clinical endodontic course. The scale of the y-axis ranges from 0 to 21. Medians and quartiles represent the results of the three groups. Asterisks mark the level of significance (* for P < 0.05; *** for P < 0.001)
The items that were used to assess students’ root canal treatments were divided into 4 stages.
Stage 1 contained items regarding the isolation of the tooth and the opening of the cavity. Test group 1 was significantly better at establishing the tension-free positioning of endodontic files by sufficiently removing orifices and parts of the pulp chamber roof than the control group (Item 3; P < 0.05). They also performed significantly better at the accurate preparation of the orifices in relation the root canal anatomy (P < 0.01). Stage 2 consisted of items regarding the determination and the control of the working length. Test group 1 was significantly better at the selection of sufficient working lengths according to the preoperative radiographs (Item 6; P < 0.01) and the adequate determination of the working lengths (Item 9; P < 0.05). Moreover, they more frequently documented the adequate working lengths and the reference points correctly (Item 10; P < 0.001). In stage 3, items for the assessment of canal preparation and irrigation were combined. Students in test group 1 were more successful in establishing tug-back with the master cone (Item 12; P < 0.01) and significantly better at performing radiographic controls of the fitting of their selected master cone (Item 13; P < 0.05). Items regarding the obturation and restoration were allocated to stage 4. When performing obturation, they shortened the root filling to a crestal level more thoroughly (Item 15; P < 0.01). Moreover, they cleaned the pulp chamber walls more efficiently from the rest of the sealer and gutta-percha (Item 16; P < 0.001). According to the post-operative radiographs of the test groups’ root canal fillings, they managed to perform better in terms of density (Item 19; P < 0.05), continuity (Item 20; P < 0.001), and extension concerning the original shape of the root canals (Item 21; P < 0.01).
The performance of test group 2, establishing the correct working lengths according to the preoperative radiographs, was significantly lower than test group 1 (Item 6; P < 0.01). However, significantly more students in test group 2 managed to achieve the adequate lengths of their root filings than in test group 1 (0.5–1.0 mm from the radiographic apex; Item 17; P < 0.05).
Treatment errors
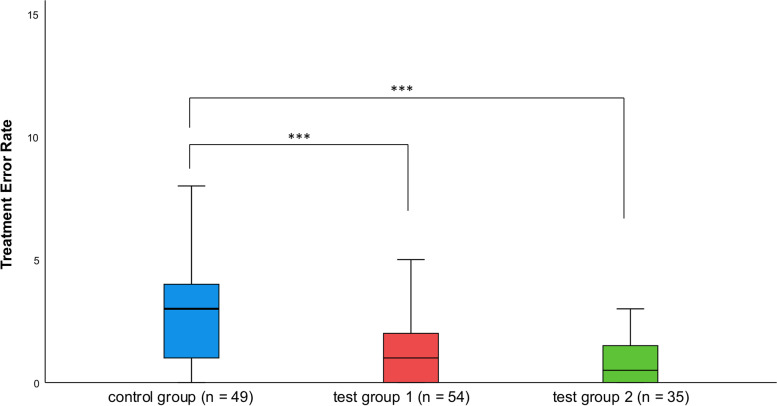
The number of treatment errors significantly decreased from 3.2 ± 2.9 in the control group to 1.2 ± 1.3 in test group 1 (P < 0.001). The number of treatment errors did not significantly differ between test group 1 and test group 2 (0.8 ± 0.9); however, it significantly differed between test group 2 and the control group (P < 0.001; Fig. 4).
Fig. 4.
Graphic of the treatment errors registered during students’ first root canal treatments on real patients during their first clinical endodontic course. The scale of the y-axis ranges from 0 to 20. Medians and quartiles represent the results of the three groups. Asterisks mark the level of significance (* for P < 0.05; *** for P < 0.001)
The treatment errors were allocated to the already mentioned stages to enable a clear presentation. There were no significant differences between the control group and test group 1 regarding errors of isolation and opening of the cavity (stage 1). Moreover, no significant differences in determining the working length (stage 2) were observed. For root canal instrumentation and irrigation (stage 3), differences between the groups were significant on several points. During root canal preparation, periapical tissue damage was significantly lower in test group 1 than in the control group (Item 6; P < 0.05). They were less likely to show incorrect root canal preparation (Item 8; P < 0.01), resulting in elbow zips, blockings of root canals, and lateral perforation of canal walls. Errors regarding the irrigation process were observed in the control group but not observed in the test group (Item 9; P < 0.05). Errors regarding obturation and restoration were summarized as stage 4. Significantly fewer radiographs with master cones perforating the apex were recorded in test group 1 (Item 10; P < 0.001). When assessing the root canal filling, in particular, fewer inhomogeneous (Item 12; P < 0.05) and discontinuous (Item 13; P < 0.05) root fillings occurred. Post-operative radiographs showed significantly more insufficiently cleaned cavities (Item 16; P < 0.01). Additional errors such as the wrong application of permanent post-endodontic filling or the wrong usage of sealer components were less frequently observed in test group 1 than in the control group (Item 20; P < 0.01). There were no significant differences between test groups 1 and 2 regarding the error rate, but there were some non-significant differences as the error rate was higher for a few items.
Evaluation of the endodontic multimedia application
A total of 89 students were eligible to participate in evaluating the endodontic multimedia application using the SUS and a 5-point Likert scale containing 14 questions. Five students did not complete the questionnaire, leading to a response rate of 94%. The reliability of the Likert scale was assessed using Cronbach’s alpha, which was 0.829 and thus indicated high internal consistency [45]. The endodontic multimedia learning application received fairly good ratings from students in both test groups (4.3 ± 0.6; Likert scale: 1–5, Table 2).
Table 2.
Assessment of the learning application regarding students’ satisfaction using a 5-point Likert scale questionnaire (test groups 1 and 2; n = 84 students)
| Item | 5 | 4 | 3 | 2 | 1 |
|---|---|---|---|---|---|
| I would recommend the learning application to someone | 51.2% (43) | 36.9% (31) | 10.7% (9) | 0% (0) | 0% (0) |
| I find the tooth illustrations appealing | 38.1% (32) | 45.2% (38) | 13.1% (11) | 0% (0) | 0% (0) |
| I find the animation of the tooth illustrations appealing | 39.1% (33) | 47.6% (40) | 10.7% (9) | 0% (0) | 0% (0) |
| I find the structure of the learning application useful | 46.4% (39) | 41.7% (35) | 8.3% (7) | 2.4% (2) | 0% (0) |
| I find the presentation of the different tooth types superfluous | 1.2% (1) | 3.6% (3) | 10.7% (9) | 33.3% (28) | 47.6% (40) |
| I find videos on artificial teeth helpful for my learning process | 56.0% (47) | 28.6% (24) | 11.9% (10) | 2.4% (2) | 0% (0) |
| I find videos on endodontic patient treatments helpful for my learning process | 71.4% (60) | 21.4% (18) | 4.8% (4) | 0% (0) | 0% (0) |
| The videos convey all the necessary aspects of endodontic treatment | 28.6% (24) | 57.1% (48) | 11.9% (10) | 1.2% (1) | 0% (0) |
| Through the videos, I can understand the endodontic treatment | 38.1% (32) | 52.4% (44) | 8.3% (7) | 0% (0) | 0% (0) |
| I find the jump marks of the videos superfluous | 1.2% (1) | 1.2% (1) | 16.7% (14) | 35.7% (30) | 44.0% (37) |
| I find the length of the videos appropriate | 41.7% (35) | 42.9% (36) | 14.3% (12) | 0% (0) | 0% (0) |
| I had difficulties operating the player | 6.0% (5) | 4.8% (4) | 4.8% (4) | 16.7% (14) | 66.7% (56) |
| I find the speed function of the player helpful | 25.0% (21) | 23.8% (20) | 38.1% (32) | 10.7% (9) | 1.2% (1) |
5 = applies strongly, 4 = applies predominantly, 3 = undecided, 2 = does not apply predominantly, 1 = does not apply
Both test groups assigned the application an excellent rating on the SUS (SUS score: 81.4, Table 3).
Table 3.
Assessment of the endodontic e-learning application on the SUS (test groups 1 and 2; n = 84 students)
| Item | 5 | 4 | 3 | 2 | 1 |
|---|---|---|---|---|---|
| I can imagine using the learning application regularly | 38.1% (32) | 44.0% (37) | 8.3% (7) | 7.1% (6) | 1.2% (1) |
| The learning application is unnecessarily complex | 0% (0) | 1.2% (1) | 10.7% (9) | 40.5% (34) | 46.4% (39) |
| The learning application is easy to use | 44.0% (37) | 38.1% (32) | 11.9% (10) | 4.8% (4) | 0% (0) |
| I would need technical support to use the learning application | 0% (0) | 3.6% (3) | 15.5% (13) | 25.0% (21) | 54.8% (46) |
| The different functions of the learning application are well-integrated | 32.1% (27) | 47.6% (40) | 19.0% (16) | 0% (0) | 0% (0) |
| The learning application contains many inconsistencies | 0% (0) | 2.4% (2) | 15.5% (13) | 52.4% (44) | 28.6% (24) |
| The learning application is quick to master | 56.0% (47) | 25.0% (21) | 15.5% (13) | 2.4% (2) | 0% (0) |
| The operation is very cumbersome | 0% (0) | 1.2% (1) | 8.3% (7) | 28.6% (24) | 60.7% (51) |
| I felt very confident using the learning application | 41.7% (35) | 38.1% (32) | 16.7% (14) | 2.4% (2) | 0% (0) |
| I had to learn many things before I could work with the learning application | 0% (0) | 3.6% (3) | 15.5 (13) | 29.8% (25) | 50.0%(42) |
5 = applies strongly, 4 = applies predominantly, 3 = undecided, 2 = does not apply predominantly, 1 = does not apply
Evaluation of the COVID-19-specific survey
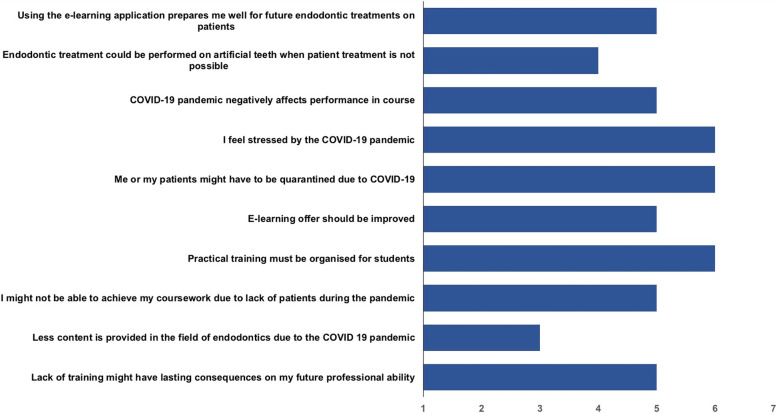
A questionnaire based on a 7-point Likert-type scale with 10 COVID-19-specific questions was distributed among the students in test group 2. The survey was completed by 35 participants, corresponding to a response rate of 100%.
For all questions, the scale ranged from 1 (fully disagree) to 7 (fully agree), with 4 as a neutral rating option. A median score for each question was calculated since the Likert-type scale data were treated as ordinal data (Fig. 5).
Fig. 5.
The bar chart presents the results of the Covid-19 survey containing 10 7-point Likert scale questions (1 = fully disagree to 7 = fully agree with 4 as a neutral response option). The X-axis shows the rating from 1 to 7, whereas the bars mark the median for each question
Discussion
E-learning has gained more importance recently in medical and dental education [46–50]. The availability of digital infrastructure and appropriate training for students and tutors are challenges associated with e-learning [51, 52]; nevertheless, digital learning has become an indispensable part of modern teaching. In 2014, Brumini et al. demonstrated dental students’ positive attitude toward e-learning [53]. As a significant benefit, e-learning applications enable students to learn at their own pace, repeatedly accessing course content and practice material as needed [35]. Various studies have indicated that e-learning enhances dental education [14, 54, 55]. As a mixture of e-learning and conventional learning, the blended learning approach has been successfully integrated into medical and dental teaching and has proven to increase students’ performance. Although some students are critical of the increased time spent at home using multimedia applications instead of face-to-face lectures [56], e-learning offers the advantage of viewing the study content repeatedly [57].
Students have preferentially adopted blended learning approaches [16, 58, 59], which is unsurprising since present generations of students are quite familiar with media and use it regularly for learning purposes [16]. Similar findings have been described in other studies, where explanatory videos have received broad approval from learners [12, 60, 61]. Excellent ratings for user-friendliness and design and technical implementation affirm the quality of the application. Good acceptance among students is crucial to adopt a learning application successfully [17].
Our results support the positive effects of e-learning. The first null hypothesis is rejected due to a significant improvement in the performance of test groups 1 and 2 compared to the control group. The e-learning application was intended to prepare students for the subject of endodontics before the first clinical endodontic course, stimulating self-learning in students as expected in flipped classroom approaches [14, 35]. For example, in 2020, Singal et al. stated that the ability to learn on one’s own is of great importance [29], which is especially true during the current COVID-19 pandemic period, with the wide use of distance learning [62].
Successfully performing root canal treatments is a highly technical procedure that requires strict adherence to procedural processes [63]. Previous research has suggested that students are better prepared to perform procedural processes through blended learning than through classical teaching methods alone [64]. Our findings show improved performances for students who used the e-learning application. Previous studies have shown that blended learning approaches positively affect students’ performances [17, 65]. When evaluating the e-learning application, students in our study conveyed its positive effect on their learning process.
Digitalization in university teaching, in general, is more topical than ever during the pandemic [21, 30, 66, 67]. The implementation of online learning seems to affect students’ motivation positively [68]. Therefore, during the pandemic, this approach, combined with converting lectures and seminars to online presentations, may have helped compensate for the lack of physical interaction in the theoretical part of our course. Apart from hands-on training on extracted and artificial teeth, only patient treatments continued to be performed in person. There was no significant difference between the test groups. Thus, the 2nd null hypothesis is rejected since conducting lectures and seminars as online events had no negative effect on the result of students’ first root canal treatment on a real patient. Due to high infection rates, physical attendance at lectures was temporarily restricted, so alternatives had to be found to ensure endodontic teaching, similar to other disciplines [20, 21]. Compared with test group 1, test group 2 was significantly less successful in determining the correct working length based on the preoperative radiographs, whereas they significantly more often established accurate root canal lengths. As the students of all groups had guidance by an experienced specialist in endodontics especially during their first treatment, a more frequent use of the video instructions could be a possible explanation for this finding. Determining the correct working lengths highly depends on experience, and the video instructions might not have been able to improve this treatment step as well as others.
Students in our department reported enjoying attending clinical endodontic courses involving patient treatments despite the pandemic and supported our efforts to continue teaching. Continuing endodontic teaching with a real patient during the pandemic was a significant challenge, and a high level of additional infection control measures was necessary to minimize the risk of infection for patients, students, and staff [27, 32]. Psychologically, mental stress and concerns about the pandemic made it challenging for students to focus on their studies [32]. Although the COVID-19 pandemic caused additional student stress, and the loss of face-to-face teaching was harsh [68], our results imply that a well-coordinated e-learning application combined with online teaching and practice on artificial teeth might have contributed to the maintenance of teaching endodontics during the pandemic, enhancing and modernizing traditional endodontic teaching methods.
As the test group 2 achieved the best results for their root canal treatments, our findings may indicate the possibility of replacing teachers with video instructions. However, there are studies that shed light on the disadvantages of online teaching without any in-person events. The delivery of online content can be differentiated as asynchronous (e.g., pre-recorded lectures, video instructions) and synchronous (e.g., live lectures, in-person seminars) [69]. Students seemed to prefer a mixture of both these forms [70]. However, they were not in favor of completely replacing face-to-face teaching with online teaching [71] as they noted a lack of communication within the group and with the lecturers [72–75]. According to a recent study, students claimed online learning to be less effective balancing theory and practice as well as in building of practical skills [76]. Previous studies have found that blended learning approaches are preferentially adopted by students [16, 58, 59]. In a randomized controlled trial, the authors could demonstrate the superiority of blended learning approaches compared to face-to-face and online approaches for the technical sensitive procedure of local anesthesia [77]. This finding is in line with studies reporting on the superiority of flipped classroom approaches [14, 58, 78]. In any event, professional staff as well as offline lessons remain crucial for successful teaching and cannot be completely replaced [76].
According to our findings, the e-learning application enabled students to achieve more effective practical exercises on artificial teeth resulting in a better understanding of the treatment steps. Several studies have investigated using artificial teeth as substitutes for natural teeth in preclinical courses [7, 10, 40, 79, 80], while others have compared different kinds of artificial teeth [81]. In the present study, artificial teeth were utilized as additional training aids in endodontic pre-course settings before entering the first clinical course, combined with an e-learning tool. Significant differences in endodontic performance between inexperienced students and experienced operators have been found [82–85]. These studies have identified the importance of students practicing manual skills before entering clinical courses. For example, a recent study considered the treatment of 6 simulated root canals reasonable to attain an adequate level of competence [86], indicating the urgent need for these training aids. However, the exclusive use of an e-learning tool without any training on artificial teeth may not have yielded these positive results.
The use of artificial teeth provides a safe environment for students, so they can practice without the risk of harming the patient when treatment errors occur. Nevertheless, training on real patients is irreplaceable for gaining endodontic skills [87]. Possible reasons for this benefit include adequate communication with the patient, possible pain development, and restricted access to the treatment site due to the patient’s anatomy. The transition from preclinical knowledge to real clinical cases is highly stressful for students [88–92], which, according to our findings, has been especially true during the COVID-19 pandemic. Therefore, it is crucial to overcome the theory–practice gap that often prevents students from successfully transferring their knowledge to a clinical situation [89, 93]. Eventually, all endodontic teaching methods aim to prepare students as effectively and realistically as possible to perform root canal treatments on actual human beings successfully.
Limitations
Our study design did not involve randomization, and there were no parallel performances of the three groups. All students in a particular semester were assigned to the same group to require no exclusion of additional learning content for one group of students within a semester. Students in the same semester could not be divided into different groups as there would have been unequal conditions for the students to pass their examinations. Furthermore, none of the students wanted to waive the opportunity for additional educational content voluntarily. Therefore, the results of the present study might have been influenced by time-dependent selection bias since a variation might have existed between the student groups and patients who were endodontically treated. Moreover, the study design did not distinguish between the effect of the e-learning application and the use of tooth models. However, both methods are effective in dental teaching [17, 77–79, 94].
Future studies should analyze the effect of the learning application more intensively, illuminating the difference in students’ performances between the use of artificial teeth and the use of artificial teeth with the learning application compared to traditional exercises on extracted teeth. Ideally, blind randomized trials with parallel performances should be used. The limitation of the small number of students per semester in dental schools could be addressed by performing multicenter studies to obtain larger cohort sizes.
Conclusion
The multimedia e-learning application improved students’ performance in the first root canal treatment on real patients. The individualized learning pace of the students and an illustration of the treatment steps enhanced the students’ theoretical and practical knowledge of endodontic treatments. Thus, practical exercise is immensely significant for students to achieve expertise and practice and gain self-confidence in complex endodontic treatments. Indeed, e-learning plays a supportive role in this process. During the COVID-19 pandemic, the e-learning application, combined with online lectures, appeared to maintain the quality of students’ endodontic treatments. However, performing root canal treatments on real patients remains crucial to provide knowledge about managing stressful situations and patients. Therefore, a possible further research approach could be evaluating students’ stress levels during patient treatments and analyzing how the video instructions helped the students with problem-solving.
Supplementary Information
Acknowledgements
We want to thank Duncan Harrop for proofreading as a native speaker Richa from Scribbr for the professional proofreading and editorial service. We also thank Doug from Scribbr for the additional professional proofreading.
Abbreviations
- COVID-19 pandemic
Coronavirus disease pandemic
- DRSK RCT
Name of the tooth model presented in this study
Authors’ contributions
CF and SYM contributed to the study’s conception and design. CF and SYM performed the material preparation and data collection, and CF performed the analysis. CF wrote the initial draft of the manuscript. All authors (CF, ML, SYM) critically reviewed previous manuscript versions, which CF edited. All authors (CF, ML, SYM) read and approved the final manuscript.
Funding
Open Access funding enabled and organized by Projekt DEAL.
Availability of data and materials
All data are available from the corresponding author upon reasonable request.
Declarations
Ethics approval and consent to participate
Ethics approval and consent to participate: The study was performed by the dental faculty of RWTH Aachen University in Germany after gaining approval from the internal ethics committee. The study was conducted in accordance with the ethical standards established in the 1964 Declaration of Helsinki and its subsequent amendments. All participants voluntarily took part in this study, and written informed consent was obtained from each participant. The participating students had the opportunity to withdraw their approval without mentioning any reasons at all times.
Consent for publication
Not applicable.
Competing interests
The authors declare that there were no competing interests.
Footnotes
Publisher’s Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Fong W, Heidarifar O, Killough S, Lappin MJ, El Karim IA. An audit on technical quality of root fillings performed by undergraduate students. Int Endod J. 2018;51(Suppl 3):e197–e203. doi: 10.1111/iej.12803. [DOI] [PubMed] [Google Scholar]
- 2.Haug SR, Solfjeld AF, Ranheim LE, Bardsen A. Impact of Case Difficulty on Endodontic Mishaps in an Undergraduate Student Clinic. Journal of Endodontics. 2018;44(7):1088–1095. doi: 10.1016/j.joen.2018.03.012. [DOI] [PubMed] [Google Scholar]
- 3.European Society of E Undergraduate curriculum guidelines for endodontology. Int Endod J. 2001;34(8):574–580. doi: 10.1046/j.0143-2885.2001.00508.x. [DOI] [PubMed] [Google Scholar]
- 4.European Society of E Quality guidelines for endodontic treatment: consensus report of the European Society of Endodontology. Int Endod Journal. 2006;39(12):921–930. doi: 10.1111/j.1365-2591.2006.01180.x. [DOI] [PubMed] [Google Scholar]
- 5.De Moor R, Hulsmann M, Kirkevang LL, Tanalp J, Whitworth J. Undergraduate curriculum guidelines for endodontology. Int Endod J. 2013;46(12):1105–1114. doi: 10.1111/iej.12186. [DOI] [PubMed] [Google Scholar]
- 6.Reymus M, Fotiadou C, Hickel R, Diegritz C. 3D-printed model for hands-on training in dental traumatology. Int Endod J. 2018;51(11):1313–1319. doi: 10.1111/iej.12947. [DOI] [PubMed] [Google Scholar]
- 7.Reymus M, Fotiadou C, Kessler A, Heck K, Hickel R, Diegritz C. 3D printed replicas for endodontic education. Int Endod J. 2019;52(1):123–130. doi: 10.1111/iej.12964. [DOI] [PubMed] [Google Scholar]
- 8.Reymus M, Stawarczyk B, Winkler A, Ludwig J, Kess S, Krastl G, Krug R. A critical evaluation of the material properties and clinical suitability of in-house printed and commercial tooth replicas for endodontic training. Int Endod J. 2020;53(10):1446–1454. doi: 10.1111/iej.13361. [DOI] [PubMed] [Google Scholar]
- 9.Reymus M, Liebermann A, Diegritz C, Kessler A. Development and evaluation of an interdisciplinary teaching model via 3D printing. Clin Exp Dent Res. 2021;7(1):3–10. doi: 10.1002/cre2.334. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Yekta-Michael SS, Farber CM, Heinzel A. Evaluation of new endodontic tooth models in clinical education from the perspective of students and demonstrators. BMC Med Educ. 2021;21(1):447. doi: 10.1186/s12909-021-02848-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Carbonaro M, King S, Taylor E, Satzinger F, Snart F, Drummond J. Integration of e-learning technologies in an interprofessional health science course. Med Teach. 2008;30(1):25–33. doi: 10.1080/01421590701753450. [DOI] [PubMed] [Google Scholar]
- 12.Smith W, Rafeek R, Marchan S, Paryag A. The use of video-clips as a teaching aide. Eur J Dent Educ. 2012;16(2):91–96. doi: 10.1111/j.1600-0579.2011.00724.x. [DOI] [PubMed] [Google Scholar]
- 13.Ramlogan S, Raman V, Sweet J. A comparison of two forms of teaching instruction: video vs live lecture for education in clinical periodontology. Eur J Dent Educ. 2014;18(1):31–38. doi: 10.1111/eje.12053. [DOI] [PubMed] [Google Scholar]
- 14.Bock A, Heitzer M, Lemos M, Peters F, Elvers D, Kniha K, Holzle F, Modabber A. “Flipped OR”: a modified didactical concept for a surgical clerkship in Oral and Maxillofacial Surgery. Br J Oral Maxillofac Surg. 2020;58(10):1245–1250. doi: 10.1016/j.bjoms.2020.03.008. [DOI] [PubMed] [Google Scholar]
- 15.Liebert CA, Lin DT, Mazer LM, Bereknyei S, Lau JN. Effectiveness of the Surgery Core Clerkship Flipped Classroom: a prospective cohort trial. Am J Surg. 2016;211(2):451–457 e451. doi: 10.1016/j.amjsurg.2015.10.004. [DOI] [PubMed] [Google Scholar]
- 16.Bock A, Modabber A, Kniha K, Lemos M, Rafai N, Holzle F. Blended learning modules for lectures on oral and maxillofacial surgery. Br J Oral Maxillofac Surg. 2018;56(10):956–961. doi: 10.1016/j.bjoms.2018.10.281. [DOI] [PubMed] [Google Scholar]
- 17.Qutieshat AS, Abusamak MO, Maragha TN. Impact of Blended Learning on Dental Students' Performance and Satisfaction in Clinical Education. J Dent Educ. 2020;84(2):135–142. doi: 10.21815/JDE.019.167. [DOI] [PubMed] [Google Scholar]
- 18.Mackenzie JS, Smith DW. COVID-19: a novel zoonotic disease caused by a coronavirus from China: what we know and what we don't. Microbiol Aust. 2020;MA20013. 10.1071/MA20013. [DOI] [PMC free article] [PubMed]
- 19.Haridy R, Abdalla MA, Kaisarly D, Gezawi ME. A cross-sectional multicenter survey on the future of dental education in the era of COVID-19: Alternatives and implications. J Dent Educ. 2020;85(4):483–493. doi: 10.1002/jdd.12498. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Iyer P, Aziz K, Ojcius DM. Impact of COVID-19 on dental education in the United States. J Dent Educ. 2020;84(6):718–722. doi: 10.1002/jdd.12163. [DOI] [PubMed] [Google Scholar]
- 21.Liu X, Zhou J, Chen L, Yang Y, Tan J. Impact of COVID-19 epidemic on live online dental continuing education. Eur J Dent Educ. 2020;24(4):786–789. doi: 10.1111/eje.12569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Desai BK. Clinical implications of the COVID-19 pandemic on dental education. J Dent Educ. 2020;84(5):512. doi: 10.1002/jdd.12162. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Paul N, Kohara S, Khera GK, Gunawardena R. Integration of Technology in Medical Education on Primary Care During the COVID-19 Pandemic: Students' Viewpoint. JMIR Medical Education. 2020;6(2):e22926. doi: 10.2196/22926. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Mishra K, Boland MV, Woreta FA. Incorporating a virtual curriculum into ophthalmology education in the coronavirus disease-2019 era. Curr Opin Ophthalmol. 2020;31(5):380–385. doi: 10.1097/ICU.0000000000000681. [DOI] [PubMed] [Google Scholar]
- 25.Wilcha RJ. Effectiveness of Virtual Medical Teaching During the COVID-19 Crisis: Systematic Review. JMIR Medical Education. 2020;6(2):e20963. doi: 10.2196/20963. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.El-Ghandour NMF, Ezzat AAM, Zaazoue MA, Gonzalez-Lopez P, Jhawar BS, Soliman MAR. Virtual learning during the COVID-19 pandemic: a turning point in neurosurgical education. Neurosurg Focus. 2020;49(6):E18. doi: 10.3171/2020.9.FOCUS20634. [DOI] [PubMed] [Google Scholar]
- 27.Sukumar S, Dracopoulos SA, Martin FE. Dental education in the time of SARS-CoV-2. Eur J Dent Educ. 2020;25(2):325–331. doi: 10.1111/eje.12608. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Quinn B, Field J, Gorter R, Akota I, Manzanares MC, Paganelli C, Davies J, Dixon J, Gabor G, Amaral Mendes R, et al. COVID-19: The immediate response of european academic dental institutions and future implications for dental education. Eur J Dent Educ. 2020;24(4):811–814. doi: 10.1111/eje.12542. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Singal A, Bansal A, Chaudhary P, Singh H, Patra A. Anatomy education of medical and dental students during COVID-19 pandemic: a reality check. Surg Radiol Anat. 2021;43(4):515–521. doi: 10.1007/s00276-020-02615-3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Chang TY, Hong G, Paganelli C, Phantumvanit P, Chang WJ, Shieh YS, Hsu ML. Innovation of dental education during COVID-19 pandemic. Journal of Dental Sciences. 2021;16(1):15–20. doi: 10.1016/j.jds.2020.07.011. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Galibourg A, Maret D, Monsarrat P, Nasr K. Impact of COVID-19 on dental education: How could pre-clinical training be done at home? J Dent Educ. 2020;84(9):949. doi: 10.1002/jdd.12360. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Loch C, Kuan IBJ, Elsalem L, Schwass D, Brunton PA, Jum'ah A. COVID-19 and dental clinical practice: Students and clinical staff perceptions of health risks and educational impact. J Dent Educ. 2021;85(1):44–52. doi: 10.1002/jdd.12402. [DOI] [PubMed] [Google Scholar]
- 33.Clemente MP, Moreira A, Pinto JC, Amarante JM, Mendes J. The Challenge of Dental Education After COVID-19 Pandemic - Present and Future Innovation Study Design. Inquiry. 2021;58:469580211018293. doi: 10.1177/00469580211018293. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.American Association of Endodontists. Treatment Standards. Chicago: American Association of Endodontists; 2018. Available from: https://www.aae.org/specialty/wpcontent/uploads/sites/2/2018/04/TreatmentStandards_Whitepaper.pdf. Accessed 9 Aug 2021.
- 35.Mitchell J, Brackett M. Dental Anatomy and Occlusion: Mandibular Incisors-Flipped Classroom Learning Module. MedEdPORTAL. 2017;13:10587. doi: 10.15766/mep_2374-8265.10587. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Al Raisi H, Dummer PMH, Vianna ME. How is Endodontics taught? A survey to evaluate undergraduate endodontic teaching in dental schools within the United Kingdom. Int Endod J. 2019;52(7):1077–1085. doi: 10.1111/iej.13089. [DOI] [PubMed] [Google Scholar]
- 37.Petersson K, Olsson H, Soderstrom C, Fouilloux I, Jegat N, Levy G. Undergraduate education in endodontology at two European dental schools. A comparison between the Faculty of Odontology, Malmo University, Malmo, Sweden and Faculty of Odontology, Paris 5 University (Rene Descartes), France. Eur J Dent Educ. 2002;6(4):176–181. doi: 10.1034/j.1600-0579.2002.00261.x. [DOI] [PubMed] [Google Scholar]
- 38.Sadr A, Rossi-Fedele G, Love RM, George R, Parashos P, Wu MC, Friedlander L, Peters O, Moule AJ, Zimet P, et al. Revised guidelines for the endodontic education of dentistry students in Australia and New Zealand (FEBRUARY 2021) Aust Endod J. 2021;47(2):327–331. doi: 10.1111/aej.12501. [DOI] [PubMed] [Google Scholar]
- 39.Goldstein LB, Trombly R, McLeod D, Goldstein JM, Lymberopoulos G. Dental Education in the Time of COVID-19 and Beyond. Compend Contin Educ Dent. 2021;42(1):47–48. [PubMed] [Google Scholar]
- 40.Bitter K, Gruner D, Wolf O, Schwendicke F. Artificial Versus Natural Teeth for Preclinical Endodontic Training: A Randomized Controlled Trial. J Endod. 2016;42(8):1212–1217. doi: 10.1016/j.joen.2016.05.020. [DOI] [PubMed] [Google Scholar]
- 41.Decurcio DA, Lim E, Nagendrababu V, Estrela C, Rossi-Fedele G. Difficulty levels of extracted human teeth used for pre-clinical training in endodontics in an Australian dental school. Aust Endod J. 2020;46(1):47–51. doi: 10.1111/aej.12355. [DOI] [PubMed] [Google Scholar]
- 42.Reich S, Simon JF, Ruedinger D, Shortall A, Wichmann M, Frankenberger R. Evaluation of two different teaching concepts in dentistry using computer technology. Adv Health Sci Educ. 2007;12(3):321–329. doi: 10.1007/s10459-006-9004-8. [DOI] [PubMed] [Google Scholar]
- 43.Foster L, Knox K, Rung A, Mattheos N. Dental students' attitudes toward the design of a computer-based treatment planning tool. J Dent Educ. 2011;75(11):1434–1442. doi: 10.1002/j.0022-0337.2011.75.11.tb05200.x. [DOI] [PubMed] [Google Scholar]
- 44.Karl M, Graef F, Eitner S, Wichmann M, Holst S, Beck N. Student attitudes towards computer-aided testing. Eur J Dent Educ. 2011;15(2):69–72. doi: 10.1111/j.1600-0579.2010.00637.x. [DOI] [PubMed] [Google Scholar]
- 45.Streiner DL. Starting at the beginning: an introduction to coefficient alpha and internal consistency. J Pers Assess. 2003;80(1):99–103. doi: 10.1207/S15327752JPA8001_18. [DOI] [PubMed] [Google Scholar]
- 46.Lugassy D, Levanon Y, Shpack N, Levartovsky S, Pilo R, Brosh T. An interventional study for improving the manual dexterity of dentistry students. Public Library of Science one. 2019;14(2):e0211639. doi: 10.1371/journal.pone.0211639. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Seifert LB, Socolan O, Sader R, Russeler M, Sterz J. Virtual patients versus small-group teaching in the training of oral and maxillofacial surgery: a randomized controlled trial. BMC Med Educ. 2019;19(1):454. doi: 10.1186/s12909-019-1887-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.de Oliveira MLB, Verner FS, Kamburoglu K, Silva JNN, Junqueira RB. Effectiveness of Using a Mobile App to Improve Dental Students' Ability to Identify Endodontic Complications from Periapical Radiographs. J Dent Educ. 2019;83(9):1092–1099. doi: 10.21815/JDE.019.099. [DOI] [PubMed] [Google Scholar]
- 49.Oliveira EY, Crosewski NI, Silva ALM, Ribeiro CTD, de Oliveira CM, Fogaca RTH, Dias FAL. Profile of Educational Technology Use by Medical Students and Evaluation of a New Mobile Application Designed for the Study of Human Physiology. J Med Syst. 2019;43(10):313. doi: 10.1007/s10916-019-1438-7. [DOI] [PubMed] [Google Scholar]
- 50.Mardani M, Cheraghian S, Naeeni SK, Zarifsanaiey N. Effectiveness of virtual patients in teaching clinical decision-making skills to dental students. J Dent Educ. 2020;84(5):615–623. doi: 10.1002/jdd.12045. [DOI] [PubMed] [Google Scholar]
- 51.Al-Balas M, Al-Balas HI, Jaber HM, Obeidat K, Al-Balas H, Aborajooh EA, Al-Taher R, Al-Balas B. Distance learning in clinical medical education amid COVID-19 pandemic in Jordan: current situation, challenges, and perspectives. BMC Med Educ. 2020;20(1):341. doi: 10.1186/s12909-020-02257-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Khatoon B, Hill K, Walmsley AD. Mobile learning in dentistry: challenges and opportunities. Br Dent J. 2019;227(4):298–304. doi: 10.1038/s41415-019-0615-x. [DOI] [PubMed] [Google Scholar]
- 53.Brumini G, Spalj S, Mavrinac M, Biocina-Lukenda D, Strujic M, Brumini M. Attitudes towards e-learning amongst dental students at the universities in Croatia. Eur J Dent Educ. 2014;18(1):15–23. doi: 10.1111/eje.12068. [DOI] [PubMed] [Google Scholar]
- 54.Rafai N, Lemos M, Kennes LN, Hawari A, Gerhardt-Szep S, Classen-Linke I. Anatomy meets dentistry! Linking anatomy and clinical practice in the preclinical dental curriculum. BMC Med Educ. 2016;16(1):305. doi: 10.1186/s12909-016-0825-8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Lara JS, Braga MM, Zagatto CG, Wen CL, Mendes FM, Murisi PU, Haddad AE. A Virtual 3D Dynamic Model of Caries Lesion Progression as a Learning Object for Caries Detection Training and Teaching: Video Development Study. JMIR Medical Education. 2020;6(1):e14140. doi: 10.2196/14140. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Cotta KISS, Almgren MM, Macías-Moriarity LZ, Mody V. Effectiveness of flipped classroom instructional model in teaching pharmaceutical calculations. Curr Pharm Teach Learn. 2016;8(5):646–653. doi: 10.1016/j.cptl.2016.06.011. [DOI] [Google Scholar]
- 57.Giuliano CAML. Evaluation of a flipped drug literature evaluation course. Am J Pharm Educ. 2016;80(4):66. doi: 10.5688/ajpe80466. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 58.Herrero JI, Quiroga J. Flipped classroom improves results in pathophysiology learning: results of a nonrandomized controlled study. Adv Physiol Educ. 2020;44(3):370–375. doi: 10.1152/advan.00153.2019. [DOI] [PubMed] [Google Scholar]
- 59.Vanka A, Vanka S, Wali O. Flipped classroom in dental education: A scoping review. Eur J Dent Educ. 2020;24(2):213–226. doi: 10.1111/eje.12487. [DOI] [PubMed] [Google Scholar]
- 60.Hew KF, Lo CK. Flipped classroom improves student learning in health professions education: a meta-analysis. BMC Med Educ. 2018;18(1):38. doi: 10.1186/s12909-018-1144-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Wong G, Apthorpe HC, Ruiz K, Nanayakkara S. An innovative educational approach in using instructional videos to teach dental local anaesthetic skills. Eur J Dent Educ. 2019;23(1):28–34. doi: 10.1111/eje.12382. [DOI] [PubMed] [Google Scholar]
- 62.Zhu H, Yan XL, Shen DJ, Zhang SN, Huang J. Application and exploration of micro-class combined with flipped classroom in cardiopulmonary resuscitation teaching for dental students. Shanghai Journal of Stomatology. 2018;27(3):333–336. [PubMed] [Google Scholar]
- 63.Galibourg A, Peters OA, Diemer F, Nasr K, Maret D. Continuing endodontic education and COVID-19: before, during and after? Int Endod J. 2020;53(11):1598–1599. doi: 10.1111/iej.13368. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 64.Moraros J, Islam A, Yu S, Banow R, Schindelka B. Flipping for success: evaluating the effectiveness of a novel teaching approach in a graduate level setting. BMC Med Educ. 2015;15:27. doi: 10.1186/s12909-015-0317-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Lee C, Kim SW. Effectiveness of a Flipped Classroom in Learning Periodontal Diagnosis and Treatment Planning. J Dent Educ. 2018;82(6):614–620. doi: 10.21815/JDE.018.070. [DOI] [PubMed] [Google Scholar]
- 66.Mukhtar K, Javed K, Arooj M, Sethi A. Advantages, Limitations and Recommendations for online learning during COVID-19 pandemic era. Pak J Med Sci. 2020;36(COVID19-S4):S27–S31. doi: 10.12669/pjms.36.COVID19-S4.2785. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Kanneganti A, Lim KMX, Chan GMF, Choo SN, Choolani M, Ismail-Pratt I, Logan SJS. Pedagogy in a pandemic - COVID-19 and virtual continuing medical education (vCME) in obstetrics and gynecology. Acta Obstet Gynecol Scand. 2020;99(6):692–695. doi: 10.1111/aogs.13885. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Hung M, Licari FW, Hon ES, Lauren E, Su S, Birmingham WC, Wadsworth LL, Lassetter JH, Graff TC, Harman W, et al. In an era of uncertainty: Impact of COVID-19 on dental education. J Dent Educ. 2021;85(2):148–156. doi: 10.1002/jdd.12404. [DOI] [PubMed] [Google Scholar]
- 69.Nasseripour M, Turner J, Rajadurai S, San Diego J, Quinn B, Bartlett A, Volponi AA. COVID 19 and Dental Education: Transitioning from a Well-established Synchronous Format and Face to Face Teaching to an Asynchronous Format of Dental Clinical Teaching and Learning. J Med Educ Curric Dev. 2021;8:2382120521999667. doi: 10.1177/2382120521999667. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Zheng M, Bender D, Lyon C. Online learning during COVID-19 produced equivalent or better student course performance as compared with pre-pandemic: empirical evidence from a school-wide comparative study. BMC Med Educ. 2021;21(1):495. doi: 10.1186/s12909-021-02909-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 71.Hattar S, AlHadidi A, Sawair FA, Alraheam IA, El-Ma'aita A, Wahab FK. Impact of COVID-19 pandemic on dental education: online experience and practice expectations among dental students at the University of Jordan. BMC Med Educ. 2021;21(1):151. doi: 10.1186/s12909-021-02584-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 72.Abbasi S, Ayoob T, Malik A, Memon SI. Perceptions of students regarding E-learning during Covid-19 at a private medical college. Pak J Med Sci. 2020;36(COVID19-S4):S57–S61. doi: 10.12669/pjms.36.COVID19-S4.2766. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Amir LR, Tanti I, Maharani DA, Wimardhani YS, Julia V, Sulijaya B, Puspitawati R. Student perspective of classroom and distance learning during COVID-19 pandemic in the undergraduate dental study program Universitas Indonesia. BMC Med Educ. 2020;20(1):392. doi: 10.1186/s12909-020-02312-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Wang K, Zhang L, Ye L. A nationwide survey of online teaching strategies in dental education in China. J Dent Educ. 2021;85(2):128–134. doi: 10.1002/jdd.12413. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 75.Kemp N, Grieve R. Face-to-face or face-to-screen? Undergraduates’ opinions and test performance in classroom vs online learning. Front Psychol. 2014;5:1278. doi: 10.3389/fpsyg.2014.01278. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 76.AlQhtani A, AlSwedan N, Almulhim A, Aladwan R, Alessa Y, AlQhtani K, Albogami M, Altwairqi K, Alotaibi F, AlHadlaq A, et al. Online versus classroom teaching for medical students during COVID-19: measuring effectiveness and satisfaction. BMC Med Educ. 2021;21(1):452. doi: 10.1186/s12909-021-02888-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Bock A, Kniha K, Goloborodko E, Lemos M, Rittich AB, Mohlhenrich SC, Rafai N, Holzle F, Modabber A. Effectiveness of face-to-face, blended and e-learning in teaching the application of local anaesthesia: a randomised study. BMC Med Educ. 2021;21(1):137. doi: 10.1186/s12909-021-02569-z. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Schmitz SM, Schipper S, Lemos M, Alizai PH, Kokott E, Brozat JF, Neumann UP, Ulmer TF. Development of a tailor-made surgical online learning platform, ensuring surgical education in times of the COVID19 pandemic. BMC Surg. 2021;21(1):196. doi: 10.1186/s12893-021-01203-5. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Decurcio DA, Lim E, Chaves GS, Nagendrababu V, Estrela C, Rossi-Fedele G. Pre-clinical endodontic education outcomes between artificial versus extracted natural teeth: a systematic review. Int Endod J. 2019;52(8):1153–1161. doi: 10.1111/iej.13116. [DOI] [PubMed] [Google Scholar]
- 80.Robberecht L, Hornez JC, Dehurtevent M, Dufour T, Labreuche J, Deveaux E, Chai F. Optimization and Preclinical Perception of an Artificial Simulator for Endodontic Training: A Preliminary Study. J Dent Educ. 2017;81(3):326–332. doi: 10.1002/j.0022-0337.2017.81.3.tb06278.x. [DOI] [PubMed] [Google Scholar]
- 81.Gancedo-Caravia L, Bascones J, Garcia-Barbero E, Arias A. Suitability of different tooth replicas for endodontic training: perceptions and detection of common errors in the performance of postgraduate students. Int Endod J. 2020;53(4):562–572. doi: 10.1111/iej.13251. [DOI] [PubMed] [Google Scholar]
- 82.Mesgouez C, Rilliard F, Matossian L, Nassiri K, Mandel E. Influence of operator experience on canal preparation time when using the rotary Ni-Ti ProFile system in simulated curved canals. Int Endod J. 2003;36(3):161–165. doi: 10.1046/j.1365-2591.2003.00625.x. [DOI] [PubMed] [Google Scholar]
- 83.Munoz E, Forner L, Llena C. Influence of operator's experience on root canal shaping ability with a rotary nickel-titanium single-file reciprocating motion system. J Endod. 2014;40(4):547–550. doi: 10.1016/j.joen.2013.08.027. [DOI] [PubMed] [Google Scholar]
- 84.Goldberg M, Dahan S, Machtou P. Centering Ability and Influence of Experience When Using WaveOne Single-File Technique in Simulated Canals. Int J Dent. 2012;2012:206321. doi: 10.1155/2012/206321. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Baumann MA, Roth A. Effect of experience on quality of canal preparation with rotary nickel-titanium files. Oral Surg Oral Med Oral Pathol Oral Radiol Endod. 1999;88(6):714–718. doi: 10.1016/S1079-2104(99)70015-6. [DOI] [PubMed] [Google Scholar]
- 86.Muñoz E, Forner L, Garcet S, Rodríguez-Lozano FJ, Llena C. Canal shaping with a reciprocating system is easy to learn. Int Endod J. 2019;52(8):1244–1249. doi: 10.1111/iej.13111. [DOI] [PubMed] [Google Scholar]
- 87.Baaij A, Ozok AR. Influence of Method of Teaching Endodontics on the Self-Efficacy and Self-Perceived Competence of Undergraduate Dental Students. Eur Endod J. 2018;3(1):31–37. doi: 10.5152/eej.2017.17048. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 88.Basagaoglu Demirekin Z, Buyukcavus MH. Effect of distance learning on the quality of life, anxiety and stress levels of dental students during the COVID-19 pandemic. BMC Med Educ. 2022;22(1):309. doi: 10.1186/s12909-022-03382-y. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Botelho M, Gao X, Bhuyan SY. An analysis of clinical transition stresses experienced by dental students: A qualitative methods approach. Eur J Dent Educ. 2018;22(3):e564–e572. doi: 10.1111/eje.12353. [DOI] [PubMed] [Google Scholar]
- 90.Harris M, Wilson JC, Holmes S, Radford DR. Perceived stress and well-being among dental hygiene and dental therapy students. Br Dent J. 2017;222(2):101–106. doi: 10.1038/sj.bdj.2017.76. [DOI] [PubMed] [Google Scholar]
- 91.Hayes A, Hoover JN, Karunanayake CP, Uswak GS. Perceived causes of stress among a group of western Canadian dental students. BMC Res Notes. 2017;10(1):714. doi: 10.1186/s13104-017-2979-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 92.Elani HW, Allison PJ, Kumar RA, Mancini L, Lambrou A, Bedos C. A systematic review of stress in dental students. J Dent Educ. 2014;78(2):226–242. doi: 10.1002/j.0022-0337.2014.78.2.tb05673.x. [DOI] [PubMed] [Google Scholar]
- 93.Chutinan S, Kim J, Chien T, Meyer HY, Ohyama H. Can an interactive case-based activity help bridge the theory-practice gap in operative dentistry? Eur J Dent Educ. 2021;25(1):199–206. doi: 10.1111/eje.12591. [DOI] [PubMed] [Google Scholar]
- 94.Hanafi A, Donnermeyer D, Schafer E, Burklein S. Perception of a modular 3D print model in undergraduate endodontic education. Int Endod J. 2020;53(7):1007–1016. doi: 10.1111/iej.13299. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Data Availability Statement
All data are available from the corresponding author upon reasonable request.