Abstract
Purpose:
The management of moderate and severe slipped capital femoral epiphysis is controversial. While in situ fixation is commonly used, the modified Dunn’s procedure is increasingly popular within high-volume centers. We compared the clinical and radiological outcomes, as well as the rates of femoral head avascular necrosis or chondrolysis in patients managed with either modified Dunn’s procedure or in situ fixation.
Methods:
A systematic search of the PubMed, Embase, The Cochrane Library, Science Direct, and Web of Science was performed in August 2021. Studies comparing outcomes and complications of modified Dunn’s procedure versus in situ fixation in patients with moderate or severe slipped capital femoral epiphysis were included.
Results:
A total of four studies were included in the final analysis. Modified Dunn’s procedure did not result in improved clinical outcomes. However, radiological outcomes as measured using Southwick angles and Alpha angles were significantly improved in the modified Dunn’s procedure group, with a mean difference of −14.68 (p < 0.00001) and −34.26 degrees (p < 0.00001), respectively, compared to in situ fixation. There was no difference in the odds of femoral head avascular necrosis or chondrolysis, with odds ratio of 0.99 (p = 0.97).
Conclusion:
Within the limits of our study, modified Dunn’s procedure did not improve clinical outcomes. There were significantly improved radiological outcomes without higher odds of femoral head avascular necrosis or chondrolysis. Further long-term studies are required to better guide management of moderate and severe slipped capital femoral epiphysis, especially in unstable slips. In the meantime, we recommend that the modified Dunn’s procedure, if done, be restricted to high-volume centers with low complication rates.
Level of evidence:
Level III—Systematic review of Level III studies.
Prospero Registration No.:
CRD42021279503.
Keywords: Slipped capital femoral epiphysis, modified Dunn’s procedure, in situ fixation, systematic review, meta-analysis, treatment
Introduction
Slipped capital femoral epiphysis (SCFE) is a common condition, affecting approximately 8 to 10 adolescents per 100,000 in the Western world.1–4 While predominantly idiopathic, significant risk factors include childhood obesity, Aboriginal or Pacific Islander descent, and male sex.1,3,5 In rare cases, SCFE can be due to endocrinopathies, such as hypothyroidism, Babinski–Fröhlich syndrome, or hyperparathyroidism; or metabolic derangements, such as hypovitaminosis D.6,7 A previous study by Loder et al. estimated that 98% of idiopathic SCFEs occur in varus, whereas the remaining occurs in valgus. 8
SCFE may be classified based on stability and severity of disease. The Loder’s classification is often used to define stability, whereby a stable slip is defined as one where the child can ambulate with or without the aid of crutches. An unstable slip is that where the child cannot ambulate even with aids. 9 On the contrary, severity of disease is classified using the Southwick’s slip angle. Mild disease is then defined as a slip angle of <30°, moderate disease is defined as a slip angle of between 30° and 50°, and severe disease is defined as a slip angle of >50°.10,11 The diagnosis of SCFE is usually based on radiographical findings; however, ultrasonography may also be utilized to both diagnose and classify the severity of disease.12,13
The current gold standard management of mild slips is percutaneous in situ fixation, usually with one or two screws. In this patient population, such methods have been shown to provide satisfactory long-term functional outcomes. 14 However, the long-term functional outcomes of in situ fixation for moderate slips are not as good,15–17 and the outcomes for severe slips have been consistently poor.18,19 Alternative treatment strategies such as serendipitous closed reduction and percutaneous fixation, and capital realignment via the modified Dunn’s procedure have been described in literature for the management of moderate and severe slips, 20 although it is unclear whether these strategies indeed improve clinical outcomes. Hence, comparative studies between treatment strategies, such as in situ fixation and modified Dunn’s procedure, with a focus on clinical outcomes are required.
In this study, we aim to compare the clinical and radiological outcomes in patients with moderate or severe SCFE treated with the modified Dunn’s procedure versus those who received percutaneous in situ fixation. We also aim to compare the odds of femoral head avascular necrosis or chondrolysis in the two procedures. To the best of the authors’ knowledge, this is the first systematic review and meta-analysis to compare the outcomes of these treatment strategies. Furthermore, research on the optimal treatment strategy for severe SCFE has previously been identified as a priority by the British Society for Children’s Orthopaedic Surgery. 21
Materials and methods
The systematic review was performed in accordance with the recommendations of Preferred Reporting Items for Systematic Reviews and Meta-Analyses (PRISMA). This systematic review protocol was registered with PROSPERO (Registration Number: CRD42021279503).
Search strategy
We performed a systematic search of the literature across PubMed, Embase, The Cochrane Library, Science Direct, and Web of Science from the date of inception of each database through to 15 August 2021. The population of interest were patients with moderate or severe SCFE. Comparisons were made between patients who received the modified Dunn’s procedure and in situ fixation. The outcomes of interest were the clinical and radiological outcomes, as well as odds of femoral head avascular necrosis or chondrolysis.
A literature search was performed using the following search terms and Boolean operators: “Dunn” OR “capital realignment” AND “pinning” OR “fixation” AND “slipped capital femoral epiphysis” OR “slipped upper femoral epiphysis.” The reference lists of eligible studies and review articles were scrutinized for any further articles, which may have been missed in the literature search. The titles and abstracts were then screened by two reviewers (TC and TS) for relevance and consideration and compiled into a provisional list. The provisional list was then assessed independently by the same two reviewers, each having read the full text for their potential inclusion. The two reviewers had consensus of the included articles.
All published studies with sufficient extractable data were included. Both stable and unstable slips were included. No gray literature search was performed. Non-comparative studies, case series, studies with less than three patients in each group, or studies that utilized closed reduction techniques for the fixation group were excluded. Studies were not excluded based upon their published language or geographic location.
Data collection and assessment of risk of bias
Data extraction was performed by the first reviewer (TC) and validated by the second reviewer (TS). The individual study characteristics and outcomes of interest were assessed. The methodological quality of studies included was assessed independently by both reviewers using the Newcastle-Ottawa Scale. Publication bias was assessed using Sterne and Egger’s funnel plots. 22
Outcomes and statistical analysis
The outcomes of interest were clinical and radiological outcomes, and odds of femoral head avascular necrosis or chondrolysis in each group. Continuous variables were expressed as mean ± standard deviation. Statistical analysis was performed using the Mantel–Haenszel method, utilizing either a fixed effect model if the heterogeneity is <50% or a random effects model if the heterogeneity is >50%. Odds ratio (OR) was used to illustrate the effects of each treatment arm on Forest plots for discrete variables, whereas mean difference (MD) was used in continuous variables. The corresponding 95% confidence interval (95% CI) and heterogeneity of data (I2) are also illustrated in both Forest plots and full text. The statistical software used in this study was RevMan 5.4 (The Cochrane Collaboration, 2020).
Results
Search results
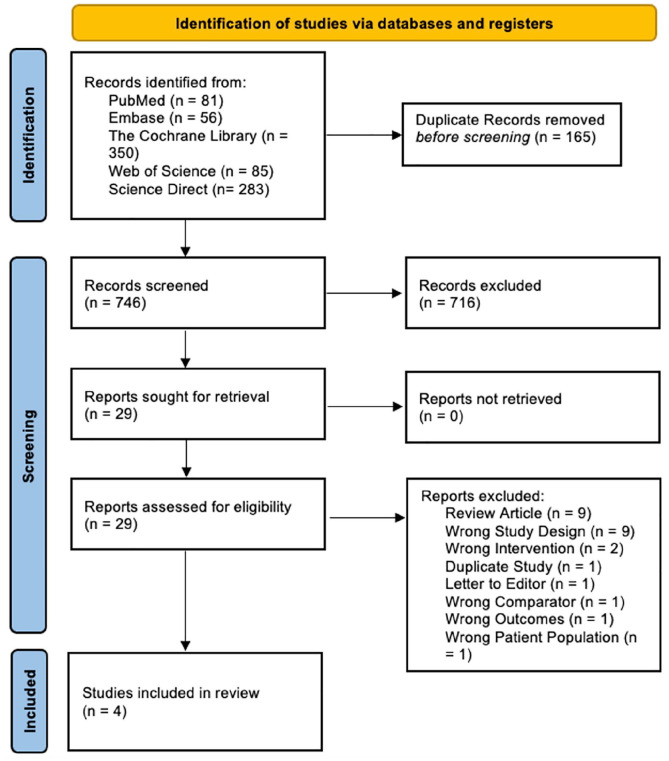
In total, 911 studies were identified with the initial search strategy; 165 duplicate studies were removed. From the remainder, a further 716 studies were excluded by screening titles and abstracts. Four studies were included in the final analysis.23–26 These are summarized in Figure 1.
Figure 1.
PRISMA flow diagram.
PRISMA: Preferred Reporting Items for Systematic Reviews and Meta-Analyses.
All four studies included were retrospective cohort studies, of which only one study enrolled both stable and unstable slips. 23 Most of the unstable slips in this study received the modified Dunn’s procedure. The remaining three studies only enrolled stable slips, as determined using the Loder’s classification. Baseline characteristics of the study populations were otherwise relatively similar, as shown in Table 1. The follow-up period, however, varied between studies, ranging from 4 to 10 years. There were more males compared to females included in all studies and groups, indicating a likely risk factor for moderate or severe slip. In total, 188 hips were analyzed, with 69 hips receiving in situ fixation and 119 hips receiving the modified Dunn’s procedure. Surgical techniques for each study were summarized in Table 2.
Table 1.
Baseline characteristics of included studies.
| Author | Location | Study design | N | Final follow-up | In situ fixation | Modified Dunn’s procedure | ||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Number of hips | Gender (M/F) | Age at surgery | BMI (kg/m2) | Preoperative Southwick angle (°) | Stability of slip (stable/unstable) | Number of hips | Gender (M/F) | Age at surgery | BMI (kg/m2) | Preoperative Southwick angle (°) | Stability of slip (stable/unstable) | |||||
| Arora et al. 23 | India | Retrospective cohort | 26 | 4 years | 18 | NS | NS | NS | 59 ± 18.02 | 16/2 | 8 | NS | NS | NS | 72.37 ± 15.83 | 0/8 |
| Galletta et al. 24 | Italy | Retrospective cohort | 103 | 10 years | 22 | 20/1 | 12.9 | 23 | NS a | 22/0 | 81 | 59/17 | 13.6 | 24.2 | NS a | 81/0 |
| Novais et al. 25 | USA | Retrospective cohort | 30 | 6 years | 15 | 9/6 | 13 | NS | 63 | 15/0 | 15 | 11/4 | 14 | NS | 65 | 15/0 |
| Trisolino et al. 26 | Italy | Retrospective cohort | 29 | 7 years | 14 | 11/3 | 13 ± 1.0 | 24 ± 4 | 62 ± 9 | 14/0 | 15 | 11/4 | 13.9 ± 2.3 | 24 ± 4 | 68 ± 11 | 15/0 |
N: total number of participants; M: male; F: female; BMI: body mass index; NS: not stated.
This study included only moderate and severe slips, but the mean preoperative Southwick angle was not published.
Table 2.
Surgical technique.
| Author | In situ fixation | Modified Dunn’s procedure |
|---|---|---|
| Arora et al. 23 | Single cannulated screw in the center of epiphysis with at least three threads across the physis Postoperative rehabilitation not described |
Ganz safe surgical dislocation with capital realignment; fixation method not described Intraoperative head vascularity assessment was performed to ensure no tension on the vascular pedicle Postoperative rehabilitation not described |
| Galletta et al. 24 | Single 6.5-mm cannulated screw Postoperatively, non-weightbearing for 6 weeks |
Ganz safe surgical dislocation with capital realignment; femoral head stabilized with single 3-mm threaded wires, and the trochanter stabilized with two fully threaded wires Posteroinferior callus formation removed to release tension over the deep branches of medial femoral circumflex artery; intraoperatively, 2-mm hole drilled in anterior femoral head before and after reduction to check for epiphyseal perfusion Postoperatively, non-weightbearing for 3 months; active abduction and passive adduction were restricted for 4 to 6 weeks |
| Novais et al. 25 | Single 6.5- or 7.3-mm cannulated screw in the center of epiphysis Postoperatively, partial weightbearing with crutches for 6 weeks |
Ganz safe surgical dislocation with capital realignment; femoral head stabilized with either two 6.5-mm cannulated screws or three 3-mm threaded wires, and the trochanter stabilized with either two or three 3.5-mm screws Posterior callus removed; no description regarding intraoperative monitoring of vascularity Postoperatively, non-weightbearing for 6 weeks followed by protected weightbearing with crutches for 6 weeks |
| Trisolino et al. 26 | Two 4.5-mm fully threaded screws Postoperatively, partial weightbearing for 6 weeks |
Ganz safe surgical dislocation with capital realignment; femoral head stabilized with threaded wires, and the trochanter stabilized with cortical screws No description regarding intraoperative monitoring of vascularity Postoperatively, non-weightbearing for 6 weeks followed by protected weightbearing with crutches for 6 weeks |
Clinical outcomes
Clinical outcomes were reported using a variety of scales. Two studies utilized the Merle d’Aubigné score:23,24 one study utilized the Heyman and Herndon Classification score 25 and the final study utilized the Non-Arthritic Hip score. 26 Due to high variability, a meta-analysis was not performed to evaluate this outcome. Utilizing their respective clinical outcome measures, two studies showed a higher proportion of “good” or “excellent” outcomes in the modified Dunn’s procedure group, as compared to the in situ fixation group.23,27 The remaining two studies did not show any improvement in clinical outcomes between groups.24,26 It should be noted that the largest series in our included studies by Galleta et al. showed no improvement in clinical outcomes.
Radiological outcomes
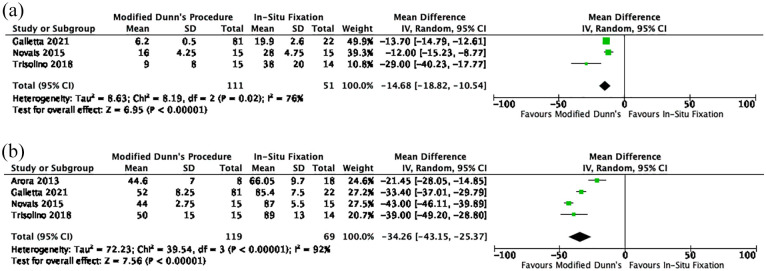
Radiological outcomes were discussed in terms of postoperative Southwick and Alpha angles. Three studies compared postoperative Southwick angles.24–26 There was significant heterogeneity between studies (I2 = 76%, p = 0.02), and hence a random effects model was utilized. Based on our meta-analysis, there was significant improvement in postoperative Southwick angles favoring the modified Dunn’s procedure group (MD = –14.68, 95% CI = –8.82 to −10.54, p < 0.00001). The results of this are shown in Figures 2(a).
Figure 2.
Postoperative radiological outcomes: (a) Southwick angle and (b) Alpha angle.
All four studies compared postoperative Alpha angles. There was significant heterogeneity between studies (I2 = 92%, p < 0.0001), and hence a random effects model was utilized. Based on the available data, there was also significant improvement in postoperative Alpha angles favoring the modified Dunn’s procedure group (MD = –34.26, 95% CI = –43.15 to −25.37, p < 0.00001). The results of this are shown in Figure 2(b).
Odds of avascular necrosis or chondrolysis
All studies reported surgical complications in both treatment arms. There was no significant heterogeneity (I2 = 27%, p = 0.25) between studies, and hence a fixed effect model was used. There was no significant difference in odds of avascular necrosis of the femoral head or chondrolysis between the two treatment arms (OR = 0.99, 95% CI = 0.43–2.27, p = 0.97). The rates of avascular necrosis or chondrolysis were 18.5% in the modified Dunn’s procedure group and 14.5% in the in situ fixation group (Figure 3).
Figure 3.
Odds of avascular necrosis or chondrolysis.
Risk of bias analysis
Risk of bias in individual studies was analyzed using the Newcastle-Ottawa Scale. The results are displayed in Table 3. All studies demonstrated adequate selection criteria. The study by Arora et al. was included despite one patient in the in situ fixation group having mild SCFE. 23 This decision was made as all other participants in this study would have otherwise met our inclusion criteria, and it is unlikely that a single patient would significantly skew the dataset. The follow-up lengths and assessments were otherwise adequate in all studies. One study by Novais et al. had a high lost to follow-up rate. 25 Sterne and Egger’s funnel plots were plotted to assess the risk of publication bias. There was symmetry observed between studies, suggesting a low risk of publication bias (Figure 4).
Table 3.
Newcastle-Ottawa Scale.
| Author | Selection | Comparability | Outcome | |||||
|---|---|---|---|---|---|---|---|---|
| Representativeness of modified Dunn’s procedure cohort | Selection of in situ fixation cohort | Ascertainment of exposure | Outcome of interest not present at the start of study | Assessment of outcome | Follow-up length | Adequacy of follow-up | ||
| Arora et al. 23 | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ | ☆ |
| Galletta et al. 24 | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ |
| Novais et al. 25 | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | |
| Trisolino et al. 26 | ☆ | ☆ | ☆ | ☆ | ☆☆ | ☆ | ☆ | ☆ |
Figure 4.

Funnel plot analysis.
Discussion
The results of our systematic review and meta-analysis suggest that the short-term clinical outcomes in patients with moderate or severe slips treated with the modified Dunn’s procedure are similar to those treated with in situ fixation. There was significant improvement in radiological outcomes (Southwick slip angle and Alpha angle), with no difference in the odds of femoral head avascular necrosis or chondrolysis.
Studies that used the modified Dunn’s procedure utilized safe surgical dislocation as described by Ganz. Capital realignment was performed and held by either threaded wires or screws. In two studies, callus was removed to reduce tension over the medial femoral circumflex artery.24,25 Intraoperative monitoring of vascularity was performed in two studies.23,24 Whereas in in-situ fixation the head is fixed in-situ to prevent further slip, the modified Dunn’s procedure is performed as an open procedure to obtain alignment, thus accounting for improved radiological parameters. Despite it being an open procedure, the reported rates of chondrolysis or avascular necrosis were not significantly higher than those who had in situ fixation, though the rates are still high in both groups (18.5% in the modified Dunn’s procedure and 14.5% in the in situ fixation). Although these studies show favorable radiological outcomes in the modified Dunn’s procedure group, this may not be generalizable to all centers, as there is an associated learning curve. 28 It is known that in technically challenging procedures, surgeon experience and expertise have a significant effect on postoperative outcomes. In addition, with almost all participants having a stable slip, it is difficult to comment on the rate of complications in unstable hips.
In patients with moderate or severe SCFE managed with in situ fixation, it could be postulated that there is potential for the development of symptomatic femoroacetabular impingement (FAI). The posteromedial displacement of the epiphysis in SCFE results in the femoral metaphysis being placed in an anterolateral position. This could potentially result in the femoral metaphysis impinging upon the anterior acetabulum on flexion of the hip. 29 In the three studies where symptoms of FAI were documented, symptomatic FAI occurred in approximately 40% of patients managed with in situ pinning, where 9/18 hips in the Arora et al. study, 7/15 hips in the Novais et al. study, and 3/14 hips in the Trisolino et al. study developed FAI.23,25,26 Although not quantified in the study by Galletta et al., it was recognized that most inferior outcomes in the in situ fixation group were due to hip pain during sports and a positive anterior impingement test. 24 However, it must be recognized that previous long-term studies have shown considerable remodeling of this deformity.30–32 Given the relatively short follow-up period in our included studies, ranging from 4 to 10 years, it is unclear how many of these patients were affected by FAI or osteoarthritis following skeletal maturity.
All studies in our analysis utilized either conventional cannulated or fully threaded screws for in situ fixation. However, this does not reflect the full spectrum of options available to orthopedic surgeons. For instance, the use of unthreaded fixation using the Hansson hook-pin, proximally threaded screws, or growing implants, such as the Pega Medical Free Gliding (FG) screws and Synthes SCFE screws, may encourage more remodeling of the hip, preventing coxa breva following fixation.33–36 Previous research has shown that in moderate to severe slips, the incidence of remodeling was 50% following conventional pinning. 37 The extent of improvement in remodeling and its impact on long-term clinical outcomes, with the use of these systems, however, have yet to be fully ascertained.
There are several limitations of our study. First, there are limited studies comparing the two interventions. The sample size in most studies is small, which may lead to small-study effect, where there is overstatement of the treatment effects. 38 All included studies were retrospective in nature, which, by design, may have introduced bias. With such small cohorts, it is likely that surgeon experience or preference may have played a role in the allocation of one intervention over the other. Second, all but one study included only stable slips, which may have significantly influenced the outcomes. In addition, there was significant variability in the measures for clinical outcomes, which precluded meta-analysis. Furthermore, there was significant heterogeneity seen in radiological outcomes, which was not reproduced in the assessment of avascular necrosis or chondrolysis rates. This may have likely been due to interobserver variability in the calculation of the radiographical values, although it is possible that methodological heterogeneity may have played a role in this.
In conclusion, our study suggests that the short- to medium-term clinical outcome of in situ fixation and the modified Dunn’s procedure was similar in patients with moderate to severe SCFE, despite significant radiological outcomes seen with the latter procedure. There was no difference in the odds of avascular necrosis, despite the fact that the modified Dunn’s procedure was performed open. Higher quality prospective randomized controlled studies with comparison between different strategies with long-term follow-up and a standardized reporting system for quantification of clinical outcomes may reliably enhance our comparison between these treatment arms to guide optimal management for this patient cohort. In the meantime, we recommend that the modified Dunn’s procedure should be restricted to high-volume centers with low complication rates.
Supplemental Material
Supplemental material, sj-docx-1-cho-10.1177_18632521221078864 for Is the modified Dunn’s procedure superior to in situ fixation?: A systematic review and meta-analysis of comparative studies for management of moderate and severe slipped capital femoral epiphysis by Tim Cheok, Thomas Smith, Morgan Berman, Matthew Jennings, Kanishka Williams, Pradeep Mathew Poonnoose, Jaideep Rawat and Bruce Foster in Journal of Children’s Orthopaedics
Acknowledgments
We would like to acknowledge the contribution of Catherine Brady, Flinders University librarian, for their assistance in performing the literature search.
Footnotes
Author contributions: T.C. performed the literature search, systematic review, risk of bias analysis, statistical analysis, and writing of the manuscript. T.S. performed the systematic review, risk of bias analysis, statistical analysis, and writing of the manuscript. M.B. and M.J. assisted in the statistical analysis and writing the manuscript. K.W. and P.M.P. assisted in writing the manuscript. J.R. and B.F. supervised and contributed to the final manuscript. All authors discussed the results and analysis, and contributed to the final manuscript.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Supplemental material: Supplemental material for this article is available online.
References
- 1. Nguyen AR, Ling J, Gomes B, et al. Slipped capital femoral epiphysis: rising rates with obesity and aboriginality in South Australia. J Bone Joint Surg Br 2011; 93(10): 1416–1423. [DOI] [PubMed] [Google Scholar]
- 2. Murray AW, Wilson NI. Changing incidence of slipped capital femoral epiphysis: a relationship with obesity. J Bone Joint Surg Br 2008; 90(1): 92–94. [DOI] [PubMed] [Google Scholar]
- 3. Lehmann CL, Arons RR, Loder RT, et al. The epidemiology of slipped capital femoral epiphysis: an update. J Pediatr Orthop 2006; 26(3): 286–290. [DOI] [PubMed] [Google Scholar]
- 4. Henrikson B. The incidence of slipped capital femoral epiphysis. Acta Orthop Scand 1969; 40(3): 365–372. [DOI] [PubMed] [Google Scholar]
- 5. Stott S, Bidwell T. Epidemiology of slipped capital femoral epiphysis in a population with a high proportion of New Zealand Maori and Pacific children. N Z Med J 2003; 116(1184): U647. [PubMed] [Google Scholar]
- 6. Loder RT, Wittenberg B, DeSilva G. Slipped capital femoral epiphysis associated with endocrine disorders. J Pediatr Orthop 1995; 15(3): 349–356. [DOI] [PubMed] [Google Scholar]
- 7. Madhuri V, Arora SK, Dutt V. Slipped capital femoral epiphysis associated with vitamin D deficiency: a series of 15 cases. Bone Joint J 2013; 95-b(6): 851–854. [DOI] [PubMed] [Google Scholar]
- 8. Loder RT, O’Donnell PW, Didelot WP, et al. Valgus slipped capital femoral epiphysis. J Pediatr Orthop 2006; 26(5): 594–600. [DOI] [PubMed] [Google Scholar]
- 9. Loder RT, Richards BS, Shapiro PS, et al. Acute slipped capital femoral epiphysis: the importance of physeal stability. J Bone Joint Surg Am 1993; 75(8): 1134–1140. [DOI] [PubMed] [Google Scholar]
- 10. Alter AH. Slipped capital femoral epiphysis: long-term follow-up study of one hundred and twenty-one patients: D. W. Boyer, M. R. Mickelson and B. Ponsetti. J Bone Joint Surg 63A: 85–95 (January), 1981. J Pediatr Surg 1981; 16(5): 773–774. [PubMed] [Google Scholar]
- 11. Southwick WO. Osteotomy through the lesser trochanter for slipped capital femoral epiphysis. J Bone Joint Surg Am 1967; 49(5): 807–835. [PubMed] [Google Scholar]
- 12. Terjesen T. Ultrasonography for diagnosis of slipped capital femoral epiphysis. Acta Orthop Scand 1992; 63(6): 653–657. [DOI] [PubMed] [Google Scholar]
- 13. Kallio PE, Lequesne GW, Paterson DC, et al. Ultrasonography in slipped capital femoral epiphysis. Diagnosis and assessment of severity. J Bone Joint Surg Br 1991; 73(6): 884–889. [DOI] [PubMed] [Google Scholar]
- 14. Carney BT, Weinstein SL, Noble J. Long-term follow-up of slipped capital femoral epiphysis. J Bone Joint Surg Am 1991; 73(5): 667–674. [PubMed] [Google Scholar]
- 15. Hansson G, Billing L, Högstedt B, et al. Long-term results after nailing in situ of slipped upper femoral epiphysis. J Bone Joint Surg Br 1998; 80(1): 70–77. [DOI] [PubMed] [Google Scholar]
- 16. Terjesen T, Wensaas A. Prognostic factors for long-term outcome of chronic slipped capital femoral epiphysis treated with fixation in situ. J Child Orthop 2017; 11(2): 114–119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Accadbled F, Murgier J, Delannes B, et al. In situ pinning in slipped capital femoral epiphysis: long-term follow-up studies. J Child Orthop 2017; 11(2): 107–109. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. de Poorter JJ, Beunder TJ, Gareb B, et al. Long-term outcomes of slipped capital femoral epiphysis treated with in situ pinning. J Child Orthop 2016; 10(5): 371–379. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Boero S, Brunenghi GM, Carbone M, et al. Pinning in slipped capital femoral epiphysis: long-term follow-up study. J Pediatr Orthop B 2003; 12(6): 372–379. [DOI] [PubMed] [Google Scholar]
- 20. Aprato A, Conti A, Bertolo F, et al. Slipped capital femoral epiphysis: current management strategies. Orthop Res Rev 2019; 11: 47–54. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Perry DC, Wright JG, Cooke S, et al. A consensus exercise identifying priorities for research into clinical effectiveness among children’s orthopaedic surgeons in the United Kingdom. Bone Joint J 2018; 100-b(5): 680–684. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Sterne JAC, Egger M, Smith GD. Investigating and dealing with publication and other biases in meta-analysis. BMJ 2001; 323(7304): 101–105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Arora S, Dutt V, Palocaren T, et al. Slipped upper femoral epiphysis: outcome after in situ fixation and capital realignment technique. Indian J Orthop 2013; 47(3): 264–271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24. Galletta C, Aprato A, Giachino M, et al. Modified Dunn procedure versus percutaneous pinning in moderate/severe stable slipped capital femoral epiphyses. Hip Int. Epub ahead of print 8 April 2021. DOI: 10.117/11207000211004862. [DOI] [PubMed] [Google Scholar]
- 25. Novais EN, Hill MK, Carry PM, et al. Modified Dunn procedure is superior to in situ pinning for short-term clinical and radiographic improvement in severe stable SCFE. Clin Orthop Relat Res 2015; 473(6): 2108–2117. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Trisolino G, Stilli S, Gallone G, et al. Comparison between modified Dunn procedure and in situ fixation for severe stable slipped capital femoral epiphysis. Acta Orthop 2018; 89(2): 211–216. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Novais EN, Maranho DA, Heare T, et al. The modified Dunn procedure provides superior short-term outcomes in the treatment of the unstable slipped capital femoral epiphysis as compared to the inadvertent closed reduction and percutaneous pinning: a comparative clinical study. Int Orthop 2019; 43(3): 669–675. [DOI] [PubMed] [Google Scholar]
- 28. Upasani VV, Matheney TH, Spencer SA, et al. Complications after modified Dunn osteotomy for the treatment of adolescent slipped capital femoral epiphysis. J Pediatr Orthop 2014; 34: 661–667. [DOI] [PubMed] [Google Scholar]
- 29. Hosalkar HS, Pandya NK, Bomar JD, et al. Hip impingement in slipped capital femoral epiphysis: a changing perspective. J Child Orthop 2012; 6(3): 161–172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Reinhardt M, Stauner K, Schuh A, et al. Slipped capital femoral epiphysis: long-term outcome and remodelling after in situ fixation. Hip Int 2016; 26(1): 25–30. [DOI] [PubMed] [Google Scholar]
- 31. Akiyama M, Nakashima Y, Kitano T, et al. Remodelling of femoral head-neck junction in slipped capital femoral epiphysis: a multicentre study. Int Orthop 2013; 37(12): 2331–2336. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32. O’Brien ET, Fahey JJ. Remodeling of the femoral neck after in situ pinning for slipped capital femoral epiphysis. J Bone Joint Surg Am 1977; 59(1): 62–68. [PubMed] [Google Scholar]
- 33. Örtegren J, Björklund-Sand L, Engbom M, et al. Unthreaded fixation of slipped capital femoral epiphysis leads to continued growth of the femoral neck. J Pediatr Orthop 2016; 36(5): 494–498. [DOI] [PubMed] [Google Scholar]
- 34. Sailhan F, Courvoisier A, Brunet O, et al. Continued growth of the hip after fixation of slipped capital femoral epiphysis using a single cannulated screw with a proximal threading. J Child Orthop 2011; 5(2): 83–88. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Morash K, Orlik B, El-Hawary R, et al. Femoral neck growth and remodeling with free-gliding screw fixation of slipped capital femoral epiphysis. J Pediatr Orthop 2021; 41(4): e309–e315. [DOI] [PubMed] [Google Scholar]
- 36. Leblanc E, Bellemore JM, Cheng T, et al. Biomechanical considerations in slipped capital femoral epiphysis and insights into prophylactic fixation. J Child Orthop 2017; 11(2): 120–127. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Jones JR, Paterson DC, Hillier TM, et al. Remodelling after pinning for slipped capital femoral epiphysis. J Bone Joint Surg Br 1990; 72(4): 568–573. [DOI] [PubMed] [Google Scholar]
- 38. Greco T, Zangrillo A, Biondi-Zoccai G, et al. Meta-analysis: pitfalls and hints. Heart Lung Vessel 2013; 5(4): 219–225. [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-cho-10.1177_18632521221078864 for Is the modified Dunn’s procedure superior to in situ fixation?: A systematic review and meta-analysis of comparative studies for management of moderate and severe slipped capital femoral epiphysis by Tim Cheok, Thomas Smith, Morgan Berman, Matthew Jennings, Kanishka Williams, Pradeep Mathew Poonnoose, Jaideep Rawat and Bruce Foster in Journal of Children’s Orthopaedics