Abstract
Background:
Recurrence remains the main challenge in the treatment of clubfoot. The primary goal of this study is to determine if ultrasound measurements are associated with recurrence after successful management with the Ponseti method. Furthermore, other factors are identified which can be associated with recurrence of the deformity.
Methods:
Seventy-six infants (114 idiopathic clubfeet), all treated with the Ponseti technique were reviewed. All patients had an ultrasound evaluation by the same radiologist at the beginning of the treatment. Recurrence, defined as the need to return to Ponseti casting, was recorded at a mean follow-up of 5 years. Measurements of association with recurrence were obtained for the following ultrasound measures: the medial talonavicular displacement (MTa-N), the medial malleolus to navicular distance (MM-N), the talocalcaneal angle (Ta-C), and the distal tibial physis to proximal calcaneal apophysis distance (Ti-C). Subsequently, a multivariate logistic regression analysis modeling recurrence examined patients’ characteristics, compliance, Achilles tenotomy, and ultrasound measurements.
Results:
Recurrence rate was 22% noted in 17 patients. On univariate analysis, relapse was associated with increased MTa-N (p = 0.038), decreased MM-N (p = 0.008), and decreased Ti-C (p = 0.023). On multivariate analysis, we identified the Ti-C as the only ultrasound measurement significantly associated with recurrence (p = 0.026). Other significant predictors for relapse in this study were noncompliance with orthosis (OR = 139.0 (95% CI: 8.7–2224.0), p < 10−3), and omitting percutaneous Achilles tenotomy in clubfoot treatment (OR = 23.9 (95% CI: 1.2–493.6), p = 0.041).
Conclusion:
The Ti-C sonographic measurement at the start of treatment can be a useful adjunct to help identify high-risk patients for recurrence of deformity. Non-compliance with bracing and omitting percutaneous Achilles tenotomy are also predictive factors.
Level of evidence:
Prognostic study, Level III
Keywords: Clubfoot, Ponseti, recurrence, ultrasound, ultrasound tools, diagnosis, risk-factors, prognosis
Introduction
The standard initial treatment of idiopathic congenital talipes equinovarus (clubfoot) is with a minimally invasive approach. 1 Today, the Ponseti method is the most applied technique worldwide. Regardless of the severity of the deformity, classified by the Dimeglio and Pirani complementary systems,2–4 the Ponseti method achieved excellent outcomes.5–8 It typically involves serial gentle manipulations and casting at weekly intervals often followed by percutaneous Achilles tenotomy and application of a single cast for 3 more weeks to allow the tenotomy to heal. After this active phase of treatment, the wear of a foot abduction brace is recommended for 4–5 years.6,9–12
Despite the very high success rate of the initial treatment, recurrence of the deformity remains relatively high and a challenge for the treating surgeon. As stated by Ponseti, the clinical response of the foot in infants cannot be adequately assessed by radiographs of the skeletally immature foot. 10 Moreover, radiographs were not helpful in predicting future relapse at 18 and 24 months of age. 13 In addition, the ability of clubfoot scoring systems to predict the risk of relapse is not completely settled. Specifically, while some investigators found better outcomes in patients with lower Dimeglio scores,14,15 others did not.16–18 More recently, clinical assessment tools such as foot pressure analysis19,20 and functional scores 21 were found to be useful in assessing outcomes after clubfoot treatment. However, it remains challenging to predict, early on, which patients are at risk of relapse.
Ultrasound allows adequate visualization of the cartilaginous structures in infants and several authors have introduced the use of ultrasound for the evaluation of the irregular ossification centers of the talus, calcaneus, and navicular bone in clubfeet.22–29 However, it requires a clear understanding of the sonographic anatomy of the normal infant’s foot as well as the clubfoot in order to obtain a comprehensive assessment of the abnormalities. Ultrasound may further allow a dynamic assessment of the foot and it has been suggested that it has the potential to monitor the effects of treatment following the Ponseti technique.22,25,29
In clubfoot, ultrasound evaluation targets key features of the patho-anatomy (Figures 1–3). The medial view, which is equivalent to an antero-posterior radiograph of the foot with emphasis on the medial aspect, has been referred to be by some authors the single most important plane in the assessment of clubfoot using ultrasound.23,24 It provides the quantification of the medial talo-navicular displacement (MTa-N) expressed as a percentage, the medial malleolus to navicular distance (MM-N), the talocalcaneal angle (Ta-C), as well as qualitative description of the talar morphology.23,25 Through the posterior sagittal view, the distal tibial physis to proximal calcaneal apophysis distance (Ti-C) has been also described to reflect the position of the os calcis in the heel.25,30
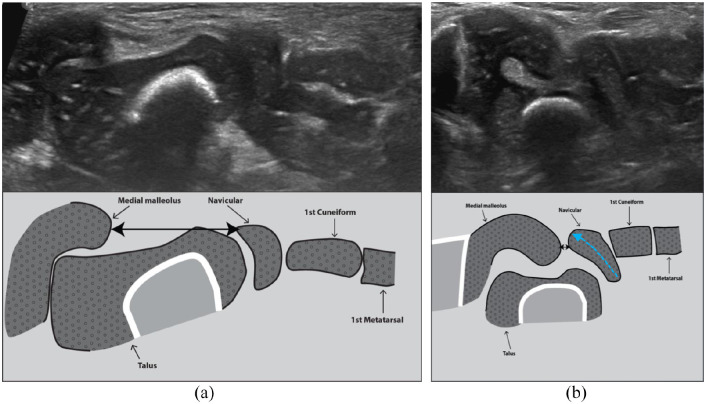
Figure 1.
(a) Medial coronal view in a normal foot. There is a normal talo-navicular alignment and normal morphology of the talus. An appropriate distance between the medial malleolus and the medial margin of the navicular (MM-N) (double black arrowhead) is also present. (b) Medial coronal view in a clubfoot. There is a medial talonavicular subluxation (MTa-N) (dotted blue arrow) and rotation of the navicular along its long axis. A decreased distance between the medial malleolus and the medial margin of the subluxated navicular (MM-N) (double black arrowhead) is also evident. Finally, the talus shows dysmorphism (foreshortened and a medial deviation of the head and neck).
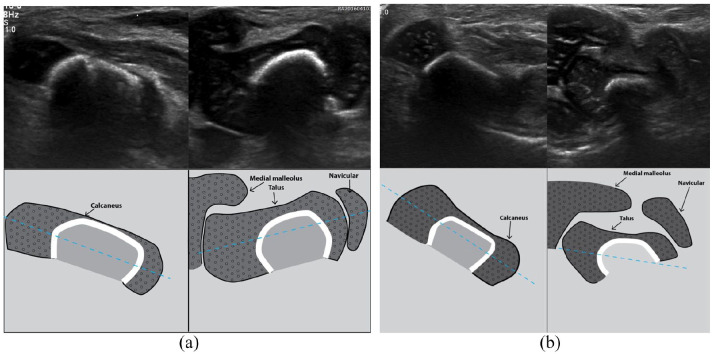
Figure 2.
(a) Medial coronal dual view in a normal foot. There is normal divergence of the talo-calcaneal angle (Ta-C) with a normal long axis of the talus oriented toward the 1st metatarsal and the calcaneus oriented toward the fifth metatarsal (blue dotted lines). (b) Medial coronal dual view in a clubfoot. Although the long axis of the calcaneus is oriented lateral to the fifth metatarsal, the talo-calcaneal divergence is decreased. This is due to the long axis of the talus being oriented proportionally further lateral than that of the calcaneus (dotted blue lines).
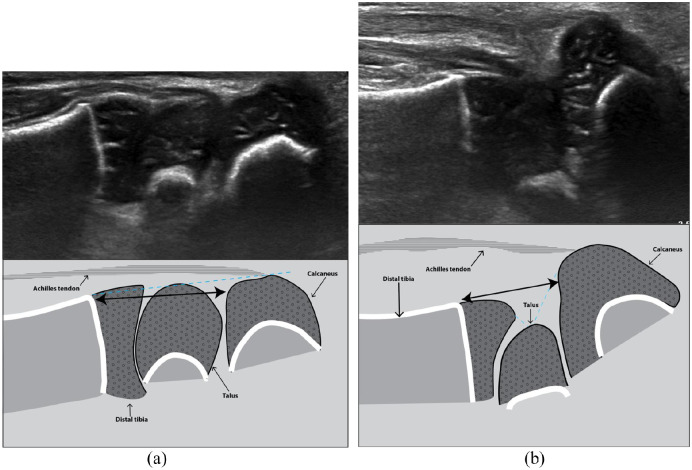
Figure 3.
(a) Posterior sagittal view in a normal foot. There is a normal alignment of the posterior aspect of the distal tibia, talus, and calcaneus (straight dotted blue line) and an appropriate distance between the distal tibial physis and the proximal calcaneal apophysis (Ti-C) (double black arrowhead). (b) Posterior sagittal view in a clubfoot. This view reflects the calcaneal position in the heel. The tibio-talo-calcaneal alignment is disrupted (broken dotted blue line) and the distance between the distal tibial physis and the proximal calcaneal apophysis (Ti-C) is decreased (double black arrowhead).
At our institution, we have been employing ultrasound to adequately describe the patho-anatomy of the clubfoot. We believe that ultrasound could add useful information at the outset of treatment and guide our treatment strategy in resistant clubfeet and/or those showing recurrence.
The purpose of this study was to identify which ultrasound measurements, made early, can be associated with the risk of recurrence in idiopathic clubfoot. Secondarily, we evaluated how other factors can influence the risk of recurrence. These factors included demographic data, compliance with foot abduction bracing and the performance of an Achilles tenotomy.
Materials and methods
Patient selection
A retrospective case-control study was performed in a single site between July 2003 and August 2009. It comprised 76 consecutive infants with 114 feet treated by three pediatric orthopedic surgeons in a pediatric university hospital center. The study has been approved by the institutional review board. The inclusion criteria were (1) idiopathic clubfoot, (2) no previous treatment of the clubfoot, (3) conservative treatment with the Ponseti method, (4) availability of ultrasound before or in the 2 weeks following the start of Ponseti casting, and (5) a minimum clinical follow-up of 3 years. A percutaneous heel-cord tenotomy under local anesthesia in the outpatient clinic was considered part of the management. Tenotomy was performed when 15° of dorsiflexion has not been obtained with serial manipulation and casting. Following the tenotomy, our protocol calls for two additional casts of 2-week duration each, to allow for tendon healing before moving to the foot abduction brace (Figure 4). Bracing was recommended full time until the age of 6 months, then for 18 hours a day until age 1, followed by nighttime wear until a minimum of age of 4 years. Compliance was a self-reported measure and defined as adherence to the prescribed use of the foot abduction brace. If care-givers were noncompliant during the 3-year follow-up, it was counted as noncompliant in this study.
Figure 4.
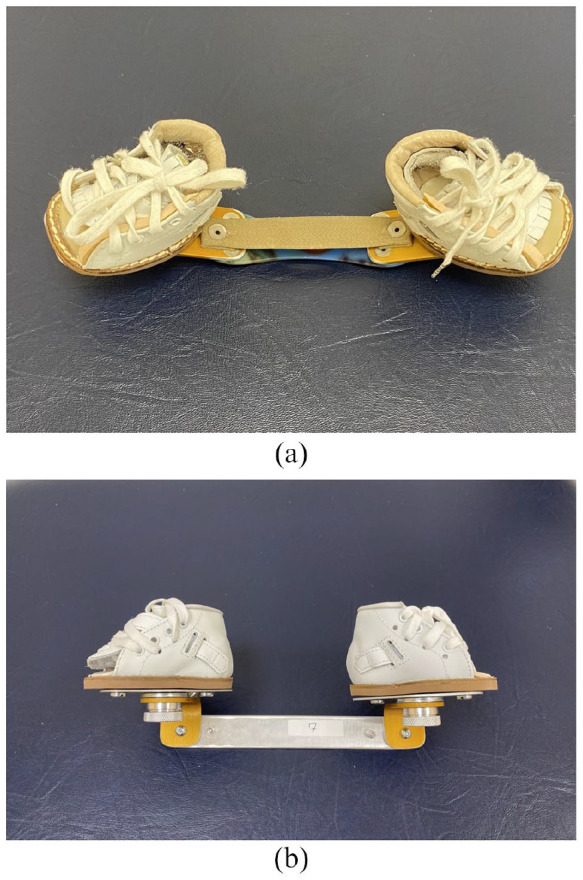
(a) The foot abduction brace used initially. Notice the more rigid non-articulated construct in this brace. (b) Articulated foot abduction brace used after an initial period of 6 months with the non-articulated brace shown in Figure 4(a).
The patients were followed up for a mean of 5.2 ± 1.2 years (range = 3.0–9.2 years). Medical charts were reviewed for patient characteristics, recurrence, compliance, performance or not of Achilles tenotomy, and clubfoot ultrasound images and reports. Recurrence was defined as the reappearance of any component of the deformity requiring return to the Ponseti method.
Ultrasound examination of the clubfoot
A dedicated foot ultrasound was done routinely for all patients before or within the first 2 weeks of starting the Ponseti casting. Twenty-one patients had an ultrasound examination done prior to any treatment, 24 patients had it after the first cast, and 31 patients had it after the second cast. The reason for delaying ultrasound examination was due to the inability of some parents to travel to the hospital at the specified date and/or the unavailability of the musculoskeletal radiologist. All ultrasounds in this study were performed systematically by a single pediatric musculoskeletal radiologist with extensive expertise in ultrasound evaluation of clubfoot.
The examination is performed in a relaxed and recently fed infant. The infant is placed in the supine position. The foot is stabilized with one hand and the examination is performed in the spontaneous position of the foot (Figure 5). A high-frequency linear probe (5–13 MHz with a footprint of 30–50 mm) was optimal to assess the foot in this age group. The standardized examination protocol at our institution used systematically a medial coronal view, a medial coronal dual view, a dorsal sagittal view, a lateral coronal view, and posterior sagittal view as described by Miron and Grimard. 25 All measurements were taken from the cartilaginous borders of the bones as visualized by ultrasound.
Figure 5.
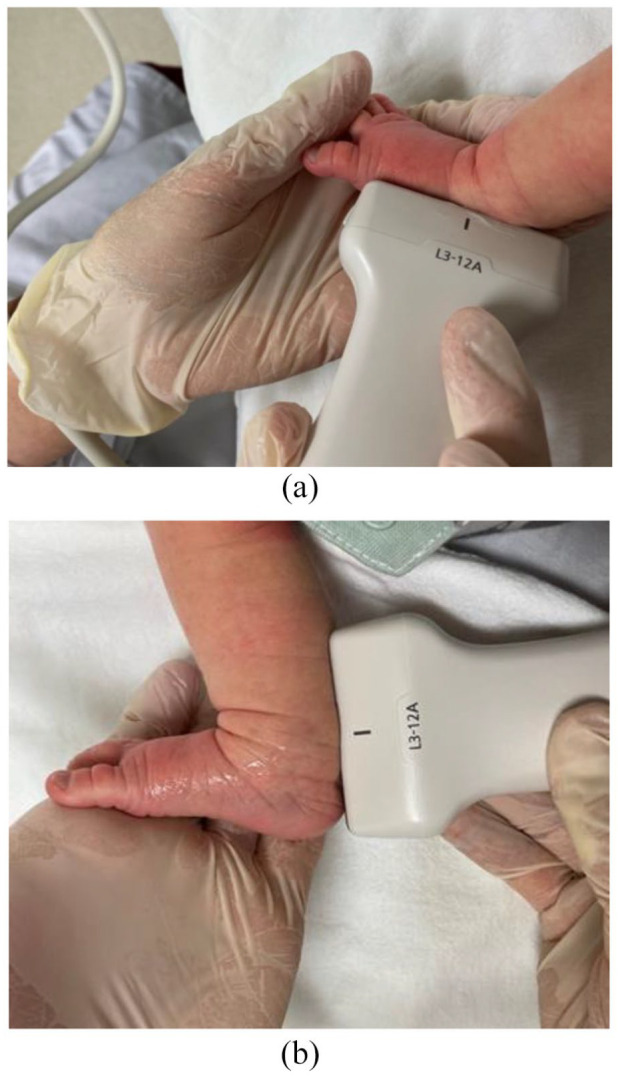
(a) Medial coronal view in a normal foot. Ultrasound probe position to obtain the medial talo-navicular displacement (MTa-N) expressed as a percentage, the medial malleolus to navicular distance (MM-N), as well as a qualitative description of the talar morphology. This probe position is also used to obtain the medial coronal dual view on which the talo-calcaneal angle (Ta-C) is assessed. (b) Posterior sagittal view in a normal foot. Ultrasound probe position to obtain the distal tibial physis to proximal calcaneal apophysis distance (Ti-C).
Four quantitative measurements were systematically obtained for all patients:
MTa-N (%): The medial talo-navicular displacement or subluxation measured on the medial coronal view (by dividing the subluxated part of the navicular bone by its long axis distance) and expressed as a percentage (Figure 1).
MM-N (mm): The medial malleolus to navicular distance measured on the medial coronal view (Figure 1).
Ta-C (°): The talo-calcaneal angle measured on the medial coronal dual view (Figure 2).
Ti-C (mm): The distal tibial physis to proximal calcaneal apophysis distance measured on the posterior sagittal view (Figure 3).
In patients with bilateral clubfeet, Gray et al. 31 found that baseline severity, response to treatment, and recurrence outcomes, among other variables, were highly correlated in the right and left feet of each patient. Accordingly, results in two limbs of the same patient do not represent independent observations and should not be analyzed as independent data points. Therefore, in our study, when analyzing ultrasound measurements for bilateral presentations, we considered the mean of both feet for each variable.
Statistical analysis
Descriptive statistics were performed for the whole cohort. The parameters were then examined for normality, and because of the large variations, direct comparisons using non-parametric Mann–Whitney U tests were performed to analyze the comparative groups: the recurrence (R) and nonrecurrence (NR) groups. To identify reliable predictors, a multivariate logistic regression analysis modeling recurrence was then conducted. For categorical characteristics, reference categories were indicated with an odds ratio of 1.0. Statistical analysis was executed using SPSS 28 software. A level of significance of 0.05 was used for all tests.
Results
Seventy-six patients with 114 idiopathic clubfeet were treated. The cohort comprised 19 female and 57 male patients. Forty patients had unilateral and 36 had bilateral involvement. Treatment was initiated at our institution at a mean age of 20 ± 32 days (range = 1–216 days). Treatment begun before 28 days of age in 84% of patients. Only one patient had treatment initiated at more than 6 months of age. This patient had successful treatment despite a delayed presentation. On average, six casts were applied to obtain correction (range = 3–10 casts). In this study, the average age at tenotomy was 55 ± 31 days. A percutaneous tenotomy was performed in 79% (60/76) of patients to achieve adequate ankle dorsiflexion after the active phase of manipulation and casting. Initial correction was obtained in all 114 feet with the Ponseti method. The mean follow-up was 5.2 ± 1.2 years (range = 3.0–9.2 years). There was no patient lost to follow-up in this study. Clubfoot recurrence was noted in 17 patients and comprised 22% of all patients (17/76).
Ultrasound measurements
The results of univariate analysis are presented in Table 1. Through the medial coronal view, the MTa-N percent displacement was first measured and found to be significantly higher in the R group compared to the NR group (49% ± 34 vs 30% ± 21, respectively, p = 0.038). The MM-N distance was measured and found to be significantly shorter in R group compared to the NR group (3.1 mm ± 2.5 vs 5.3 mm ± 3.0, respectively, p = 0.008). Through the medial coronal dual view, the Ta-C angle was measured. No statistical significance was found for this parameter between both groups (27°± 14 vs 31°± 12, respectively, p = 0.281). Finally, through the posterior sagittal view, the Ti-C distance was found to be significantly shorter in the R group compared to the NR group (12.5 mm ± 2.7 vs 14.2 mm ± 2.8, respectively, p = 0.023).
Table 1.
Univariate analysis of ultrasound measurements with respect to clubfoot recurrence at a mean follow-up of 5 years after Ponseti treatment.
| Group | N = 76 (patients) | Medial Talonavicular displacement (%) | Medial malleolus to navicular distance (mm) | Talonavicular angle (°) | Distal tibial physis to proximal calcaneal apophysis distance (mm) |
|---|---|---|---|---|---|
| Recurrence | 17 | 49 ± 34 | 3.1 ± 2.5 | 27 ± 14 | 12.5 ± 2.7 |
| No recurrence | 59 | 30 ± 21 | 5.3 ± 3.0 | 31 ± 12 | 14.2 ± 2.8 |
| p value † | 0.038* | 0.008* | 0.281 | 0.023* | |
p values are reported for significance of association using Mann–Whitney U tests.
Statistical significance < 0.05.
Predictive factors
The results of the multivariate logistic regression analysis modeling recurrence are reported in Table 2. No significant relationship was detected, for the demographic variables of age, gender, and laterality. Among ultrasound measurements, only the Ti-C distance was found to be a risk factor for clubfoot recurrence (p = 0.026). The other ultrasound measurements, MTa-N, Ta-C, and MM-N did not show statistical significance. Noncompliance with the foot abduction brace was the most significant risk factor for recurrence and was reported to be 76% (13/17) in the R group compared to only 8% (5/59) in the NR group. In other terms, families who did not comply with bracing had 139 times more risk of clubfeet recurrence in their children than compliant families (OR = 139.0 (95% CI: 8.7–2224.0, p < 10−3)). Interestingly, when present, family noncompliance was noted early on after the first 3 months of bracing in half the time. The overall rate of Achilles tenotomy in this study was 79% (60/76). Specifically, 59% (10/17) in R group compared to 85% (50/59) in the NR group. Not including a percutaneous heel-cord tenotomy in the initial management of clubfoot hence appeared to increase recurrence. In fact, the risk that a clubfoot will relapse is increased 23.9 times in non-tenotomized clubfeet compared with tenotomized ones (OR = 23.9 (95% CI: 1.2–493.6); p = 0.041) (Table 2).
Table 2.
Multivariate analysis from 76 patients modeling clubfoot recurrence at a mean follow-up of 5 years after Ponseti treatment.
| Variables | Recurrence (N = 17 patients) | No recurrence (N = 59 patients) | Odds ratio [95% confidence interval] | p-value † | |
|---|---|---|---|---|---|
| Age at first cast (days) | 16 ± 24 | 19 ± 30 | 0.39 | ||
| Gender | Male | 13 (76%) | 43 (73%) | 2.7 [0.2–33.7] | 0.442 |
| Female | 4 (24%) | 16 (27%) | 1.0 | ||
| Laterality | Unilateral | 9 (53%) | 31 (53%) | 1.7 [0.2–19.2] | 0.658 |
| Bilateral | 8 (47%) | 28 (47%) | 1.0 | ||
| Compliance | No | 13 (76%) | 5 (8%) | 139.0 [8.7–2224.0] | <10−3* |
| Yes | 4 (26%) | 54 (92%) | 1.0 | ||
| Percutaneous Achilles tenotomy | No | 7 (41%) | 9 (15%) | 23.9 [1.2–493.6] | 0.041* |
| Yes | 10 (59%) | 50 (85%) | 1.0 | ||
| Medial talonavicular displacement (%) | 49 ± 34 | 30 ± 21 | 0.675 | ||
| Medial malleolus to navicular distance (mm) | 3.1 ± 2.5 | 5.3 ± 3.0 | 0.767 | ||
| Talocalcaneal angle (°) | 27 ± 14 | 31 ± 12 | 0.534 | ||
| Distal tibial physis to proximal calcaneal apophysis distance (mm) | 12.5 ± 2.7 | 14.2 ± 2.8 | 0.026* | ||
Continuous variables are expressed as the mean ± standard deviation.
p values are reported for multivariate logistic regression analysis modeling recurrence.
Statistically significant.
Discussion
Ultrasound can view the cartilaginous ossification centers of the tarsal bones in great detail. Therefore, quantifying key features in the patho-anatomy of the infant with clubfoot is more accurately assessed with ultrasound than by clinical and plain X-rays alone. With ultrasound, the long axes of the talus and calcaneus that subtend the Ta-C angle can be easily determined. In contrast, on plain radiographs, it is difficult to adequately measure this angle because the talus and calcaneus have a round aspect as they are only partially ossified at the initial assessment. In this study, the sonographic Ta-C was not associated with recurrence and hence not helpful. Our results were in line with findings by Dobbs et al analyzing this angle by radiography. 16
The initial MTa-N displacement and the MM-N distance differed between the R and NR group although none had a predictive effect for recurrence on multivariate analysis. Since 54 patients had the ultrasound measurement obtained after 1 or 2 casts, the MTa-N and the MM-N may have been partially corrected already and thus did not correlate with relapse. Future studies analyzing ultrasound measurements obtained strictly prior to any treatment could define more accurately the prognostic value of these variables.
The results of this study show that the Ti-C distance, when measured early using ultrasound, is associated with a risk of recurrence. It is suggested therefore that the Ti-C distance can be employed on repeated ultrasound evaluations as a guide for treatment. We hypothesize that a Ti-C distance below a certain threshold will maintain the hindfoot in equinus leading to a loss of ankle dorsiflexion and over time may predispose for the need to return to casting. A prospective study employing serial ultrasounds may help to determine these threshold values and further guide treatment.
In addition, the results of this study suggest that a heel-cord tenotomy may be protective against relapse. No complications were observed in the 87 percutaneous heel-cord tenotomies performed under local anesthesia in an outpatient setting. Despite the safety and simplicity of the procedure, care must be taken to perform the procedure adequately and at the best time as described by Ponseti.9–12 An early or late tenotomy in the course of the treatment could lead to a “rocker-bottom” deformity or a relapse. 10
Demographic features such as age, gender, and laterality had no impact on recurrence in this study similar to other authors’ findings.16,17
Finally, noncompliance with the use of the foot abduction brace remains the strongest predictor for recurrent deformity at long-term follow-up as demonstrated by the 76% rate in the R group. Compliance was assessed by parents’ verbal responses regarding the use of the foot abduction brace. We realize that assessment of compliance with treatment based on verbal responses only may introduce a reporting bias in both groups. Nevertheless, our findings are in agreement with previous studies that established the importance of compliance in clubfoot management.16,17
In addition, there are a number of other limitations to this preliminary study. First, this is a retrospective study that can introduce reporting biases. Second, the differences in the ultrasound parameters of MM-N and Ti-C distances between the recurrence and non-recurrence groups are 2.2 and 1.7 mm, respectively. Although the differences are statistically significant, they may not be clinically significant. In addition, the authors are not aware of any study that evaluates the margin of error in the measurement of these parameters. Intra- and inter-observer studies could determine if these findings can be generalizable to other clinicians. Third, we recognize that not all ultrasounds were performed before the onset of treatment. The two casts done before the first ultrasound in some of the clubfeet may have partially or fully corrected some of the components of the clubfoot deformity. This partial correction can potentially make it difficult to accurately determine whether some of the ultrasound measurements correlated with relapse. However, the fact that the Ti-C distance stood out despite the opportunity of having some feet treated for 2 weeks shows that it is, in our opinion, a good measure to employ for the identification of clubfeet that are at risk for recurrence.
In the future, prospective studies of clubfeet investigated since birth by repeated ultrasound and clinical assessments may help further define the role of ultrasound in the prediction of clubfoot recurrence in the setting of the Ponseti technique. In our experience, such routine addition of ultrasound examinations, at the start of treatment and recently adding another follow-up examination just before bracing, seems to add only a reasonable amount of time and cost to the management of clubfoot. Threshold values for these ultrasound parameters can then be determined on initial and follow-up examinations, and subsequently be more useful to guide the progression of treatment.
Conclusion
Ultrasound can be employed as a modality for the evaluation of the patho-anatomy of clubfeet in infants. It can be a useful adjunct to identify high-risk patients for recurrence in the treatment of clubfoot following the Ponseti method. In this study, we found that the Ti-C distance was a useful sonographic measurement that can predict later recurrence. Therefore, a diminished Ti-C on initial ultrasound examination should prompt the surgeon to strongly consider a percutaneous Achilles tenotomy and a closer follow-up to help with bracing compliance.
Acknowledgments
The authors thank Philippe Labelle for his expertise and assistance in the drawing of the figures. The authors also thank the photography service of the CHU Sainte-Justine for the acquisition of the pictures with the patients. Finally, the authors acknowledge Dr Karim Z Masrouha from NYU Langone Medical Center for the invaluable input and help he provided in the redaction of this manuscript.
Footnotes
Author contributions: I.N. (EPOS member) made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published; agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. M.-C.M. made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published; agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. G.G. made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published; agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. A.A.Z. made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published; agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved. P.(P.) G. made substantial contributions to the conception or design of the work; or the acquisition, analysis, or interpretation of data for the work; drafting the work or revising it critically for important intellectual content; final approval of the version to be published; agreement to be accountable for all aspects of the work in ensuring that questions related to the accuracy or integrity of any part of the work are appropriately investigated and resolved.
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
References
- 1. Morcuende JA, Dolan LA, Dietz FR, et al. Radical reduction in the rate of extensive corrective surgery for clubfoot using the Ponseti method. Pediatrics 2004; 113(2): 376–380. [DOI] [PubMed] [Google Scholar]
- 2. Pirani SHD, Sekeramayi F. A reliable and valid method of assessing the amount of deformity in the congenital clubfoot deformity. J Bone Joint Surg 2008; 90: 53. [Google Scholar]
- 3. Dimeglio A, Bensahel H, Souchet P, et al. Classification of clubfoot. J Pediatr Orthop B 1995; 4(2): 129–136. [DOI] [PubMed] [Google Scholar]
- 4. Cosma D, Vasilescu DE. A clinical evaluation of the Pirani and Dimeglio idiopathic clubfoot classifications. J Foot Ankle Surg 2015; 54(4): 582–585. [DOI] [PubMed] [Google Scholar]
- 5. Zionts LE, Ebramzadeh E, Morgan RD, et al. Sixty years on: Ponseti method for clubfoot treatment produces high satisfaction despite inherent tendency to relapse. J Bone Joint Surg-Am 2018; 100(9): 721–728. [DOI] [PubMed] [Google Scholar]
- 6. Ponseti IV, Smoley EN. The classic: congenital club foot—the results of treatment. Clin Orthop Relat Res 2009; 467(5): 1133–1145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Cooper DM, Dietz FR. Treatment of idiopathic clubfoot: a thirty-year follow-up note. J Bone Joint Surg Am 1995; 77(10): 1477–1489. [DOI] [PubMed] [Google Scholar]
- 8. Laaveg SJ, Ponseti IV. Long-term results of treatment of congenital club foot. J Bone Joint Surg Am 1980; 62(1): 23–31. [PubMed] [Google Scholar]
- 9. Ponseti IV, Campos J. Observations on pathogenesis and treatment of congenital clubfoot. Clin Orthop Relat Res 1972; 84: 50–60. [DOI] [PubMed] [Google Scholar]
- 10. Ponseti IV. Congenital clubfoot: fundamentals of treatment. New York: Oxford University Press, 1996. [Google Scholar]
- 11. Ponseti IV. Clubfoot management. J Pediatr Orthop 2000; 20(6): 699–700. [DOI] [PubMed] [Google Scholar]
- 12. Staheli L. Clubfoot: Ponseti management. Revised ed. Seattle, WA: Global HELP Organization, 2009. [Google Scholar]
- 13. Richards BS, Faulks S, Razi O, et al. Nonoperatively corrected clubfoot at age 2 years: radiographs are not helpful in predicting future relapse. J Bone Joint Surg Am 2017; 99(2): 155–160. [DOI] [PubMed] [Google Scholar]
- 14. Zhang W, Richards BS, Faulks ST, et al. Initial severity rating of idiopathic clubfeet is an outcome predictor at age two years. J Pediatr Orthop B 2012; 21(1): 16–19. [DOI] [PubMed] [Google Scholar]
- 15. Sangiorgio SN, Ebramzadeh E, Morgan RD, et al. The timing and relevance of relapsed deformity in patients with idiopathic clubfoot. J Am Acad Orthop Surg 2017; 25(7): 536–545. [DOI] [PubMed] [Google Scholar]
- 16. Dobbs MB, Rudzki JR, Purcell DB, et al. Factors predictive of outcome after use of the Ponseti method for the treatment of idiopathic clubfeet. J Bone Joint Surg Am 2004; 86(1): 22–27. [DOI] [PubMed] [Google Scholar]
- 17. Zhao D, Li H, Zhao L, et al. Prognosticating factors of relapse in clubfoot management by Ponseti method. J Pediatr Orthop 2018; 38(10): 514–520. [DOI] [PubMed] [Google Scholar]
- 18. Jochymek J, Peterkova T. Are scoring systems useful for predicting results of treatment for clubfoot using the Ponseti method. Acta Ortop Bras 2019; 27(1): 8–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Herd F, Ramanathan AK, Cochrane LA, et al. Foot pressure in clubfoot: the development of an objective assessment tool. Foot 2008; 18(2): 99–105. [DOI] [PubMed] [Google Scholar]
- 20. Sinclair MF, Bosch K, Rosenbaum D, et al. Pedobarographic analysis following Ponseti treatment for congenital clubfoot. Clin Orthop Relat Res 2009; 467(5): 1223–1230. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Bohm S, Sinclair MF. The PBS Score: a clinical assessment tool for the ambulatory and recurrent clubfoot. J Child Orthop 2019; 13(3): 282–292. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Aurell Y, Andriesse H, Johansson A, et al. Ultrasound assessment of early clubfoot treatment: a comparison of the Ponseti method and a modified Copenhagen method. J Pediatr Orthop B 2005; 14(5): 347–357. [DOI] [PubMed] [Google Scholar]
- 23. Aurell Y, Johansson A, Hansson G, et al. Ultrasound anatomy in the neonatal clubfoot. Eur Radiol 2002; 12(10): 2509–2517. [DOI] [PubMed] [Google Scholar]
- 24. Chami M1DA, Daoud A, Maestro M, et al. Ultrasound contribution in the analysis of the newborn and infant normal and clubfoot: a preliminary study. Pediatr Radiol 1996; 26(4): 298–302. [DOI] [PubMed] [Google Scholar]
- 25. Miron MC, Grimard G. Ultrasound evaluation of foot deformities in infants. Pediatr Radiol 2016; 46(2): 193–209; quiz 190. [DOI] [PubMed] [Google Scholar]
- 26. Tolat V, Boothroyd A, Carty H, et al. Ultrasound: a helpful guide in the treatment of congenital talipes equinovarus. J Pediatr Orthop B 1995; 4(1): 65–70. [PubMed] [Google Scholar]
- 27. Hamel J, Becker W. Sonographic assessment of clubfoot deformity in young children. J Pediatr Orthop B 1996; 5(4): 279–286. [DOI] [PubMed] [Google Scholar]
- 28. Shiels WE, 2nd, Coley BD, Kean J, et al. Focused dynamic sonographic examination of the congenital clubfoot. Pediatr Radiol 2007; 37(11): 1118–1124. [DOI] [PubMed] [Google Scholar]
- 29. Kuhns LR, Koujok K, Hall JM, et al. Ultrasound of the navicular during the simulated Ponseti maneuver. J Pediatr Orthop 2003; 23(2): 243–245. [PubMed] [Google Scholar]
- 30. Chawla S, Gupta M, Pandey V, et al. Clinico-sonographical evaluation of idiopathic clubfoot and its correction by Ponseti method: a prospective study. Foot 2017; 33: 7–13. [DOI] [PubMed] [Google Scholar]
- 31. Gray K, Gibbons P, Little D, et al. Bilateral clubfeet are highly correlated: a cautionary tale for researchers. Clin Orthop Relat Res 2014; 472(11): 3517–3522. [DOI] [PMC free article] [PubMed] [Google Scholar]