Abstract
This paper provides an overview of some of the most memorable sessions that were (co)organised by the Allied Respiratory Professionals Assembly during the 2021 European Respiratory Society International Congress, which was held online for the second consecutive year due to the COVID-19 pandemic. Early Career Members from Assembly 9 summarised the content of the sessions (three oral communication sessions, two symposia and one Expert View) with the support of the chairs from the four Assembly groups: Respiratory Function Technologists and Scientists (Group 9.01); Physiotherapists (Group 9.02); Nurses (Group 9.03); and Psychologists and Behavioural Scientists (Group 9.04). The sessions covered the following topics: impact of COVID-19 on lung function and healthcare services, and the importance of quality assurance and technology in lung function assessment; diagnosis and management of sarcopenia in patients with chronic respiratory disease; maintenance of the effects of pulmonary rehabilitation; solutions outside the hospital for the management of patients with COVID-19 in need of health care; the nursing perspective during the COVID-19 pandemic; and psychological and behavioural issues in respiratory care. This highlights article provides valuable insight into the latest scientific data and emerging areas affecting clinical practice of allied respiratory professionals.
Short abstract
This article provides an overview of outstanding sessions that were (co)organised by @ERS_Assembly9 during #ERSCongress 2021 https://bit.ly/332uZWy
Introduction
The virtual 2021 European Respiratory Society (ERS) International Congress provided the allied respiratory professionals with a wide range of outstanding sessions (co)organised by Assembly 9 including Symposia, Expert Views, Skills Labs, and 189 abstracts spread over oral communication and e-poster sessions.
In this article, the four groups of Assembly 9 highlight some of the most memorable sessions of the ERS Congress, targeting delegates who were present in the virtual sessions as well as those unable to attend. Early Career Members of the assembly (including respiratory function technologists and scientists, physiotherapists, nurses, and psychologists and behavioural scientists) were invited to summarise the latest scientific and clinical insights presented in the following sessions: three oral presentation sessions on the impact of COVID-19 on lung function and health services and quality assurance in lung function assessment, the nursing perspective during the COVID-19 pandemic, and psychological and behavioural issues in respiratory care; two symposia on the diagnosis and management of sarcopenia in patients with chronic respiratory disease and the maintenance of the pulmonary rehabilitation effects; and an Expert View on the implementation of solutions outside the hospital for the management of patients with COVID-19 in need of healthcare. The next pages provide a summary of these sessions, along with important take-home messages, hoping to inspire readers to keep up to date in their areas of interest.
Group 9.01: Respiratory Function Technologists and Scientists
Oral presentation: Impact of COVID-19, quality assurance and technology on pulmonary function
This oral presentation session (session number 295) included communications on the impact of COVID-19 on lung function and healthcare services, and on the importance of quality assurance and technology to assess lung function.
Ventilation heterogeneity after COVID-19 (O. Savushkina, Russia)
Savushkina et al. [1] presented findings from a cross-sectional study investigating the influence of COVID-19 on ventilation heterogeneity. The study used the multiple-breath nitrogen washout test in post-COVID subjects with no chronic respiratory disease and examined the relationship between the lung clearance index (LCI) and pulmonary function parameters. The study demonstrated that ventilation heterogeneity was detected in 85% cases 63 days after the onset of COVID-19. Additionally, there were significant correlations between LCI, pulmonary function and impulse oscillometry (IOS) parameters.
Evaluation of patient attendance to respiratory physiology in the midst of the COVID-19 pandemic (S. Yearsley, UK)
S. Yearsley presented, on behalf of Hurst et al. [2], retrospective collated attendance data from two respiratory physiology laboratories (north midlands, UK) during the COVID-19 pandemic (1 January 2019–31 December 2020). The data demonstrated that the “did not attend” (DNA) rate of 8.1% exceeded the 5.2% DNA rate from the Hospital Episode Statistics rate for outpatient appointments (April–October 2020). This equates to an approximate cost to the National Health Service of GBP 261 171 [3]. Post-service resumption DNA rates increased (7.8% versus 9.2%) but it was also observed that, with targeted communication, the DNA rate decreased 2.7-fold, which demonstrates the importance of verbal communication prior to appointments to improve outpatient attendance during the pandemic.
Implementation of the 2017 ERS methacholine challenge standard (I. Steenbruggen, The Netherlands)
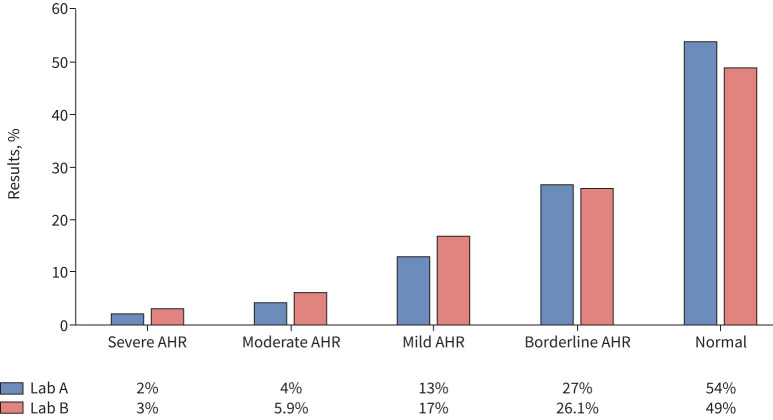
Steenbruggen et al. [4] presented their study determining the percentage of patients with positive and negative methacholine challenge tests (MCTs). The classification category for the positive tests additionally determined if there was a difference in provocative dose causing a 20% fall in forced expiratory volume in 1 s (PD20) between males and females. In total, 253 results from two laboratories were retrospectively reviewed. The results demonstrated the utility of MCT in either confirming or excluding airway hyperresponsiveness (AHR), with results presented in figure 1, showing the AHR classification according to the 2017 ERS methacholine challenge standard [5]. Findings from this study also highlighted that men achieved significantly higher PD20 than women.
FIGURE 1.
Classification of airway hyperresponsiveness (AHR) according to the European Respiratory Society 2017 technical standard [5]. Lab: laboratory. Reproduced and modified from [4] with permission from the authors.
Evaluation of the Global Lung function Initiative reference values for spirometry and diffusion capacity (K. De Soomer, Belgium)
De Soomer et al. [6] presented results from a retrospective analysis evaluating the quality of the Global Lung Initiative (GLI) reference values [7, 8] in an Antwerp population with no known cardiac and respiratory disease history. Overall, it was demonstrated that the GLI reference values suitably predicted lung function. However, it was shown that the values of the forced expiratory volume in 1 s (FEV1)/forced vital capacity (FVC) ratio were lower than predicted in tall subjects, as were diffusing capacity of the lung for carbon monoxide values in older female populations. These findings could result in an increase in suspected prevalence of obstructive and diffusion disorders in these groups.
Pulmonary airway resistance variability in normal biologic quality control subjects among pulmonary function testing systems across British Columbia (C.D. Mottram, USA)
Mottram et al. [9] presented a study that investigated the variability of the panting and tidal breathing techniques when measuring airway resistance (Raw) and/or specific conductance (sGaw) in biological quality control (BioQC) subjects amongst different pulmonary testing systems across British Columbia, Canada. Raw and sGaw data were analysed from 168 sessions over a 6-month period submitted to British Columbia's Diagnostic Accreditation Programme. Analysis of the data suggested that, in BioQC subjects, a coefficient of variation (CV) ≤10% would be an acceptable range for Raw and sGaw measurements. Findings also suggested that the panting technique showed the least degree of CV variability. This knowledge may be useful for laboratories implementing BioQC checks.
Do bacterial/viral filters impact quality assurance verification of ultrasonic spirometers? (L. Robertson, UK)
Robertson et al. [10] presented results from a quality control study determining whether application of bacterial/viral filters (BVFs) impacted expiratory and inspiratory volume verification accuracy of Easy-on PC ultrasonic spirometers at different flow rates. Their findings highlighted that the proximal position, which is the usual site for BVF placement, significantly impacted the accuracy of expiratory volume verification at low flow rates, whereas with the BVF placed distally, the expiratory volume verification was achieved at all flow rates but the inspiratory volume verification was not. From this work, it can be recommended that, if one wishes to apply a BVF on the Easy-On ultrasonic spirometer to reduce cross infection risk, it should be placed distally only if expiratory volumes are of clinical importance and not inspiratory volumes.
Breath detection algorithms affect lung function outcomes (M. Oestreich, Switzerland)
Oestreich et al. [11] presented a study about breath detection algorithms in children, as breath detection is essential in calculating outcomes in multiple-breath washout (MBW). This is especially important in children, in whom irregular breathing is frequent. The authors produced a novel algorithm for breath detection, and compared it to algorithms used in MBW software from trials collected in children and adolescents. The results demonstrated that in trials with normal tidal breathing, there was no difference in outcomes between the software and the algorithm. However, greater challenges in breath detection were found in young children, as in 14% of trials in children aged 5–10 years, the number of breaths detected differed by ≥10% and the LCI differed up to 40.5% (mean difference 3.6%). It was concluded that, as the MBW technique relies on cumulative analysis of all washout breaths, rejection of breaths should be limited. Findings demonstrated that the new breath detection algorithm, based on reversal and presence of carbon dioxide, could be an alternative algorithm to those currently used.
Real-world application of spirometry quality control deep-learning algorithm (S. Stanojevic, Canada)
Stanojevic et al. [12] described the results of a study that validated a recently developed spirometry quality control software based on a deep-learning algorithm [13]. Spirometry data were collected from a pre-school population and from a healthy adult population. Data were evaluated by the quality control software using 2005 American Thoracic Society/ERS standards [14]. Manoeuvre and quality acceptability were compared with trained operators at the time of testing. Overall, findings showed that the quality control software was in agreement with the technicians’ review in the different populations. This study provides evidence for the clinical use of the software for reviewing quality of spirometry results, saving clinicians’ time.
Use of artificial intelligence for improving quality control of oscillometry (C. Veneroni, Italy)
Veneroni et al. [15] presented a study about the use of machine learning methods to reliably classify artefact free breaths in IOS. This artefact detection is fundamental for situations when testing cannot be supervised. In total, 932 measurements were collected from 134 patients using a multifrequency stimulus at 5, 11 and 19 Hz following the ERS standards [16]. The results demonstrated that the feature selection performed by a wrapper method combined with an Adaboost tree model provided the best performance in classifying artefacts. Additionally, automatically classified tests differed from the manually classified ones by >0.5 cmH2O·s·L−1 in <5% of measurements. The authors concluded that supervised machine learning techniques can reliably detect IOS measurements and this would be of value in home monitoring settings, where tests cannot be supervised.
Effects of respiratory muscle training on quality of life, physical function, and psychological state in post-COVID syndrome (T. Del Corral Nuñez-Flores, Spain)
Del Corral Nuñez-Flores et al. [17] presented late-breaking work from a double-blind randomised controlled trial involving post-COVID-19 subjects, where the effects of high-intensity home-based respiratory muscle training over 8 weeks were studied on quality of life, physical and pulmonary function, and psychological and cognitive state. The results showed that subjects in the experimental group improved quality of life in regard to breathlessness, muscle fatigue, respiratory muscle strength, cardiorespiratory endurance, anxiety and depression levels, post-traumatic stress disorder (PTSD), and cognition function when compared to the control group, but no between-group differences were observed in pulmonary function and peripheral muscle strength. This study demonstrates the benefits of home-based respiratory muscle training on quality of life and functional characteristics in people with post-COVID-19 syndrome, where symptoms of breathlessness and fatigue are common.
Take-home messages
To reduce cross-infection risk when using the Easy-on ultrasonic spirometer, the BVF should be applied distally.
Recently developed spirometry quality control software showed overall good agreement with technicians’ review and, therefore, software could be used clinically to review spirometry data quality and save clinicians’ time.
A home-based respiratory muscle training programme can improve quality of life, symptoms, and physical, cognitive and psychological function of people with post-COVID-19 syndrome in the short term.
Group 9.02: Physiotherapists
Symposium: Sarcopenia in chronic respiratory disease: new definitions, assessment and treatment options
In this symposium (session 210), four expert speakers provided an update on the latest knowledge on sarcopenia definition and diagnosis, and its assessment and management, in the context of chronic respiratory diseases.
Update on recent definitions and diagnosis of sarcopenia (G. Bahat, Turkey)
G. Bahat started by explaining that sarcopenia was first clinically defined in 1998 solely by the presence of low muscle mass [18]. It was only in 2010 that a change in the paradigm happened, with the publication of several consensus reports integrating decreased muscle function into the definition of sarcopenia [19–22]. Since the age-related decline in muscle strength begins before the decline in muscle mass and the former is also 2–5 times faster [23], it is possible that by only including the presence of low muscle mass in the definition of sarcopenia, many cases of older adults with reduced muscle strength would be overlooked. Therefore, low muscle strength has become the main characteristic of sarcopenia in the current consensus definitions (table 1) [24–26]. G. Bahat concluded the talk by emphasising that future studies should include muscle strength in their sarcopenia definition.
TABLE 1.
Current definitions of sarcopenia
| EWGSOP2 [ 24 ] | SCWD [ 25 ] | SDOC [ 26 ] | |
| Probable sarcopenia | Low muscle strength | ||
| Sarcopenia | Low muscle strength + low muscle quantity/quality | Low muscle strength + low muscle quantity/quality | Low muscle strength + low physical performance |
| Severe sarcopenia | Low muscle strength + low muscle quantity/quality + low physical performance | ||
| Primary sarcopenia | Age-related, with no other evident specific cause | Age-related, with no other evident specific cause | |
| Secondary sarcopenia | Secondary to a systemic disease (e.g. chronic respiratory disease) | Secondary to a systemic disease (e.g. chronic respiratory disease) |
EWGSOP: European Working Group in Sarcopenia in Older People; SCWD: Society of Sarcopenia, Cachexia and Wasting Disorders; SDOC: Sarcopenia Definition and Outcomes Consortium.
Malnutrition and sarcopenia assessment (A. Schols, The Netherlands)
A. Schols highlighted the importance of considering the different metabolic phenotypes, since sarcopenia is observed in different metabolic syndromes, such as cachexia (characterised by an additional loss of body weight and fat mass) and sarcopenic obesity (characterised by adiposity) [27]. Different metabolic phenotypes result in different clinical risks (e.g. increased cardiovascular/mortality risk or impaired physical performance), which are stratified based on body composition and change in body weight [27]. For screening purposes, the SARC-F, the SARC-CalF or the sarcopenia index can be used [28]. Nevertheless, a thorough assessment of all sarcopenia domains, i.e. muscle mass (whole-body magnetic resonance imaging, computed tomography, dual-energy X-ray absorptiometry, bioelectrical impedance and anthropometric measures), muscle strength (quadriceps strength, handgrip strength and chair stand test) and physical performance (gait speed, short physical performance battery, timed up-and-go test and 6-min walk test) is recommended [28]. To capture malnutrition, additional measures such as the MUST and the SNAQ tools, and information on dietary intake and nutrients deficiency are also important.
Underlying mechanisms and pharmacological approaches for treatment of sarcopenia (N. Greening, UK)
The third talk of the symposium focused on skeletal muscle loss, particularly in COPD. N. Greening explained that there are multiple triggers for sarcopenia in COPD and their underlying mechanisms are linked [29]. Disuse atrophy, hypoxia and inflammation are the most notable drivers of muscle loss [29]. To counteract this muscle loss, some anabolic therapies have been used, such as testosterone [30], bimagrumab [31] and selective androgen receptor modulator. Although these anabolic interventions result in increased muscle mass and some improvements in muscle strength, no improvements in the functional level (e.g. 6-min walk test) of patients with COPD have been found [30, 31]. Nevertheless, it is possible that these anabolic interventions play a role in specific individuals and circumstances, such as during acute exacerbations of COPD, where it is crucial to prevent the loss of muscle mass that occurs during hospitalisation [32]. N. Greening finished the talk highlighting that it would also be important to consider muscle endurance, neural adaptations and oxidative capacity when studying sarcopenia.
Modalities of pulmonary rehabilitation, including exercise training for sarcopenia in chronic lung disease (M. Maddocks, UK)
M. Maddocks emphasised that, overall, ∼22% of patients with COPD have sarcopenia [33]. The international clinical practice guidelines for sarcopenia strongly recommend the prescription of resistance training [34]; nevertheless, most of the evidence informing the guidelines comes from studies in nonsarcopenic patients. Moreover, there is wide variety in the exercise programmes delivered; thus, the exact way to design an exercise programme for patients with sarcopenia remains to be determined [35]. Previous studies in patients with COPD have shown that: 1) patients with sarcopenia respond well to pulmonary rehabilitation and 28% are even able to reverse sarcopenia [36]; and 2) the combination of endurance or interval training with resistance training might be optimal in patients with sarcopenia [37]. Recently, electromyostimulation has also shown potential to improve muscle strength and function in sarcopenic patients [38]. M. Maddocks concluded the talk by drawing attention to the promising results of the SPRINTT (Sarcopenia and Physical Frailty in Older People: Multi-Component Treatment Strategies) trial [39], which will be published shortly.
Take-home messages
Sarcopenia is defined by low muscle strength and low muscle quality/quantity, and it is essential that studies start assessing sarcopenia comprehensively, i.e. including muscle mass, muscle strength and physical performance measures.
Anabolic interventions improve muscle mass in patients with COPD but that does not translate into improvements in muscle function.
Pulmonary rehabilitation is an evidence-based intervention for the management of sarcopenia in patients with chronic respiratory diseases.
Symposium: maintenance of the beneficial effects of pulmonary rehabilitation: the role of digital health
This symposium (session 348) featured presentations on the incorporation of new technologies to optimise maintenance of pulmonary rehabilitation outcomes, including a synthesis of the current state of knowledge and a patient's testimony.
Patient's perspective (J.M. Fourrier, France)
J.M. Fourrier described the experience as a patient with the use of new technologies for monitoring physical activity. In his opinion, the most significant difficulties associated with activities of daily living are dyspnoea, pain and muscle fatigue, which can be managed by engaging in physical activity. J.M. Fourrier uses digital technology (Fitbit smartwatch) to help monitor daily exercise and health status. The user interface tracks the patient's achievement and enables him to connect with a coach who conducts group exercises in real time. J.M. Fourrier emphasised that he was not aware of any individuals dissatisfied with the rehabilitation programme; all patients experienced an improvement in quality of life. He concluded that exercise has become a natural part of his daily life, partly thanks to digital health technology, for which he is grateful.
Natural decline of (extra)pulmonary features in patients with COPD: a slippery slope (L.E.G.W. Vanfleteren, Sweden)
L.E.G.W. Vanfleteren outlined four areas of natural deterioration in patients with COPD: 1) lung function decline; 2) exacerbations and the natural history of COPD; 3) alterations in body composition over time; and 4) comorbidities. With regards to disease exacerbations, there is a window of opportunity ∼5 years after the first exacerbation during which pulmonary rehabilitation programmes should be implemented. After this time, the risk of another exacerbation, or even death, increases dramatically. The factors that influence disease exacerbations were also recalled: prior exacerbations, worse dyspnoea, reduced lung function, comorbid cardiovascular disease, history of gastro-oesophageal reflux, comorbid depression, poorer quality of life, female sex, elevated white blood cell count and elevated eosinophil count. Concerning changes in body composition, L.E.G.W. Vanfleteren discussed the prospective European Community Respiratory Health Survey study that suggested that moderate and high weight gain over a 20-year period is associated with accelerated FVC and FEV1 decline, while weight loss delays the deterioration of the lungs. The presentation was concluded by pointing out the positive impact of pulmonary rehabilitation on each of the listed areas of natural decline.
Concepts, goals, challenges and effects of maintenance programmes after pulmonary rehabilitation (C. Rochester, USA)
C. Rochester structured her presentation around three topics: 1) rationale for maintenance pulmonary rehabilitation; 2) the effects of maintenance programmes; and 3) challenges in the delivery of maintenance programmes (without digital health technologies), including areas for future research. The first section summarised the well-documented effects of pulmonary rehabilitation for patients with different chronic respiratory diseases as well as factors that impact people's ability to continue exercise/active after pulmonary rehabilitation, i.e. motivation, home environment, weather, financial and family issues. A longitudinal study indicating different long-term (12 months) effects of pulmonary rehabilitation was also presented [40]. It was mentioned that the form of maintenance training (supervised versus unsupervised) also affects its effectiveness over time and supervised programmes may decrease the risk of respiratory-related hospitalisation. The challenges of maintaining pulmonary rehabilitation outcomes include a limited capacity of existing programmes, a limited number of healthcare professionals, funding and reimbursement limitations, travel/transport to maintenance programmes, and the low priority of insurance companies for preventive health. Future research areas may include: 1) optimal maintenance strategies across different patient groups; 2) impact of patients’ choice of options for maintenance programmes; 3) real-world cost-effectiveness of maintenance programmes; and 4) a combination of targeted maintenance/repetition of programme rehabilitation programmes or novel models of maintenance using digital health technologies.
Take the active option: physical activity coaching programmes (H. Demeyer, Belgium)
H. Demeyer focused on the role of physical activity to maintain pulmonary rehabiliation effects, and discussed the relationship between changes in physical activity and in exercise capacity, as both are targeted through different interventions. Physical activity coaching programmes aim to increase physical activity focusing on low-intensity activities in an unsupervised way, which can be done through digital technologies. Research on the effectiveness of coaching programmes showed that, in stable patients with COPD, such programmes yield a significant increase in physical activity, but effectiveness was less clear when implemented during pulmonary rehabilitation. A small number of studies evaluating long-term physical activity coaching were also highlighted. The literature indicates that coaching programmes do not enhance exercise capacity (6-min walking distance) beyond the minimal clinically important difference. This raises the question whether maintaining and improving physical activity provides sufficient benefit. A long-term comparison of physical activity and exercise capacity in patients participating in a 3-month pulmonary rehabilitation programme only versus patients participating in pulmonary rehabilitation with an additional 3-month coaching programme was also presented. In both cases, the trend was similar, with a decrease in both parameters in a similar manner 12 months after the intervention [41]. However, research conducted by H. Demeyer's team (data not published) indicated that implementation of additional coaching sessions after completion of a 3-month pulmonary rehabilitation programme resulted in the maintenance of physical activity levels, whereas the “usual care” group not participating in coaching sessions after pulmonary rehabilitation decreased their levels of physical activity. Nevertheless, a reduced exercise capacity was noted in both groups after completion of PR.
Role of digital health to improve maintenance (B. Caulfield, Ireland)
This presentation addressed the requirements for and components of successful pulmonary rehabiliation maintenance strategies using digital tools. B. Caulfield started by recalling the results of the latest Cochrane meta-analysis [42] showing strong evidence for the effectiveness of supervised maintenance programmes on quality of life, but low effectiveness on disease exacerbations and hospitalisations in patients with COPD, and suggested that this area could be enhanced by digital technologies. Slevin and co-workers [43–46] performed a series of semistructured interviews with patients with COPD and healthcare professionals about the use of digital technologies in the maintenance phase after pulmonary rehabilitation. Patients indicated that digital technologies provided them with an opportunity for self-management and enhanced communication with healthcare professionals. Clinicians indicated benefits in the availability of interappointment data and enhanced consultation efficiency, and recognised the role of digital technology to empower patients’ self-management. Barriers to the adoption of digital technologies were also discussed. Patients primarily identified a lack of perceived usefulness and digital literacy, while clinicians mentioned the lack of quality data, little evidence base and resource constraints. Based on these data, the requirements of digital health technologies in patients with COPD were determined. Such a hypothetical system must be effective in terms of health-related quality of life, exacerbations and functional status. It should also be safe, sustainable and appropriate to implement in patients’ daily lives. Therefore, supplementing the traditional management system, or partial replacement by digital health, can be carried out through devices addressing the following areas: measurement and monitoring, information and education, encouragement and engagement, peer support, and augmented exercise.
Take-home messages
Benefits of maintenance programmes after pulmonary rehabilitation are well-established; however, their effectiveness diminishes over time if there is no regular contact with the healthcare team.
Available technology can be implemented in a comprehensive approach to monitoring patients’ health condition, as well as for exercise training and physical activity coaching.
Integrating digital health into the healthcare system requires further research that incorporates both patient and clinician perspectives.
Group 9.03: Nurses
Experts View: Hospital at home for the management of COVID-19
This Experts View session (session 16) highlighted the need to relieve hospitals during the COVID-19 pandemic, giving patients access to hospital care and increasing the resilience of the healthcare systems. Safe alternatives to healthcare services were provided to patients with COVID-19, enabling treatment, monitoring and rehabilitation.
A medicalised hotel (C. Hernández, Spain)
C. Hernández presented a successful adaptation of a four-star hotel in Barcelona, Spain, by a hospital-at-home team to provide hospital-level care to patients with COVID-19. In the period from March to May 2020, in the Hospital Clinic de Barcelona, 2410 patients were hospitalised due to COVID-19; 21.4% of patients were transferred to the medicalised hotel [47]. The main challenges arose from multidisciplinary teamwork, and there was particular importance given to separate clean and dirty areas. The equipment was also critical alongside professional experiences. The patients’ experiences [48] were analysed very carefully, and the better experiences were related to patients who claimed to have been treated with respect. In summary, C. Hernández stated that the medicalised hotel is a safe alternative to conventional hospitals for patients with noncritical COVID-19 and can relieve hospitals from the overload.
Covid@Home (L. Brien, Ireland)
L. Brien described the rapid setup and performance of a virtual monitoring service for patients with COVID-19. This service allowed patients to be in their homes and access telehealthcare performed by a multidisciplinary team and health technologies with the objective of monitoring their health. Over 14 days, eligible patients had access to the programme, were monitored four times a day and had a telephone service available that they could use when necessary. After discharge, patients were referred to post-COVID-19 rehabilitation as needed. This intervention alone was safe and responsible for reducing the length of hospital stay for patients with COVID-19, which lead to increasing bed availability. In addition, patient monitoring enabled a quick response to silent hypoxia and acute deterioration, which led to the reassurance of patients during the post-hospital period. L. Brien stated that open communication between home and hospitals teams was decisive to the success of the interventions.
Take-home messages
There are safe and adequate alternatives to the hospital regarding the treatment of patients with COVID-19.
Teamwork and compromise were crucial elements regarding the reorganisation of healthcare solutions.
Oral presentation: Nursing perspective during the COVID-19 pandemic
This oral presentation session (session 187) provided an overview of state-of-the-art advances in nursing interventions and experience during onset of COVID-19 pandemic, focusing on three main themes: impact on nursing practice; innovation in healthcare delivery; and patients’ perspectives.
Living with the risk of being infected: COPD patients’ experiences during the coronavirus pandemic (C.A. Mousing, Denmark)
Mousing and Sørensen [49] explored the perspectives of living with the risk of being infected with coronavirus in Danish patients with COPD (n=13) using individual semistructured interviews. They found that living with the risk of being infected greatly affected the everyday life of patients with moderate to severe COPD. There is a need to develop targeted interventions aimed at providing adequate information, supporting hope and maintaining warm distancing contact to ease symptoms and provide comfort to patients.
A negotiation of respiratory risk in the first phase of the COVID-19 pandemic (L. Welch, UK)
During the initial phase of the COVID-19 pandemic, various guidelines on infection control were published [50], which led to mixed messages in the early stages of the pandemic [51]. Welch et al. [52] presented a nursing response to respiratory risk during the pandemic, where concerns were expressed regarding the working environment, the supply and availability of adequate personal protective equipment, and unsafe working practice. Almost half of the respondents (48.6%) reported undertaking aerosol-generating procedures. L. Welch reinforced that earlier and clearer guidance of infection control is required to ensure clinical safety and preparation for the future respiratory pandemics [51].
Awake proning in patients with COVID-19 (W. Stilma, The Netherlands)
Prone positioning in selected patients with severe early-stage acute respiratory distress syndrome improves survival [53] and has been widely accepted only in recent years [54]. Stilma et al. [55] performed a clinical appraisal of the available literature and personal clinical experiences of healthcare workers in various settings around the world to formulate guidelines for awake prone positioning, with recommendations for its use. The authors concluded that awake proning is an attractive and safe adjunctive treatment for hypoxaemia refractory to supplemental oxygen in patients with COVID-19 acute respiratory failure.
Noninvasive positive pressure ventilation training programme for general ward healthcare workers during COVID-19 outbreak (A. Godono, Italy)
The COVID-19 pandemic had a severe impact on the healthcare system, and affected the availability of beds in hospitals and intensive care units [56]. Godono et al. [57] evaluated the efficiency of a noninvasive positive pressure ventilation (NPPV) training programme targeting healthcare professionals on general wards. The authors concluded that the training programme improved healthcare professionals’ confidence levels in managing NPPV devices in non-intensive care units and could be a crucial element to improve patients’ outcomes.
The impact of the COVID-19 pandemic on Portuguese rehabilitation nurses (M. Padilha, Portugal)
Padilha and Silva [58] assessed the impact of the pandemic on Portuguese rehabilitation nurses through an online questionnaire: the number of hours worked per week, the patient/nurse ratio and the complexity of patients with COVID. Participants reported that the complexity of respiratory patients has increased while the satisfaction with the quality of nursing care has decreased during the pandemic. The COVID-19 pandemic posed several challenges to nurses but rehabilitation nurses played a central role in stabilising, rehabilitating and reintegrating patients with COVID-19 [59].
Virtual consultations as follow up on home oxygen therapy for patients with COPD: a patient perspective (H. Schmidt, Denmark)
Schmidt et al. [60] presented a qualitative study encompassing semistructured interviews with 20 patients with COPD on long-term oxygen therapy to uncover patients’ experiences with virtual consultation, thereby ensuring patient-centred clinical practice. Findings revealed that virtual consultation was considered air- and energy-preserving due to avoiding transportation, waiting time and handling oxygen tanks, and not having to involve others for help with transportation. Most participants emphasised their fear and vulnerability in relation to COVID-19, so being able to stay at home was a welcome initiative.
The SWISS nurse: respiratory nursing care without any borders – an admission avoidance winter pressure initiative (E. Rickards, UK)
Over the last 7 years, across the north of England, UK, respiratory admissions have risen three times faster than general admissions [61]. The study by Rickards et al. [62] introduced the role of a specialist respiratory nurse (SWISS nurse) within the emergency department, who provides ongoing support, equitable care for all patients and organises long-term chronic disease management. A total of 240 admissions were prevented after 5 months with the creation of this specialist respiratory nurse position. In conclusion, this initiative improves connections with the community respiratory teams.
Nurse-led community care (A. Madden, Ireland)
Madden et al. [63] implemented a community virtual ward with the support of telemedicine to deliver specialist respiratory care in the community. Patients with exacerbations of asthma or COPD and/or at risk of deterioration were followed up by an advanced nurse practitioner and supported by community nurses. In addition, an online electronic health record was accessible to the community and hospital clinicians. As the pandemic progressed, many countries reorganised their healthcare delivery systems and implemented digital communication tools to provide secure virtual care [64].
Was our step-down virtual COVID ward safe and effective? (D. Jennings, UK)
Jennings et al. [65] demonstrated a virtual ward model of care and its effectiveness on patients’ outcomes. 89 patients were admitted to the virtual ward and findings showed that readmission rates within the 6-week period were similar to national figures (<10%). Mean mood and anxiety scores improved between days 1 and 14, and there was no increase in readmission rates for patients who required continuous positive airway pressure during admission and discharged patients with prescribed oxygen therapy. Patients’ feedback on the virtual ward model of care was positive and the authors concluded that the system was very useful for patients, especially to those with chronic conditions.
Promoting physical activity by the respiratory nurses (S. Rocha, Portugal)
Pulmonary rehabilitation is the most effective nonpharmacological treatment strategy to control symptoms and progression of COPD [66]. Rocha et al. [67] assessed the impact and effectiveness of the respiratory nurses’ interventions on the treatment of the patients involved in the programme (n=46). Interventions were adapted for each patient according to their individual characteristics. The average score of the physical activity domain of the London Chest Activity of Daily Living scale was 5.17 at baseline and 3.87 at the end of the programme (p<0.05). Findings showed the positive impact of nursing interventions in physical activity by improving the individual skills and self-care behaviour of patients with COPD.
Take-home messages
Virtual consultations and follow-up are an effective measure in monitoring patients with chronic respiratory disease.
There is a need for targeted interventions aimed at giving adequate information, supporting hope and maintaining warm distancing contact.
Psychological support must be integrated as a part of the virtual model care for the respiratory patients.
Group 9.04: Psychologists and behavioural scientists
Oral presentation: Psychological and behavioural issues in respiratory care
This oral presentation session (session 59) was the inaugural session with abstracts submitted to the novel Psychologists and Behavioural Scientists group (9.04). The session focused on the role of psychological issues in healthcare providers, caregivers and patients in COVID-19 and other respiratory conditions.
No gender differences in neural gating of respiratory sensations in COPD patients: preliminary findings (Y. Denutte, Belgium)
Based on the neural gating model of respiratory sensations (NGRS), Denutte et al. [68] presented the results of an electroencephalography (EEG) study of gender differences in dyspnoea perception. According to the NGRS, dyspnoea results from reduced neural gating of respiratory afferent signals into the cerebral cortex and it was hypothesised that female patients would show reduced NGRS. EEG measurements were performed on 11 female and 15 male patients with COPD when presented with paired inspiratory occlusions. The results indicated no significant gender differences in NGRS but larger studies are needed to confirm these findings. Identifying relevant biological, psychological and behavioural predictors of differences in dyspnoea perception is highly important in the holistic and patient-centred approach to COPD care.
Translation and initial validation of the Danish version of the COPD Anxiety Questionnaire (S. Rubio-Rask, Denmark)
The COPD Anxiety Questionnaire (CAF) was originally constructed in German to measure disease-specific anxiety in patients with COPD across five domains: 1) fear of dyspnoea; 2) fear of disease progression; 3) fear of physical activity; 4) fear of social exclusion; and 5) sleep-related worries. On behalf of Rubio-Rask et al. [69], I. Farver-Vestergaard presented their Danish translation of the questionnaire (CAF-DK), as well as a study performing the initial validation of the CAF-DK in a sample of 260 patients with COPD (238 electronic responses and 22 paper responses). Results showed that Cronbach's α values for the total and domain-scale scores were comparable to those of the original CAF, as was the correlation coefficients between CAF-DK and concurrent measures (General Anxiety Disorder-7 and the COPD Assessment Test). In conclusion, the CAF-DK can be used to measure COPD-specific anxiety in Danish-speaking patients, yet further studies are needed to explore the psychometric properties of the CAF, compared with other disease-specific measures of anxiety in COPD.
Optimism, exacerbations and health outcomes of pulmonary rehabilitation in patients with COPD (T. Janssens, Belgium)
Pulmonary rehabilitation is a cost-effective treatment for patients with COPD but not all patients benefit from this treatment to the same extent. Janssens et al. [70] presented the results of a prospective study focusing on the role of optimism as a predictor of treatment response across 3-week inpatient pulmonary rehabilitation and 6-month follow-up in 370 patients with COPD. Results showed that higher levels of optimism at baseline were associated with lower depressive symptoms and better health status across all timepoints. Contrary to what was hypothesised, the positive associations between optimism and health status were limited to patients that did not experience an exacerbation during follow-up. These findings confirm the role of patient beliefs on outcome trajectories but also highlight boundaries of these effects.
Technology-dependent children with respiratory problems on a home care programme: exploring the family experience (M. Galogavrou, Greece)
An increasing number of children have respiratory problems needing paediatric home care, which as a major impact on the parents and home environment. Galogavrou et al. [71] presented the results of an observational study on parents’ perceptions of paediatric healthcare services and family well-being for children (n=51, 27 boys) depending on paediatric home care (mechanical ventilation n=25, oxygen dependent n=13, tracheostomy n=8, noninvasive ventilation n=5). Most parents had completed higher education, were employed and were married. Results showed high levels of satisfaction with care. Nevertheless, 27.4% of parents reported moderate or severe depressive symptoms and 35.2% reported moderate to severe anxiety symptoms. These findings suggest a need for attention to parental wellbeing in this population.
Psychological functioning and lifestyle behaviours of patients with idiopathic pulmonary fibrosis: a prospective study (A. Delameillieure, Belgium)
Idiopathic pulmonary fibrosis (IPF) is a rare and severe lung disease with a relatively poor prognosis that, beyond the physical symptoms, impacts psychological and behavioural factors. Delameillieure et al. [72] presented the results of a prospective study on psychological functioning and lifestyle behaviours of patients with IPF, conducted at the University Hospitals Leuven, Belgium. The cohort of patients (n=66; 72% male; mean age 70 years) were included at IPF diagnosis and completed questionnaires assessing depression, anxiety, sun protection, physical activity and alcohol intake at each hospital visit during the following 2 years. Results showed that a considerable proportion of patients experienced symptoms of anxiety and depression, as well as suboptimal lifestyle behaviour patterns across the illness trajectory. However, response rates were low and conclusions should therefore be made with caution. Nonetheless, the identification of psychological and lifestyle factors across the illness trajectory is an important step towards providing IPF care that is more holistic and patient centred.
Mental health during COVID-19 in Dutch adolescents and adults with cystic fibrosis or primary ciliary dyskinesia and their caregivers (M. Verkleij, The Netherlands)
Patients with cystic fibrosis or primary ciliary dyskinesia (PCD) and their caregivers have a high risk of developing anxiety or depressive symptoms. Furthermore, COVID-19 related measures, such as national lockdowns and social distancing, have a potential for negative impact on mental health. Verkleij et al. [73] presented the results of a prospective study investigating changes in anxiety, depression and resilience in Dutch adolescents with cystic fibrosis or PCD (n=41) and caregivers of patients (n=69) during the second wave of the COVID-19 pandemic. Results showed overall high prevalence of anxiety symptoms (31–53% reporting at least mild depressive symptoms, nine-item Patient Health Questionnaire score >5; 33–36% reporting at least mild anxiety symptoms, seven-item Generalised Anxiety Disorder Assessment score >5) during the second lockdown. However, anxiety and depressive symptoms were unchanged compared to pre-pandemic measures. These results highlight a continued mental health burden in patients with cystic fibrosis or PCD and their caregivers.
Psychological sequelae among health personnel treated for COVID-19 at the Hassan II hospital in Agadir (F. Bounoua, Morocco)
The COVID-19 pandemic has led to increased demands on healthcare professionals, especially healthcare workers on the front line of management of COVID-19. Bounoua et al. [74] presented results of an observational study investigating anxiety and depressive symptoms as well as potential PTSD in staff of a single Moroccan hospital treated for COVID-19 (n=67; 58% women, 32% with comorbidities and 3% needing intensive care treatment). From these, 64% of participants reported residual symptoms after recovery. Only 42% of participants did not report anxiety or depressive symptoms (measured using the Hospital Anxiety and Depression Scale (HADS)) and 10% of participants showed symptoms of PTSD. These results show a strong psychological impact in this group of healthcare workers treated for COVID-19 and highlights the need for psychological support.
Impact of COVID-19 on mental health: a traumatic event (S. Houben-Wilke, The Netherlands)
Residual symptoms of COVID-19 have been reported but longer-term symptoms and psychological burden in patients with residual symptoms remains unclear. On behalf of Houben-Wilke et al. [75], M. Van Herck presented the results of a prospective survey investigating symptoms of anxiety and depression (using HADS) as well as PTSD in a group of participants (n=239, 62 hospitalised) 3 and 6 months after confirmed COVID-19 diagnosis. Participants reported good health status before infection (79% in hospitalised versus 90% in nonhospitalised patients, p<0.05). Considering the whole sample, 35% of patients reported symptoms of anxiety 3 months after infection, which was not reduced at 6 months, and nearly 50% of patients reported symptoms of anxiety 3 months after infection, with a small reduction after 6 months. 40% of patients were at risk of PTSD 3 months after infection, which was reduced to 30% 6 months after infection. Symptoms of anxiety, depression and PTSD were comparable among hospitalised and nonhospitalised patients. Findings suggest that a substantial proportion of patients with residual symptoms after COVID-19 show psychological complications, and awareness of healthcare providers and access to care are needed to address these problems.
Sex differences in mental health of hospitalised patients with COVID-19 (Z. Barmparessou, Greece)
COVID-19 hospitalisation can pose a considerable mental burden on patients, even after hospital discharge. Barmparessou et al. [76] presented the results of a survey performed in a large COVID-19 reference hospital in Athens, Greece. Depression, anxiety, PTSD, sleeping difficulties and quality of life were assessed in 131 patients 1–2 months after discharge from COVID-19 hospitalisation. Prevalence rates of clinically significant symptom levels were high (PTSD 50%; sleep disorder 41%; anxiety 35%; depression 20%), suggesting a considerable general mental burden on patients upon COVID-19 hospital discharge. Moreover, prevalence rates were significantly higher for female than male patients, in spite of females spending fewer days at the hospital. As this was a cross-sectional study with no non-COVID-19 control group, no causal inferences could be made. However, the results do highlight the potential need for mental health screening and follow-up in patients that have been hospitalised with COVID-19.
Take-home messages
Respiratory conditions are associated with psychological distress in patients and caregivers.
Psychological and behavioural aspects of the respiratory disease show associations with important health outcomes.
Measuring psychological distress is a first step towards the identification of psychological healthcare needs in patients with respiratory disease.
Concluding remarks
This article provides valuable insights on the latest scientific data and emerging areas affecting the clinical practice of allied respiratory professionals presented at the Virtual 2021 ERS International Congress. We look forward to seeing you in Barcelona in 2022 for another highly successful ERS Congress.
Footnotes
Conflict of interest: F. Machado declares a PhD grant from Fundação para a Ciência e Tecnologia (reference: SFRH/BD/147200/2019) and support from Bijzonder Onderzoeksfonds – Bilaterale Samenwerking (BOF BILA) from Hasselt University (BOF BILA reference: DOC/SCHLBOSE/190/522). I. Farver-Vestergaard declares payment or honoraria from Boehringer Ingelheim, Novartis and Roche, in the 36 months prior to manuscript submission. K.P. Sylvester declares payment or honoraria from Circassia, Vyaire Medical and NDD Medical Technologies, in the 36 months prior to manuscript submission. A. Šajnić declares unpaid roles as Chair of the European Respiratory Society Nursing Group and as a member of the European Lung Foundation Advisory Professional Committee. J. Cruz declares payment or honoraria from Circassia, Vyaire Medical and NDD Medical Technologies, in the 36 months prior to manuscript submission. All other authors declare no competing interests.
Support statement: F. Machado's work is supported by Fundação para a Ciência e Tecnologia (reference: SFRH/BD/147200/2019) and by Bijzonder Onderzoeksfonds – Bilaterale Samenwerking (BOF BILA) from Hasselt University (BOF BILA reference: DOC/SCHL-BOSE/190/522). J. Cruz acknowledges the support of the Center for Innovative Care and Health Technology (ciTechCare), funded by Portuguese national funds provided by Fundação para a Ciência e Tecnologia (FCT) (UIDB/05704/2020).
References
- 1.Savushkina O, Cherniak A, Zaitsev A, et al. Ventilation heterogeneity after COVID-19. Eur Respir J 2021; 58: Suppl. 65, OA2681. [Google Scholar]
- 2.Hurst C, Yearsley S, Stone H, et al. Evaluation of patient attendance to respiratory physiology in the midst of the COVID-19 Pandemic. Eur Respir J 2021; 58: Suppl. 65, OA2682. [Google Scholar]
- 3.National Health Service Foundation Trust . 2019 Outpatients project – Results published. https://www.nhsbenchmarking.nhs.uk/news/2019-outpatients-project-results-published. Date last updated: 17 October 2019. Date last accessed: October 19 2021.
- 4.Steenbruggen I, De Laat P, Van De Geijn AHM, et al. Implementation of the 2017 ERS Methacholine Challenge Standard. Eur Respir J 2021; 58: Suppl. 65, OA2683. [Google Scholar]
- 5.Coates AL, Wanger J, Cockcroft DW, et al. ERS technical standard on bronchial challenge testing: general considerations and performance of methacholine challenge tests. Eur Respir J 2017; 49: 1601526. doi: 10.1183/13993003.01526-2016 [DOI] [PubMed] [Google Scholar]
- 6.De Soomer K, Casas L, Vaerenberg H, et al. Evaluation of the Global Lung function initiative reference values for spirometry and diffusion capacity. Eur Respir J 2021; 58: Suppl. 65, OA2684. [Google Scholar]
- 7.Quanjer PH, Stanojevic S, Cole TJ, et al. Multi-ethnic reference values for spirometry for the 3–95-yr age range: the global lung function 2012 equations. Eur Respir J 2012; 40: 1324–1343. doi: 10.1183/09031936.00080312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Stanojevic S, Graham BL, Cooper BG, et al. Official ERS technical standards: Global Lung Function Initiative reference values for the carbon monoxide transfer factor for Caucasians. Eur Respir J 2017; 50: 1700010. doi: 10.1183/13993003.00010-2017 [DOI] [PubMed] [Google Scholar]
- 9.Mottram CD, Mccaskill T, Road J, et al. Pulmonary airway resistance variability in normal biologic quality control subjects among pulmonary function testing systems across British Columbia. Eur Respir J 2021; 58: Suppl. 65, OA2685. [Google Scholar]
- 10.Robertson L, Lowry R, Sylvester K. Do bacterial/viral filters impact quality assurance verification of ultrasonic spirometers? Eur Respir J 2021; 58: Suppl. 65, OA2686. [Google Scholar]
- 11.Oestreich M-A, Frauchiger B, Latzin P, et al. Breath detection algorithms effect lung function outcomes. Eur Respir J 2021; 58: Suppl. 65, OA2687. [Google Scholar]
- 12.Stanojevic S, Powell P, Hall G, et al. Real-world application of Spirometry Quality Control Deep-Learning Algorithm. Eur Respir J 2021; 58: Suppl. 65, OA2688. [Google Scholar]
- 13.Das N, Verstraete K, Stanojevic S, et al. Deep-learning algorithm helps to standardise ATS/ERS spirometric acceptability and usability criteria. Eur Respir J 2020; 56: 2000603. doi: 10.1183/13993003.00603-2020 [DOI] [PubMed] [Google Scholar]
- 14.Miller MR, Hankinson J, Brusasco V, et al. Standardisation of spirometry. Eur Respir J 2005; 26: 319–338. doi: 10.1183/09031936.05.00034805 [DOI] [PubMed] [Google Scholar]
- 15.Veneroni C, Acciarito A, Pompilio P, et al. Use of artificial intelligence for improving quality control of oscillometry. Eur Respir J 2021; 58: Suppl. 65, OA2689. [DOI] [PubMed] [Google Scholar]
- 16.King GG, Bates J, Berger KI, et al. Technical standards for respiratory oscillometry. Eur Respir J 2020; 55: 1900753. doi: 10.1183/13993003.00753-2019 [DOI] [PubMed] [Google Scholar]
- 17.Del Corral Nuñez-Flores T, Fabero-Garrido R, Plaza-Manzano G, et al. Effects of respiratory muscle training on quality of life, physical function, and psychological state in Post-COVID Syndrome. Eur Respir J 2021; 58: Suppl. 65, OA2690. [Google Scholar]
- 18.Baumgartner RN, Koehler KM, Gallagher D, et al. Epidemiology of sarcopenia among the elderly in New Mexico. Am J Epidemiol 1998; 147: 755–763. doi: 10.1093/oxfordjournals.aje.a009520 [DOI] [PubMed] [Google Scholar]
- 19.Cruz-Jentoft AJ, Baeyens JP, Bauer JM, et al. Sarcopenia: European consensus on definition and diagnosis. Age Ageing 2010; 39: 412–423. doi: 10.1093/ageing/afq034 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Morley JE, Abbatecola AM, Argiles JM, et al. Sarcopenia with limited mobility: an international consensus. J Am Med Dir Assoc 2011; 12: 403–409. doi: 10.1016/j.jamda.2011.04.014 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Muscaritoli M, Anker S, Argiles J, et al. Consensus definition of sarcopenia, cachexia and pre-cachexia: joint document elaborated by Special Interest Groups (SIG) “cachexia-anorexia in chronic wasting diseases” and “nutrition in geriatrics”. Clin Nutr 2010; 29: 154–159. doi: 10.1016/j.clnu.2009.12.004 [DOI] [PubMed] [Google Scholar]
- 22.International Working Group on Sarcopenia . Sarcopenia: an undiagnosed condition in older adults. Current consensus definition: prevalence, etiology, and consequences. J Am Med Dir Assoc 2011; 12: 249–256. doi: 10.1016/j.jamda.2011.01.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Mitchell WK, Atherton PJ, Williams J, et al. Sarcopenia, dynapenia, and the impact of advancing age on human skeletal muscle size and strength; a quantitative review. Front Physiol 2012; 3: 260. doi: 10.3389/fphys.2012.00260 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Cruz-Jentoft AJ, Bahat G, Bauer J, et al. Sarcopenia: revised European consensus on definition and diagnosis. Age Ageing 2019; 48: 16–31. doi: 10.1093/ageing/afy169 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Bauer J, Morley JE, Schols AM, et al. Sarcopenia: a time for action. An SCWD position paper. J Cachexia Sarcopenia Muscle 2019; 10: 956–961. doi: 10.1002/jcsm.12483 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Bhasin S, Travison TG, Manini TM, et al. Sarcopenia definition: the position statements of the sarcopenia definition and outcomes consortium. J Am Geriatr Soc 2020; 68: 1410–1418. doi: 10.1111/jgs.16372 [DOI] [PubMed] [Google Scholar]
- 27.Schols AM, Ferreira IM, Franssen FM, et al. Nutritional assessment and therapy in COPD: a European Respiratory Society statement. Eur Respir J 2014; 44: 1504–1520. doi: 10.1183/09031936.00070914 [DOI] [PubMed] [Google Scholar]
- 28.van Bakel SI, Gosker HR, Langen RC, et al. Towards personalized management of sarcopenia in COPD. Int J Chron Obstruct Pulmon Dis 2021; 16: 25. doi: 10.2147/COPD.S280540 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Langen R, Gosker H, Remels A, et al. Triggers and mechanisms of skeletal muscle wasting in chronic obstructive pulmonary disease. Int J Biochem Cell Biol 2013; 45: 2245–2256. doi: 10.1016/j.biocel.2013.06.015 [DOI] [PubMed] [Google Scholar]
- 30.Casaburi R, Bhasin S, Cosentino L, et al. Effects of testosterone and resistance training in men with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 2004; 170: 870–878. doi: 10.1164/rccm.200305-617OC [DOI] [PubMed] [Google Scholar]
- 31.Polkey MI, Praestgaard J, Berwick A, et al. Activin type II receptor blockade for treatment of muscle depletion in chronic obstructive pulmonary disease. A randomized trial. Am J Respir Crit Care Med 2019; 199: 313–320. doi: 10.1164/rccm.201802-0286OC [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.McAuley HJ, Harvey-Dunstan TC, Craner M, et al. Longitudinal changes to quadriceps thickness demonstrate acute sarcopenia following admission to hospital for an exacerbation of chronic respiratory disease. Thorax 2021; 76: 726–728. doi: 10.1136/thoraxjnl-2020-215949 [DOI] [PubMed] [Google Scholar]
- 33.Benz E, Trajanoska K, Lahousse L, et al. Sarcopenia in COPD: a systematic review and meta-analysis. Eur Respir Rev 2019; 28: 190049. doi: 10.1183/16000617.0049-2019 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Dent E, Morley J, Cruz-Jentoft A, et al. International clinical practice guidelines for sarcopenia (ICFSR): screening, diagnosis and management. J Nutr Health Aging 2018; 22: 1148–1161. doi: 10.1007/s12603-018-1139-9 [DOI] [PubMed] [Google Scholar]
- 35.Cruz-Jentoft AJ, Sayer AA. Sarcopenia. Lancet 2019; 393: 2636–2646. doi: 10.1016/S0140-6736(19)31138-9 [DOI] [PubMed] [Google Scholar]
- 36.Jones SE, Maddocks M, Kon SS, et al. Sarcopenia in COPD: prevalence, clinical correlates and response to pulmonary rehabilitation. Thorax 2015; 70: 213–218. doi: 10.1136/thoraxjnl-2014-206440 [DOI] [PubMed] [Google Scholar]
- 37.Covey MK, Collins EG, Reynertson SI, et al. Resistance training as a preconditioning strategy for enhancing aerobic exercise training outcomes in COPD. Respir Med 2014; 108: 1141–1152. doi: 10.1016/j.rmed.2014.06.001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Teschler M, Heimer M, Schmitz B, et al. Four weeks of electromyostimulation improves muscle function and strength in sarcopenic patients: a three-arm parallel randomized trial. J Cachexia Sarcopenia Muscle 2021; 12: 843–854. doi: 10.1002/jcsm.12717 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.SPRINTT Trial Consortium . IMI1 Final Project Report Public Summary. Innovative Medicines Initiative, 2020. [Google Scholar]
- 40.Soicher JE, Mayo NE, Gauvin L, et al. Trajectories of endurance activity following pulmonary rehabilitation in COPD patients. Eur Respir J 2012; 39: 272–278. doi: 10.1183/09031936.00026011 [DOI] [PubMed] [Google Scholar]
- 41.Altenburg WA, ten Hacken NH, Bossenbroek L, et al. Short- and long-term effects of a physical activity counselling programme in COPD: a randomized controlled trial. Respir Med 2015; 109: 112–121. doi: 10.1016/j.rmed.2014.10.020 [DOI] [PubMed] [Google Scholar]
- 42.Malaguti C, Dal Corso S, Janjua S, et al. Supervised maintenance programmes following pulmonary rehabilitation compared to usual care for chronic obstructive pulmonary disease. Cochrane Database Syst Rev 2021; 8: CD013569. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Slevin P, Kessie T, Cullen J, et al. A qualitative study of chronic obstructive pulmonary disease patient perceptions of the barriers and facilitators to adopting digital health technology. Digit Health 2019; 5: 2055207619871729. doi: 10.1177/2055207619871729 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Slevin P, Kessie T, Cullen J, et al. Exploring the potential benefits of digital health technology for the management of COPD: a qualitative study of patient perceptions. ERJ Open Res 2019; 5: 00239-2018. doi: 10.1183/23120541.00239-2018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Slevin P, Kessie T, Cullen J, et al. Exploring the barriers and facilitators for the use of digital health technologies for the management of COPD: a qualitative study of clinician perceptions. QJM 2020; 113: 163–172. [DOI] [PubMed] [Google Scholar]
- 46.Slevin P, Kessie T, Cullen J, et al. A qualitative study of clinician perceptions regarding the potential role for digital health interventions for the management of COPD. Health Informatics J 2021; 27: 1460458221994888. doi: 10.1177/1460458221994888 [DOI] [PubMed] [Google Scholar]
- 47.Torrallardona-Murphy O, Pericàs JM, Rabaneda-Lombarte N, et al. Medicalized Hotel as an alternative to hospital care for management of noncritical COVID-19. Ann Intern Med 2021; 174: 1338–1340. doi: 10.7326/M21-1873 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Cervera M, Escarrabill J, Palou E, et al. Patient's Experiences in a Medicalized Hotel for Covid-19 Acute Care Support. An Observational Study with a Cross-Sectional Design. Am J Respir Crit Care Med 2021; 203: A3190. [Google Scholar]
- 49.Mousing CA, Sørensen D. Living with the risk of being infected: COPD patients’ experiences during the coronavirus pandemic. Eur Respir J 2021; 58: Suppl. 65, OA1503. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 50.Birgand G, Mutters NT, Otter J, et al. Analysis of national and international guidelines on respiratory protection equipment for COVID-19 in healthcare settings. medRxiv 2020; pre-print [ 10.1101/2020.04.23.20077230]. [DOI] [Google Scholar]
- 51.Bird P, Badhwar V, Fallon K, et al. High SARS-CoV-2 infection rates in respiratory staff nurses and correlation of COVID-19 symptom patterns with PCR positivity and relative viral loads. J Infect 2020; 81: 452–482. doi: 10.1016/j.jinf.2020.06.035 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 52.Welch L, Roberts N, Lippiett K, et al. A negotiation of respiratory risk in the first phase of the Covid-19 pandemic. Eur Respir J 2021; 58: Suppl. 65, OA1504. [Google Scholar]
- 53.Scholten EL, Beitler JR, Prisk GK, et al. Treatment of ARDS With Prone Positioning. Chest 2017; 151: 215–224. doi: 10.1016/j.chest.2016.06.032 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Paul V, Patel S, Royse M, et al. Proning in non-intubated (PINI) in times of COVID-19: case series and a review. J Intensive Care Med 2020; 35: 818–824. doi: 10.1177/0885066620934801 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Stilma W, Bos L, Pisani L, et al. Awake proning in patients with COVID-19. Eur Respir J 2021; 58: Suppl. 65, OA1505. [Google Scholar]
- 56.Sánchez-Úbeda EF, Sánchez-Martín P, Torrego-Ellacuría M, et al. Flexibility and bed margins of the Community of Madrid's Hospitals during the first wave of the SARS-CoV-2 Pandemic. Int J Environ Res Public Health 2021; 18: 3510. doi: 10.3390/ijerph18073510 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Godono A, Gavetti D, Clari M, et al. Non-invasive positive pressure ventilation training program for general wards healthcare workers during Covid-19 outbreak. Eur Respir J 2021; 58: Suppl. 65, OA1506. [Google Scholar]
- 58.Padilha M, Silva R. The impact of the COVID-19 pandemic on Portuguese rehabilitation nurses. Eur Respir J 2021; 58: Suppl. 65, OA1507. [Google Scholar]
- 59.Vitacca M, Carone M, Clini EM, et al. Joint statement on the role of respiratory rehabilitation in the COVID-19 crisis: the Italian position paper. Respiration 2020; 99: 493–499. doi: 10.1159/000508399 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Schmidt HC, Tulinius G, Christensen HM. Virtual consultations as follow up on home oxygen therapy for patients with COPD: A patient perspective. Eur Respir J 2021; 58: Suppl. 65, OA1508. [Google Scholar]
- 61.British Lung Foundation . Out in the cold – lung disease, the hidden driver of NHS winter pressure. https://www.blf.org.uk/policy/out-in-the-cold. Date last accessed: 25 November 2021. Date last updated: 2017.
- 62.Rickards E, Ascough L, Sibley S, et al. The SWISS Nurse; respiratory nursing care without any borders. An admission avoidance winter pressure initiative. Eur Respir J 2021; 58: Suppl. 65, OA1509. [Google Scholar]
- 63.Madden A, Cushen B, Lewis C. Nurse-led community care. Eur Respir J 2021; 58: Suppl. 65, OA1510. [Google Scholar]
- 64.Temesgen ZM, DeSimone DC, Mahmood M, et al. Health care after the COVID-19 pandemic and the influence of telemedicine. Mayo Clin Proc 2020; 95: S66–S68. doi: 10.1016/j.mayocp.2020.06.052 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Jennings D, Hills K, Briscoe J, et al. Late Breaking Abstract - Was our step-down virtual covid ward safe and effective? Eur Respir J 2021; 58: Suppl. 65, OA1511. [Google Scholar]
- 66.Wada JT, Borges-Santos E, Porras DC, et al. Effects of aerobic training combined with respiratory muscle stretching on the functional exercise capacity and thoracoabdominal kinematics in patients with COPD: a randomized and controlled trial. Int J Chron Obstruct Pulmon Dis 2016; 11: 2691–2700. doi: 10.2147/COPD.S114548 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Rocha SMP, Rodrigues MF, Marques G, et al. Late Breaking Abstract - Promoting physical activity by the Respiratory Nurses. Eur Respir J 2021; 58: Suppl. 65, OA1512. [Google Scholar]
- 68.Denutte Y, Reijnders T, Gosselink R, et al. No gender differences in neural gating of respiratory sensations in COPD patients – preliminary findings. Eur Respir J 2021; 58: Suppl. 65, OA183. [Google Scholar]
- 69.Rubio-Rask S, Farver-Vestergaard I, Hilberg O, et al. Translation and initial validation of the Danish version of the COPD-Anxiety Questionnaire. Eur Respir J 2021; 58: Suppl. 65, OA184. [Google Scholar]
- 70.Janssens T, Geidl W, Carl J, et al. Optimism, exacerbations and health outcomes of pulmonary rehabilitation in patients with COPD. Eur Respir J 2021; 58: Suppl. 65, OA185. [Google Scholar]
- 71.Galogavrou M, Hatziagorou E, Vantsi P, et al. Technology-dependent children with respiratory problems on a home care program: Exploring the family experience. Eur Respir J 2021; 58: Suppl. 65, OA186. [Google Scholar]
- 72.Delameillieure A, Dobbels F, Leceuvre K, et al. Psychological functioning and lifestyle behaviours of patients with idiopathic pulmonary fibrosis: a prospective study. Eur Respir J 2021; 58: Suppl. 65, OA187. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Verkleij M, Noij L, Hashimoto S, et al. Mental health during COVID-19 in Dutch adolescents and adults with cystic fibrosis (CF) or primary ciliary dyskinesia (PCD) and their caregivers. Eur Respir J 2021; 58: Suppl. 65, OA188. [DOI] [PubMed] [Google Scholar]
- 74.Bounoua F, Moubachir H, Serhane H. Psychological sequelae among health personnel treated for COVID 19 at the Hassan II hospital in Agadir. Eur Respir J 2021; 58: Suppl. 65, OA189. [Google Scholar]
- 75.Houben-Wilke S, Goërtz Y, Delbressine J, et al. Impact of COVID-19 on mental health: a traumatic event. Eur Respir J 2021; 58: Suppl. 65, OA190. [Google Scholar]
- 76.Barmparessou Z, Pappa S, Pappas A, et al. Sex differences in mental health of hospitalized patients with COVID-19. Eur Respir J 2021; 58: Suppl. 65, OA191. [Google Scholar]