Abstract
Background:
Continuum of care [COC] for maternal health care [MHC] refers to continuity of care that has been considered as a core principle and framework to underpin strategies and programs to save the lives and promote wellbeing of mothers and newborns. However, the status of the continuum of care for maternal health care is not well studied. Thus, the objective of this analysis is to examine the status of the continuum of care for maternal health care and current recommendations in Low- and Middle-Income Countries.
Methods:
Our review followed the scoping review methods. We searched for relevant studies in the PubMed, and Cochrane Library databases. Additionally, lateral searching was carried out from google scholar, reference lists of the included studies and supplemented by a gray literature search. One reviewer screened the full list, which was randomly split into two halves and independently screened by other 2 reviewers. The 2 reviewers independently extracted the data and discrepancies were resolved through discussion.
Results:
A total of 1259 records were identified through the databases and others searching strategies. Of these, 13 studies were included in the review and the year of their publication was from 2015 to 2019, more than half (53.8 %) of the included studies were from African countries. As to the source of data 53.8% of them were from countries’ Demographic Health Survey [DHS], and all of them were cross sectional study by design. The general picture shows a decline in use of the services as women move along the continuum of care from pregnancy to childbirth and postnatal, and the highest gap was noticed between institutional delivery and postnatal care. The completion status differs from country to country and 60% in Cambodia during the 2010 CDHS but, 5% in Ratanakiri, Cambodia in 2015.
Conclusion and recommendations:
The status of continuum of care for maternal health care is varies across the countries. Also, there is limited studies on the continuum of maternal health care and more than half of the studies on this area were from countries’ Demographic Health Survey and all of them were cross sectional by design. Furthermore, none of the reviewed studies considered status of continuum of care and birth outcomes. Hence, it is decisive to estimate the status of completion of continuum of care, completion, and its effect on birth outcomes in countries like Ethiopia where the burden of maternal and newborn mortality is high.
Plain English summary
Continuum of care for maternal health care means the continuity of care during prenatal, delivery and postnatal. It has been considered as core strategies to save the lives of mothers and newborns.
We searched for relevant studies in the databases and gray literature. Two reviewers performed data extraction independently. A total of 1259 records were identified through searching. Thirteen studies were included in the review. More than half of the studies included were from African countries. Demographic Health Survey [DHS] reported from these countries formed the main source of data. All of them were cross sectional study by design.
The general picture shows a decline in the use of the health services as women move along the continuum of care from ANC to PNC. The completion status varies across countries.
Keywords: Maternal, newborn, child health, continuum of care, completion, LMIC
Introduction
Continuum of care (CoC) for maternal health care (MHC) is the continuity of individual care that has been considered as a core principle and framework to underpin strategies and programs to save the lives of mothers and babies and promote overall health. 1
The assumption behind the concept of CoC for MHC is that the health and well-being of women, newborns, and children are closely intertwined and should be managed in an integrated approach. The COC model demands ensuring availability and access to essential health services for women and childhood interventions with a purpose of ensuring the needs of each group included in policies and programs1-3
The continuum of care for MNCH has 2 dimensions-the time and place. The period is the lifecycle care that was given during adolescence, pregnancy, childbirth, postnatal, and childhood period linking with the place including household, community and health facilities. The effect at each time period depends on the foundation set in the preceding time period, ensuring more comprehensive health care for each woman at each level results in saving more lives at less cost in a more integrated and efficient way. 4
The continuum of care recognizes the relationship between MHC at different time periods and places. An effective CoC for MNCH is a means to reduce the burden of maternal, neonatal and child death and improve their health, well-being, and survival.2,3
Evidences demonstrated that the lack of appropriate care at all levels has been associated with poor maternal and newborn health outcomes.1,5,6 Despite the progress in improving reproductive, maternal, neonatal and child health, disproportions remain high in Low and Middle-Income Countries (LMICs). For example, only 14% of women in Sub-Saharan Africa received all services: at least 1 ANC, 4 or more ANC, delivery with a Skilled Birth Attendant, Postnatal Care (PNC) check within 24 hours, and family planning counseling within 1 year of birth. 7
Findings from Tanzania indicated only 10% of women followed the recommended pathway in the care continuum: 4 ANC contact, skilled attendance at delivery and at least 1 postnatal visit. 8 Evidence from Ghana indicated 86.1% of women had ANC4 plus while 75.6% give birth at health facility; this drastically fell to 25.4% for PNC within 48 hours and only 8.0% had completed the continuum of care. 9
Similarly, the trend in the CoC for maternal and newborn health in South Asia shows a decline in use of services as women moves along the continuum of care from pregnancy to childbirth and postnatal care, and only one-fourth of women received all the services provided during pregnancy, delivery, and postpartum.7,10
Study in Cambodia indicated 90% of women received ANC, while 19% dropped on the pathway, 71% continued for skilled birth and only 60% went for the full range of services. 11 In Pakistan the completion rate has increased from 15% in 2006 to 27% in 2012 12 and in Nepal only 27% of women used all 3 components of MHC. 13
In Ethiopia, 32% of women had ANC 4 plus despite a higher proportion of them had gone for first ANC (62%) suggesting the completion rate was low, only 26% used institutional delivery and 17% of women and 13% of newborns received PNC within the first 2 days of birth. 14 Also, according to the 2019 Mini Demographic and Health Survey the ANC 4 plus was 43%, while births attended in a health facility was 48% but, PNC within the first 2 days of birth was 34%. 15 Even though, it is assumed that utilization of one level of MHC is related to the subsequent (next) level of care usage but, there is high drop out in between each care levels. However, in LMICs, still MHC utilization is low in relation with the taken effort and the completion of CoC status is not well documented. For instance, it is unclear whether in Ethiopia the 17% PNC users were from the 26% institutional delivery users or the 26% institutional delivery users were from the 32% 4 or more ANC user.
Therefore, conducting analysis on this area is vital to generate strong evidences by examining the existing evidence, identifying gaps, the types of existing evidence on the area to forward logical questions and call for the use of different research approaches that will be used to address gaps more effectively. Hence, the objective of this scoping review is to examine the status of continuum of care for maternal health care and existing recommendations in the LMICs.
Methods
Scoping review is an ideal tool to determine the scope or coverage of a body of literature on area and give clear indication of the volume of literature and studies available as well as an overview (broad or detailed) of its focus. 16 Thus, this review was aimed to provide overview of the nature, scope, extent, sources and types of evidences and literatures available on status and recommendations on continuum of care for maternal health care using the established scoping review methodology, and map the key concepts.
Objective
The object of this review is to examine and describe available evidence on the status of continuum of care for maternal health care, and existing evidences in LMICs.
Participants/ Population
In this review the participants/clients were women who are candidates for maternal health services (ANC, Institutional delivery and PNC) use as per the World Health Organization [WHO] recommendation.
Concept
The main concept for this review was completion of the continuum of care for maternal health care (ANC, Institutional delivery and PNC) use as per the World Health Organization (WHO) recommendation. The concept of this review is directed to women’s desire to use the maternal health service as per the standard, which in turn can be used as framework to underpin strategies and programs that save the lives, promote well-being, improve health and survival, and reduce maternal, newborn, and child death
Context
The context for this review was low and middle income countries (LMICs) to widen the study coverage and generate strong evidences as their health care practices are almost similar.
Inclusion and exclusion criteria
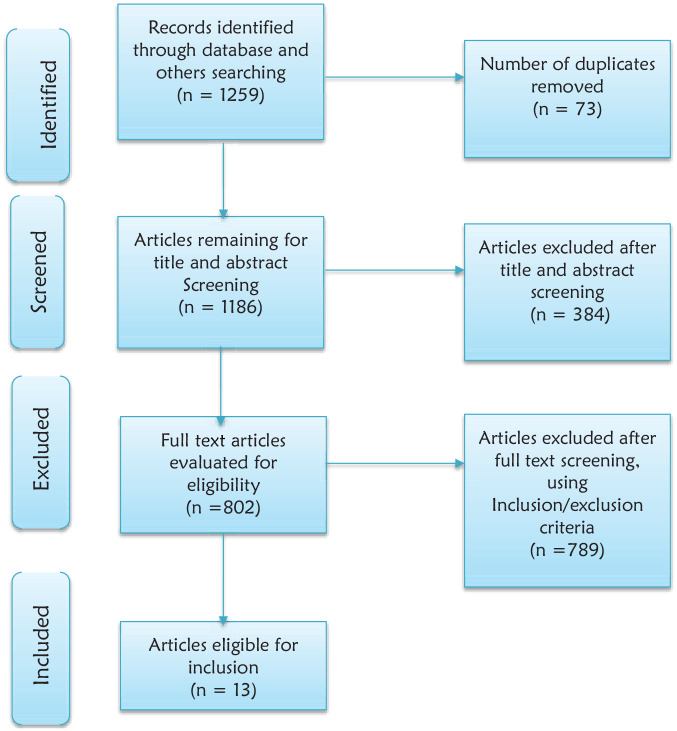
Any systematic review and primary studies evaluating continuum of care for maternal health care in LMICs, irrespective of their study design, reported in the English language published between 1 January 2000 and September 2019, given that the issue of MGD started in 2000 were considered for inclusion (Figure 1).
Figure 1.
Diagrammatic presentation of the procedure for selection of studies included to study the maternal health care in Low- and Middle-Income Countries.
Search strategy
A 3-step search strategy was used. An initial search of MEDLINE (via PubMed), Cochrane Library databases for relevant articles was followed by analysis of text words contained in the title and abstract, and index terms used to describe the article. Then, a second search was made using all the identified keywords; index terms, Truncation, Boolean operators, MeSH terms for MEDLINE across all databases included.
Thirdly, the reference list of all the studies, reports and articles were searched for additional studies. Four databases PubMed, Cochrane library, Google scholar and Google were used for searching to identify all the related articles and reports in LMICs. Titles and abstracts were examined for the following search terms” Patient Dropouts,” “Continuity of Patient Care,” “Maternal Health Services,” “Prenatal Care,” “Parturition,” “Postnatal Care,” and “Developing Countries.” The retrieved studies were exported into the reference manager 5.3, and duplicates were subsequently removed.
The search strategy identified; a total of 1259 articles from the 3 identified databases. After duplicates were removed 1186 records were left. Titles and abstracts were examined based on pre-determined criteria and 802 articles shortlisted for full text review. A total of 802 full text articles were screened independently by 2 reviewers based on inclusion criteria, eventually, 13 study articles were included in the final review.
Data extraction and analysis
The general characteristics of the included studies were summarized using the developed template and the themes in the articles that were aligned with the review objective. The template contained categories for descriptive characteristics of the included studies, like Author/s, Journal, year of publication, type of the study, study design, country of origin, rationale of the study, study population, sample size, outcomes of the study, key findings related to the review, limitations, and recommendations. This iterative process involved reading, annotating, highlighting and evaluating literature in the included studies (Table 1).
Table 1.
The characteristics of studies included to study maternal health care in Low- and Middle-Income Countries: A scoping Review.
| Author and year | Study area | Source of the data | Study design | Sample size | Findings related to the review % | Recommendations of the study | Limitations of the study | |||
|---|---|---|---|---|---|---|---|---|---|---|
| Any or ANC4+ | ANC4+ and SBA | ANC4+, SBA &PNC /CoC | ||||||||
| Wang and Hong17 | Cambodia | Secondary: CDHS 2010 | Cross-sectional | 6472 | 90 | 71 | 60 | Quality of ANC connected to SBAs and PNC | Using 48 h after delivery as the cutoff | |
| Yeji et al18 | Ghana | Primary | Cross-sectional | 1500 | 86 | NI | 8 | Other designs | CoC is measured based on women’s recall response | |
| Akinyemi et al19 | Nigeria | Secondary: NDHS 2013 | Cross-sectional | 20 467 | [Any] 60.6 | 22.5 | 11.4 | Further studies to fully understand why women do not complete the CoC | Reasons for dropout between delivery and sixth week of PNC as such data not collected in NDHS | |
| Iqbal et al20 | Pakistan | Secondary: PDHS | CB cross sectional | 5724 for 2006/7 | 28 | 20 | 15 | No causal relationships displayed because of nature of the design used | Lack of uniformity in variables, the information is based on self-reports and may be biased | |
| 7461 for 2012/13 | 38 | 32 | 27 | |||||||
| Singh et al21 | The nine MCH priority countries for USAID | Cross-sectional | 18 036 | Nine countries | 37.9 | 28.3 | 16.9 | Better future studies focus on which geographic or administrative areas need the most focus | Not possible to study the quality of services, Study designs was subject to recall bias | |
| S. Asian | 38.8 | 29.2 | 24.5 | |||||||
| SSA | 37.5 | 28.0 | 13.9 | |||||||
| Mohan et al22 | Tanzania | Primary | Cross-sectional | 1931 | 66.5 | 65 | 10.3 | The status of CoC for MNCH services in a non-project setting | Not account for content delivered or quality of the content delivered and design | |
| Tamang23 | Nepal | Secondary: NMICS 2014 | Cross sectional | 2048 | NI | 53.1 | 45.7 | In-depth exploration of the barriers and community perceptions | ||
| Hamed et al24 | Egypt | Primary | Cross-sectional | 2790 | 90 | 85 | 50.4 | The information is based on self-reports | Study populations are rural women | |
| Kikuchi et al25 | Cambodia | Primary | Cross-sectional | 377 | 32.6 | 19.1 | 5 | Interventions or longitudinal studies | Selection bias, recall bias | |
| CSA and ICF et al26
(Unpublished) |
Ethiopian | Primary | CB cross sectional | 1281 | 39.9 | 31.1 | 12.1 | Improving early initiation and quality of ANC | Prone to recall bias as the data collected retrospectively | |
| Chaka et al27 | Ethiopia | Secondary: EDHS 2016 | CB cross sectional | 1342 | 31.8 | NI | 9.1 | Tracking the progress and factors influence completion of the CoC | Who died due to childbirth related complications were not included and recall bias | |
| Sakuma et al28 | Lao PDR | Primary | CB cross sectional | 263 | 54.4 | 30.4 | 6.8 | Promotion of early ANC and family [male] involvement | Deceased women were not included, information and recall bias | |
| Dereje et al (Unpublished) 29 | Ethiopia | Secondary: AMHDS | CB cross sectional | 438 | 25.2 | 18.5 | 9.7 | Early booking during antenatal period | Social desirability bias, selection bias, recall bias | |
Abbreviations: AMHDS, Arba Minch Health and Demographic Surveillance; CB, Community based; EDHS, Ethiopian Demographic Health Survey; Lao PDR, Lao People’s Democratic Republic: one of East Asia’s poorest; NI, Not indicated; NMICS, Nepal Multiple Indicator Cluster Survey; SBA, skilled birth attendance; The 9 MCH priority countries for USAID: Bangladesh, Nepal, Pakistan, Ethiopia, Malawi, Rwanda, Senegal, Tanzania, and Uganda.
Results
Descriptions of the studies
The review included studies from all regions in low- and middle-income countries [LMICs]. During the search process 1259 articles unique citations were identified. Finally, based on inclusion criteria 13 articles were retained for final review. The primary aim of this scoping review was to collate all the available evidence on the current status of continuum of care for maternal health care in low- and middle-income countries [LMICs]. Also, it thoroughly identified and summarized the existing literatures and characterized the evidences using the template developed for this purpose like: categories of available literatures, their study designs, country of origin, outcomes, key findings, limitations, and recommendations to organize the themes in the literatures that were aligned with the reviewing objective and to indicate the gaps that needs to be the forthcoming researcher focuses (Table 1) and the results were summarized under their themes as given below.
Descriptions of the included articles
As to the year of publication of the included articles (studies), it was between 2015 and 2019. More than half (53.8%) of them were from African countries and further analysis from countries’ Demographic Health Survey [DHS]. All of the studies were quantitative in type and cross-sectional study by design.
Service utilization level
The proportion of women who received antenatal care, delivered by skilled birth attendants/institutional delivery and postnatal care differed across the countries. The general trend shows a decline in use of services as women move along the continuum of care from pregnancy to childbirth and postnatal care and the highest gap was sensed between institutional delivery and postnatal utilization.
The completion status was paradoxical and varies from country to country. For instance, 60% in Cambodia during the 2010 CDHS and 5% in Ratanakiri, Cambodia in 2015. However, none of the included studies considered the completion status of the 3 maternal health care utilization and birth outcomes.
Limitations of the included studies
The reported limitations of the included studies were differing from article to article and includes: the use of secondary data, maternal complications that could affect use of maternal care are not included, the precision of information on the content of maternal health care (subject to women’s misreport) and 48 hours after delivery used as the cutoff point (operationalization of variables). 28 Others highlighted as CoC services were measured based on women’s recall response, data on the location of respondents (rural/urban) and distance to a health facility, the reasons for dropout between delivery and sixth week PNC were not ascertained.18,19
As more than half of the studies were from the DHS data of the countries, the lack of uniformity in variables, study designs, self-reports, absence of information on the quality of care in the DHS data, the time-lag between use of services and date of survey may leads to recall bais, selection bais, social desirability, who died due to childbirth related complications were excluded, sample size, study population and not detecting causal relationship amongst reported limitations (Table 1).16,20-23,25-29,30
Recommendations of the included studies
Some of the included studies showed their recommendation explicitly while it was lacking in the other studies. And the informed recommendations were: further studies that take into account the missed variables like community and facility-level factors, working on quality of ANC, early booking for ANC, male involvement, utilization and birth outcome, other study design like cluster randomized trials and longitudinal, systematic review, conducting the study in a non-project setting, a qualitative study that relevant to social, cultural and economic factors, integration of the strategies, strengthening the health systems and community mobilization in general (Table 1).
Discussion
Antenatal care provides the best window of opportunity to promote maternal and child health service practice and the completion of maternal health care increases womens’ chances of better birth outcome but, many Ethiopian mothers deliver at home and fail to attend facility delivery and postnatal care after receiving antenatal care. 31
This review which included 13 articles published between 2015 and 2019 revealed more than half of them were from African countries and further analysis from countries’ Demographic Health Survey (DHS). All of the studies were quantitative in type and cross-sectional study by design. The completion status varied from country to country and ranges from, 60% in Cambodia and 5% in Ratanakiri. In Ethiopia it ranges from 9.1% to 12.1%.
This review included current literature/evidence from the DHS of several countries. Despite the strengths of the studies due to coverage of large population and inclusion of all regions within the countries, the data did not capture vital information such as location of the respondents, distance to the health facility, quality of services, the exact time of service utilization. Moreover they had the limitations of being descriptive and cross-sectional by design, and subject to respondents’ recall bias.9,17,21 Owing to all these limitations of the DHS, it was not possible to concluded the status of CoC for MHC as the DHS data fail to addresses the above mention points like: quality of services, the exact time of service utilization, women’s recall of events, which can be affected by the period of recall as well as the women’s situation at the time of the event and expect that women are more likely to misreport or misclassify events the earlier the birth occurred. May be the freely availability of the countries DHS data and resource limitation to conduct studies in large scale in low- and middle-income countries were the main reason why we enforced to calculate the completion rate using DHS with all its drawbacks.
Each element of the continuum of care for maternal health care provides essential and potentially lifesaving services and can be used to avert birth related complications. However, the completion status of the maternal health care was in paradoxical situation and varies from country to country. The greatest gap was detected between institutional delivery and postnatal care. Also, none of the retrieved literatures touched the completion status of continuum of care for maternal health care and birth outcomes which is among the indicators used to measure the quality of the rendered services for them particularly in regions of the world where the burden of maternal and newborn morbidity and mortality is higher. Moreover, despite the considerable emphasis to the completion of maternal health service utilization in almost all African countries, particularly in Ethiopia, the contributing factors and health behaviors of the mothers is still a budding and less understood area which needs further studies with strong design.
This review also toughs the limitations of the included studies and the reported limitations were different across the included studies and some of the studies had limitation related to the comprehensiveness of the variables, some were the effect of the time-lag between use of the services and date of survey, variables uniformity, selection bias, recall bias, social desirability, and study population, operationalization of variables, study designs and quantitativeness of the study. Even though, this review was limited to LMICs and few electronic databases, documentation of these problem was used to create the opportunity to designate researchers where the gaps were and where they have to emphasis in the for coming studies to fill the gaps.
Generally, knowing the limitations and recommendations of the existing literatures in this area help us to know what we have to take into account like: the missed variables, the service utilization, and birth outcome, systematic review to generate strong evidences, other study design like cluster randomized trials and longitudinal, qualitative studies to fill the indicated gaps to make the evidence in the indicated area more comprehensive.
Conclusion
Our scoping review provides a broad and a comprehensive review of current available literature on completion of maternal health service utilization. The status of completion of care for maternal health care is varies across the countries. Also, there is limited studies on the continuum of maternal health care and more than half of the studies on this area were from countries’ Demographic Health Survey and all of them were cross sectional by design.
Recommendation
Based on the summary of the review results, the reviewers recommend well-structured, comprehensive, and robust study designs such as RCT or longitudinal based primary research in the area to fill the indicated gaps and recommendation. Furthermore, studying the effect completion of maternal health service utilization on birth outcomes in regions of the world where the burden of newborn mortality is highest like Ethiopia vital.
Acknowledgments
We would like to express our very great appreciation to the team for their commitment and valuable contribution from the planning to the finalization of this work. Secondly, our appreciation extends to Jimma University, friends and family for their backing during this work.
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Availability of Data and Materials: The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Authors’ Contributions: SB, GT, MA, AK Protocol development, SB and AK searching, screening and full text evaluation for eligibility and data extraction and analysis, and all authors read and approved the final manuscript.
Ethics Approval and Consent to Participate: Manuscript has adhered to the ethical standards. However, consent to participate is not applicable.
ORCID iD: Sena Belina Kitila  https://orcid.org/0000-0003-1913-110X
https://orcid.org/0000-0003-1913-110X
References
- 1. Kerber KJ, de Graft-Johnson JE, Bhutta ZA, Okong P, Starrs A, Lawn JE. Continuum of care for maternal, newborn, and child health: from slogan to service delivery. Lancet. 2007;370:1358-1369. [DOI] [PubMed] [Google Scholar]
- 2. World Health Organization. A Policy Guide for Implementing Essential Interventions Maternal, Newborn and Child Health (RMNCH): a Multisectoral Policy Compendium for RMNCH. World Health Organization, 2014. [Google Scholar]
- 3. Sines BE, Tinker A, Ruben J. The Maternal–Newborn–Child Health Continuum of Care: A Collective Effort to Save Lives. Save the Children Population Rference Bureau, 2006. [Google Scholar]
- 4. Hogan MC, Foreman KJ, Naghavi M, et al. Maternal mortality for 181 countries, 1980-2008: a systematic analysis of progress towards Millennium Development Goal 5. Lancet. 2010;375:1609-1623. [DOI] [PubMed] [Google Scholar]
- 5. International Federation of Red Cross and Red Crescent Societies. Maternal, Newborn and Child Health Framework. 2013. [Google Scholar]
- 6. Kc A, Bhandari A, Pradhan YV, et al. State of maternal, newborn and child health programmes in Nepal: What May a continuum of care model mean for more effective and efficient service delivery? J Nepal Health Res Counc. 2011;9:92-100. [PubMed] [Google Scholar]
- 7. Owili PO, Muga MA, Chou YJ, Hsu YE, Huang N, Chien LY. Erratum to: associations in the continuum of care for maternal, newborn and child health: a population-based study of 12 sub-Saharan Africa countries. BMC Public Health. 2016;16:1064-1115. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Mohan D, LeFevre AE, George A, et al. Analysis of dropout across the continuum of maternal health care in Tanzania: findings from a cross-sectional household survey. Health Policy Plan. 2017;32:791-799. [DOI] [PubMed] [Google Scholar]
- 9. Yeji F, Shibanuma A, Oduro A, et al. Continuum of care in a maternal, newborn and Child Health Program in Ghana: low completion rate and multiple obstacle factors. PLoS One. 2015;10:e0142849-e0142849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Alva S, Wang W, Koblinsky M. The continuum of care for maternal and newborn health in south Asia: determining the gap and its implications. In: Paper Submitted to the Annual Meeting of the Population Association of America, Washington, DC, ICF International; 2011; 1–6. [Google Scholar]
- 11. Wang W, Hong R. Levels and determinants of continuum of care for maternal and newborn health in Cambodia-evidence from a population-based survey. BMC Pregnancy Childbirth. 2015;15:62-69. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Iqbal S, Maqsood S, Zakar R, Zakar MZ, Fischer F. Continuum of care in maternal, newborn and child health in Pakistan: analysis of trends and determinants from 2006 to 2012. BMC Health Serv Res. 2017;17:189-215. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Kafle RB, Dulal KP, Pandey KP. Continuum of Maternal Health Care and the Use of Postpartum Family Planning in Nepal. DHS Working Paper No. 133. Rockville, MD: ICF; 2017. [Google Scholar]
- 14. CSA (CSA) [Ethiopia] and I 2016. ED and HS, Addis Ababa, Ethiopia, and Rockville, Maryland UC. Central Statistical Agency (CSA) [Ethiopia] and ICF. Ethiopia Demographic and Health Survey 2016. CSA and ICF; 2016. [Google Scholar]
- 15. Ethiopian Public Health Institute (EPHI) [Ethiopia] and ICF. Ethiopia Mini Demographic and Health Survey 2019: Key Indicators. EPHI and ICF; 2019. [Google Scholar]
- 16. Munn Z, Peters MDJ, Stern C, Tufanaru C, McArthur A, Aromataris E. Systematic review or scoping review? Guidance for authors when choosing between a systematic or scoping review approach. BMC Med Res Methodol. 2018;18:143-147. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Wang W, Hong R. Completing the Continuum of Care for Maternal and Newborn Health in Cambodia: Who Drops Out? DHS Further Analysis Reports No. 85. ICF International; 2013. [Google Scholar]
- 18. Yeji F, Shibanuma A, Oduro A, et al. Continuum of Care in a Maternal, Newborn and Child Health Program in Ghana: Low Completion Rate and Multiple Obstacle Factors. PLoS ONE 2015;10(12): e0142849. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Akinyemi et al. Patterns and determinants of dropout from maternity care continuum in Nigeria. BMC Pregnancy and Childbirth 2016;16: 282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Iqbal S, Maqsood S, Zakar R, et al. Continuum of care in maternal, newborn and child health in Pakistan: analysis of trends and determinants from 2006 to 2012. BMC Health Services Research 2017;1-15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Singh K, Story WT, Moran AC. Assessing the continuum of care pathway for maternal health in South Asia and Sub-Saharan Africa. Matern Child Health J. 2016;20:281-289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Mohan D, Lefevre AE, George A, Mpembeni R, Bazant E, Rusibamayila N, et al. Analysis of dropout across the continuum of maternal health care in Tanzania: findings from a cross-sectional household survey. Health Policy Plan 2017;March:791–9. [DOI] [PubMed] [Google Scholar]
- 23. Tamang TM. Factors Associated with Completion of Continuum of Care for Maternal Health in Nepal. Int J Prev Med. 2017;1–23.28217263 [Google Scholar]
- 24. Hamed AF, Roshdy E, Sabry M. Egyptian status of continuum of care for maternal, newborn , and child health: Sohag Governorate as an example. International Journal of Medical Science and Public Health 2018;7(6):417–26. [Google Scholar]
- 25. Kikuchi K, Yasuoka J, Nanishi K, Ahmed A, Nohara Y, Nishikitani M, et al. (2018) Postnatal care could be the key to improving the continuum of care in maternal and child health in Ratanakiri, Cambodia. PLoS ONE 13(6): e0198829. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. Central Statistical Agency (CSA) [Ethiopia] and ICF. 2016. Ethiopia Demographic and Health Survey 2016. Addis Ababa, Ethiopia, and Rockville, Maryland, USA: CSA and ICF. [Google Scholar]
- 27. Chaka EE, Parsaeian M, Majdzadeh R. Factors associated with the completion of the continuum of care for maternal, newborn, and child health services in Ethiopia. Multilevel model analysis. Int J Prev Med 2019;10:136. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28. Sakuma S, Yasuoka J, Phongluxa K, Jimba M. Determinants of continuum of care for maternal, new born, and child health services in rural Khammouane, Lao PDR. PLoS ONE 2019;14(4) : e0215635. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Haile Dereje, Kondale Mekdes, Andarge Eshetu, Tunje Abayneh, Fikadu Teshale, Boti Nigussie. Level of completion along continuum of care for maternal and child health services and factors associated with it among women in Arba Minch Zuria Woreda, Gamo Zone, Southern Ethiopia: a community based cross-sectional study. PLoS ONE 2020;15(6):e0221670. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30. Singh Kavita, Story William T., Moran Allisyn C.. Assessing the Continuum of Care Pathway for Maternal Health in South Asia and Sub-Saharan Africa. Matern Child Health J. 2016;20(2):281–289. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Fekadu GA, Ambaw F, Kidanie SA. Facility delivery and postnatal care services use among mothers who attended four or more antenatal care visits in Ethiopia: further analysis of the 2016 demographic and health survey. BMC Pregnancy Childbirth 2019;19:64-69. [DOI] [PMC free article] [PubMed] [Google Scholar]