Abstract
Background
Although previous evidence confirms the effects of sleep deprivation on mental health and wellbeing, due to the interaction effects of sleep and mood on each other, the influence of sleep improvement has received less attention.
Objective
This study aimed to find whether binaural beat technology can enhance sleep quality and thus post-sleep mood.
Methods
Twenty healthy students participated in this pilot study. All subjects were investigated for two weeks (a baseline week and an experimental week). In the first week, there was no intervention, but in the second week, all subjects were exposed to a 90 min binaural beat in the delta frequency range. The individuals’ sleep was monitored for two weeks using a sleep diary form, and a Profile of Mood State questionnaire was employed to assess their mood at the end of the first and second weeks.
Results
Auditory stimulation with delta binaural beat enhanced sleep parameters such as sleep failure, the number of awakenings, real duration of sleep, sleep quality, and feeling following the waking of the individuals. Finally, students’ moods improved by reducing anxiety and anger, but other mood parameters did not indicate a significant difference.
Conclusion
The findings of this study confirmed that auditory stimulation with a delta binaural beat seems to be a low-cost and alternative method for medicine and other treatment methods with side effects.
Application
This study demonstrates the use of technology with a neuroergonomics approach to improve sleep and mood disorders.
Keywords: Brainwave entrainment, neurostimulation, mental state, sleepness, sleep quality
Precision
The quantity and quality of sleep were improved in this study as a result of auditory stimulation with delta binaural beat. Participants also had a better post-sleep mood, along with a significant reduction in anxiety and anger; in addition, they were more satisfied with their sleep and reported feeling better afterward.
Introduction
Sleep disorders and poor sleep quality are extremely common and linked to a wide range of physical and mental health issues. 1 Sleep is believed to be a predictor of the next day's mood.2,3 On the other hand, sleep deprivation causes mood disturbances, which are characterized by increased fatigue and decreased energy, alertness, and memory, as well as an increase in negative components such as stress, depression, frustration, and uncertainty.4–6 Mood disturbances are often thought to be the primary symptoms of mental health disorders such as depression and anxiety.7–9
According to previous research, sleep difficulties occur in all age groups, including the elderly and adolescents. 10 Further, Pagel 11 discovered that 69.7% of students with poor GPAs had difficulties falling asleep in a study on sleep and waking habits. Furthermore, 65.6% of the most recent group indicated that they walk constantly at night because they cannot sleep, and 72.7% of those with poor sleep quality expressed difficulties concentrating and paying attention during the day.
In addition, many students experience difficulty with sleep initiation, sleep maintenance, morning fatigue, everyday sleepiness, and nightmares, as well as waking up earlier than usual in the morning. 12 Insufficient sleep and sleep deprivation cause neurological, behavioral, and physiological changes. 13 It is associated with academic failure and reduced normal daily performance in students’ classrooms, 14 keeps them from attending classes or makes them drowsy in class; 15 moreover, it induces fatigue and discomfort during the day 16 and causes or worsens stress and anxiety symptoms in students. 17 Considering that sleep deprivation or poor sleep quality and mental health affect each other, improving students’ sleep quality is an important factor in their overall mental health. 18
The use of self-care techniques by individuals to enhance their sleep at home is one study topic, which has been examined on insomnia. According to numerous studies, the use of brainwave entrainment by light or sound stimulation is an intervention that shows good benefits in treating diseases such as cognitive function, headache/migraine, and premenstrual syndrome and promoting relaxation and recovery.19–22 Although the impact of auditory stimulation on sleep improvement has not been well investigated yet, 23 evidence suggests that it can be utilized to help sleep.24,25
Auditory beats that are monaural (e.g. physical beats to both ears) or binaural (different sinusoidal waves with similar frequencies presented to each ear separately) are new instruments in the non-invasive method.26,27
When two sound waves are simultaneously applied to two nearby frequencies in the left and right ears, the brain can recognize the frequency difference between the two sounds. 28 Furthermore, a virtual third wave is perceived by the brain as a binaural beat with the frequency difference between the two sounds.29–31 For instance, when a sinusoidal 250-Hz pure tone is supplied to the left ear and a 256-Hz tone is simultaneously presented to the right ear, the brain perceives an amplitude variation with a frequency rate of 6 Hz. 28
As a result, different studies have focused on the psychological effects of the binaural beats of various frequencies and reported substantial evidence in this regard.32–35 Consequently, the impact of binaural beats on the anxiety score has been identified in several studies. For example, in patients suffering from anxiety, the use of delta-frequency binaural beats resulted in a reduction in anxiety after the intervention. 36 In addition, daily use of binaural beats reduced anxiety in patients with mild anxiety disorders in the beta/delta range. 37 Another research demonstrated that using the 2.5-Hz delta binaural beat for 40 min decreased anxiety in healthy participants. 38 Additionally, it was shown that theta binaural beat can suppress stress and anxiety prior to surgery, 36 and beta binaural beat can improve alertness. 39 Recent research has also represented that beta binaural beat enhances word recognition and has an effect on long-term memory, 40 while gamma binaural beat could improve short-term memory. 41
The physical sleep process may be established by objective indicators; however, the subjective impression is a highly significant factor in sleep quality assessment.42,43 Although several studies have confirmed that using binaural beats decreases anxiety and other negative emotions, few studies have examined the effect of this intervention on the delta frequency (3 Hz) during sleep. Accordingly, the current study sought to investigate whether the sleep quality of students can be improved by a 3 Hz binaural beat and whether this leads to the enhancement of the post-sleep state.
Methods
Participants
Twenty healthy students (10 females and 10 males aged 20–30 years) were voluntarily included in this pre-experimental study. The required sample size was determined based on an expected effect size of sleep quality levels and mood post-intervention. de Niet et al. 44 conducted a meta-analysis and suggested that the music intervention has a moderate effect on sleep quality in five RCTs, and this sample size was appropriately powered to detect a medium effect size. In another study by Abeln et al., 42 higher subjective ratings of sleep and awakening quality, sleepiness, and motivational state were obtained during eight weeks of brainwave entrainment among 18 young sub-elite male soccer players.
The study population consisted of non-dormitory college students of three graduate classes of Tehran University of Medical Sciences who met the study requirements. The inclusion criteria included being 30 years or younger, having no insomnia, poor sleep quality, or other sleep-related problems (It was evaluated with PSQIa and ISIb questionnaires with a score of ISI<7 and PSQI<5), and having no current or past depression and history of psychiatric disorders. Only younger students were investigated in this study because there is a difference between old and young individuals regarding sleep quality that influences their behavioral and mood responses in different situations. On the other hand, the exclusion criteria were medicine consumption and certain medical conditions impairing sleep or state of awareness. All participants were requested to have a consistent sleep schedule throughout the research and avoid alcoholic and caffeinated beverages 24 and 12 h before the test, respectively.
Ethical considerations
The study was approved by the Ethics Committee of Tehran University of Medical Sciences. The purpose of the study was explained to the participants, and they were requested to sign a permission form.
Procedure
First, each participant was requested to complete the demographic information questionnaire, PSQI, and ISI in order to assess their history of insomnia, poor sleep quality, or other sleep disorders, as well as mental problems. ISI and PSQI are self-assessment instruments that evaluate insomnia symptoms and their negative effects on people's lives over the previous two weeks, 45 while PSQI investigates sleep quality and disturbances over a month. 46 All participants were trained on sleep hygiene and asked to follow it during the study.
This study was conducted over two consecutive weeks, corresponding to baseline and interventional weeks. There was no intervention during the first week (baseline) to assess the status of each person's sleep parameters and mood prior to the intervention. Then, participants were given a piece of binaural beat music to listen to for the next one week of the intervention phase. A sleep diary and the Profile of Mood State (POMS) were used during these two weeks. They were told when and how to complete the required questionnaires.
For two weeks, Sleep Diary Questionnaire was daily answered shortly after waking up (about 30–60 min) within an individually set time period. The timeframe was assigned to standardize the time and conditions for answering questions. Participants were asked to complete the POMS questionnaire on two nights, one week apart, at the end of the first (before the intervention) and second (after the intervention) weeks.
The Sleep Diary is a revised version of Morin's Sleep Diaries; 47 it is a popular technique for collecting sleep data and contains questions about the quantity and quality of sleep the night before, including going to bed time, inability to start sleeping (the time it takes for a person to fall asleep), and the number of times they wake up during the night. This allows us to estimate the duration of actual sleep (the amount of time the patient feels “truly” sleeping), the feeling after waking up, and the sleep quality; the answers to these items are rated on a scale ranging from extremely terrible to great.
The POMS was first designed by McNair et al. in 1981 to detect instantaneous mood disorders, and is now used to measure the strength of each of the described sub-scales. This questionnaire contains 65 items that are answered on a 5-point scale (“0 = Not at all” to “4 = Very strong”) for the period of the “past week, including today” and belonging to scales such as anxiety, depression, anger, vigor, fatigue, and confusion. 48 Six scores are derived from the questionnaire, one for each of the six mood states. To determine the total number of mood disorders, the scores of the five negative mood components (i.e. depression, anxiety, fatigue, confusion, and anger) should be added, followed by subtracting the positive mood factor score (vigor). A high score indicates a negative mood linked to behaviors such as anxiety, anger, depression, and other unpleasant emotions, whereas a low number represents a positive mood. 49 In a study conducted in Iran, the reliability coefficient of this questionnaire was in the range of 0.69–0.84. 50
The stimulus in this investigation was a 3-Hz binaural beat on a 174-Hz carrier tone that was created specifically for the study by Audacity software. A tone of 174 and 177 Hz were played in the left and right ear, respectively. Considering that the threshold of auditory stimulation during sleep is 60 dB SPL, 51 the binaural beat was set between 60 and 75 dB SPL with a sound level meter at the individual's ear. These levels were marked, and individuals selected their most comfortable volume within this range (The majority of people chose 60 dB). Considering that the average time to complete a regular sleep cycle is 90 min, 52 this frequency was also provided for 90 min. Participants were informed to listen to music before going to bed and turn down the volume to a comfortable level so that not to disturb them. It was impossible to stop the music by lowering the volume since it is known that the binaural beat is felt even when the signal is below the threshold of hearing.26,42 They were told to use stereo headphones to listen to music while lying down and relaxing, with their eyes closed and the lights turned out.
Data analysis
The data were analyzed using the SPSS22 statistical software. The percentage and frequency, as well as mean and standard deviation (SD) were utilized to express qualitative and quantitative data, respectively. For all tests, the significance level was set at 0.05. The paired t-test (for data with normal distribution) and Wilcoxon test (for data with abnormal distribution) were used to determine the effect of binaural beats on moods before and after the intervention. The normality of the data distribution was confirmed by Smirnov Kolmogorov and Shapiro–Wilk tests. The mean score of each component of the POMS questionnaire and its overall score had a normal distribution when using this test.
Results
Twenty-four healthy students were chosen for this investigation although four people were removed from the study (due to not attending the study during the intervention phase), and eventually, the data of twenty people underwent analysis. Subjects’ demographic and baseline data are summarized in Table 1. Only 20% of the subjects had a history of smoking but none of them were current smokers. Female students made up 50% of the study population.
Table 1.
Demographic and baseline data for all subjects of the study.
| Parameter | (Mean ± SD) |
|---|---|
| Age | 27.5 ± 2.5 |
| BMI (kg/m2) | 24.3 ± 1.9 |
| ISI score | 6.9 ± 2 |
| PSQI, overall score | 4 ± 1.6 |
The results of this study are divided into primary and secondary outcomes. The primary outcomes (for assessing the sleep quality of participants) were evaluated using the Sleep Diary Questionnaire and sleep parameters. However, the secondary outcomes (for evaluating the mood of the subjects) were assessed by the POMS questionnaire, and the parameters of anxiety, depression, anger, vigor, fatigue, and confusion were examined, the results of both are described in detail as follows.
Sleep parameters
All sleep parameters without and with the intervention are provided in Table 2. The mean differences in these sleep parameters were investigated by an independent t-test. The mentioned parameters were compared for differences between the first and second weeks. The comparison of the parameters of the sleep diary before to during the intervention revealed significant changes. The results showed that the average duration of sleep latency and the number of awakenings during the night for a week of utilizing binaural beat by the intended subjects were significantly shorter compared to those who did not utilize any sound before retiring to sleep on the first week (P < 0.001). The mean duration of actual night sleep and waking time in the morning was significantly longer in the second week in comparison to the first week with intervention (P < 0.001). The Sleep Diary Questionnaire asked participants to rate their sleep quality and how they felt after waking up on a scale of very bad to excellent, thus the findings indicated that the frequency of sleep quality and how they felt after waking up were significantly different before and after the intervention (P < 0.001). When employing the binaural beat, the majority of the samples (70%) described their sleep quality as good to excellent, and their feeling after waking up (80%) was rated as good to very good.
Table 2.
Mean and standard deviation of sleep parameter on the first (without intervention) and second week (with intervention) and the result of paired t-test on sleep diary parameter.
| Parameter | Without intervention | With intervention | Paired t-test | |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | P-value | |
| Time standing up | 6.15 ± 0.74 | 6.55 ± 0.81 | −0.4 ± 0.77 | <0.001 |
| Sleep latency | 19.1 ± 4.15 | 7.23 ± 2.9 | 11.8 ± 3.13 | <0.001 |
| Number of awaking | 2.06 ± 0.73 | 1.06 ± 0.65 | 1 ± 0.69 | <0.001 |
| Total sleep time | 6.05 ± 0.91 | 7.3 ± 0.85 | −1.25 ± 1.28 | <0.001 |
Mood state
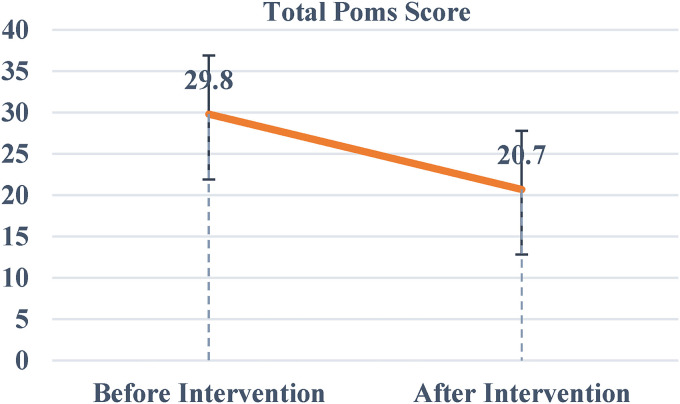
Based on the results (Figure 1), the mean (SD) of the overall Mood State Questionnaire score was 29.8 + 7.1 and 20.7 + 7.9 on the first (without intervention) and second (with intervention) night, respectively. The total mood state scoring before and after the intervention differs significantly at P = 0.006. Table 3 presents the mean (SD) of six POMS subcomponents before and after the intervention.
Figure 1.
The mean and standard deviation of the total POMS questionnaire score on the first (before intervention) and second night (after intervention).
Table 3.
Mean and standard deviation of POMS components first (without intervention) and second night (with intervention) and the results of a paired t-test on the mean total score of mood and its sub-components before and after intervention.
| Parameter | First night | Second night | Paired t-test | |
|---|---|---|---|---|
| Mean ± SD | Mean ± SD | Mean ± SD | P-value | |
| Anxiety | 9.8 ± 2.6 | 8 ± 2 | 1.8 ± 1.9 | 0.019 |
| Depression | 10.5 ± 2.2 | 9.6 ± 3.2 | 0.9 ± 2.37 | 0.262 |
| Anger | 8.4 ± 2.1 | 6.4 ± 1.8 | 2 ± 2.30 | 0.023 |
| Vigor | 15.8 ± 3.2 | 18 ± 3.3 | −2.2 ± 3.36 | 0.068 |
| Fatigue | 7.9 ± 2.9 | 6.6 ± 1.8 | 1.3 ± 2.86 | 0.186 |
| Confusion | 9 ± 2 | 8.1 ± 2.6 | 0.9 ± 2.07 | 0.204 |
| Total score | 29.8 ± 7.1 | 20.7 ± 7.9 | 9.1 ± 8.08 | 0.006 |
The statistical analysis of individual mood subcomponents indicated that only anxiety and anger differences were significant (P = 0.019 and P = 0.023) both before and post-intervention. However, despite a reduction in the other negative components and an increase in the positive component (vigor), there was no statistically significant difference between depression, vigor, fatigue, and confusion before and after the intervention (Table 3).
Discussion
The influence of delta binaural beat technology on the sleep and post-sleep mood of students was investigated in this pilot study. The findings revealed that the applied binaural beat enhanced sleep diary sheet factors such as sleep failure, the number of awakenings throughout the night, real duration of sleep, sleep quality, and feeling following the waking of the individuals. Therefore, in comparison to the first week without stimulation, all sleep parameters showed a significant improvement due to stimulation in the second week. These results are in line with those of previous studies on the use of auditory stimulation to improve sleep problems. For instance, Zhou et al. 53 found that the use of pink noise had a significant impact on enhancing sleep quality by increasing maintained time. Likewise, Golroo et al. 54 reported that using pink noise enhances the length of deep sleep and thus improves sleep stability and quality.
The findings of this study also confirmed that individuals reported enhanced quality sleep and increased sleep satisfaction after one week of using delta binaural beats. These data could point to an increase in delta activity due to brainwave entrainment during the night, and eventually better sleep. Delta activity has a frequency of 3 Hz, and the applied binaural beat in this study had a frequency of 3 Hz as well. However, more extensive research and recording of brain wave activities during stimulation are required, and it is advised that this issue be addressed in future studies.
On the other hand, studying the mood states both before and after a delta binaural beat intervention demonstrated that after the intervention, participants had a lower overall mood score than before, indicating that they had a better mood after utilizing the delta binaural beat. In addition, a decrease in the mean score values of all negative mood components (e.g. anxiety, depression, anger, fatigue, and confusion), while an increase in the mean value of the vigor score (a positive component of mood) was observed in the one-to-one review of the mood components after the intervention compared to before the intervention (Table 3). This implies that people generally had less anxiety, depression, anger, fatigue, and confusion after the intervention and had a greater sense of vigor.
The statistical examination of the data indicated that despite a decrease in the negative components and an increase in the positive component, this change was statistically significant only in the total score of mood (P = 0.006), anxiety (P = 0.019), and anger (P = 0.023), while it was not significant in the other components. In contrast, the results of the present investigation on anxiety reduction due to the application of binaural beats are consistent with those of Wahbeh et al. (2007) and Jirakittayakorn and Wongsawat (2017). In the study by Wahbeh et al., 55 anxiety levels decreased with the delta binaural beat after the procedure. Similarly, Jirakittayakorn and Wongsawat 33 found a significant reduction in stress and anxiety following the usage of the binaural beat. The total mood score in the current study also decreased significantly, which is in accordance with the findings of Young, 56 representing that using binaural beats resulted in relaxation. Likewise, Vera Ablen concluded that using binaural beats improved participants’ psychological states. 42 Owens et al. 57 also found that increasing sleep duration improved sleep quality and thus lowered mood problems in a group of teenagers.
Therefore, by a significant decrease in the overall score of mood, anxiety, and anger in this study, the usage of delta binaural beats could generally enhance people's mood and thus reduce their anxiety and anger. Anxiety and anger can be easily changed by this intervention because they can be caused by minor daily situations. However, for other characteristics such as depression, there may be many chronic aspects that, while reduced, have not been able to show a significant difference under the influence of our short-term intervention. As a result, this intervention may have an impact on other parameters over a longer period of time, which should be considered in future investigations.
Considering that sleep deprivation, low quality of sleep, and mental health have an impact on each other, the improvement of the quality of sleep for students is a major component of mental health. 18 Sleep has an impact on brain function, mood, and overall wellness. According to studies, students with mood disorders such as depression had lower sleep quality, delayed initiation of sleep, and frequent nighttime awakenings. Low sleep quality in students is also connected with sadness, anger, irritability and fatigue symptoms, and negative moods. 58 Researchers at the University of Pennsylvania discovered that persons who were deprived of sleep had higher levels of stress, anger, sadness, anxiety, and confusion, but their mood considerably improved following a period of normal sleep. 59
Many studies have evaluated the influence of auditory stimulation with binaural beats, white noise, pink noise, and other noises on sleep quality and mood, either concurrently or individually. In the study by LaAnne et al. 60 on college students, the rate of sleep latencies, as well as night wake-up and general sleep issues decreased when students used white noise each night. The use of binaural beats increased athletes’ sleep quality and post-sleep mood in a trial by Vera Ablen. 42 As a consequence, the findings of previous studies on sleep parameters are compatible with those of the current study. The use of delta binaural beats in this trial, as in other investigations, resulted in a reduction in sleep onset latency, a decrease in the frequency of nighttime awakenings, and an improvement in real sleep length. In addition, the subjects’ sleep quality and feelings after waking up represented an improvement. Overall, it was demonstrated that using the delta binaural beat can improve students’ sleep and mood.
Listening to binaural beats seems to be a relatively safe, simple, and flexible technique for altering or enhancing the function of the brain. Contrarily, Wahbeh et al. 55 reported the adverse side effects of listening to binaural beats for 60 days according to subject interviews, although safety was informally assessed, and long-term safety issues were not taken into consideration.
However, reports on the side effects of using binaural beats are extremely rare, and there have been no reported dangers during controlled studies. The most dangerous thing about binaural beats is the same as listening to too loud music. Listening to sound for a long period of time at or above 85 decibels may cause hearing loss in the long term. 61 Similarly, evidence exists on potential unwanted side effects in this regard. For example, some studies reported that the repetitive and unnatural sound of the binaural beat could make people feel uncomfortable.62,63 In addition, binaural beats seem to feel uncomfortable in the sense that repeated auditory stimuli cause anxiety and depression. 64 However, a limited body of research has focused on the relationship between binaural beats and subjective emotions.30,65 In the present study, no side effects were reported by participants, and people did not feel uncomfortable hearing the binaural beat.
According to these results, using delta binaural beats may improve mood and relaxation by reducing anxiety and anger in a person since other mood parameters did not indicate a significant difference. This is most likely due to the small sample size and a short period of intervention. Furthermore, future research should focus on the impact of this intervention on a larger population. Finally, it is ideal for individuals to use a binaural beat for a longer period of time (e.g. one month) in order to estimate its long-term effect.
Conclusion
Based on the findings of this pilot study, auditory stimulation with a delta binaural beat could enhance sleep and mood state. In other words, the usage of delta binaural beats, as well as the influence of one's sleep may affect people's moods. This implies that utilizing the delta binaural beat on the night of the intervention generated a state of calm, which resulted in a reduction in anxiety and anger, as well as a better overall mood. On the other hand, the effect of this intervention on sleep represents that falling asleep early and getting a full night's sleep, as well as reducing the number of nighttime awakenings will result in a better mood and less anxiety and anger.
Considering that sleep quality and mood improve each other, boosting sleep quality and quantity and hence reported mood in this study indicates that delta binaural beats can affect sleep and post-sleep mood. As a result, it seems that this technology can be used to improve conditions such as insomnia, frequent night awakenings, anxiety, and general mood and introduced as an alternative to costly procedures or pharmaceuticals with numerous adverse effects. However, it should be noted that consistent use over a long period of time is required for achieving such benefits. Auditory stimulation with a delta binaural beat during sleep appears to be a beneficial approach for supporting and improving students’ sleep quality in a non-invasive, time-saving, and comfortable method. The primary evidence and approach for future elaborations are provided within this pilot study.
Key point
Delta binaural beat causes people to fall asleep earlier, wake up less during sleep, and getting a full night's sleep.
People will feel better after sleeping with delta binaural beats since they will be more satisfied with their sleep.
An increase in sleep quality can help to improve mood.
Getting a good night's sleep should lower anxiety and make people feel less angry.
Acknowledgments
The authors express their gratitude to Tehran University of Medical Sciences, as well as all volunteered students for their trust, involvement, and time.
Conflict of interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: The study was approved by the ethics committee of Tehran University of Medical Sciences.
Funding: The authors disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was funded by Tehran University of Medical Sciences.
ORCID iD: Roya Dabiri https://orcid.org/0000-0002-9868-007X
Notes: a. Pittsburgh Sleep Quality Index. b. Insomnia Severity Index.
References
- 1.Foley D, Ancoli-Israel S, Britz P, et al. Sleep disturbances and chronic disease in older adults: results of the 2003 national sleep foundation sleep in America survey. J Psychosom Res 2004; 56: 497–502. [DOI] [PubMed] [Google Scholar]
- 2.Blaxton JM, Bergeman CS, Whitehead BR, et al. Relationships among nightly sleep quality, daily stress, and daily affect. Gerontology 2017; 72: 363–372. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Totterdell P, Reynolds S, Parkinson B, et al. Associations of sleep with everyday mood, minor symptoms and social interaction experience. Sleep 1994; 17: 466–475. [DOI] [PubMed] [Google Scholar]
- 4.Bonnet MHJS. Effect of sleep disruption on sleep, performance, and mood. Sleep 1985; 8: 11–19. [DOI] [PubMed] [Google Scholar]
- 5.Brendel DH, Reynolds C, III, Jennings J, et al. Sleep stage physiology, mood, and vigilance responses to total sleep deprivation in healthy 80-year-olds and 20-year-olds. Psychophysiology 1990; 27: 677–685. [DOI] [PubMed] [Google Scholar]
- 6.Reynolds CF, III, Kupfer DJ, Hoch CC, et al. Sleep deprivation in healthy elderly men and women: effects on mood and on sleep during recovery. Sleep 1986; 9: 492–501. [DOI] [PubMed] [Google Scholar]
- 7.Chung K-F, Cheung M-MJS. Sleep-wake patterns and sleep disturbance among Hong Kong Chinese adolescents. 2008; 31: 185–194. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Pandina GJ, Garibaldi GM, Revicki DA, et al. Psychometric evaluation of a patient-rated most troubling symptom scale for depression: findings from a secondary analysis of a clinical trial. Int Clin Psychopharmacol 2010; 25: 51–59. [DOI] [PubMed] [Google Scholar]
- 9.Zimmermann TM, Clouth J, Elosge M, et al. Patient preferences for outcomes of depression treatment in Germany: a choice-based conjoint analysis study. J Affect Disord 2013; 148: 210–219. [DOI] [PubMed] [Google Scholar]
- 10.Mousavi F, Golestan B. Insomnia in the elderly population: a study in hospital clinics of Tehran, Iran. J Sleep Res 2009; 18: 481–482. [DOI] [PubMed] [Google Scholar]
- 11.Pagel JF, Kwiatkowski C. Sleep complaints affecting school performance at different educational levels. Front Neurol 2010; 1: 125. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Eller T, Aluoja A, Vasar V, et al. Symptoms of anxiety and depression in Estonian medical students with sleep problems. Depress Anxiety 2006; 23: 250–256. [DOI] [PubMed] [Google Scholar]
- 13.Simpson N, Dinges DF. Sleep and inflammation. Nutr Rev 2007; 65: S244–S252. [DOI] [PubMed] [Google Scholar]
- 14.Ng E, Ng D, Chan C. Sleep duration, wake/sleep symptoms, and academic performance in Hong Kong secondary school children. Sleep Breathing 2009; 13: 357–367. [DOI] [PubMed] [Google Scholar]
- 15.Lund HG, Reider BD, Whiting AB, et al. Sleep patterns and predictors of disturbed sleep in a large population of college students. J Adolescent Health 2010; 46: 124–132. [DOI] [PubMed] [Google Scholar]
- 16.Forquer LM, Camden AE, Gabriau KM, et al. Sleep patterns of college students at a public university. J Am Coll Health 2008; 56: 563–565. [DOI] [PubMed] [Google Scholar]
- 17.Fernández-Mendoza J, Vela-Bueno A, Vgontzas AN, et al. Nighttime sleep and daytime functioning correlates of the insomnia complaint in young adults. J Adolesc 2009; 32: 1059–1074. [DOI] [PubMed] [Google Scholar]
- 18.Momayyezi M. Relationship between quality of sleep and mental health in female students of Shahid Sadoughi university of medical sciences (2015). J Fund Mental Health 2017; 20: 167–171. [Google Scholar]
- 19.Budzynski T, Budzynski H, Sherlin L, et al. Audio-Visual Stimulation: Research and Clinical Practice. 2011: 137–153.
- 20.Collura TF and David Siever CET. Auditory-vsual entrainment in relation to mental health and EEG. New York, NY: Academic, 2009, pp. 195–225. [Google Scholar]
- 21.Tang H-Y. Academic performance: A new look at physiological and psychosocial factors. University of Washington, 1998.
- 22.Teplan M, Krakovska A, Štolc SJIjop. EEG Responses to long-term audio–visual stimulation. 2006; 59: 81–90. [DOI] [PubMed] [Google Scholar]
- 23.Tang H-Y, Vitiello MV, Perlis M, et al. A pilot study of audio–visual stimulation as a self-care treatment for insomnia in adults with insomnia and chronic pain. Appl Psychophysiol Biofeedback 2014; 39: 219–225. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Rhodes LJH-SJ. Use of the hemi-sync super sleep tape with a preschool-aged child. Hemi-Sync 1993; 11: 4–5. [Google Scholar]
- 25.Wilson E. Preliminary study of the Hemi-Sync sleep processor. Colorado Association for Psychophysiologic Research, 1990.
- 26.Oster GJSA. Auditory beats in the brain. Sci Am 1973; 229: 94–103. [DOI] [PubMed] [Google Scholar]
- 27.Schwarz DW, Taylor PJCN. Human auditory steady state responses to binaural and monaural beats. Clin Neurophysiol 2005; 116: 658–668. [DOI] [PubMed] [Google Scholar]
- 28.Oster G. Auditory beats in the brain. Sci Am 1973; 229: 94–103. [DOI] [PubMed] [Google Scholar]
- 29.Lavallee CF, Koren SA, Persinger M, et al. A quantitative electroencephalographic study of meditation and binaural beat entrainment. J Altern Complement Med 2011; 17: 351–355. [DOI] [PubMed] [Google Scholar]
- 30.Perez HDO, Dumas G, Lehmann AJE. Binaural beats through the auditory pathway: from brainstem to connectivity patterns. Eneuro 2020; 7. doi: 10.1523/ENEURO.0232-19.2020 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Tang H-YJ, Vitiello MV, Perlis M, et al. Open-loop neurofeedback audiovisual stimulation: a pilot study of its potential for sleep induction in older adults. Appl Psychophysiol Biofeedback 2015; 40: 183–188. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Garcia-Argibay M, Santed MA, Reales J. Binaural auditory beats affect long-term memory. Psychol Res 2019; 83: 1124–1136. [DOI] [PubMed] [Google Scholar]
- 33.Jirakittayakorn N, Wongsawat Y. Brain responses to a 6–Hz binaural beat: effects on general theta rhythm and frontal midline theta activity. Front Neurosci 2017; 11: 365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Reedijk SA, Bolders A, Hommel B. The impact of binaural beats on creativity. Front Hum Neurosci 2013; 7: 786. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Walker MP, van Der Helm E. Overnight therapy? The role of sleep in emotional brain processing. Psychol Bull 2009; 135: 731. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Padmanabhan R, Hildreth A, Laws D. A prospective, randomised, controlled study examining binaural beat audio and pre-operative anxiety in patients undergoing general anaesthesia for day case surgery. Anaesthesia 2005; 60: 874–877. [DOI] [PubMed] [Google Scholar]
- 37.Le Scouranec R-P, Poirier R-M, Owens JE, et al. Use of binaural beat tapes for treatment of anxiety: a pilot study of tape preference and outcomes. Altern Ther Health Med 2001; 7: 58. [PubMed] [Google Scholar]
- 38.Wahbeh H, Calabrese C, Zwickey H. Binaural beat technology in humans: a pilot study to assess psychologic and physiologic effects. J Alternat Complement Med 2007; 13: 25–32. [DOI] [PubMed] [Google Scholar]
- 39.Lane JD, Kasian SJ, Owens JE, et al. Binaural auditory beats affect vigilance performance and mood. Physiol Behav 1998; 63: 249–252. [DOI] [PubMed] [Google Scholar]
- 40.Garcia-Argibay M, Santed MA, Reales JM. Binaural auditory beats affect long-term memory. Psychol Res 2019; 83: 1124–1136. [DOI] [PubMed] [Google Scholar]
- 41.Jirakittayakorn N, Wongsawat Y. Brain responses to a 6-Hz binaural beat: effects on general theta rhythm and frontal midline theta activity. Front Neurosci 2017; 11: 365. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 42.Abeln V, Kleinert J, Strüder HK, et al. Brainwave entrainment for better sleep and post-sleep state of young elite soccer players–A pilot study. Eur J Sport Sci 2014; 14: 393–402. [DOI] [PubMed] [Google Scholar]
- 43.Heitmann J, Cassel W, Ploch T, et al. Measuring sleep duration and sleep quality. Bundesgesundheitsblatt, Gesundheitsforschung, Gesundheitsschutz 2011; 54: 1276–1283. [DOI] [PubMed] [Google Scholar]
- 44.De Niet G, Tiemens B, Lendemeijer B, et al. Music-assisted relaxation to improve sleep quality: meta-analysis. J Adv Nurs 2009; 65: 1356–1364. [DOI] [PubMed] [Google Scholar]
- 45.Bastien CH, Vallières A, Morin C. Validation of the insomnia severity index as an outcome measure for insomnia research. Sleep Med 2001; 2: 297–307. [DOI] [PubMed] [Google Scholar]
- 46.Buysse DJ, Reynolds CF, III, Monk TH, et al. The Pittsburgh sleep quality index: a new instrument for psychiatric practice and research. Psychiatry Res 1989; 28: 193–213. [DOI] [PubMed] [Google Scholar]
- 47.Carney CE, Buysse DJ, Ancoli-Israel S, et al. The consensus sleep diary: standardizing prospective sleep self-monitoring. Sleep 2012; 35: 287–302. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.McNair DM, Lorr M, Droppleman LF. EdITS Manual for the Profile of Mood States (POMS). Educational and industrial testing service, 1992.
- 49.Ebrahimpour Z, Sharifi GR, Shakibaei A, et al. The effect of Winning/Losing on Profiles of Mood States and salivary cortisol concentration in female handball player. 2008.
- 50.Shafieizadeh A, Zahedi H. NORM OF PROFILE OF MOOD STATES FOR MALE PHYSICAL EDUCATORS. 2007.
- 51.Williams HL, Hammack JT, Daly RL, et al. Responses to auditory stimulation, sleep loss and the EEG stages of sleep. 1964. [DOI] [PubMed]
- 52.Guilleminault C, Kreutzer M. Normal sleep. Sleep. Boston, MA: Springer, 2003, pp.3–9. [Google Scholar]
- 53.Zhou J, Liu D, Li X, et al. Pink noise: effect on complexity synchronization of brain activity and sleep consolidation. J Theor Biol 2012; 306: 68–72. [DOI] [PubMed] [Google Scholar]
- 54.Golrou A, Sheikhani A, Nasrabadi AM, et al. Enhancement of sleep quality and stability using acoustic stimulation during slow wave sleep. Int Clin Neurosci J 2018; 5: 126–134. [Google Scholar]
- 55.Wahbeh H, Calabrese C, Zwickey H, et al. Binaural beat technology in humans: a pilot study to assess psychologic and physiologic effects. J Altern Complement Med 2007; 13: 25–32. [DOI] [PubMed] [Google Scholar]
- 56.Young C-W, Tsai C-Y, Zheng S-R, et al. Investigate the effect of eeg for relaxation using binaural beats. Yilan, Taiwan: 7th ISMAB 2014.
- 57.Owens JA, Belon K, Moss P, et al. Impact of delaying school start time on adolescent sleep, mood, and behavior. Arch pediatr adolesc med 2010; 164: 608–614. [DOI] [PubMed] [Google Scholar]
- 58.Bower B, Bylsma LM, Morris BH, et al. Poor reported sleep quality predicts low positive affect in daily life among healthy and mood-disordered persons. J Sleep Res 2010; 19: 323–332. [DOI] [PubMed] [Google Scholar]
- 59.Dinges DF, Pack F, Williams K, et al. Cumulative sleepiness, mood disturbance, and psychomotor vigilance performance decrements during a week of sleep restricted to 4–5 hours per night. 1997; 20: 267–277. [PubMed] [Google Scholar]
- 60.Forquer LM and Merle Johnson C. Continuous white noise to reduce sleep latency and night wakings in college students. Sleep Hypn 2007; 9: 60. [Google Scholar]
- 61.Sliwinska-Kowalska M and Davis A. Noise-induced hearing loss. Noise Health 2012; 14: 274. [DOI] [PubMed] [Google Scholar]
- 62.Crespo A, Recuero M, Galvez G, et al. Effect of binaural stimulation on attention and EEG. Arch Acoust 2013; 38: 517–528. [Google Scholar]
- 63.Noor WMFWM, Zaini N, Norhazman H, et al. Dynamic encoding of binaural beats for brainwave entrainment. In: 2013 IEEE International Conference on Control System, Computing and Engineering, 2013, pp.626–630: IEEE. [Google Scholar]
- 64.Watkins E. Constructive and unconstructive repetitive thought. Psychological bulletin 2008; 134: 163. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Munro BA, Searchfield G. The short-term effects of recorded ocean sound with and without alpha frequency binaural beats on tinnitus perception. Complement Ther Med 2019; 44: 291–295. [DOI] [PubMed] [Google Scholar]