Abstract
Background
Coronavirus disease 2019 (COVID-19) has spread worldwide since 2020, placing a huge burden on medical facilities. In the field of respiratory medicine, there has been a decrease in the number of patients. While many pulmonologists have been receiving patients with COVID-19, the actual effects on respiratory care have not been elucidated. Therefore, we conducted this study to clarify the effects of COVID-19 on medical care in the field of respiratory medicine.
Methods
We conducted a questionnaire survey among 749 hospitals belonging to the Board-Certified Member system of the Japanese Respiratory Society on the effects of COVID-19 from November 2021.
Results
Responses were obtained from 170 hospitals (23%), in approximately 70% of which the respiratory medicine department was the main department involved in managing COVID-19. The number of spirometry and bronchoscopy tests decreased by 25% and 15%, respectively, and the number of both outpatients and inpatients decreased in 93% of hospitals. Among respiratory diseases, the number of patients hospitalized for usual pneumonia, bronchial asthma, and chronic obstructive pulmonary disease decreased greatly by 30%–45%. In 62% of hospitals, the biggest effect of the COVID-19 pandemic was the greater burden in terms of the clinical workload due to COVID-19.
Conclusions
Although the number of tests and non-COVID-19 outpatients and inpatients decreased in respiratory medicine departments during the COVID-19 pandemic, the workload increased due to COVID-19, resulting in a great increase in the clinical burden.
Keywords: Coronavirus disease 2019, Spirometry, Bronchoscopy, Clinical burden
Abbreviations: COVID-19, coronavirus disease 2019; SARS-CoV-2, severe acute respiratory syndrome coronavirus-2; COPD, chronic obstructive pulmonary disease
1. Introduction
A new infectious disease, namely coronavirus disease 2019 (COVID-19), caused by a novel coronavirus (severe acute respiratory syndrome coronavirus-2 [SARS-CoV-2]), was first reported in December 2019. It is currently more than 2 years since the first infected person was reported in Japan in January 2020. However, variant strains, such as the delta and omicron variants, have also appeared, and to date, COVID-19 has tremendous effects on many medical institutions and healthcare workers.
To clarify the role of respiratory medicine departments and issues that should be addressed in treating COVID-19, the Japanese Respiratory Society conducted a series of four questionnaire surveys in 2020 [1]. The survey results revealed that viewing the medical care system over time, the proportion of facilities that could perform polymerase chain reaction tests for SARS-CoV-2 increased, while the proportion of facilities that could manage extracorporeal membrane oxygenation was unchanged. Additionally, excessive workloads of 150% or more among healthcare workers, stress from lack of personal protective equipment and the risk of infection, and harassment from the people around them were also highlighted, all of which have not improved sufficiently over time. Increased clinical workloads and large psychological burdens have also been reported in other surveys in Japan [2].
Experience gained from this pandemic is valuable and should be considered in future measures, while actual situations are widely monitored. In this study, aimed at understanding the status of medical services, such as the number of patients and tests in respiratory medicine departments, we conducted a survey to examine how medical services have changed during the COVID-19 pandemic.
2. Materials and methods
The survey was performed in 749 core and associate hospitals in the Board-Certified Member system of the Japanese Respiratory Society. The survey response period was set for 1 month in November 2021 but was extended for additional 2 weeks. With the cooperation of the administrative department of each hospital, one person representing respiratory medicine senior fellows was asked to respond to a web survey, the content of which is shown in Table 1 . The survey examined the effects of COVID-19 from November 2021. The number of tests (spirometry and bronchoscopy) and the number of patients were divided into seven 6-month periods, from January 2018 to June 2021, with January–June 2018 designated as period 1, July–December 2018 as period 2, January–June 2019 as period 3, July–December 2019 as period 4, January–June 2020 as period 5, July–December 2020 as period 6, and January–June 2021 as period 7.
Table 1.
List of questions in the questionnaire.
| 1 | Does your hospital treat patients with COVID-19? | ||||||
| 2 | When treating COVID-19, is the respiratory medicine department the main department, a concurrent department, or provides cooperation only? | ||||||
| 3 | Do you have an infectious disease department? | ||||||
| 4 | Does your hospital provide online outpatient consultations? | ||||||
| 5 | If so, what is the approximate percentage of online consultations among all outpatient consultations? | ||||||
| 6 | Has your hospital set up a specialty outpatient clinic for COVID-19 sequelae? | ||||||
| 7 | In the specialty outpatient clinic for sequelae, is the respiratory medicine department the main department, a collaborating department, or provides support only? | ||||||
| |||||||
| 2018 | 2019 | 2020 | 2021 | ||||
| Jan–Jun | Jul–Dec | Jan–Jun | Jul–Dec | Jan–Jun | Jul–Dec | Jan–Jun | |
| Bronchoscopy test | |||||||
| Respiratory function test | |||||||
| 8 | Please input the number of tests into the above table. | ||||||
| 9 | If the number of bronchoscopy tests decreased after 2020, what is the major reason? | ||||||
| 10 | If the number of respiratory function tests decreased after 2020, what is the major reason? | ||||||
| |||||||
| 11 | Please write the number of patients in all outpatient clinics and the respiratory medicine outpatient clinic during the same periods as above. | ||||||
| 12 | If the number of patients in all outpatient clinics increased after 2020, what is the major reason? | ||||||
| 13 | If the number of patients in all outpatient clinics decreased after 2020, what is the major reason? | ||||||
| 14 | If the number of patients in the respiratory medicine outpatient clinic increased after 2020, what is the major reason? | ||||||
| 15 | If the number of patients in the respiratory medicine outpatient clinic decreased after 2020, what is the major reason? | ||||||
| |||||||
| 16 | Please write the number of hospitalized patients in all clinical departments and the respiratory medicine department during the same periods as above. | ||||||
| 17 | If the number of inpatients in all departments increased after 2020, what is the major reason? | ||||||
| 18 | If the number of inpatients in all departments decreased after 2020, what is the major reason? | ||||||
| 19 | If the number of inpatients in the respiratory medicine department increased after 2020, what is the major reason? | ||||||
| 20 | If the number of inpatients in the respiratory medicine department decreased after 2020, what is the major reason? | ||||||
| |||||||
| 21 | Please write the number of inpatients admitted for bronchial asthma attacks, COPD exacerbation, pneumonia other than COVID-19, interstitial pneumonia, and lung cancer during the same periods as above. | ||||||
| 22 | What has been the biggest effect of the COVID-19 pandemic on respiratory examinations, treatment, and care in your department? | ||||||
COVID-19, coronavirus disease 2019; COPD, chronic obstructive pulmonary disease.
Responses were obtained from 170 (23%) of the 749 hospitals, although there were missing entries on the trends in the numbers of outpatient and inpatient. As a result, 10 hospitals were excluded during assessment of the patient numbers. When calculating the percentages of reasons for these changes, cases with no responses were not included in the denominators. Responses to a free description question on the examinations, treatment, and care that were the most largely affected by the COVID-19 pandemic were received from 150 hospitals, of which 49 gave multiple responses. The analysis was performed using both percentages of the 199 responses and those of the number of hospitals.
3. Results
Patients with COVID-19 were treated at 97% of responding hospitals (165 hospitals), in 67% of which (111 hospitals) the department of respiratory medicine was the main department for this treatment. Even in hospitals with infectious disease departments (28%; 48 hospitals), the respiratory medicine department was the main department treating COVID-19 in 50% (24 hospitals) (in 33% [16 hospitals] treatment was provided jointly by these departments, and in 17% [eight hospitals], the respiratory medicine department was a supporting department). Online consultations (including by telephone) were performed at 21% of the responding hospitals (35 hospitals), of which 94% (33 hospitals) provided these online consultations to less than 5% of outpatients. Specialty outpatient clinics for COVID-19 sequelae were set up at only 9% of hospitals (15 hospitals), among which the respiratory department was the main department treating COVID-19 sequelae at 47% (seven hospitals), treatment was provided jointly with another department at 33% (five hospitals), and the respiratory department was a supporting department at 20% (three hospitals).
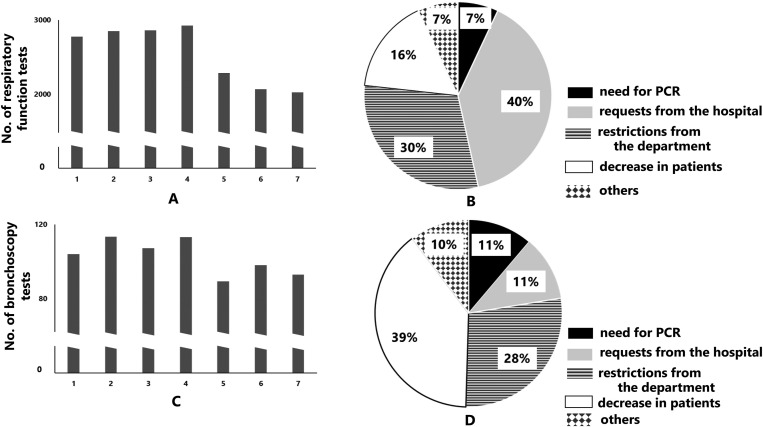
Fig. 1 shows the changes in the number of tests. The number of respiratory function tests decreased by approximately 25% from before to after the spread of COVID-19. After January 2020, the number decreased to 90% of hospitals (144 hospitals). The most common reason (40%) was the request to avoid conducting such tests at the hospital, followed by restrictions from the clinical department (30%). Bronchoscopy tests decreased similarly by approximately 15%, and from January 2020 there were decreases in these examinations at 78% of hospitals (125 hospitals). The most common reason provided was a decrease in the number of patients who needed bronchoscopy (39%), followed by restrictions in the departments (28%).
Fig. 1.
Changes in the number of pulmonary function tests and bronchoscopic examinations. (A) Number of pulmonary function tests. Period 1: January–June 2018, Period 2: July–December 2018, Period 3: January–June 2019, Period 4: July–December 2019, Period 5: January–June 2020, Period 6: July–December 2020, Period 7: January–June 2021 (same below). (B) Reason for the decrease in pulmonary function tests. (C) Number of bronchoscopic examinations. (D) Reason for the decrease in bronchoscopic examinations.
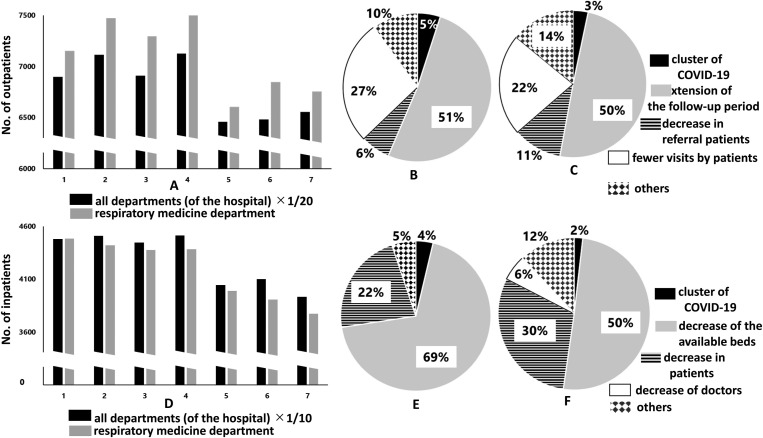
Fig. 2 shows the trends in the numbers of outpatients and inpatients. For outpatients, the decrease was approximately 7% in all clinical departments (data for all departments are shown at 1/20 of the actual total), and about 8% in respiratory medicine departments. Among hospitals, there were decreases in all clinical departments in 93% of hospitals (149 hospitals), and in the respiratory medicine department in 83% (133 hospitals). The reasons given for the decline were extensions of the follow-up periods (51% and 55%, respectively) and fewer visits from patients (27% and 22%, respectively). Regarding inpatients, the number decreased by approximately 10% in all clinical departments (shown at 1/10 in the figure), and approximately 12% even in respiratory medicine departments. Among hospitals, there were decreases in all clinical departments in 92% of hospitals (148 hospitals), and in the respiratory medicine department in 76% (122 hospitals). The most common reasons given were a decrease in the number of available beds since the beds were utilized for COVID-19 patients (69% and 50%, respectively), and a decrease in the number of patients (22% and 30%, respectively).
Fig. 2.
Change in the number of outpatients and inpatients. (A) Changes in the number of outpatients in all clinical departments and the respiratory medicine department. (B) Reason for the decrease in the number of outpatients in all departments. (C) Reason for the decrease in the number of outpatients in the respiratory medicine department. (D) Changes in the number of inpatients in all clinical departments and the respiratory medicine department. (E) Reason for the decrease in the number of inpatients in all clinical departments. (F) Reason for the decrease in the number of inpatients in the respiratory medicine department. Periods 1–7: Refer to Fig. 1.
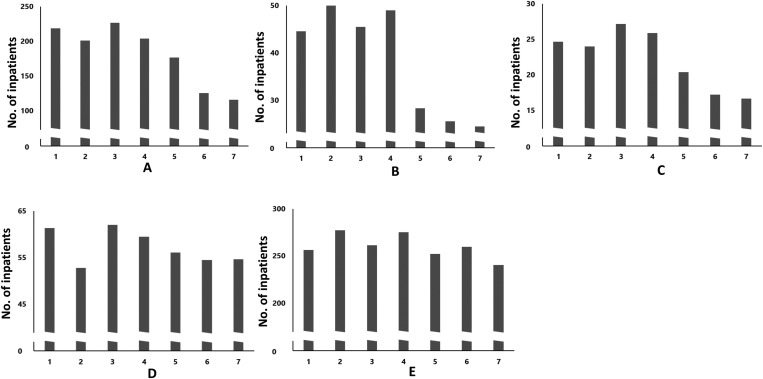
Fig. 3 shows the changes in the number of inpatients with different respiratory diseases. Marked decreases were seen in pneumonia, and exacerbation of asthma or chronic obstructive pulmonary disease (COPD) from before to after the spread of COVID-19 (35%, 45%, and 28%, respectively). However, there was little effect on patients with interstitial pneumonia and lung cancer (7% and 6%, respectively).
Fig. 3.
Change in the number of respiratory disease inpatients. (A) Pneumonia other than COVID-19, (B) bronchial asthma, (C) COPD, (D) interstitial pneumonia, and (E) lung cancer.
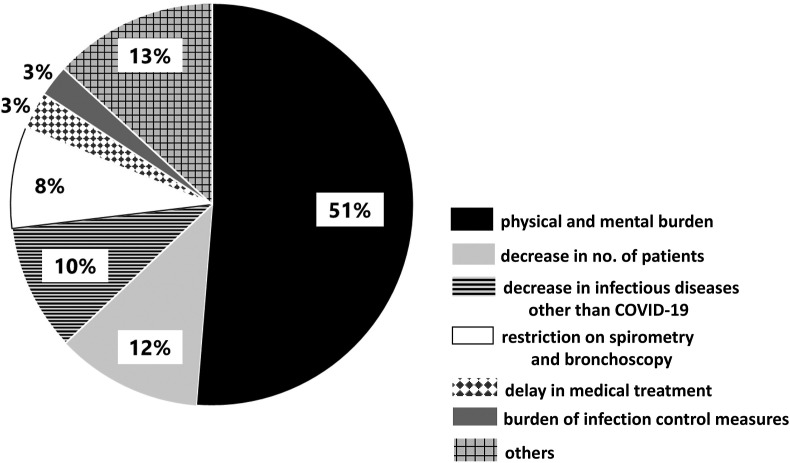
Finally, respondents were asked to freely describe the largest effect of the COVID-19 pandemic. One hundred and ninety-nine responses were obtained from 150 hospitals. Fig. 4 shows the percentage distribution of different categories of issues derived from the 199 responses. The most common issue was the physical and mental burden due to the clinical workload, accounting for 51% of responses. In terms of the number of hospitals, 62% (93/150) described an increase in burden from the workload. Specifically, in addition to COVID-19 in both inpatient and outpatient settings, there were burdens from infection control measures at the hospital (including those associated with the responses for cluster outbreaks), consultation for the suspicious radiological images, dispersal of patient wards, and other issues. Other matters described were decreases in the number of patients with respiratory diseases other than COVID-19 to 12% (in 23 hospitals), decreases in infectious diseases other than COVID-19 to 10% (20 hospitals), and the strict enforcement and burden of infection control measures, such as masks and hand-washing. Sixteen hospitals (8%) mentioned decreases in respiratory function tests and bronchoscopy. Other responses were the closure of tuberculosis beds, decreases in revenue, training venues, decrease in the number of doctors entering medical stations, and training time and academic activities.
Fig. 4.
What has been the biggest effect of the COVID-19 pandemic on respiratory examinations, treatment, and care? Free descriptions were aggregated, and the results are shown. The percentage shown is relative to the total number of responses (199 issues from 150 hospitals).
4. Discussion
In this study, the role of respiratory medicine departments in COVID-19 treatment was found to be vital, and in approximately 70% of hospitals providing COVID-19 treatment, the main department in charge was the respiratory medicine department. About 30% of hospitals had infectious disease departments, but even in about half of those hospitals, the respiratory medicine department was primarily responsible for providing COVID-19 care. This likely explains that the increase in the clinical workload was given as the largest effect of COVID-19 in about half of the hospitals, despite the decrease of approximately 25% and 15% in respiratory function tests and bronchoscopies, respectively performed, and decreases in the number of both outpatients and inpatients from before to after the spread of COVID-19 in all clinical departments, as well as in respiratory medicine departments.
There is a risk of infection to healthcare workers from pulmonary function tests and bronchoscopies [3,4], and both the Japanese Respiratory Society [5] and the Japan Society for Respiratory Endoscopy [6] called for caution in March 2020 by putting off non-essential and non-urgent tests. In this survey, the most common reason for the decrease in spirometry was an advisory calling for avoidance of such tests from the hospital (40%), followed by voluntary restraint from the respiratory department (30%), and in the case of bronchoscopy, a decrease of patients requiring it (39%), followed by voluntary restraint from the departments (28%). In addition, insufficient staff and/or time is thought to have contributed to this restraint. Infections or the occurrence of clusters of COVID-19 from these tests have so far not been reported. The decrease in these tests may lead to delays in diagnosis and treatment. For pulmonary function tests essential for the diagnosis of COPD, measures to mitigate the effects on medical care were adopted. They included the publication of the “Working diagnosis and initial management of COPD during the COVID-19 pandemic” [7] by the Japanese Respiratory Society for treatment to be administered even without pulmonary function tests.
The most common reason for the decrease in patients was the extension of the return period in outpatient clinics, followed by patients refraining from medical examinations both in respiratory medicine departments and overall. For inpatients, the number of beds had to be decreased to ensure the availability of beds for patients with COVID-19. This explains the decrease of inpatients by approximately 70% in hospitals overall, and most inpatients even in respiratory medicine wards. Second, the number of inpatients with respiratory diseases other than COVID-19 also decreased. Regarding inpatients with respiratory diseases, cases of pneumonia, bronchial asthma attacks, and COPD exacerbations greatly decreased, although the decrease in interstitial pneumonia and lung cancer cases was minimal. The number of patients hospitalized with asthma showed similar trends from 2017 to 2019, even in studies using databases in Japan [8], but in 2020 (from the ninth week onward), there was a large decrease compared with the previous 3 years. This decrease could be due to a decrease in cases of viral infection as a result of standard infection control measures, such as face masks and hand disinfection for SARS-CoV-2, restrictions on going out, and other factors [9,10]. The decrease in outpatient and inpatient admissions apart from asthma may also be the result of fewer opportunities for infection. However, considering that lung cancer has also decreased by 6%, this may be linked to delays in treatment, which may lead to future excess deaths. Concerning the cause of deaths in 2020, respiratory diseases as a cause of death decreased by 10.6%, influenza decreased by 70%, and pneumonia greatly decreased by approximately 18%, bronchial asthma 22%, and COPD 10% compared with causes of deaths in 2019 and earlier [11].
About half of the respondents stated that the largest effect of the COVID-19 pandemic was the burden on the clinical workload, with the burden of COVID-19 falling significantly on respiratory medicine departments. Various burdens were described, not just due to the treatment of patients with COVID-19, but also in terms of COVID-19 infection control and consultations, staff shortages, and transfers of patients without COVID-19 in the hospital. Some responses stated that the largest effect was increased coordination with other departments, such as COVID-19 treatment and shifting patients with non-COVID-19 pneumonia conditions to other departments. Moreover, in 7% of hospitals, mental stress from increases in the clinical workload and increased non-clinical work, and the risk of SARS-CoV-2 infection in healthcare workers were given the largest effects. The psychological burden and burnout of healthcare workers from the COVID-19 pandemic and harassment of healthcare workers have also been reported previously [1,[12], [13], [14]]. Measures to prevent these events are also thought to be important.
Online medical consultations were provided in 21% of hospitals, but, in almost all cases, this accounted for fewer than 5% of outpatients. Web conferencing has become a standard practice in the COVID-19 pandemic, and it will be necessary to raise the proportion of regular online medical care in the future in preparation for pandemics. In addition, only 9% of hospitals had established clinics to manage the aftereffects of COVID-19. This could be because hospitals are at their limit just handling the acute phase of COVID-19. However, COVID-19 is known to cause several sequelae, including malaise, coughing, mental symptoms, and respiratory dysfunction [15]. Appropriate management of these manifestations will be necessary.
The low response rate (about 23%) for this questionnaire could be due to the short response period, although the mean response rate in four sequential surveys conducted in 2020 was 24.9%, which is comparable to the response rate for the present study. However, this could be due to time constraints from ongoing pandemic management efforts; thus, some hospitals indicated they could not respond to the survey because they were too busy. In addition, since 97% of the responding hospitals provided COVID-19 treatment, hospitals that did not provide COVID-19 treatment may have not responded to this survey.
5. Conclusions
In conclusion, the numbers of tests, outpatients, and inpatients decreased during the COVID-19 pandemic compared with those before the pandemic, along with decreases in respiratory diseases other than COVID-19, particularly patients hospitalized with pneumonia, bronchial asthma, and COPD. Since the respiratory medicine department was the primary center of COVID-19 care in 67% of hospitals, it is reasonable that the burden of the clinical workload and mental stress from the COVID-19 pandemic was most strongly felt by respiratory specialists. Conversely, there was an inevitable reduction in the number of tests and outpatients. However, medical care in respiratory departments was shown to be greatly affected by the pandemic.
Funding source
None.
IRB information
The study was approved by the Institutional Ethics Committee of Kochi University School of Medicine (approval number 2021–129, approval date 2021/10/4).
Conflict of Interest
The authors have no conflicts of interest.
Acknowledgements
The survey was conducted based on a request from the Japanese Medical Science Federation. We would like to thank each supervising physician at the facility who took time out of their very busy schedules to participate in this survey. We also thank Ms. Nozomi Hakamada of the Japanese Respiratory Society for her contribution to the development of the questionnaire.
References
- 1.Kamada K., Konno S., Kaneko T., Fukunaga K., Hasegawa Y., Yokoyama A. The effect of the outbreak of COVID-19 on respiratory physicians and healthcare in Japan: serial nationwide surveys by the Japanese Respiratory Society. Respir Investig. 2021;59:792–798. doi: 10.1016/j.resinv.2021.07.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Matsuno T., Kobayashi D., Taki F., Sakamoto F., Uehara Y., Mori N., et al. Prevalence of health care worker burnout during the coronavirus disease 2019 (COVID-19) pandemic in Japan. JAMA Netw Open. 2020;3 doi: 10.1001/jamanetworkopen.2020.17271. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Huang Y., Tan C., Wu J., Chen M., Wang Z., Luo L., et al. Impact of coronavirus disease 2019 on pulmonary function in early convalescence phase. Respir Res. 2020;21:163. doi: 10.1186/s12931-020-01429-6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Reddy P.D., Nguyen S.A., Deschler D. Bronchoscopy, laryngoscopy, and esophagoscopy during the COVID-19 pandemic. Head Neck. 2020;42:1634–1637. doi: 10.1002/hed.26221. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.https://www.jrs.or.jp/uploads/uploads/files/information/20200327_statement.pdf (in Japanese) [accessed 11 March 2022].
- 6.http://www.jsre.org/info/2003_covid19_2.pdf (in Japanese) [accessed 11 March 2022].
- 7.Shibata Y., Muro S., Yokoyama A., Hashimoto S. Statement from the Japanese Respiratory Society: working diagnosis and initial management of COPD during the COVID-19 pandemic. Respir Investig. 2021;59:385–388. doi: 10.1016/j.resinv.2021.03.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Abe K., Miyawaki A., Nakamura M., Ninomiya H., Kobayashi Y. Trends in hospitalizations for asthma during the COVID-19 outbreak in Japan. J Allergy Clin Immunol Pract. 2021;9:494–496. doi: 10.1016/j.jaip.2020.09.060. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Gupta A., Bush A., Nagakumar P. Asthma in children during the COVID-19 pandemic: lessons from lockdown and future directions for management. Lancet Respir Med. 2020;8:1070–1071. doi: 10.1016/S2213-2600(20)30278-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.So J.Y., O'Hara N.N., Kenaa B., Williams J.G., deBorja C.L., Slejko J.F., et al. Population decline in COPD admissions during the COVID-19 pandemic associated with lower burden of community respiratory viral infections. Am J Med. 2021;134:1252–1259. doi: 10.1016/j.amjmed.2021.05.008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.https://www.mhlw.go.jp/toukei/saikin/hw/jinkou/geppo/nengai20/dl/gaikyouR2.pdf (in Japanese) [accessed 11 March 2022].
- 12.Soo R.J.J., Chiew C.J., Ma S., Pung R., Lee V. Decreased influenza incidence under COVID-19 control measures, Singapore. Emerg Infect Dis. 2020;26:1933–1935. doi: 10.3201/eid2608.201229. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Thatrimontrichai A., Weber D.J., Apisarnthanarak A. Mental health among healthcare personnel during COVID-19 in Asia: a systematic review. J Formos Med Assoc. 2021;120:1296–1304. doi: 10.1016/j.jfma.2021.01.023. [DOI] [PubMed] [Google Scholar]
- 14.Blevins D., Henry B.F., Sung M., Edelman E.J., Black A.C., Dawes M., et al. Well-being of health care professionals treating opioid use disorder during the COVID-19 pandemic: results from a national survey. Psychiatr Serv. 2021 doi: 10.1176/appi.ps.202100080. 10.1176. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.https://www.mhlw.go.jp/content/000860932.pdf (in Japanese) [accessed 11 March 2022].