Abstract
Introduction
This study was designed to determine the respiratory safety of improvised respirators based on modified full-face snorkel masks, making comparisons with a purpose-designed mask
Methods
This is a prospective crossover study conducted on ten recruits. Volunteers wore snorkel masks mated to an anaesthetic heat and moisture exchange filter. The system was worn at rest then during exercise. Gases were sampled from the mask at 5-min intervals.
Results
The modified snorkel was satisfactory in seven participants. For three carbon dioxide concentrations were >1%. Two participants exposed to excessive CO2 also experienced oxygen concentrations <19%. All participants exposed to unsatisfactory gas mixtures were non-white.
Conclusions
Modifying snorkel masks changes the way that gases circulate through the system. These modifications increase the risk of rebreathing in some users, which may yield an unsafe gas mixture. These improvised masks cannot be recommended as a substitute for purpose-designed equipment.
Keywords: Personal protective equipment, COVID-19, safety
Introduction
Shortfalls in personal protective equipment (PPE) during the first wave of COVID-19 led many groups to repurpose snorkel masks as respirators. The most widely available proposal was based on a full-face Decathlon snorkel mask mated to a heat and moisture exchange (HME) filter by a 3 D-printed adaptor.
These are already being used by staff in many healthcare facilities without rigorous quality assessment. This study was designed to test the gases delivered by such an improvised system.
Methods
Comparisons were made between a Sundstrom SR-100 reusable mask (Sundstrom Safety AG, Lagan, Sweden) and an assembly comprising a Decathlon full-face snorkel mask (Decathlon, Villeneuve d’Ascq, France), an adaptor made using a Prusa i3 Mk2 printer (Pruza Research, Praha, Czech Republic), and a ClearTherm 3 HME filter (Intersurgical, Wokingham, UK).
Inspired oxygen (FiO2) and carbon dioxide (FiCO2) concentration was measured every 5 min using the analyser of a Dräger Primus anaesthetic machine (Dräger UK, Hemel Hempstead, UK). Twenty minutes wearing each mask were spent at rest, then 20 min of light exercise using an aerobic stepper to simulate physical work. A 5-min washout (with the mask doffed) was inserted between phases.
A convenience sample of ten was selected based on recommendations provided in the British Standard for mask certification. 1 Recruitment was purposeful to ensure a mix of gender and ethnicity.
Results
Six males and four females were recruited. Three participants were white, two black, four Asian, and one of ‘other’ ethnicity. The mean (95% CI) age was 38.6 (33·8–43·4) and mean (95% CI) BMI was 27·8 (23·5–32·2). There were no significant differences in BMI by gender (p = 0·44) or ethnicity (p = 0·49).
Gas composition overall did not significantly differ between test phases (Table 1), however the improvised respirator delivered FiCO2 >1% (the limit specified in British Standards 2 ) for three individuals. Nine measures from these participants showed CO2 over 1% (seven measured at rest, two on exertion). For two participants the 2% FiCO2 safety limit imposed by the study protocol was breached, requiring testing be abandoned. Hypercapnic mixtures coincided with low FiO2 in two participants.
Table 1.
Gas analysis by test-phase.
| Measure |
Rest phase |
Exercise phase |
p | ||
|---|---|---|---|---|---|
| Mean | 95%CI | Mean | 95%CI | ||
| Improvised system | |||||
| Inspired O2 (%) | 19.7 | 19.0–20.3 | 19.9 | 19.4–20.3 | 0.14 |
| Inspired CO2 (kPa) | 0.5 | 0.1–0.9 | 0.0 | 0.0–0.6 | 0.07 |
| Purpose-designed system | |||||
| Inspired O2 (%) | 20.1 | 20.0–20.2 | 20.0 | 19.9–20.1 | 0.223 |
| Inspired CO2 (kPa) | 0.2 | 0.1–0.3 | 0.2 | 0.1–0.3 | 0.375 |
The two participants in whom the test was stopped early for safety reasons were of Asian ethnicity. The third participant exposed to >1% CO2 (but for whom the test did not breach safety limits) was of ‘other’ ethnicity. A third participant, of black ethnicity, requested their test be stopped due to discomfort.
The purpose-designed mask delivered acceptable gas compositions and comfort at all test points.
Discussion
The improvised system did not provide a universally safe gas mixture. Some speculation on the point of failure is possible.
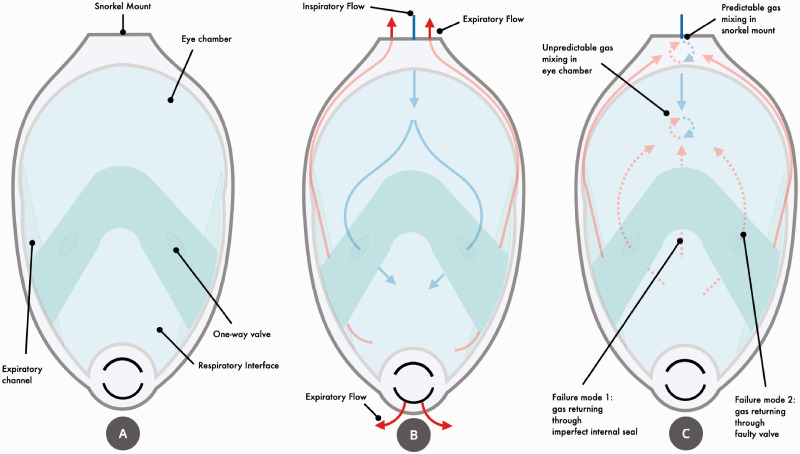
The mask is functionally divided into two compartments separated by a membrane (Figure 1). Fresh air reaches the respiratory chamber via a chamber in front of the eyes. One-way valves prevent expired gases returning to the eye chamber. Expiratory flow is directed through unvalved channels running along the outer edges of the mask back towards the snorkel mount, and through a valved outlet on the front of the mask.
Figure 1.
Schematic diagram depicting components of the facemask (a), normal gas paths through the system (b), and potential sources of inspiratory and expiratory gas mixture (c).
Inspired and expired gases can mix in the adaptor, and no valves separate the adaptor from the eye-chamber. The degree to which the streams mix varies with respiratory effort and rate, but will occur to some degree in all users.
Problems worsen if unidirectional flow between eye-chamber and respiratory interface cannot be maintained, for example by faulty valves or an inadequate seal of the internal membranes. We believe this to be the source of failure in our three participants given the high degree of rebreathing observed. Although it is not known how these snorkel masks were developed, a potential deficiency of even purpose-designed respirators is that the original measurements on which they were based was largely taken from white males. 3 Facial dimensions differ significantly by gender and ethnicity, 4 so it is plausible that the masks’ internal membrane does not reliably seal in some users.
Prolonged exposure to high FiCO2 is hazardous. 5 Inspired concentrations above 1% yield observable increases in minute volumes, and a subjective sensation of dyspnoea begins at 2%. Impaired CO2 elimination can result in drowsiness, confusion, and in extreme cases, unconsciousness. Improvised masks could therefore be hazardous when worn over a period of duty.
Finally, this study makes no claims on the improvisation’s filtration efficacy (i.e. viral protection). We address this issue fully in a related paper, 6 but in brief our data cast doubt on whether improvised systems provide viral protection for most users.
Our data suggest that improvised respirators cannot be recommended as a substitute for purpose-designed equipment.
Acknowledgements
We are very grateful to the following individuals and organisations for their support of the study: Richard Kirwan for invaluable assistance sourcing and managing equipment for the study; Stuart Robey (InterSurgical UK) for kindly donating the HME filters; The Department of Anaesthetics for donating funds to enable purchasing of the snorkel masks; James Bradshaw, Head of Digital Technology at Formula 1, and Luke Isawzko, Mechanical Design Engineer at Formula 1 for assisting with design and 3D printing the adaptors used in the study; Dr Sophie Ragbourne for her kind assistance with data collection.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iD: Paul R Greig https://orcid.org/0000-0003-3161-5641
References
- 1.BS EN 149:2001+A1 2009. Respiratory protective devices – filtering half-masks to protect against particles – requirements, testing, marking.
- 2.BS EN 136 1998. Respiratory protective devices – full face masks – requirements, testing, marking.
- 3.Bailar J, Meyer E, Pool R. Assessment of the NIOSH head-and-face anthropometric survey of US respirator users. Washington, DC: National Academies Press, 2007. [Google Scholar]
- 4.Zhuang Z, Landsittel D, Benson S, et al. Facial anthropometric differences among gender, ethnicity and age groups. Ann Occup Hygiene 2010; 54: 391–402. [DOI] [PubMed] [Google Scholar]
- 5.Seter AJ. Allowable exposure limits for carbon dioxide during extravehicular activity. Moffet Field, CA, USA: Ames Research Center, National Aeronautics and Space Administration, 1993. [Google Scholar]
- 6.Greig PR, Bradshaw J, Carvalho C, et al. STRIPE-1: a crossover trial comparing the protective efficacy of improvised snorkel-based FFP3 masks against purpose-designed equipment. 2020.