Abstract
With the declaration of coronavirus 2019 (COVID-19) as a pandemic, intensive care units across the globe began to prepare for large numbers of patients. For many years, UK Intensive Care Units (ICUs) have been at high capacity, while facing staffing shortages. In order to prepare for the predicted increased work caring for large numbers with COVID-19, staff were redeployed from other clinical areas to help. Many of these staff had no previous ICU experience. In this article, we share our experiences redeploying medical staff from an extensive range of backgrounds, and how we utilised those staff to maximise use of their existing skills, together with reflections from a variety of redeployed staff members.
Keywords: Covid, coronavirus, ICU, critical care, redeployment
Introduction
In March 2020, the World Health Organisation (WHO) declared the spread of a novel coronavirus, referred to as “severe acute respiratory syndrome coronavirus 2” (SARS-CoV-2), as a pandemic. 1 Reports of Italian critical care units being overwhelmed by the number of patients began to circulate,2,3 while simultaneously suggesting the UK would face similar case numbers two weeks after Italy. 4
Centrally calculated COVID-19 case number predictions from NHS England (NHSE) for our area were for many times our Intensive Care Unit (ICU) capacity, and all Trusts were advised to prepare for large numbers of COVID-19 patients requiring respiratory support. 5 To assist, staff were redeployed to ICU from other clinical areas. Many of these staff had no ICU experience or had even been inside an ICU before.
In this article, we share our experience of redeploying medical staff from an extensive range of other areas, and how we utilised these staff to maximise use of their existing skills, together with the reflections of groups of staff who were redeployed.
Organisation of critical care services
Excluding the respiratory ward and HDU areas, we divided the critical care services into 3 distinct areas of approximately equal bed numbers.
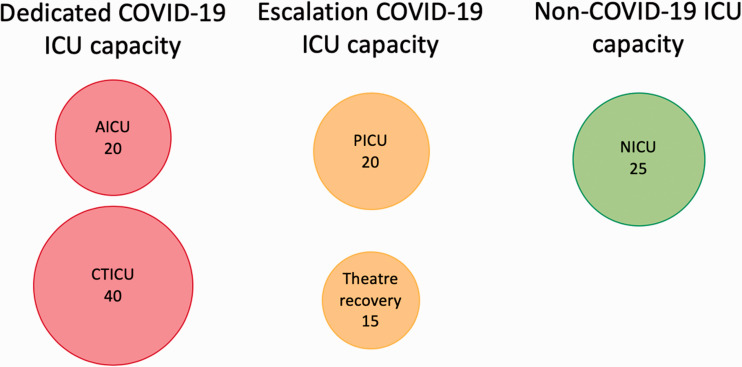
Each of these areas would normally care for different cohorts of critically ill patients. There was a graded and step-wise process of escalation as increasing numbers of COVID-19 patients were admitted. The cessation in elective workload offered additional capacity in the cardiothoracic and neurosurgical ICUs (Figure 1).
Figure 1.
COVID-19 capacity planning with escalation capacity. Dedicated capacity included general Adult Intensive Care unit (AICU) with 20 beds and Cardiothoracic ICU (CTICU) with 40 beds. Escalation was possible to the paediatric ICU (PICU) and theatre recovery. Our non-COVID-19 patients requiring intensive care were placed in the neuro ICU (NICU) which had a capacity of 25 beds.
Distribution of roles
Regarding the medical workforce, from nearly 200 potential new staff from all breadths of speciality and seniority, we identified some groups to utilise in specific ways to maximise their benefit:
Proning teams
We allocated orthopaedic surgeons to develop proning teams. Orthopaedic staff have experience placing patients in the prone position for surgery, and many units had recognised this pre-existing skillset previously. 6 We expanded this concept and paired our orthopaedic staff with occupational and physiotherapists, who also have extensive experience in safely positioning patients.
Line-insertion teams
We allocated experienced renal physicians, together with trainee radiologists to develop line-insertion teams. Renal physicians are skilled at placing a variety of lines for haemodialysis. The trainee radiologists as part of their training partake in minimally invasive procedures such as stenting and providing central access for the delivery of chemotherapy. 7
Tracheostomy teams
We allocated consultant ENT/Maxillofacial surgeons to develop dedicated surgical tracheostomy theatre slots in lieu of their cancelled elective surgery theatre time. Given the predicted long-term ventilation times of ICU COVID-19 patients, we anticipated that we might require a service to support the numbers of patients requiring tracheostomy.
Intubation teams
Our anaesthetic department developed a 24/7 intubation team. The prediction of over 30 COVID-19 patients needing intubation and ventilation every day, would have rapidly swamped our services.
Allocating staff to these specific roles meant that the training required for them was minimal. By distributing these tasks, the staff with ICU experience were freed up to focus on core ICU care and decision making.
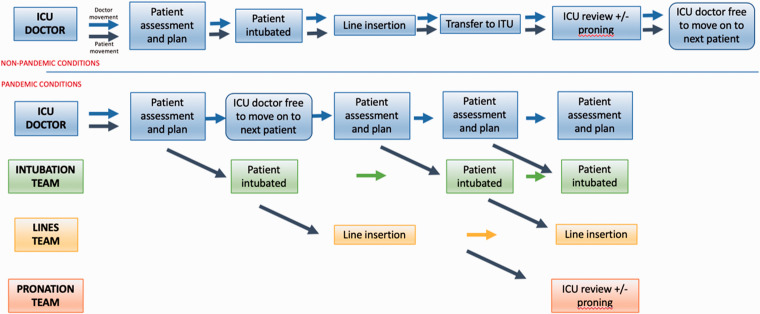
From the initial referral of a COVID-19 patient to critical care services, each team had a well-defined point at which their services would be required (see Figure 2). The aim was to ensure that there was adequate support for the clinicians with critical care experience to allow them to assess a patient and formulate a plan, then be free to move to the next patient whilst ensuring that key tasks were carried out promptly by competent staff.
Figure 2.
Admissions pathway for patients under normal (top) and pandemic (bottom) conditions. Note the uncoupling of patient and doctor movement and the use of the redeployed doctors to enable greater utilisation of an intensivist’s specialist skills, whilst other teams take over task-specific aspects of management.
In addition, a large number of general volunteers were re-deployed across the critical care areas, to support the core ICU work force. Existing ICU staff underwent significant changes to their working patterns to ensure that there was a number of senior ICU-trained staff available 24/7. This meant the re-deployed staff always had support and advice immediately available.
To ensure smooth and flexible working across all the areas, including the ability for mutual support, shift times for all staff were unified.
We based a level of redundancy into our rota system to allow for significant staff absence (25–30%). Vacancy rates this high were not observed (on average, approximately 15%), but if vacancy was high in one area, staff could be redistributed from another area.
Managing the peak
As the workload increased, the urgency built. We ensured the ICU experienced staff were in place first, and then supported them with the other redeployed staff. Our stepwise approach to re-deployment and the separate teams listed above, did lead to advantages later, giving us flexibility to release teams back to their usual areas at different times.
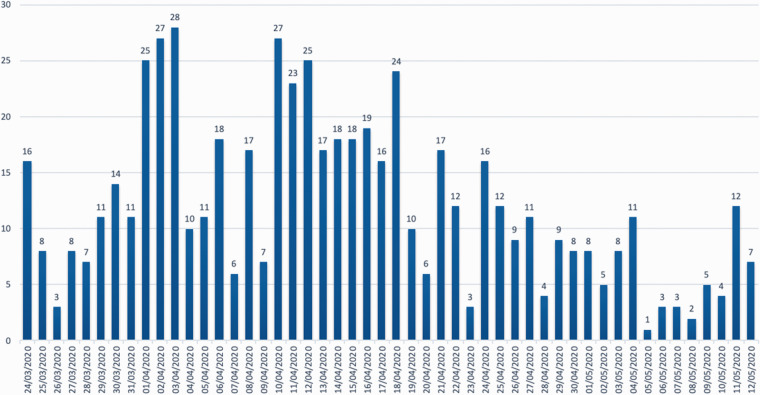
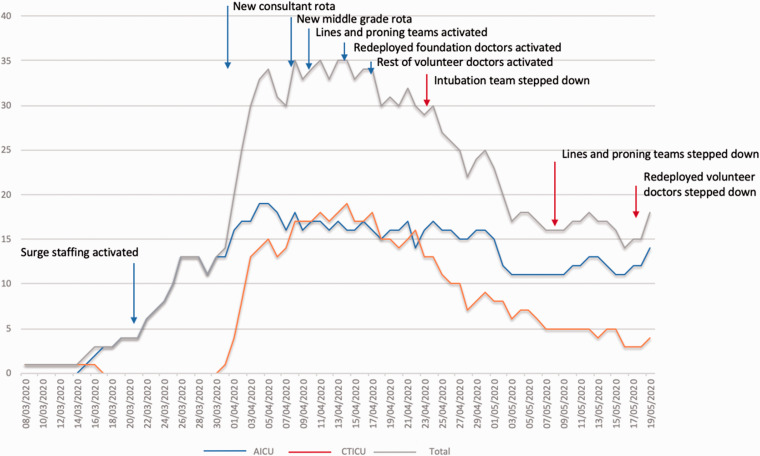
On the 31st March we had 14 COVID-19 patients in ICU. On the 3rd April we had 30 and by the 8th April we had 35 patients (see Figures 3 and 4).
Figure 3.
Total hospital admissions, per day, with confirmed COVID-19.
Figure 4.
Total critical care occupancy of suspected or confirmed COVID-19 cases across the critical care areas, with deployment and step-down dates of various staff groups. “Surge staffing” refers to an additional airway trained registrar on every shift. The AICU was filled to near-capacity first, and then the CTICU was used.
On the 25th April we had less than 30 COVID-19 patients in ICU, and on the 3rd May we had less than 20 COVID-19 patients in ICU. During this time, the need for the intubation, proning and line-insertion teams reduced, and these teams were released from ICU. Other volunteers were gradually phased down in a stepwise manner, in the subsequent weeks.
The step-down of the surge workforce allowed us to maintain a little slack in the system while ensuring staff could be re-escalated rapidly if needed.
Reflections from ICU
ICU overview
In the short preparation time before the surge, we had to re-think our staffing models entirely, re-distribute our existing staff to ensure an equitable spread of the workforce, and open our arms to help and support from other areas.
We built in redundancy for anticipated vacancy in our rotas, which had advantages and disadvantages. The downsides of this spare capacity were that the rota was comparatively tough for each person, and at times there were almost too many people present. The upside was ease in ensuring minimum staffing levels were achieved, even in the presence of moderate vacancy rates, but also the facility for teaching to take place.
For our existing staff, the unsettling nature of complete rota changes, with very little notice, and movement into unfamiliar critical care areas, had a negative effect on morale, although this was largely negated by the camaraderie of pandemic working. Where possible, we could have communicated changes with more notice, and planned the step-wise escalation and step-down of rotas further in advance.
Allocating some re-deployed staff into task-based groups was very successful. It meant that whole tasks could be delegated away from ICU-trained clinicians, allowing them to focus on other core tasks. It also had the un-anticipated benefit of those redeployed staff feeling that their existing skills were valued and used. Finally, it added flexibility to the stepwise process for escalating and de-escalating staffing.
Overall, if faced with the same scenario again, there are only a few things we would do differently. Firstly, significant advanced planning of the step-wise escalation and step-down of rotas would ease the pressure (and long hours) that were necessary at the time. Related to this, advanced communication and as much notice as possible to the affected staff would hugely help the overall spirit and morale of all staff groups.
Ophthalmologists
With most of our workload being elective procedures, our own speciality was reduced to about 10% of its normal capacity. We wanted to help, so volunteered ourselves for redeployment. We were initially worried how useful we would be, given how different our normal jobs are compared to caring for critically ill patients, but we found ways in which our skills could be useful within the ICU environment. We were energised by the ability to learn practical skills, and to provide ophthalmic teaching. We were also able to provide rapid review in concerns of eye disease or proning injury.
With a week’s notice we were inducted and started work. The urgency of this redeployment could not be avoided but gave us little time to come to terms with the shock of our new roles. Our working patterns changed, going back to doing night shifts after what was a gap of nearly a decade for some of us. Despite these changes, the ICU staff helped immensely by being supportive and the positive feedback we received during our time gave us great motivation to do what we could to help.
Overall, we were impressed by the care taken in shared decision making, consideration of human factors, compassion and communication in relation to patients, relatives and staff, even under these difficult circumstances. The multidisciplinary redeployed cohort brought with them different and interlocking skills, and our experience underlined the value in this diversity.
Lines team
Lines teams were derived from renal and radiology backgrounds, and a range of grades from consultant to ST1. The rota was designed such that renal doctors, who were all able to insert invasive lines independently, worked initially with the most experienced radiology trainee, to develop their skills to complete independence. There was then provision for these radiology trainees to work with a less experienced colleague to build up the latter’s line skills, as well as gaining teaching experience themselves. This proved fortuitous as there were unanticipated national shortages of dialysate suitable for CVVHDF, and so the renal doctors took on additional responsibilities with switching the ICU to running intermittent haemodialysis.
Working with radiology colleagues was a wonderful experience as their ultrasound skills are much more sophisticated than ours, whereas the practical aspects of central venous lines are our stock-in-trade.
As we began to switch to intermittent haemodialysis (IHD) from CVVHDF, due to the national shortages of dialysate fluid, the experiences were more management-based: thinking about the logistics of setting up a new dialysis unit, inside a COVID-19 zone, and for critically unwell patients. In this way, our existing skills were really highly valued by the ICU, and the overall experience will surely serve me well in a future job interview!
Foundation doctors
One advantage Foundation Doctors (FDs) had over other redeployed staff is that we are used to moving to a new clinical area every few months, and so our major concern was of being in a clinical scenario where we felt required to work above our level of training. Our working pattern changed to include nights, and this came with advantages and disadvantages. The night shifts provided a greater exposure to more complex clinical scenarios. This exposure has improved our confidence in managing the critically unwell patient. Out of hours shifts also provided increased opportunities for learning new skills such as line insertions. The disadvantages involved occasionally feeling isolated at night, especially in cases of emergency where there are fewer doctors available on the unit.
At times the PPE, the complexity of the ICU care provided, and the uncertainty of the future were both physically and emotionally exhausting for us. However, the entire FD cohort agrees that our experience on ICU throughout the pandemic has been overwhelmingly positive, and we have learnt the incredible importance of team working.
Proning team – Orthopaedic surgeon
Together with occupational and physiotherapists, we entered the proning training with some excitement and trepidation, a strong “band of brothers” bond forming between us from the off.
Led by an incredible group of ICU physios, we leapt into the work. The department was busy. They had lost staff to isolation and illness. The conditions in PPE were uncomfortable. It quickly became apparent just how demanding the manoeuvre of proning was on manpower numbers and just why our assistance was needed.
The difficulties of the patients themselves became a collective experience of its own form. Seeing so many intubated patients who were so clinically fragile; watching the awful disruption to their physiological parameters from the action of proning them; observing the abject fear in those awake within the ICU setting, and trying my best, from behind my mask, gown and layers of gloves, to reassure them where possible.
Proning team perspective – Physiotherapy assistant
I volunteered to help in the ICU, hoping that my skills with patient handling would be of use to the busy ICU team. A week later I was standing in the small donning room that would become my headquarters for the next few weeks. I met my team: a pairing of therapists and orthopaedic surgeons: helpful, knowledgeable, professional and able to share a joke, I felt at ease. We’d all been provided with very thorough training.
We proned or supinated patients as needed, following the nursing instructions. Things just clicked, and we worked seamlessly. When the prone patients were re-adjusted and safe, we helped roll and clean other patients. All to reduce the workload on the ICU nursing and medical staff.
It was fascinating to see another element of the NHS machinery and learn about a completely different area of work. Pairing therapists with orthopaedic surgeons did seem to provide a great balance of different skills. I felt so valued to be able to utilise my skills in a new way to help. We all had our part to play in that first wave, and I am so glad that my role allowed me to be useful extra help on the front lines.
Intubation team
We were asked to set up the intubation team to support the ICU by intubating patients with COVID-19 whose condition required ventilation. The team would attend intubation calls from the ED, critical care units and from the COVID-19 wards. We had a week’s notification to form a fully functional intubation team rota. There was a sense of urgency as the news from the rapidly escalating number of cases in London hospitals suggested that a surge would require not one but several intubation teams.
We decided that the team would have a minimum of 4 personnel, to ensure a safe balance between working in unfamiliar environments, dealing with very sick patients, and the risks of performing aerosol-generating procedures in patients with COVID-19. The intubation team comprised of 2 anesthetists, at least one of which was a consultant, an operating department practitioner (ODP) or anaesthetic nurse, and another member of staff who could either be a nurse/nursing assistant/trainee ODP.
Staffing the intubation team was perhaps biggest challenge we faced. Registrars were being deployed to ICU and around 20% of the anaesthetic department workforce was either in isolation or shielding at the time. To provide a 24-hour resident service and minimise risks to the team members, we felt it important that the intubation team rota draw from a large pool of staff rather than rely on a few keen individuals who had volunteered for this role. All anaesthetists were asked to volunteer a day and night shift alongside their regular work pattern.
The team needed appropriate PPE to ensure their safety. At this stage there was a lot of conflicting advice on the appropriate levels of PPE and many of the staff had failed fit testing on the FFP3 masks. We secured the Force 10 (full face) and Force 8 (mouth and nose) masks which helped us with recruitment of personnel to the team.
Reflecting overall on our experience, the feedback from the team members was very positive and suggested that having two anaesthetists was an excellent decision as having a “buddy” made it easier to deal with more complex situations. Providing appropriate PPE helped the team members to function with confidence.
Conclusion
In order to prepare for the predicted surge in COVID-19 patients, we increased the capacity of our critical care beds and utilised doctors from all specialties and grades to support the existing ICU staff.
We placed staff in roles where their existing skills could be more easily transferrable and ensured that appropriate support was put in place. We found that by organising some redeployed staff into specific task-oriented teams, this allowed for clear delineation of their roles. It also allowed us to ensure that staff felt appropriately supported and their own training was supported where possible.
We found that staff from broad specialities were able to work in an environment where knowledge and management styles were shared and discussed. In no other time would such collaboration of specialties have been warranted or even possible.
When asked to work outside of one’s own comfort zone, it would be natural to have feelings of apprehension and stress. In general, we found that the feedback we received from redeployed staff was of a positive experience, and to that we attribute the organisation of the roles that allowed us to ensure that no staff member was asked to work unsupported outside of their own capabilities. The redeployed staff members gained skills that would not only serve them in good stead should there be a further surge in demand for critical care beds, but also skills and knowledge that will benefit them in their career as a doctor, regardless of specialty.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
ORCID iDs
Jennifer Doyle https://orcid.org/0000-0002-8828-7725
Eleanor MJS Smith https://orcid.org/0000-0001-9524-4697
Charlotte Willis https://orcid.org/0000-0003-3525-5006
Thomas Stevenson https://orcid.org/0000-0003-3615-7539
References
- 1.World Health Organization. Report Novel Coronavirus (2019-nCoV) situation reports, www.who.int/emergencies/diseases/novel-coronavirus-2019/situation-reports (accessed 2 June 2020).
- 2.Nacoti M, Ciocca A, Giupponi A, et al. At the Epicenter of the Covid-19 Pandemic and Humanitarian Crises in Italy: Changing Perspectives on Preparation and Mitigation. NEJM Catal Innov Care Deliv 2020; 10.1056/CAT.20.0080; (published online March 21, 2020), doi:10.1056/CAT.20.0080.
- 3.Grasselli G, Pesenti A, Cecconi M. Critical care utilization for the COVID-19 outbreak in Lombardy, Italy: early experience and forecast during an emergency response. JAMA 2020; 323: 1545–1546. [DOI] [PubMed] [Google Scholar]
- 4.Fiona G. Covid-19: weathering the storm. Bmj 2020; 368: m1199. [Google Scholar]
- 5.Sir Simon Stevens NHS Chief Executive. Letter to Chief executives of all NHS Trusts and Foundation Trusts, www.england.nhs.uk/coronavirus/wp-content/uploads/sites/52/2020/03/urgent-next-steps-on-nhs-response-to-covid-19-letter-simon-stevens.pdf (2020, accessed 2 June 2020).
- 6.Houston J, Smith D, Nguyen A, et al. Proning in Covid-19; what, why, how? A brief for orthopaedic surgeons. The Transient Journal 2020; (published online April 28, 2020).
- 7.Royal College of Radiologists. Interventional radiology; speciality training curriculum. Implementation, www.rcr.ac.uk/sites/default/files/interventional_radiology_curriculum_2020.pdf. (2020, accessed 2 June 2020).