Abstract
Purpose of the Review:
The prevalence of mental and substance use disorders is three to five times higher than that of the general population. Psychosocial interventions are effective in identifying and managing mental health and substance use disorders. This article aims to review the randomized control studies which have used nonpharmacological interventions alone or in combination with pharmacological interventions for managing mental and substance use disorders in prison/correctional settings.
Collection and Analysis of Data:
Studies included were randomized control trials and pilot randomized studies that assessed the impact of psychosocial interventions for prisoners with mental disorders and substance use disorders. A comprehensive search for articles was done by the primary author (Sreekanth Nair Thekkumkara) in the following databases: PubMed, ProQuest, PsychArticles, and Google Scholar (search engine), for the period June 1, 2000, to December 31, 2020.
Results and Conclusions:
The 21 studies included in the review had a sample size of 34 to 759. The settings of all the interventions were the prison and different types of psychosocial interventions were provided across the studies. The average duration of intervention ranged between 10 min and 120 min with the frequency of one to six sessions per week for 1 to 36 months. All the 21 Randomized Control Trials (RCTs) were nonIndian studies. Overall, the results of the included studies showed significant improvement postintervention (motivational intervention, interpersonal therapy, cognitive behavior therapy, positive psychology intervention, music therapy, and acceptance and commitment therapy) on primary outcome measures such as symptom severity of depression, anxiety, and substance abuse prisoners. Positive effects were observed on secondary outcome measures such as motivation, aggression, follow up rates, and recidivism. A limited number of studies have focused on evaluating psychosocial interventions in prison settings. Most of the interventions were tested in prisoners with substance use disorder alone or in those with dual diagnoses and in high-income countries.
Keywords: Prison, Jail inmates, Mental disorders, Substance use disorders, Psychosocial, Peer intervention
The prevalence of mental health problems in prisons has been three to five times higher than the general population.1–4 Among prisoners, the common mental health problems include anxiety, depression, suicide, and sleep and substance use disorders (SUDs). 5 Studies report that environmental factors in prison include overcrowding, poor hygiene, abuse, poor quality of food, lack of activity, drug use, and forced solitude. Individual factors such as guilt of committing the crime, shame, and a sense of poor social support can all worsen prisoners’ mental health. 6 Undetected, underdetected, and undertreated mental health and substance use disorders among prisoners are increasing public health problems. 7 Most of the studies report poor access to treatment to these problems in prison.1, 8
Psychosocial interventions for mental health problems and SUDs are interpersonal or informational activities, techniques, or strategies that target biological, behavioral, cognitive, emotional, interpersonal, social, or environmental factors to improve health functioning and well-being. 9 Only a few systematic reviews have addressed the effectiveness of various psychological interventions conducted in prison settings for managing mental illnesses and SUDs.10–12 A comprehensive systematic review conducted by Yoon et al. (2017) included studies published until May 2015. However, the review excluded studies with outcomes for substance use and studies that did not provide data to calculate effect size. 11 In this context, the current study aimed to review the randomized controlled trials (RCTs) that used nonpharmacological interventions alone or in combination with pharmacological interventions for managing mental illness and SUDs in prison/ correctional settings.
Methods
Identification and Selection of Studies
We have reported this review based on the Preferred Reporting Items for Systematic Reviews and Meta-Analysis (PRISMA) guidelines 13 and Cochrane collaboration 14 recommendations. The first author (Sreekanth Nair Thekkumkara) did a comprehensive search for articles published between June 1, 2000, and December 31, 2020, in the following databases: PubMed, ProQuest, PsychArticles, and Google Scholar (academic search engine). The search terms used were related to correctional settings such as jail and prisons interventions, therapies, and psychosocial interventions for mental illness and substance abuse, using a combination of “AND” and “OR.” The search strategy has been provided as a supplementary file. The primary outcome measures considered were symptom reduction and improvement. Secondary outcomes considered include reoffending and aggression associated with mental illness or substance use.
Study Eligibility
Type of Study
We included all RCTs and pilot RCTs published between January 1, 2000, and December 31, 2020.
Sample of the Studies
All the studies selected were required to have patients with any of the following mental health disorders as the primary diagnosis or any of the following comorbidity: Schizophrenia, mood (affective) disorders, neurotic, stress-related disorders, and mental and behavioral disorders because of psychoactive substance use, as per International Classification of Diseases (ICD-10) and equivalent diagnosis from the other system (Diagnostic Statistical Manual IV-TR/V).15, 16 The study settings could be in the correctional facility, including juvenile correctional facility, prison, or jail.
Interventions
Studies describing any individual or group psychosocial interventions conducted for prisoners with schizophrenia, mood (affective) disorders, neurotic, stress-related disorders, and mental and behavioral disorders because of psychoactive substance use (and substance use disorders/dependence) in prison settings were included in the review. Interventions for suicide prevention and deliberate self-harm in prison were also included.
Population
The review included studies that had their sample prisoners under the sentence of a court exercising criminal jurisdiction or court-martial, including persons detained in prison under the criminal code of the particular country.
Language
The review was limited to published literature in the English language.
Exclusion Criteria
We excluded studies with fewer than ten experimental subjects and prepost (single group) and feasibility studies. Studies that reported psychosocial interventions for Posttraumatic Stress Disorder (PTSD) only, studies that examined interventions conducted for prisoners with personality disorders, rehabilitation process of prisoners without any mental health conditions or SUDs, and studies conducted in places other than prison or jail were excluded too. Interventions for medical conditions were also excluded.
Data Extraction, Quality Assessment, and Data Analysis
Data were extracted using a data extraction form developed for the study. The parameters recorded included selection criteria and type of participants, intervention, study design, outcome measures, and results. Sreekanth Nair Thekkumkara screened titles and abstracts and selected articles that met the inclusion criteria. He did data extraction and screening independently, and Aarti Jagannathan and Krishna Prasad Muliyala independently reviewed the selected articles based on the inclusion criteria. The authors discussed any disagreements and arrived at a consensus. The sources of biases were assessed to ensure the quality of the studies. Sreekanth Nair Thekkumkara, Aarti Jagannathan, and Krishna Prasad Muliyala evaluated the risk of bias independently according to the Cochrane risk of bias tool for RCTs. They categorized the studies as having low risk, high risk, and unclear risk of bias, based on random sequence generation, allocation concealment, blinding of participants and personnel, blinding of outcome assessment, incomplete outcome data, selective reporting, and other sources of bias. 14 The reasons for excluding studies were documented.
Results
Literature Review
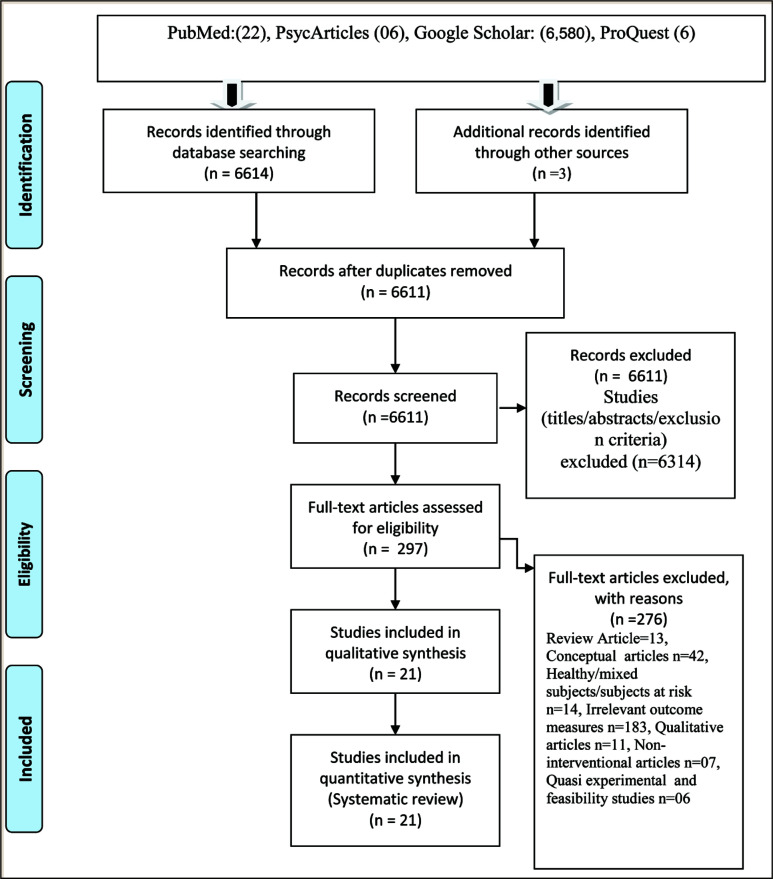
The literature search retrieved a total of 6,614 studies/articles published during the period. Figure 1 shows the PRISMA flowchart of the selection process. Two hundred ninety-seven articles were included in the screening after removing duplicates. The number of studies was further reduced to 21 after removing 276 articles. The 21 RCTs included in the systematic review are summarized in Table S1.
Figure 1. Prisma Flow Chart.
Study Characteristics
In the review, though interventions were similar in a few studies,17–21 the outcome variables, outcome assessment, and duration of the intervention were heterogeneous and therefore not conducive for a meta-analysis.
Socio-Demographic Details
The sample size of the participants in the included studies ranged from 34 to 759. Twenty studies were conducted in high-income countries (USA 10,18, 19, 21–28 UK 3,29–31 Netherlands 1, 32 Norway 1, 33 Spain 2,34, 35 China 2,36, 37 and Sweden 1 38 ; one study was conducted in an upper-middle-income country Malaysia). 39 There were no studies that were conducted in middle-income or lower- income countries.
Types of Psychosocial Interventions
The intervention group underwent different therapies such as motivation enhancement therapy (MET),17, 18, 21, 28, 40 seeking safety program, 41 cognitive behavior therapy (CBT), 42 interpersonal therapy (IPT), 25 acceptance and commitment therapy (ACT),34, 35 cognitive behavioral suicidal prevention therapy (CBSP), 43 group interpersonal psychotherapy,24, 44 music therapy,33, 37 art therapy, 36 group psychological intervention, 31 and mindfulness-based relapse prevention intervention. 27 The average duration of intervention in the studies ranged from 10 min to 120 min, with the frequency of sessions being one per week to six per week across one month to six months. The follow-up period ranged from 1 month to 12 months. The control group in most studies underwent standard care with pharmacological therapy, CBT, IPT, relaxation techniques, or educational programs. In some studies, the control group was not provided any intervention or was waitlisted. In all the studies, the focus was on the primary outcome measures such as symptom severity and motivation; only three studies highlighted secondary outcome measures such as aggression, 45 follow-up rates, 17 and cost-effectiveness. 24
Interventions for Substance Use and Mental Disorders
Four studies adapted brief motivational intervention (MI) for alcohol and SUDs.17, 21, 28, 40 The majority of the interventions included in the review were delivered by trained mental health professionals (MHPs) in prison. Only in one study intervention was provided by trained prison staff. 32 One study that compared the effectiveness of MI delivered by professionals after obtaining training in different modes, such as workshop mode, individually supervised and a combination of both modes found that the substance use reduced in all three groups. 38
Most of the interventions in the review (14 studies) were provided for prisoners with SUDs alone or dual diagnosis. Interventions in four studies were for prisoners with depression alone, in another study was for suicide prevention in prison, in two other studies were to improve the mental wellbeing of prisoners with schizophrenia, and in two other studies were for any common mental disorders (CMDs). Three studies (one provided in group format and another two studies in individual form) compared IPT with treatment as usual (TAU) among the prisoners with depression and showed improvement in anxiety symptoms.24, 44
One of the interventions for prisoners with SUDs was mindfulness- based relapse prevention, a structured program similar to mindfulness-based stress reduction and included yoga with additional discussion of applying mindfulness to prevent relapse to drug and alcohol use. The study demonstrated a reduction in craving and substance use in the intervention arm. 27 The interventions for SUDs reduced craving, the risk associated with substance use, harmful use, and drug-related criminal activity and improved follow-up rates.
Other interventions that showed a moderate effect on the outcome variables include CBT (n = 2) and ACT (n = 1).35, 43 Studies on music therapy (n = 2) to engage prisoners with depressive and anxiety disorders and associated problems found that compared with standard care in the prison, anxiety and depression in the music therapy group decreased significantly at mid-test (after ten sessions) and posttest (after 20 sessions); self-esteem improved substantially among the participants in the music therapy group.33, 37 Further, one of the art-based interventions among prisoners with schizophrenia decreased the levels of anxiety, depression, and anger and increased social interaction and medication compliance compared to the waitlisted group. 36
Four pilot RCTs were included in our review. One 44 discussed the practicality of conducting a group IPT for female prisoners diagnosed with mental health problems. The group IPT consisted of 60 min to 75 min group sessions, three times per week for eight weeks, plus pregroup, mid-group, and postgroup individual sessions in prison. Another pilot, randomized study about structured writing therapy interventions 42 consisted of three phases: Self-confrontation, cognitive reappraisal, and sharing/farewell for prisoners with posttraumatic stress disorder (PTSD) with SUD. This study found a significant decrease in PTSD severity from mid-treatment to posttreatment in the intervention group. In contrast, there were no significant changes in the outcome abstinence from the substance in the TAU group from posttreatment to follow-up. Another pilot study41, 21 compared ACT with CBT for prisoners with polysubstance use and demonstrated that ACT showed greater results than CBT in abstinence rates. In the CBT group, reductions were observed in the levels of anxiety sensitivity at posttreatment and at 12-month and 18-month follow-up. People in the ACT group had decreased scores in anxiety severity index (ASI) cognitive subscale at 18-month follow-up.
Overall, the included studies showed significant improvement postintervention (MI, IPT, CBT, positive psychology intervention, music therapy, and ACT) on primary outcome measures such as symptom severity of depression, anxiety, substance abuse, and deliberate self-harm. Positive effects were observed on secondary outcome measures such as motivation, aggression, follow-up rates, and recidivism. These have been summarized in Table S1. The quality of studies included in the review was assessed using the Cochrane collaboration of risk of bias tool (S 2).
Discussion
The review highlights the benefits of addressing the psychosocial issues of prisoners with SUDs and comorbid conditions, such as reduction of symptoms severity and abstinence from substance use.
Most studies focused on the management of SUDs (14 out of 21 studies), and only seven focused on mental illness. The reason for this result could be the high prevalence of substance use among prisoners compared to other MI.8, 41 Several theories in criminology have also established the connection between crime and the use of substances.46–48 We also observed a lack of studies for managing aggression and crime associated with substance use in the prison setting.46–48
Only one intervention was directly related to suicide prevention, 43 though prevalence studies have reported high rates of suicide among prisoners. 49 Suicide rates are 9 to 14 times higher than the general population, because of multiple factors such as institutional factors, individual vulnerabilities, and poor coping skills. The first phase of imprisonment, the early phase of long-term sentences, history of psychiatric illness, suicidal behavior, intoxication, and isolation have been considered risk factors for suicide in prisons. 43 Therefore, there is a need to develop and evaluate comprehensive psychosocial interventions to prevent suicide among prisoners.
Only two studies had tested psychosocial interventions for prisoners with severe mental health problems, even though their prevalence is high in the prisons. 1 Only six studies focused on prisoners with CMD such as depression and anxiety disorders. Studies report challenges in designing RCTs in prison settings, including practical difficulties in randomization, lack of cooperation from the prison authorities, and poor sensitization among the staff for referral. 11
Music therapy effectively reduced anxiety and depression, as measured by symptom severity and self-esteem, among male prisoners.33, 37 However, it is essential to examine its effectiveness for other populations such as female prisoners and adolescent delinquents and investigate different outcomes (e.g., social skills, aggression management, impulse control, empathy) relating to psychosocial wellbeing, behaviors, and cognitive functions.50, 51
In most studies,18, 33, 35, 44, 52 significant improvement was noted in primary and secondary outcomes.32, 38, 44, 53 The nonsignificant difference in results in some of the studies could be attributed to small sample size, duration and type of intervention, possible level of expertise or training of the persons who delivered the interventions, fidelity, and performance/adherence levels of the participants. Most interventions focused on symptom severity and improvement; however, outcome variables such as cost-effectiveness of conducting the intervention, time duration of the interventions, and their feasibility and long-term outcomes have not been assessed in many studies. This information is crucial in developing a country-specific intervention package or adapting existing interventions in low-resource settings.
Most interventions were provided by either MHP or trained prison staff. One study used peer-group interventions to address SUD among the prisoners, 52 which improved substance use. Most studies have been conducted in higher- income or upper-middle-income countries, and there is an absence of published studies from lower and middle-income countries such as India. In high-income countries, the mental health care budget covers the services in the prison setting. 54 The mental health care budget is only 1.6% of India’s health budget. 55 Also, our findings suggest an improvement in the outcome measures through MHP-led interventions. However, there is a poor ratio of dedicated MHP to prisoners in the lower, middle-income countries. Thus, alternative systems that utilize existing resources need to be explored. One such cost-effective approach could be through training and using peers (prisoners who are ready to engage in voluntary activities) to screen and provide essential psychosocial support to prisoners with CMDs or SUDs, under the supervision of MHPs. Studies have reported the benefits of peer-led intervention programs in various settings, including prisons.52, 56–58 The models presented in these studies can be culturally adapted and tested in the prison settings in India.
Strengths
The selection of studies was restricted to RCTs and quasi-experimental studies. While reporting, we adhered to the PRISMA guidelines. The quality of all the trials was assessed independently by three authors using the robust Cochrane Collaboration’s tool for assessing risk of bias in randomized trials.
Limitations
We reviewed papers published in the English language only and hence may have missed studies published in other languages. We did not include studies that examined outcomes such as distress, psychological wellbeing, or self-esteem only. We also excluded interventions conducted for PTSD, considering the low prevalence of PTSD in prisons(0.3%) in India. 59 Meta-analysis was not possible because of the heterogeneity in the outcome variables, interventions, intervention duration, and follow-up period. We excluded studies that examined interventions conducted for prisoners with personality disorders.
However, one of the purposes of the review was to summarize a broad range of interventions for various mental disorders and SUDs that can potentially be tested for feasibility and effectiveness in resource-poor settings.
Conclusions and Future Directions
A limited number of studies have evaluated psychosocial interventions in prison settings. Most interventions were tested in prisoners with SUDs alone or those with dual diagnoses and in high-income countries. There is a need to develop sustainable and viable models of care in resource-poor settings. Innovative peer-support interventions could effectively deliver mental health care for prisoners with mental health problems in such settings.
Supplemental Material
Supplemental material for this article is available online.
Footnotes
Declaration of Conflicting Interests: The authors declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The authors received no financial support for the research, authorship, and/or publication of this article.
References
- 1.Fazel S and Danesh J. Serious mental disorder in 23000 prisoners: A systematic review of 62 surveys. Lancet, 2002; 359(9306): 545–550. [DOI] [PubMed] [Google Scholar]
- 2.Daniel AE. Preventing suicide in prison: A collaborative responsibility of administrative, custodial, and clinical staff. J Am Acad Psychiatry Law, 2006; 34: 165–175. [PubMed] [Google Scholar]
- 3.Swetz A, Salive ME, Stough T, et al. The prevalence of mental illness in a state correctional institution for men. J Prison Jail Health, 1989; 8(1): 3–15. [Google Scholar]
- 4.Watson R, Stimpson A, and Hostick T. Prison health care: A review of the literature. Int J Nurs Stud, 2004; 41: 119–128. [DOI] [PubMed] [Google Scholar]
- 5.Brinded PM, Simpson AI, Laidlaw TM, et al. Prevalence of psychiatric disorders in New Zealand prisons: A national study. Aust N Z J Psychiatry., 2001; 35(2): 166–173. [DOI] [PubMed] [Google Scholar]
- 6.Møller L, Gatherer A, Juergens R, et al. Health in prisons: A WHO guide to the essentials in prison health. World Health 2007: 179. http://www.euro.who.int/__data/assets/pdf_file/0009/99018/E90174.pdf [Google Scholar]
- 7.Uche N and Princewill S. Clinical factors as predictors of depression in a Nigerian prison population. Afr J Psychiatry (South Africa), 2016; 19(1): 1–6. http://www.embase.com/search/results?subaction=viewrecord&from=export&id=L608524330%5Cn http://dx.doi.org/10.4172/2378-5756.1000345%5Cn http://sfx.library.uu.nl/utrecht?sid=EMBASE&issn=19948220&id=doi:10.4172%2F2378-5756.1000345&atitle=Clinical+factors+as+p [Google Scholar]
- 8.Steadman HJ, Osher FC, Robbins PC, et al. Prevalence of serious mental illness among jail inmates. Psychiatr Serv, 2009; 60(6): 761–765. [DOI] [PubMed] [Google Scholar]
- 9.Elliott JO. Psychosocial interventions for mental and substance use disorders: A framework for establishing evidence-based standards, by Institute of Medicine (IOM). J Soc Work Pract Addict, 2016; 16(3): 323–324. [Google Scholar]
- 10.Morgan RD, Flora DB, Kroner DG, et al. Treating offenders with mental illness: A research synthesis. Law Hum Behav, 2012; 36(1): 37–50. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yoon IA, Slade K, and Fazel S. Outcomes of psychological therapies for prisoners with mental health problems: A systematic review and meta-analysis. J Consult Clin Psychol, 2017; 85: 783–802. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Batastini AB, King CM, Morgan RD, et al. Telepsychological services with criminal justice and substance abuse clients: A systematic review and meta-analysis. Psychol Serv, 2016; 13(1): 20–30. [DOI] [PubMed] [Google Scholar]
- 13.Title T. PRISMA 2009 Checklist PRISMA 2009 checklist. PLoS Med, 2009. http://currents.plos.org/disasters/files/2013/11/Power-OUtages-PRISMA-2009-Checklist.pdf [Google Scholar]
- 14.S Green; JPT Higgins. Cochrane Handbook for Systematic Reviews of Interventions - Version 5.0.2. Cochrane Collaboration 2009. http://www.cochrane.org/handbook/handbook-information
- 15.World Health Organization. The ICD-10 classification of mental and behavioural disorders: Diagnostic criteria for research. World Health Organization, 1993. [Google Scholar]
- 16.American Psychiatric Association. DSM-5 diagnostic classification. In: Diagnostic and Statistical Manual of Mental Disorders. American Psychiatric Association; 2013. [Google Scholar]
- 17.Davis TM, Baer JS, Saxon AJ, et al. Brief motivational feedback improves post- incarceration treatment contact among veterans with substance use disorders. Drug Alcohol Depend, 2003; 69(2): 197–203. [DOI] [PubMed] [Google Scholar]
- 18.Stein MD, Caviness CM, Anderson BJ, et al. A brief alcohol intervention for hazardously drinking incarcerated women: Research report. Addiction, 2010; 105(3): 466–475. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Stein LAR, Clair M, Lebeau R, et al. Motivational interviewing to reduce substance-related consequences: Effects for incarcerated adolescents with depressed mood. Drug Alcohol Depend, 2011; 118(2–3): 475–478. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kopak AM, Dean L V., Proctor SL, et al. Effectiveness of the rehabilitation for addicted prisoners trust (RAPt) programme. J Subst Use, 2015; 20(4): 254–261. [Google Scholar]
- 21.Owens MD and McCrady BS. A pilot study of a brief motivational intervention for incarcerated drinkers. J Subst Abuse Treat, 2016; 68: 1–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Davis TM, Baer JS, Saxon AJ, et al. Brief motivational feedback improves post-incarceration treatment contact among veterans with substance use disorders. Drug Alcohol Depend, 2003; 69(2): 197–203. [DOI] [PubMed] [Google Scholar]
- 23.Rowe M, Bellamy C, Baranoski M, et al. A peer-support, group intervention to reduce substance use and criminality among persons with severe mental illness. Psychiatr Serv, 2007; 58(7): 955–961. [DOI] [PubMed] [Google Scholar]
- 24.Johnson JE and Zlotnick C. A pilot study of group interpersonal psychotherapy for depression in substance-abusing female prisoners. J Subst Abuse Treat, 2008; 34(4): 371–377. [DOI] [PubMed] [Google Scholar]
- 25.Johnson JE and Zlotnick C. Pilot study of treatment for major depression among women prisoners with substance use disorder. J Psychiatr Res, 2012; 46(9): 1174–1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Johnson JE, Stout RL, Miller TR, et al. Randomized cost-effectiveness trial of group interpersonal psychotherapy (IPT) for prisoners with major depression. J Consult Clin Psychol, 2019; 87(4): 392–406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Lyons T, Womack VY, Cantrell WD, et al. Mindfulness-based relapse prevention in a jail drug treatment program. Subst Use Misuse, 2019; 54(1): 57–64. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Stein LAR, Martin R, Clair-Michaud M, et al. A randomized clinical trial of motivational interviewing plus skills training vs. relaxation plus education and 12-Steps for substance using incarcerated youth: Effects on alcohol, marijuana and crimes of aggression. Drug Alcohol Depend, 2020. February 1; 207: 107774. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Pratt D, Tarrier N, Dunn G, et al. Cognitive-behavioural suicide prevention for male prisoners: A pilot randomized controlled trial. Psychol Med, 2015; 45(16): 3441–3451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 30.Lennox C, Kirkpatrick T, Taylor RS, et al. Pilot randomised controlled trial of the ENGAGER collaborative care intervention for prisoners with common mental health problems, near to and after release. Pilot Feasibility Stud, 2018; 4: 15. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Taylor PJ, Playle R, Robling M, et al. A randomized controlled trial of a group psychological intervention to increase locus of control for alcohol consumption among alcohol-misusing Short-term (male) prisoners (GASP). Addiction, 2020. October 1 (cited 2021, August 27); 115(10): 1844–1854. [DOI] [PubMed] [Google Scholar]
- 32.van Dam D, Ehring T, Vedel E, et al. Trauma-focused treatment for posttraumatic stress disorder combined with CBT for severe substance use disorder: A randomized controlled trial. BMC Psychiatry, 2013; 13: 172. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Gold C, Assmus J, Hjørnevik K, Qvale LG, Brown FK, Hansen AL, et al. Music therapy for prisoners: Pilot randomised controlled trial and implications for evaluating psychosocial interventions. Int J Offender Ther Comp Criminol, 2014; 58(12): 1520–1539. [DOI] [PubMed] [Google Scholar]
- 34.Lanza PV, García PF, Lamelas FR, et al. Acceptance and commitment therapy versus cognitive behavioral therapy in the treatment of substance use disorder with incarcerated women. J Clin Psychol, 2014; 70(7): 644–657. [DOI] [PubMed] [Google Scholar]
- 35.González-Menéndez A, Fernández P, Rodríguez F, et al. Long-term outcomes of acceptance and commitment therapy in drug-dependent female inmates: A randomized controlled trial. Int J Clin Health Psychol, 2014; 14(1): 18–27. [Google Scholar]
- 36.Qiu HZ, Ye ZJ, Liang MZ, et al. Effect of an art brut therapy program called go beyond the schizophrenia (GBTS) on prison inmates with schizophrenia in mainland China—A randomized, longitudinal, and controlled trial. Clin Psychol Psychother, 2017. September 1 (cited 2021, August 27); 24(5): 1069–1078. [DOI] [PubMed] [Google Scholar]
- 37.Chen XJ, Hannibal N, and Gold C.. Randomized trial of group music therapy with Chinese prisoners: Impact on anxiety, depression, and self-esteem. Int J Offender Ther Comp Criminol, 2016. July 1 (cited 2021, June 9); 60(9): 1064–1081. [DOI] [PubMed] [Google Scholar]
- 38.Forsberg LG, Ernst D, Sundqvist K, et al. Motivational interviewing delivered by existing prison staff: A randomized controlled study of effectiveness on substance use after release. Subst Use Misuse, 2011; 46: 1477–1485. [DOI] [PubMed] [Google Scholar]
- 39.Mariamdaran SD, Madya NA, and Ishak NA. The effectiveness of PPP intervention on aggression, depression and ability changes among prison inmates in Malaysia. Procedia - Soc Behav Sci, 2014; 112: 47–56. [Google Scholar]
- 40.Stein LAR, Lebeau R, Colby SM, et al. Motivational interviewing for incarcerated adolescents: Effects of depressive symptoms on reducing alcohol and marijuana use after release. J Stud Alcohol Drugs, 2011; 72(3): 497–506. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.Wolff N, Frueh BC, Shi J, et al. Effectiveness of cognitive-behavioral trauma treatment for incarcerated women with mental illnesses and substance abuse disorders. J Anxiety Disord, 2012; 26(7): 703–710. [DOI] [PubMed] [Google Scholar]
- 42.Lanza PV, García PF, Lamelas FR, et al. Acceptance and commitment therapy versus cognitive behavioral therapy in the treatment of substance use disorder with incarcerated women. J Clin Psychol, 2014; 70(7): 644–657. [DOI] [PubMed] [Google Scholar]
- 43.Pratt D, Tarrier N, Dunn G, et al. Cognitive-behavioural suicide prevention for male prisoners: A pilot randomized controlled trial. Psychol Med, 2015; 45(16): 3441–3451. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Johnson JE and Zlotnick C.. Pilot study of treatment for major depression among women prisoners with substance use disorder. J Psychiatr Res, 2012; 46(9): 1174–1183. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Rowe M, Bellamy C, Baranoski M, et al. A peer-support, group intervention to reduce substance use and criminality among persons with severe mental illness. Psychiatr Serv, 2007; 58(7): 955–961. [DOI] [PubMed] [Google Scholar]
- 46.Benda BB. Gender differences in life-course theory of recidivism: A survival analysis. Int J Offender Ther Comp Criminol, 2005; 49(3): 325–342. [DOI] [PubMed] [Google Scholar]
- 47.Bahr SJ, Masters AL, and Taylor BM. What works in substance abuse treatment programs for offenders? Prison J, 2012; 92: 155–174. [Google Scholar]
- 48.Coviello DM, Zanis DA, Wesnoski SA, et al. Does mandating offenders to treatment improve completion rates?. J Subst Abuse Treat, 2013; 44(4): 417–425. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Frühwald S and Frottier P.. Suicide in prison. Lancet, 2005; 366(9493): 1242–1244. doi: 10.1016/S0140-6736(05)67327-8 [DOI] [PubMed] [Google Scholar]
- 50.Bowes N, McMurran M, Williams B, et al. Treating alcohol-related violence: Intermediate outcomes in a feasibility study for a randomized controlled trial in prisons. Criminal Justice Behav, 2012; 39(3): 333–344. [Google Scholar]
- 51.Sung HE. Prevalence and risk factors of violence-related and accident-related injuries among state prisoners. J Correctional Health Care, 2010. (cited 2021, June 9); 16(3): 178–187. [DOI] [PubMed] [Google Scholar]
- 52.Rowe M, Bellamy C, Baranoski M, et al. A peer-support, group intervention to reduce substance use and criminality among persons with severe mental illness. Psychiatr Serv, 2007; 58(7): 955–961. [DOI] [PubMed] [Google Scholar]
- 53.Bowes N, McMurran M, Evans C, et al. Treating alcohol-related violence: A feasibility study of a randomized controlled trial in prisons. J Forensic Psychiatry Psychol, 2014; 25(2): 152–163. [Google Scholar]
- 54.White P and Whiteford H. Prisons: Mental health institutions of the 21st century? Med J Aust, 2006; 185(6): 302–303. [DOI] [PubMed] [Google Scholar]
- 55.Das A. Union budget 2019: Sitharaman’s aims to boost India’s digital payment. Inc42, 2019. [Google Scholar]
- 56.South J, Woodall J, Kinsella K, et al. A qualitative synthesis of the positive and negative impacts related to delivery of peer-based health interventions in prison settings. BMC Health Serv Res, 2016; 16(1): 525. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.South J, Bagnall A-M, Hulme C, et al. A systematic review of the effectiveness and cost-effectiveness of peer-based interventions to maintain and improve offender health in prison settings.Southampton, UK: NIHR Journals Library; 2014 Oct. (Health Services and Delivery Research, No. 2.35). https://www.ncbi.nlm.nih.gov/books/NBK260146/doi:10.3310/hsdr02350 [PubMed]
- 58.Lloyd-Evans B, Mayo-Wilson E, Harrison B, et al. A systematic review and meta-analysis of randomised controlled trials of peer support for people with severe mental illness. BMC Psychiatry, 2014; 14(1): 39. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 59.Math SB, Murthy P, Parthasarathy R, et al. Mental health and substance use problems in prisons. The Bangalore prison mental health study; local lessons for national action. NIMHANS, 2011. ISBN NO: 81-86430-00-8 Publication no: 78
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material for this article is available online.