Abstract
We describe a simple, cost-efficient, double-selective method for isolation of wild-type poliovirus from sewage samples containing vaccine polioviruses and other enteroviruses, with a detection limit of 18 to 50 PFU per 1 to 2 liters of sewage. By this method we were able to process 1,700 sewage samples collected between 1991 and 1996, from which 10,472 plaques were isolated, 41 of them being identified as wild-type polioviruses.
Environmental surveillance has been recognized as one of the methods which can be used to monitor the circulation of wild-type poliovirus in populations, for evaluation of the effectiveness of polio immunization, and for epidemiological investigations (3, 10, 11, 14, 19, 21, 26). In Israel, environmental surveillance was implemented in 1989 following an outbreak of poliomyelitis (9, 24, 25). Laboratory analysis of sewage samples involves several steps, for which various protocols were developed (1, 2, 8, 14, 22, 28). The presence of oral polio vaccine and nonpoliovirus enteroviruses (NPEV) often complicates such protocols. We therefore developed a double-selective tissue culture system based on the preferential growth of polioviruses on HEp-2 cells compared with NPEV (13) and selection against vaccine-derived polioviruses at 40°C (18).
Raw sewage samples were collected from central sewage treatment facilities of 36 communities all over the country by either automatic composite sampling over 24 h, manual “grab” sampling every half hour during the two peak-capacity morning hours, or continuous absorption sampling by placement of a gauze pad in the sewage stream for 24 to 48 h. One to two liters of sewage or the soaked gauze pads were kept at 4°C and then treated within 1 to 13 days of collection.
For virus extraction, the samples were allowed to settle for at least 24 h at 4°C. Most of the top (aqueous) phase was discarded, and the bottom 250 ml, including sediment, was retained. Virus extraction was performed as initially described by Berg et al. (1, 2). Twenty milliliters of Freon 113, 30 ml of glycine buffer (pH 9.0), and 0.5 g of Bentonite were added to the sewage sample, which was then homogenized for 1 to 2 min at low speed and sedimented for 20 min at 4,000 rpm (6,000 × g) and 4°C. A 100-ml portion of the supernatant was kept and mixed with 4 ml of 10× concentrated tissue culture medium M199 supplemented with antibiotics (final concentrations: penicillin, 400 U/ml; streptomycin, 0.8 mg/ml; nystatin (Mycostatin), 50 U/ml; and neomycin, 0.5 mg/ml). Sewage samples collected on gauze pads were placed in containers with 100 to 200 ml of saline (enough to cover the pad), 20 ml of Freon 113, 30 ml of glycine buffer (pH 9.0), and 0.5 g of Bentonite. The container was shaken vigorously for 30 min, the gauze pad was removed, and the solution was treated in the same way as the liquid samples. The samples were used to inoculate tissue cultures (see below). If no viruses were isolated, 40 ml of the sample was subjected to ultracentrifugation at 4°C in a Beckman L7 ultracentrifuge with an SW28 rotor at 27,000 rpm (150,000 × g). The pellet was resuspended in 14 ml of M199 medium containing all antibiotics. If too many plaques were found, the sample was diluted and reinoculated.
BGM (Buffalo green monkey) cells (6) were used for the initial isolation of enterovirus plaques. The cells were maintained in M199 medium containing 10% fetal calf serum. Each of three 10-cm tissue culture plates with BGM cells was inoculated with 4.5 ml of the treated sewage sample. The rest of the treated sample was stored at −20°C. Enterovirus plaques were isolated by standard protocols (9).
HEp-2 (human larynx carcinoma) cells were used for selection of wild-type poliovirus. The cells were plated at 2 × 105/ml in tissue culture tubes and grown in Eagle’s minimal essential medium containing 10% fetal calf serum and antibiotics at 37°C and permitted to form monolayers. Plaques isolated on BGM cells were collected into 0.2 ml of M199 medium and transferred to the HEp-2 tubes and incubated at 40°C in 5% CO2 for 5 days in a sealed incubator to maintain constant temperature. Tubes showing cytopathic effect (CPE) were subpassaged back on BGM cells and analyzed by microneutralization assays for identification of viral isolates according to standard protocols (28). Polyclonal antibodies were used for virus typing, and monoclonal antibodies were used for intratypic differentiation between wild-type and vaccine strains. The monoclonal antibodies were supplied by Radu Crainic, Pasteur Institute, Paris (5, 27).
We have evaluated every step in our protocol. The fractionation of virus particles in sewage samples was examined to reassess the results of previous studies (1, 2), which showed that the organic and particulate materials in an environmental sample are highly enriched in virus particles. We have compared the number of enterovirus plaques obtained on BGM cells after plating 15-ml extracts from the 250-ml bottom phases (containing most of the organic material) with the number obtained after plating extracts from the 750-ml top phases of 15 randomly selected, 1-liter sewage samples. The average numbers of plaques per milliliter obtained were 0.58 and 0.30 from the bottom and the top phases, respectively. Thus, on average, there were 145 PFU in the 250-ml bottom phases and 225 PFU in the 750-ml top phases, which corresponds to 40% and 60% in the bottom and top phases, respectively.
To reevaluate the selective power of HEp-2 cells in comparison to BGM cells (13, 28) and to obtain appropriate assay conditions, we inoculated HEp-2 and BGM cells concomitantly with six NPEV strains—Echovirus 3, Echovirus 7, Echovirus 9, Echovirus 30, Coxsackievirus A21, and Coxsackievirus B3 (wild type isolates from our laboratory)—and the three wild-prototype polioviruses Mahoney, MEF-1, and Saukett (obtained from Radu Crainic, Pasteur Institute, Paris), which were titrated to end point at 37°C. The results are shown in Table 1. This experiment confirmed that HEp-2 cells are highly permissive for growth of wild-type polioviruses and less permissive for growth of most other NPEV. Thus, a significant degree of selectivity could be obtained if the cultures were maintained for only 5 days. However, the actual level of selectivity for unknown wild-type enteroviruses could be assessed only during field trials, as described below.
TABLE 1.
Replication of wild-type polioviruses and enteroviruses on BGM and HEp-2 cells
| Virus | BGM
|
HEp-2
|
||
|---|---|---|---|---|
| Virus titer (log TCID50) | Days to full CPE | Virus titer (log TCID50) | Days to full CPE | |
| Poliovirus type 1 | 7.25 | 5 | 6.50 | 5 |
| Poliovirus type 2 | 7.00 | 5 | 7.00 | 5 |
| Poliovirus type 3 | 7.50 | 5 | 7.25 | 5 |
| Echovirus 3 | 4.25 | 8 | 4.75 | 8 |
| Echovirus 7 | 7.50 | 8 | 0.25 | 10 |
| Echovirus 9 | 0.05 | 10 | 0.05 | 10 |
| Echovirus 30 | 4.00 | 8 | 0.25 | 10 |
| Coxsackievirus B3 | 6.75 | 8 | 0.25 | 10 |
| Coxsackievirus A21 | 0.05 | 10 | 0.05 | 10 |
The RCT (reproductive capacity at supraoptimal temperature) marker is not a definitive marker, and when used as a selector it will allow growth of about 1% of vaccine-derived type 1 and 2 isolates and 30% of type 3 isolates while selecting against 30 to 35% of the wild-type 1,2 and 3 isolates (18). However, it can provide a fast and easy way for screening a large number of isolates. We have not reassessed the selectivity of the RCT marker, since it is well established.
We have combined the two selective tools, growth on HEp-2 cells and growth at 40°C, to eliminate the high background of NPEV and vaccine-derived polioviruses by propagation of plaque-purified enteroviruses on HEp-2 cells at 40°C for 5 days. Only isolates which grew at these conditions were further analyzed.
To assess the detection limit of our isolation and double-selection protocol, we performed a reconstruction experiment. Half of each of the bottom phases from three arbitrary sewage samples (with varied volumes) were spiked with 100 50% tissue culture infective doses (TCID50) (approximately 100 PFU) of wild poliovirus type 1, while the second half remained untreated. Both groups were processed concomitantly according to the standard protocol, and each plaque which passed the selection of HEp-2 cells at 40°C was further identified as a poliovirus or NPEV. When the nonspiked group of samples was found to be negative for wild-type poliovirus, we could consider the poliovirus plaques obtained from the spiked samples as resulting only from the spiking virus. The results of this experiment are shown in Table 2. The average number of poliovirus type 1 plaques obtained from the spiked samples was 5, which corresponds to a 5% recovery rate. If a 40-ml sample was concentrated by ultracentrifugation and inoculated instead of the 14.5 ml of unconcentrated sample used in the standard protocol, the recovery rate increased to 14%. This means that the bottom phase of a sewage sample must contain at least 20 PFU (100%) of wild-type poliovirus to meet the minimum of one plaque detectable after processing (5%), and taking into account the distribution of virus between the bottom and the top phases calculated above (40% and 60%, respectively) it implies that the entire sewage sample should contain at least 50 PFU (or 18 PFU if concentration of the extract by ultracentrifugation is to be used). Thus, the overall detection limit of our standard protocol was 18 to 50 PFU per sewage sample.
TABLE 2.
Recovery rates of wild poliovirus type 1 from sewage samples
| Sample no. | No. of TCID50 inoculateda | No. of PFU inoculatedb | No. of poliovirus type 1 plaques obtainedc | % Recoveryd |
|---|---|---|---|---|
| 1 | 100 | 86 | 3 | 3.5 |
| 2 | 100 | 119 | 4 | 3.4 |
| 3 | 100 | 102 | 9 | 8.8 |
| Avg | 100 | 102 | 5 | 5 |
Twenty milliliters of a stock of 5 × 106 TCID50/ml, diluted 106-fold, was inoculated into half of each of the sewage samples.
Each dilution used for inoculation was titrated in parallel by plaque assay on the same BGM monolayer used for processing the sewage sample.
Following selection in HEp-2 cells and identification of poliovirus type 1 plaques.
Number of poliovirus type 1 plaques obtained per number of PFU inoculated.
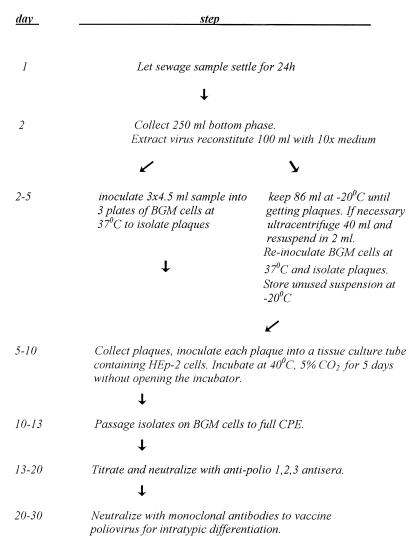
The new protocol was implemented in mid-1991 and has been in use without any significant changes between 1991 and 1996. A flow chart of the entire protocol is shown in Fig. 1. Completion of the entire protocol took between 3 and 5 weeks. However, the first indication that a wild-type poliovirus was found in a sewage sample could be obtained between 10 and 14 days after inoculation.
FIG. 1.
Flow chart of the wild-type poliovirus isolation protocol.
The selective protocol allowed us to increase the number of plaques screened by the double selection, thereby increasing the chances of isolating wild-type poliovirus. A comparative evaluation of the efficiencies of the protocols used before 1991 (selection for wild-type poliovirus on BGM cells at 40°C) and since mid-1991 (selection for wild-type poliovirus on HEp-2 cells at 40°C) is based on the information presented in Table 3. Between 1992 and 1996, 1,545 sewage samples were processed by the new protocol, while about 253 were processed by the old method (in 1989 and 1990). During 1991 the new protocol was first introduced and continuously changed and improved, and thus we did not include this year in the statistics.
TABLE 3.
Number and type of environmental isolates obtained between 1989 and 1996
| Year | No. of:
|
|||||
|---|---|---|---|---|---|---|
| Sewage samples processed | Plaques screened | Isolates analyzed by neutralization | NPEV isolates | Vaccine poliovirus isolates | Wild-type poliovirus isolates | |
| 1989a | 85 | 727 | 213 | 206 | 7 | 0 |
| 1990a | 168 | 1,463 | 231 | 224 | 7 | 1 |
| 1991c | 157 | 584 | 26 | 2 | 21 | 3 |
| 1992b | 260 | 1,823 | 16 | 9 | 7 | 0 |
| 1993b | 284 | 1,605 | 17 | 10 | 7 | 0 |
| 1994b | 291 | 3,030 | 14 | 7 | 3 | 4 |
| 1995b | 382 | 3,601 | 47 | 7 | 10 | 30 |
| 1996b | 328 | 829 | 35 | 25 | 7 | 3 |
Selection for wild-type poliovirus on BGM cells at 40°C.
Selection for wild-type poliovirus on HEp-2 cells.
Method b gradually replaced method a during the year.
The average number of plaques screened annually by the selective system increased by 1.8-fold, from 1,095 in 1989 and 1990 to 1978 between 1992 and 1996. In contrast, the average number of isolates subjected to neutralization analysis each year was reduced from 222 in 1989 and 1990 to 26 between 1992 and 1996, a ninefold decrease. This dramatic decrease resulted primarily from the elimination of the NPEV by selective propagation on HEp-2 cells. The average annual number of vaccine-derived poliovirus isolates was small before and after 1991. (During 1991 we deliberately isolated vaccine-derived strains at 37°C as part of the assessment of the new protocol.) We did not expect to find changes in this parameter because vaccine-derived polioviruses grow equally well on BGM and HEp-2 cells (data not shown) and are selected against by growth at 40°C, a step which was included in both the old and the new protocols. Between 1989 and 1996 we isolated 41 wild-type poliovirus plaques from 17 sewage samples.
The goal of developing a fast and cost-efficient method for a continuous, country-wide and years-long environmental surveillance for wild-type poliovirus has been achieved. The use of 250 ml from the bottom phase after settling, which is enriched in organic material and contains 40% of the viral particles, rather than the entire 1- to 2-liter sample allowed fast processing of several samples in parallel without the need for special equipment. Addition of concentration steps by various methods, such as flocculation, adsorption on aluminum hydroxide, or polyethylene glycol (PEG) precipitation (10, 17, 23, 26), would have complicated the protocol, which could become more labor-intensive. Recently, we have tested a protocol that included concentration of virus from the top phase by PEG precipitation, which required centrifugation of large volumes and several extraction steps. This protocol aims at obtaining all of the virus particles found in a sewage sample. However, in our hands only 18% of the enterovirus PFU were recovered (data not shown).
We continue to examine various ways to further concentrate our samples in order to increase the recovery rate. We prefer to avoid concentration of large volumes and too many extraction steps to keep our protocol as simple and handy as possible.
For virus isolation, the use of the RCT marker (18), combined with the selective power of the HEp-2 cell line (13), yielded a double-selective system, which substantially reduced the number of plaques analyzed by neutralization assays and allowed us to screen practically every enterovirus isolate. There is still a nonnegligible chance that some wild-type poliovirus strains with an RCT− phenotype will be lost during this selection process. However, the proportion (30 to 35%) is far less than the proportion of isolates that would have been neglected (90%) without the 40°C selection, because it would have taken too much time and effort to analyze all of them.
Since 1988 no clinical cases of poliomyelitis have occurred in Israel or the Palestinian territories in spite of the clear evidence of wild-type poliovirus circulation obtained through the environmental surveillance. All but one of the wild-type isolates were poliovirus type 1, and they were detected in four episodes, which were termed silent outbreaks: one in October 1990 (type 3), the second between May and October 1991, the third between October 1994 and June 1995, and the fourth in December 1996. This suggests that our technique is sensitive enough to detect poliovirus which circulates in the population at a relatively low intensity that is not sufficient to cause morbidity in a well-vaccinated population. A rough calculation (11a) suggests that in industrialized countries examination of about 1 ml of a sewage sample even without concentration theoretically allows detection of poliovirus circulation in a population of 10,000 people if about 100 individuals are excreting the virus. Addition of a concentration step is much needed to detect circulation of viruses in larger communities without polio.
Our protocol is relatively simple and incorporates techniques recommended by the World Health Organization (WHO) for poliovirus isolation and identification. These techniques are available in WHO National Centers all over the world and thus are highly suitable for immediate application anywhere, including developing countries which are on the verge of eradicating poliomyelitis. In such places as the Gaza Strip the current method is sensitive enough, and it could be implemented in addition to the acute flaccid paralysis surveillance required by the WHO (28).
Today new techniques have become available, such as the initial isolation of polioviruses in recombinant mouse L-cells expressing the cloned poliovirus receptor gene (12, 15, 20). These cell lines allow isolation of polioviruses exclusively, rather than other human enteroviruses (12, 20). Other suggested innovations include the use of enzyme-linked immunosorbent assays and molecular methods instead of neutralization assays for virus identification (4, 7, 16, 23, 27). We are exploring these options as alternatives to our current methods for future application. However, only a true field trial will allow a real evaluation of their applicability in the context of continuous environmental surveillance.
Acknowledgments
We thank Robert Armon, Abed Nassar, and the late Eli Katzenelson for their help in the evaluation of the extraction and selection protocols, Zehava Grossman for critically reading the manuscript, and Etti Tilles for typing it.
REFERENCES
- 1.Berg G, Dahling D R. Methods for recovering viruses from river water solids. Appl Environ Microbiol. 1980;39:850. doi: 10.1128/aem.39.4.850-853.1980. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Berg G, Safferman R S, Dahling D R, Berman D, Hurst C J. USEPA manual of methods for virology. EPA-600/4-84-013. U.S. Washington, D.C: Environmental Protection Agency; 1984. Methods for recovering viruses from toxic sludges and solids; pp. 8.1–8.14. [Google Scholar]
- 3.Bottinger M, Herrstrom E. Isolation of polioviruses from sewage and their characteristics. Experience over two decades in Sweden. Scand J Infect Dis. 1992;24:151–155. doi: 10.3109/00365549209052605. [DOI] [PubMed] [Google Scholar]
- 4.Chezzi C, Schoub B D. Differentiation between vaccine related and wild-type polioviruses using a heteroduplex mobility assay. J Virol Methods. 1996;62:93–102. doi: 10.1016/s0166-0934(96)00552-6. [DOI] [PubMed] [Google Scholar]
- 5.Crainic R, Couillin P, Blondel B, Cabau N, Boué A, Horodniceanu F. Natural variation of poliovirus neutralization epitopes. Infect Immun. 1983;41:1217–1225. doi: 10.1128/iai.41.3.1217-1225.1983. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Dahling D R, Berg G, Berman D. BGM, a continuous cell line more sensitive than primary Rhesus and African Green for recovery of viruses from water. Health Lab Sci. 1974;11(4):275–282. [PubMed] [Google Scholar]
- 7.De L, Nottay B, Yang C F, Holloway B P, Pallansch M, Kew O. Identification of vaccine-related polioviruses by hybridization with specific RNA probe. J Clin Microbiol. 1995;33:562–571. doi: 10.1128/jcm.33.3.562-571.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Grabow W, De Villiers J C, Erasmus B, Erasmus D, Engelbrecht L. Viruses in waste water from an informal settlement. Proceedings of the Biennial Conference of the Water Institute of Southern Africa, Port Elizabeth, South Africa, 20 to 23 May, 1996. Johannesburg, South Africa: Water Institute of Southern Africa; 1996. [Google Scholar]
- 9.Grandien M, Forsgren M, Ehrnst A. Enteroviruses and reoviruses. In: Schmidt N J, Emmons R W, editors. Diagnostic procedures for viral, rickettsial, and chlamidial infections. 6th ed. Washington, D.C: American Public Health Association; 1988. pp. 513–579. [Google Scholar]
- 10.Green M S, Handsher R, Cohen D, Melnick J, Slepon R, Mendelson E, Danon Y. Age differences in immunity against wild and vaccine strains of poliovirus prior to the 1988 outbreak in Israel and response to booster I immunization. Vaccine. 1993;11:75–81. doi: 10.1016/0264-410x(93)90342-u. [DOI] [PubMed] [Google Scholar]
- 11.Horstmann D M, Emmons J, Gimpel L, Subrahmanyan T, Riordan J T. Enterovirus surveillance following community-wide oral poliovirus vaccination program: a seven year study. Am J Epidemiol. 1973;97:173–186. doi: 10.1093/oxfordjournals.aje.a121498. [DOI] [PubMed] [Google Scholar]
- 11a.Hovi, T. Personal communication.
- 12.Hovi T, Stenvik M. Selective isolation of poliovirus in recombinant murine cell line expressing the human poliovirus receptor gene. J Clin Microbiol. 1994;32:1366–1368. doi: 10.1128/jcm.32.5.1366-1368.1994. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Johnston S L G, Siegel C S. Presumptive identification of enteroviruses with RD, HEp-2, and RMK cell lines. J Clin Microbiol. 1990;28:1049–1050. doi: 10.1128/jcm.28.5.1049-1050.1990. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Kew O, De L, Yang C F, Nottay B, Pallansch M. The role of virologic surveillance in the global initiative to eradicate poliomyelitis. In: Kustak E, editor. Control of virus diseases. New York, N.Y: Marcel Dekker; 1993. pp. 215–246. [Google Scholar]
- 15.Koike S, Itoshi H, Ise I, Okitsu A, Yoshida M, Iizuka N, Takeuzi K, Takegami T, Nomoto A. The poliovirus receptor protein is produced both as membrane-bound and secreted forms. EMBO J. 1990;9:3217–3224. doi: 10.1002/j.1460-2075.1990.tb07520.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Marques E, DaSilva E E, Dos Santos V M, Kew O, Martins M T. Application of the polymerase chain reaction (PCR) to poliomyelitis surveillance through the analyses of sewage samples. World J Microbiol Biochem. 1993;9:566–569. doi: 10.1007/BF00386295. [DOI] [PubMed] [Google Scholar]
- 17.Martins M T, Marques E, Soares L A. A comparative study of methods for concentration of human enteric viruses from sewage. Water Sci Technol. 1982;14:273–279. [Google Scholar]
- 18.Nakano J H, Milford M H, Thieme M L, Nottay B. Parameters for differentiating vaccine derived and wild poliovirus strains. Prog Med Virol. 1978;24:178–206. [PubMed] [Google Scholar]
- 19.Nelson D B, Circo R, Evans A S. Strategic viral surveillance of sewage during and following an oral poliovirus vaccine campaign. Am J Epidemiol. 1967;86:641–652. doi: 10.1093/oxfordjournals.aje.a120773. [DOI] [PubMed] [Google Scholar]
- 20.Pipkins P A, Wood D J, Racaniello V R, Minor P D. Characterization of L cells expressing the human poliovirus receptor for specific detection of poliovirus in vitro. J Virol Methods. 1993;41:333–340. doi: 10.1016/0166-0934(93)90022-j. [DOI] [PubMed] [Google Scholar]
- 21.Poyry T, Stenvik M, Hovi T. Viruses in sewage waters during and after a poliomyelitis outbreak and subsequent nationwide oral poliovirus vaccination campaign in Finland. Appl Environ Microbiol. 1988;54:371–374. doi: 10.1128/aem.54.2.371-374.1988. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schaub S A, Sagik B P. Association of enteroviruses with natural and artificially introduced colloidal solids in water and infectivity of solids-associated virions. Appl Microbiol. 1975;30:212–222. doi: 10.1128/am.30.2.212-222.1975. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Shieh Y S C, Wait D, Tai L, Sobsey M D. Methods to remove inhibitors in sewage and other fecal wastes for enterovirus detection by the polymerase chain reaction. J Virol Methods. 1995;54:51–66. doi: 10.1016/0166-0934(95)00025-p. [DOI] [PubMed] [Google Scholar]
- 24.Slater P E, Orenstein W A, Morag A, et al. Poliomyelitis outbreak in Israel in 1988: a report with two commentaries. Lancet. 1990;335:1192–1198. doi: 10.1016/0140-6736(90)92705-m. [DOI] [PubMed] [Google Scholar]
- 25.Swartz T A, Handsher R. Israel in the elimination phase of poliomyelitis. Public Health Rev. 1993;21:99–106. [PubMed] [Google Scholar]
- 26.Tambini G, Andrus J K, Marques E, Boshell J, Pallansch M, de Quadros C A, Kew O. Direct detection of wild poliovirus circulation by stool survey of healthy children and analysis of community wastewater. J Infect Dis. 1993;168:1510–1514. doi: 10.1093/infdis/168.6.1510. [DOI] [PubMed] [Google Scholar]
- 27.Van der Avoort H G A M, Hull B, Hovi T, Pallansch M, Kew O, Crainic R, Wood D, Mulders M, Van Loon A. Comparative study of five methods for intratypic differentiation of polioviruses. J Clin Microbiol. 1995;33:2562–2566. doi: 10.1128/jcm.33.10.2562-2566.1995. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.World Health Organization. Manual for the virological investigation of poliomyelitis. Geneva, Switzerland: World Health Organization; 1997. [Google Scholar]