Abstract
Early recognition of Lyme carditis is critical to preventing unnecessary pacemaker implantation for conduction abnormalities associated with this tick-born infection. Patients who do receive a pacemaker should be considered for device extraction after the completion of their antibiotic therapy if they recover normal atrioventricular node conduction. (Level of Difficulty: Intermediate.)
Key Words: AV block, Lyme carditis, Lyme disease, pacemaker
Abbreviations and Acronyms: AV, atrioventricular; IDSA, International Diseases Society of America; IV, intravenous; LC, Lyme carditis; PPM, permanent pacemaker; SILC, Suspicious Index in Lyme Carditis
Central Illustration
Lyme disease is a vector-borne illness resulting from the transmission of the bacterium Borrelia burgorgeri by an Ixodes tick bite.1 Lyme carditis (LC) is a manifestation of disseminated Borrelia, seen in as many as 3% to 10% of cases of LD.2 Significant immunologic and autoimmunologic reactions occur within the myocardium as a result of direct invasion by the spirochete, leading to a disruption in normal electrical conduction.3 This manifests in a wide range of cardiac arrhythmias and conduction disorders, most commonly atrioventricular (AV) blocks.4
Learning Objectives
-
•
To highlight the importance of considering Lyme carditis in the differential diagnosis for high-degree AV block.
-
•
To discuss the benefits of early device interrogation in patients who have been treated for Lyme carditis and received a pacemaker during their treatment.
-
•
To outline a management algorithm for the safe removal of pacemakers in patients with treated Lyme carditis.
We present 2 patients with LC who underwent successful pacemaker explantation after the treatment of their infection. The aim of this paper is to highlight the importance of early follow-up in patients with treated LC who have undergone permanent pacemaker (PPM) placement and to outline our approach to safe pacemaker extraction.
Case Presentations
The clinical characteristics, course, and follow-up details for our patients can be seen in Table 1.
Table 1.
Summary of Lyme Carditis Cases
| Case 1 | Case 2 | |
|---|---|---|
| Patient demographics | 48-year-old woman | 59-year-old man |
| Presenting symptoms | Dizziness, shortness of breath | Dizziness, 2 episodes of nonprodromal syncope |
| Lyme symptoms (including erythema migrans) | Nonspecific rash on abdomen 3 months prior, myalgia | Headache, myalgia |
| Initial ECG/telemetry | Complete heart block | Atrial fibrillation with slow ventricular response and pauses |
| SILC score | 8 | 4 |
| Lyme serology | Positive | Positive |
| Echocardiogram | Normal LV function, moderate MR, mild TR, left atrial enlargement | Normal LV function, aortic sclerosis, mild AR, mild biatrial enlargement |
| Pacemaker device | Medtronic W3DR01 Azure S DR MRI | St. Jude Medical 2272 Assurity MRI |
| Antibiotic treatment | Ceftriaxone 2 grams, IV once daily for 4 weeks | Doxycycline 100 mg orally, twice daily for 3 weeks |
| Follow-up ECG | NSR with HR 65, PR 166 ms, QRS 84 ms | NSR with HR 79, PR 178 ms, QRS 90 ms |
| Device interrogation | 14 weeks after pacemaker insertion: ventricular pacing <1% | 38 weeks after pacemaker insertion: ventricular pacing <1% |
| Time to total conduction recovery (based on pacemaker HR histograms) | 4 weeks | 7 weeks |
| Stress test results | HR response 165 beats/min with 1:1 conduction (BRUCE 10:50 min, achieving maximum work level) | HR response 150 beats/min with 1:1 conduction (BRUCE 10:02 min, achieving maximum work level) |
| Successful device explantation (number of weeks after insertion) | 19 weeks | 42 weeks |
| Lead Borrelia tissue sampling results | Negative | Negative |
AR = aortic regurgitation; ECG = electrocardiogram; HR = heart rate; IV = intravenous; LV = left ventricle; MR = mitral regurgitation; NSR = normal sinus rhythm; TR = tricuspid regurgitation.
Case 1
A 48-year-old woman presented with shortness of breath and dizziness secondary to complete heart block (Figure 1). Her SILC (Suspicious Index in Lyme Carditis) score was 8 (Table 2).5 Given the presence of symptomatic bradycardia, she was transferred to a tertiary hospital for pacemaker implantation. Several days later, her Lyme serology returned reactive, and she was given a 4-week course of daily ceftriaxone 2 grams IV.
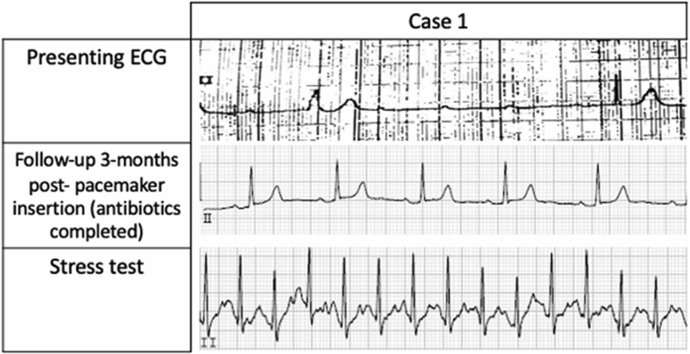
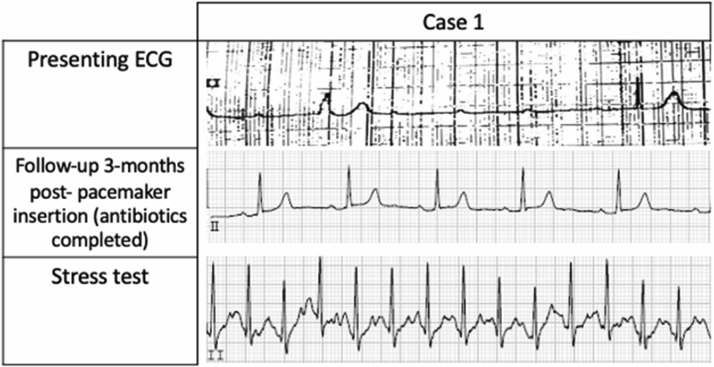
Figure 1.
Lead II Strips From the ECGs in Case 1
Electrocardiograms (ECGs) collected on presentation, after pacemaker insertion, and on stress testing.
Table 2.
Suspicious Index in Lyme Carditis Score11
| Constitutional symptomsa | 2 |
| Outdoor activity/endemic area | 1 |
| Sex male | 1 |
| Tick bite | 3 |
| Age <50 years | 1 |
| Rash: erythema migrans | 4 |
Used to evaluate the likelihood that a patient’s high-degree atrioventricular block is caused by Lyme carditis. The total summed score indicates low (0 to 2), intermediate (3 to 6), or high (7 to 12) suspicion of Lyme carditis.
Fever, malaise, arthralgia, dyspnea.
Case 2
A 58-year-old man presented with dizziness and syncope (SILC score of 4). His initial electrocardiogram showed atrial fibrillation with slow ventricular response. During his admission he experienced symptomatic pauses lasting 4 to 10 seconds. He was transferred for pacemaker implantation. His Lyme serology subsequently returned reactive, and he was given a 3-week course of oral doxycycline 100 mg twice daily.
Follow-up for both patients
The patients were referred to the device clinic at our institution. Upon interrogation, both devices showed normal AV conduction with <1% ventricular pacing (postinsertion week 14 for case 1 and week 38 for case 2). Using the previously published LC protocol, both patients underwent exercise stress testing and were able to maintain 1:1 conduction at a heart rate >120 beats/min.6 They both underwent clinically indicated pacemaker explantation and lead extraction. The lead tips were stored in a dried tube in a −20 °C freezer. The pacemaker lead specimens were then tested for Borrelia DNA by quantitative polymerase chain reaction amplification (Supplemental Appendix).
Discussion
Patients with LC rarely require PPM implantation for the treatment of high-degree AV block, inasmuch as most patients recover normal conduction after the administration of appropriate antibiotics.7 As such, it is important to rule out reversible causes of high-degree AV block before device implantation in patients without risk factors for conduction abnormalities. The International Diseases Society of America (IDSA) recommends 14 to 21 days of antibiotics for LC, with intravenous (IV) ceftriaxone for hospitalized patients and oral amoxicillin or doxycycline in the outpatient setting.8 Early treatment of LC with antibiotics is associated with a good prognosis.9 Most cases of high-degree AV block resolve within the first 10 days of antibiotic treatment (range, 3-42 days).9 Should a patient with LC experience symptomatic bradycardia, a temporary-permanent transvenous pacemaker should be placed to allow for mobilization.9 Our practice is to admit patients on IV antibiotics until 1:1 AV nodal conduction has recovered. Once there is AV nodal recovery, predischarge stress testing is recommended to assess stability, as outlined by Yeung, et al.9 Patients are typically discharged to take oral antibiotics to complete their 21-day course. In the cases outlined above, the antibiotic regimens (chosen by peripheral hospitals) were not in keeping with the IDSA guidelines. Fortunately, the patients still had complete resolution of their conduction abnormalities. Additionally, although Lyme serology samples were submitted for analysis before the placement of their PPMs, the results had not returned before implantation. Both patients should have had their conditions stabilized with a temporary pacing device until the results of Lyme testing were available.
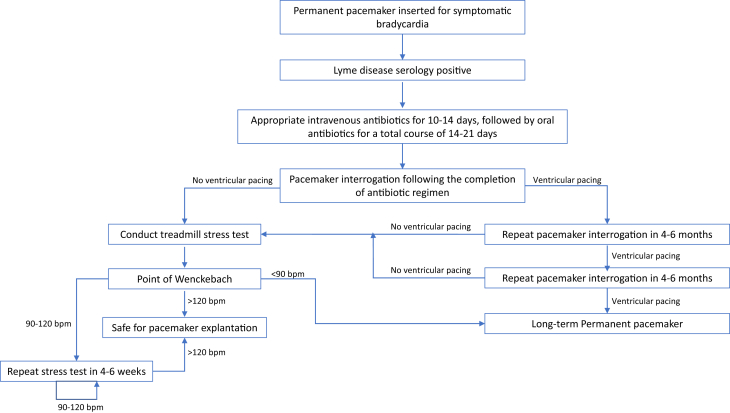
If a PPM is inserted before the confirmation of LC, pacemaker explantation is possible. A systematic approach to pacemaker explantation is necessary to ensure adequate patient safety. A flowchart summarizing our algorithm is presented in Figure 2. Pacemaker interrogation should occur after antibiotic completion. If there is no ventricular pacing, the patient should undergo an exercise stress test to assess their AV node function. If the patient can maintain 1:1 AV conduction at a heart rate >120 beats/min, device explantation should be arranged. If they are unable to maintain 1:1 conduction at >120 beats/min, stress testing should be repeated. For patients with ongoing ventricular pacing, reinterrogation should occur in 4 to 6 months. The PPM should remain in situ for patients with ongoing ventricular pacing after repeated interrogations.
Figure 2.
Algorithm for Permanent Pacemaker Extraction in Lyme Carditis
Clinical algorithm for safe pacemaker extraction in those who have had a permanent pacemaker placed during their treatment course for Lyme carditis.
Within the first year of insertion, transvenous lead extraction has a high success rate and a low complication rate. The removal of recently placed leads can usually be achieved by direct traction. In devices implanted over a long term, fibrotic lead attachments often develop at the tip and throughout the length, including in the veins and endocardial structures, which increases the risk of complications associated with lead removal.10 This highlights the importance of close follow-up so that early pacemaker explantation can be arranged if clinically indicated.
Myocardial biopsy specimens in patients with LC have demonstrated transmural inflammatory infiltrates with characteristic band-like endocardial lymphocyte infiltration and occasionally visualized spirochetes.11 In our study, the negative quantitative polymerase chain reaction amplification for Borrelia on the extracted pacemaker leads may suggest complete resolution of the infection and a greater likelihood of successful pacemaker explantation in the long term. Immunofluorescence studies in mouse models inoculated with Lyme showed Borrelia in the AV junction, epicardium, and less commonly the myocardium.2 It is therefore possible that Borrelia infiltration in our patients was concentrated in the conduction system rather than the myocardium where the lead tips were secured.
A breadth of literature has been published on the diagnosis and management of early disseminated LC; however, few studies have looked at long-term outcomes in patients with treated LC.5, 6, 7,9 To our knowledge, there have been no documented studies of pacemaker explantation after the resolution of LC. Early follow-up is important to assess for normal conduction patterns in patients who have had pacemakers inserted as part of the management of early disseminated LC. The utility of Borrelia testing on myocardial tissue from extracted leads remains unknown.
Take-Home Message
Pacemaker explantation is a potential option for patients with treated LC who have undergone proper testing to ensure that normal cardiac conduction has resumed.
Funding Support and Author Disclosures
The authors have reported that they have no relationships relevant to the contents of this paper to disclose.
Footnotes
The authors attest they are in compliance with human studies committees and animal welfare regulations of the authors’ institutions and Food and Drug Administration guidelines, including patient consent where appropriate. For more information, visit the Author Center.
Appendix
For supplemental material, please see the online version of this paper.
Appendix
References
- 1.Semmler D., Blank R., Rupprecht H.J. Complete AV block in Lyme carditis: an important differential diagnosis. Clin Res Cardiol. 2010;99:519–526. doi: 10.1007/s00392-010-0152-8. [DOI] [PubMed] [Google Scholar]
- 2.Robinson M.L., Kobayashi T., Higgins Y., Calkins H., Melia M.T. Lyme carditis. Infect Dis Clin North Am. 2015;29:255–268. doi: 10.1016/j.idc.2015.02.003. [DOI] [PubMed] [Google Scholar]
- 3.Muehlenbachs A., Bollweg B.C., Schulz T.J., et al. Cardiac tropism of Borrelia burgdorferi: an autopsy study of sudden cardiac death associated with Lyme carditis. Am J Pathol. 2016;186:1195–1205. doi: 10.1016/j.ajpath.2015.12.027. [DOI] [PubMed] [Google Scholar]
- 4.Scheffold N., Herkommer B., Kandolf R., May A.E. Lyme carditis: diagnosis, treatment and prognosis. Dtsch Arzteb Int. 2015;112:202–208. doi: 10.3238/arztebl.2015.0202. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Besant G., Wan D., Yeung C., Blakely C., et al. Suspicious index in Lyme carditis: systematic review and proposed new risk score. Clin Cardiol. 2018;4:1611–1616. doi: 10.1002/clc.23102. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Yeung C., Baranchuk A. Systematic approach to the diagnosis and treatment of Lyme carditis and high-degree atrioventricular block. Healthcare. 2018;6:119. doi: 10.3390/healthcare6040119. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Wang C.N., Yeung C., Enriquez A., et al. Long-term outcomes in treated Lyme carditis. Curr Probl Cardiol. 2021:100939. doi: 10.1016/j.cpcardiol.2021.100939. [DOI] [PubMed] [Google Scholar]
- 8.Lantos P.M., Rumbaugh J., Bockenstedt L.K., et al. Clinical practice guidelines by the Infectious Diseases Society of America (IDSA), American Academy of Neurology (AAN), and American College of Rheumatology (ACR): 2020 guidelines for the prevention, diagnosis and treatment of Lyme disease. Clin Infect Dis. 2021;71:e1–e48. doi: 10.1093/cid/ciaa1215. [DOI] [PubMed] [Google Scholar]
- 9.Yeung C., Baranchuk A. Diagnosis and treatment of Lyme carditis: JACC Review Topic of the Week. J Am Coll Cardiol. 2019;73:717–726. doi: 10.1016/j.jacc.2018.11.035. [DOI] [PubMed] [Google Scholar]
- 10.Farooqi F.M., Talsania S., Hamid S., Rinaldi C.A. Extraction of cardiac rhythm devices: indications, techniques and outcomes for the removal of pacemaker and defibrillator leads. Int J Clin Pract. 2010;64:1140–1147. doi: 10.1111/j.1742-1241.2010.02338.x. [DOI] [PubMed] [Google Scholar]
- 11.Duray P.H. Histopathology of clinical phases of human Lyme disease. Rheum Dis Clin North Am. 1989;15:691–710. [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.