Abstract
Background
Bangladesh is a lower-middle-income country affected by a severe lack of mental health service availability due to a scarcity of mental health experts, limited mental health literacy, and community stigma. In other low and middle-income countries, the online provision of mental health care services has addressed issues affecting service availability, accessibility, mass awareness of services, and stigma.
Objective
The current study sought to understand stakeholders' perceptions of the potential of digital media-based mental health care delivery in strengthening Bangladesh's mental health system.
Method
Online in-depth interviews were conducted with seven psychiatrists and eleven people with lived experiences of mental health issues. In addition, two online focus groups were conducted with ten psychologists and nine mental health entrepreneurs. A thematic analysis of the audio transcriptions was used to identify themes.
Result
Stakeholders perceived that the benefits of digital media-based mental health services included the potential of increasing the awareness, availability, and accessibility of mental health services. Participants recommended: the rehabilitation of existing pathways; the use of social media to raise awareness; and the implementation of strategies that integrate different digital-based services to strengthen the mental health system and foster positive mental health-seeking behaviors.
Conclusion
Growing mental health awareness, combined with the appropriate use of digital media as a platform for distributing information and offering mental services, can help to promote mental health care. To strengthen mental health services in Bangladesh, tailored services, increased network coverage, and training are required on digital mental health.
Abbreviations: MH, Mental Health; PWLE, People with Lived Experiences of Mental Health Issues; DALYs, Disability-Adjusted Life-Years; CMD, Common Mental Health Disorders; LMIC, Low and Middle-Income Country; HIC, High Income Country; COVID-19, Coronavirus Disease 2019; KII, Key Informant Interviews; FGD, Focus Group Discussions; IDI, In-Depth Interviews; UHC, Universal Health Coverage; WHO, World Health Organization; IRB, Institutional Review Board; COREQ, Consolidated Reporting Criteria for Qualitative Studies
Keywords: Mental health, Digital technology, Health system, E-mental health, Internet, Bangladesh
Highlights
-
•
Digital technology has the scope to improve mental health care pathway by increasing MH literacy, health-seeking behavior, and service availability
-
•
To integrate digital technology to strengthen mental health services, tailored services, increased network coverage are required
-
•
Structured usage of social media and capacity building of the non-health professionals are recommended to strengthen the mental health system
1. Introduction
The global burden of mental health (MH) conditions is a major public health concern accounting for 32.4% of years lived with disability (YLDs) and 13% of disability-adjusted life-years (DALYs) (Hossain et al., 2014; Mathers, 2008; Vigo et al., 2016). A recent systematic review showed a higher prevalence (14.2%) of common mental health disorders (CMD) in South Asian countries compared to worldwide prevalence, whereas depressive disorders accounted for 9.8 million DALYs (Ogbo et al., 2018; Naveed et al., 2020; Polanczyk et al., 2015).
Mental health care systems of low- and middle-income (LMIC) countries are closely linked to and enmeshed in the larger social and economic settings, resulting in significant inequities in access for community members (Ngui et al., 2010). Factors such as lack of awareness, stigma, government apathy, inadequacy in health systems infrastructure, limited policy considerations, and shortages of MH professionals contribute to these gaps in the MH care system (Siriwardhana et al., 2013; Hanisch et al., 2016; Trivedi et al., 2007). This is also the case in Bangladesh, where the MH care system faces complex challenges due to low financial resourcing: 0.5% of the total health budget is allocated to ensuring MH services (Sakib, 2021; Alam et al., 2020; Islam and Biswas, 2015). MH service availability is inadequate, with low numbers of MH professionals and few service facilities and hospitals (Hasan et al., 2021). Rural primary and secondary healthcare facilities lack MH care services, with most MH services centralized in urban areas (Hasan et al., 2021). In primary care settings, a lack of training on MH for nurses and community health workers leads to missed or sub-optimally managed cases of mental disorders (WHO, 2007).
Furthermore, a lack of MH literacy has led to individual and community stigma, impacting MH help-seeking behavior at the community level (Arafat et al., 2021). These issues create significant barriers to MH service provision in Bangladesh, as in other LMICs (Collins et al., 2011; Semrau et al., 2015; Thara, 2012; Acharibasam and Wynn, 2018). Insights from other LMICs support the potential for online availability of MH information and services to address the scarcity of MH human resources and lack of MH services in Bangladesh (Hasan et al., 2021; Arafat et al., 2021).
Widespread use of digital media has offered innovations for increasing mental health awareness and service provision in many countries (Arafat et al., 2021; Bucci et al., 2019; Zhou et al., 2020; Hungerbuehler et al., 2016; Maulik et al., 2017). For instance, blogs on various websites, social media platforms, and smartphone apps have been used to share information about self-help and increase mental health literacy (Parikh and Huniewicz, 2015; Barnett et al., 2021). The effectiveness of digital media-based solutions has been demonstrated in China, India, Singapore, Australia, and many other countries, during crises such as pandemics and natural disasters (Zhou et al., 2020; Kanuri et al., 2020). During the COVID-19 pandemic, China provided telemedicine and psychoeducation through several online platforms like WeChat and Tencent QQ (Zhou et al., 2020). Similarly, the Australian government offered psychosocial support services through text messaging, online chat platforms, telephone, videoconference, online group chat, self-help platforms, e-mail, websites, mobile apps before and after the COVID-19 pandemic for common mental health issues, self-harm, and suicide (Zhou et al., 2020; Wilson et al., 2020). Podcasts have been used in an accessible and educational manner both by mental health specialists and the general public to provide and acquire mental health-related information in the United States (Casares, 2022).The promising contribution of digital technology in LMICs has also been reported in a systematic review (Naslund et al., 2017). The review mentioned about successful utilization of teleconferencing, mobile app, web-based screening tools, online platforms in many developing countries including Somaliland, South Africa, India, Brazil, Chile, Sri Lanka to support mental healthcare delivery in clinical and community settings (Naslund et al., 2017).
Evidence demonstrates that some LMICs have successfully adopted digital technology to raise awareness, screen, diagnose and manage common mental health disorders for a wider populations (Maulik et al., 2017; Amos et al., 2020). Bangladesh has adopted various digital health services to promote and protect public health, including mental health, which has gained greater uptake since the COVID-19 pandemic (Islam et al., 2021a). The introduction of digital health services, including telemedicine, remote data collection, surveillance, follow-up, and human resource development, shows the potential for a wider-scale roll-out of services. Artificial intelligence-based mobile applications and tele-psychotherapy services through e-mail, text messaging, and audio or video conferencing have been widely used in Bangladesh since 2020 (Arafat et al., 2021; Islam et al., 2021a; Soron and Chowdhury, 2021).
Thus, digital technology has the potential to address mental health conditions in Bangladesh by increasing awareness of mental health, enhancing access to mental health professionals, reducing costs and improving time efficiency of care, and facilitating remote service delivery (Acharibasam and Wynn, 2018). Although digital MH initiatives have been implemented, there remains a need to generate evidence about the advantages, possible barriers, and areas for improvement to implement better digital mental health services (Hasan et al., 2021; Arafat et al., 2021; Berry et al., 2019). Despite the successes of digital technology, there are considerable barriers to and inequities in digital MH care. Regarding rural and underprivileged populations in Bangladesh, digital MH service delivery inequities exacerbate due to low access to digital technology, a lack of therapeutic alliance among service users and health service providers, data privacy issues, and other organizational challenges. If these barriers are not addressed, MH care inequity will worsen, and treatment gap will increase. Hence, identifying these barriers is critical when trying to increase the availability, accessibility, and affordability of MH care through digital technology (Arafat et al., 2021). The experiences and recommendations from the relevant MH stakeholders, including service providers and service users, can contribute to designing evidence and need-based digital MH care services. Hence, this qualitative study aimed to explore the perceived benefits and challenges associated with the digital delivery of MH care services in Bangladesh and develop recommendations to design more accessible and available technology-based MH support programs and services in Bangladesh.
2. Methods
2.1. Design
This qualitative study attempted to explore the role of MH care services delivered through digital media in Bangladesh by analyzing the perceptions and insights from MH professionals, entrepreneurs, and service users. Various qualitative interview techniques were employed, including key informant interviews (KII), focus group discussions (FGD), and in-depth interviews (IDI) among three MH stakeholders and service users.
2.2. Study population
The study involved MH service providers [Psychiatrists (n = 7) and Psychologists (n = 10)], eminent MH advocates from civil society organizations [Entrepreneurs (n = 9)], and people with lived experiences of various MH issues who had received MH care services [PWLE (n = 11)]. Data collection was conducted online via the Zoom platform. The study design adhered to the consolidated reporting criteria for qualitative studies (COREQ) (Tong et al., 2007) (Appendix A).
Different recruitment strategies were employed for the different participant groups. MH service providers and entrepreneurs were purposively recruited based on their professional experiences, academic background and clinical exposure. Given the stigma associated with mental illness or seeking mental health services in Bangladesh, PWLE who had received digital MH care services were purposively recruited from the existing network of the lead author with the service providers and entrepreneurs in Bangladesh. Detailed information about the study was sent to MH service providers (psychiatrists and psychologists) and entrepreneurs via e-mails. We contacted the PWLE by telephone and were then followed up with an e-mail sharing the details of the study. The online sessions began with an explanation of the research objectives and the process of asking for informed consent. All participants provided consent to record and transcribe the interviews and focus group discussions before data collection commenced. Table 1 illustrates the qualitative methods utilized and the sample sizes associated with each kind of stakeholder.
Table 1.
Qualitative method and sample size.
| Methods | Stakeholders | Types of organization |
Total number (n = 37) | |
|---|---|---|---|---|
| Public institutions | Private institutions | |||
| KII (key informant interview) | Psychiatrists | 5 | 2 | 7 |
| FGD (focus group discussion) | Psychologists | 4 | 6 | 10 |
| Entrepreneurs | 0 | 9 | 9 | |
| IDI (in-depth interview) | People with lived experiences (PWLE) | – | – | 11 |
2.3. Ethical considerations
The study was approved by the Institutional Review Board (IRB) of the icddr,b which included a Research Review Committee and an Ethics Review Committee (PR 20094). Study participants provided their informed consent to record and note the discussions before starting the interviews. No sensitive or private questions were asked to any stakeholder groups.
2.4. Data collection method
The research team developed semi-structured interview guidelines for the study participants (Appendix B). The questions aimed to understand participants' perspectives about the role of digital technology in MH care services in Bangladesh. Any communication medium that uses one of several encoded machine-readable data formats was referred to as ‘digital media’ for the purposes of this study and included software, digital photos, digital video, web pages, websites, and social media. All the interviews and discussions were conducted by the lead author, supported by other authors who took notes. Each interview lasted 40–50 min, and FGDs lasted for 120 min on average. Key informant interviews (KII) sought to acquire in-depth information from individuals who had first-hand knowledge and experience of MH and its service provision in Bangladesh. They were conducted with psychiatrists working in private and public MH sectors.
In-depth interviews (IDI) were employed to understand participants' experiences who had received online and offline MH care services for MH conditions like anxiety, panic attack, suicidal thoughts, depression, and substance abuse disorders, among others. Pseudonyms are used in reporting to maintain the confidentiality of the participants. Focus group discussions (FGDs) were conducted with psychologists and MH entrepreneurs to gather people from similar backgrounds and generate collective information about the research topic. The psychologists included clinical, educational, or counseling professionals and had between 7 and 23 years of experience. MH entrepreneurs were selected from leading non-government MH organizations. They were recruited based on their years of providing services, MH-related social media activities, advocacy, and community services. Data saturation was reached when no new data emerged from the interviews.
2.5. Data management
Recorded interviews and FGDs were transcribed and translated into English by two of the authors. The lead author thoroughly reviewed all the documents to ensure the research data's quality and consistency.
2.6. Data analysis
An inductive thematic analysis approach was used to analyze the data (Clarke et al., 2015). The authors first acquainted themselves with the interview data by reading the transcripts. Next, they manually coded the transcripts. The initial thematic codes emerged through an iterative procedure via several meeting sessions among the authors. The coded data were separated into a data matrix built into Microsoft Excel to create coding frameworks. Coded data was transferred into a datasheet and organized under themes and sub-themes informed by the research objectives. Every level of data analysis was discussed with the research team and all co-authors.
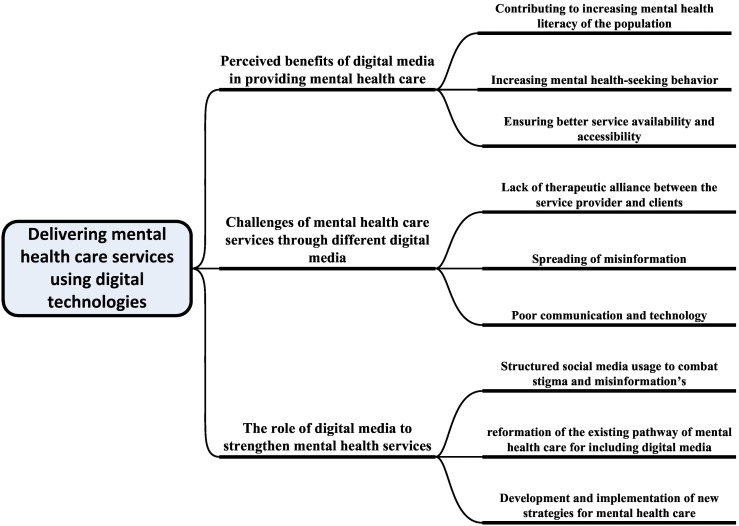
3. Results
The majority of the participants from all stakeholder groups were female. Most stakeholders had 10–15 years of experience providing MH and related services. The psychiatrist key informants were mostly male (Table 2). Three significant themes emerged: (i) perceived benefits of digital media in providing MH care, (ii) challenges of MH care services through digital media, and (iii) the role of digital media in strengthening MH services. These were supported by nine subthemes, summarized in Fig. 1. The quotes from the other stakeholders are referred to in the text and given in full in the supplementary section (Appendix C).
Table 2.
Profile of the stakeholders.
| Characteristics | Focus group discussion (n = 19) | Key informant interviews (n = 7) | In-depth interviews (n = 11) |
|---|---|---|---|
| Gender | |||
| Male | 2 | 6 | 2 |
| Female | 17 | 1 | 9 |
| Years of experiences | |||
| 10–15 | 11 | 3 | – |
| 15+ | 8 | 4 | – |
| Profession | |||
| Mental health service providers (Psychiatrist and Psychologist) |
10 | 7 | – |
| Mental health entrepreneurs | 9 | – | – |
| Health service users (Clients) | – | – | 11 |
Fig. 1.
Thematic distribution of the findings.
3.1. Perceived benefits of digital media in providing MH care
Both MH service providers (n = 26) and service users (n = 11) spoke about the perceived benefits of digital media in providing MH care, across various domains. These are discussed below.
3.1.1. Contributing to increasing the mental health literacy of the population
The majority of the service providers (n = 10/17) and users (n = 7/11) stated that digital MH services share different MH-related information and content in the websites, web pages and social media, thereby facilitating mass dissemination and awareness. In this regard, one participant said,
“You [community members] can quickly acquire the MH information from online platforms, and you can easily become conscious of your MH status.”
Psychiatrist 4
One PWLE added that the information available on online social media platforms helps people know about the basic symptoms of different MH problems. They stated:
“Social media platforms, like [the] Women Support Initiative Forum, Moner Bondhu, Identity inclusion, play an important role as they publish educational contents on MH which help people to know about their MH conditions.”
- PWLE 1
Some entrepreneurs (n = 3) expressly indicated social media as the easiest method to disseminate information about MH intervention in interesting ways, such as videos and animations, which effectively increases mass awareness. One said:
“Normally, our organization and UNDP (donor) collaborate to raise awareness among a large group of people through our Facebook page and YouTube channel. We are trying to raise awareness by making animation films, cartoons andmeditation platforms”
- Entrepreneur 6
3.1.2. Increasing mental health seeking behavior
Some stakeholders (n = 9) highlighted that digital media plays a crucial role in positively influencing MH care-seeking behaviors by self-referral when needed. One PLWE specifically mentioned that:
“In previous days, our parents did not know about MH conditions. But nowadays due to continuous exposure to MH-related information, even with the mobile text-based services, they are aware and take their child to the MH experts.”
- PWLE 8
Some psychiatrists (n = 6), psychologists (n = 2) and entrepreneurs (n = 4) stated that online content and advertisements educated the community about the necessity of timely care-seeking. One psychiatrist shared that:
“The advertisements about numerous MH experts in social media inspires the community to seek necessary supports when needed”
- Psychiatrist 6.
One psychologist also stated that this helped address questions of inequity so that individuals from different parts of the country could become aware of the MH management options:
“People from outside Dhaka can take and continue their counseling as it happens online. This proves that community level's MH-seeking behaviors increased due to the digital media.”
- Psychologist 7
Online platforms could help address some of the stigma-related concerns that people have. One entrepreneur also highlighted that online platforms could assure privacy and contribute to the community's increased MH-seeking behavior:
“Sometimes we get many questions anonymously about sex and reproductive health affecting their MH, and we also provide the services with the privilege of anonymity.”
- Entrepreneur 6
Stakeholders, especially service providers (n = 8), underlined digital media platforms' role in providing uninterrupted MH services during the COVID-19 pandemic because they didn't require an in-person presence for service delivery. In this regard, one psychologist noted:
“Now tele-counseling services have been increased even more in the pandemic which is beneficial for delivering services throughout the country. We have been providing uninterrupted MH services through the digital media platforms”
- Psychologist 1
However, one psychiatrist shared concern about the lack of MH experts available to deal with the increased need for MH care services during the COVID-19 pandemic:
“We provide telemedicine services from tertiary care centers to primary facilities during this pandemic. Due to the shortage of psychiatrists and the surge of service-seeking needs, we have to struggle to provide sufficient time to all patients. So, it will be easier to deliver quality services if human resources increase.”
- Psychiatrist 6
According to service providers, the availability of online MH services also contributes to increased treatment adherence by service users. In regards to support, two psychiatrists stated that it was easier for service users to attend their advised follow-up visits online as it reduced the distance and schedule-related challenges. One participant explained,
“Another benefit of online MH services is that it enables people from different places to receive the services during the lockdown. So now it is easy to provide better follow-up and treatment adherence and to help to improve their prognosis.”
-Psychiatrist 1
However, one PWLE provided a contrasting perspective, stating that, even if the services are convenient, the quality of online MH services might differ from face-to-face services:
“To me, face-to-face sessions are more connecting than the online sessions as the service providers can follow the facial expressions. The users can comply well with the therapeutic exercises as well.”
- PWLE 10
3.1.3. Ensuring better service availability and accessibility
According to the stakeholders, digital MH care plays a significant role in providing better MH care service availability and accessibility. The PLWE (n = 11/11) mentioned that it was easy to seek care on the digital platforms to ensure instant availability of the service providers. One participant stated,
“Because of these online services, we don't need to worry about time limitations. I can communicate with my psychologist any time and schedule my session according to my convenience with no loss of time.”
- PWLE 4
One of the entrepreneurs said that even if a provider is unavailable when needed, service users can get instant help through their MH apps.
“People may obtain our services immediately by using our mobile application, and we provide them with the answer to their queries.”
- Entrepreneur 5
Most psychologists (n = 6) acknowledged the greater service accessibility and availability of MH services by using online platforms; this was especially beneficial for people in remote locations of Bangladesh. Low-income migrants outside the country could also readily access digital MH care services. On this note, one psychologist stated,
“Anyone outside Dhaka (capital city) can get online MH services anywhere. Even people from abroad can access the online services of Bangladeshi MH experts as they desire someone who can understand them without any linguistic and cultural barriers and also financial concerns.”
– Psychologist 8
Another significant perspective shared by the stakeholders was about the contribution of digital media in simplifying the process of service provision, removing transportation and scheduling barriers for accessing care. One PWLE stated,
“Commuting in Dhaka city is troublesome because of traffic jams. I can receive my service from my psychiatrist from home without wasting time.”
- PWLE 8
Psychologists indicated that digital media made service provision easier too by reducing the costs involved in delivering care, for example, reducing the financial investment involved in securing a physical space. One psychologist noted,
“As professionals, we had to rent physical spaces to ensure therapeutic set-up for face to face counseling sessions. This indirectly increased the treatment cost both for us and our clients. Moreover, we used to set specific schedules for our clients, but we both had to deal with challenges due to traffic and distance, which caused our schedules to be delayed. But now, because we conduct sessions online, clients can join timely.”
– Psychologist 7
3.2. Challenges of providing mental health care services through digital media
The majority of the stakeholders (n = 20/37) shared the perceived challenges of MH care services provided through digital media.
3.2.1. Lack of therapeutic alliance between service providers and users
Both PWLE (n = 3) and service providers (reported in 3 focus groups) had experienced communication gaps during digital services. In this regard, one psychologist shared,
“The negative side of online counseling is that I cannot see my patient, and everyone doesn't feel comfortable sharing their difficulties in a digital session. As I cannot see them in person, I miss out on reading their body language, impacting the overall session. I cannot see their expression during audio sessions and only hear their voices.”
- Psychologist 8
Service providers noted that face-to-face sessions allow them to monitor an individual's emotions by observing their body language. This is challenging to do during an online call given that a virtual session creates added difficulties in determining whether the client is talking positively or being emotional. According to the participants, the presence of both the service providers and clients during a session can better impact in MH interventions. One of the PLWE further supported this insight stating,
“If we can see a person's eye and face, it helps assurance during a session. This is why online sessions are challenging for some of the clients.”
– PWLE 8
One PWLE who was diagnosed with severe MH conditions shared this concern, stating -
“When I took face-to-face services, my therapist tried some stress-relieving exercises and taught me some easily doable strategies. Now, as I am taking online sessions, I don't feel the same.”
- PWLE 3
Some stakeholders (n = 4) raised concerns that severe MH illnesses need intensive advanced management with psychiatric drugs, which is not feasible online. One psychiatrist mentioned,
“Online psychiatric sessions can be challenging for schizophrenia or bipolar patients as there are guidelines and a list of permitted drugs for online sessions from BCPS (Bangladesh College of Physicians and Surgeons). So, we cannot always prescribe the needed drugs through online counseling.”
- Psychiatrist 4
Stakeholders (n = 6) shared their concern about the quality of the care via digital media as the environment might not be suitable. One psychiatrist noted,
“Two or three people who were under my treatment stopped seeking online services saying that technology is never going to interpret their complete feelings. Also, as we provide services from home, this is very common to get distracted by surrounding household activities. This is one of the shortcomings of technology-based MH services.”
-Psychiatrist 4
These comments highlighted that digital MH service provision brought with it other considerations in terms of accommodation; as one PWLE added,
“Some people don't have privacy in their home as they have children and share their room, interrupting their privacy during online sessions.”
- PWLE 9
In some circumstances, the lack of privacy that was necessary for effective MH service delivery often caused clients to discontinue counseling services
“People assume service providers, can not ensure the privacy and decide to discontinue the consultations.”
-Entrepreneur 6
3.2.2. Spreading misinformation
While digital media offered many benefits in terms of addressing the stigma associated with mental illness; it also created opportunities to compound stigma or to exacerbate limited understandings of MH. Seven service providers in this study mentioned that social media might misguide people with misleading information, a trend that was heightened during the pandemic. One psychiatrist emphasized this issue, saying,
“During COVID-19, some platforms created undue tension among the population due to the wrong presentation of the contents, which was rather harmful.”
- Psychiatrist 3
One PWLE mentioned that social media can have significant influences on an individual's MH with negative news and peer support,
“Technology can divert our MH in different directions. Honestly, there are many conflicting opinions and unproductive criticism on the social media, which continuously affect our MH negativelyi”
- PWLE 6
The comments from the stakeholders reflected the need for proper monitoring of the digital platforms to ensure the proper dissemination of MH information.
3.2.3. Poor communication and technology
Effective digital MH service delivery relies on reliable technological infrastructure. Slight interruptions on electricity and network could have significant impacts on service provision and access. Network drop-outs or signal variations could breach the flow of the conversations in a session, negatively affecting the experience of people seeking MH care. This dissatisfaction was shared by some PWLE and psychologists (n = 4), who expressed frustration with the device and connectivity issues during the critical moments of a session. For example, three service providers (n = 3) mentioned that the weak internet connections in remote and rural areas make the online services inaccessible to many people. When they could connect, these issues made the actual session labored, meaning that their usefulness was significantly constrained:
“Internet connectivity issue is a big challenge as we have to reschedule frequently. Because of this, the session gets tedious, and both of us lose interest.”
-Psychologist 7
The digital divide, where people had varying expertise in using devices, platforms, apps and programs according to socio-demographic features, further compounded the connectivity issues noted in rural areas, as one PWLE noted:
“Technology-based services are unfamiliar to rural residents; they are unaware of operating the devices and using the services properly.”
PWLE-1, Female
This means that service users, especially people from rural areas, need to learn how to use the device and its interfaces, in addition to addressing all of the other considerations – finding a private space, allocating time, ensuring a good internet connection – in order to have an effective MH care session.
Questions of education and learning extended to health care workers; because of the different backgrounds of service providers, there was some variation in the nature of services provided which needed to be taken into account. Seven of the stakeholders mentioned that a lack of trained professionals at different levels in providing digital MH services limited the efficacy of these services. This meant that the providers had to make commitments to training and education that extended beyond their service provision role:
“Community health workers and other health care providers need training on providing digital MH care services as it requires professional set-up and certain therapeutic skills.”
- Psychiatrist 1
3.3. Recommendations about the critical role of digital media to strengthen mental health services
The MH service providers (n = 26) and PWLE (n = 11) shared ideas for strengthening MH care services via digital media integration.
3.3.1. Structured social media usage to combat stigma and misinformation
Stakeholders asserted the need for structured social media usage to prevent the spreading of misleading MH-related information and increase MH literacy. One of the common recommendations was to initiate collaborative efforts of the other health and MH service providers to create and share content via their social media platforms. In this way, evidence-based information could reach the community. One psychologist noted that,
“MH experts who provide services and those involved in research can use social media to disseminate their knowledge, findings, and common facts. Apart from combatting the existing stigma, I believe this will boost people's trust and confidence in seeking care.”
-Psychologist 4
By addressing misinformation, the provision of evidence-based information on MH could further reinforce the effectiveness of mental health care by generating and reinforcing trust in the MH care system. This was a high priority for the service provider participants; as one psychologist outlined,
“We can create posts about available trustable MH experts through authentic online platforms so that people can understand their qualifications and experiences and decide from where and whom to seek care”
- Psychologist 7
However, on this note, some service providers (n = 3) mentioned that there was also a need to consider the overflow of information in social media and the need to customize the social media platforms to control misinformation. One psychiatrist noted,
“Everyone nowadays is an MH advocate and sharing information without the appropriate expertise, which is misleading. A certain level of commitment is necessary before establishing an online MH forum.”
- Psychiatrist 3
These comments speak to both a knowledge-based role (in terms of service provision) and the affordances of the social media platforms themselves, to ensure settings prevented misinformation from disseminating. Furthermore, the service providers (n = 15) added that proper validation is necessary to prevent digital media-based malpractice related to MH. One psychiatrist explained this in further detail,
“I believe it is critical to communicate information about our certification and qualifications with clients so that we can enlighten them before they engage with unknown service providers, which can prevent malpractice in social media.”
- Psychiatrist 6
Moreover, given the lack of a therapeutic alliance and the challenges this poses, such as possible malpractice during online sessions, entrepreneurs also added,
“As a monitoring entity is absent, no one can remove misleading information or stop the harmful practice. There should be a licensing body like the Bangladesh dental and medical council for the psychologists.”
- Entrepreneur 5
Such comments speak to an increasing role for government or non-government agencies to better support MH care delivery through policy or accreditation processes.
3.3.2. Reformation of the existing pathway of mental health care for including digital media
Most service providers and users (n = 14) also proposed reforming the existing MH services to include digital media to strengthen overall MH care and reduce the treatment gap, especially in marginal areas.
However, as outlined above, a severe lack of network availability and technology glitches were significant challenges. To mitigate this challenge, stakeholders (n = 10) suggested increasing advocacy at the government level to focus on technological advancements to improve the networking system. One PWLE noted,
“Government has to come forward with a positive attitude to improve the internet and networking system at the village level as online MH services will require a better network and internet so that the services do not get interrupted.”
- PWLE 8
In making such suggestions, these participants are calling for a whole-of-government orientation towards digital service provision – which could extend well beyond MH services. This speaks to broader questions of digital connectivity and the digital divide.
Some service providers developed strategies to overcome connectivity issues and shared that they attend online sessions by using the facilities at primary care facilities from the tertiary centers.
“Suppose we can ensure internet connection at the Upazila/primary care level. In that case, it will be possible to build better communication between peripheral facilities with the central health system and deliver improved tele-MH services.”
- Psychiatrist 5
Digital MH services require particular expertise. Stakeholders mentioned the capacity building of the existing non-health professionals on digital MH services especially, at primary care facilities. Favoring this, one psychologist stated,
“The service providers who are delivering online MH services should be trained in different relevant aspects particularly to build rapport and effective communication through digital media.”
– Psychologist 9
Participants (n = 7).also felt that a great emphasis should be given to training the MH workforce to ensure the quality of digital-based service delivery:
“Digital technology plays a great role, but we need to train service providers to ensure the finest delivery. Experts should facilitate training on how to provide telemedicine and the recommended level of information that a service provider shall share. We need more workforce to accomplish these targets.”
– Psychiatrist 5
However, another service provider stressed the need for educating the rural and elderly population apart from training the workforce for a better outcome. The psychiatrist said:
“Village people cannot easily understand many digitalized things like modern apps, payment methods, connection with the service provider, etc. We can train lay health workers to train elderly and rural people about how they can get MH treatment digitally, or we can see them or give therapy after listening to their problems.”
- Psychiatrist 3
Integrating low-cost digital MH services was another suggestion of the stakeholders (n = 6) to help the community with all socioeconomic characteristics.
“In our society, people don't agree to take expensive MH support. So, it should be cost-effective, especially for students and females with economic uncertainty.”
- PWLE 7
Though these opinions, stakeholders voiced the strategies to reduce MH care inequity in rural and underprivileged areas through integrating of digital technology-based services and capacity building of service providers and users.
3.3.3. Designing and implementing new strategies for mental health care
Participants felt that the digital space held significant potential for addressing questions of inequity and related barriers to MH service provision. Designing new ways of providing digital MH services was suggested by several service providers (n = 7). One psychologist suggested launching more MH apps,
“We should develop various online apps such as identification tools, self-care and meditation to help the community to support their well-being and MH.”
- Psychologist 5
Another psychologist shared the idea of developing evidence-based online educative materials as well as therapeutic services to promote treatment adherence and enhance self-efficacy in the mental health care journey. They noted:
“We can share online materials that we use in a counseling therapy session with our clients. Like apps, links, etc., they could exercise those at home.”
– Psychologist 10
Furthermore, most service providers suggested that online learning materials and interventions should be disseminated in easily understandable language. Supporting this, one entrepreneur stated,
“MH-related information or content should be published in Bangla (mother tongue) so that everyone understands the meaning and comply.”
– Entrepreneur 7
The shift to digital services in MH care reflects broader shifts in both the accessibility of online MH care provision and the acceptability of such platforms. Highlighting this as one of the (positive) impacts of the ongoing COVID-19 pandemic, one stakeholder shared the prospect of adopting digital MH services as a proactive way of addressing the service limitations that exist in Bangladesh:
“We are more dependent on digital media in this COVID-19, so we can use digital media to provide MH services.”
- Entrepreneur 7
Furthermore, digital MH care offers the potential to expand such services beyond the individual to other members of the family or household. Citing the rise of family conflicts during the COVID-19 pandemic and the importance of ensuring the family's overall well-being, one psychologist suggested a productive role for online family counseling:
“When an individual of a family receives counseling, it will not be fully effective if the other family members do not realize the importance of MH care. So, it requires a concerted effort to ensure the overall growth of the family.”
- Psychologist 8
4. Programmatic implication of the findings
The study findings suggest that efforts at both the MH service provider and policy levels are required to provide optimal MH care (Table 3). It is critical to provide cost-effective and high-quality services tailored to community members' needs. Additionally, mass promotion of digital MH services and capacity building of service providers and lay health workers is required to guide the general public in the appropriate use of digital services. Further, the government should also implement legislation and policies and initiate a multi-sectoral effort to strengthen digital MH services, focusing on regulation and universal coverage.
Table 3.
Programmatic implication of the findings.
| Areas of interest | Constraints/barriers | Favorable factors | Opportunities for interventions |
|---|---|---|---|
| Challenges of providing mental health care services through digital media | The communication gap between service providers and users Lack of cost-effective mental health services for the overall population |
Increased demand for digital mental health services | Training mental health professionals to provide mental health support effectively through digital media Integrating low-cost digital mental health services in universal health coverage |
| Unable to prescribe all kinds of psychiatric drugs online | Existence of telemedicine services for other health issues | Regulation and monitoring of digital mental health services so that professionals can provide need-based care. Tailoring of need specific personalized care guided by evidence and community interest Strengthening psychiatric care pathway through telemedicine |
|
| Maintaining a proper therapeutic environment Lack of privacy of mental health services |
Available good examples of successful cases of digital services | Creating evidence-based guidelines and rules for both users and service providers to ensure quality of care. Proper advertisements of successful stories. |
|
| Misleading information about mental health-related issues creats misconceptions Malpractice among mental health service providers Lack of certification and licensing body for providing authentic mental health support |
Digital-based mental health-related platforms are available Existence of mental health act 2018 |
Establishing monitoring and evaluation body to ensure ethical practice and improve the quality of care, mental health-related information on the websites Encourage other health and mental health service providers to create and share mental health content via their social media platforms. Proper implementation of the mental health act and monitoring the overall mental health services. |
|
| Weak digital communication system and technological issues Lack of digital apps for mental health services Lack of knowledge of using digital media and devices effectively |
Widespread use of mobile phones nationwide People are receiving mental health care through digital media Presence of lay health workers |
Strengthening digital communication system and expanding the reach of strong telecommunication system Increasing advocacy at the government level to focus on technological advancement to improve the networking system. Launching apps and software for mental health to share evidence-based online educative materials and therapeutic services for the general population. Capacity building of lay health workers in training community people in using digital mental health services |
|
| Lack of collaboration among different level health and mental health service providers | Presence of medical and non-medical mental health service providers | Creation of governmental forum for gathering different level mental health service providers for increased collaboration and | |
| Lack of knowledge among population about mental health care and services. | Existence different mental health services in Bangladesh | Mass promotion of mental health professionals and services through digital media about the qualifications. |
5. Discussion
Previous international studies have assessed and evaluated the potential of various digital MH care services and offer insights into the potential for such services in LMIC settings (Arafat et al., 2021; Zhou et al., 2020; Hungerbuehler et al., 2016; Amos et al., 2020; Berry et al., 2019). However, limited research has been undertaken on digital MH care in Bangladesh. This qualitative study is one of the first to explore how stakeholders and community members perceived the role of digital media in influencing MH care-seeking behavior. While the benefits were clearly articulated, participants shared their concerns regarding the various challenges of digital MH care and provided recommendations on strengthening digital MH care services.
According to our findings, one of the significant benefits of digital media was increased mass awareness and MH literacy by disseminating readily available MH-related information, especially during the pandemic. For instance, given that there are reportedly more than 2.1 billion global social media users per day, digital media offers the potential to reach a large population in a short time frame and across geographic distances (Latha et al., 2020). In coherence with our findings, globally, a range of digital platforms (social media, instant messaging applications, video conferencing, animations etc.) have been utilized as a viable method in raising mass awareness and providing care (Siriwardhana et al., 2013; Hanisch et al., 2016; Trivedi et al., 2007; Arafat et al., 2021; Hungerbuehler et al., 2016; Maulik et al., 2017; Amos et al., 2020; Berry et al., 2019; Iqbal, 2020; Ifdil et al., 2020). Digital media-based MH content has been demonstrated as leading to increased healthcare-seeking behaviors among the population, another significant benefit of such services (Siriwardhana et al., 2013; Hanisch et al., 2016; Trivedi et al., 2007; Arafat et al., 2021; Hungerbuehler et al., 2016; Maulik et al., 2017; Amos et al., 2020).
In Bangladesh, there are limited psychiatrists and psychologists for a population of 163 million people, which highlights the potential role of an integrated digitally-based mental health services (Sakib, 2021; Alam et al., 2020; Islam and Biswas, 2015; Kemp et al., 2022). Currently, various digital media-based solutions are provided by NGOs: Kaan Pete Roi, for example, acts as a suicide prevention helpline (Khan et al., 2021), while the mobile app MAYA provides countrywide health and mental healthcare services through doctors and psychologists via SMS and telecommunication (MAYA, 2022). Furthermore, peer support services and online counseling session services through WhatsApp are provided by different online social media platforms (WSIF, 2018). With the support of existing resources of mental service providers, evidence-based solutions from other countries can be adopted and customized for integrating digital health interventions for strengthening mental health care in Bangladesh.
The stakeholder participants in the current study confirmed both availability and heightened usage of digital mental health services in recent times, especially during the COVID-19. The promotion of service providers on social media platforms and the availability of telemedicine and counseling services have stimulated self-referrals, particularly in the ongoing pandemic (Latha et al., 2020; Koonin et al., 2020; Stoll et al., 2020; Syed Masud Ahmed et al., 2015). The pandemic has provoked fear, anxiety, and depression symptoms among the general population, resulting in an urgent need for MH care (Fountoulakis et al., 2022; Islam et al., 2021b). Digital media assisted in the non-disruption of the existing non-digital MH care pathways even with social isolation (Di Carlo et al., 2021). These findings align with prior studies demonstrating the breakthrough role of digital MH care during COVID-19, and highlighting their applicability for future crises (Arafat et al., 2021; Zhou et al., 2020).Digital platforms allow the service providers to avoid costly physical infrastructure expenses while ensuring MH care at the convenience and comfort of the service users (Trivedi et al., 2007; Islam and Biswas, 2015; Hasan et al., 2021; WHO, 2007; Acharibasam and Wynn, 2018; Moner Bondhu, n.d.; Women Support Inititative Forum- WSIF, n.d.; Leite et al., 2020). Similarly, factors such as easy accessibility, privacy, mobility, and ample population coverage in a short time frame have been reported as benefits of utilizing digital media platforms (Trivedi et al., 2007; Islam and Biswas, 2015; Hasan et al., 2021; Acharibasam and Wynn, 2018).
Despite the benefits, both service providers and users expressed concerns regarding distant mental health care, such as lack of in-person presence and breach of confidentiality. Communication gaps due to unavailability of non-verbal cues and asynchronous time delay in the feedback were also identified as possible contributors to a therapeutic relationship breakdown between service user and provider (Acharibasam and Wynn, 2018; Amos et al., 2020; Islam et al., 2021c; Pesämaa et al., 2004). Furthermore, privacy was a concern: participants reported being worried about their counseling sessions being overhead by surrounding people, while unsecured network connections led to concerns about compromised confidentiality of information, causing mistrust in services (Li et al., 2018). Similar findings were reported in previous studies, where cyberbreaches of confidentiality and communication were some of the negative aspects of digital MH care services (Amos et al., 2020; Leite et al., 2020; Pesämaa et al., 2004; Hjelm, 2005). Video conferencing, having open discussions of session plans and establishing a written contract to confirm mutual agreement may be used to mitigate the mentioned challenges (Leite et al., 2020; Pesämaa et al., 2004; Li et al., 2018).
The digital divide has an impact in Bangladesh. Our study findings demonstrated that poor network connections and technology illiteracy in peripheral regions are other major challenges of digital MH care and may result in the digital exclusion of populations (Berry et al., 2019). Technology skills training of community people may be an acceptable solution to avoid digital exclusion (Berry et al., 2019). Publicly mobilizing community resources and engaging non-profit institutions for such training and support have been extensively efficient in providing MH care via digital technology in rural areas of LMICS, including Bhutan and Nepal (Kumar, 2011; Thara and Padmavati, 2013). Our findings also infer that misinformation and stigmas spread by social media can negatively impact MH and healthcare-seeking behavior among service users. MH is already a stigmatized issue, and misleading information on social media can build on these stigmas (Li et al., 2018). Stigmatized individuals may feel devalued by, and discriminated from others, leading them to adopt harmful coping mechanisms such as secrecy or withdrawal from health care (Hasan, 2020; Moses, 2009; Mascayano et al., 2015). Therefore it is highly recommended that digital MH care services adopt anti-stigma campaigns via digital media to combat misinformation and inappropriate content, as proven effective in earlier studies (Fountoulakis et al., 2022; Hasan, 2020). Similarly, LMICs like Uganda and India have also declared various focused anti-stigma programs at policy and community levels (Fountoulakis et al., 2022; Hasan, 2020; Moses, 2009). Moreover, these mitigation pathways suggested by the studies from developing countries can also be adapted in Bangladesh to achieve comprehensive MH care.
In contrast to the various challenges, the stakeholders also emphasized various recommendations for strengthening mental health care services. These involved different levels of governance in establishing solutions: social media should be used in a structured manner to prevent the online dissemination of stigmas and inappropriate information, which may require the involvement of social media platforms. In this regard, different health professionals can be directly involved in content development and sharing. They should also maintain transparency regarding their qualifications, enabling them to build trustful relationships with their clients; accreditation with formal bodies may play an important role. Online content should be robustly monitored and evaluated in collaboration with government bodies to provide trusted platforms.
Past literature suggests that training in digital technology skills can decentralize health care services in hard-to-reach areas (Naslund et al., 2017). Our findings also recommended the increased training of specialized and non-specialized MH care professionals who will train the community to use digital health care efficiently.
Another significant recommendation of our stakeholders includes developing and implementing new strategies for MH care such as online applications such as apps, various forms of counseling options like family counseling, etc. These recommendations are supported by prior online-based initiatives like lists of available help information, self-help applications as potential MH illness prevention tools, and online peer-support communities (Koonin et al., 2020; Stoll et al., 2020; Fountoulakis et al., 2022). Overall, our study findings supported the literature and provided additional insights into the strengths, challenges, and recommendations of digital MH care in a limited resource setting like Bangladesh.
6. Strength and limitations
The prime strength of this study lies in engaging the prominent stakeholders and getting their diverse insights on the issue. Views and perceptions from four different sets of participants helped limit subjective bias. Participants were selected purposively, which may have led to a social desirability bias to have positive insights on the study topic causing social desirability bias, and the limited sample size (n = 37) might lack information from a holistic point of view. These findings are potentially very relevant to other limited-resource settings, although generalizability is limited due to the qualitative study design.
7. Conclusion
Given the increased burden of MH disorders globally and the ongoing COVID-19 pandemic circumstances, the shift to digital mental health care was the most suitable option for service users and providers in Bangladesh. Hence, it was much needed to explore the contemporary perspectives and document the key stakeholders' viewpoints regarding the widely used digital mental health care services. These study findings revealed how digital MH care was perceived as beneficial to increasing MH literacy and accessible by the people despite the challenges induced by the pandemic. The study findings set the foundation for further longitudinal studies on digital MH care to assess the effectiveness and explore perspectives of diverse root-level stakeholders expanding the geographic areas.
8. Relevance for clinical practice
In a low-resource setting like Bangladesh, integrating digital technology into the MH system has the potential to provide available, accessible, and affordable care throughout the country. MH professionals can adopt digital technology in their daily practice to deliver MH interventions, and disseminate MH awareness. The findings support that MH care delivered through digital technologies can be adopted and replicated in other settings like Bangladesh and will guide researchers to collect more evidence to improve their practice.
Funding
This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
CRediT authorship contribution statement
Conceptualization: KK. Methodology: KNK, JS. Analysis and interpretation of data: KNK, JS, RBM. Writing - original draft preparation: JS, RM. Writing - review and editing: KNK, NW, THD. Critical revision of the manuscript: KNK, NW, DC, THD. Supervision: KNK. All authors have read and approved the manuscript.
Availability of data and materials
The qualitative data used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Declaration of competing interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
Acknowledgments
Acknowledgement
The authors would like to thank all the stakeholders who participated in this study. icddr,b is grateful to Bangladesh government, Canada, Sweden and the UK for providing core/unrestricted support.
Footnotes
Supplementary data to this article can be found online at https://doi.org/10.1016/j.invent.2022.100544.
Contributor Information
Kamrun Nahar Koly, Email: koly@icddrb.org.
Jobaida Saba, Email: kazi.jobaida.saba@gmail.com.
Rasma Muzaffar, Email: rasma.muzaffar@gmail.com.
Rifath Binta Modasser, Email: rifathalina456@gmail.com.
Tasdik Hasan M, Email: m.hasan@monash.edu.
David Colon-Cabrera, Email: david.coloncabrera@monash.edu.
Narelle Warren, Email: narelle.warren@monash.edu.
Appendix A. Supplementary data
Supplementary material
References
- Acharibasam J.W., Wynn R. Telemental health in low-and middle-income countries: a systematic review. Int. J. Telemed. Appl. 2018;2018 doi: 10.1155/2018/9602821. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Alam F., Hossain R., Ahmed H.U., Alam M.T., Sarkar M., Halbreich U. Stressors and mental health in Bangladesh: current situation and future hopes. BJPsych Int. 2020:1–4. doi: 10.1192/bji.2020.57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Amos P.M., Bedu-Addo P., Antwi T. Experiences of online counseling among undergraduates in some Ghanaian Universities. SAGE Open. 2020;10(3) 2158244020941844. [Google Scholar]
- Arafat M.Y., Zaman S., Hawlader M.D.H. 2021. Telemedicine Improves Mental Health in COVID-19 Pandemic. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Barnett A., Savic M., Pienaar K., Carter A., Warren N., Sandral E., et al. Enacting 'more-than-human' care: clients' and counsellors' views on the multiple affordances of chatbots in alcohol and other drug counselling. Int. J. Drug Policy. 2021;94 doi: 10.1016/j.drugpo.2020.102910. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Berry N., Lobban F., Bucci S. A qualitative exploration of service user views about using digital health interventions for self-management in severe mental health problems. BMC Psychiatry. 2019;19(1):1–13. doi: 10.1186/s12888-018-1979-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bucci S., Schwannauer M., Berry N. The digital revolution and its impact on mental health care. Psychol. Psychother. Theory Res. Pract. 2019;92(2):277–297. doi: 10.1111/papt.12222. [DOI] [PubMed] [Google Scholar]
- Casares D.R., Jr. Embracing the podcast era: trends, opportunities, & implications for counselors. J. Creat. Ment. Health. 2022;17(1):123–138. [Google Scholar]
- Clarke V., Braun V., Hayfield N. Thematic analysis. Qual. Psychol. 2015;222:248. [Google Scholar]
- Collins P.Y., Patel V., Joestl S.S., March D., Insel T.R., Daar A.S., et al. Grand challenges in global mental health. Nature. 2011;475(7354):27–30. doi: 10.1038/475027a. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Di Carlo F., Sociali A., Picutti E., Pettorruso M., Vellante F., Verrastro V., et al. Telepsychiatry and other cutting-edge technologies in COVID-19 pandemic: bridging the distance in mental health assistance. Int. J. Clin. Pract. 2021;75(1) doi: 10.1111/ijcp.13716. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Fountoulakis K.N., Karakatsoulis G., Abraham S., Adorjan K., Ahmed H.U., Alarcón R.D., et al. Results of the COVID-19 mental health international for the general population (COMET-G) study. Eur. Neuropsychopharmacol. 2022;54:21–40. doi: 10.1016/j.euroneuro.2021.10.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hanisch S.E., Twomey C.D., Szeto A.C., Birner U.W., Nowak D., Sabariego C. The effectiveness of interventions targeting the stigma of mental illness at the workplace: a systematic review. BMC Psychiatry. 2016;16(1):1–11. doi: 10.1186/s12888-015-0706-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hasan M.T. 2020. Addressing the COVID-19 Related Stigma and Discrimination: A Fight Against Infodemic in Bangladesh. [Google Scholar]
- Hasan M.T., Anwar T., Christopher E., Hossain S., Hossain M.M., Koly K.N. The current state of mental healthcare in Bangladesh: part 1–an updated country profile. BJPsych Int. 2021:1–5. doi: 10.1192/bji.2021.41. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hjelm N. Benefits and drawbacks of telemedicine. J. Telemed. Telecare. 2005;11(2):60–70. doi: 10.1258/1357633053499886. [DOI] [PubMed] [Google Scholar]
- Hossain M.D., Ahmed H.U., Chowdhury W.A., Niessen L.W., Alam D.S. Mental disorders in Bangladesh: a systematic review. BMC Psychiatry. 2014;14(1):1–8. doi: 10.1186/s12888-014-0216-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hungerbuehler I., Valiengo L., Loch A.A., Rössler W., Gattaz W.F. Home-based psychiatric outpatient care through videoconferencing for depression: a randomized controlled follow-up trial. JMIR Ment. Health. 2016;3(3) doi: 10.2196/mental.5675. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ifdil I., Fadli R.P., Suranata K., Zola N., Ardi Z. Online mental health services in Indonesia during the COVID-19 outbreak. Asian J. Psychiatr. 2020;51 doi: 10.1016/j.ajp.2020.102153. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Iqbal M.H. Telemedicine: an innovative twist to primary health care in rural Bangladesh. J. Prim. Care Community Health. 2020;11 doi: 10.1177/2150132720950519. 2150132720950519. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam A., Biswas T. Mental health and the health system in Bangladesh: situation analysis of a neglected domain. Am. J. Psychiatry Neurosci. 2015;3(4):57–62. [Google Scholar]
- Islam M.M., Islam M.M., Ahmed F., Rumana A.S. Creative social media use for Covid-19 prevention in Bangladesh: a structural equation modeling approach. Soc. Netw. Anal. Min. 2021;11(1):1–14. doi: 10.1007/s13278-021-00744-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Islam M.N., Khan S.R., Islam N.N., Rezwan-A-Rownok M., Zaman S.R., Zaman S.R. Springer; 2021. A Mobile Application for Mental Health Care During COVID-19 Pandemic: Development and Usability Evaluation with System Usability Scale. International Conference on Computational Intelligence in Information System. [Google Scholar]
- Islam M.R., Sultana M.S., Khan A.H., Hossain S., Sikder M.T., Hasan M.T., et al. Fear and depressive symptoms amid COVID-19: a cross-sectional pilot study among adult population in Bangladesh. Heliyon. 2021;7(7) doi: 10.1016/j.heliyon.2021.e07395. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kanuri N., Arora P., Talluru S., Colaco B., Dutta R., Rawat A., et al. Examining the initial usability, acceptability and feasibility of a digital mental health intervention for college students in India. Int. J. Psychol. 2020;55(4):657–673. doi: 10.1002/ijop.12640. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kemp C.G., Concepcion T., Ahmed H.U., Anwar N., Baingana F., Bennett I.M., et al. Baseline situational analysis in Bangladesh, Jordan, Paraguay, the Philippines, Ukraine, and Zimbabwe for the WHO Special Initiative for Mental Health: Universal Health Coverage for Mental Health. PLoS One. 2022;17(3) doi: 10.1371/journal.pone.0265570. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Khan A.R., Arendse N., Ratele K. Suicide prevention in Bangladesh: the current state and the way forward. Asian Soc. Work Policy Rev. 2021;15(1):15–23. [Google Scholar]
- Koonin L.M., Hoots B., Tsang C.A., Leroy Z., Farris K., Jolly B., et al. Trends in the use of telehealth during the emergence of the COVID-19 pandemic—United States, January–March 2020. Morb. Mortal. Wkly Rep. 2020;69(43):1595. doi: 10.15585/mmwr.mm6943a3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kumar A. Mental health services in rural India: challenges and prospects. Health. 2011;3(12):757–761. [Google Scholar]
- Latha K., Meena K., Pravitha M., Dasgupta M., Chaturvedi S. Effective use of social media platforms for promotion of mental health awareness. J. Educ. Health Promot. 2020;9 doi: 10.4103/jehp.jehp_90_20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Leite H., Hodgkinson I.R., Gruber T. New development:‘Healing at a distance’—telemedicine and COVID-19. Public Money Manag. 2020;40(6):483–485. [Google Scholar]
- Li A., Jiao D., Zhu T. Detecting depression stigma on social media: a linguistic analysis. J. Affect. Disord. 2018;232:358–362. doi: 10.1016/j.jad.2018.02.087. [DOI] [PubMed] [Google Scholar]
- Mascayano F., Armijo J.E., Yang L.H. Addressing stigma relating to mental illness in low-and middle-income countries. Front. Psych. 2015;6:38. doi: 10.3389/fpsyt.2015.00038. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathers C. World Health Organization; 2008. The Global Burden of Disease: 2004 Update. [Google Scholar]
- Maulik P.K., Kallakuri S., Devarapalli S., Vadlamani V.K., Jha V., Patel A. Increasing use of mental health services in remote areas using mobile technology: a pre–post evaluation of the SMART mental health project in rural India. J. Glob. Health. 2017;7(1) doi: 10.7189/jogh.07.010408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- MAYA 2022. https://m.mayaiswithyou.com/ Available from:
- Moner Bondhu .
- Moses T. Self-labeling and its effects among adolescents diagnosed with mental disorders. Soc. Sci. Med. 2009;68(3):570–578. doi: 10.1016/j.socscimed.2008.11.003. [DOI] [PubMed] [Google Scholar]
- Naslund J.A., Aschbrenner K.A., Araya R., Marsch L.A., Unützer J., Patel V., et al. Digital technology for treating and preventing mental disorders in low-income and middle-income countries: a narrative review of the literature. Lancet Psychiatry. 2017;4(6):486–500. doi: 10.1016/S2215-0366(17)30096-2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Naveed S., Waqas A., Chaudhary A.M.D., Kumar S., Abbas N., Amin R. Prevalence of common mental disorders in South Asia: a systematic review and meta-regression analysis. Front. Psych. 2020:11. doi: 10.3389/fpsyt.2020.573150. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ngui E.M., Khasakhala L., Ndetei D., Roberts L.W. Mental disorders, health inequalities and ethics: a global perspective. Int. Rev. Psychiatry. 2010;22(3):235–244. doi: 10.3109/09540261.2010.485273. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ogbo F.A., Mathsyaraja S., Koti R.K., Perz J., Page A. The burden of depressive disorders in South Asia, 1990–2016: findings from the global burden of disease study. BMC Psychiatry. 2018;18(1):333. doi: 10.1186/s12888-018-1918-1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Organization WH . 2007. WHO-AIMS Report on Mental Health System in Bangladesh. [Google Scholar]
- Parikh S.V., Huniewicz P. E-health: an overview of the uses of the internet, social media, apps, and websites for mood disorders. Curr. Opin. Psychiatry. 2015;28(1) doi: 10.1097/YCO.0000000000000123. [DOI] [PubMed] [Google Scholar]
- Pesämaa L., Ebeling H., Kuusimäki M.-L., Winblad I., Isohanni M., Moilanen I. Videoconferencing in child and adolescent telepsychiatry: a systematic review of the literature. J. Telemed. Telecare. 2004;10(4):187–192. doi: 10.1258/1357633041424458. [DOI] [PubMed] [Google Scholar]
- Polanczyk G.V., Salum G.A., Sugaya L.S., Caye A., Rohde L.A. Annual research review: a meta-analysis of the worldwide prevalence of mental disorders in children and adolescents. J. Child Psychol. Psychiatry. 2015;56(3):345–365. doi: 10.1111/jcpp.12381. [DOI] [PubMed] [Google Scholar]
- Sakib S.N. Anadolu Agency; 2021. Bangladesh: mental health stigma a barrier to care.https://www.aa.com.tr/en/asia-pacific/bangladesh-mental-health-stigma-a-barrier-to-care/2208229# Available from: [Google Scholar]
- Semrau M., Evans-Lacko S., Alem A., Ayuso-Mateos J.L., Chisholm D., Gureje O., et al. Strengthening mental health systems in low-and middle-income countries: the emerald programme. BMC Med. 2015;13(1):1–9. doi: 10.1186/s12916-015-0309-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Siriwardhana C., Adikari A., Van Bortel T., McCrone P., Sumathipala A. An intervention to improve mental health care for conflict-affected forced migrants in low-resource primary care settings: a WHO MhGAP-based pilot study in Sri Lanka (COM-GAP study) Trials. 2013;14(1):1–7. doi: 10.1186/1745-6215-14-423. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Soron T.R., Chowdhury Z. Monerdaktar: a large online mental health service to improve access to care in Bangladesh during the COVID-19 pandemic. Eur. Psychiatry. 2021;64(S1):S39–S40. [Google Scholar]
- Stoll J., Sadler J.Z., Trachsel M. The ethical use of telepsychiatry in the Covid-19 pandemic. Front. Psych. 2020;11:665. doi: 10.3389/fpsyt.2020.00665. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Syed Masud Ahmed B.B.A., Anwar Iqbal, Begum Tahmina, Huque Rumana, Khan Jahangir A.M., Nababan Herfina, Osman Ferdaus Arfina, Dhaka University . World Health Organization; 2015. Bangladesh health system review.https://iris.wpro.who.int/bitstream/handle/10665.1/11357/9789290617051_eng.pdf Available from: [Google Scholar]
- Thara R. Using mobile telepsychiatry to close the mental health gap. Curr. Psychiatry Rep. 2012;14(3):167–168. doi: 10.1007/s11920-012-0267-x. [DOI] [PubMed] [Google Scholar]
- Thara R., Padmavati R. Community mental health care in South Asia. World Psychiatry. 2013;12(2):176. doi: 10.1002/wps.20042. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tong A., Sainsbury P., Craig J. Consolidated criteria for reporting qualitative research (COREQ): a 32-item checklist for interviews and focus groups. Int. J. Qual. Health Care. 2007;19(6):349–357. doi: 10.1093/intqhc/mzm042. [DOI] [PubMed] [Google Scholar]
- Trivedi J.K., Goel D., Kallivayalil R.A., Isaac M., Shrestha D.M., Gambheera H.C. Regional cooperation in South Asia in the field of mental health. World Psychiatry. 2007;6(1):57. [PMC free article] [PubMed] [Google Scholar]
- Vigo D., Thornicroft G., Atun R. Estimating the true global burden of mental illness. Lancet Psychiatry. 2016;3(2):171–178. doi: 10.1016/S2215-0366(15)00505-2. [DOI] [PubMed] [Google Scholar]
- Wilson A., Moretto N., Langbecker D., Snoswell C.L. Use of reimbursed psychology videoconference services in Australia: an investigation using administrative data. Value Health Reg. Issues. 2020;21:69–73. doi: 10.1016/j.vhri.2019.07.007. [DOI] [PubMed] [Google Scholar]
- Women Support Inititative Forum- WSIF https://wsifbd.com/ Available from:
- WSIF Women support initiative forum. 2018. https://wsifbd.com/ Available from:
- Zhou X., Snoswell C.L., Harding L.E., Bambling M., Edirippulige S., Bai X., et al. The role of telehealth in reducing the mental health burden from COVID-19. Telemed. e-Health. 2020;26(4):377–379. doi: 10.1089/tmj.2020.0068. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplementary material
Data Availability Statement
The qualitative data used and/or analyzed during the current study are available from the corresponding author on reasonable request.