Abstract
As exclusive e-cigarette use increases and combustible cigarette use declines among American youth, tracking and reporting social, racial, and economic disparities as they emerge will increasingly be an important surveillance activity. E-cigarette harm evaluation should also look beyond the immediate physical harms, and include social and financial harms as well.
Keywords: Adolescent, e-cigarettes, educational attainment, fundamental causes, social inequality, vaping
Foxon and Selya (2020) document that the prevalence of exclusive e-cigarette use among United States (US) youth has substantially increased around 2010, whereas exclusive combustible cigarette (cigarette) use continuously declined [1]. This evidence is consistent with e-cigarette use diverting youth from cigarette use, which suggests a net public health benefit, insofar as e-cigarettes are less harmful, and increased prevalence does not generate cigarette users later [1]. However, asking how harmful e-cigarettes are requires an interrogation of what harms, inflicted on whom and, specifically, on which social class?
Cigarettes were largely unassociated with social class before information about their health harms became well-known [2], then, social disparities emerged. Access to health information is a privilege, and the fact that social gradients in health outcomes emerge as information is uncovered has been reproduced many times. This is consistent with fundamental cause theory, in which access to flexible resources (e.g. knowledge, money, power, and prestige) protects individuals from health outcomes as well as their causes and wider consequences [3]. Health inequities emerging from unequal access to information are produced and reproduced so that class gradients persist over time; as harmful effects of one cause are eliminated, new ones emerge [3]. These gradients are further potentiated by other vectors of oppression (e.g. racism). Even in the face of high socio-economic status (SES), racial/ethnic minorities continue to experience worse health outcomes and increased risk of disease or weaker protective effects of class [4].
How does this historic legacy of cigarette use relate to e-cigarette use? E-cigarettes are less harmful than cigarettes when considering carcinogens and chemicals [5,6]. However, studying additional potential harms is critical [7–9]. In the United States, for example, around 3000 people have been hospitalized for illnesses linked to tetrahydrocannabinol (THC)-containing vape products and dozens have died, prompting reactive federal regulation [10]. This suggests that in a rapidly changing marketplace of products, ongoing assessment of risks is key.
Harms of e-cigarettes may also move beyond the respiratory. Cigarette-using youth have lower high school graduation and college attendance rates than non-using youth, and lower SES through the life course [11] because of shared risk factors, complex and reinforcing selection, and causation mechanisms (e.g. social networks [12] and neurocognitive factors [13]). How these same differences in education, income, and financial stability are reproduced in e-cigarette users requires explicit monitoring, because social class is perhaps the largest and most preventable cause of death worldwide [2,3,14,15]. Arrests for cigarette-related crimes also disproportionately pattern by social class and race, leading to increased incarceration and injury (e.g. Eric Garner was killed in New York City in 2014 in an incident arising from unlicensed cigarette selling [16]).
Overall, if youth begin to view e-cigarettes as potentially harmful to health, fundamental cause theory shows that we can expect disparities in use to emerge. That is, individuals with flexible resources may reduce their use of e-cigarettes, whereas those with limited flexible resources may continue to use e-cigarette at a stable or increased rate. Additionally, as federal regulations limiting access to e-cigarettes increase, we can further expect harms because of use of these products, including material deprivation and incarceration patterned by class and race, to be reproduced.
On the other hand, e-cigarettes may help to reduce the 500000 smoking-related deaths/year in the United States [17], insofar as individuals use e-cigarettes as a replacement for cigarettes. Here too, disparities emerge; e-cigarette accessibility as a smoking cessation aid is restricted among racial/ethnic minorities and social class [18]. Therefore, to the extent that e-cigarettes are an effective harm reduction technique, we can again expect disparities to emerge.
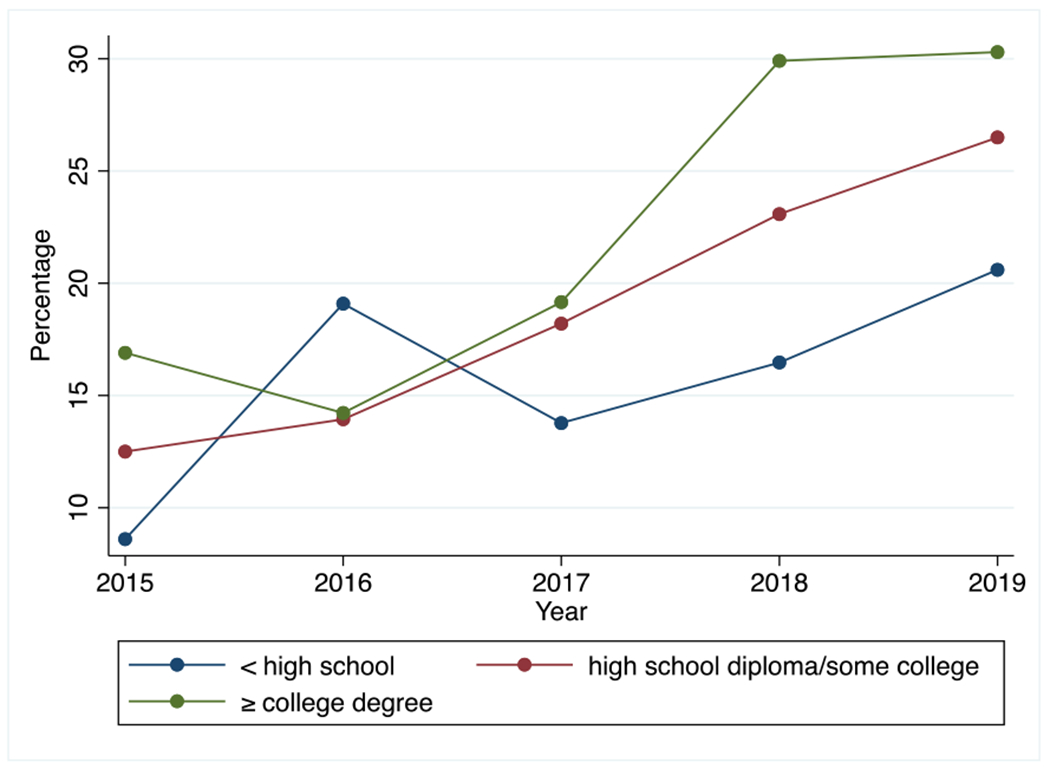
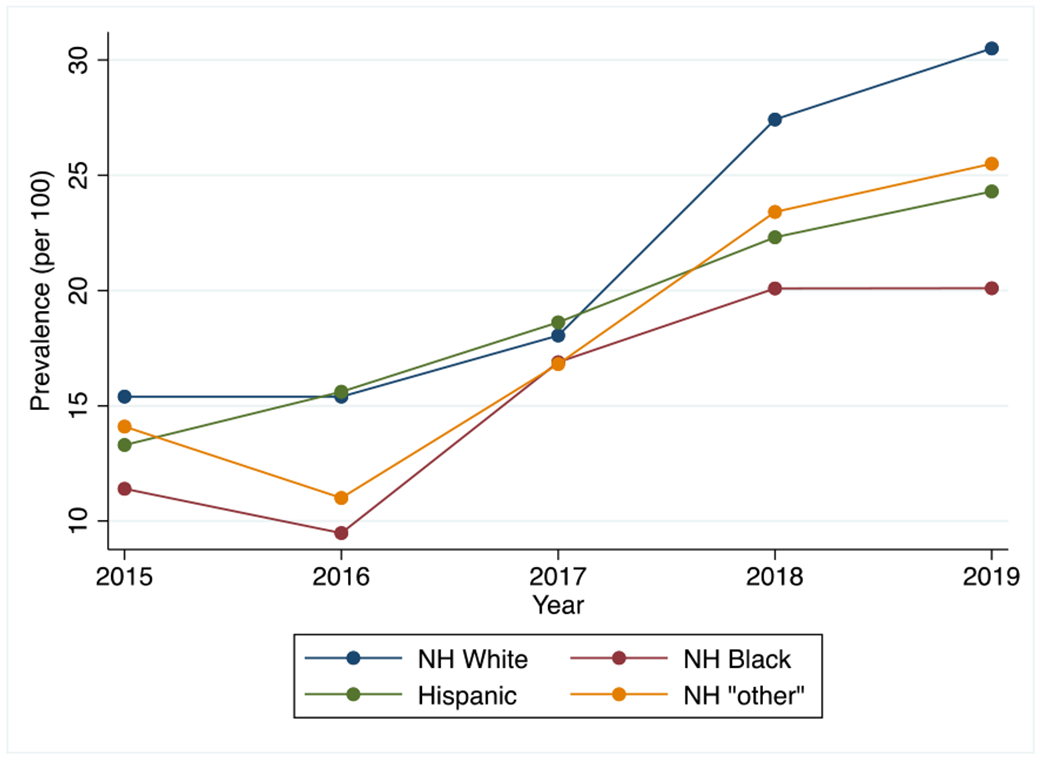
What do we currently know about the socio-demographics of exclusive e-cigarette using youth in the United States? Our analysis of data from Monitoring the Future suggests that the prevalence of lifetime exclusive e-cigarette use is highest among the most socially advantaged adolescents: those who are white and have parents who are highly educated (see Figs 1 & 2). Yet, differences by social class are emerging. The increase in e-cigarette use from 2015 to 2019 was highest among low SES adolescents (risk difference [RD] = 138.5%) and lowest among high SES adolescents (RD = 78.6%). By race, white adolescents remain the most likely to exclusively use e-cigarettes and to increase the most across recent years. However, we can anticipate racial disparities emerging if negative health information about e-cigarette use becomes public.
Figure 1.
Lifetime exclusive e-cigarette use among adolescents from 2015–2019 by race/ethnicity. [Colour figure can be viewed at wileyonlinelibrary.com]
Figure 2.
Lifetime exclusive e-cigarette use among adolescents from 2015–2019 by parents SES (education only). [Colour figure can be viewed at wileyonlinelibrary.com]
Given the tobacco industry’s deception regarding the “safety” and harms of cigarette and tobacco use [7], it is possible that the e-cigarette industry could follow a similar trend, wherein potential harms of e-cigarettes will not be disclosed until health effects can no longer be ignored. Like cigarette use, there will likely be a complex array of factors that lead to inequities in e-cigarette use and associated adverse consequences, such as the influence of e-cigarette industries, lack of nicotine and e-liquid flavoring control policies, and differential access to health information and cessation services. We can use what we know about historic trends in cigarette use and changes in policy, knowledge of associated harms, and treatment and prevention techniques to see that a similar scenario may happen with e-cigarette use, in which marginalized adolescents will be the ones harmed by the potential ill effects of e-cigarettes. Understanding the extent of potential disparities, how they emerge and how they result in harm, is critical to set a research and action agenda before these harms emerge if we have any chance of their prevention.
Footnotes
Declaration of interests
None.
References
- 1.Foxon F, Selya AS Electronic cigarettes, nicotine use trends and use initiation ages among US adolescents from 1999 to 2018. Addiction 2020; 115: 2369–78. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Phelan JC, Link BG Controlling disease and creating disparities: a fundamental cause perspective. J Gerontol B Psychol Sci Soc Sci 2005. Oct 1; 60: S27–S33. [DOI] [PubMed] [Google Scholar]
- 3.Phelan JC, Link BG, Tehranifar P Social conditions as fundamental causes of health inequalities: theory, evidence, and policy implications. J Health Soc Behav 2010. Mar; 51: S28–S40. [DOI] [PubMed] [Google Scholar]
- 4.Assari S, Bazargan M Minorities’ diminished returns of educational attainment on hospitalization risk: National Health Interview Survey (NHIS). Hospital Pract Res 2019; 4: 86–91. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.McNeill A, Brose L, Calder R, Bauld L, Robson D Evidence review of e-cigarettes and heated tobacco products 2018, A Report Commissioned by Public Health England. London: Public Health England; 2018. [Google Scholar]
- 6.McNeill A, Hajek P Underpinning evidence for the estimate that e-cigarette use is around 95% safer than smoking: authors’ note. London: Public Health England; 2018. [Google Scholar]
- 7.Rowell TR, Tarran R Will chronic e-cigarette use cause lung disease? Am J Physiol Lung Cell Mol Physiol 2015. Dec 15; 309: L1398–L1409. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Wu Q, Jiang D, Minor M, Chu HW Electronic cigarette liquid increases inflammation and virus infection in primary human airway epithelial cells. PLoS ONE 2014. Sep 22; 9: e108342. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Lerner CA, Sundar IK, Yao H, Gerloff J, Ossip DJ, McIntosh S, et al. Vapors produced by electronic cigarettes and e-juices with flavorings induce toxicity, oxidative stress, and inflammatory response in lung epithelial cells and in mouse lung. PLoS ONE 2015. Feb 6; 10: e0116732. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Outbreak of lung injury associated with the use of e-cigarettes, or vaping, products. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Updated February 25, 2020. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html. Accessed July 19, 2020. [Google Scholar]
- 11.Gilman SE, Martin LT, Abrams DB, Kawachi I, Kubzansky L, Loucks EB, et al. Educational attainment and cigarette smoking: a causal association? Int J Epidemiol 2008. Jun 1; 37: 615–24. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Henneberger AK, Mushonga DR, Preston AM Peer influence and adolescent substance use: a systematic review of dynamic social network research. Adolesc Res Rev 2020. January; 2: 1–7. [Google Scholar]
- 13.Yuan M, Cross SJ, Loughlin SE, Leslie FM Nicotine and the adolescent brain. J Physiol 2015. Aug 15; 593: 3397–412. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Flaskerud JH, DeLilly CR, Flaskerud JH Social determinants of health status. Issues Ment Health Nurs 2012. Jun 29; 33: 494–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Cockerham WC, Hamby BW, Oates GR The social determinants of chronic disease. Am J Prev Med 2017. Jan; 52: S5–S12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Powell KJ Making #BlackLivesMatter: Michael Brown, Eric Garner, and the specters of black life—toward a hauntology of blackness. Cult Stud – Crit Meth 2016. Jun; 16: 253–60. [Google Scholar]
- 17.Tobacco: Fast Facts. Atlanta (GA): U.S. Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Chronic Disease Prevention and Health Promotion, Office on Smoking and Health; Updated February 25, 2020. https://www.cdc.gov/tobacco/basic_information/e-cigarettes/severe-lung-disease.html. Accessed July 19, 2020. [Google Scholar]
- 18.Giovenco DP, Spillane TE, Merizier JM Neighborhood differences in alternative tobacco product availability and advertising in new York City: implications for health disparities. Nicotine Tob Res 2019. Jul; 21: 896–902. [DOI] [PMC free article] [PubMed] [Google Scholar]


