Abstract
Background/Objectives:
Geriatric consultation has been shown to benefit some types of older patients hospitalized for acute illness and injury. However, in our institution, requests for consultation are variable, resulting in some requests occurring too late in the hospital course for optimal clinical benefit. Our objective was to test if an interprofessional intervention improved the use and timing of geriatric consultation on a hospitalist service.
Design:
Difference-in-differences (DID), which measures the difference in improvement over time between intervention and control team patients attributable to the intervention.
Setting:
1000-bed U.S. Academic Medical Center
Participants:
A total of 7038 patients aged 60 years or older admitted to a general medicine hospitalist service: n=718 on intervention teams, n=686 historical controls, n=5634 on control teams (concurrent and historic)
Intervention:
On 2 of 11 hospitalist teams, a geriatrician attended multidisciplinary discharge rounds twice weekly. The geriatrician advised on benefit of a geriatric consult for patients older than 60.
Measurements:
Primary outcome was percent of hospitalizations resulting in a geriatric consultation. Secondary outcome was time-to-geriatric consultation in days. Both outcomes were controlled for age, gender, co-morbidity, mean daily utilization, and admission in the prior 30 days. In the primary analysis, length of stay was controlled.
Results:
The intervention increased percent of patients with a geriatric consultation (DID=increase of 2.35% absolute percentage-points, CI=+ 0.59, +4.39%) and decreased time to consult (DID=3.61 fewer days, CI=−1, −7).
Conclusion:
An interprofessional intervention that focused on hospitalist ordering practices increased utilization of appropriate geriatric consultation and decreased time to consult. This model of interprofessional effort is effective. Future adaptations are needed to target scarce geriatric resources without increasing overall utilization.
Keywords: geriatric consultation, discharge planning, quality improvement
INTRODUCTION
The number of specialized geriatric providers has not kept pace with the increasing geriatric population, leading to calls for new models of care facilitating delivery of geriatric expertise.1
While units dedicated to the care of older patients have significant benefits, 2–4 they are rare. A common alternative, geriatric consultation, has been associated with improved mortality and functional status5,6 in selected clinical scenarios such as hip fracture 7 or general traumatic injury.8 However, a recent meta-analysis showed an effect only on short-term mortality.9
One reason that units may be more effective than consultation services is that units provide proactive geriatric evaluation, in contrast to consultation which is reactive to clinical (e.g., delirium) or social complications (e.g., discharge disposition). At our institution, our motivation was to improve timing and usefulness of multidisciplinary geriatric consultation for patients on the general medicine service. We desired to reduce consults requested late in the patient’s stay, sometimes on the day of potential discharge. With limited resources on our consultation team (one geriatrician, nurse, and social worker), our aim was not to expand consults to all older patients, but rather focus on those with greatest need. We hypothesized that our intervention would increase geriatric consults and decrease time to consult, increasing proactive rather than reactive care. We used a difference-in-differences design, a stronger method than a simple pre-post comparison, to control for concurrent and potentially confounding changes in health care.
METHODS
Setting & Design
This study took place between July 1, 2013 and June 30, 2014 at Michigan Medicine, a 1000-bed academic medical center, on the general direct care medicine hospitalist service. This service consists of 11 teams staffed by hospitalists alone without mid-level providers. Usual care includes weekday discharge rounds between the hospitalist and case manager.
Patient Sample & Data
The original sample consisted of all admissions to the 11 hospitalist teams during the study period. The primary unit of analysis was each inpatient admission of a patient age 60 or older. Patients were considered as having received the intervention if they were admitted to an intervention team. For this novel intervention we studied both concurrent controls (teams not participating in the intervention) as well as historic controls (patients hospitalized on all teams for one year prior to the intervention). The data set was obtained from the administrative medical record and billing data and included gender, age, admission and discharge dates, death date, procedures and physician visits, diagnosis codes for all inpatient and outpatient care within 2 years, and the diagnosis-related group (DRG).
Intervention
2 of the 11 teams agreed to participate in the intervention. No changes were made to the workflow of the remaining 9 teams. The intervention consisted of a geriatrician (one of five rotating physicians) joining discharge rounds on Mondays and Thursdays, approximately 30 minutes for two team meetings. The geriatrician made case-by-case recommendations about which patients might benefit from a formal geriatric assessment. The attending hospitalist made the final decision of a formal consult. A palliative care physician concurrently participated with the focus on improving palliative care consultation orders and timing (results are reported elsewhere).10
Measures
Exposure variable:
Hospital billing data was used to match each day of hospital care to a hospitalist and then correlated with the weekly hospitalist schedule to determine team assignment. The modal physician was used to assign teams. If a patient changed teams during the hospitalization, the final team was assigned. For a small number of patients, no clear hospitalist team could be identified because they were admitted by an overnight physician and discharged the next morning or transferred immediately to another service (e.g., intensive care, surgery). This method of determining team assignment was validated by blinded medical record review to determine the actual team providing care, using a random sample of 200 patients, which yielded 96.83% percent agreement and kappa of .78.
Outcomes:
The primary outcome was the change in the proportion of admitted patients receiving a geriatric consult, measured as the absolute difference in percent of hospitalizations with a consult during the intervention year minus the percent of hospitalizations with a consult in the prior year. Thus, the hospitalization was considered to be the primary unit of analysis. We first matched the rotating geriatrician schedule to professional claims. Unbilled visits were not captured. Time-to-consultation was calculated as days from admission to date of first geriatric consultation note. This method of measuring the outcomes was validated with blinded chart review of a random sample of 200 hospitalizations (half with a known geriatric consultation), which yielded 98.17% agreement and kappa of .96 for occurrence of a geriatric consultation, and agreement of 98.36% and kappa of .97 for the exact date of the initial geriatric consult.
We controlled for factors affecting geriatric consultation: age, gender, prior recent admissions, Charlson comorbidity score (CCS)11, length of stay (LOS) and relative value units (RVUs) per day. We used a lookback period of 2 years across all inpatient and outpatient records to calculate CCS. Recent readmission was defined as discharge within 30 days from the hospital system. RVUs per day were determined as an average of RVUs associated with all billed Common Procedural Terminology codes for procedures, evaluation, and management across the hospitalization.
Analysis
We first compared baseline characteristics between intervention versus control patients using one-way analysis of variance for continuous variables (age, RVUs/day, LOS, CCS) and chi-squared tests for proportions (gender, recent admission). Our primary analysis included the change in proportion receiving a geriatric consult (present versus absent) between the intervention and control groups over time using a difference-in-differences (DID) model. This method12 compares pre- and post- data between the control versus intervention groups to analyze differences in the change of a proportion over time. The data is analyzed as a logistic regression, with intervention versus control group as the primary predictor variable, and pre- vs post-time period indicator variable as a second predictor, and the interaction between the two variables to evaluate the statistical significance of the “DID”. We used predicted probabilities resulting from the logistic regression model to determine the DID.12 We bootstrapped the sample 1000 times to obtain 95% confidence intervals (median, 97.5th and 2.5th observations, holding continuous covariables at their means and categorical covariables at their modes). To control for clustering of patients within physicians who may have different practice patterns and responses to the intervention, we included a physician random effect.
Second, we compared time-to-consultation between intervention and control groups. We visually inspected Kaplan-Meier curves to ensure similar hazard functions, followed by a Cox proportional hazard model. Then, we estimated the DID in days-to-consultation, which we obtained from parametric survival analysis. This method is similar to obtaining median life expectancy, or the time over which half the population have died. However, in this study, where consultation occurs in much fewer than half of the patients, estimated median time-to-consult is heavily influenced by the few patients with long length of stay, resulting in estimates in median time-to-consult that are longer than the typical LOS. Therefore, to test the DID associated with the intervention on a more generalizable hospital population, we based results on an earlier time-point, when 5% rather than 50% of the population has achieved a geriatric consultation. We controlled for the same factors as in the primary analysis except LOS (omitted due to correlation with exposure time). The baseline distribution of cumulative hazard was selected based on the lowest Aikake’s criterion.13 The final model was bootstrapped 1000 times to obtain minimum expected days to achieve consultation on ≥5% of the population, using 97.5th and 2.5th estimates (units of whole days) as the 95% confidence intervals, controlling for covariables held at their means/modes. We used Stata 14 for all analyses.
RESULTS
Hospitalized Patient Characteristics
Of 7687 patients aged ≥60 years admitted during the two-year period, 7038 (91.56%) had sufficient data to assign to a hospitalist team (Supplemental Figure S1). There were no significant differences in patient age, gender, length of stay, and recent admission between intervention and control hospitalizations (Table 1).
Table 1.
Comparison of Patient and Hospitalization Characteristics between Intervention and Control Team Patients during Intervention Phase
| N=3422 | Control patients (n=2704 patients) n (%) or M±SD |
Intervention Group (n=718) n (%) or M±SD |
p-value |
|---|---|---|---|
| Age | 73.38 ± 9.30 | 73.60 ± 9.27 | 0.565 |
| Male | 1420 (52.51) | 395 (55.01) | 0.233 |
| RVUs per day* | 7.82 ± 3.93 | 7.98 ± 4.85 | 0.343 |
| CCS♯ | 3.69 ± 2.8 | 3.73 ± 2.78 | 0.768 |
| Readmitted patient⋲ | 485 (17.93) | 116 (16.16) | 0.265 |
| Length of Stay | 5.87 ± 6.37 | 6.19 ± 7.89 | 0.269 |
RVUs per day: average intensity of hospital care and resource utilization, expressed as relative value units associated with submitted charges over the hospitalization divided by length of stay
Readmitted patient: Admission date (for this hospitalization) was within 30 days of another inpatient discharge in this healthcare system
CCS=Charlson Co-morbidity Score
Proportion Receiving Geriatric Consultation
Univariate analyses
Of 7038 hospitalizations analyzed, 307 (4.36%) included a geriatric consult. For teams receiving the intervention, the percent including geriatric consultation increased from 4.37% in the year prior to 6.96% after the start of the intervention (a difference in absolute percentage points of 2.59% [95% CI 0.18–5.00%]). Intervention teams also received more consultations in concurrent comparison to control teams (6.96% versus 3.70%, a 3.27% [95% CI 1.27, 5.26%] absolute change).
There was no significant secular change over time in percent of geriatric consultation among only the control teams (4.33% to 3.70%, change = −.64% [95% CI −.39, +1.66%]).
Multivariable Analyses
In the multivariable model, which adjusted for age, gender, recent admission, LOS, CCS, and controlled individual physician effects, the predicted percent of patients receiving a geriatric consult increased by 2.16% absolute percentage-points over the study period for the intervention patients, compared to a 0.21% absolute percentage-point decrease in proportion receiving consults among the control patients. This yielded a positive 2.35% absolute change in percentage points [95% CI 0.59%−4.39%], the DID, between the two groups (Figure 1). This increase in consultations translates into an increase of 1.5 new consults per week if this intervention were applied to the entire hospitalist service.
Figure 1. Effect of Intervention on Geriatric Consultation (DID) (N=7038).
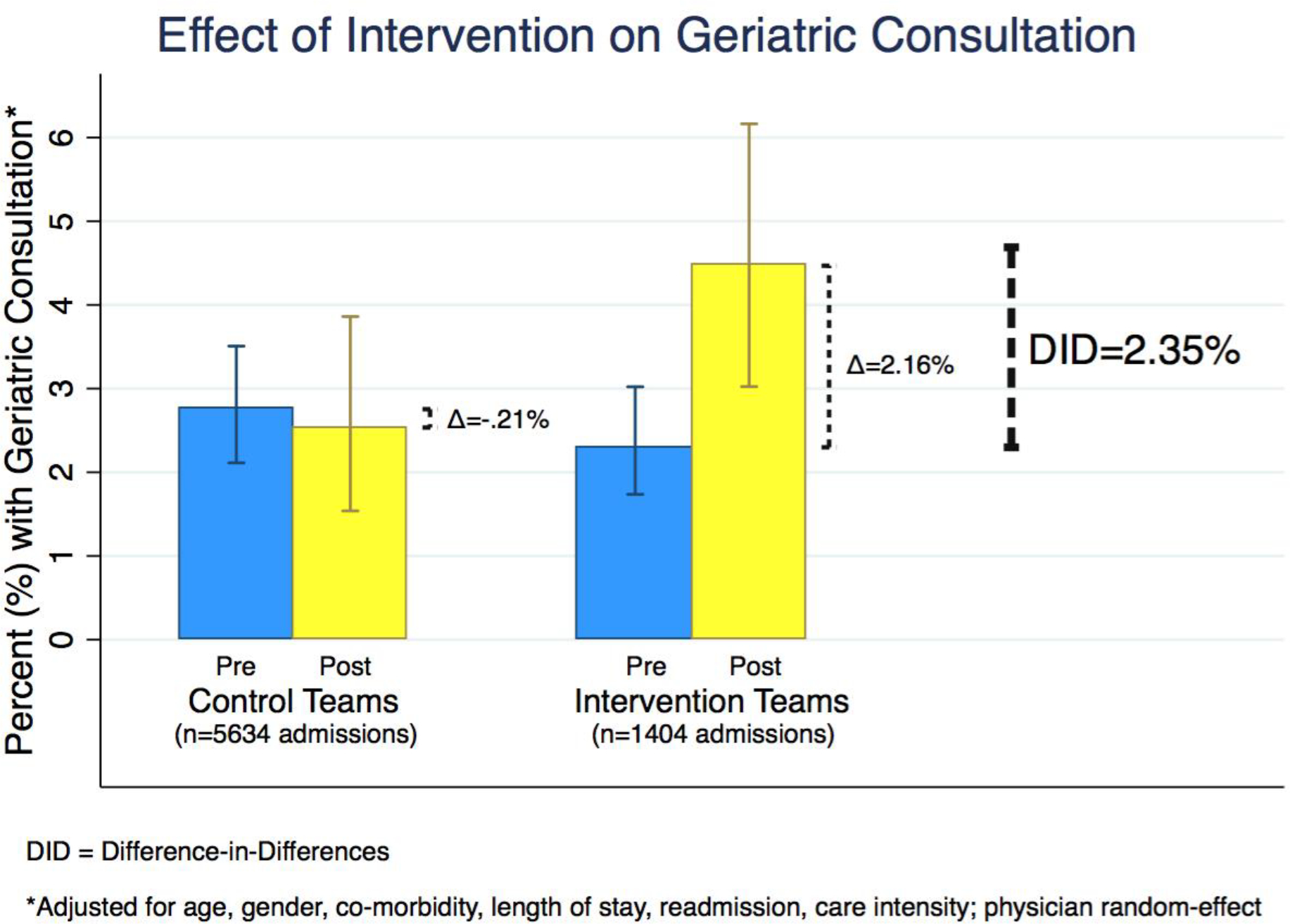
DID = Difference-in-Differences
*The predicted percentages are based on a multivariable logistic regression model including the full interaction between intervention versus control and post- versus pre-intervention time, random-effect for physician, holding constant the mean or modal values of the covariables: a male patient age 74, 7.8 average relative value units (RVUs) charged per day, Charlson comorbidity score of 3.7 points, length of stay of 6 days, with no 30-day recent hospitalization.
Time to Geriatric Consultation
The intervention group had the shortest time to consult, as demonstrated by their cumulative proportion of patients receiving a consultation (Figure 2). Using time to consult as the outcome in a Cox proportional hazard model, the unadjusted HR associated with the DID was statistically significant (HR 1.87 [1.10–3.16]). Considering parametric survival models, the best fit hazard distribution was log-normal. Controlling for covariables and holding covariables constant (at means or modes), expected days to achieve geriatric consultation on 5% of admitted patients decreased by 2.07 days in the intervention group and increased by 1.53 days in the control group, yielding a net decrease, or mean DID, of 3.61 days [95% CI 1 to 7 whole days].
Figure 2. Intervention Effect on Time to Geriatric Consult.
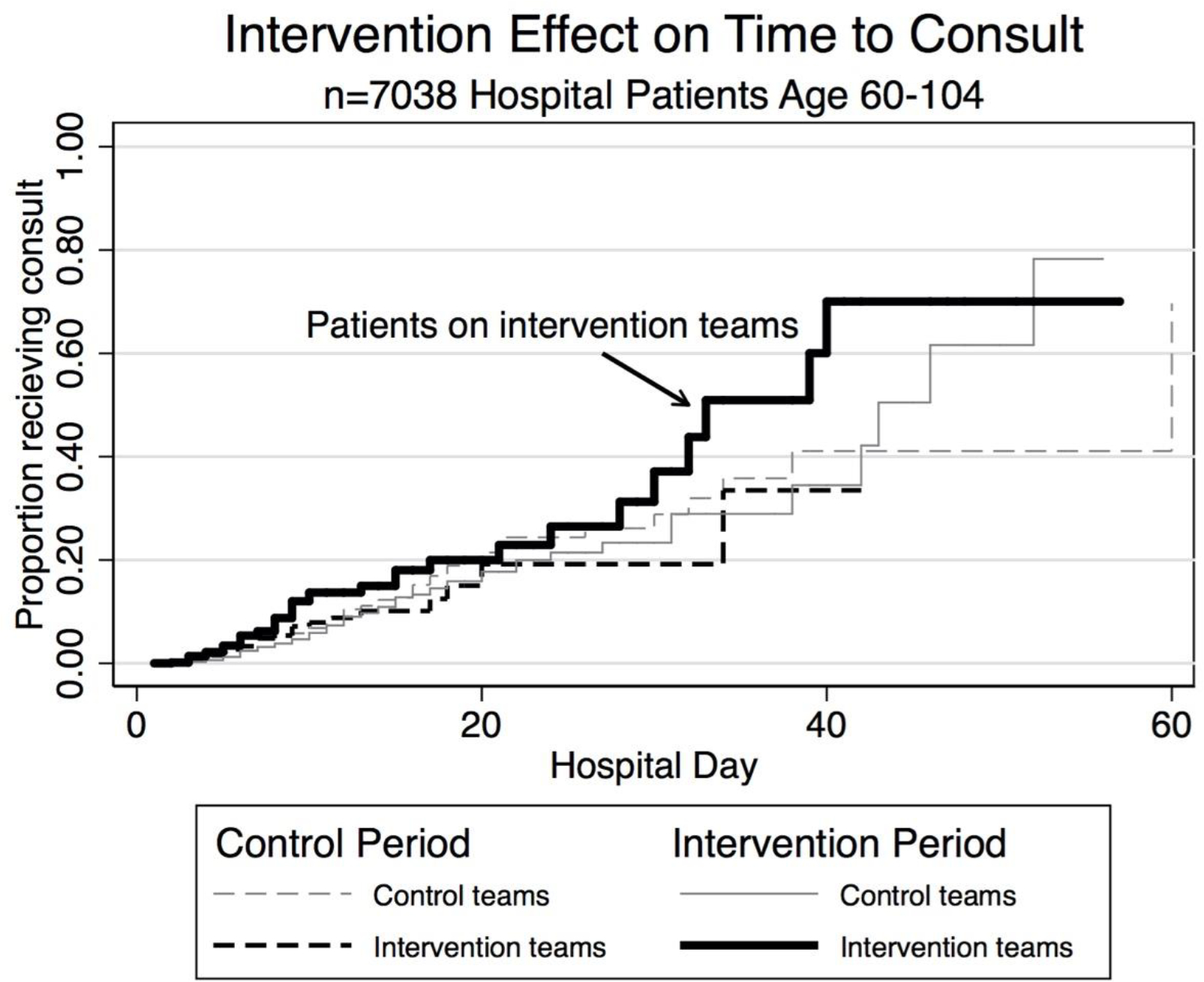
Kaplan-Meier curves of cumulative proportion of sample receiving a geriatric consultation, by intervention versus control teams. The darker solid line represents the intervention teams during the intervention. The concurrent control teams are represented by the gray solid line, intervention team patients prior to the intervention by the darker dashed line, and the control team patients prior to the intervention by the dashed grey line.
DISCUSSION
New models to efficiently increase the impact of geriatricians are desperately needed.1 We found that shared interprofessional rounds between geriatricians and hospitalists increased geriatric consultation by 2.35% of all admitted older patients to a general medicine hospitalist service and decreased the time to consult by nearly 4 days.
In this study, we increased the rigor of measure by comparing change over time for the intervention with a control group, using a difference-in-differences approach, thus decreasing risk of biased results from secular changes in the healthcare system. Our findings suggest that a minimally-resource intensive model can effectively target complex services (geriatric consultation). Second, because we controlled for effect of individual physicians (who crossed intervention and control groups), our results suggest that the more important factor in delivering earlier geriatric consults was the intervention itself, rather than hospitalist characteristics.
Our results should be viewed in light of several limitations. To feasibly allow for geriatric staff to participate, we limited the intervention to twice weekly. Therefore, patients who were admitted and discharged between enhanced discharge meetings could not directly receive the intervention. We included all patients in the analysis (intention-to-treat), which conservatively biased our findings towards no result. These results may not generalize to hospitals without capacity to handle additional geriatric consultations. However, we believe that even hospitals with less-robust geriatric services have an interest in improving the efficiency of their specialty care. This intervention could be used to increase effectiveness of a lone geriatrician, e.g., to triage less-urgent geriatric questions to outpatient resources. A future direction would include detailed chart review for appropriateness and quality of care, and measure of how many unnecessary consults we prevented (which we anecdotally noted but could not study in this design). Lastly, although we provided consultations earlier in the hospital course (i.e., decreased days to consult), we could not test for effect on post-consultation length of stay. Such an investigation would require prospective recording of expected length of stay which we plan for future study.
In conclusion, scheduled interprofessional rounds between hospitalists and geriatric specialists facilitate proactive patient-centered use of scarce geriatric services.
Supplementary Material
Flow of data (hospitalizations) from 2 years of administrative hospital data into four groups by time and intervention versus control in order to conduct a differences-in-differences study on change over time of outcomes.
Impact statement:
We certify that this work is novel. This research offers an impactful intervention in the acute hospital setting that improves the provision and timing of inpatient geriatric consultation services.
ACKNOWLEDGEMENT
Sponsor’s Role: The funder of this work was Blue Cross Blue Shield of Michigan (PI Khateeb), who did not have any role in the interpretation of the results or manuscript preparation.
This research was presented, in part, at the 2016 Annual Scientific Research Meeting in Long Beach, California. This research was supported through Blue Cross Blue Shield of Michigan Foundation (BCBSM- 15-PAF07639 01/2016–3/2017).
Footnotes
Conflict of Interest: The authors have no conflicts of interest to declare.
REFERENCES
- 1.Institute of Medicine. Retooling for an Aging America: Building the Health Care Workforce. Washington DC2008. [PubMed] [Google Scholar]
- 2.Fox MT, Persaud M, Maimets I, et al. Effectiveness of Acute Geriatric Unit Care Using Acute Care for Elders Components: A Systematic Review and Meta-Analysis. Journal of the American Geriatrics Society. 2012;60(12):2237–2245. doi: 10.1111/jgs.12028. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Landefeld CS, Palmer RM, Kresevic DM, Fortinsky RH, Kowal J. A Randomized Trial of Care in a Hospital Medical Unit Especially Designed to Improve the Functional Outcomes of Acutely Ill Older Patients. New England Journal of Medicine. 1995;332(20):1338–1344. doi: 10.1056/nejm199505183322006. [DOI] [PubMed] [Google Scholar]
- 4.Counsell SR, Holder CM, Liebenauer LL, et al. Effects of a multicomponent intervention on functional outcomes and process of care in hospitalized older patients: a randomized controlled trial of Acute Care for Elders (ACE) in a community hospital. J Am Geriatr Soc. 2000;48(12):1572–1581. [DOI] [PubMed] [Google Scholar]
- 5.Hogan DB, Fox RA. A prospective controlled trial of a geriatric consultation team in an acute-care hospital. Age Ageing. 1990;19(2):107–113. [DOI] [PubMed] [Google Scholar]
- 6.Hogan DB, Fox RA, Badley BW, Mann OE. Effect of a geriatric consultation service on management of patients in an acute care hospital. CMAJ: Canadian Medical Association Journal. 1987;136(7):713–717. http://www.ncbi.nlm.nih.gov/pmc/articles/PMC1491925/. [PMC free article] [PubMed] [Google Scholar]
- 7.Marcantonio ER, Flacker JM, Wright RJ, Resnick NM. Reducing delirium after hip fracture: a randomized trial. J Am Geriatr Soc. 2001;49(5):516–522. [DOI] [PubMed] [Google Scholar]
- 8.Tillou A, Kelley-Quon L, Burruss S, et al. Long-term postinjury functional recovery: outcomes of geriatric consultation. JAMA Surg. 2014;149(1):83–89. doi: 10.1001/jamasurg.2013.4244. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Deschodt M, Flamaing J, Haentjens P, Boonen S, Milisen K. Impact of geriatric consultation teams on clinical outcome in acute hospitals: a systematic review and meta-analysis. BMC Med. 2013;11:48. doi: 10.1186/1741-7015-11-48. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Khateeb R, Puelle MR, Firn J, Saul D, Chang R, & Min L (2018). Interprofessional Rounds Improve Timing of Appropriate Palliative Care Consultation on a Hospitalist Service. Am J Med Qual, 2018. Apr. Epub ahead of print. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Deyo RA, Cherkin DC, Ciol MA. Adapting a clinical comorbidity index for use with ICD-9-CM administrative databases. J Clin Epidemiol. 1992;45(6):613–619. [DOI] [PubMed] [Google Scholar]
- 12.Karaca-Mandic P, Norton EC, Dowd B. Interaction Terms in Nonlinear Models. Health Services Research. 2012;47(1 Pt 1):255–274. doi: 10.1111/j.1475-6773.2011.01314.x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Akaike H A new look at the statistical model identification. IEEE Trans Autom Control. 1974;19(6):716–723. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Flow of data (hospitalizations) from 2 years of administrative hospital data into four groups by time and intervention versus control in order to conduct a differences-in-differences study on change over time of outcomes.


