Abstract
Background
Increasing health costs, demand and patient multimorbidity challenge the sustainability of healthcare systems. These challenges persist and have been amplified by the global pandemic.
Objectives
We aimed to develop an understanding of how the sustainable performance of healthcare systems (SPHS) has been conceptualised, defined and measured.
Design
Scoping review of peer-reviewed articles and editorials published from database inception to February 2021.
Data sources
PubMed and Ovid Medline, and snowballing techniques.
Eligibility criteria
We included articles that discussed key focus concepts of SPHS: (1) definitions, (2) measurement, (3) identified challenges, (4) identified solutions for improvement and (5) scaling successful solutions to maintain SPHS.
Data extraction and synthesis
After title/abstract screening, full-text articles were reviewed, and relevant information extracted and synthesised under the five focus concepts.
Results
Of 142 included articles, 38 (27%) provided a definition of SPHS. Definitions were based mainly on financial sustainability, however, SPHS was also more broadly conceptualised and included acceptability to patients and workforce, resilience through adaptation, and rapid absorption of evidence and innovations. Measures of SPHS were also predominantly financial, but recent articles proposed composite measures that accounted for financial, social and health outcomes. Challenges to achieving SPHS included the increasingly complex patient populations, limited integration because of entrenched fragmented systems and siloed professional groups, and the ongoing translational gaps in evidence-to-practice and policy-to-practice. Improvement strategies for SPHS included developing appropriate workplace cultures, direct community and consumer involvement, and adoption of evidence-based practice and technologies. There was also a strong identified need for long-term monitoring and evaluations to support adaptation of healthcare systems and to anticipate changing needs where possible.
Conclusions
To implement lasting change and to respond to new challenges, we need context-relevant definitions and frameworks, and robust, flexible, and feasible measures to support the long-term sustainability and performance of healthcare systems.
Keywords: PUBLIC HEALTH, Health policy, HEALTH SERVICES ADMINISTRATION & MANAGEMENT
Strengths and limitations of this study.
This scoping review addresses a knowledge gap by providing a comprehensive synthesis of the literature including definitions, measurement, challenges, solutions for improvement and scaling up successful solutions to maintain sustainable performance of healthcare systems (SPHS).
The review methodology was guided by the Preferred Reporting Items for Systematic review and Meta-Analysis extension for Scoping Reviews statement, and we searched multiple databases and used complementary snowballing techniques to increase comprehensiveness.
The use of the Hawker and Authority Accuracy Coverage Objectivity Date Significance quality appraisal tools provided an assessment of the quality of literature on the SPHS.
Our review is limited in scope to countries with health systems of relevance to Australia, and this limits the generalisability of our results to low-income or middle-income countries.
Background
Globally, healthcare spending is tracking above and beyond economic growth.1 Challenges facing healthcare systems include an ageing population and subsequent rise of chronic diseases and multimorbidity2 3 and increasingly expensive new medical technologies.3 4 It is estimated that approximately 30% of care delivered by healthcare systems is low-value, attributable mainly to administrative overheads, bureaucracy, overdiagnosis, overtreatment or other factors.5 Systems lacking coordination and integration across clinical disciplines and healthcare sectors also result in wasteful spending through both care duplication and omission of needed care.6 If healthcare spending follows current trajectories, governments suggest that healthcare systems will begin to become unaffordable.3 This leads us to the question: ‘what is the current thinking about interventions and initiatives to make healthcare systems more sustainable?’. Understanding how healthcare system sustainability is conceptualised underpins the implementation and evaluation of system-wide interventions that aim to improve performance. Although literature about the sustainability of individual innovations and improvement programmes is growing,7 the broad question of whole-of-system sustainability is rarely studied.
Sustainability itself has remained an ambiguous topic in the literature. Sustainability suggests that healthcare systems should be built to last, and able to adapt and endure, ensuring that resources are expended efficiently and responsibly to maintain or improve individual and population health and well-being.8 To be sustainable, a healthcare system must adequately deliver across financial, social and environmental concerns.4 This triple bottom-line is difficult to achieve consistently over time. For example, sustainable health services may need additional short-term investments to be financially beneficial in the long term.1
The healthcare system is defined as one that delivers care to those who need it across many different settings. It includes key components: capacity— including physical, capital and human assets; organisational structure, both formal and informal; finances—including mechanisms for funding allocations, ownership and solvency; patients or clients and their characteristics and needs; and care processes and infrastructure.9
Healthcare system sustainability is difficult to measure in practice and requires ongoing long-term monitoring and evaluation of appropriate indicators. One potential way to conceptualise and operationalise sustainability is an assessment of the sustainable performance of healthcare systems (SPHS). Although past reviews have addressed the sustainability of improvement programmes and policies in the healthcare system,7 10 11 they did not specifically address how SPHS is conceptualised in the medical literature. As a response, this study was designed using a systems science lens to fill this gap in knowledge by reviewing publications that report on or discuss the SPHS.
Objectives
This scoping review of health and medical literature aims to develop an understanding of how SPHS has been conceptualised, defined, and measured, and to scope the identified challenges and potential solutions to achieving and maintaining SPHS.
Methods
Study design
In keeping with scoping review methodology,12 our inclusion criteria were broad, and our search was comprehensive to capture the state of knowledge about SPHS. We included literature reviews, primary empirical articles (including qualitative, quantitative and mixed-methods studies), case studies, opinion pieces and editorials published in English from database inception to February 2021. To be included, studies had to report on, or discuss in detail, aspects of healthcare systems sustainability, resilience or performance improvement, and could cover improvements in cost-effectiveness, affordability, safety, quality, equity or access, while creating or realising value (table 1). Only articles that addressed the research objectives and provided insights into current knowledge of sustainability in healthcare delivery systems were included. Articles on environmental sustainability; those investigating discrete improvement programmes implemented in specific healthcare settings including studies on specific diseases or programmes (eg, studies on vaccination programmes for a specific disease); and studies with a specific focus on COVID-19 were out of scope, as we applied a system-wide lens rather than a disease-specific focus (table 1).
Table 1.
Inclusion and exclusion criteria
| Inclusion criteria* | Exclusion criteria |
|
|
*To be eligible for inclusion, articles needed to demonstrate one or more of the inclusion criteria.
SPHS, sustainable performance of healthcare systems.
Information sources
In consultation with an experienced university medical librarian, we developed a search strategy using key words and MeSH terms and conducted an advanced search of PubMed and Ovid Medline (online supplemental file 1). Additional relevant articles were identified by hand searching reference lists of included articles (snowballing).
bmjopen-2021-059207supp001.pdf (46.6KB, pdf)
Study selection
Guided by the Preferred Reporting Items for Systematic review and Meta-Analysis extension for Scoping Reviews (PRISMA-ScR) statement,13 14 and the methodological framework for scoping reviews,12 screening of the article titles and abstracts was conducted by four reviewers (JHolt, JHerkes, GD and EM) using the predetermined inclusion and exclusion criteria (table 1). Reviewers screened a 5% sample of the titles and abstracts while applying the inclusion and exclusion criteria and the team then met to discuss any discrepancies, before screening continued. The full-text review was then conducted by a second reviewer team (JHerkes, YZ, GD, IM and GL) in consultation with JHolt and EM. Discrepancies were resolved in team meetings in consultation with JB as arbitrator.
Quality assessment of individual studies
To understand the scope of the quality of included articles, Hawker et al’s Quality Assessment Tool was applied as it enables quality assessment among many different article types including quantitative, qualitative or mixed-methods empirical research studies or literature reviews.15 The Quality Assessment Tool contains nine categories (abstract and title; introduction and aims; method and data; sampling; data analysis; ethics and bias; results; transferability or generalisability; and implications and usefulness) and a total quality score can be calculated (maximum score=36), where higher scores denote higher quality.15–17 For quality assessment of opinion or commentary pieces, the Authority Accuracy Coverage Objectivity Date Significance (AACODS) checklist was used.12 17
Data extraction
Characteristics of included articles, year of publication, country of origin and article type were tabulated. A purpose-designed Excel spreadsheet was used to extract relevant details from each article. The Excel spreadsheet was piloted by three reviewers on five articles and adjusted as needed.
Patient and public involvement
No patients or public were involved.
Results
Study selection
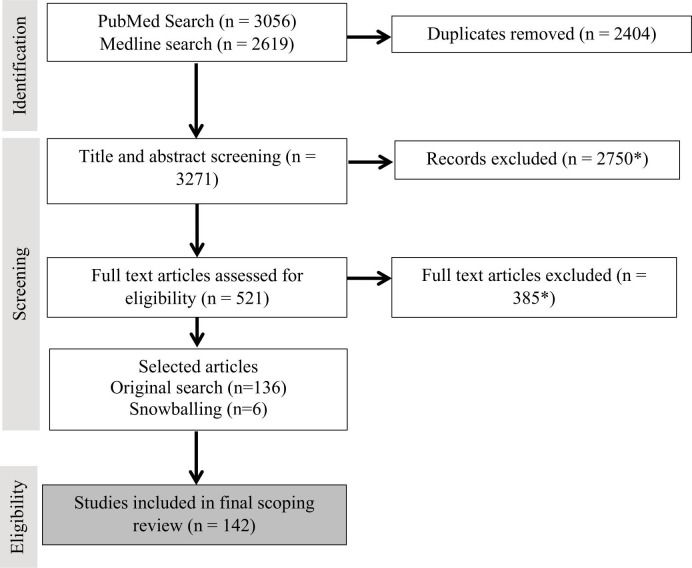
Of 5675 articles identified in the database searches, 2404 were duplicates, leaving 3271 articles. Undertaking independent title and abstract screening of 5% of articles, two reviewers achieved an acceptable level of agreement (kappa=0.6).18 A further 2750 articles were excluded, leaving 521 articles for full-text review. A substantial level of agreement was achieved on review of 5% of full-text articles undertaken independently by four reviewers JHerkes, YZ, GD and IM; (kappa=0.7).18 After full-text review, 136 articles were included. Eighty-three additional articles were identified from snowballing, and six met the inclusion criteria, for a total of 142 articles included for data extraction (figure 1). See online supplemental file 2 for further details.
Figure 1.
Preferred Reporting Items for Systematic Reviews and Meta-Analyses flow diagram summarising the review and reasons for article exclusion. *Full text articles and snowballed articles excluded for the following reasons. Note that some articles were excluded for multiple reasons. Reasons for article exclusion are below.
bmjopen-2021-059207supp002.pdf (526KB, pdf)
| Reason | Excluded at title/abstract screening (N) | Excluded at full text review (N) |
| Disaster or emergency | 199 | 3 |
| Foreign aid, equity or community healthcare | 598 | 20 |
| Occupational health and safety | 69 | 2 |
| Environmental sustainability | 89 | 5 |
| Not relevant to Australia, for example, low-resource setting | 730 | 82 |
| Not about systems, for example, single disease or programme | 1291 | 109 |
| Preventative, for example, regarding vaccination or nutrition | 277 | 18 |
| Not relating to healthcare delivery, for example, regarding animal care or food safety | 46 | 0 |
| Regarding physiology/pharmacology | 44 | 0 |
| Does not in another way define, measure, identify challenges, opportunities for improvement or scale up of sustainability in the healthcare system | 398 | 166 |
| Other, for example, article not written in English, full text not available | 4 | 95 |
Study characteristics
Of the included articles, 18 were review articles (either systematic or narrative), 82 were editorial or opinion pieces, 37 were primary empirical studies and 5 were a brief narrative review combined with an empirical study (classified as empirical for simplicity). Empirical studies used a wide variety of data collection techniques and included qualitative analysis of interviews,19 survey results,20 21 analysis of hospital data records22 23 and economic analysis.24–28 The included articles described studies that covered various geographic locations, most commonly Canada (n=22), the USA (n=22), Australia (n=23, including two which involved Australia and New Zealand), the UK (n=6), the Netherlands (n=2) and one each from the following countries: Austria, Italy, Northern Ireland, Malaysia, Malta, New Zealand, Oman, the Philippines, Portugal, Scotland and Spain. The remainder of studies referred to geographical regions such as the European Union, or to multiple nations, for example one included the USA, the UK and Australia29 and another included Australia, Ireland, Austria and Denmark.30
The data extraction sheet included the citation, study aims, study design, themes addressed and additional relevant information about SPHS. Details of the 142 included articles are summarised in online supplemental file 2. Of the 142, most identified challenges (n=94, 66%) and proposed ways to improve SPHS (n=89, 62%) while fewer discussed measuring SPHS (n=48, 34%), or sustaining and scaling change (n=47, 33%) and fewer still provided any definition of SPHS (n=38, 27%).
Quality of included studies
Forty-three empirical studies scored 25–34 points on the Hawker’s Quality Assessment Tool,15 and 29 were of high quality, 13 moderate quality and 1 borderline low quality.16 None were excluded due to low quality (online supplemental file 3). The quality of editorial and opinion pieces (n=99) was analysed according to the AACODS criteria, and 72 articles ranked ‘yes’ for all criteria indicating high quality (online supplemental file 3).
bmjopen-2021-059207supp003.pdf (462.3KB, pdf)
Defining SPHS
Definitions of SPHS were provided by 38 publications including 25 opinion pieces, 7 review articles and 6 empirical studies (table 2). The definitions fell into three broad groupings: (1) fiscal sustainability, (2) human resource sustainability and acceptance of change by stakeholders and (3) system adaptability and improvement (table 2). Definitions focused on continual improvement,29 and embeddedness of changes into the healthcare system in the long term.31–33
Table 2.
Definitions of sustainable performance of healthcare systems
| Definition | Exemplar quotes | Relevant references | ||
| Empirical articles | Editorials or opinion pieces | Reviews | ||
| Fiscal sustainability | ‘The WHO considers fiscal sustainability as a requirement, rather than an objective, of health financing policy. Sustainability of healthcare financing therefore cannot be interpreted as a reduction of healthcare costs, but rather as a predictable growth or control of health expenditures’.24 | 35 36 64 127 | 24 32–34 37 39 56 | 40 41 104 127 128 |
| Human resource sustainability and acceptability to stakeholders | ‘It has been increasingly recognised that getting HR policy and management “right” has to be at the core of any sustainable solution to health system performance’32 129 ‘A sustainable health system also has acceptability to key constituents, including patients and health professionals’.33 |
64 | 32–34 38 56 67 83 90 129–132 | 31 104 |
| Adaptability and improvement over time to create a future-focused intervention | ‘A sustainable health system … [has] adaptability, because health and health care needs are not static (i.e., a health system must respond adaptively to new diseases, changing demographics, scientific discoveries, and dynamic technologies in order to remain viable)’.33 ‘Ensuring that sufficient resources are available over the long term to provide timely access to quality services that address Canadians’ evolving health needs’.133 |
36 43 | 4 33 39 42 56 67 78 83 89 98 108 131–135 | 31 49 88 104 128 |
Several articles defined SPHS in terms of fiscal sustainability.24 32–37 Examples included discussions of sustainability of rural primary care services in the face of ongoing policy change to reimbursement and practice incentives,36 adoption of new funding models to ensure availability of medicines24 and hospital capital investments to improve patient access to care.35 Articles also discussed the importance of balancing financial interests with social and ecological interests.38 Several papers conceptualised SPHS as the continuation of programmes after the cessation of external program-specific funding.39–41
Four articles42–45 discussed SPHS through the lens of a learning healthcare system, a system in which ‘science, informatics, incentives, and culture are aligned for continuous improvement and innovation’.46 These articles focused predominantly on using data and evidence to support system adaptability and improvement over time.
Measuring SPHS
The measurement of SPHS was addressed through theoretical discussions across the 24 editorials and 7 review articles, and by proposing, developing or applying frameworks or indicators in 17 empirical studies (table 3). These frameworks and indicators were heterogeneous and included financial, social and healthcare outcomes47 with some articles highlighting the limitations of widely used financial metrics.34 48 Although heterogeneous,40 measures were undertaken at three broad outcome levels: (1) individual (eg, continued health benefits for patients or healthcare providers); (2) organisational (eg, continuation of innovations, hospital-level fiscal improvements) or (3) community (eg, continued use of programmes, services or healthcare interventions).
Table 3.
Summary of established and novel frameworks suggested for measuring SPHS
| Established framework name | Rationale for use |
| Organisational Change Model (OCM) | To measure the success of sustained organisational change, according to faculty member survey respondents51 |
| Analysis of hospital records (eg, payroll records) | Measuring staff turnover, workforce supply and financial sustainability22 26 |
| Evaluation of health networks | To evaluate the effectiveness and sustainability of health networks136 |
| Novel framework name | Rationale for development |
| Q* Scale | To measure performance at the hospital level50 |
| Dynamic Sustainability Framework (DSF) | To investigate the fit between the intervention, the practice setting, and the ecological system39 To improve measurement of SPHS beyond patient outcomes only40 |
| Resilience Indicator | To highlight the systemic relevance of primary care network systems to quantify healthcare resilience54 |
| eMergy (embodied energy) Sustainability Index | To address the lack of qualitative indicators for sustainability49 |
| Future Health Index (FHI) | To identify preparedness of countries to build sustainable health systems55 |
| Health Care Sustainability Framework (HCSF) | To measure the relationships between political and fiscal sustainability of an intervention52 |
| Responsible Innovations for Health (RIH) Framework | To identify interventions that suitably address five domains (population health, healthcare system, economic, organisational, environmental)53 |
| Research Lifecycle Framework | To enhance the impact of the Learning Health System by operationalising research innovations into clinical practice45 |
| Value Of Diagnostic Information (VODI) Framework | To outline the multidimensional benefits and potential of healthcare diagnostics114 |
*SPHS, sustainable performance of healthcare systems.
A variety of new SPHS measures were proposed, developed, modified or tested in research environments20 22 45 49–51 to address current deficits in available measures (table 3). For example, the Q*Scale was designed to combine data on caseload, patient satisfaction and physician aptitude, such that changes in hospital performance could be more effectively monitored.50 In contrast, the Dynamic Sustainability Framework seeks to investigate the fit between the intervention, practice settings, contexts and cultures, healthcare policies, and the broader ecology within which healthcare systems operate, including sociopolitical systems.39 Similarly, the Healthcare Sustainability Framework (HCSF) and the Responsible Innovations for Health framework, recognise the importance of accounting for the needs and trends of the population, workforce and financial constraints.52 53 Alternative models utilising a scoring system (eg, using the Resilience Indicator) were based on data-driven simulation modelling,54 or theoretical composite indicators of the value of healthcare systems.54 55
Identified challenges to SPHS
Ninety-four articles, including 60 editorials, 22 empirical studies and 12 reviews, identified challenges to SPHS across three main themes: (1) increasingly complex patient populations; (2) ongoing gaps between evidence, policy and practice and (3) concerns of system fragmentation and need for integration for a more streamlined adoption and sustainment of interventions.
Increasingly complex patient populations,3 23 54 56–63 including patients with multi-morbidity21 54 58 59 61 64–66 and greater demand for effective aged care, under already strained healthcare budgets3 27 56 67–73 were frequently discussed. The increasing demands and expectations of patients for healthcare of the highest quality challenges healthcare systems to meet this demand.4 21 58 59 61 74 75
The gaps between evidence, policy and practice40 76 77 continue to threaten SPHS as does limited investment in building workforce capacity and stakeholder involvement.30 43 The challenge of increasing public scrutiny and the need to balance financial, environmental and social sustainability were also recognised.28 38 78–80
The fragmented nature of healthcare systems including power imbalances among the health professions, and resistance to changes in the scope of practice was reported to limit team approaches to care.81 82 Siloed care delivery models can become misaligned with the complexity of the healthcare system and the complexity of patient needs.52 83–85 Other publications reported lack of collaboration between public and private hospitals72 86 and widening gaps in care quality in rural/remote regions due to limited resources.23 36 72 87 Poor integration of primary care with the broader healthcare system was also seen as challenging SPHS.60 88
Opportunities for improvement of SPHS
To address the challenges posed requires more than a one-time simple ‘fix’. Continued adaptation in response to local contexts, and ongoing monitoring and evaluation are required to support the sustainment of effective solutions and to anticipate future needs and solutions.51 Twelve review articles, 19 empirical articles and 56 editorials discussed opportunities to improve SPHS.
Greater strategic investment in the system,34 48 69 70 89 including funding novel interventions,26 40 80 90 91 and capacity building programmes for staff30 92 were advocated. Workplace culture in healthcare was identified as an important factor for SPHS. The importance of physician well-being was highlighted,44 76 93 94 and was strongly linked with organisational culture.17 The importance of mentorship, teaching and leadership were also highlighted as enablers of organisational improvements.19 43 75 76 Building healthcare system cultures that support medical graduates was viewed as crucial.38 94–96 Promoting incentives for generalist doctors to practice rurally was thought to address the current geographical gap in access to healthcare.44 87 95–97
The promotion of desired attitudes, values and ideals of healthcare organisations was also recognised for achieving SPHS. Specifically, the value of patient-centred care and evidence-based medicine,30 44 58 63 65 97–99 and collaboration between and within healthcare facilities and disciplines was highlighted as important for SPHS.42 64 86 99–102 Support by management that values the workforce, uses robust data-driven hospital management systems, and accessible, shared electronic medical record systems was also acknowledged as vital.74 103
The importance of political stability and bridging the jurisdictional-federal divide in federated healthcare systems (such as in the USA, Canada and Australia) was important for effective unified healthcare system functioning.24 69 70 104–106 It is not only organisational culture in healthcare,107 but the broader organisation, governance and regulation of the healthcare system that are important for SPHS.108–110
Community involvement is an important factor that bolsters capacity to implement and sustain change.103 Empowering patients to care for their own health, and building confidence among caregivers to deliver some aspects of care, reduces burden on the healthcare system.58 Community involvement via Community Based Participatory Research bolstered equity and improved outcomes of care111 and responding to recommendations from citizen panels also improved SPHS.73 102 112
As technology advances, so does the ability to harness it to promote the sustainability of healthcare systems.33 For example, point-of-care electronic prompts were used in one study of hospital surgical wards to decrease rates of hospital-acquired infections.113 Embedding artificial intelligence and big data analytics hold promise to support efficient and effective service delivery to improve SPHS.83 Other studies have suggested greater adoption of telemedicine to reduce travel time and costs4 as complementary support to patients,91 to improve diagnostics,114 and as a platform to promote prevention of illness,23 as contributing to SPHS.
Sustaining and scaling change in SPHS
Forty-seven articles addressed this theme, including 9 reviews, 11 empirical articles and 27 editorials. As interventions are often implemented with limited and/or short-term (2–3 years) evaluation plans, demonstrating SPHS is often elusive.40 Robust evaluations using relevant SPHS indicators embedded alongside implementation, from the outset, to support adaptations and decisions about ongoing investments were advocated.104 115 One article proposed that federal funding agencies should perceive funding implementations of health innovations as ongoing strategic investments rather than time-limited projects.42
The importance of accepting changes or adaptations to proposed interventions were also highlighted.116 117 For example, Greenhalgh et al117 reported on a 3-year case study follow-up of a healthcare system transformation and found that adaptations of the intervention to local contexts was important for sustainment of the intervention.
A recurring sentiment in the articles reviewed was the importance of support for the continuation of interventions from leaders and stakeholders.57 98 103 107 118 119 Leaders and managers have a clear role in supporting staff throughout the processes of reforms and changes, by providing opportunities for codesign, education including e-learning, and building peer networks89 120 while creating open communication to involve front-line staff in planning and implementation.103 121 For example, one article suggested that pharmacists should be involved in developing hospital discharge procedures to improve medication safety and adherence.122 In more recent articles, policy-makers and political leaders are highlighted as important change agents, as long as they work in concert with front-line health staff.104 119 123
Transparent healthcare policies and algorithms for equitable distribution of healthcare funds were advocated, and particularly prioritised by rural areas.36 48 Beyond the government, communities and multi-sectorial partners,56 collaborations among hospitals, medical schools and physicians were also highlighted as vital for SPHS.47
Although publications in our review predominantly urged for the sustainability of innovations, recent literature also highlights the need for discontinuation or redesign of programmes that have become ineffective or irrelevant over time.4 39 117 This is important to achieve sustainability as it ensures that value is maintained in the healthcare system.124
Discussion
Definitions of SPHS were rarely offered, with only 27% of included articles providing any definition of SPHS while referring to the concept of SPHS. When definitions were provided, they mainly centred on financial and workforce sustainability, and a variety of concepts related to adaptability, improvement and innovation for the future. The lack of definitions and variability in definitions creates significant limitations for the interpretation of the current body of literature on SPHS. As a first step to address this limitation, we would urge authors discussing SPHS to provide a definition that is relevant to their context. Furthermore, there were interesting contrasts in the boundaries adopted to describe the ‘healthcare system’ in the included papers which has also been identified by others.125 For example, some studies measured SPHS at a single hospital level,50 whereas others addressed it at a national system level,126 making comparisons across studies difficult. In the future, as evidence about SPHS develops it may be possible to create nuanced measures, definitions, and approaches to SPHS as applied to different healthcare system levels and contexts.
The long-standing approach to measure SPHS in terms of financial outcomes is increasingly becoming more sophisticated through the development of newer more nuanced frameworks and indicators that account for health and societal benefits while factoring in the complex and dynamic nature of healthcare systems. Although new frameworks and measures, for example, the Future Health Index,55 the Q*Scale50 and the Resilience Indicator54 have been proposed, the evidence for the practical application of such frameworks and measures in the real world was limited.
The most common opportunities for improving SPHS related to building supportive and functional workplace and organisational cultures that promote collaboration, transparency, patient-centredness and community participation. The adoption of technological advances including greater use of linked up information technology platforms to provide intelligence about aspects of SPHS were also discussed in the literature.4 23 33 91 113 Importantly, policy and political stability over time was also recognised as a supportive factor for SPHS, especially when implementing innovations and interventions that require longer-term horizons to demonstrate their impacts on SPHS.24 40 69 70 77 104–106 This aligns with findings from a recent systematic review that specifically focused on the sustainability of health improvement programmes.44
The increasing adoption of pragmatic implementation trials in healthcare research is an important advance to support effectiveness testing in real-life situations rather than in contrived randomised controlled trials that are difficult to implement at scale in real-world settings to meet the needs of changing populations.46 121
Table 4 provides a summary of the current evidence about SPHS under five headings: defining sustainability; measuring it; associated challenges of realising sustainable performance; identifying opportunities for improvement and creating, sustaining and scaling SPHS. This provides an important starting point for future research in the field.
Table 4.
Summary of key findings under the five SPHS focus areas analysed in this review
| Criteria | Explanation | Key points from included articles |
| Defining sustainability | What do we mean by SPHS? |
|
| Measuring | How do we measure SPHS? |
|
| Associated challenges | What challenges are associated with SPHS? |
|
| Opportunities for improvement | What helps improve SPHS? |
|
| Sustaining and scaling | What initiatives for have been used to improve and maintain to SPHS (or value)? |
|
SPHS, sustainable performance of healthcare systems.
Strengths and limitations
Methodological strengths of the current review include the use of the PRISMA-ScR statement to guide the review, including searching multiple databases and using snowballing techniques to increase comprehensiveness. Although formal quality appraisal is not recommended for scoping reviews, we felt it was important to also understand the scope of the quality of articles being published in addition to understanding their content and findings about SPHS.
As described earlier, the heterogenous nature of the current literature and limited use of definitions and frameworks made synthesis challenging. Our choice to limit the current review to studies reporting on SPHS in high-income countries further limits generalisability to other settings including in low-income and middle-income countries (LMICs).
Future research directions
This article summarises the current scope of the literature on SPHS and provides an important starting point for future research. Although new SPHS measures and frameworks that include factors other than financial inputs and outputs have been proposed, their usefulness needs to be evaluated in the real-world healthcare ecosystem in the future. Taking a broad system-wide lens, our focus was on the SPHS in healthcare delivery settings and did not specifically consider individual programmes for specific diseases, conditions or settings. In addition, the role of preventative care and broader public health prevention measures such as vaccination programmes, should be a focus for future research. Research on the specific effect of the COVID-19 pandemic on SPHS is warranted to inform future responses to similar broad-ranging global threats to SPHS.113 115 Understanding the scope of SPHS in LMICs is important for the future development of SPHS and future research is needed to summarise current knowledge, interventions, programmes and measures of SPHS in these settings.
Conclusion
There is broad agreement that the sustainability of healthcare systems and their performance levels are increasingly being challenged. Our review confirms that the concept of SPHS is important and is frequently discussed in the health and medical literature. The field of SPHS is expanding with recent publications defining SPHS in terms other than the traditional financial measures. This places more emphasis on acceptability of the system to patients, healthcare providers and other stakeholders, adaptation and resilience, and sufficient nimbleness to absorb new evidence and innovations to support continuous improvements.
It is unlikely that we will, nor should we, settle on a single definition of SPHS. We would favour definitions that are robust but flexible to ensure their utility in the many and varied healthcare system contexts, however, authors and editors should strive to ensure that a definition is provided in any discussions of SPHS. We need sophisticated yet practical indicators of SPHS that capture sustainability beyond the traditional financial measures. Such measures have been proposed in the research literature, but their utility needs to be tested in real-world settings. The current literature suggests that SPHS is improved by strengthening workplace cultures, continuous workforce development, direct health consumer and community involvement, and swift adoption and embedding of new evidence and technologies that are proven to have an advantage over current practice.
Supplementary Material
Acknowledgments
We gratefully acknowledge Kelly Nguyen for administrative and logistical support.
Footnotes
Twitter: @YvonneZurynski
Contributors: JB conceptualised the study and led the team’s work. EM, JHerkes, JHolt and YZ developed the search strategy. EM, JHerkes, JHolt, GL, GD and YZ conducted the abstract review, and JHerkes, GD, GL, IM and YZ full-text review and data extraction, with JB acting as arbitrator when needed. JHerkes, IM and GD conducted the quality assessment. YZ and JHerkes drafted the manuscript with input from GD and NKH, and all authors contributed their comments and approved of the final version of the manuscript. JB is the guarantor for this study.
Funding: This work was supported by the NHMRC Partnership Centre for Health System Sustainability (Grant ID 9100002) and NHMRC Investigator Grant APP1176620.
Competing interests: None declared.
Patient and public involvement: Patients and/or the public were not involved in the design, or conduct, or reporting, or dissemination plans of this research.
Provenance and peer review: Not commissioned; externally peer reviewed.
Supplemental material: This content has been supplied by the author(s). It has not been vetted by BMJ Publishing Group Limited (BMJ) and may not have been peer-reviewed. Any opinions or recommendations discussed are solely those of the author(s) and are not endorsed by BMJ. BMJ disclaims all liability and responsibility arising from any reliance placed on the content. Where the content includes any translated material, BMJ does not warrant the accuracy and reliability of the translations (including but not limited to local regulations, clinical guidelines, terminology, drug names and drug dosages), and is not responsible for any error and/or omissions arising from translation and adaptation or otherwise.
Data availability statement
All data relevant to the study are included in the article or uploaded as supplementary information.
Ethics statements
Patient consent for publication
Not applicable.
Ethics approval
This study does not involve human participants.
References
- 1.OECD . Fiscal sustainability of health systems: bridging health and finance perspectives. Paris, France: OECD Publishing, 2015. [Google Scholar]
- 2.GBD 2015 DALYs and HALE Collaborators . Global, regional, and national disability-adjusted life-years (DALYs) for 315 diseases and injuries and healthy life expectancy (HALE), 1990-2015: a systematic analysis for the global burden of disease study 2015. Lancet 2016;388:1603–58. 10.1016/S0140-6736(16)31460-X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Amalberti R, Nicklin W, Braithwaite J. Preparing National health systems to cope with the impending tsunami of ageing and its associated complexities: towards more sustainable health care. Int J Qual Health Care 2016;28:412–4. 10.1093/intqhc/mzw021 [DOI] [PubMed] [Google Scholar]
- 4.Coiera E, Hovenga EJS. Building a sustainable health system. Yearb Med Inform 2007:11–18. [PubMed] [Google Scholar]
- 5.Fisher ES, Bynum JP, Skinner JS. Slowing the growth of health care costs--lessons from regional variation. N Engl J Med 2009;360:849–52. 10.1056/NEJMp0809794 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Zhi M, Ding EL, Theisen-Toupal J, et al. The landscape of inappropriate laboratory testing: a 15-year meta-analysis. PLoS One 2013;8:e78962-e. 10.1371/journal.pone.0078962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Braithwaite J, Ludlow K, Testa L, et al. Built to last? the sustainability of healthcare system improvements, programmes and interventions: a systematic integrative review. BMJ Open 2020;10:e036453. 10.1136/bmjopen-2019-036453 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Australian Institute of Health Innovation . Purpose, NHMRC Partnership Centre for Health System Sustainability, 2017. Available: https://www.healthsystemsustainability.com.au/about-us-2/purpose-of-nhmrc-partnership-centres/
- 9.Piña IL, Cohen PD, Larson DB, et al. A framework for describing health care delivery organizations and systems. Am J Public Health 2015;105:670–9. 10.2105/AJPH.2014.301926 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Lennox L, Maher L, Reed J. Navigating the sustainability landscape: a systematic review of sustainability approaches in healthcare. Implement Sci 2018;13:27. 10.1186/s13012-017-0707-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Stirman SW, Kimberly J, Cook N, et al. The sustainability of new programs and innovations: a review of the empirical literature and recommendations for future research. Implement Sci 2012;7:17. 10.1186/1748-5908-7-17 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Arksey H, O'Malley L, O’Malley LO. Scoping studies: towards a methodological framework. Int J Soc Res Methodol 2005;8:19–32. 10.1080/1364557032000119616 [DOI] [Google Scholar]
- 13.Moher D, Liberati A, Tetzlaff J, et al. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med 2009;6:e1000097. 10.1371/journal.pmed.1000097 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Shamseer L, Moher D, Clarke M, et al. Preferred reporting items for systematic review and meta-analysis protocols (PRISMA-P) 2015: elaboration and explanation. BMJ 2015;349:g7647. 10.1136/bmj.g7647 [DOI] [PubMed] [Google Scholar]
- 15.Hawker S, Payne S, Kerr C, et al. Appraising the evidence: reviewing disparate data systematically. Qual Health Res 2002;12:1284–99. 10.1177/1049732302238251 [DOI] [PubMed] [Google Scholar]
- 16.Lorenc T, Pettigrew M, Whitehead M. Appendix 5: quality assessment for the systematic review of qualitative evidence. In: Research PH, ed. Crime, fear of crime and mental health: synthesis of theory and systematic reviews of interventions and qualitative evidence. 2.2. Southampton, United Kingdom: NIHR Journals Library, 2014. [PubMed] [Google Scholar]
- 17.Braithwaite J, Herkes J, Ludlow K, et al. Association between organisational and workplace cultures, and patient outcomes: systematic review. BMJ Open 2017;7:e017708. 10.1136/bmjopen-2017-017708 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Landis JR, Koch GG. The measurement of observer agreement for categorical data. Biometrics 1977;33:159–74. 10.2307/2529310 [DOI] [PubMed] [Google Scholar]
- 19.Stockdale SE, Zuchowski J, Rubenstein LV, et al. Fostering evidence-based quality improvement for patient-centered medical homes: initiating local quality councils to transform primary care. Health Care Manage Rev 2018;43:168–80. 10.1097/HMR.0000000000000138 [DOI] [PubMed] [Google Scholar]
- 20.Lizarondo L, Turnbull C, Kroon T, et al. Allied health: integral to transforming health. Aust Health Rev 2016;40:194–204. 10.1071/AH15044 [DOI] [PubMed] [Google Scholar]
- 21.Robertson J, Walkom EJ, Henry DA. Health systems and sustainability: doctors and consumers differ on threats and solutions. PLoS One 2011;6:e19222. 10.1371/journal.pone.0019222 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Fox LA, Walsh KE, Schainker EG. The creation of a pediatric hospital medicine dashboard: performance assessment for improvement. Hosp Pediatr 2016;6:412–9. 10.1542/hpeds.2015-0222 [DOI] [PubMed] [Google Scholar]
- 23.Pencheon D. Developing a sustainable health and care system: lessons for research and policy. J Health Serv Res Policy 2013;18:193–4. 10.1177/1355819613503633 [DOI] [PubMed] [Google Scholar]
- 24.Inotai A, Petrova G, Vitezic D, et al. Benefits of investment into modern medicines in Central-Eastern European countries. Expert Rev Pharm Out 2014;14:71–9. 10.1586/14737167.2014.868314 [DOI] [PubMed] [Google Scholar]
- 25.Sepehri A. Does autonomization of public hospitals and exposure to market pressure complement or debilitate social health insurance systems? Evidence from a low-income country. Int J Health Serv 2014;44:73–92. 10.2190/HS.44.1.e [DOI] [PubMed] [Google Scholar]
- 26.Zhao Y, Russell DJ, Guthridge S, et al. Long-Term trends in supply and sustainability of the health workforce in remote Aboriginal communities in the Northern Territory of Australia. BMC Health Serv Res 2017;17:836. 10.1186/s12913-017-2803-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Sonnenreich P, Geisler L. Covering the cost of the cure: from hepatitis C to cancer, new therapies are straining a system plagued by inefficiency. P T 2016;41:565–89. [PMC free article] [PubMed] [Google Scholar]
- 28.Stuart B, D'Onofrio CN, Boatman S, et al. Choices: promoting early access to end-of-life care through home-based transition management. J Palliat Med 2003;6:671–83. 10.1089/109662103768253849 [DOI] [PubMed] [Google Scholar]
- 29.Rees GH. Organisational readiness and lean thinking implementation: findings from three emergency department case studies in New Zealand. Health Serv Manage Res 2014;27:1–9. 10.1177/0951484814532624 [DOI] [PubMed] [Google Scholar]
- 30.Ammentorp J, Bigi S, Silverman J, et al. Upscaling communication skills training - lessons learned from international initiatives. Patient Educ Couns 2021;104:352–9. 10.1016/j.pec.2020.08.028 [DOI] [PubMed] [Google Scholar]
- 31.Braithwaite J, Marks D, Taylor N. Harnessing implementation science to improve care quality and patient safety: a systematic review of targeted literature. Int J Qual Health Care 2014;26:321–9. 10.1093/intqhc/mzu047 [DOI] [PubMed] [Google Scholar]
- 32.Shigayeva A, Coker RJ. Communicable disease control programmes and health systems: an analytical approach to sustainability. Health Policy Plan 2015;30:368–85. 10.1093/heapol/czu005 [DOI] [PubMed] [Google Scholar]
- 33.Fineberg HV. Shattuck Lecture. A successful and sustainable health system--how to get there from here. N Engl J Med 2012;366:1020–7. 10.1056/NEJMsa1114777 [DOI] [PubMed] [Google Scholar]
- 34.Sepehri A, Chernomas R. Is the Canadian health care system fiscally sustainable? Int J Health Serv 2004;34:229–43. 10.2190/HW0X-VA0Q-F99K-EP4V [DOI] [PubMed] [Google Scholar]
- 35.Kerr R, Hendrie DV. Is capital investment in Australian hospitals effectively funding patient access to efficient public hospital care? Aust Health Rev 2018;42:501. 10.1071/AH17231 [DOI] [PubMed] [Google Scholar]
- 36.Buykx P, Humphreys JS, Tham R, et al. How do small rural primary health care services sustain themselves in a constantly changing health system environment? BMC Health Serv Res 2012;12:81. 10.1186/1472-6963-12-81 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Cashin A. The challenge of nurse innovation in the Australian context of universal health care. Collegian 2015;22:319–24. 10.1016/j.colegn.2014.03.006 [DOI] [PubMed] [Google Scholar]
- 38.Buttigieg SC. Innovation strategies and health system guiding principles to address equity and sustainability in responsible innovation in health; comment on "What Health System Challenges Should Responsible Innovation in Health Address? Insights From an International Scoping Review". Int J Health Policy Manag 2019;8:570–2. 10.15171/ijhpm.2019.50 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Chambers DA, Glasgow RE, Stange KC. The dynamic sustainability framework: addressing the paradox of sustainment amid ongoing change. Implement Sci 2013;8:117. 10.1186/1748-5908-8-117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Scheirer MA. Is sustainability possible? A review and commentary on empirical studies of program sustainability. Am J Eval 2005;26:320–47. 10.1177/1098214005278752 [DOI] [Google Scholar]
- 41.Gruen RL, Elliott JH, Nolan ML, et al. Sustainability science: an integrated approach for health-programme planning. Lancet 2008;372:1579–89. 10.1016/S0140-6736(08)61659-1 [DOI] [PubMed] [Google Scholar]
- 42.Embi PJ, Richesson R, Tenenbaum J, et al. Reimagining the research-practice relationship: policy recommendations for informatics-enabled evidence-generation across the US health system. JAMIA Open 2019;2:2–9. 10.1093/jamiaopen/ooy056 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Enticott J, Braaf S, Johnson A, et al. Leaders' perspectives on learning health systems: a qualitative study. BMC Health Serv Res 2020;20:1087. 10.1186/s12913-020-05924-w [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Clancy C. Creating world-class care and service for our Nation’s finest: How Veterans Health Administration Diffusion of Excellence Initiative is innovating and transforming Veterans Affairs health care. Permanente Journal 2019;23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 45.Kilbourne AM, Braganza MZ, Bowersox NW. Research lifecycle to increase the substantial real-world impact of research: accelerating innovations to application. Med Care 2019;57 Suppl:S206–12. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Smith M, Saunders R, et al. , Committee on the Learning Health Care System in A, Institute of M . Best care at lower cost: the path to continuously learning health care in America. Washington (DC): National Academies Press (US), 2013. [PubMed] [Google Scholar]
- 47.Kepros JP, Opreanu RC. A new model for health care delivery. BMC Health Serv Res 2009;9:57. 10.1186/1472-6963-9-57 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Dhalla I. Canada’s health care system and the sustainability paradox. Can Med Assoc J 2007;177:51–3. 10.1503/cmaj.061064 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Garde S, Hullin CM, Chen R, et al. Towards sustainability of health information systems: how can we define, measure and achieve it? Stud Health Technol Inform 2007;129:1179–83. [PubMed] [Google Scholar]
- 50.Solon O, Woo K, Quimbo SA, et al. A novel method for measuring health care system performance: experience from QIDS in the Philippines. Health Policy Plan 2009;24:167–74. 10.1093/heapol/czp003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Molfenter T, Gustafson D, Kilo C, et al. Prospective evaluation of a Bayesian model to predict organizational change. Health Care Manage Rev 2005;30:270–9. 10.1097/00004010-200507000-00011 [DOI] [PubMed] [Google Scholar]
- 52.Birch S, Murphy GT, MacKenzie A, et al. In place of fear: aligning health care planning with system objectives to achieve financial sustainability. J Health Serv Res Policy 2015;20:109–14. 10.1177/1355819614562053 [DOI] [PubMed] [Google Scholar]
- 53.Pacifico Silva H, Lehoux P, Miller FA, et al. Introducing responsible innovation in health: a policy-oriented framework. Health Res Policy Syst 2018;16:90. 10.1186/s12961-018-0362-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Lo Sardo DR, Thurner S, Sorger J, et al. Quantification of the resilience of primary care networks by stress testing the health care system. Proc Natl Acad Sci U S A 2019;116:23930–5. 10.1073/pnas.1904826116 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Shen H, Sui Y, Fu Y. Using social choice theory and acceptability analysis to measure the value of health systems. PLoS One 2020;15:e0235531. 10.1371/journal.pone.0235531 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Crisp N. What would a sustainable health and care system look like? BMJ 2017;358:j3895. 10.1136/bmj.j3895 [DOI] [PubMed] [Google Scholar]
- 57.Shaw J, Wong I, Griffin B, et al. Principles for health system capacity planning: insights for healthcare leaders. Healthc Q 2017;19:17–22. 10.12927/hcq.2017.25016 [DOI] [PubMed] [Google Scholar]
- 58.Scott IA. Is modern medicine at risk of losing the plot? Med J Aust 2006;185:213–6. 10.5694/j.1326-5377.2006.tb00534.x [DOI] [PubMed] [Google Scholar]
- 59.Robertson TM, Lofgren RP. Where population health misses the mark: breaking the 80/20 rule. Acad Med 2015;90:277–8. 10.1097/ACM.0000000000000627 [DOI] [PubMed] [Google Scholar]
- 60.Pisco L, Pinto LF. From Alma-Ata to Astana: the path of primary health care in Portugal, 1978-2018 and the genesis of family medicine. Cien Saude Colet 2020;25:1197–204. 10.1590/1413-81232020254.31222019 [DOI] [PubMed] [Google Scholar]
- 61.Jessup RL, O'Connor DA, Putrik P, et al. Alternative service models for delivery of healthcare services in high-income countries: a scoping review of systematic reviews. BMJ Open 2019;9:e024385. 10.1136/bmjopen-2018-024385 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Rudnicka E, Napierała P, Podfigurna A, et al. The World Health Organization (WHO) approach to healthy ageing. Maturitas 2020;139:6–11. 10.1016/j.maturitas.2020.05.018 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Quaglio G, Figueras J, Mantoan D, et al. An overview of future EU health systems. An insight into governance, primary care, data collection and citizens' participation. J Public Health 2018;40:891–8. 10.1093/pubmed/fdy054 [DOI] [PubMed] [Google Scholar]
- 64.Pereno A, Eriksson D. A multi-stakeholder perspective on sustainable healthcare: from 2030 onwards. Futures 2020;122:102605. 10.1016/j.futures.2020.102605 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Knutson DJ. The role of strategic alliances in ensuring health care quality: a health care system perspective. Clin Ther 1997;19:1572–8. 10.1016/S0149-2918(97)80029-X [DOI] [PubMed] [Google Scholar]
- 66.Delgado P. Meeting the challenge of chronic conditions in a sustainable manner: building on the AHC learning. Healthc Pap 2016;15 Spec No:90–5. 10.12927/hcpap.2016.24504 [DOI] [PubMed] [Google Scholar]
- 67.Costa-Font J, Levaggi R. Innovation, aging, and health care: Unraveling "silver" from "red" herrings? Health Econ 2020;29 Suppl 1:3–7. 10.1002/hec.4187 [DOI] [PubMed] [Google Scholar]
- 68.Veillard J, Denny K. Transformation through clinical and social integration: meeting the needs of high users of healthcare. Healthc Pap 2014;14:4–7. 10.12927/hcpap.2015.24102 [DOI] [PubMed] [Google Scholar]
- 69.Stoelwinder JU. Final report of the National Health and Hospitals Reform Commission: will we get the health care governance reform we need? Med J Aust 2009;191:387–8. 10.5694/j.1326-5377.2009.tb02846.x [DOI] [PubMed] [Google Scholar]
- 70.Stoelwinder JU, Paolucci F. Sustaining Medicare through consumer choice of health funds: lessons from the Netherlands. Med J Aust 2009;191:30–2. 10.5694/j.1326-5377.2009.tb02671.x [DOI] [PubMed] [Google Scholar]
- 71.Magnan S, Fisher E, Kindig D, et al. Achieving accountability for health and health care. Minn Med 2012;95:37–9. [PubMed] [Google Scholar]
- 72.Armstrong BK, Gillespie JA, Leeder SR, et al. Challenges in health and health care for Australia. Med J Aust 2007;187:485–9. 10.5694/j.1326-5377.2007.tb01383.x [DOI] [PubMed] [Google Scholar]
- 73.Ganann R, Peacock S, Garnett A, et al. Capacity development among academic trainees in community-based primary health care research: the aging, community and health research unit experience. Prim Health Care Res Dev 2019;20:e139. 10.1017/S1463423619000732 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 74.Al Dhawi AA, West DJ, Spinelli RJ, et al. The challenge of sustaining health care in Oman. Health Care Manag 2007;26:19–30. 10.1097/00126450-200701000-00003 [DOI] [PubMed] [Google Scholar]
- 75.Thistlethwaite JE, Dunston R, Yassine T. The times are changing: workforce planning, new health-care models and the need for interprofessional education in Australia. J Interprof Care 2019;33:361–8. 10.1080/13561820.2019.1612333 [DOI] [PubMed] [Google Scholar]
- 76.Dunn PM, Arnetz BB, Christensen JF, et al. Meeting the imperative to improve physician well-being: assessment of an innovative program. J Gen Intern Med 2007;22:1544–52. 10.1007/s11606-007-0363-5 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Woodward GL, Iverson A, Harvey R, et al. Implementation of an agency to improve chronic kidney disease care in Ontario: lessons learned by the Ontario renal network. Healthc Q 2015;17 Spec No:44–7. 10.12927/hcq.2014.24009 [DOI] [PubMed] [Google Scholar]
- 78.Mackenzie J. The old care paradigm is dead, long live the new sustainable care paradigm: how can GP commissioning consortia meet the demand challenges of 21st century healthcare? London J Prim Care 2011;4:65–9. 10.1080/17571472.2011.11493330 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Pencheon D. Making health care more sustainable: the case of the English NHS. Public Health 2015;129:1335–43. 10.1016/j.puhe.2015.08.010 [DOI] [PubMed] [Google Scholar]
- 80.Lewis S. Can a learning-disabled nation learn healthcare lessons from abroad? Healthc Policy 2007;3:19–28. 10.12927/hcpol.2007.19388 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Edwards N, Rowan M, Marck P, et al. Understanding whole systems change in health care: the case of nurse practitioners in Canada. Policy Polit Nurs Pract 2011;12:4–17. 10.1177/1527154411403816 [DOI] [PubMed] [Google Scholar]
- 82.Lozano I, Rondán J, Vegas JM, et al. Sustainability of the health system: beyond cost-effectiveness analyses. Rev Esp Cardiol 2016;69:880–1. 10.1016/j.rec.2016.05.002 [DOI] [PubMed] [Google Scholar]
- 83.Vainieri M, Noto G, Ferre F, et al. A performance management system in healthcare for all seasons? Int J Environ Res Public Health 2020;17. 10.3390/ijerph17155590. [Epub ahead of print: 03 08 2020]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 84.Farmanova E, Kirvan C, Verma J, et al. Triple aim in Canada: developing capacity to lead to better health, care and cost. Int J Qual Health Care 2016;28:830–7. 10.1093/intqhc/mzw118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 85.Iskrov G, Stefanov R, Ferrelli RM. Health systems for rare diseases: financial sustainability. Ann Ist Super Sanita 2019;55:270–5. 10.4415/ANN_19_03_13 [DOI] [PubMed] [Google Scholar]
- 86.Buttigieg SC, Schuetz M, Bezzina F. Value chains of public and private health-care services in a small EU island state: a SWOT analysis. Front Public Health 2016;4:201. 10.3389/fpubh.2016.00201 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Atmore C. The role of medical generalism in the New Zealand health system into the future. N Z Med J 2015;128:50–5. [PubMed] [Google Scholar]
- 88.Barbazza E, Kringos D, Kruse I, et al. Creating performance intelligence for primary health care strengthening in Europe. BMC Health Serv Res 2019;19:1006. 10.1186/s12913-019-4853-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Thompson RE. Sustainability as the lynch pin of public policy and industry initiatives. Physician Exec 1998;24:52–5. [PubMed] [Google Scholar]
- 90.Buchan JM, Naccarella L, Brooks PM. Is health workforce sustainability in Australia and New Zealand a realistic policy goal? Aust Health Rev 2011;35:152–5. 10.1071/AH10897 [DOI] [PubMed] [Google Scholar]
- 91.McGorry PD, Hamilton MP. Stepwise expansion of evidence-based care is needed for mental health reform. Med J Aust 2016;204:351–3. 10.5694/mja16.00120 [DOI] [PubMed] [Google Scholar]
- 92.Ehrlich C, Kendall E. Integrating collaborative place-based health promotion coalitions into existing health system structures: the experience from one Australian health coalition. Int J Integr Care 2015;15:e047. 10.5334/ijic.2012 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 93.Levine S, O'Mahony S, Baron A, et al. Training the workforce: description of a longitudinal interdisciplinary education and mentoring program in palliative care. J Pain Symptom Manage 2017;53:728–37. 10.1016/j.jpainsymman.2016.11.009 [DOI] [PubMed] [Google Scholar]
- 94.Lega F, Prenestini A, Spurgeon P. Is management essential to improving the performance and sustainability of health care systems and organizations? A systematic review and a roadmap for future studies. Value in Health 2013;16:S46–51. 10.1016/j.jval.2012.10.004 [DOI] [PubMed] [Google Scholar]
- 95.Wakerman J, Humphreys JS. Sustainable workforce and sustainable health systems for rural and remote Australia. Med J Aust 2013;199:S14–17. 10.5694/mja11.11639 [DOI] [PubMed] [Google Scholar]
- 96.Wakerman J, Humphreys JS. Sustainable primary health care services in rural and remote areas: innovation and evidence. Aust J Rural Health 2011;19:118–24. 10.1111/j.1440-1584.2010.01180.x [DOI] [PubMed] [Google Scholar]
- 97.Lehoux P, Roncarolo F, Silva HP, et al. What health system challenges should responsible innovation in health address? Insights from an international scoping review. Int J Health Policy Manag 2019;8:63–75. 10.15171/ijhpm.2018.110 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Marcotte LM, Moriates C, Wolfson DB, et al. Professionalism as the bedrock of high-value care. Acad Med 2020;95:864–7. [DOI] [PubMed] [Google Scholar]
- 99.Braithwaite J, Vincent C, Nicklin W, et al. Coping with more people with more illness. Part 2: new generation of standards for enabling healthcare system transformation and sustainability. Int J Qual Health Care 2019;31:159–63. 10.1093/intqhc/mzy236 [DOI] [PubMed] [Google Scholar]
- 100.Tsasis P. Chronic disease management and the home-care alternative in Ontario, Canada. Health Serv Manage Res 2009;22:136–9. 10.1258/hsmr.2009.009002 [DOI] [PubMed] [Google Scholar]
- 101.Niraula S. Strategizing health technology assessment for containment of cancer drug costs in a universal health care system: case of the pan-Canadian oncology drug review. Cancer 2019;125:3100–3. 10.1002/cncr.32209 [DOI] [PubMed] [Google Scholar]
- 102.Bentley C, Peacock S, Abelson J, et al. Addressing the affordability of cancer drugs: using deliberative public engagement to inform health policy. Health Res Policy Syst 2019;17:17:17. 10.1186/s12961-019-0411-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 103.Rosser M. Advancing health system integration through supply chain improvement. Hcq 2006;9:4:62–6. 10.12927/hcq.2006.17906 [DOI] [PubMed] [Google Scholar]
- 104.Derakhshani N, Doshmangir L, Ahmadi A, et al. Monitoring process barriers and enablers towards universal health coverage within the sustainable development goals: a systematic review and content analysis. Clinicoecon Outcomes Res 2020;12:459–72. 10.2147/CEOR.S254946 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 105.Guyon Ak'ingabe, Hancock T, Kirk M, et al. The weakening of public health: a threat to population health and health care system sustainability. Can J Public Health 2017;108:e1–6. 10.17269/cjph.108.6143 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 106.Bessler JS, Ellies M. Values and value-a vision for the Australian health care system. Aust Health Rev 1995;18:6–17. [PubMed] [Google Scholar]
- 107.Ferrelli RM, Fantini B, Taruscio D. Health systems sustainability for rare diseases. Preface. Ann Ist Super Sanita 2019;55:249–50. 10.4415/ANN_19_03_09 [DOI] [PubMed] [Google Scholar]
- 108.Walsh K. Strengthening primary care: the role of e-learning. Educ Prim Care 2019;30:267–9. 10.1080/14739879.2019.1641751 [DOI] [PubMed] [Google Scholar]
- 109.Bogaert P, van Oers H, Van Oyen H, et al. Towards a sustainable EU health information system infrastructure: a consensus driven approach. Health Policy 2018;122:1340–7. 10.1016/j.healthpol.2018.10.009 [DOI] [PubMed] [Google Scholar]
- 110.Fridell M, Edwin S, von Schreeb J, et al. Health system resilience: what are we talking about? A scoping review mapping characteristics and keywords. Int J Health Policy Manag 2020;9:6–16. 10.15171/ijhpm.2019.71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 111.Casale CR, Clancy CM. Commentary: not about us without us. Academic Medicine 2009;84:1333–5. 10.1097/ACM.0b013e3181b6afd0 [DOI] [PubMed] [Google Scholar]
- 112.Nagle L, Pitts B. Citizen perspectives on the future of healthcare. Healthc Q 2012;15:40–5. 10.12927/hcq.2012.22914 [DOI] [PubMed] [Google Scholar]
- 113.Schwann NM, Bretz KA, Eid S, et al. Point-of-care electronic prompts: an effective means of increasing compliance, demonstrating quality, and improving outcome. Anesth Analg 2011;113:869–76. 10.1213/ANE.0b013e318227b511 [DOI] [PubMed] [Google Scholar]
- 114.Wurcel V, Cicchetti A, Garrison L, et al. The value of diagnostic information in personalised healthcare: a comprehensive concept to facilitate bringing this technology into healthcare systems. Public Health Genomics 2019;22:8–15. 10.1159/000501832 [DOI] [PubMed] [Google Scholar]
- 115.Huynh AK, Hamilton AB, Farmer MM, et al. A pragmatic approach to guide implementation evaluation research: strategy mapping for complex interventions. Front. Public Health 2018;6. 10.3389/fpubh.2018.00134 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 116.Kilbourne AM, Braganza MZ, Bowersox NW, et al. Research lifecycle to increase the substantial real-world impact of research: accelerating innovations to application. Med Care 2019;57 Suppl 10 Suppl 3:S206–12. 10.1097/MLR.0000000000001146 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 117.Greenhalgh T, Macfarlane F, Barton-Sweeney C, et al. "If we build it, will it stay?" A case study of the sustainability of whole-system change in London. Milbank Q 2012;90:516–47. 10.1111/j.1468-0009.2012.00673.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 118.McVeigh J, MacLachlan M, Gilmore B, et al. Promoting good policy for leadership and governance of health related rehabilitation: a realist synthesis. Global Health 2016;12:49. 10.1186/s12992-016-0182-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 119.De Santis M. Integrated care for healthcare sustainability for patients living with rare diseases. Ann Ist Super Sanita 2019;55:276–82. 10.4415/ANN_19_03_14 [DOI] [PubMed] [Google Scholar]
- 120.McIntosh E, Nagelkerk J, Vonderheid SC, et al. Financially viable nurse-managed centers. Nurse Pract 2003;28:40–51. 10.1097/00006205-200303000-00009 [DOI] [PubMed] [Google Scholar]
- 121.Wutzke S, Benton M, Verma R. Towards the implementation of large scale innovations in complex health care systems: views of managers and frontline personnel. BMC Res Notes 2016;9:327. 10.1186/s13104-016-2133-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 122.Burgess LH, Cohen MR, Denham CR. A new leadership role for pharmacists: a prescription for change. J Patient Saf 2010;6:31–7. 10.1097/PTS.0b013e3181d108cb [DOI] [PubMed] [Google Scholar]
- 123.Hanney S, Kanya L, Pokhrel S. WHO Health Evidence Network Synthesis Reports. What is the evidence on policies, interventions and tools for establishing and/or strengthening National health research systems and their effectiveness? Copenhagen: WHO Regional Office for Europe, 2020. [PubMed] [Google Scholar]
- 124.Braithwaite J, Glasziou P, Westbrook J. The three numbers you need to know about healthcare: the 60-30-10 challenge. BMC Med 2020;18. 10.1186/s12916-020-01563-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 125.Braithwaite J, Churruca K, Long JC, et al. When complexity science meets implementation science: a theoretical and empirical analysis of systems change. BMC Med 2018;16:63. 10.1186/s12916-018-1057-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 126.Bramesfeld A, Amaddeo F, Caldas-de-Almeida José, et al. Monitoring mental healthcare on a system level: country profiles and status from EU countries. Health Policy 2016;120:706–17. 10.1016/j.healthpol.2016.04.019 [DOI] [PubMed] [Google Scholar]
- 127.Braithwaite J, Zurynski Y, Ludlow K, et al. Towards sustainable healthcare system performance in the 21st century in high-income countries: a protocol for a systematic review of the grey literature. BMJ Open 2019;9:e025892. 10.1136/bmjopen-2018-025892 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 128.Abimbola S, Baatiema L, Bigdeli M. The impacts of decentralization on health system equity, efficiency and resilience: a realist synthesis of the evidence. Health Policy Plan 2019;34:605–17. 10.1093/heapol/czz055 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 129.Buchan J. What difference does ("good") HRM make? Hum Resour Health 2004;2:6. 10.1186/1478-4491-2-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 130.Hovenga EJS. Impact of data governance on a nation's healthcare system building blocks. Stud Health Technol Inform 2013;193:24–66. [PubMed] [Google Scholar]
- 131.Editorial. Healthc Q 2020;22:1–2. 10.12927/hcq.2020.26092 [DOI] [PubMed] [Google Scholar]
- 132.Craig N, Robinson M. Towards a preventative approach to improving health and reducing health inequalities: a view from Scotland. Public Health 2019;169:195–200. 10.1016/j.puhe.2019.02.013 [DOI] [PubMed] [Google Scholar]
- 133.Rosenberg-Yunger ZRS, Daar AS, Singer PA, et al. Healthcare sustainability and the challenges of innovation to biopharmaceuticals in Canada. Health Policy 2008;87:359–68. 10.1016/j.healthpol.2008.02.004 [DOI] [PubMed] [Google Scholar]
- 134.Barasa EW, Cloete K, Gilson L. From bouncing back, to nurturing emergence: reframing the concept of resilience in health systems strengthening. Health Policy Plan 2017;32:iii91–4. 10.1093/heapol/czx118 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 135.Lehoux P, Williams-Jones B, Miller F, et al. What leads to better health care innovation? arguments for an integrated policy-oriented research agenda. J Health Serv Res Policy 2008;13:251–4. 10.1258/jhsrp.2008.007173 [DOI] [PubMed] [Google Scholar]
- 136.Cunningham FC, Ranmuthugala G, Westbrook JI, et al. Tackling the wicked problem of health networks: the design of an evaluation framework. BMJ Open 2019;9:e024231. 10.1136/bmjopen-2018-024231 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 137.Tricco AC, Ashoor HM, Cardoso R, et al. Sustainability of knowledge translation interventions in healthcare decision-making: a scoping review. Implementation Sci 2015;11:55. 10.1186/s13012-016-0421-7 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
bmjopen-2021-059207supp001.pdf (46.6KB, pdf)
bmjopen-2021-059207supp002.pdf (526KB, pdf)
bmjopen-2021-059207supp003.pdf (462.3KB, pdf)
Data Availability Statement
All data relevant to the study are included in the article or uploaded as supplementary information.