Abstract
Introduction
Live Broadcast of Surgical Procedures (LBSP) has gained popularity in conferences and educational meetings in the past few decades. This is due to rapid advancement in both Minimally Invasive Surgery (MIS) that enable transmission of the entire operative field and transmission ease and technology to help broadcast the operation to a live audience. The aim of this study was to update the evidence with specific emphasis on the patient safety issues related to LBSP in MIS.
Methods
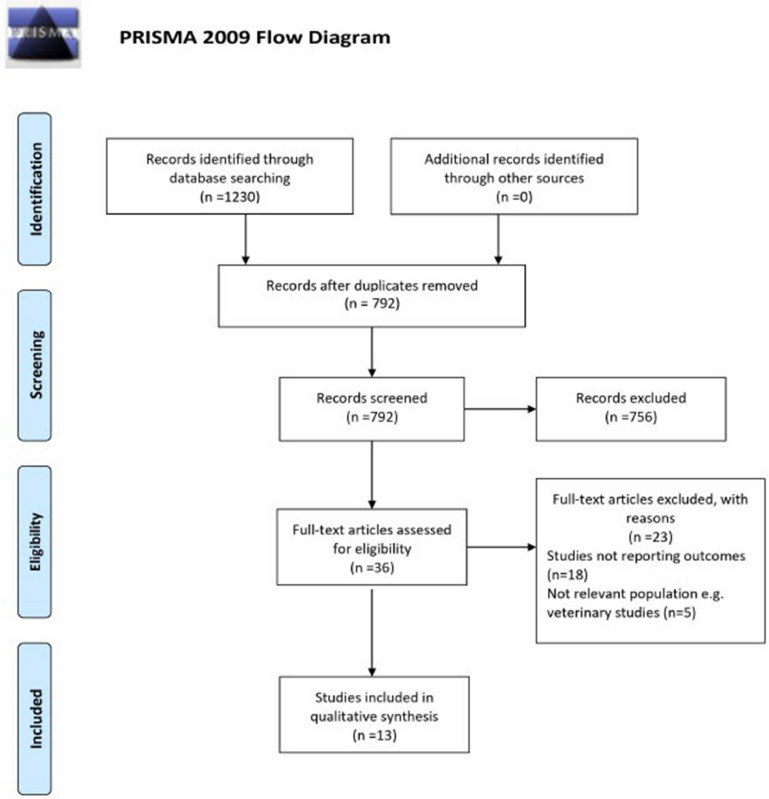
A systematic review of the literature was performed using Medline, Embase and Pubmed using defined search terms related to LBSP in educational events across all surgical specialities, in accordance with the PRISMA guidelines. We also consolidated the prior guidelines and position statements on this topic. Outcomes included reports on the educational value of LBSP as well as patient safety outcomes and ethical issues that were captured by clinical outcomes.
Results
A total 1230 abstracts were identified with 27 papers meeting the inclusion criteria (13 original articles and 14 position statements/guidelines). All studies highlighted the educational benefits of LBSP but without clear measure of these benefits. Clinical outcomes were not compromised in 9 studies but were inferior in the remaining 4, including lower completion rate of endoscopic surgery and higher rate of re-operation. Only nine studies complied with dedicated consent forms for LBSP with no consistent approach of reporting on maintaining patient confidentiality during LBSP.
There was a lack of recommendation on standardised approach of reporting on LBSP including the outcomes across the 14 published guidelines and positions statements.
Conclusions
Live Broadcast of Surgical Procedures can be of educational value but patient safety may be compromised. A standardised framework of reporting on LBSP and its outcomes is required from an ethical and patient safety perspective.
PROSPERO registration
CRD42021256901.
Supplementary Information
The online version contains supplementary material available at 10.1007/s00464-022-09072-6.
Keywords: Live, Surgery, Broadcast, Safety
Background
Live broadcast of surgical procedures (LBSP) has gained popularity in the past few decades and is commonly used in educational events such as conferences and live digital learning events. It is regarded as an opportunity for experts to demonstrate novel techniques and emerging technology especially in complex procedures for the benefit of a targeted audience [1].
This has been particularly applied to the field of Minimally Invasive Surgery (MIS) such as robotic, laparoscopic and or endoscopic techniques as the operative field can be live streamed to a large audience. It can also be an opportunity to see how an experienced surgeon would deal with intraoperative complications, including the decision making process of how they respond to unexpected findings/events. This has been commonly used within the context of educational conferences and events where narration provided allows the audience to engage and interact with the experts through the moderator(s).
There have been, however, some patient safety and ethical concerns during these live surgery broadcast [2]. Surgeons will often travel to perform LBSP outside their normal institutions, which may result in ‘jet lag’ and added fatigue that can alter their performance. Importantly, these surgeries are often complex techniques and or emerging technology which can be technically demanding, adding more stress on the surgical team. Additionally, surgeons often work with potentially unfamiliar teams and equipment which may add further anxiety to the performing surgeon, who may already feel under more pressure to perform in front of a large audience.
Furthermore, the extra personnel required to conduct the live transmission may contribute to distraction to the operating team and may affect the level of infection control in the theatre environment. Finally, expert surgeons do not routinely follow-up those patients and so will be reliant on the host team to care for them postoperatively. Given the likelihood complexity of those cases, host teams may be not familiar with the associated risks and complications.
An evidence synthesis was performed in 2014 looking at the educational value and patient safety of LBSP [3]. They found a comparable rate of complications between procedures performed as LBSP compared to non-LBSP. However, the success rate in some procedures was lower in LBSP group, as demonstrated in endoscopic completion rate. Since the last review, there has been a rapid uptake of MIS across all specialities with more reports on the application LBSP in surgical training. This, however, has been significantly impacted by the unprecedented COVID-19 pandemic with the cancellation of national and international meetings [4]. Alternative ways of remote teaching such as webinars have been widely adopted during the pandemic, but it is unclear if LBSP should be an integral part of this virtual teaching. Therefore, it was necessarily to update the evidence synthesis and re- appraise the literature.
The focus of this review is patient safety issues related to LBSP in Minimally Invasive Surgery (MIS), but a more global view on the matter is also addressed such as ethics and confidentiality.
Methods
Search strategy
A comprehensive review of the literature was conducted in accordance with the Preferred Reporting Items for Systematic Review and Meta-Analysis (PRISMA) guidelines [5]. The PubMed, Embase and Medline electronic databases were used and a search of the data from 1 March 2005 till 20 February 2021 was performed. The start date was chosen to reflect some of the earliest substantial reports on LBSP in the literature (excluding case reports). Search terms used combinations of “broadcast”, “live surgery”, “safety”, “ethic” and “live surgical broadcast” separated by the Boolean operator “AND”, were used. The search was performed independently by two separate authors. A further search was performed on 10 October 2020 with search terms “COVID-19”, “live surgery”, “live surgical broadcast”, in order to capture any reported literature during the pandemic to date. A subsequent manual search of the related study references was conducted in order to capture reports that were missed in the initial search, and all identified suitable studies were included. Abstracts and conference entries were excluded at initial screening due to the inability of capturing complete sets of data.
Study selection
Studies were eligible for inclusion if they were written in the English language and available in full text. More specifically the following inclusion criteria were used: randomised controlled studies, controlled trials or cohort studies reporting the outcomes of LBSP among all surgical specialties; studies that reported broadcast in conferences as well as other educational events and the guidelines on LBSP across the different surgical bodies and institutions were also included.
There was no restriction on the type of MIS that was conducted and a wide range of procedures were included.
Studies were excluded if the total number of cases used was less than ten. All duplicate studies or studies using the same data set were excluded. All studies using paediatric patients were not included. Only studies reporting outcomes of procedures and complications were included, studies just reporting on delivery of LBSP or ethics were excluded. Finally, reports on social media transmission that were not broadcast live were also excluded.
Outcome measures
The number of patients, demographics (age and sex), type of surgery and reported outcomes and complications were recorded. This included success of procedure (there was heterogeneity in the reporting of this outcome dependant on the surgery performed), return to theatre and readmissions. Complications reported were compared to those patients who were not involved in LBSP.
Additionally, data on ethics, were also captured including dedicated consent forms for LBSP, maintain confidentiality through the live surgery broadcast and reporting on outcomes of those procedures.
Data extraction and analysis
Data extraction was performed independently by two separate authors (MA and MC). After the initial screening of titles and abstracts, articles which fulfilled the eligibility criteria were identified and full text accessed for further analysis.
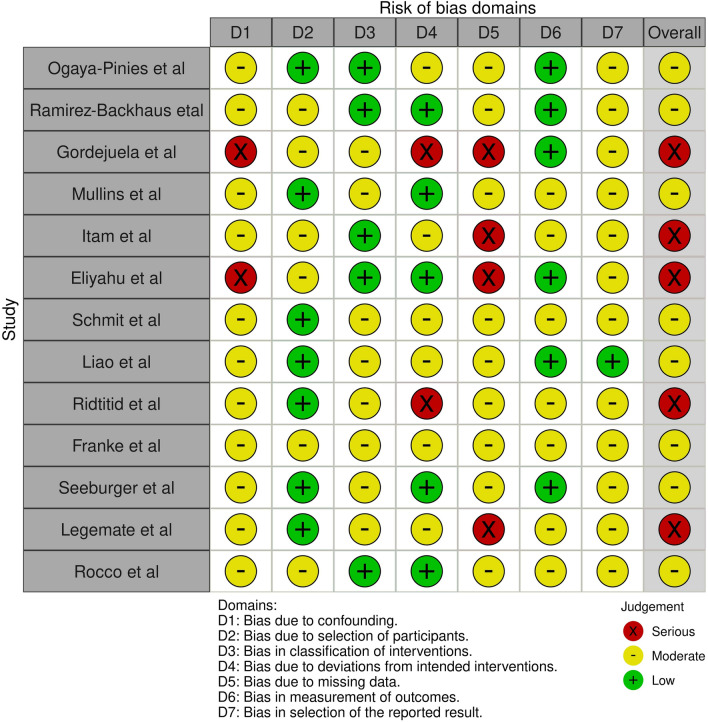
The methodological quality of the studies was assessed using the Risk of Bias in Non-randomised Studies of Interventions tool (ROBINS-1).
The results are described using a narrative analysis, and primarily grouped by the outcome assessed. Meta-analysis could not be performed on the data due to the heterogeneity of the studies as most of the studies were not statistically comparable.
Results
Demographics
The search strategy identified 1230 abstracts. After removal of duplicates and exclusions were made, 27 final manuscripts were selected for data extraction, including thirteen original papers and fourteen guidelines/position statements. The PRISMA diagram is summarised in Fig. 1.
Fig. 1.
PRISMA Diagram
Eight papers reported on events performed at a single centre while five were multicentre studies in the analysed 13 full text papers [6–18]. Eight papers reported on events live streamed from a European country, with the remainder being from the USA and Asia. Only two of the papers reported on the number of attendees at their event [8, 18] (Table 1).
Table 1.
| Authors | Journal | Study type | Year | single /multi | Country | Name of the article | Consent | Ethics | Demography | Audience | Number of LBSP | Procedures | Surgical Approach | Outcome measure | Clinical Outcome | Complications |
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Ogaya-Pinies et al | European Urology Focus | Retrospective case matched | 2019 | Single centre | USA | Safety of Live Robotic Surgery: Results from a Single Institution | Dedicated | Adhered to the EAU code of conduct for LBSP, patient anonymity and confidentiality maintained at all time, no sponsoring allowed and patient advocate present at all times | Presented at local, national and international congress, single centre, performed by single surgeon, did not mention numbers presented to, procedures performed in home institution | International | 36 | Robotic-assisted radical prostatectomy | Robotic (n = 36) | Intraoperative (operative time, EBL, lymphadenectomy) Postoperative (LOS, complications, time to potency/continence) Pathological (positive surgical margins) | No difference | No difference |
| Ramirez-Backhaus et al | Urology | Prospective case controlled | 2019 | Single centre | Spain | Live Surgery for Laparoscopic Radical Prostatectomy-Does it Worsen the Outcomes? A Single-centre Experience | Dedicated | Not stated | Presented locally live in auditorium in courses. Surgeries performed by 3 different surgeons | National | 23 | Laparoscopic prostatectomy | Laparoscopic (n = 23) | Intraoperative (operative time, EBL, intraoperative complications) Pathological (Positive surgical margins, biochemical recurrence) Postoperative (complications, re-operations) | Higher positive surgical margin in LBSP | No difference |
| Gordejuela et al | Surgery for obesity and related diseases | Retrospective unadjusted cohort | 2017 | Single centre | Spain | Live surgery courses: retrospective safety analysis after 11 editions | Dedicated | Patient anonymity maintained at all times, no personal data reported to the audience, approved by local ethics board | Presented at international bariatric course, each edition approximately 100 surgeons in attendance. Local and international surgeons. Broadcast at institution auditorium | International | 107 | obesity surgery | Laparoscopic (n = 98) Endoscopic (n = 10) | Morbidity Re-operations Presentations to the emergency department | Lower success in LBSP | Higher is LBSP |
| Mullins et al | Urology | Retrospective unadjusted cohort | 2012 | Multicentre | USA | Live robotic surgery: Are outcomes compromised? | Dedicated |
Patient identity was protected at all times in accordance with Health Insurance Portability and Accountability Act regulations. No breach in confidentiality occurred during these cases |
Cases performed by 5 different surgeons at home and distant institutions, multi-institutional, broadcast via teleconference | National | 39 | Robotic-assisted partial nephrectomy | Robotic (n = 39) | EBL Operating time LOS Surgical margins Perioperative complications | No difference | No difference |
| Itam et al | Female pelvic medicine and recons surgery | Retrospective unadjusted cohort | 2020 | single centre | UK | Female Urology and Urogynaecology: The Outcome of Patients Participating in Live Surgical Broadcasts | Dedicated | Followed code of conduct adapted from the EAU publication | Presented in annual Female Urology and Urogynaecology Master class. All surgery performed by same six consultants (4 urology and 2 urogynaecology) | National | 53 | Urogynae cology |
SUI surgery POP repair VVF closure UD excision Surgery for mesh complications/urethroplasty 2nd-Stage SNM Formation of Mitrofanoff channel Botulinum toxin A injections/ FSTL insertion |
30- and 90-day complications. Surgical success(defined in the paper) | No difference | No difference |
| Eliyahu et al | JACC: Cardiovascular Interventions | Retrospective unadjusted cohort | 2012 | Single centre | Israel | Patient safety and outcomes from live case demonstrations of interventional cardiology procedures | Dedicated |
Only mention is that the study was done with compliance with the local human studies committee |
Conferences were national and international, majority of operators were from the home institution with few cases from overseas | International | 103 | IR procedures (cardiac = 66; carotid = 15; peripheral = 1; valvular = 2; congenital = 12; ablation = 7) | Percutaneous interventional (n = 103) | In hospital (myocardial infarction, stroke, death, unsuccessful procedures, minor complications) Discharge to 30 days (myocardial infarction, stroke, death, repeat intervention) | No difference | No difference |
| Schmit et al | Endoscopy | Retrospective case matched | 2005 | Single centre | Belgium |
Complications of endoscopic retrograde cholangiopancreatography during live endoscopy workshop demonstrations |
None stated | Not described, but mention that true emergencies such as cholangitis were not delayed | Presented in annual endoscopy workshops in Erasmus University Hospital in Brussels. Mixture of foreign and local experts. Numbers presented to not mentioned | National | 168 | ERCP | Endoscopic (n = 168) | Delay to ERCP (in order to transmit) Duration of ERCP Complications Success of procedure ( complete, partial or complete failure) Repeat procedure | No difference | No difference |
| Liao et al | Am J Gastroentrology | Retrospective case matched | 2009 | Multicentre | China |
How safe and successful are live demonstrations of therapeutic ERCP? A large multicentre study |
No indication if dedicated, just stated 'written informed consent was obtained' | Study was approved by the Ethics Committee of local institutions | Presented at 36 endoscopy conferences across 14 centres in China. Presented by a mixture of local, domestic, visiting and local experts. Numbers attending not stated | International | 406 | ERCP | Endoscopic (n = 406) | Success (Complete, partial, complete failure) Complications | Lower success in LBSP | No difference |
| Ridtitid et al | Surg endoscopy | Retrospective case matched | 2012 | Single centre | Thailand |
Outcome of endoscopic retrograde cholangiopancreatography during live endoscopy demonstrations |
Dedicated |
Conference program was approved by the Chulalongkorn University Medical Institutional Review Board and TAGE |
Annual LD workshop in Thialand King Chulalongkorn Memorial hospital in collaboration with Thai Association for Gastrointestinal Endoscopy. LBSP performed by overseas experts only, no mention of numbers attending | International | 82 | ERCP | Endoscopic (n = 82) | Success (Complete, partial, complete failure) Complications Duration of procedure LOS | Lower success in LBSP | No difference |
| Franke et al | JACC: Cardiovascular Interventions | Retrospective unadjusted cohort | 2009 | Multicentre | Germany/Italy |
Complications of carotid stenting during live transmissions |
Dedicated | Not stated | 22 international conferences from 3 high volume centres, 2 in Germany and 1 in Italy. Guest performed the LBSP. No mention on numbers attending | International | 186 | Carotid stenting | Percutaneous interventional (n = 186) | Technical success, complications, rate of myocardial infarction, mortality | No difference | No difference |
| Seeburger et al | European Journal of cardiothoracic surgery | Retrospective unadjusted cohort | 2011 | multicentre | Germany/Belgium | Live broadcasting in cardiac surgery does not increase the operative risk |
Patients were consented for the surgical procedure and gave permission for live broadcasting to the respective meeting audience and recording of the procedure the day before surgery |
Adhered to the conduct of live surgery developed by the EACTS Techno College Committee, but no specific mention of confidentiality |
Performed in 4 clinical sites across Germany and Belgium and broadcast across 32 scientific meetings across Germany and Belgium to international audience. Mixture of local and guest operators. Numbers not mentioned | International | 250 | Cardiac surgery |
Mitral valve 126 Aortic valve 34 CABG 29 Aortic 15 Atrial fibrillation 13 Heart failure 7 Congenital 26 |
Mortality, complications, re-operation | No difference | No difference |
| Legemate et al | World Journal of Urology | Retrospective unadjusted cohort | 2017 | Single centre | Netherlands | Outcome from 5-year live surgical demonstrations in urinary stone treatment: are outcomes compromised? | No indication if dedicated | Not mentioned, only generic recommendations on ethics are included in the discussion but no description on what was implemented in the study | Streamed from academic centre in the Netherlands, mixture of host and guest surgeons. International setting. Delivered as part of 2 day course, no information on number of participants | International | 151 | Ureterorenoscopic (URS) and percutaneous nephrolithotomy (PNL) urinary stone procedures | URS = 95, Percutaneous = 56 | Intraoperative complications Postoperative complications, operation time, length of hospital stay, stone-free rate and retreatment rate | No significant difference in rate of intraoperative and postoperative complication rate. No difference in the complication grade score. However, operation time significantly higher in LSD-URS group, retreatment rate higher in LSD-URS group. Multiple logistical regression showed no increase in risk in LBSP group | No statistically significant difference |
| Rocco et al | World Journal of Urology | Retrospective unadjusted cohort | 2018 | Multicentre | Europe | Live surgery: highly educational or harmful | Not mentioned for the pooled studies, at end stated not needed and says from 2014 adhered to EAU guidelines |
From 2014, all the live surgeries have been organised according to the ethical rules as published by the EAU |
Annual attendance approximately 538 surgeons, Data from the Congress Challenge in Laparoscopy and Robotics (CILR). International audience. Multi-surgeon and multi-institution |
International | 224 |
Laparoscopic: Radical prostatectomy, Partial nephrectomy, Nephrectomy, Cystectomy, Retroperitoneal lymphadenectomy, Sacral colpopexy, pyeloplasty, bladder diverticulectomy repair. Robotic: Radical prostatectomy, Partial nephrectomy, Cystectomy, Pyeloplasty, Ureteral reimplantation, ureterolysis, sacral colpopexy, kidney transplant, fistula repair |
Laparoscopic = 164, Robotic 60 | Mortality and complications. Postoperative Morbidity Index | LBSP safe with acceptable outcomes over the 12-year time frame | Low complication rate in LBSP |
Eight papers were retrospective unadjusted cohort studies [8–11, 15–18], four retrospective case matched [6, 12–14] and one prospective case matched [7]. They addressed a wide range of specialities including urology, endoscopy, upper gastrointestinal surgery and cardiac interventions.
Patient safety outcomes
Of the 13 papers included, nine reported no difference in the complications nor the rate of success of the procedures performed (Table 1).
Four papers reported inferior outcomes in live broadcast. Ramirez-Backhaus et al. looked into the outcomes of LBSP in laparoscopic radical prostatectomy [7]. 23 patients were broadcasted live compared to 46 matched controls. They found no difference in the rate of perioperative or postoperative complications. However, they reported a significant difference in the rate of positive surgical margins in the LBSP group (43.5% vs 17.4%).
Ruiz de Gordejuela et al. analysed data obtained from bariatric courses, where LBSP was performed over a ten-year period [8]. Procedures performed included Laparoscopic Roux-en-Y gastric bypass, sleeve gastrectomy as well as endoscopic procedures. These were compared to patients undergoing similar procedures, not broadcast live. However, they were not matched controls. They found higher complication rates in LBSP and higher rate of re-operation needed. In the LBSP group, 13% of patients experienced complications as follows: Clavien type 1 (4 cases), Clavien type II (3 cases) and Clavien type III (6 cases) with bleeding being the most common complication (72.4%). This is compared to 6.7% in the group not performed as LBSP.
The two other studies reported inferior outcomes related to completion of the procedures during Endoscopic Retrograde Cholangio pancreatography (ERCP). Liao et al. investigated ERCPs broadcast live and compared them to matched controls across 36 conferences [13]. There was no statistically significant difference in the rate of complications between patients in LBSP and control (10.3% vs. 8.6%). However, there was a lower success rate in the live broadcast group (94.1% vs. 97.5%). Ridtitid et al. similarly searched the difference in outcomes and success rate in 82 risk-stratified ERCPs performed during live broadcast compared to matched controls [14]. The complexity of the ERCP was divided as per the grading proposed by Cotton et al. [19]. Patients who had level 1 and 2 procedures were classified as the standard group and patients who had level 3 and 4 procedures were classified as the complex group. They found that in technically simpler procedures there was no significant difference in the complications or success rate between LBSP and matched controls. However, the success rate was significantly lower in those procedures performed live compared to controls (73% vs. 90%; OR, 0.3; 95% CI 0.14–0.69) in more complex ERCPs. The overall success rate in the LBSP group was lower than controls (81% vs. 91%; OR, 0.4; 95% CI 0.21–0.85), but the complication rates were overall similar (6% vs. 3%; OR, 2.2; 95% CI 0.68–7.19).
Legemate et al. reported on the use of LBSP in ureterorenoscopic (URS) and percutaneous nephrolithotomy (PNL) urinary stone procedures and compared them to patients not performed as LBSP (unmatched). No statistically significant difference in the complication rate was found when compared to routine surgical practice. However, they found that the anaesthetic time was significantly longer in the LBSP group undergoing ureterorenoscopic procedures. They also found the retreatment rate was higher in this group. Subsequent multiple logistic regression analyses revealed that there is no association between LBSP and inferior outcomes (after adjusting for confounding variables) and so the authors concluded that LBSP does not compromise patient safety [17].
Ethics, confidentially and consenting
Dedicated consent forms were reported to be used in only 9 studies [6–11, 14–16]. One study reported on a pooled sample of data across several events and there heterogeneity in reporting dedicated consent [18]. In those that included a dedicated consent process, there was a lack of clarity of the contents of the consent form for LBSP.
Four of the 13 studies did not expand how they maintained ethics and confidentiality [7, 12, 15, 17] during the live surgery broadcast and 5 papers only mentioned that either their study was approved by the local ethics committee or they adhere to their associated guidelines, without further clarification.
Analysis of LBSP guidelines
14 guidelines were identified spanning across different surgical associations, representing four cardiothoracic, one urology, five endoscopy and one from ophthalmology. The remaining three were published by Royal Colleges of Surgeons of England and Australia and The Royal Australian and New Zealand College of Ophthalmologists [1, 20–32].
All guidelines and position statements addressed the issue of patient safety (Table 2). The majority are in agreement that a moderator must be present in order to facilitate the interaction between the operator and the audience. This is in order to allow the operator to fully focus on the procedure and avoid distraction. There is unanimous agreement that if is felt that continued broadcasting will have an adverse effect on the patient, it should be immediately terminated. There was, however, no proposed framework on a reporting mechanism of patient outcomes during and following LBSP except by the European Association of Urology [1].
Table 2.
| Name of the guidelines | Source | Year | Type/Methodology | Consent | Safety of patients in the OR | Protecting patient confidentiality |
|---|---|---|---|---|---|---|
|
Royal College of Surgeons Position Statement |
Royal College of Surgeons of England |
2017 | Guideline |
• Dedicated consent for the LBSP • Patient needs to have capacity • Emphasise no advantage or disadvantage of participating |
• Unnecessary personnel and equipment should be avoided in the operating room(OR) • The recording of the video should not interfere with the procedure • LBSP should be immediately terminated if there is an adverse effect on procedure • If there is interaction with the audience a moderator should be present • If the surgeon is not present to care for the patient postoperatively then a delegated member of the host team needs to be identified |
• Patient's personal information needs to be handled with great care to avoid breaching confidentiality • LBSP should not breach the relationship of trust between, surgeon, patient and operating team |
| Broadcast of Surgical Procedures as a Teaching Instrument in Cardiothoracic Surgery | American Association for Thoracic Surgery | 2008 |
Joint opinion between the American Association for Thoracic Surgery (AATS) and The Society of Thoracic Surgeons (STS) |
• LBSP consent must be obtained by the operating surgeon himself • The patient must be informed of potential increased risk of harm as well as audience number and educational value |
• LBSP is less acceptable with greater scheduling constraints, greater complexity of procedure, greater interaction with audience, less familiarity of the OR environment • The surgeon should be very familiar with the procedure and the medical equipment • Where ever possible the surgery should be broadcast from the surgeon’s home theatre • Preferably the surgeon's own team should participate, or at least members highly fluent in the same language • Video crew should not interfere with the operation • Discussions should be one way from surgeon to audience. If a great need for two way exists this should be done through a moderator |
• The attending surgeon should take all steps to protect the patient's personal privacy and confidentiality of all medical information |
| Guidelines to Live Presentation of Thoracic and Cardiovascular Surgery |
The Japanese society for Cardio- vascular surgery |
2007 | Guideline |
• Dedicated consent by the surgeon should be obtained directly with the patient and the patient should be informed that there may be added risk • The consent must be signed on paper • Consent also needs to be obtained from the ethics committee where the procedure will take place |
• The surgeon must not allow any interference with the surgery in the quest for superior imaging • Complex procedures should be avoided • The surgeon should be ideally performing the surgery in his home institution; if this is not possible preparations must be in place to adjust the environment |
• Personal information must be carefully managed. When displaying procedures, great care needs to be taken to ensure that no personal information is visible |
| EAU Policy on Live Surgery Events | European Association of Urology | 2014 | Systematic review and internet/panel-based consensus |
• A specific Informed Consent to Live Surgery addendum • Must be completed, signed by the local and guest • Surgeons, and retained in the patient’s medical records • The patient has right to withdraw consent at any time • The patient must meet the operating surgeon the day before surgery to consent |
• The operating surgeon must submit in advance preference for equipment • Anaesthetists must be involved in the planning process. Assistants should be suitably registered and experienced • All unnecessary equipment or personnel should not be in theatre • Representatives from industry should only be present if their presence is mandatory and should be appropriately registered by the host hospital • Delays for live proceedings must be avoided • An experienced urologist must be present to act as patient advocate • Presence of one or more moderators is recommended. Outcomes and complications must be submitted to the EUA Live surgery registry and documented in the revised Martin criteria |
• Patient dignity, anonymity and confidentiality to be maintained at all times |
| SCAI/ACCF/HRS/ESC/SOLACI/APSIC Statement on the Use of Live Case Demonstrations at Cardiology Meetings |
American College of Cardiology Foundation, the Heart Rhythm Society, and the Society for Cardio- vascular Angiography and Interventions |
2010 | Expert Consensus |
• The patient must be counselled on the procedure by an experienced physician • Two separate consent processes are needed for the procedure and LBSP • The patient can withdraw consent at any time without penalty |
• A moderator should be present • Serious complications should be dealt with "off camera" • Visiting operator should work with an operator highly familiar with the lab and equipment |
• The patient's identify should not be identified at any time • Care needs to be taken to not inadvertently display patient information on monitors |
| A guideline for live endoscopy courses: an ASGE white paper |
American Society for Gastrointestinal Endoscopy |
2001 | Guideline | • An informed consent is required which includes course details and who the operator will be |
• A host physician needs to be in the OR as well as the main operator • Careful placement of audio–visual equipment is needed • The operator needs to have familiarity with the facilities and staff • Representatives of industry must not interfere with patient care |
• Careful placement of audio–visual equipment to accommodate this |
|
Recommendations of the ESGE workshop on ethical legal issues concerning live demonstrations in digestive endoscopy. First European Symposium on Ethics in Gastroenterology and Digestive Endoscopy |
ESGE | 2003 | Expert opinion | • Consent to be obtained by local organiser detailing the procedure and also consenting for the live broadcast including advantages and disadvantages |
• The performing physician should be assisted by two moderators, at least one of whom is local • The moderator has the final decision for the treatment • Only staff involved in the treatment of the patient/audio–visual transmission should be present in the room • Industry representatives should be carefully avoided • The moderator should act as the interface between the expert and the audience |
• Acknowledged potential difficulty and the need to maintain confidentiality and privacy of the patient |
| Live endoscopy events (LEEs): European Society of Gastrointestinal Endoscopy Position Statement – Update 2014 | ESGE | 2014 | Guidelines |
• A separate additional consent specific to live endoscopy should be signed • Patient must be informed that they can withdraw their consent at any time or refuse to participate |
• Independent patient advocate should be present • A pre-procedure discussion should take place with the staff • The operator should agree all equipment needed in advance • Excessive prolongation must be avoided • There should be two moderators one in the clinical room and one at the conference centre • The moderator must interrupt the procedure if the patient is at risk of harm • Avoid high risk patients • Only personnel involved in the procedure/education should be in the clinical room • Representatives of industry must not interfere with the procedure |
• Every attempt must be made to keep all confidential information anonymous |
| Live transmission of surgery | Royal Australian College of Surgeons | 2016 | Position statement | • The patient needs to be counselled on the risks of the operation and the specific risks of LBSP |
• The operator must be prepared to terminate the procedure if necessary • The operator must be prepared to change the planned procedure if circumstances dictate • The operator should be familiar with the staff and procedure room • The operator should know who the audience will be • There needs to be a moderator to co-ordinate the interaction between the operator and the audience |
• Patient confidentiality needs to be maintained at all times |
| OMED recommendations for the ethical performance of live endoscopy demonstrations | World Endoscopy Organisation | 2016 | Position statement |
• The expert should be introduced to the patient and have the opportunity to discuss the indication and treatment proposed • Informed consent must be obtained and must include the advantages and disadvantages of the live course element |
• A course director must be identified who has final authority over decisions • The operator must be assisted by at least one moderator in the endoscopy room including one from the local staff • Interactive discussions should not influence clinical decisions taken • The number of personnel in the room should be limited to those involved in performing the procedure, teaching and operating the audio–visual equipment |
• Patient confidentiality needs to be respected including image acquisition and documentation |
| Updated guidelines for live endoscopy demonstrations | American Society for Gastrointestinal Endoscopy | 2010 | Position statement |
• The consenting process must include involvement in LBSP • The patient must be assured that the standard of care will not change based on their involvement |
• A patient ombudsman (with no conflict of interest) should be present • The procedure should be preferentially performed by the patient's treating physician • There must be no representatives of industry during the transmission |
• Patient confidentiality including health records should be at all times maintained |
| Live Case Demonstration of Interventional Cardiology Procedures | American College of Cardiology Foundation | 2012 | Position statement |
• The patient needs to consented on the risks of live transmission, increased risk of infection, prolongation of anaesthesia, increased contrast use, increased radiological exposure, distraction of the operator leading to complications, increased risk of disclosure of patient information • A dedicated consent form should be used and patients should be informed that they will have no clinical benefit from participating in live procedure |
• Procedures should be performed in a 'home' institution where equipment and facilities are familiar • A moderator should be present |
• Patient confidentiality including health records should be at all times maintained |
| Live transmission of surgery | The Royal Australian and New Zealand College of Ophthalmologists | 2013 | Position statement |
The use of pre-recorded video should be used over live transmission in all circumstances. Exceptions include: • Thorough analysis of the 17-point list detailed in the position statement has been undertaken prior to the procedure • The conclusion drawn from consideration from each of the points weigh in favour of the patient's best interests • Analysis of each factor has been recorded and distributed to the patient, surgeon, organisers and operational facility • Approval needs to be obtained from the RANZCO president, which must be in writing with a copy of the analysis |
• 17-point checklist as outlined the position statement | • Patient confidentiality including health records should be at all times maintained |
| Advisory Opinion—Live Surgery | American Academy of Ophthalmology | 2020 | Expert opinion |
• A patient’s consent needs to be comprehensive and include risks of live surgery, the potential distraction of surgeon and patient, the possibility of breaches of confidentiality, alternatives to live surgery • Coercion must be avoided, decision to withdraw needs to be respected |
• The surgeon needs to be familiar with the equipment prior to the LBSP • The surgeon needs to be competent at the procedure being performed • There needs to be suitable patient selection |
• The consent process needs to include the increased risk of breach of confidentiality; special consideration should be given to maintaining the confidential relationship between the physician and patient |
All guidelines encouraged familiarity with the location and equipment. Therefore, some recommend that where possible the surgeon should perform the procedure from their ‘home’ institution. Where this is not possible, they should familiarise themselves with the environment beforehand and should be working with a team highly familiar with the workplace. They should submit preferences for equipment beforehand in order to avoid unfamiliarity during the procedure. Personnel in theatre should be kept to a minimum and non-clinical staff must not interfere with the procedure.
There is also unanimous agreement among all the published guidelines for the need to have a dedicated consent process for LBSP. The consent should include discussion about the risks of LBSP to the patient such as increased surgeon distraction and the possible breaches of confidentiality. Also the consent should declare that there are potentially limited benefits to the patient to participate in LBSP. In a proportion of guidelines, there is a necessity for the operating surgeon or physician to meet and be involved in the consenting process with the patient in person before the procedure.
All guidelines stated that all attempts need to be made to protect patient confidentiality during and after the procedure. This involves the protection of patient identifiable information appearing on monitors and screens inadvertently.
The patient needs to at all times be reassured that they may refuse or withdraw their consent at any point without their care being affected. If their procedure is delayed due to withdrawal of consent, all attempts must be made to re-arrange their procedure in a timely manner. There must be no coercion of the patient.
Quality assessment
Using the ROBINS-I tool, eight of the studies had an overall moderate risk of bias and five studies had a serious risk of bias (Fig. 2).
Fig. 2.
Risk of bias (ROBINS-1)
Educational value
There was a paucity of original objective data reporting the educational value among the papers.
In their synthesis, Brunckhorst et al. addressed the educational value of LBSP. They note the lack of objective data on the subject. The majority of data reported is through subjective surveys showing participants rating LBSP highly as an educational tool. Only one study reported by Brunckhorst et al. addressed the validity of LBSP objectively. McIntyre et al. compared students in operating theatres against students watching LBSP. In the LBSP group, students asked four times as many questions compared to the group in the operating theatre and had fewer questions unanswered [3].
From the included studies in this synthesis, none measured objectively the educational value.
Discussion
Live surgical broadcast is now widely used among the different surgical specialities due to the perceived educational value of these events. Patient safety concerns however have been raised over the outcomes of patients during LBSP, owing to the different circumstances in which their surgery is being performed. Given the global impact of the pandemic on educational events, the role of live surgery broadcast within the context of virtual training curricula became more unclear. We felt it was appropriate to re-visit this topic, update the literature on LBSP and summarise the outcomes and the wider issue of ethics and patient safety in relation to MIS.
Educational value
Although the literature in this review highlighted the potential educational value of LBSP, it was difficult to draw a conclusion on the magnitude of benefits as this often was not objectively measured and was subjectively reported via surveys. Attempts have been made to do this via questionnaires after events by Skouras et al. [33], which was not included in the analysis as they did not report on clinical outcomes. They conducted surveys to examine the educational value of plastics and ENT live and or pre-recorded surgical events. They found that participants consistently reported that live events were of more educational value than pre-recorded videos. Participants felt that they acquired practical tips which they can apply to their own practice to a greater extent than in pre-recorded videos. Also, the interactive nature of the live surgery meant that they were more alert and engaged throughout. In contrast, Legemate et al. explored the views of urologists and participants in an educational event where LBSP was used, as well as pre-recorded unedited videos. Participants felt overall the education value was similar and a substantial percentage of the surgeons performing the LBSP reported that they felt that live surgery did not provide optimal circumstances for patient safety. Therefore, the authors advocated the use of more pre-recorded unedited videos [34].
Patient safety
Patient safety was the main focus of this review and it was addressed by the success of the procedure and or the complication rate. In this review, we found almost one-third of the papers reported inferior outcomes with LBSP such as less favourable oncological outcomes [7], failure to complete the procedure endoscopically (partial success in 35 cases [8.6%] and complete failure in 24 cases [5.9%] as reported by Liao et al.; partial success in 6 cases [12%] and failure in 8 cases [15%], as reported by Ridtitid et al.). In the series reported by Ruiz de Gordejuela et al., 6 patients required early re-operation and at follow-up 11 required revision. These inferior outcomes are noteworthy as they will have impacted significantly on patient care. The lack of success in endoscopic procedures will have resulted in repeat procedures with associated risks and in the case of outcomes reported by A. G. Ruiz de Gordejuela et al., the greater rate of revision surgery and complications will have worsened patient outcome. The greater rate of positive surgical margins should be emphasised as an area of concern as going forward this may adversely affect the oncological outcome for the patient.
These patient safety concerns have led some institutions to ban the use of LBSP in their meetings, such as the American College of Surgeons and the American College of Obstetricians and Gynaecologists. [3] Others such as the Royal Australian and New Zealand College of Ophthalmologists (RANZCO) have advised its use only in exceptional circumstances and have set out a checklist of points to be analysed prior to approval. In all other cases pre-recorded video is the preferred option.
It should be noted that a large proportion of LBSP remains unreported. Therefore, there is no rigorous analysis of patient outcomes and hence the level of patient safety remains unknown in these events. There may also be reluctance to report on events that show inferior patient outcomes. This, along with the availability of alternatives to LBSP, may have discouraged some surgical societies from adopting its use.
These studies highlighted a number of concerns with LBSP which can be of significant impact on patient care and outcome. This highlights the stressing need for formal regulation of LBSP and developing a quality assurance framework that encompass dedicated consenting, maintaining confidentiality as well as a reporting on operative and postoperative outcomes for patients involved in LBSP. Additional, further studies are required to develop objective evaluation of the potential educational values of these events and translate these benefits into a safer environment such as the use of pre-recorded unedited videos to minimise patient harm.
The potential negative impact of live surgery broadcast can be explained by a number of factors including, surgeons, fatigue, operating with unfamiliar teams and equipment in addition to the pressure to perform in front of a large audience.
Khan et al. explored LBSP from the view point of the surgeons performing the procedures. A small proportion of surgeons reported significant anxiety and reduced surgical quality when performing LBSP. This proportion increased significantly when LBSP was being performed in a foreign institution [35]. Finch et al. explored surgeons’ views on the educational value and safety of LBSP verses ‘As-live unedited surgical broadcast’ (ALB). The educational value was felt to be similar between both formats but it was felt there are greater patient safety benefits with ALB. Also of note respondents were significantly less likely to recommend themselves, a relative or friend to be a patient in LBSP [36].
In order to ensure safety at events with LBSP, surgical societies and institutions have published 14 guidelines and frameworks to maximise patient safety. While there are a small number of societies who outright ban LBSP at their meetings [3], a larger proportion note the educational value and advise operating surgeons and physicians to work in the scope of the guidelines in order to uphold patient safety as the priority.
Consent
This review has also compared the outcomes of the 13 original studies against the recommendations from the summary of 14 prior guidelines and position statements. Although there is unanimous agreement among all the published guidelines for the need to have a dedicated consent process for LBSP, this was not the case when the 13 papers were reviewed. This highlighted the need to improve the quality of reporting on the consent process during LBSP, stating the separate risks of being involved in live surgery, the potential added risks such as surgeon distraction and delays due to transmission.
Patient confidentiality
This review has also highlighted an important point related to protection of patients’ confidentiality during LBSP. This was clearly stated in all guidelines but not robustly reported on by the 13 studies. Standardisation of reporting on these important ethical matters in LBSP manuscripts should be an essential requirement to reassure the surgical community that these ethical standards of maintaining patient confidentiality are upheld throughout the LBSP.
Overall, there was a lack of recommendation on standardised approach of reporting on LBSP including the outcomes across the 14 published guidelines and positions statements. This needs to be a requirement in order to evaluate the safety of LBSP. This has been supported by the EAU, which has an established LBSP registry. This includes an application form as well as a check list which incorporates a wide range of requirements such pre-operative checks (selection of surgeon, consent and preparation of the patient), intraoperative (personnel, presence of moderators) and postoperative care (entering outcomes into the EAU live surgery registry, daily dedicated ward round and communication with the operating surgeon if any deviations occur).
This study has a number of limitations. We acknowledge that number of the studies in this review were modest with no randomised controlled trials and have moderate risk of bias in the quality assessment criteria. However, the 13 studies included a considerable sample size with some comparing LBSP to a matched controlled group. Secondly, we acknowledge that not all live surgical procedures broadcast are reported in the literature, which limits the generalisability of this review and the ability to capture key data to analyse the true educational value and safety of LBSP. Additionally, we conducted this review only on English-language studies and relevant articles in other languages may have been missed. Furthermore, most of the included studies did not report on fundamental issues such as measuring the potential educational values vs. the potential risk of LBSP. It was therefore not possible to draw a conclusion based on these reports. Finally, it was not possible in this synthesis to produce a meta-analysis due to the heterogeneity in reporting outcomes and complications among the included studies.
Nevertheless, this review has heightened a number of points in relation to the relevance of LBSP as part of virtual teaching curriculum during and post the pandemic. First, adherence to a high level of standards during LBSP must be maintained during and after the broadcast including maintaining patient confidentiality and reporting on patient outcomes. Secondly, there are logistical issues with conducting LBSP and the educational values must be balanced with those concerns including patient safety and confidentiality. Alternative teaching ways should also be explored such as streaming pre-recorded unedited videos, allowing the audience to see the procedure being performed while also gaining useful insights on how the surgeon deals with unexpected events, while minimising the risk by being outside the environment of a live surgical event. Finally, there is a need to study the role and potential impact of live demonstration on simulation models such as human cadavers, which could enhance the teaching experience without impacting on patient safety.
Conclusions
Live Broadcast of Surgical Procedures can be of educational value but patient safety and outcomes may be compromised. Further research is required to develop a standardised framework of reporting on live surgery and its outcomes from an ethical and patient safety perspective.
Supplementary Information
Below is the link to the electronic supplementary material.
Acknowledgements
To Professor Andrea Pietrabissa for supporting and promoting this project
Funding
There are no financial declarations for this paper.
Declarations
Conflict of interest
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sector.
Disclosures
Authors Mina Awad, Manish Chowdhary, Shady Hermena, Sara El Falaha, Naim Slim and Nader K Francis have no conflicts of interest or financial ties to disclose.
Ethical approval
No ethical approval was deemed necessary, as this was an evaluation study of an educational tool outside clinical settings.
Footnotes
Previous presentations: The data in this paper has, in part, been presented at the following meetings: European Association of Endoscopic Surgery, Virtual Congress June 2020.
Publisher's Note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
- 1.Artibani W, Ficarra V, Challacombe BJ, Abbou CC, Bedke J, Boscolo-Berto R, Brausi M, de la Rosette JJ, Deger S, Denis L, Guazzoni G, Guillonneau B, Heesakkers JP, Jacqmin D, Knoll T, Martínez-Piñeiro L, Montorsi F, Mottrie A, Piechaud PT, Rane A, Rassweiler J, Stenzl A, Van Moorselaar J, Van Velthoven RF, van Poppel H, Wirth M, Abrahamsson PA, Parsons KF. EAU policy on live surgery events. Eur Urol. 2014;66(1):87–97. doi: 10.1016/j.eururo.2014.01.028. [DOI] [PubMed] [Google Scholar]
- 2.Duty B, Okhunov Z, Friedlander J, Okeke Z, Smith A. Live surgical demonstrations: an old, but increasingly controversial practice. Urology. 2012;79(185):e7–11. doi: 10.1016/j.urology.2011.12.037. [DOI] [PubMed] [Google Scholar]
- 3.Brunckhorst O, Challacombe B, Abboudi H, Khan MS, Dasgupta P, Ahmed K. Systematic review of live surgical demonstrations and their effectiveness on training. Br J Surg. 2014;101(13):1637–1643. doi: 10.1002/bjs.9635. [DOI] [PubMed] [Google Scholar]
- 4.Al-Jabir A, Kerwan A, Nicola M, Alsafi Z, Khan M, Sohrabi C, O'Neill N, Iosifidis C, Griffin M, Mathew G, Agha R. Impact of the Coronavirus (COVID-19) pandemic on surgical practice - Part 1. Int J Surg. 2020;79:168–179. doi: 10.1016/j.ijsu.2020.05.022. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. BMJ. 2021;372:71. doi: 10.1136/bmj.n71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Ogaya-Pinies G, Abdul-Muhsin H, Palayapalayam-Ganapathi H, Bonet X, Rogers T, Rocco B, Coelho R, Hernandez-Cardona E, Jenson C, Patel V. Safety of live robotic surgery: results from a single institution. Eur Urol Focus. 2019;5(4):693–697. doi: 10.1016/j.euf.2017.08.004. [DOI] [PubMed] [Google Scholar]
- 7.Ramírez-Backhaus M, Bertolo R, Mamber A, Ferrer ÁG, Mir MC, Rubio-Briones J. Live surgery for laparoscopic radical prostatectomy-does it worsen the outcomes? A single-center experience. Urology. 2019;123:133–139. doi: 10.1016/j.urology.2018.10.001. [DOI] [PubMed] [Google Scholar]
- 8.Ruiz de Gordejuela AG, Ramos AC, Neto MG, Nora M, Torres García AJ, Sánchez Pernaute A, Gebelli JP. Live surgery courses: retrospective safety analysis after 11 editions. Surg Obes Relat Dis. 2018;14(3):319–324. doi: 10.1016/j.soard.2017.12.008. [DOI] [PubMed] [Google Scholar]
- 9.Mullins JK, Borofsky MS, Allaf ME, Bhayani S, Kaouk JH, Rogers CG, Hillyer SP, Kaczmarek BF, Tanagho YS, Stifelman MD. Live robotic surgery: are outcomes compromised? Urology. 2012;80(3):602–607. doi: 10.1016/j.urology.2012.03.050. [DOI] [PubMed] [Google Scholar]
- 10.Itam S, Pakzad M, Hamid R, Ockrim J, Vashisht A, Cutner A, Greenwell T. Female urology and urogynecology: the outcome of patients participating in live surgical broadcasts. Female Pelvic Med Reconstr Surg. 2020;26(9):554–557. doi: 10.1097/SPV.0000000000000634. [DOI] [PubMed] [Google Scholar]
- 11.Eliyahu S, Roguin A, Kerner A, Boulos M, Lorber A, Halabi M, Suleiman M, Nikolsky E, Rispler S, Beyar R. Patient safety and outcomes from live case demonstrations of interventional cardiology procedures. JACC Cardiovasc Interv. 2012;5(2):215–224. doi: 10.1016/j.jcin.2011.09.023. [DOI] [PubMed] [Google Scholar]
- 12.Schmit A, Lazaraki G, Hittelet A, Cremer M, Le Moine O, Devière J. Complications of endoscopic retrograde cholangiopancreatography during live endoscopy workshop demonstrations. Endoscopy. 2005;37(8):695–699. doi: 10.1055/s-2005-870137. [DOI] [PubMed] [Google Scholar]
- 13.Liao Z, Li ZS, Leung JW, Zhang X, Zhang ST, Ji M, Fan ZN, Zhi FC, Li YM, Chen XX, Lu L, Ren X, Jia GF, Huang LY, Lv NH, Xie WF, Ge ZZ, Chao WS. ERCP Live Demonstration and Education Study Group How safe and successful are live demonstrations of therapeutic ERCP? A large multicenter study. Am J Gastroenterol. 2009;104(1):47–52. doi: 10.1038/ajg.2008.39. [DOI] [PubMed] [Google Scholar]
- 14.Ridtitid W, Rerknimitr R, Treeprasertsuk S, Kongkam P, Khor CJ, Kullavanijaya P. Outcome of endoscopic retrograde cholangiopancreatography during live endoscopy demonstrations. Surg Endosc. 2012;26(7):1931–1938. doi: 10.1007/s00464-011-2130-2. [DOI] [PubMed] [Google Scholar]
- 15.Franke J, Reimers B, Scarpa M, Span S, Thieme M, Wunderlich N, Scheinert D, Sievert H. Complications of carotid stenting during live transmissions. JACC Cardiovasc Interv. 2009;2(9):887–891. doi: 10.1016/j.jcin.2009.06.013. [DOI] [PubMed] [Google Scholar]
- 16.Seeburger J, Diegeler A, Dossche K, Lange R, Mohr FW, Schreiber C, Vanermen H, Falk V. Live broadcasting in cardiac surgery does not increase the operative risk. Eur J Cardiothorac Surg. 2011;40(2):367–371. doi: 10.1016/j.ejcts.2010.11.069. [DOI] [PubMed] [Google Scholar]
- 17.Legemate JD, Zanetti SP, Baard J, Kamphuis GM, Montanari E, Traxer O, de la Rosette JJ. Outcome from 5-year live surgical demonstrations in urinary stone treatment: are outcomes compromised? World J Urol. 2017;35(11):1745–1756. doi: 10.1007/s00345-017-2050-4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.Rocco B, Grasso AAC, De Lorenzis E, Davis JW, Abbou C, Breda A, Erdogru T, Gaston R, Gill IS, Liatsikos E, Oktay B, Palou J, Piéchaud T, Stolzenburg JU, Sun Y, Albo G, Villavicencio H, Zhang X, Disanto V, Emiliozzi P, Pansadoro V. Live surgery: highly educational or harmful? World J Urol. 2018;36(2):171–175. doi: 10.1007/s00345-017-2118-1. [DOI] [PubMed] [Google Scholar]
- 19.Cotton PB, Eisen G, Romagnuolo J, Vargo J, Baron T, Tarnasky P, Schutz S, Jacobson B, Bott C, Petersen B. Grading the complexity of endoscopic procedures: results of an ASGE working party. Gastrointest Endosc. 2011;73:868–874. doi: 10.1016/j.gie.2010.12.036. [DOI] [PubMed] [Google Scholar]
- 20.Royal College of Surgeons of England. Live Surgery Broadcasts Position Statement. http://www.rcseng.ac.uk/publications/docs/live-surgery-broadcasts-position-statement
- 21.Sade RM (2008) American Association for Thoracic Surgery Ethics Committee; Society of Thoracic Surgeons Standards and Ethics Committee. Broadcast of surgical procedures as a teaching instrument in cardiothoracic surgery. Ann Thorac Surg. 86(2):357–61 [DOI] [PubMed]
- 22.Japanese Society for Cardiovascular Surgery. Guidelines to Live Presentations of Thoracic and Cardiovascular Surgery. https://plaza.umin.ac.jp/~jscvs/guidelines-to-live-presentation-2/
- 23.Dehmer GJ, Douglas JS Jr, Abizaid A, Berg JW, Day J, Hall R, Leon MB, Hijazi ZM, Marchlinski F, Park SJ, Popma JJ (2010) Society for Cardiovascular Angiography and Interventions; American College of Cardiology Foundation; Heart Rhythm Society; European Society of Cardiology; Sociedad Latinoamericana de Cardiología Intervencionista; Asian Pacific Society of Interventional Cardiology; Mended Hearts, Inc. SCAI/ACCF/HRS/ESC/SOLACI/APSIC statement on the use of live case demonstrations at cardiology meetings: assessments of the past and standards for the future. J Am Coll Cardiol. 56(15):1267–82. [DOI] [PubMed]
- 24.Carr-Locke DL, Gostout CJ, Van Dam J. A guideline for live endoscopy courses: an ASGE White Paper. Gastrointest Endosc. 2001;53(6):685–688. doi: 10.1067/mge.2001.114413. [DOI] [PubMed] [Google Scholar]
- 25.Devière J, Ponchon T, Beilenhoff U, Neuhaus H, Costamagna G, Schmit A, Kruse A, Spicak J, Nowak A (2003) Recommendations of the ESGE workshop on Ethical-Legal Issues Concerning Live Demonstrations in Digestive Endoscopy. First European Symposium on Ethics in Gastroenterology and Digestive Endoscopy, Kos, Greece, June. Endoscopy 35(9):765–7 [DOI] [PubMed]
- 26.Dinis-Ribeiro M, Hassan C, Meining A, Aabakken L, Fockens P (2015) European Society of Gastrointestinal Endoscopy. Live endoscopy events (LEEs): European Society of Gastrointestinal Endoscopy Position Statement - Update 2014. Endoscopy 47(1):80–6 [DOI] [PubMed]
- 27.Royal Australian College of Surgeons. Live transmission of surgery (2016). https://www.surgeons.org/en/about-racs/position-papers/live_transmission_of_surgery_2016
- 28.Organisation Mondiale d’Endoscopie Digestive. OMED Recommendations for the Ethical Performance of Live Endoscopy Demonstrations. http://www.worldendo.org/wp-content/uploads/2016/03/omed_guideline_ethics.pdf
- 29.Loren DE, Azar R, Charles RJ, Dumot JA, Farooq F, Gopal DV, Jaffe DL, Shami VM, Sharma VK, Chak A. (2010) ASGE CME Programs Committee. Updated guidelines for live endoscopy demonstrations. Gastrointest Endosc. 71(7):1105–7 [DOI] [PubMed]
- 30.Farb A, Zuckerman B. Live case demonstration of interventional cardiology procedures: a regulatory perspective. JACC Cardiovasc Interv. 2012;5(2):225–227. doi: 10.1016/j.jcin.2011.11.006. [DOI] [PubMed] [Google Scholar]
- 31.The Royal Australian and New Zealand College of Opthalmologists. Live transmission of surgery. 2013. https://ranzco.edu/wp-content/uploads/2018/11/POSITION-STATEMENT-live-transmission-of-surgery.pdf
- 32.American Academy of Opthalmology. Advisory Opinion - Live Surgery. 2020. https://www.aao.org/ethics-detail/advisory-opinion-live-surgery
- 33.Skouras G, Skouras A, Skoura E (2021) Evaluation of Live Surgery Meetings: Our Experience with the "Live Makeover Aesthetic Surgery Symposium". Plast Reconstr Surg Glob Open. 9(1):e3350 [DOI] [PMC free article] [PubMed]
- 34.Legemate JD, Zanetti SP, Freund JE, Baard J, de la Rosette JJMCH. Surgical teaching in urology: patient safety and educational value of 'LIVE' and 'SEMI-LIVE' surgical demonstrations. World J Urol. 2018;36(10):1673–1679. doi: 10.1007/s00345-018-2291-x. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Khan SA, Chang RT, Ahmed K, Knoll T, van Velthoven R, Challacombe B, Dasgupta P, Rane A. Live surgical education: a perspective from the surgeons who perform it. BJU Int. 2014;114(1):151–158. doi: 10.1111/bju.12283. [DOI] [PubMed] [Google Scholar]
- 36.Finch W, Masood J, Buchholz N, Turney BW, Smith D, Wiseman O. Would You Want to Be the Patient? "Live Surgical Broadcast" or "As-Live Unedited Surgical Broadcast". J Endourol. 2015;29(7):821–829. doi: 10.1089/end.2014.0580. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.