Abstract
Young children (0–4 years) represent the next population in whom the SARS-CoV-2 (COVID) vaccine will be available. Addressing parental feelings about vaccination will be important to optimize uptake. In this study, online surveys were administered in 78 perinatal women in the Northeast United States (Vermont) between January and July 2021. Women reported vaccine intention by indicating their plans to have their child vaccinated. Response choices included vaccinate as soon as possible, vaccinate but not immediately, or no intention to vaccinate. Subsequently, women rated their readiness to vaccinate children if offered the COVID vaccine tomorrow on an 11-point scale from 0 (definitely not get the vaccine) to 10 (definitely get the vaccine). Factors influencing ratings were measured categorically. General vaccine hesitancy was measured with the Parent Attitudes about Childhood Vaccinations scale. While many individual participants changed readiness to vaccinate children between baseline and follow-up; readiness in the study cohort remained unchanged. Approximately 50% of participants were likely to have their young children vaccinated. Concerns about vaccine safety was the largest driver of hesitancy. Importantly, even in a cohort highly adherent to childhood vaccines, hesitancy toward general childhood vaccines predicted decreased readiness for young children to receive the COVID vaccine. Our data provide evidence that maternal attitudes about the COVID vaccine are not fixed but overall readiness remains low, that prior adherence to childhood vaccine schedules will not predict vaccine behavior related to the COVID vaccine, and that public health messaging should emphasize messaging targeting vaccine safety in children.
Abbreviations: PACV, Parent Attitudes about Childhood Vaccinations; COVID, SARS-CoV-2
Keywords: COVID-19, COVID vaccine, Vaccine hesitancy, Childhood vaccination, COVID-19 vaccine
1. Introduction
Since COVID (SARS-CoV-2) appeared in the United States, >79 million cases, and 970,000 deaths have been attributed to COVID infection (March 23,2022) (Johns Hopkins University). The impact on children is not yet clear, however a recent study by Kim et al reports young children (0–4 years) with COVID were hospitalized more frequently than older children (Kim et al., 2021). Approval of the COVID vaccine in older children and the Delta and Omicron variants have significantly increased the burden experienced by the youngest children, not yet eligible for vaccination (Marks et al., 2022a, Marks et al., 2022b). In fact, hospitalization rates in this population reached 15.4 per 100,000 during the Omicron surge, 5 times higher than during the Delta wave (Marks et al., 2022b). Hospitalization rates in 5–11 year olds and 12–18 year olds also increased during the Omicron wave (2.4 and 5.9 per 100,000 respectively) but remained lower than those of the youngest children (Marks et al., 2022b).
Ample evidence supports COVID vaccination in children to decrease hospitalization. For example, the Center for Disease Control data shows unvaccinated children 5–11 are three times as likely to require hospitalization than those who are fully vaccinated. Similarly, infected adolescents are twice as likely to require hospitalization if they are unvaccinated. Although vaccination rates in eligible children have been increasing, overall they remain low; approximately 60% in adolescents and 30% in children 5–11 years (April 2022) (Hamel et al., 2021, Mayo Foundation for Medical Education and Research., 2022).
Kelly et al. reported high intention to vaccinate children (73%) in April 2020, however more recent reports indicate less than half of parents’ intend to vaccinate their children against COVID(Kelly et al., 2021, Ruggiero et al., 2021). Longitudinal data on parental attitudes toward COVID vaccination for young children are lacking; but fluctuations in the pandemic, and vaccine messaging will likely have an impact on parental vaccine hesitancy. Thus, we sought to examine factors associated with intention and readiness to vaccinate children across two timepoints in the pandemic.
2. Methods
2.1. Study population
In June 2020, women who received obstetric care at University of Vermont Medical Center were enrolled in a longitudinal study assessing the effects of COVID on perinatal women and their children. Eligible women were 18 or older, pregnant, or had an infant 6 months old or younger. Participants were recruited if they indicated interest in research studies or if they met inclusion criteria by medical record review. Potential participants were ed a study description and link to consent information. Overall enrollment rate was approximately 10%. Between January 2021 and February 2021 participants completed an online baseline assessment of general vaccine hesitancy and beliefs about administering the COVID vaccine to children. An online follow-up assessment was administered 5 months later.
All aspects of the study were approved by the University of Vermont Institutional Review Board. Participants provided informed consent prior to data collection.
2.2. Measures
Vaccine hesitancy was assessed with the Parent Attitudes about Childhood Vaccinations (PACV) (Opel et al., 2011a, Opel et al., 2013). The PACV measures hesitancy toward typical childhood vaccinations. Specific measures include perceptions of severity of vaccine preventable disease, benefits of vaccination, susceptibility toward preventable diseases and barriers to vaccination (Opel et al., 2011a). Women who were pregnant with their first child did not complete the PACV.
Intention to vaccinate children was assessed with the question: “Which of the following applies to your plans about the COVID vaccine for your child(ren)?” Response options were “I plan on getting the COVID vaccine … as soon as it is available to them,” “…but after other children” and “I do not plan on getting the COVID vaccine for my children”.
Readiness to vaccinate children was measured with the question “If you were offered the COVID vaccine tomorrow, what would you do?” Participants indicated their readiness on a visual analog scale with 0 “I definitely would not get the vaccine” and 10 “I would definitely get the vaccine” labeled.
Participants indicated the biggest factor driving the rating of their intentions and rated their worry about their children contracting COVID. Responses included “I am concerned about my child getting very sick,” “I want to protect my family against COVID,” “I want to be able to normalize their social life,” “I am concerned about the side effects,” “I don’t think it will protect them against COVID,” “They have already had COVID,” and “Other.”.
For statistical analysis, women who rated their readiness to have their child vaccinated against COVID as 7 or greater were considered “likely” to have their children vaccinated, those with readiness scores between 3 and 6 were “unsure” and those with scores less than 3 considered “unlikely.” For examination of readiness over time, those who were likely to have their children vaccinated at follow-up (or both baseline and follow-up) were considered “stayed high or increased”,while “stayed low or decreased” describes participants who were persistently unlikely or unsure or who decreased from likely on the follow-up survey.
2.3. Statistical analysis
The PACV was scored per validation studies; scores >50 represent vaccine hesitancy (Opel et al., 2011b). A two-sided paired t-test was calculated on baseline vs follow-up readiness score. Frequencies and descriptive statistics were calculated with chi square and t-tests comparing between the groups.
Univariate logistic regression was used to assess associations between vaccine readiness and demographic variables, worry about COVID and PACV score. Then stepwise logistic regression was completed using demographic and predictor variables to establish the best fit model predicting readiness for vaccination.
3. Results
78 women participated in the vaccine survey at both baseline and follow-up; mean age was 33 years (SD = 4.0). 81% of participants had a 4-year degree or higher, and 95% were white (Table 1).
Table 1.
Univariate analyses of demographic and predictor variables by readiness to vaccinate children.
| Total population | Persistently low, or decreased readiness to have children vaccinated | Persistently high or increased readiness to have children vaccinated | Significance | ||||
|---|---|---|---|---|---|---|---|
| N | 78 |
38 |
40 |
||||
| Mean or N | SD or % | Mean or N | SD or % | Mean or N | SD or % | ||
| Maternal age | 33 | 4 | 31 | 3 | 35 | 4 | <0.001 |
| Income | 0.187 | ||||||
| <$30,000 | 6 | 8% | 4 | 11% | 2 | 5% | |
| $30-$59,999 | 15 | 19% | 11 | 29% | 4 | 10% | |
| $60-$99,999 | 28 | 36% | 12 | 32% | 16 | 40% | |
| $100-$140,000 | 19 | 24% | 7 | 18% | 12 | 30% | |
| >$140,000 | 10 | 13% | 4 | 10% | 6 | 15% | |
| Education | 0.001 | ||||||
| <4 year degree | 15 | 19% | 13 | 34% | 2 | 5% | |
| 4 year degree | 30 | 39% | 15 | 39% | 15 | 38% | |
| >4 year degree | 33 | 42% | 10 | 26% | 23 | 57% | |
| Baby age at follow-up (weeks) | 48 | 18 | 50 | 16 | 46 | 19 | 0.279 |
| Baby age at baseline (weeks) | 27 | 18 | 29 | 16 | 25 | 19 | 0.3134 |
| Vaccination status at follow-up | 0.001 | ||||||
| unvaccinated | 13 | 17% | 12 | 32% | 1 | 3% | |
| vaccinated | 65 | 83% | 26 | 68% | 39 | 97% | |
| PACV† score | 10 | 13 | 17 | 16 | 4 | 6 | <0.001 |
*N = 71, Only 3 participants scored >50, the lower threshold representing vaccine hesitancy †PACV: Parent Attitudes about Child Vaccinations.
3.1. Vaccine behaviors
The majority of participants believed general vaccines are safe, and only 10% had ever delayed a childhood vaccine for a reason other than illness. The mean PACV score was 10, well below the threshold indicating vaccine hesitancy. Even so, PACV score was correlated with women’s readiness to vaccinate their children (correlation coefficient −0.50, p value < 0.001 for both survey timepoints).
3.2. Intentions
At baseline, 42% of women intended to have their children vaccinated as soon as the vaccine was available. At follow-up 5 months later, this proportion increased to 49%. Those who did not intend to have their children vaccinated decreased minimally between the two timepoints (22% baseline vs 20% follow-up). Lastly, those who intended to wait until other children received the COVID vaccine decreased from baseline to follow-up. None of these small differences met statistical significance.
3.3. Readiness
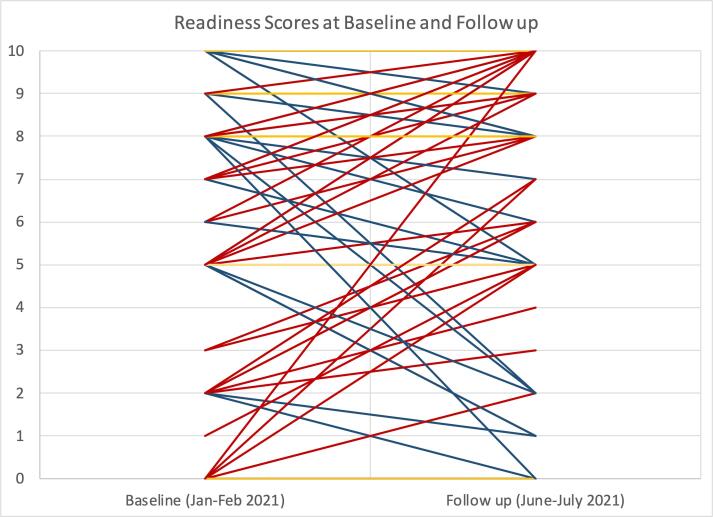
The mean readiness score was not statistically different between timepoints (5.2 baseline vs 5.9 follow-up; p = 0.065; dRM (−0.06 to 0.57). At baseline 45% of participants were likely to have children vaccinated, 23% unsure, and 32% unlikely; compared to 51%, 22% and 27% respectively at follow-up. Though change in readiness across the study population was not significantly different, many participants changed their rating between timepoints (Fig. 1).
Fig. 1.
Participant ratings of readiness to vaccinate children at baseline and follow-up. Above, red lines represent increased readiness, blue lines represent decreased, yellow are stable reediness scores. Lines represent baseline/follow-up pairs which exist in the data at least once to depict the diversity of change in readiness between the timepoints. However, mean scores at both timepoints are not significantly different. (For interpretation of the references to colour in this figure legend, the reader is referred to the web version of this article.)
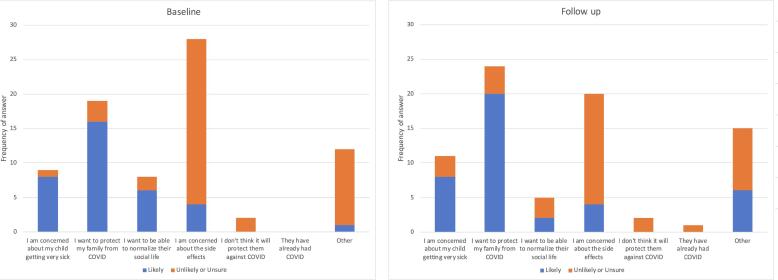
3.4. Factors driving readiness
In both time periods, women who were unsure or unlikely to have their children vaccinated overwhelmingly reported concern about vaccine side effects was driving their decision. In contrast, most participants who were likely to have their children vaccinated indicated wanting to protect their family from COVID as the driving factor (Fig. 2).
Fig. 2.
Driving Factors of Readiness Rating at Baseline and Follow-up by Likelihood of Having Children Vaccinated. Between baseline and follow-up, concern about children getting very sick and desire to protect one’s family from COVID increased, particularly among those likely to vaccinate children. Simultaneously, concern about the side effects decreased at follow-up, but remained the most common factor driving readiness rating among those unsure or unlikely to have children vaccinated.
3.5. Predicting readiness to vaccinate children
The final model predicting participants readiness to vaccinate children included maternal age and PACV score only. Education level, concern about children contracting COVID, household income, infant age, and maternal vaccination status at follow-up did not improve the model. The final model indicated higher maternal age (OR 1.42 (1.14–1.77); p = 0.002) and lower PACV scores (OR 0.86 (0.77–0.95); p = 0.002) were associated with increased readiness to vaccinate children.
4. Discussion
Our results demonstrate persistently low readiness to have children vaccinated against COVID among mothers with low vaccine hesitancy toward childhood vaccinations. Though many individuals changed their intention and readiness between timepoints, the overall readiness of the study cohort remained around 50%. This is consistent with cross-sectional surveys of parents in the winter of 2020–21 (Ruggiero et al., 2021, Szilagyi et al., 2021). It is also similar to the current vaccination rates (as of April 2022) in eligible adolescents (60%) and higher than vaccination rates in children 5–11 (30%) (Hamel et al., 2021, Mayo Foundation for Medical Education and Research., 2022). Although our study takes place before the appearance of the Omicron variants, 80% of parents of unvaccinated children report the Omicron variant does not impact their likelihood to have their child vaccinated (Hamel et al., 2021). Studies prior to the Omicron variants estimated 50–80% of the population would need to be immune for herd immunity to prevent transmission (Omer et al., 2020, Sanche et al., 2020). The increased transmissibility of Omicron variants means that herd immunity will require even higher rates of immune individuals (Liu & Rocklov, 2022). Therefore, current rates of intention to vaccinate are lower than necessary to have a lasting impact.
Our study adds longitudinal measurement to literature on parent’s attitudes toward the COVID vaccine. Our baseline survey was conducted prior to widespread availability of the COVID vaccine in adults, while at the second timepoint all participants were eligible for vaccines themselves. However, vaccine readiness overall was stable indicating improved vaccine messaging and/or penetration is needed. Surprisingly 2/3rd of those with low scores of readiness were vaccinated themselves, therefore public health messaging will likely need to specifically address benefits and safety of COVID vaccines in children.
Similar to prior studies, concern about side effects was reported as the major factor driving vaccine hesitancy. This sample of mothers were particularly compliant with childhood vaccines, suggesting prior vaccine adherence does not predict readiness to accept the COVID vaccine. Even among this highly adherent population, PACV scores were strongly predictive of persistent or increasing readiness to have children vaccinated. It appears even low levels of mistrust, or hesitation related to childhood vaccines influences feelings related to COVID vaccines. Therefore, though COVID specific messaging is necessary, strategies used to improve childhood vaccine adherence generally may have a role in messaging about the COVID vaccine. Lastly, maternal age was the strongest predictor of vaccine readiness suggesting outreach optimized for younger mothers will be important.
With any study related to COVID, context is key. This study occurred in Vermont before and after widespread availability of adult COVID vaccines. Vermont had the highest vaccination rates in the country during the follow-up period with 66–69% of all Vermonters being fully vaccinated between July and August 2021 (Mathieu et al., 2021). We do not believe our data to be generalizable across the country, but instead represent a “best case scenario.” Therefore, the findings of persistently low levels of intention and readiness to vaccinate young children are striking and suggest achieving high vaccine coverage for young children nationwide will require significant effort.
4.1. Limitations
The study was primarily white, vaccine compliant, highly educated women. Future work will need to examine vaccine hesitancy in more diverse populations as previous studies have shown variability based on sociodemographic factors (Szilagyi et al., 2021). The sample size is modest, introducing the potential to fail to reject null hypotheses. Though our data did not demonstrate a statistical difference in readiness score between timepoints, the effect size confidence interval is wide. Most would consider the upper limit (0.57) a “subtle” effect (Goulet-Pelletier & Cousineau, 2018); therefore, we feel our results do not represent meaningful change between timepoints. Lastly, we were not able to measure other influential factors related to vaccine readiness and hesitancy including social media consumption, which has been shown to impact vaccine hesitancy (Wilson & Wiysonge, 2020). Considering these limitations, there may be even lower readiness to vaccinate children against COVID among a heterogenous population, further emphasizing the importance of continued efforts to reach parents, particularly of young children.
4.2. Conclusion
In sum, our data raise concerns about women’s current intentions to have children vaccinated against COVID. If overall vaccine readiness is similar to our population, the population at large will be far below vaccination rates needed to achieve herd immunity. However, our data also demonstrate women have changed their opinions about vaccination, some becoming less ready while others increased readiness. Therefore, one should not assume attitudes about COVID vaccinations are entrenched. It is well known that Pediatricians represent one of the most trusted sources of information related to vaccines, however most parents have yet to talk with their physician about the COVID vaccine (Kaiser Family Foundation, 2021). As we have yet to see increases in overall readiness with current messaging strategies, it is critical for pediatric providers to talk with families about the COVID vaccine, even for those in whom it is not yet approved.
Disclosures
The authors have no conflicts of interest relevant to this article to disclose. Study sponsors were not involved in the study design, data collection, analysis or interpretation of the data, nor in the writing or submitting of the manuscript. The first draft was completed by Dr. Cioffredi, the corresponding author.
Funding sources
This work was supported by the National Institutes of Health: [grant numbers: R34DA050283-01S; UG1OD024955, P20 GM103644], and The Children’s Miracle Network. The authors listed include all team members who have significantly contributed to the work.
CRediT authorship contribution statement
Leigh-Anne Cioffredi: Conceptualization, Methodology, Formal analysis. Kaelyn L. Kohlasch: Investigation, Data curation. Elina Thomas: Data curation. Alexandra S. Potter: Project administration, Funding acquisition, Supervision.
Declaration of Competing Interest
The authors declare that they have no known competing financial interests or personal relationships that could have appeared to influence the work reported in this paper.
References
- Goulet-Pelletier J.-C., Cousineau D. A review of effect sizes and their confidence intervals, Part I: The Cohen’sd family. Quantitative Methods Psychol. 2018;14(4):242–265. [Google Scholar]
- Hamel L., Kirzinger A., Lopes L., Kearney A., Sparks G., Brodie M. Kaiser Family Foundation; 2021. KFF COVID-19 vaccine monitor: January 2021. [Google Scholar]
- Johns Hopkins University. COVID-19 United States Cases by County Johns Hopkins University. Retrieved Sept 9, 2021 from https://coronavirus.jhu.edu/us-map.
- Kaiser Family Foundation. (2021). KFF COVID-19 Vaccine Monitor: Parents and the Pandemic. https://www.kff.org/coronavirus-covid-19/poll-finding/kff-covid-19-vaccine-monitor-parents-and-the-pandemic/.
- Kelly B.J., Southwell B.G., McCormack L.A., Bann C.M., MacDonald P.D.M., Frasier A.M., Bevc C.A., Brewer N.T., Squiers L.B. Predictors of willingness to get a COVID-19 vaccine in the U.S. BMC Infect. Dis. 2021;21(1):338. doi: 10.1186/s12879-021-06023-9. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Kim T.Y., Kim E.C., Agudelo A.Z., Friedman L. COVID-19 hospitalization rate in children across a private hospital network in the United States: COVID-19 hospitalization rate in children. Arch. Pediatr. 2021;28(7):530–532. doi: 10.1016/j.arcped.2021.07.004. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Liu Y., Rocklov J. The effective reproduction number for the omicron SARS-CoV-2 variant of concern is several times higher than Delta. J. Travel Med. 2022 doi: 10.1093/jtm/taac037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks K.J., Whitaker M., Agathis N.T., Anglin O., Milucky J., Patel K., Pham H., Kirley P.D., Kawasaki B., Meek J., Anderson E.J., Weigel A., Kim S., Lynfield R., Ropp S.L., Spina N.L., Bennett N.M., Shiltz E., Sutton M., Talbot H.K., Price A., Taylor C.A., Havers F.P., Roland J., Surgnier J., Lyons C., Openo K., Teno K., Kohrman A., Bye E., Cline C., Muse A., Cafferky V., Billing L., Abdullah N., Schaffner W., McCaffrey K. Hospitalization of infants and children aged 0–4 years with laboratory-confirmed COVID-19—COVID-NET, 14 States, March 2020–February 2022. MMWR Morb. Mortal. Wkly. Rep. 2022;71(11):429–436. doi: 10.15585/mmwr.mm7111e2. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Marks K.J., Whitaker M., Anglin O., Milucky J., Patel K., Pham H., Chai S.J., Kirley P.D., Armistead I., McLafferty S., Meek J., Yousey-Hindes K., Anderson E.J., Openo K.P., Weigel A., Henderson J., Nunez V.T., Como-Sabetti K., Lynfield R., Ropp S.L., Smelser C., Barney G.R., Muse A., Bennett N.M., Bushey S., Billing L.M., Shiltz E., Abdullah N., Sutton M., Schaffner W., Talbot H.K., Chatelain R., George A., Taylor C.A., McMorrow M.L., Perrine C.G., Havers F.P., Reingold A., Alden N., Kawasaki B., Correa M., Lyons C., Fawcett E., Ward K., Bilski K., Bye E., Hancock E.B., Khalifa M., Rowe A., Spina N., Cafferky V., Popham K., Hawkins S., Markus T., McCaffrey K., Price A. Hospitalizations of children and adolescents with laboratory-confirmed COVID-19 — COVID-NET, 14 States, July 2021–January 2022. MMWR Morb. Mortal. Wkly. Rep. 2022;71(7):271–278. doi: 10.15585/mmwr.mm7107e4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mathieu E., Ritchie H., Ortiz-Ospina E., Roser M., Hasell J., Appel C., Giattino C., Rodes-Guirao L. A global database of COVID-19 vaccinations. Nat. Hum. Behav. 2021;5(7):947–953. doi: 10.1038/s41562-021-01122-8. [DOI] [PubMed] [Google Scholar]
- Mayo Foundation for Medical Education and Research. (2022). U.S. COVID-19 vaccine tracker: See your state’s progress. Mayo Foundation for Medical Education and Research. Retrieved April 6, 2022 from https://www.mayoclinic.org/coronavirus-covid-19/vaccine-tracker.
- Omer S.B., Yildirim I., Forman H.P. Herd immunity and implications for SARS-CoV-2 control. JAMA. 2020;324(20):2095–2096. doi: 10.1001/jama.2020.20892. [DOI] [PubMed] [Google Scholar]
- Opel D.J., Mangione-Smith R., Taylor J.A., Korfiatis C., Wiese C., Catz S., Martin D.P. Development of a survey to identify vaccine-hesitant parents: the parent attitudes about childhood vaccines survey. Hum. Vaccin. 2011;7(4):419–425. doi: 10.4161/hv.7.4.14120. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Opel D.J., Taylor J.A., Mangione-Smith R., Solomon C., Zhao C., Catz S., Martin D. Validity and reliability of a survey to identify vaccine-hesitant parents. Vaccine. 2011;29(38):6598–6605. doi: 10.1016/j.vaccine.2011.06.115. [DOI] [PubMed] [Google Scholar]
- Opel D.J., Taylor J.A., Zhou C., Catz S., Myaing M., Mangione-Smith R. The relationship between parent attitudes about childhood vaccines survey scores and future child immunization status: a validation study. JAMA Pediatr. 2013;167(11):1065–1071. doi: 10.1001/jamapediatrics.2013.2483. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Ruggiero K.M., Wong J., Sweeney C.F., Avola A., Auger A., Macaluso M., Reidy P. Parents' intentions to vaccinate their children against COVID-19. J. Pediatr. Health Care. 2021;35(5):509–517. doi: 10.1016/j.pedhc.2021.04.005. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Sanche S., Lin Y.T., Xu C., Romero-Severson E., Hengartner N., Ke R. High contagiousness and rapid spread of severe acute respiratory syndrome coronavirus 2. Emerg. Infect. Dis. 2020;26(7):1470–1477. doi: 10.3201/eid2607.200282. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Szilagyi P.G., Shah M.D., Delgado J.R., Thomas K., Vizueta N., Cui Y., Vangala S., Shetgiri R., Kapteyn A. Parents' intentions and perceptions about COVID-19 vaccination for their children: results from a national survey. Pediatrics. 2021 doi: 10.1542/peds.2021-052335. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Wilson S.L., Wiysonge C. Social media and vaccine hesitancy. BMJ Glob. Health. 2020;5(10):e004206. doi: 10.1136/bmjgh-2020-004206. [DOI] [PMC free article] [PubMed] [Google Scholar]