Abstract
Objectives
To demonstrate three‐hundred and sixty degrees of maxillary sinus (MS) surgical approaches using cadaveric dissections, highlighting the step‐by‐step anatomy of each procedure.
Methods
Two latex‐injected cadaveric specimens were utilized to perform surgical dissections to demonstrate different approaches to the MS. The procedures were documented with macroscopic images and endoscopic pictures.
Results
Dissections were performed to approach the MS medially (endoscopic maxillary antrostomy and ethmoidectomy), anteriorly (Caldwell–Luc), superiorly (transconjunctival/transorbital approach), inferiorly (transpalatal approach), and posterolaterally (preauricular hemicoronal approach).
Conclusion
A number of approaches have been described to address pathology in the MS. Surgeons should be familiar with indications, limitations, and surgical anatomy from different perspectives to approach the MS. This paper illustrates anatomic approaches to the MS with detailed step‐by‐step cadaveric dissections and case examples.
Keywords: anatomy, Caldwell–Luc, dissection, endoscopic sinus surgery, infratemporal fossa, maxillary sinus, pterygopalatine fossa
Highlights
This paper provides a comprehensive review of surgical approaches to the MS, allowing for three‐hundred and sixty degrees of access, along with detailed step‐by‐step cadaveric dissections.
INTRODUCTION
The maxillary sinus (MS) is the largest of all paired paranasal sinuses and is a central structure for facial growth and formation. It is the first sinus to develop, in the third to fourth month of intrauterine life. 1 The MS is situated inferior to the orbit, superior to the alveolar process of the maxilla and maxillary teeth, posterior to the anterior wall of the maxilla, lateral to the nasal cavity, medial to the infratemporal fossa, and anterior to the pterygopalatine fossa. 1 The primary blood supply and innervation to this region are the internal maxillary artery (IMAX) and trigeminal nerve branches, respectively.
The MS is a key anatomic region for rhinologists, head and neck surgeons, and maxillofacial surgeons. 1 A number of infectious, inflammatory, traumatic, and neoplastic pathologies can affect this anatomic area, frequently requiring surgical intervention. 2 , 3 , 4 , 5 However, the anatomy of this sinus and the surrounding anatomic region can be challenging if not anatomically well‐understood. Although most otolaryngologists are very familiar with the endoscopic maxillary antrostomy, approaches to the MS from other areas are decidedly less familiar. However, depending on the pathology that needs to be addressed, it is imperative for surgeons to be familiar with multiple approaches to the MS to optimally approach a given pathology
The purpose of this study is to demonstrate the anatomic step‐by‐step dissection of five different surgical approaches to the MS from medial, anterior, inferior, superior, and posterolateral. This study illustrates the intimate relationship between the MS and key nearby anatomic landmarks and offers readers the ability to better understand the anatomy in the region and nuances of surgical approaches.
METHODS
Two latex‐injected human head specimens were utilized to perform step‐by‐step dissections to the MS. An embalmed specimen was used for the transconjunctival, preauricular hemicoronal, and Caldwell–Luc (CL) approaches and a fresh cadaver for the endoscopic anterior ethmoidectomy/antrostomy and transpalatal approaches. The steps of each procedure were documented following the previous protocols using photodocumentation techniques for microscopic images and 0‐ and 30‐degree scopes for endoscopic pictures. 6 All data were obtained in accordance with the guidelines of the Committee for Cadaveric use in Research.
RESULTS
The medial wall maxillary antrostomy/anterior ethmoidectomy approach
The medial wall of the MS is located just lateral to the nasal cavity and communicates to the nasal cavity via the natural ostium, just behind the uncinate process. 1
Endoscopic sinus surgery (ESS) comprises one of the most popular approaches in otolaryngology and neurosurgical centers to address inflammatory and neoplastic disease. It allows for a minimally invasive approach with minimal morbidity. 7 This technique is most commonly used for chronic rhinosinusitis, 8 but is also useful for select MS tumors. It can also be expanded to include maxillary mega‐antrostomies, endoscopic medial maxillectomy, and the initial step for a transpterygoid approach. 4 , 9 Although it is a relatively simple procedure, it is important to recognize key steps in the procedure to avoid common mistakes such as incompletely incorporating the natural ostium into the antrostomy or injuring the nasolacrimal duct.
Maxillary antrostomy/anterior ethmoidectomy step‐by‐step dissection (Figure 1)
Figure 1.
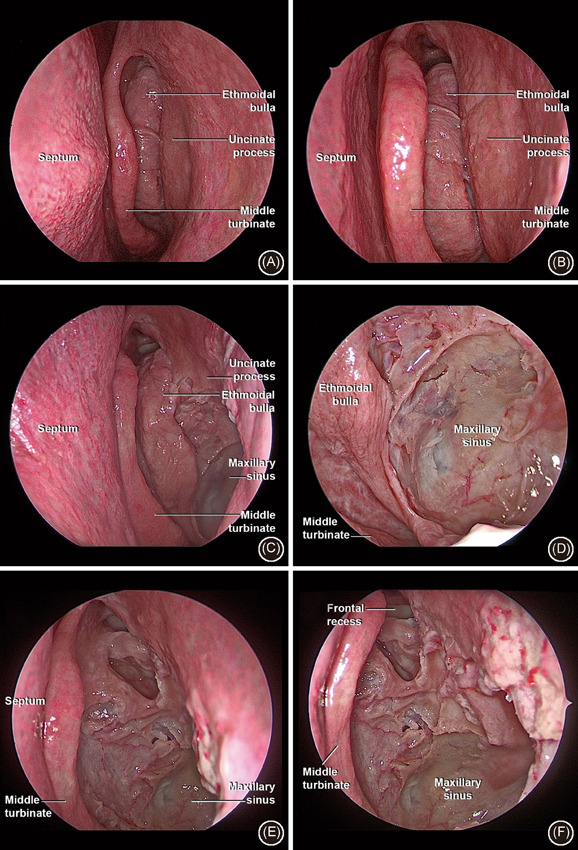
Endoscopic anterior ethmoidectomy (antrostomy) approach. (A) Endoscopic overview of the left nasal cavity and middle meatus; (B) medialization of middle turbinate with better visualization of ethmoid bulla; (C) immediately after completion of uncinectomy and initial expansion of the antrostomy; (D) further enlargement of the antrostomy posteriorly to connect the natural and any accessory ostium of MS; (E) complete removal of bulla; (F) overview of final aspect of maxillary sinus anterior ethmoidectomy
-
1.
Using a 0‐ or 30‐degree endoscope in the nasal cavity, identify the middle meatus between the middle turbinate and the lateral nasal wall.
-
2.
Gentle medialize the middle turbinate with a cottle elevator in the central portion of the turbinate.
-
3.
Identify the edge of the uncinate process, 5–10 mm posterior to the maxillary line.
-
4.
Dissect the uncinate process in a retrograde fashion from its posterior free edge towards its anterior attachment to the nasolacrimal duct.
-
5.
Identify the natural MS ostium, immediately posterior to uncinate process attachment, located in a parasagittal plane.
-
6.
Dilate the natural ostium posteriorly and then expand with through‐cutting instrumentation.
-
7.
Enlarge the antrostomy posteriorly and ensure inclusion of any accessory ostium of the MS. The final appearance is a “pear‐shape” with a larger opening posteriorly and a small opening towards the natural ostium anteriorly.
-
8.
Identify the ethmoid bulla and enter this in the medial and inferior portion using a ball probe at its natural ostium. Further dissection is carried out with Kerrison rongeurs or microdebrider instruments.
-
9.
Identify bulla lumen and completely remove the face of the bulla.
-
10.
Ensure to avoid injury to the anterior ethmoidal artery in the ethmoidal roof, superiorly to the upper extent of the bulla.
-
11.
Figure 2 demonstrates a case example of utilization of the maxillary antrostomy/anterior ethmoidectomy.
Figure 2.
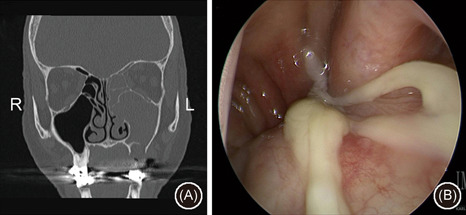
Case example of utilization of maxillary antrostomy and anterior ethmoidectomy for a left‐sided odontogenic sinusitis; (A) coronal noncontrast CT scan demonstrating left‐sided maxillary and anterior ethmoid sinus opacification adjacent to a bony defect on the sinus floor with periapiacal abscess and (b) endoscopic exam demonstrating purulence emanating from the middle meatus and draining into the nasopharynx. CT, computed tomography
The anterior wall and CL (anterior transmaxillary) approach
The anterior wall of the MS is a concave‐shaped surface and contains a bulging in inferolateral portion, referred to as the canine eminence. The anterior wall also contains the infraorbital foramen (IOF), located in the midline of the wall approximately 5–8 mm below to inferior orbital rim. 1
The CL operation was the most common approach for the MS prior the advent of ESS. First described over 100 years ago by Caldwell (1893) and Luc (1897), the CL still remains an excellent option for odontogenic neoplasms, tumors, trauma, as well to pterygopalatine and infratemporal fossa. 10 In the modern era, this approach is especially useful to reach MS neoplasms with anterior attachment points that are difficult to access through an endoscopic medial maxillectomy. It is also a useful adjunct to endoscopic cranial base approaches to allow contralateral access to lateral lesions (contralateral transmaxillary approach) or to allow improved instrument manipulation during endoscopic ipsilateral approaches to Meckel's cave and infratemporal fossa. Lastly, it can be an option to approach pathology in the masticator space or lateral recess of the sphenoid sinus. 7 , 11 , 12
CL (anterior transmaxillary) step‐by‐step dissection (Figure 3)
Figure 3.
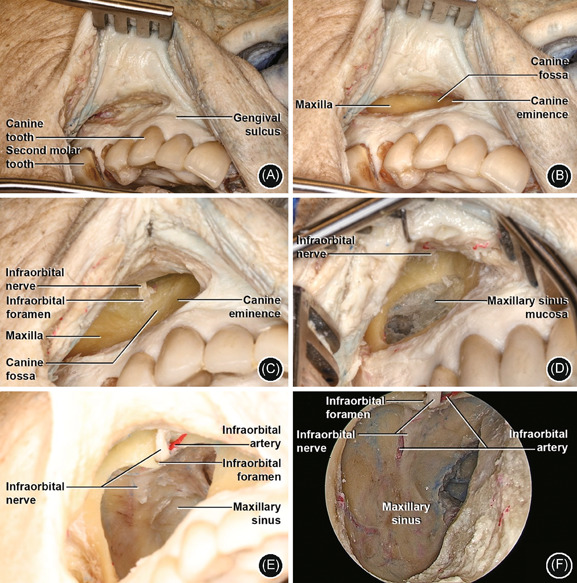
Caldwell–Luc (anterior transmaxillary) approach. (A) Right side: incision between the canine tooth and second molar, about 5 mm above gingival sulcus; (B) detachment of periosteum of maxilla and identification of canine fossa and eminence inferior and medially; (C) identification of IOF and ION in the central‐superior area; (D) window in anterior wall (3 cm diameter) with visualization of maxillary sinus mucosa. ION in central‐superior area; (E) removal of sinus mucosa and opening into the MS cavity. Visualization of ION and IOA; (F) 4 mm 0‐degree endoscope MS anterior view with ION and IOA in the posterior wall. IOA, infraorbital artery; IOF, infraorbital foramen; ION, infraorbital nerve; MS, maxillary sinus
-
1.
Evert the right superior lip and create an incision between the canine tooth and second molar, about 5 mm above gingival sulcus (to facilitate multilayer suture closure at the conclusion of the case).
-
2.
Dissect superiorly in a subperiosteal plane and identify medially the canine fossa and eminence and proceed laterally and superior to it.
-
3.
Continue dissection until the level of the IOF level with clear visualization of the infraorbital nerve (ION).
-
4.
Just below the ION level, open an ample window in the anterior wall of MS (approximately 3 cm of diameter) and remove sinus mucosa. Alternatively, the bony entrance can be carried out under the guidance of intraoperative navigation, ensuring that the entrance is above the dental roots.
-
5.
Following drilling to completely open of the sinus wall, carefully with ION under visualization. Dissection can also be completed with Kerrison rongeurs.
-
6.
0 or 30‐degree endoscopes can then be utilized to provide magnified vision into the sinus to facilitate additional dissection.
-
7.
Figure 4 demonstrates a case example of utilization of the CL technique.
Figure 4.
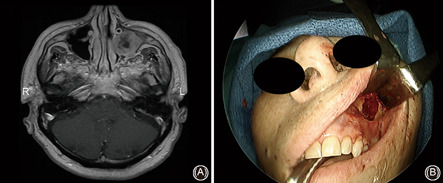
Case example of utilization of a Caldwell–Luc approach; left‐sided maxillary sinus squamous cell carcinoma requiring a combined endoscopic medial maxillectomy and Caldwell–Luc approach; (A) axial T1 postgadolinium MRI scan showing left‐sided maxillary sinus tumor and (B) intraoperative photo demonstrating Caldwell–Luc approach through the anterior wall of the maxillary sinus. MRI, magnetic resonance imaging
The superior wall and transconjunctival approach
The superior wall or “roof” of the MS, synonymous with the orbital floor, contains two notable structures: the ION and infraorbital artery (IOA). As IMAX and the trunk of V2 exits the pterygopalatine fossa, they give off the posterior superior alveolar nerve (PSAN) and posterior superior alveolar artery, respectively. The ION and IOA then continue to run from posterior to anterior in the infraorbital canal (IOC) until the IOF level. The IOC can be variably surrounded by thick or thin bone and can be invested in a layer of periosteum. Therefore, surgeons must be aware of the anatomic variations to avoid possible injuries.
It is also important to highlight the anatomical relationship between the inferior oblique muscle (IOM) and the orbital floor. The IOM differs from all the other extraocular muscles which originate in the common tendinous ring and, instead, arises from the anterior medial margin of the orbital floor with its insertion on the inferoposterior aspect of the globe on the lateral side. It is responsible for the abduction, elevation, and extortion of the eye and intraoperative damage can cause severe complications such as impaired ocular motility and diplopia. 13 , 14 To avoid injuries, the transconjunctival approach follows a subperiosteal detachment of the orbital floor and preserves the IOM attachment in the periorbita, similar to the orbital trauma interventions.
The transconjunctival approach has been described using a pre‐ or postseptal dissection and provides rapid access to the inferior orbital rim and inferior orbit wall. 15 The technique is a useful option for a number of maxillofacial and paranasal sinus surgeries. It has a favorable esthetic profile and a low risk of complications. 16
In regard to the MS, the transconjunctival approach can be utilized for direct access to the ION which may be involved in pathologic processes such as perineural invasion from malignancy, for access to the inferior orbital fissure or as an adjunctive approach to MS neoplasms with orbital involvement.
Transconjunctival step‐by‐step dissection (Figure 5)
Figure 5.
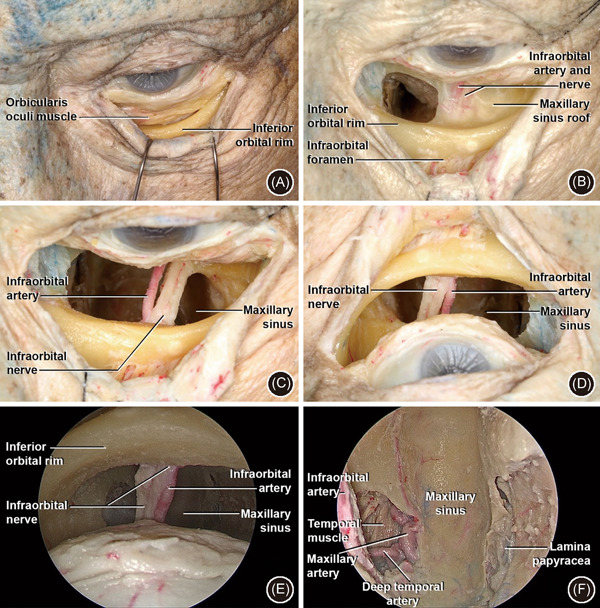
Transconjunctival approach. (A) Left side: conjunctival incision just below to lower border of the tarsus with detachment between septum and orbicularis oculi muscle in the orbital rim; (B) subperiosteal detachment of orbital floor and identification of ION and IOA. The IOF with ION and IOA are identified in the anterior surface of the inferior orbital rim. A window has been opened in the orbit floor medial to the ION; (C) the bone has been drilled medial and lateral to the ION and IOA—anatomic view; (D) surgical view; of C (E): 0‐degree endoscopic superior view of MS, with ION and IOA—surgical view; (F): 0 degree endoscopic superior view of MS, with IMAX and DTA laterally (on the left) and papyracea lamina medially (on the right)—surgical view. DTA, deep temporal artery; IMAX, internal maxillary artery; IOA, infraorbital artery; IOF, infraorbital foramen; ION, infraorbital nerve; MS, maxillary sinus
-
1.
Left side preseptal approach: Conjunctival incision just below the lower border of the tarsus.
-
2.
Lateral canthotomy, as needed.
-
3.
Detachment of the plane between septum and orbicularis oculi muscle in inferior orbital rim direction.
-
4.
Exposure of inferior orbital rim and visualization of ION and IOA coming from IOF.
-
5.
Dissect posteriorly to complete the subperiosteal detachment of the orbital floor until the ION and IOA are well exposed.
-
6.
Drill just medial to the ION to facilitate an opening into the MS superior wall.
-
7.
Similarly, drill just lateral to the ION to create a lateral opening into the MS superior wall, dissecting intervening bone of the orbital floor as needed to facilitate access to the MS, while maintaining the integrity of the ION.
-
8.
A 0‐degree endoscopic superior view of MS. In this figure, the lateral wall of MS was opened to expose deep temporal artery (DTA) and IMAX.
-
9.
Figure 6 demonstrates two case examples of pathology that were addressed via the transorbital/transconjunctival approach.
Figure 6.
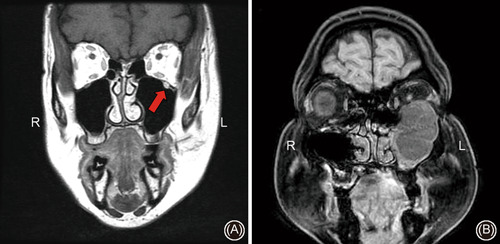
Case examples of pathology requiring a transconjunctival approach; (A) coronal T1 postgadolinium MRI scan demonstrating left infraorbital nerve enlargement and hyperintensity from perineural invasion from cutaneous malignancy (red arrow) and (B) coronal T1 postgadolinium MRI scan demonstrating a large left‐sided V2 schwannoma requiring a combined endoscopic and Caldwell–Luc approach for resection and adjuvant transconjunctival approach for orbital floor reconstruction. MRI, magnetic resonance imaging
The inferior wall and transpalatal approach
The inferior wall of the MS is intimately associated with the alveolar process of maxilla and the roots of the superior teeth. Although not commonly used as an isolated technique, it is possible to reach the inferior wall of MS easily using transpalatal procedure, with or without endoscopic assistance.
Traditionally, the transpalatal approach has involved transecting the soft and hard palates and has been utilized for access to the clivus, craniocervical junction, and nasopharynx. 17 However, with increased utilization of expanded endonasal approaches to the clivus and craniovertebral junction, transpalatal approaches are utilized less commonly. However, transoral maxillectomies maintain an important role for oral cavity malignancies with alveolar or MS involvement. Similarly, MS neoplasms with extension through the palate into the oral cavity usually require transoral approaches, often in conjunction with transnasal endoscopic approaches.
An isolated transpalatal approach to the MS may be considered in cases of boney lesions along the floor of the MS such as intraosseous hemangiomas, odontogenic neoplasms, or as an adjunctive approach to oral‐antral fistula repair.
Tanspalatal step‐by‐step dissection (Figure 7)
Figure 7.
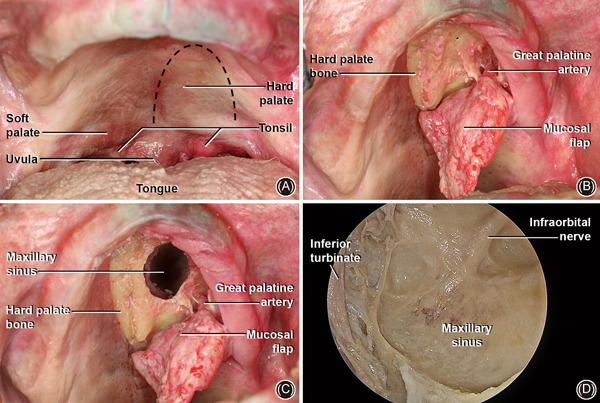
Transpalatal approach. (A) Overview of the oral cavity with hard palate visualization and inverted “U” incision in left hemipalatal region. (B) Mucoperiosteal flap with hard palate bone exposure. Greater palatine artery in inferior/lateral portion of hard palate; (C) a burr hole has been performed in the hard palate with an inferior view of the MS, mucosal flap, and GPA; (D) 4 mm 0‐degree endoscopic inferior overview of MS with ION in the posterior wall. GPA, great palatine artery; ION, infraorbital nerve; MS, maxillary sinus
-
1.
With the mouth open with a retractor, an inverted “U” incision in the hemi‐palate is carried out to the junction of the soft palate, respecting the hard palate midline.
-
2.
A mucoperiosteal flap is then elevated to expose the hard palate bone until transition with soft palate level.
-
3.
Identify and preserve the great palatine artery in the inferior/lateral aspect of the dissection.
-
4.
Drill an approximately 1.5 cm diameter burr hole in the anterior to the medial portion of the hard palate to access the MS. This can be further expanded with drill or Kerrison rongeurs.
-
5.
A 0‐ or 30‐degree endoscope can then be utilized for a magnified view of the MS opening.
-
6.
Figure 8 demonstrates a case utilizing the transpalatal approach.
Figure 8.
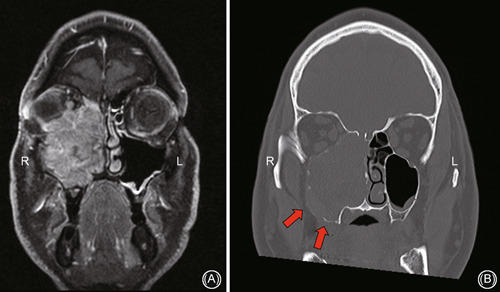
Case example of a right‐sided maxillary sinus mucosal melanoma requiring a combined transpalatal and transfacial approach with orbital exenteration; (A) coronal T1 postgadolinium MRI scan showing intraorbital extension and (B) coronal noncontrast CT scan demonstrating bony erosion and tumor involvement along the floor of sinus necessitating transpalatal approach. CT, computed tomography; MRI, magnetic resonance imaging
The posterior and lateral walls and preauricular hemicoronal approach
The posterior and lateral aspects of the MS are also accessible via a preauricular hemicoronal approach. The lateral wall of the MS abuts the infratemporal fossa and also borders the posterior superior alveolar canal. The posterior wall of the MS is comparatively narrow with the other wall of the MS and interfaces with the pterygopalatine fossa, containing IMAX branches, V2, and pterygopalatine ganglion. 1
The coronal and also hemicoronal approach are commonly applied in neurosurgery and craniofacial approaches. First described in 1907 by Hartley and Kenyon, it later gained increased visibility in craniomaxillofacial surgery in Le Fort II and III procedures. 18 These approaches are consolidated to access frontal, temporal, and especially zygomatic areas, that correspond to 45% of trauma of midface. 19 However, they can also provide an excellent view of posterior/lateral wall of MS. In addition, this approach can be utilized to harvest a temporoparietal fascia flap and allow transmaxillary access to the central skull base for cranial base reconstruction. 20 , 21
Preauricular hemicoronal step‐by‐step dissection (Figure 9)
Figure 9.
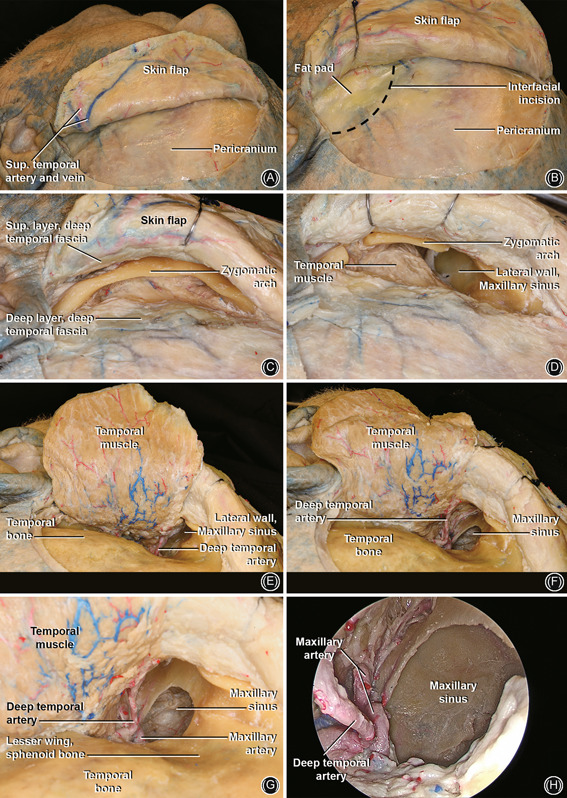
Preauricular hemicoronal approach. (A) Left side: incision 1–2 cm posterior to the hairline extending from the preauricular area towards the forehead midline. (B) Raise the skin flap above the periosteal layer. An incision is performed at the level of the fat pad (black dashed line) 3–4 cm above supraorbital ridge, and dissection is carried out anteriorly in an interfascial plane to expose the zygoma. The superficial layer of the deep temporal fascia is kept with the skin flap to protect the frontal branches of the facial nerve that runs superficial to the superficial layer of the deep temporal fascia. (C) Overview of the zygoma and the superficial layer of the deep temporal fascia superiorly; (D) osteotomies in the lateral and medial portion of the zygomatic arch; (E) elevation of the temporal muscle flap and visualization of posterior/lateral wall of MS. Note the DTA; (F) open window in the lateral wall of MS. (G) Enlarged view of (F), note the DTA and IMAX; (H) 0 degree endoscopic lateral view of MS. DTA, deep temporal artery; IMAX, internal maxillary artery; MS, maxillary sinus
-
1.
Create an incision 1–2 cm posterior to the hairline extending from the tragus in a preauricular trajectory until midline forehead in the temporal region.
-
2.
A skin flap is raised anteriorly.
-
3.
To preserve the facial nerve frontal branches, an interfascial (between superficial and deep layer of deep temporal fascia) incision is performed approximately 3–4 cm above the supraorbital ridge.
-
4.
Exposure of the zygomatic arch and the creation of osteotomies to remove the middle 1/3 of the zygomatic arch will help with further elevation and mobilization of the temporal muscle flap.
-
5.
Incise approximately 1 cm below the superior attachment of temporal muscle and raise the temporal muscle flap until visualization of the lateral/posterior walls of MS is achieved.
-
6.
Identify the DTA and IMAX just lateral to the posterolateral wall of the MS.
-
7.
Drill approximately 2 cm diameter burr hole into the lateral wall to exposure the MS cavity.
-
8.
Visualize with a 0‐degree endoscopic lateral/posterior view of MS with a focus in DTA and IMAX.
-
9.
Figure 10 demonstrates cases requiring a preauricular hemicoronal approach.
Figure 10.
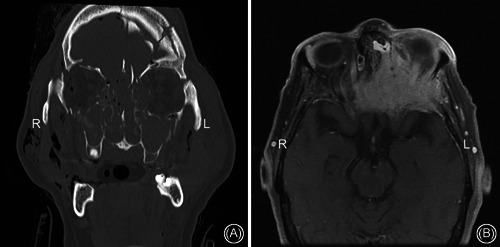
Case examples of pathology necessitating a preauricular hemicoronal approach; (A) noncontrast coronal CT scan of extensive maxillofacial trauma including zygomatic complex fractures and (B) axial T1 postgadolinium MRI scan of sinonasal squamous cell carcinoma requiring a combined craniotomy and hemicoronal approach. CT, computed tomography; MRI, magnetic resonance imaging
DISCUSSION
The MS is a pyramidal‐shaped sinus situated between the first premolar anteriorly and second molar posteriorly 1 and is typically 36–45 mm in height, 25–35 in width, and 38–45 mm anterior–posterior in length. 22 The primary innervation in this region is supplied by the maxillary nerve (V2), which is the second division of the trigeminal ganglion. It continues forward through the orbital floor (superior wall of MS), through the IOC until the IOF and provides sensation to the mid‐face. The most important branch to MS is the PSAN, which arises from the V2 trunk and runs along the infratemporal surface of the maxilla, innervating the mucosa of the MS, as well as the posterior maxillary molars. Its primary blood supply is through the sphenopalatine artery, the terminal branch of the IMAX, which passes through the pterygopalatine fossa and into the nasal cavity at the posterior wall of the MS.
The MS interfaces with the orbit superiorly, the pterygopalatine fossa posteriorly, the infratemporal fossa posterolaterally and nasal cavity medially. As such, it is the focal point of a variety of pathologies include inflammatory, infectious, odontogenic, and neoplastic. Furthermore, the MS can serve as the entry corridor to a number of important regions including the masticator space, lateral recess of the sphenoid sinus and infratemporal fossa.
Despite endoscopic approaches becoming the most commonly utilized method to access the MS, external approaches continue to play an important role. In the modern era, an external approach is often paired with an endoscopic transnasal approach to facilitate access and visualization. A classic neoplasm that may require a combined approach is a large juvenile angiofibroma. Although much of the tumor resection is often feasible via an endoscopic transnasal approach, an anterior transmaxillary approach is often necessary to help with lateral tumor dissection in the infratemporal fossa and to facilitate lateral ligation of the IMAX. In some cases, a hemicoronal approach to the posterolateral aspect of the MS and infratemporal fossa is also necessary. Table 1 summarizes the main indications, contraindications and ideal cases of each illustrated approach.
Table 1.
Indications, contraindications, and ideal cases for selected approaches to the maxillary sinus
| Approaches | Indications | Contraindications | Ideal cases |
|---|---|---|---|
| Medial wall maxillary antrostomy/anterior ethmoidectomy | Inflammatory and neoplastic diseases of MS; MS mega‐antrostomies; endoscopic medial maxillectomy; initial step for transpterygoid approach | Malignancy with inability to complete an endoscopic resection | Chronic rhinosinusitis; complications of acute rhinosinusitis; select MS tumors |
| Caldwell–Luc (anterior transmaxillary approach) | Inflammatory and neoplastic diseases of MS; facial trauma; to reach the pterygopalatine and infratemporal fossa; adjunct to endoscopic cranial base approaches (contralateral transmaxillary); instrument manipulation during endoscopic ipsilateral approaches (to Meckel's cave and infratemporal fossa); pathology in the masticator space or lateral recess of the sphenoid sinus | Anterior wall of MS with severe bone dysplasia; lesion accessible through an endoscopic endonasal approach | Odontogenic neoplasms; MS tumors with attachment in MS anterior wall; facial trauma |
| Transconjunctival | Maxillofacial trauma; to access the ION or the inferior orbital fissure; adjunctive approach to MS with orbital involvement tumors | Lesion not reachable with transconjunctival incision even with addition of lateral canthotomy | Access to the ION, which may be involved in pathologic processes such perineural invasion from malignancy; zygomatic complex trauma |
| Transpalatal | Oral cavity malignancies with alveolar or MS involvement; MS boney lesions with extension through the MS floor or palate into the oral cavity (often added to transnasal endoscopic approaches); adjunctive approach to oral‐antral fistula repair | Severe trismus; tumor extends too lateral to midline | Boney lesions along the floor of the MS: intraosseous hemangiomas or odontogenic neoplasms; adjunctive approach to oral‐antral fistula repair |
| Hemicoronal | To access frontal, temporal, and zygomatic areas; tumors of posterior/lateral wall of MS; transmaxillary access to the central skull base (temporoparietal fascia flap) | Male pattern alopecia (relative contraindication) | Zygomatic complex fractures; tumors of posterior/lateral wall of MS (infratemporal fossa) |
Abbreviation: MS, maxillary sinus.
CONFLICT OF INTERESTS
The authors declare that there are no conflict of interests.
ETHICS STATEMENT
All data were obtained in accordance with the guidelines of the Committee for Cadaveric use in Research.
AUTHOR CONTRIBUTIONS
Natália C. Rezende: idea generation, study design, dissection, data collection, analysis, manuscript drafting, manuscript approval. Carlos D. Pinheiro‐Neto: idea generation, study design, dissection, data collection, analysis, manuscript drafting, manuscript approval. Luciano C. P. C. Leonel: idea generation, study design, dissection, data collection, analysis, manuscript drafting, manuscript approval. Jamie J. Van Gompel: idea generation, study design, data analysis, manuscript drafting, manuscript approval. Maria Peris‐Celda: idea generation, study design, dissection, data collection, analysis, manuscript drafting, manuscript approval. Garret Choby: idea generation, study design, dissection, data collection, analysis, manuscript drafting, manuscript approval.
Supporting information
Supporting information.
ACKNOWLEDGMENT
None declared.
Rezende NC, Pinheiro‐Neto CD, Leonel LCPC, Van Gompel JJ, Peris‐Celda M, Choby G. Three‐hundred and sixty degrees of surgical approaches to the maxillary sinus. World J Otorhinolaryngol Head Neck Surg. 2022;8:42‐53. 10.1002/wjo2.12
DATA AVAILABILITY STATEMENT
All authors had full access to all data.
REFERENCES
- 1. Whyte A, Boeddinghaus R. The maxillary sinus: physiology, development and imaging anatomy. Dentomaxillofac Radiol. 2019;48:20190205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Cho DY, Hwang PH. Results of endoscopic maxillary mega‐antrostomy in recalcitrant maxillary sinusitis. Am J Rhinol. 2008;22:658‐662. [DOI] [PubMed] [Google Scholar]
- 3. Woo HJ, Hwang PH, Kaplan MJ, Choby G. Clinical characteristics and prognostic factors of malignant tumors involving pterygopalatine fossa. Head Neck. 2020;42:281‐288. [DOI] [PubMed] [Google Scholar]
- 4. Wang EW, Gullung JL, Schlosser RJ. Modified endoscopic medial maxillectomy for recalcitrant chronic maxillary sinusitis. Int Forum Allergy Rhinol. 2011;1:493‐497. [DOI] [PubMed] [Google Scholar]
- 5. Peng R, Thamboo A, Choby G, Ma Y, Zhou B, Hwang PH. Outcomes of sinonasal inverted papilloma resection by surgical approach: an updated systematic review and meta‐analysis. Int Forum Allergy Rhinol. 2019;9:573‐581. [DOI] [PubMed] [Google Scholar]
- 6. Leonel L, Carlstrom LP, Graffeo CS, et al. Foundations of advanced neuroanatomy: technical guidelines for specimen preparation, dissection, and 3D‐photodocumentation in a surgical anatomy laboratory. J Neurol Surg B Skull Base. 2021;82:e248‐e258. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Masterson L, Al Gargaz W, Bath AP. Endoscopic Caldwell‐Luc technique. J Laryngol Otol. 2010;124:663‐665. [DOI] [PubMed] [Google Scholar]
- 8. Cantillano P, Rubio F, Naser A, Nazar R. Revision endoscopic sinonasal surgery. Acta Otorrinolaringol Esp. 2017;68:1‐8. [DOI] [PubMed] [Google Scholar]
- 9. Costa ML, Psaltis AJ, Nayak JV, Hwang PH. Long‐term outcomes of endoscopic maxillary mega‐antrostomy for refractory chronic maxillary sinusitis. Int Forum Allergy Rhinol. 2015;5:60‐65. [DOI] [PubMed] [Google Scholar]
- 10. Şahin MM, Yılmaz M, Karamert R, et al. Evaluation of Caldwell‐Luc operation in the endoscopic era: experience from past 7 years. J Oral Maxillofac Surg. 2020;78:1478‐1483. [DOI] [PubMed] [Google Scholar]
- 11. Mercier E, Cunningham MJ. Is antral choanal polyp best managed by an endoscopic or Caldwell‐Luc approach. Laryngoscope. 2021;131:705‐706. [DOI] [PubMed] [Google Scholar]
- 12. Snyderman CH, Gardner PA, Wang EW, Fernandez‐Miranda JC, Valappil B. Experience with the endoscopic contralateral transmaxillary approach to the petroclival skull base. Laryngoscope. 2021;131:294‐298. [DOI] [PubMed] [Google Scholar]
- 13. Shin HJ, Lee SH, Ha TJ, Song WC, Koh KS. Intramuscular nerve distribution of the inferior oblique muscle. Curr Eye Res. 2020;45:215‐220. [DOI] [PubMed] [Google Scholar]
- 14. Shin HJ, Shin KJ, Lee SH, Koh KS, Song WC, Gil YC. Location of the inferior oblique muscle origin with reference to the lacrimal caruncle and its significance in oculofacial surgery. Br J Ophthalmol. 2016;100:179‐183. [DOI] [PubMed] [Google Scholar]
- 15. Bernardini FP, Nerad J, Fay A, Zambelli A, Cruz AA. The revised direct transconjunctival approach to the orbital floor. Ophthalmic Plast Reconstr Surg. 2017;33:93‐100. [DOI] [PubMed] [Google Scholar]
- 16. El‐Anwar MW, Elsheikh E, Hussein AM, Tantawy AA, Abdelbaki YM. Transconjunctival versus subciliary approach to the infraorbital margin for open reduction of zygomaticomaxillary complex fractures: a randomized feasibility study. Oral Maxillofac Surg. 2017;21:187‐192. [DOI] [PubMed] [Google Scholar]
- 17. London NR Jr., Chan J, Carrau RL. Transpalatal approaches to the skull base and reconstruction: indications, technique, and associated morbidity. Semin Plast Surg. 2020;34:99‐105. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Rajmohan S, Tauro D, Bagulkar B, Vyas A. Coronal/hemicoronal approach—a gateway to craniomaxillofacial region. J Clin Diagn Res. 2015;9:PC01‐PC05. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19. Kharkar VR, Rudagi BM, Kini Y. Modification of the hemicoronal approach to treat fractures of the zygomatic complex. J Maxillofac Oral Surg. 2010;9:270‐272. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Patel M, Stadler M, Snyderman C, et al. How to choose? Endoscopic skull base reconstructive options and limitations. Skull Base. 2010;20:397‐404. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Fortes FS, Carrau RL, Snyderman CH, et al. Transpterygoid transposition of a temporoparietal fascia flap: a new method for skull base reconstruction after endoscopic expanded endonasal approaches. Laryngoscope. 2007;117:970‐976. [DOI] [PubMed] [Google Scholar]
- 22. Tiwana PS, Kushner GM, Haug RH. Maxillary sinus augmentation. Dent Clin North Am. 2006;50:409‐424. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supporting information.
Data Availability Statement
All authors had full access to all data.


