Abstract
Objectives
The purpose of this study is to describe the impact of the pandemic on poisoning in children under 18 years presenting to a tertiary care paediatric emergency department (ED) in Canada.
Methods
We utilized the Canadian Hospitals Injury Reporting and Prevention Program (CHIRPP) surveillance data to identify children presenting to the Hospital for Sick Children for poisonings during two time periods: pre-pandemic (March 11 to December 31, 2018 and 2019) and pandemic (March 11 to December 31, 2020). Primary outcomes investigated the change in proportion for total poisonings, unintentional poisonings, recreational drug use, and intentional self-harm exposures over total ED visits. Secondarily, we examined the change in proportion of poisonings between age, sex, substance type, and admission requirement pre-pandemic versus during pandemic.
Results
The proportions significantly increased for total poisonings (122.5%), unintentional poisonings (127.8%), recreational drug use (160%), and intentional self-harm poisonings (104.2%) over total ED visits. The proportions over all poisoning cases also significantly increased for cannabis (44.3%), vaping (134.6%), other recreational drugs (54.5%), multi-substance use (29.3%), and admissions due to poisonings (44.3%) during the pandemic.
Conclusion
Despite an overall decrease in ED visits, there was a significant increase in poisoning presentations to our ED during the pandemic compared with pre-pandemic years. Our results will provide better insight into care delivery and public health interventions for paediatric poisonings.
Keywords: Child health, Emergency department, Health surveillance, Injury, Pandemic, Poisoning
On March 11, 2020, the World Health Organization (WHO) declared the COVID-19 outbreak a pandemic, which led to provinces across Canada implementing various public health measures, such as stay-at-home orders, curfews, and lockdowns to control the spread of SARS-CoV-2 (1). Schools and nonessential businesses were closed, recreation facilities and sports teams, clubs, and camps were suspended, and children as well as adults were encouraged to stay home unless there was an essential reason to leave the house. These extensive interventions around the world dramatically influenced the patterns of emergency department (ED) visits, such as the total numbers, the proportion of injuries including poisoning and ingestions, and the proportion of ED visits related to mental health.
In the United States, national syndromic surveillance data reported that ED visits declined by 42% between April 2019 and April 2020 (2), and for paediatric hospitals in the United States, ED visit rates decreased by 45.7% over 2017 to 2019 versus 2020 (3). In Canada, ED visits declined by 50% between April 2019 and April 2020 (4) and the number of ED visits across Canada’s network of tertiary care paediatric centres decreased by 58% (5).
Although the COVID-19 pandemic was associated with a marked decrease in paediatric ED visits, visits related to injuries, poisonings, and mental health accounted for a greater proportion of all ED visits (3,5,6,7,8,9,10). Moreover, outside the ED, the daily number of calls to poison centres due to exposure to cleaners and disinfectants increased sharply during the first 2 months of the pandemic. The increase in poison centre calls was observed in all age groups but particularly in children less than 5 years old (11). Another report highlighted that the frequency of alcohol and cannabis use increased significantly during the pandemic by Canadian adolescents (12). Furthermore, several studies show that the pandemic and social isolation restrictions led to an increase prevalence of anxiety, depression, and suicidal ideation due to loneliness and/or stress (13,14,15,16).
To date, there has been no specific exploration of paediatric ingestion-related injuries during the COVID-19 pandemic in Canada. The objective of this study was to determine whether there was an increase in unintentional poisoning, recreational drug use, and intentional self-harm poisoning presentations during the COVID-19 pandemic, when compared with pre-pandemic, and if so, to describe the proportional changes in demographics, hospitalization, and drug-related variables for patients under 18 years of age presenting to a tertiary care paediatric ED in Canada.
METHODS
We performed a cross-sectional study of all paediatric poisoning-related ED visits presenting to The Hospital for Sick Children in Toronto, Canada, comparing data from March 11 to December 31 to the same time window 2 years prior (i.e., March 11 to December 31, 2018 and 2019). The Hospital for Sick Children is a large, urban tertiary referral centre for paediatrics and paediatric trauma located in Toronto, Canada. Given the known seasonality of ingestions, we only included encounters from March 11 to December 31, starting on March 11 as that was the time point of the WHO’s global pandemic declaration and the first “stay at home order” in Toronto, Ontario, Canada in March 2020.
Data collection
We identified encounters for children <18 years of age for intentional and unintentional poisonings using external cause-of-injury matrices from the Canadian Hospitals Injury Reporting and Prevention Program (CHIRPP). The electronic CHIRPP (eCHIRPP) database is a national injury and poisoning surveillance system that prospectively collects information with richly detailed injury and poisoning information (17) including standardized intent codes, which allow for stratification by intentional self-harm, recreational use, and unintentional exposure in our data analysis. Furthermore, the CHIRPP database is unique in that it includes a narrative and descriptive section that helps us verify that the patient knowingly was using substances as a suicide/self-harm attempt as well as identify unintentional injuries due to recreational drug misuse or by exploratory behaviour. The eCHIRPP database is managed by the Public Health Agency of Canada. The eCHIRPP database at SickKids has a 100% capture rate for all injuries and poisonings presenting to the ED. Demographic and admission information was also collected from eCHIRPP.
Outcomes
The primary outcomes were the proportion of paediatric ED visits per year for unintentional poisonings, recreational drug use, and intentional self-harm poisonings. The secondary outcomes were age, sex, hospitalization, and the types of substances used. We reviewed eight groups of substances: (1) acetaminophen, (2) alcohol, (3) cannabis, (4) opioids, (5) nonacetaminophen over-the-counter (OTC) drugs such as ibuprofen, vitamins, naproxen, and diphenhydramine, (6) nonopioid-related prescription drugs such as alprazolam, clobazam, fluoxetine, and lorazepam, (7) vaping, and (8) other recreational drugs such as cocaine, crystal methamphetamine, ecstasy, lysergic acid diethylamide, and psilocybin in the pre-pandemic versus pandemic periods. We also examined the occurrence of multi-substance use versus single substance use for pre-pandemic versus pandemic periods.
Statistical analysis
Data were summarized using standard descriptive statistics. Chi-square tests were conducted to compare the proportion of poisoning versus nonpoisoning-related ED visits pre-pandemic (March 11 to December 31, 2018 to 2019) versus during the pandemic (March 11 to December 31, 2020), subclassified by the following poisoning presentations: (1) unintentional use, (2) recreational use, or (3) intentional self-harm use. Chi-square tests were also conducted to examine the difference in proportion of age categories, sex, hospitalization, multi-substance use, and substance types used pre-pandemic versus pandemic periods. All P values reported represent two-sided tests of significance, and results were deemed statistically significant at P<0.05. All analyses were completed using IBM SPSS Statistics version 28 (Chicago, IL).
RESULTS
A total of 1,079 cases of poisoning were identified during the study period: 323 in 2018, 335 in 2019, and 421 in 2020 during the first wave of COVID-19. Sixty percent were females. The age distribution of the total cases of poisonings showed a bimodal distribution. The first peak included those aged 0 to 5 years old (29.2% of total cases), and the second peak included children aged 11 to 18 (66.5% of total cases). See Table 1 for a description of poisonings before and during the pandemic.
Table 1.
Summary table of changes to the demographics, hospitalization, and substance types for all poisoning cases in the pre-pandemic periods (2018 and 2019) with the pandemic period (2020)
| Pre-pandemic (2018) | Pre-pandemic (2019) | During pandemic (2020) | P | |
|---|---|---|---|---|
| n=323 | n=335 | n=421 | ||
| Demographics | ||||
| Age category (years) | ||||
| 0–5 | 103 (31.9%) | 91 (27.2%) | 121 (28.7%) | 0.794 |
| 6–10 | 13 (4%) | 23 (6.9%) | 24 (5.7%) | 0.872 |
| 11–15 | 126 (39%) | 131 (39.1%) | 133 (31.6%) | 0.013 |
| 16–18 | 81 (25.1%) | 90 (26.9%) | 143 (34.0%) | 0.005 |
| Gender (female) | 200 (61.9%) | 187 (55.8%) | 258 (61.2%) | 0.42 |
| Hospitalization | ||||
| Admission | 83 (25.7%) | 76 (22.7%) | 135 (32.1%) | 0.0045 |
| Substance types | ||||
| Acetaminophen | 41 (12.7%) | 30 (9.0%) | 37 (8.8%) | 0.286 |
| Alcohol | 84 (26%) | 75 (22.4%) | 94 (22.3%) | 0.487 |
| Cannabis | 93 (28.8%) | 91 (27.2%) | 170 (40.4%) | <0.001 |
| Opioids | 13 (4.0%) | 13 (3.9%) | 12 (2.9%) | 0.341 |
| Over-the-counter | 66 (20.4%) | 48 (14.3%) | 92 (21.9%) | 0.065 |
| Prescription | 76 (23.5%) | 78 (23.3%) | 84 (20.0%) | 0.183 |
| Recreational drugs | 22 (6.8%) | 23 (6.9%) | 44 (10.5%) | 0.037 |
| Vaping | 6 (1.9%) | 26 (7.8%) | 48 (11.4%) | <0.001 |
| Multi-substance | 96 (29.7%) | 95 (28.4%) | 158 (37.5%) | 0.004 |
Primary outcomes
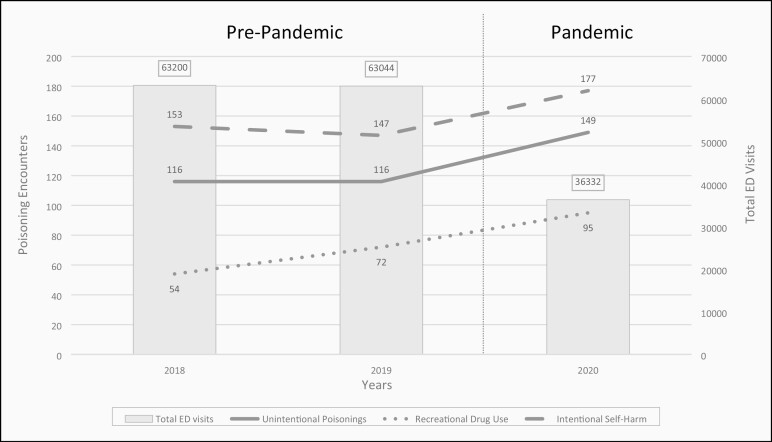
Observed ED encounters for unintentional poisonings, recreational drug use, and intentional self-harm as well as total ED visits by study years are displayed in Figure 1. The proportion of total poisonings significantly increased from 52 per 10,000 ED visits pre-pandemic to 117 per 10,000 ED visits during the pandemic, χ2 (1, N=162,576)=173.973, P≤0.001. During the pandemic, the proportion of encounters for unintentional poisonings significantly increased from 18 per 10,000 ED visits to 41 per 10,000 ED visits, χ2 (1, N=162,576)=61.816, P≤0.001), the proportion of recreational drug use significantly increased from 10 per 10,000 ED visits to 26 per 10,000 ED visits, χ2 (1, N=162,576)=54.32, P≤0.001, and the proportion of intentional self-harm poisonings significantly increased from 24 per 10,000 ED visits to 49 per 10,000 ED visits, χ2 (1, N=162,576)=60.053, P≤0.001) compared with pre-pandemic encounters. To test whether the increase in poisonings were occurring on the backdrop of already increasing paediatric encounters for unintentional, recreational, and intentional self-harm poisonings, we compared 2018 to 2019. Unintentional poisonings remained unchanged, 18 per 10,000 ED visits vs 18 per 10,000 ED visits, χ2 (1, N=126,244)=0.0004, P=0.985. Recreational poisonings remained unchanged, 9 per 10,000 ED visits versus 11 per 10,000 ED visits, χ2 (1, N=126,244)=2.619, P=0.106. Finally, intentional self-harm poisonings also remained unchanged, 24 per 10,000 ED visits versus 23 per 10,000 ED visits, χ2 (1, N=126,244)=0.106, P=0.745).
Figure 1.
Observed encounters for unintentional poisonings, recreational drug use, and intentional self-harm poisonings from March 11 to December 31, 2018–2020 with total ED visit counts from the same time period.
Secondary outcomes
Summary of differences in proportion for age, sex, hospitalization, and type of substances during 2018, 2019, and 2020 are shown in Table 1. We separated the ED encounters by 4 different age groups: 0 to 5 years (infants and toddlers), 6 to 10 years (school-aged), 11 to 15 years (young teens), and 16 to 18 years (teens). There were significant changes in the distribution of the age groups pre-pandemic versus during pandemic. The proportion of young teens (11 to 15 years) changed from 39.1% (pre-pandemic) to 31.6% (during the pandemic), χ2 (1, N=1,079)=6.252, P=0.013, while the proportion of teens (16 to 18 years) changed from 26.0% (pre-pandemic) to 34.0% (during the pandemic), χ2 (1, N=1,079)=7.848, P=0.005.
There was no statistical difference between sex, χ2 (1, N=1,079)=0.651, P=0.42 in the pandemic versus pre-pandemic study periods.
The proportion of poisonings that required hospital admission significantly increased from 24.2% pre-pandemic to 32.1% during the pandemic, χ2 (1, N=1,079)=8.004, P=0.0045.
There were no significant changes in the proportion of acetaminophen, alcohol, opioids, OTC, and prescription type groups; however, the proportion of cannabis cases significantly increased from 28% to 40.4%, χ2 (1, N=1,079)=17.787, P<0.001; the proportion of vaping significantly increased from 4.86% to 11.4%, χ2 (1, N=1,079)=15.514, P<0.001; and the proportion of other recreational drug cases increased from 6.8% to 10.5%, χ2 (1, N=1,079)=4.332, P<0.037. We also observed that the proportion of multi-substance cases in the pre-pandemic cohort vs. pandemic cohort increased from 29.0% to 37.5%, χ2 (1, N=1,079)=8.416, P<0.004.
DISCUSSION
In this Canadian paediatric study, following the declaration of the COVID-19 pandemic by the WHO on March 11, 2020, the frequency of ED visits for all poisoning presentation types increased. Specifically, contrary to a drop by 42.4% in the total number of ED visits during the pandemic, the proportions of unintentional, recreational, and intentional drug exposures more than doubled during the pandemic, and related hospitalizations increased by a third. Preliminary data from the Canadian Institute for Health Information (CIHI) reported similar findings on general hospital visits for substance use that increased for Canadians between March and September 2020 compared with the same period in 2019 (18). The reduction of ED visits during the pandemic was largely attributed to fear of COVID-19 exposure in the hospital setting (19,20).
It is worth noting that not only did our relative numbers of poisonings increase significantly (i.e., proportion of ED visits), but our absolute numbers also increased. This is detailed in Figure 1, showing that the increase in numbers is not simply a factor of fewer ED visits.
The biggest change in proportion for age groups was seen in the teen group where the presentation of teens increased by a third. The main reasons for teen poisonings are due to intentional self-harm and recreational drug use (21), and this was consistent for cannabis, vaping, other recreational drug use, and multi-substance drug use seen at our institution during the pandemic. The recreational use of cannabis was legalized by the Canadian federal government and took effect on October 17, 2018, while E-cigarettes containing nicotine became legal in Canada in May 2018 and cannabis extracts, including vaping products, became legal for sale in Canada on October 17, 2019. The introduction of the above laws in Canada may have caused the shift in proportion where visits for cannabis increased by more than a third and vaping cases more than doubled from pre-pandemic to pandemic periods, while ED visits for alcohol intoxications slightly decreased.
The increased frequency of poisonings due to recreational use and self-harm seen at our institution suggests that there may be negative consequences to the extended lockdown measures that disrupt daily lives and normal social interactions (12,13,14,15,16). According to the Centers for Disease Control and Prevention, 13% of Americans reported starting or increasing substance use as a way of coping with stress or emotions related to COVID-19 (22). A Canadian study confirmed that anxiety and depression increased since the onset of COVID-19 and that one-third of Canadians with anxiety and depression reported an increase in alcohol and cannabis use during the pandemic, while the quantity and quality of mental health support systems have decreased (23). Additionally, our findings of increased hospital admissions suggests that these ingestions may be more severe in nature (i.e., requiring hospitalization instead of simply observation in the ED); however, this will need to be further examined with more detailed chart reviews.
One study reported that the majority of unintentional poisonings that are due to exploratory/unsupervised behaviour occur in the 0 to 5 years age group (21). The increase in frequency of unintentional poisonings in the 0 to 5 age group seen at our institution during the pandemic coincides with school closures during Ontario’s lockdown. This is aligned with a report in California that during lockdown, and with schools closed, there was an increase in calls to the California Poison Control System during school hours due to paediatric exploratory behaviour (24). This is also consistent with other reports that found a significant increase in exposures to cleaners and disinfectants during the pandemic among young children (11,25).
Limitations of our study include data from a single paediatric hospital and dependence upon eCHIRPP codes for classification. Although eCHIRPP is rigorously quality-controlled and prospectively collected, analysis is reliant on the accuracy of patient/caregiver self-reported information. Also, for the purposes of our analysis, we treated the pre-pandemic and during pandemic cohorts as independent, however, it is possible that a small proportion of patients presented multiple times and would be captured in both groups. Another limitation of our study is that our results do not capture the effects of the outcome over time. Future research with interrupted time series analysis, preferably after the pandemic is over, will help show important trends following each wave of the pandemic as well as trends following the measured government responses over time.
CONCLUSION
Overall, we found a significant increase in the proportion of unintentional, recreational drug use, and intentional self-harm poisonings during the pandemic compared with pre-pandemic years, as well as the proportion of hospitalizations due to poisoning. The biggest change in proportion for age groups was seen in the teen group where the presentation of teens increased by a third. There were significantly more cases of cannabis, vaping, other recreational drug use, and multi-substance use in the pandemic cohort compared with pre-pandemic. Continued surveillance of these trends will allow planning and advocating for public health education and inform service delivery measures in the ongoing COVID-19 pandemic and potentially in future pandemics. Specific interventions should be made for child-proofing the home environment for infants and toddlers and increased resources are required to address adolescent mental health and substance use.
MANUSCRIPT FUNDING
The authors received no funding related to this manuscript.
POTENTIAL CONFLICTS OF INTEREST
All authors: No reported conflicts of interest. All authors have submitted the ICMJE Form for Disclosure of Potential Conflicts of Interest. Conflicts that the editors consider relevant to the content of the manuscript have been disclosed.
SUPPLEMENT FUNDING
This article is part of a special supplement on the impact of the COVID-19 pandemic on children and youth. Production of this supplement was made possible through a financial contribution from the Public Health Agency of Canada. The views expressed herein do not necessarily represent the views of the Public Health Agency of Canada.
REFERENCES
- 1. Nussbaumer-Streit B, Mayr V, Dobrescu AI, et al. Quarantine alone or in combination with other public health measures to control COVID-19: a rapid review. Cochrane Database Syst Rev 2020;9:CD013574. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2. Hartnett KP, Kite-Powell A, DeVies J, et al. ; National Syndromic Surveillance Program Community of Practice. . Impact of the COVID-19 pandemic on emergency department visits—United States, January 1, 2019–May 30, 2020. MMWR Morb Mortal Wkly Rep 2020;69(23):699–704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3. DeLaroche AM, Rodean J, Aronson PL, et al. Pediatric emergency department visits at US children’s hospitals during the COVID-19 pandemic. Pediatrics 2021;147(4):e2020039628. [DOI] [PubMed] [Google Scholar]
- 4. Diebel S, Boissonneault E.. A Pan-Canadian narrative review on the protocols for COVID-19 and Canadian Emergency Departments. Int J Med Stud 2021; 9(2):157–61. [Google Scholar]
- 5. Finkelstein Y, Maguire B, Zemek R, et al. Effect of the COVID-19 pandemic on patient volumes, acuity, and outcomes in pediatric emergency departments: A nationwide study. Pediatr Emerg Care 2021; 37(8):427–34. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Esteban PL, Coll JQ, Martínez MX, Biayna JC, Delgado-Flores L.. Has COVID-19 affected the number and severity of visits to a traumatology emergency department? Bone Jt Open 2020;1(10):617–20. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Heppner Z, Shreffler J, Polites A, Ross A, Thomas JJ, Huecker M.. COVID-19 and emergency department volume: The patients return but have different characteristics. Am J Emerg Med 2021;45:385–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Haddadin Z, Blozinski A, Fernandez K, et al. Changes in pediatric emergency department visits during the COVID-19 pandemic. Hosp Pediatr 2021;11(4):e57–60. [DOI] [PubMed] [Google Scholar]
- 9. Sokoloff WC, Krief WI, Giusto KA, et al. Pediatric emergency department utilization during the COVID-19 pandemic in New York City. Am J Emerg Med 2021;45:100–4. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. Chaiyachati BH, Agawu A, Zorc JJ, Balamuth F.. Trends in pediatric emergency department utilization after institution of coronavirus disease-19 mandatory social distancing. J Pediatr 2020;226:274–7.e1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Chang A, Schnall AH, Law R, et al. Cleaning and disinfectant chemical exposures and temporal associations with COVID-19—National Poison Data System, United States, January 1, 2020-March 31, 2020. MMWR Morb Mortal Wkly Rep 2020;69(16):496–8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Dumas TM, Ellis W, Litt DM.. What does adolescent substance use look like during the COVID-19 pandemic? Examining changes in frequency, social contexts, and pandemic-related predictors. J Adolesc Health 2020;67(3):354–61. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13. Leeb RT, Bitsko RH, Radhakrishnan L, Martinez P, Njai R, Holland KM.. Mental health-related emergency department visits among children aged <18 years during the COVID-19 pandemic—United States, January 1–October 17, 2020. MMWR Morb Mortal Wkly Rep 2020;69(45):1675–80. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Krass P, Dalton E, Doupnik SK, Esposito J.. US pediatric emergency department visits for mental health conditions during the COVID-19 pandemic. JAMA Netw Open 2021;4(4):e218533. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Torales J, O’Higgins M, Castaldelli-Maia JM, Ventriglio A.. The outbreak of COVID-19 coronavirus and its impact on global mental health. Int J Soc Psychiatry 2020;66(4):317–20. [DOI] [PubMed] [Google Scholar]
- 16. Shah K, Mann S, Singh R, Bangar R, Kulkarni R.. Impact of COVID-19 on the mental health of children and adolescents. Cureus 2020;12(8):e10051. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Crain J, McFaull S, Thompson W, et al. Status report—The Canadian hospitals injury reporting and prevention program: A dynamic and innovative injury surveillance system. Health Promot Chronic Dis Prev Can 2016;36(6):112–7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18. Canadian Institute for Health Information. Unintended Consequences of COVID-19: Impact on Harms Caused by Substance Use. Ottawa, ON: CIHI; 2021. [Google Scholar]
- 19. Lazzerini M, Barbi E, Apicella A, Marchetti F, Cardinale F, Trobia G.. Delayed access or provision of care in Italy resulting from fear of COVID-19. Lancet Child Adolesc Health 2020;4(5):e10–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20. Mantica G, Riccardi N, Terrone C, Gratarola A.. Non-COVID-19 visits to emergency departments during the pandemic: The impact of fear. Public Health 2020;183:40–1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Gummin DD, Mowry JB, Beuhler MC, et al. 2019 Annual Report of the American Association of Poison Control Centers’ National Poison Data System (NPDS): 37th Annual Report. Clin Toxicol 202058:(12), 1360–541. [DOI] [PubMed] [Google Scholar]
- 22. Czeisler ME, Lane RI, Petrosky E, et al. Mental health, substance use, and suicidal ideation during the COVID-19 pandemic—United States, June 24–30, 2020. MMWR Morb Mortal Wkly Rep 2020;69(32):1049–57. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Dozois DJA; Mental Health Research Canada. . Anxiety and depression in Canada during the COVID-19 pandemic: A national survey. Can Psychol 2021;62(1):136–42. [Google Scholar]
- 24. Levine M, Minns A, Ontiveros S, Thomas SH, Cantrell FL.. Evaluating the impact of home quarantine during the coronavirus pandemic on pediatric exploratory ingestions. Clin Toxicol (Phila) 2021;59(7):673–4. [DOI] [PubMed] [Google Scholar]
- 25. Kuehn BM. Homeless shelters face high COVID-19 risks. JAMA 2020;323(22):2240. [DOI] [PubMed] [Google Scholar]