Abstract
Introduction:
We sought to investigate the association between receipt of an opioid pain reliever (OPR) in the emergency department (ED) and downstream acute health care utilization.
Methods:
Within Kaiser Permanente Northern California, we identified opioid-naïve patients, ages 18–64, who were treated and discharged from the ED for a painful, low-severity condition between January 1, 2017, and December 31, 2017. We also identified patients who received an OPR, either administered in the ED or obtained at a Kaiser Permanente Northern California pharmacy within 7 days of ED arrival, and investigated subsequent acute care utilization in cases with at least 1 ED, urgent care, or inpatient visit within 1 month or 3 months of the index encounter or 2 visits within 12 months.
Results:
Of the 39,468 adults included in our study, 50.7% were female, 55.0% were non-White, and 25.2% received an OPR in association with their index ED encounter. After adjustment, we found that patients who received an OPR had greater odds of downstream acute care utilization than those who did not, with odds ratios of 1.68, 1.53, and 1.50 at 1, 3, and 12 months, respectively (all p < 0.05).
Conclusion:
Patients who received an OPR at their index encounter had substantially increased odds of a subsequent ED, urgent care, or inpatient visit. This effect was most pronounced early in follow-up and persisted for the duration of the study period. Receipt of an OPR among opioid-naïve adults for a painful, low-severity condition is associated with increased downstream acute care utilization.
Introduction
The opioid epidemic in the United States is an ongoing public health emergency. Drug overdoses are the country’s leading cause of injury-related deaths.1 Deaths from both heroin and opioid pain reliever (OPR) overdoses have quadrupled over the past 2 decades, and overdose deaths continue to rise in many areas despite widespread recognition of the epidemic.2,3 Health care costs and utilization have increased proportionately with the rise in OPR availability.4 Drug misuse and abuse led to 2.5 million emergency department (ED) visits in 2011, of which 1.4 million were related to OPRs, and the costs associated with OPR abuse were estimated at nearly $56 billion in 2007.5,6 Prescriptions for OPRs have started to decline; by 2015, more opiate overdoses were caused by heroin and synthetic opioids (fentanyl) than by OPRs, although the first exposure for many patients with opioid use disorder is still through an OPR.7–9
Many patients seek relief from acutely painful conditions in the ED, and it is appropriate that some are treated with an OPR.10,11 In the past several years, new regional and national guidelines have been shown to increase the safety of prescribing OPRs and decrease overall prescriptions. OPR prescriptions written during ED encounters are more likely to align with Centers for Disease Control guidelines than are prescriptions written in other care settings.12 Unfortunately, there is evidence that some patients develop opioid use disorder after an initial OPR prescription in the ED, even when those prescriptions follow OPR best practices.13,14
The association of an initial OPR prescription to opioid-naïve patients in the ED with downstream acute care utilization is not well understood. Long-term opioid use is associated with an increase in acute care utilization, including a higher frequency of outpatient and ED visits, and this relationship appears to be dose dependent.15,16 In addition, OPR prescriptions at hospital discharge have been found to lower the odds of planned, posthospitalization follow-up encounters.17 Understanding the relationship between an initial OPR ED prescription and demand for downstream acute care may provide a broader understanding of the potential impacts of OPRs on patient health, beyond the severe consequences of addiction, overdose, and death, as well as on the long-term costs to health systems.
In this study, conducted within a large integrated health care delivery system in Northern California, we analyzed ED encounters among opioid-naïve patients with low-acuity complaints for which pain typically improves rapidly and with whom follow-up acute care utilization was not anticipated. We examined demographic factors associated with receipt of an OPR during or immediately following the ED visit and the association between receipt of an OPR and subsequent acute care utilization.
Methods
Study Population
We conducted a retrospective cohort study among members of Kaiser Permanente Northern California, a large integrated health care delivery system providing comprehensive inpatient, ED, and ambulatory care for more than 4 million people. Kaiser Permanente Northern California includes 21 medical centers with associated EDs that manage more than 1 million ED visits annually.
Using electronic health records (EHRs) and health plan pharmacy databases, we identified adult patients with active Kaiser Permanente membership, ages 18–64 years, who were treated for an acute, painful, low-severity condition and discharged from a Kaiser Permanente Northern California ED between January 1, 2017, and December 31, 2017. We were specifically interested in prescribing practices and downstream utilization among patients not taking OPRs at the time of their ED visit; we therefore excluded patients who were previously prescribed or administered an OPR from a Kaiser Permanente Northern California pharmacy or hospital within the 6 months before the index visit, based on Kaiser Permanente Northern California pharmacy dispensations.
As with prior studies, we focused on common acute, painful, and low-acuity diagnoses for which substantial unplanned follow-up care and recurrent OPRs were not anticipated.17 We identified the International Classification of Diseases, 10th revision (ICD-10) diagnostic codes with the top 10 highest frequencies of OPR receipt among Emergency Severity Index level IV and V encounters in our system and used these to develop our study cohort.18,19 This list included lumbago (M54.5x), sprains and strains (S43.xx, S46.xx), joint pain (M25.5x), toothaches (K08.8x, K08.9), external abscesses (K12.2, L03.xxx, L02.xx, L98.3), pharyngitis (J02.x), uncomplicated open hand wounds (S61.xxx), corneal abrasions (S05.xx), and herpes zoster (B02.xx). Primary diagnostic codes are assigned by the ED and are identified as the most serious, life-threatening, or resource-intensive diagnosis from the visit. Of note, the list of ICD-10 diagnostic codes among level IV and V charts that most often received an OPR also included forearm fractures. We did not include patients with fractures in this study because of the greater expected need for acute follow-up care for these patients. Table 1 lists the medications considered an OPR in our study.
Table 1.
Opioid pain relievers prescribeda
| Type of Opioid | Frequency | Percentage of total OPRs |
|---|---|---|
| Hydrocodone | 12,835 | 47.7% |
| Oxycodone (with acetaminophen and aspirin) | 3873 | 14.6% |
| Morphine (intravenous and oral) | 2356 | 8.7% |
| Tramadol (and with acetaminophen) | 1288 | 4.7% |
| Codeine (and with acetaminophen and guaifenesin) | 1180 | 4.4% |
| Fentanyl (including intravenous, patch, and oral) | 351 | 1.3% |
| Methadone | 205 | 0.8% |
| Buprenorphine (including patch, naloxone, nasal spray) | 52 | 0.2% |
| Meperidine IV | 12 | 0.0% |
| Oxymorphone | 7 | 0.0% |
aIncludes opioid pain relievers administered to the study population in the emergency department and those filled within 7 days of the index emergency department visit.
OPRs = opioid pain relievers.
Only the first eligible encounter for each patient during the study period was included. We limited our cohort to patients with less expected need for OPR prescriptions and therefore excluded those with active malignancy receiving chemotherapy or hospice, palliative, or comfort care. Patients without health plan pharmacy benefits or with greater than a 45-day gap in membership coverage in the 6 months preceding or the 12 months following the index encounter were also excluded. Prior studies have found that 90% of medications dispensed for Kaiser Permanente Northern California enrollees are captured in Kaiser Permanente Northern California’s pharmacy database, and 100% are captured for the 94% of enrollees with a drug benefit.20
Predictor Variables and Outcome Measure
Patient age, sex, and self-reported race/ethnicity were obtained from EHRs, whereas neighborhood median household income and neighborhood median level of education were based on 2010 US Census block data and patient address on the date of the index ED visit. Race/ethnicity was classified as non-Hispanic White, Asian (including Pacific Islander and Asian Hispanic), Black (including Black Hispanic), Hispanic, and other or unknown. Patient comorbidities were measured by calculating the Charlson Comorbidity Index (CCI), using comorbidity data from the 12 months preceding the index ED visit.21 The length of stay for each ED encounter was also obtained from the EHRs. Dichotomous acute care utilization in the 6 months before the index ED visit (prior ED, urgent care, or inpatient visit versus no visits) was also obtained as a predictor variable. Patients were categorized as having received an OPR if 1 was administered during their index ED visit or if they filled an OPR prescription within 7 days of the visit at any Kaiser Permanente Northern California pharmacy.
Our primary outcome measure was a dichotomous measure of acute care utilization following the index ED visit, assessed at 3 time points: 1 month, 3 months, and 12 months. Patients met the criteria for acute care utilization if they had at least 1 ED, urgent care, or inpatient visit within 1 month or 3 months of the index ED visit or 2 visits (urgent care, ED, or hospitalization) in the following 12 months. A recent study examining the association of unplanned acute care utilization after hospital discharge among those that did and did not receive an OPR used similar time intervals and a similar definition of unplanned health care utilization.17 Our primary analysis was among all ED patients with an eligible diagnosis; we conducted a sensitivity analysis among patients with a chief complaint of lumbago.
Statistical Analysis
We employed Chi-square testing to compare categorical sociodemographic covariates (age, gender, race/ethnicity, neighborhood median household income, neighborhood median education) and clinical covariates (CCI [0, 1–2, 3+], ED length of stay [by quantile], and prior acute care utilization) between those who were and were not dispensed an OPR. Multivariable logistic regression was performed to assess predictors of acute care utilization for each time point. We also conducted a multivariable logistic regression to assess patient-level factors associated with receipt of an OPR. Because missingness in covariates, 549 subjects were not used in the multivariable analyses. A sensitivity analysis included only patients with lumbago as their indexing diagnosis because this was the second largest diagnosis group overall and the group with the highest rate of OPR receipt in our original analysis. Data management and analyses were performed in Statistical Analysis Systems (SAS) 9.4, and a p value of < 0.05 was considered statistically significant. This study was approved by the Kaiser Permanente Northern California Institutional Review Board with a waiver of consent.
Results
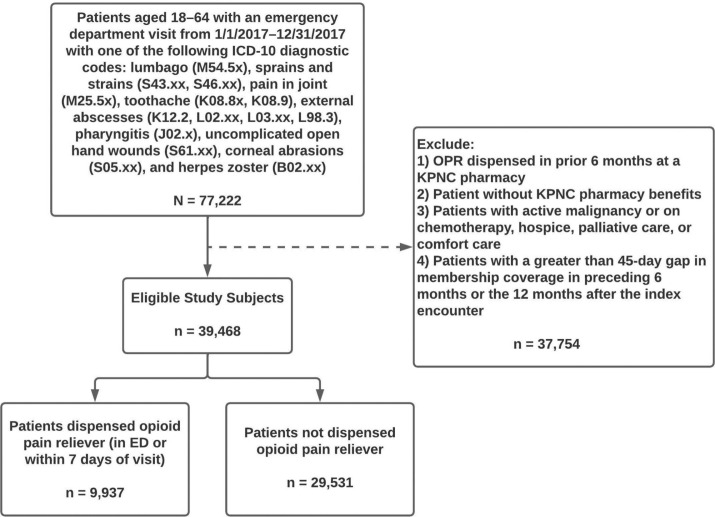
There were 39,468 adults who presented to a Kaiser Permanente Northern California ED with 1 of the 9 selected low-acuity diagnoses during the specified 1-year study period from January 1, 2017, to December 31, 2017 (see Figure 1). Of these 39,468 patients, 50.7% were female. Younger adults, ages 18–30 years old, comprised 25.9% of our study population, whereas adults ages 31–50 and 51–64 years comprised 41.7% and 32.5%, respectively (Table 2). The self-reported race/ethnicity of the patients studied included 45.0% White, 23.9% Hispanic, 13.2% Black, 11.7% Asian, and 6.1% multiple or other races/ethnicities. We found that 52.4% of eligible patients lived in neighborhoods with a neighborhood median household income below $80,000, and 16.6% lived in neighborhoods with a median education of high school or below. Most patients (69.2%) had no significant comorbidities (CCI of 0). The 3 most common diagnoses were uncomplicated hand wounds (25.3% of encounters), lumbago (24.5% of encounters), and joint pain (15.6% of encounters).
Figure 1.
Cohort assembly of 39,468 adult patients, ages 18–64 years, treated in the emergency department for an acutely painful, low-severity condition between January 1, 2017, and December 31, 2017. ED = emergency department; ICD-10 = International Classification of Diseases, 10th revision; KPNC = Kaiser Permanente Northern California; OPR = opioid pain reliever.
Table 2.
Sociodemographic and clinical characteristics of patients with emergency department visits for low-severity, painful complaints (N = 39,468)
| Characteristic | ED Visits, n (%)a |
|---|---|
| Total | 39,468 (100%) |
| Age | |
| 18–30 y | 10,206 (25.86%) |
| 31–50 y | 16,446 (41.67%) |
| 51–64 y | 12,816 (32.47%) |
| Race/ethnicity | |
| Asian | 4635 (11.74%) |
| Black | 5224 (13.24%) |
| Hispanic | 9448 (23.94%) |
| Multiple/other | 2403 (6.09%) |
| White | 17,758 (44.99%) |
| Sex | |
| Female | 20,020 (50.72%) |
| Male | 19,448 (49.28%) |
| Neighborhood median household income | |
| ≤ $80,000 | 20,407 (52.43%) |
| > $80,000 | 18,512 (47.57%) |
| Neighborhood median education | |
| High school or below | 6561 (16.62%) |
| Some college or above | 32,907 (83.38%) |
| CCI | |
| 0 | 27,324 (69.23%) |
| 1–2 | 9722 (24.63%) |
| 3+ | 2422 (6.14%) |
| Diagnosis | |
| Corneal abrasions | 1882 (4.77%) |
| External abscesses | 5217 (13.22%) |
| Herpes zoster | 524 (1.33%) |
| Lumbago | 9665 (24.49%) |
| Pain in joint | 6137 (15.55%) |
| Pharyngitis | 4585 (11.62%) |
| Sprains and strains | 1458 (3.70%) |
| Toothache | 29 (0.07%) |
| Uncomplicated hand wounds | 9970 (25.26%) |
aED visit percentages represent within-column proportions.
CCI = Charlson Comorbidity Index; ED = emergency department.
In our study cohort, 9937 patients (25.2%) had an OPR dispensed in the ED or at a Kaiser Permanente Northern California pharmacy within 7 days of the index visit. The majority of these patients had an OPR dispensed from a pharmacy (80.9%), whereas a smaller proportion (19.1%) had OPRs dispensed only during the ED encounter.
We found differences in OPR prescriptions by patient demographic factors, comorbidity burden, and ED diagnosis in bivariate analysis. The 3 diagnoses with the highest rates of OPR dispensing were lumbago (44.6%), herpes zoster (43.5%), and joint pain (34.3%). Older patients (ages 51–64) were significantly more likely to receive an OPR compared to younger patients (p < 0.01), as were female patients compared to male patients (p < 0.01) (Table 3). Compared to Black, White, and Hispanic patients, Asian patients were significantly less likely to receive an OPR (p < 0.01). Patients living in neighborhoods with lower median income and education levels, patients with higher CCI (compared to lower), and patients with an acute care encounter in the 6 months preceding their index ED visit were significantly more likely to receive an OPR (all p < 0.01). In the adjusted analysis, older female patients and those with higher CCI had increased odds of receiving an OPR, whereas Asian patients and patients who identified their race/ethnicity as multiple or other (compared to White) had lower odds of receiving an OPR (Table 4).
Table 3.
Patient characteristics of those receiving an opioid pain reliever
| Characteristic | Prescribed OPR, n (%)a | |
|---|---|---|
| Total | 9937 (25.18%) | |
| Age | ||
| 18–30 y | 1551 (15.20%) | p < 0.01 |
| 31–50 y | 4359 (26.50%) | |
| 51–64 y | 4027 (31.42%) | |
| Race/ethnicity | ||
| Asian | 859 (18.53%) | p < 0.01 |
| Black | 1394 (26.68%) | |
| Hispanic | 2377 (25.16%) | |
| Multiple/other | 553 (23.01%) | |
| White | 4754 (26.77%) | |
| Sex | ||
| Female | 5228 (26.11%) | p < 0.01 |
| Male | 4709 (24.21%) | |
| Neighborhood median household income | ||
| ≤ $80,000 | 5352 (26.23%) | p < 0.01 |
| > $80,000 | 4448 (24.03%) | |
| Neighborhood median education | ||
| High school or below | 1737 (26.47%) | p < 0.01 |
| Some college or above | 8200 (24.92%) | |
| CCI | ||
| 0 | 5956 (21.80%) | p < 0.01 |
| 1–2 | 2984 (30.69%) | |
| 3+ | 997 (41.16%) | |
| Diagnosis | ||
| Corneal abrasions | 211 (11.21%) | p < 0.01 |
| External abscesses | 1212 (23.23%) | |
| Herpes zoster | 228 (43.51%) | |
| Lumbago | 4306 (44.55%) | |
| Pain in joint | 2103 (34.27%) | |
| Pharyngitis | 590 (12.87%) | |
| Sprains and strains | 357 (24.47%) | |
| Toothache | 8 (27.59%) | |
| Uncomplicated hand wounds | 922 (9.25%) |
aPrescribed OPR percentages represent within-row proportions. All p values calculated using Chi-square test.
CCI = Charlson Comorbidity Index; OPR = opioid pain reliever.
Table 4.
Adjusted odds of receiving an opioid pain reliever based on patient characteristics
| Characteristic | Odds Ratio | 95% CI |
|---|---|---|
| Age | ||
| 18–30 y | Reference | |
| 31–50 y | 1.96 | (1.84–2.09) |
| 51–64 y | 2.20 | (2.05–2.36) |
| Race/ethnicity | ||
| White | Reference | |
| Asian | 0.64 | (0.59–0.69) |
| Black | 0.96 | (0.91–1.03) |
| Hispanic | 0.97 | (0.91–1.03) |
| Multiple/other | 0.83 | (0.75–0.92) |
| Sex | ||
| Female | Reference | |
| Male | 0.92 | (0.86–0.96) |
| Neighborhood median household income | ||
| ≤ $80,000 | Reference | |
| > $80,000 | 0.93 | (0.89–0.98) |
| Neighborhood median education | ||
| High school or below | Reference | |
| Some college or above | 0.96 | (0.89–1.02) |
| CCI | ||
| 0 | Reference | |
| 1–2 | 1.43 | (1.35–1.51) |
| 3+ | 1.99 | (1.81–2.17) |
CI = confidence interval; CCI = Charlson Comorbidity Index.
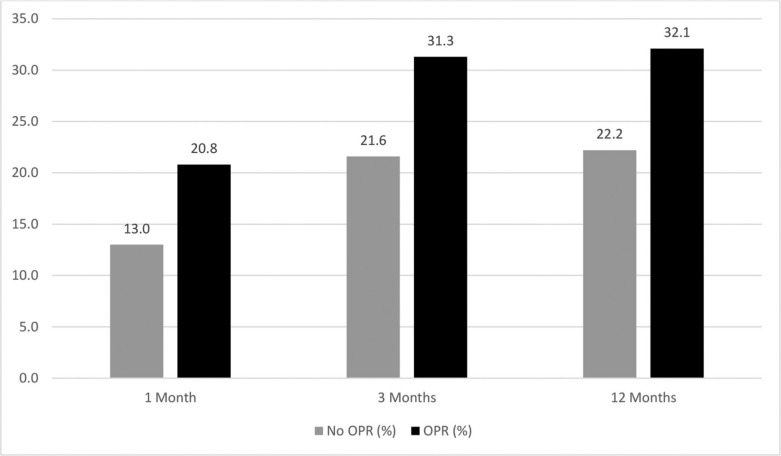
We found 5901 patients (15.0%) had at least 1 urgent care, ED, or inpatient encounter within 1 month of their index ED visit. This number increased to 9494 (24.1%) individuals at 3 months; at 12 months, 9736 (24.7%) individuals had at least 2 subsequent acute care encounters. Of the 9937 individuals who had an OPR dispensed in the ED or at a Kaiser Permanente Northern California pharmacy within 7 days, 20.8% had at least 1 acute care encounter at 1 month, 31.3% had at least 1 encounter at 3 months, and 32.1% had at least 2 encounters at 12 months, compared to those who had not received an OPR (13.0%, 21.6%, and 22.2%, respectively, with p < 0.01) (Figure 2). After adjusting for patient demographic and comorbidity data, the odds of acute care utilization among those who received an OPR compared to those who did not was 1.54 (95% confidence interval [CI] = 1.44–1.64) at 1 month, 1.42 (95% CI = 1.34–1.51) at 3 months, and 1.40 (95% CI = 1.32–1.49) at 12 months (Table 5). In addition, the odds of acute care utilization were higher among younger patients, Black patients (compared to White patients at 3 months and 12 months only), female patients (significant only in the models of acute care utilization at 3 and 12 months), those with a higher CCI, those with acute care utilization in the 6 months before their index ED visit, and those living in areas with a lower median education level. The odds of acute care utilization were lower among Asian patients (compared to White patients) (Table 5). In a sensitivity analysis including only patients with lumbago as their indexing diagnosis, the odds of downstream acute care utilization among those who received an OPR were also significantly increased at each of the time points studied: 1.80 (95% CI = 1.58–2.04) at 1 month, 1.47 (95% CI = 1.32–1.63) at 3 months, and 1.23 (95% CI = 1.11–1.37) at 12 months (see Appendix A).
Figure 2.
Percentage of patients who had at least 1 acute care visit at 1 and 3 months after their index emergency department visit or at least 2 acute care visits at 12 months, comparing those who did and did not receive an opioid pain reliever. All differences between patients who did and did not receive an opioid pain reliever are significant (p < 0.01). Acute care visits are defined as urgent care, emergency department, or inpatient visits. OPR = opioid pain reliever.
Table 5.
Adjusted odds of higher acute care utilization by receipt of opioid pain reliever and patient characteristicsa
| Patient characteristics | 1 month OR (95% CI) |
3 months OR (95% CI) |
12 months OR (95% CI) |
|---|---|---|---|
| Prescribed OPR | |||
| No | Reference | — | — |
| Yes | 1.54 (1.44–1.64) | 1.42 (1.34–1.51) | 1.40 (1.32–1.49) |
| Age | |||
| 18–30 y | Reference | — | — |
| 31–50 y | 0.86 (0.80–0.93) | 0.85 (0.79–0.90) | 0.77 (0.72–0.83) |
| 51–64 y | 0.84 (0.77–0.91) | 0.81 (0.75–0.87) | 0.70 (0.65–0.75) |
| Race/ethnicity | |||
| White | Reference | — | — |
| Asian | 0.84 (0.76–0.94) | 0.80 (0.73–0.87) | 0.70 (0.64–0.77) |
| Black | 1.07 (0.98–1.18) | 1.26 (1.17–1.36) | 1.61 (1.50–1.74) |
| Hispanic | 0.96 (0.89–1.04) | 0.98 (0.92–1.05) | 0.99 (0.92–1.06) |
| Multiple/other | 1.06 (0.93–1.20) | 1.01 (0.90–1.12) | 1.07 (0.95–1.20) |
| Sex | |||
| Female | Reference | — | — |
| Male | 0.99 (0.93–1.06) | 0.87 (0.82–0.91) | 0.76 (0.72–0.80) |
| Neighborhood median income | |||
| ≤ $80,000 | Reference | - | - |
| > $80,000 | 1.14 (1.06–1.21) | 1.02 (0.97–1.08) | 0.90 (0.85–0.96) |
| Neighborhood median education | |||
| High school or below | Reference | — | — |
| Some college or above | 0.91 (0.84–0.99) | 0.91 (0.84–0.98) | 0.88 (0.81–0.94) |
| CCI | |||
| 0 | Reference | — | — |
| 1–2 | 1.34 (1.24–1.43) | 1.47 (1.38–1.56) | 1.89 (1.78–2.00) |
| 3+ | 1.83 (1.64–2.05) | 2.28 (2.07–2.52) | 3.65 (3.30–4.04) |
| Prior acute care utilization | |||
| No | Reference | — | — |
| Yes | 1.88 (1.76–2.00) | 2.28 (2.16–2.41) | 3.38 (3.20–3.56) |
| ED length of stay | 1.01 (1.00–1.01) | 1.00 (1.00–1.00) | 1.01 (1.00–1.01) |
aSeparate models were run for the 1-month, 3-month, and 12-month intervals, with higher acute care utilization at 1 and 3 months defined as ≥ 1 urgent care, emergency department, or inpatient encounter and at 12 months defined as ≥ 2 such encounters. The primary predictor for each time point was an opioid prescription at or within 7 days of the index emergency department visit, and all analyses were adjusted for the above-listed covariates. Primary acute care utilization is defined as ≥ 1 urgent care, emergency department, or inpatient encounter in the 6 months before the indexing encounter. Emergency department length of stay is included as a continuous variable with 10-minute units.
CCI = Charlson Comorbidity Index; CI = confidence interval; ED = emergency department; OR = odds ratio; OPR = opioid pain reliever.
Discussion
In this large sample of adult patients presenting to an ED with an acutely painful, low-severity complaint who had not received an OPR in the prior 6 months, we observed a significant association between OPR prescription and subsequent unplanned acute care utilization after controlling for multiple patient characteristics. The effect was most pronounced in early follow-up among patients who received an OPR, who were found to have 68% greater odds of an acute care encounter in the following month compared to those who did not receive an OPR. Although the effect size decreased slightly over time, patients who received an OPR were also significantly more likely to have higher acute care utilization at 3 and even 12 months. An additional sensitivity analysis was conducted only on the subset of patients with a lumbago diagnosis, which again demonstrated this association.
The exact reason for this observed increase in care-seeking behavior among patients who received an OPR cannot be fully elucidated from our study. We purposely analyzed a cohort of patients with low-acuity diagnoses for which we would expect minimal need for return ED visits, urgent care, or hospital care, and we adjusted for comorbidities and demographic information to try to limit confounding by disease severity. Despite this, we suspect this difference in unplanned acute care use in many cases may be because patients who received an OPR had a more complicated or painful condition and needed to return for worsening symptoms. An additional hypothesis is that this difference in care-seeking behavior may be at least partially explained by initial exposure to OPRs. The return visit may have been secondary to an unintended consequence of OPR use or seeking another prescription.
Prior studies in other settings have suggested that OPR use is associated with increased health care utilization.15–17 An earlier study found that patients undergoing abdominal surgery with preoperative opioid use had higher rates of hospital readmission and higher health care costs for up to 12 months after the procedure.22 Another study found that patients who received an OPR for shoulder or spine pain in an outpatient clinic had higher rates of downstream health care utilization and higher costs in the year following initial OPR use compared to those who did not receive an OPR.23 To our knowledge, this is the first study of the association between OPR prescriptions for low-acuity complaints in an ED and unplanned, acute care-seeking behavior. This study contributes to the growing body of evidence that receipt of an OPR prescription can have unintended consequences on patient health and is associated with an increase in health care expenditures.
Overall, about 1 in 4 patients received an OPR following their index ED visit. This is significantly lower than the nearly 40% reported in similarly designed national studies from the early 2000s, but it is comparable to a more recent study of discharged ED patients.24,25 The differences between this study and those from the early 2000s may reflect the exclusion of patients with more severe and therefore potentially more painful complaints, as well as national trends of decreasing opioid prescriptions.25 During the study period, a region-wide opioid safety initiative with substantial physician training led to a decrease in OPR prescriptions across clinical settings.26
Our findings regarding the patient characteristics associated with dispensing of an OPR both parallel and contrast other studies. Similar to an earlier study, patients of self-identified Asian ethnicity received prescription pain relief at the lowest rates compared to other ethnic groups.27 Other studies have reported that cultural variation in the expression of pain and other aspects of pain reporting may contribute to observed differences in the pain management of people of Asian ethnicity, and this finding does warrant further investigation.25,28 In contrast to several studies that report fewer opioid prescriptions given to Black patients as compared to White patients25,28–31, we found that, after controlling for multiple demographic and comorbid conditions, there was no significant difference in the dispensing of OPRs between these groups.
Limitations
The conclusions of our study are limited by the possibility that there were differences in pain level or disease severity between patients who did and did not receive an OPR in the ED. Unfortunately, pain scores are not reliably captured from the ED in our EHRs. In an attempt to limit confounding, we adjusted for ED length of stay, included only low-severity, treat and release visits for specific conditions for which unplanned acute care would not be expected, and adjusted for patient characteristics to limit variability between populations.
As with most retrospective studies, there exists the possibility of missing or incomplete data. In this study, we are limited by our reliance on records of opioids dispensed at Kaiser Permanente pharmacies. Prescriptions filled at non–Kaiser Permanente pharmacies were not included in this analysis, and we therefore likely underestimated the number of opioids prescribed after the index visit. In addition, we used dispensing data, as opposed to actual consumption, employing methodologies used by similar studies.32,33 We further defined OPR exposure as either administration of an OPR in the ED or filling a prescription within 7 days of the encounter. There may be small differences between the groups of patients who used OPRs in the ED versus those who filled a prescription immediately afterward. We did not exclude patients for whom non-OPRs were contraindicated because of limitations in accurate electronic capture. We relied on coded diagnoses to abstract our cohort; it is possible that we missed patients who did not receive an appropriate diagnosis code and may therefore have undercounted the true population.
Based on study methods, we are unable to assess a causal link between what occurred during the index ED visit and downstream acute care use. We did not obtain diagnoses from the recurrent visits and therefore have no way of knowing if these subsequent encounters were for opioid-related complications, the same painful complaint present at the patients’ initial ED visit, or other reasons entirely. We also did not separate urgent care, ED, and inpatient visits, and the reasons for visits to these venues may have differed. Lastly, our findings may not be generalizable to settings with less access to outpatient (non-ED or nonurgent care) follow-up or with different patient cost sharing for ED or inpatient visits.
Conclusion
We present data from a large, diverse population across 21 EDs in an integrated health care delivery system with a comprehensive EHR and pharmacy database that allowed for the capture of health care utilization and OPR dispensing across settings. We found that dispensing an OPR to opioid-naïve ED patients with certain low-acuity diagnoses was associated with a significant increase in unplanned acute care at 1 month, 3 months, and 12 months following their index visit. Our findings provide a nuanced perspective regarding how OPRs may have substantial and durable effects on patients’ subsequent care-seeking behavior. More research is needed to evaluate the cause and medical appropriateness of this observed increase in acute care utilization.
Acknowledgments
We would like to thank Mamata Kene, MD, Cynthia Campbell, PhD, MPH, and Joan Lo, MD, for reviewing and providing comments on the manuscript.
Appendix
Appendix A:
Sensitivity analysis with adjusted odds of higher acute care utilization among only patients with an indexing diagnosis of lumbago who received an OPR compared to those who did not, as well as adjusted odds of higher acute care utilization by patient characteristic
| Patient characteristic | 1 month OR (95% CI) | 3 months OR (95% CI) | 12 months OR (95% CI) |
|---|---|---|---|
| Prescribed OPR | |||
| No | Reference | – | – |
| Yes | 1.80 (1.58-2.04) | 1.47 (1.32-1.63) | 1.23 (1.11-1.37) |
| Age | |||
| 18-30 y | Reference | – | – |
| 31-50 y | 0.84 (0.70-1.01) | 0.82 (0.71-0.95) | 0.73 (0.64-0.84) |
| 51-64 y | 0.88 (0.73-1.07) | 0.84 (0.72-0.98) | 0.68 (0.58-0.79) |
| Race/ethnicity | |||
| White | Reference | – | – |
| Asian | 0.62 (0.49-0.80) | 0.63 (0.52-0.76) | 0.59 (0.49-0.71) |
| Black | 1.10 (0.92-1.30) | 1.10 (0.95-1.28) | 1.31 (1.14-1.51) |
| Hispanic | 0.93 (0.79–1.09) | 0.89 (0.78–1.02) | 0.96 (0.84-1.09) |
| Multiple/other | 0.95 (0.72-1.24) | 0.91 (0.73-1.14) | 1.01 (0.81-1.25) |
| Sex | |||
| Female | Reference | – | – |
| Male | 1.00 (0.88-1.13) | 0.86 (0.78-0.96) | 0.71 (0.64-0.79) |
| Neighborhood median income | |||
| ≤ $80,000 | Reference | – | – |
| > $80,000 | 0.99 (0.86-1.13) | 0.91 (0.81-1.02) | 0.93 (0.83-1.04) |
| Neighborhood median education | |||
| High school or below | Reference | – | – |
| Some college or above | 0.95 (0.79-1.13) | 0.92 (0.80-1.06) | 0.78 (0.68-0.90) |
| CCI | |||
| 0 | Reference | – | – |
| 1–2 | 1.33 (1.16-1.54) | 1.44 (1.28-1.61) | 1.80 (1.61-2.01) |
| 3+ | 1.76 (1.41-2.18) | 2.21 (1.84-2.66) | 3.30 (2.75-4.00) |
| Prior acute care utilization | |||
| No | Reference | – | – |
| Yes | 2.39 (2.01-2.72) | 2.73 (2.46-3.03) | 3.40 (3.07-3.76) |
| ED length of stay | 1.00 (1.00-1.01) | 1.00 (1.00-1.00) | 1.00 (0.99-1.00) |
Separate models were run for the 1-month, 3-month, and 12-month intervals, with higher acute care utilization defined at 1 and 3 months as ≥ 1 urgent care, emergency department, or inpatient encounter and at 12 months as ≥ 2 such encounters. The primary predictor for each time point was opioid prescription at or within 7 days of the index emergency department visit, and all analyses were adjusted for the listed covariates. Primary acute care utilization is defined as ≥ 1 urgent care, emergency department, or inpatient encounter in the 6 months prior to the indexing encounter. Emergency department length of stay is included as a continuous variable with 10-minute units.
CCI = Charlson Comorbidity Index; CI = confidence interval; ED = emergency department; OR = odds ratio; OPR = opioid pain reliever.
Footnotes
Author Contributions: All authors were involved in the conception, plan, and design of the study. Julia Wei, MPH, performed the data acquisition and statistical analyses. Nathan Juergens, MD, MPH, and Dana Sax, MD, MPH, wrote the manuscript with input from all authors.
Conflicts of Interest: None declared
Funding: The study was funded through the Kaiser Permanente Department of Graduate Medical Education.
References
- 1.Warner M, Chen LH, Makuc DM, Anderson RA, Miniño AM. Drug poisoning deaths in the United States, 1980–2008. NCHS Data Brief 2011;(81):1–8. DOI: 10.1002/9780470976012.ch1 [DOI] [PubMed] [Google Scholar]
- 2.Gomes T, Tadrous M, Mamdani M, Paterson JM, Juurlink DN. The burden of opioid-related mortality in the United States. JAMA Netw Open. 2018;1(2):e180217. DOI: 10.1001/jamanetworkopen.2018.0217 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Scholl L, Seth P, Kariisa M, Wilson N, Baldwin G. Drug and opioid-involved overdose deaths — United States, 2013–2017. MMWR Morb Mortal Wkly Rep 2019;67:1419–1427. DOI: 10.15585/mmwr.mm675152e1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Kern DM, Zhou S, Chavoshi S, et al. Treatment patterns, healthcare utilization, and costs of chronic opioid treatment for non-cancer pain in the United States. Am J Manag Care 2015;21(3):e222–234. https://www.ajmc.com/view/treatment-patterns-healthcare-utilization-and-costs-of-chronic-opioid-treatment-for-non-cancer-pain-in-the-united-states [PubMed] [Google Scholar]
- 5.Substance Abuse and Mental Health Services Administration . Highlights of the 2011 Drug Abuse Warning Network (DAWN) findings on drug-related emergency department visits. The DAWN Report. Rockville, MD: US Department of Health and Human Services, Substance Abuse and Mental Health Services Administration; 2013. [PubMed] [Google Scholar]
- 6.Birnbaum HG, White AG, Schiller M, Waldman T, Cleveland JM, Roland CL. Societal costs of prescription opioid abuse, dependence, and misuse in the United States. Pain Med 2011;12(4):657–667. DOI: 10.1111/j.1526-4637.2011.01075.x [DOI] [PubMed] [Google Scholar]
- 7.Pergolizzi, JV Jr, Rosenblatt M, LeQuang JA. Three years down the road: The aftermath of the CDC guideline for prescribing opioids for chronic pain. Adv Ther 2019;36(6):1235–1240. DOI: 10.1007/s12325-019-00954-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Zhu W, Chernew ME, Sherry TB, Maestas N. Initial opioid prescriptions among U.S. commercially insured patients, 2012–2017. N Engl J Med 2019;380:1043–1052. DOI: 10.1056/NEJMsa1807069 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Overdose death rates - Trends & statistics . National Institutes of Health, National Institute on Drug Abuse. Accessed June 2020. https://www.drugabuse.gov/drug-topics/trends-statistics/overdose-death-rates
- 10.Hoppe JA, Nelson LS, Perrone J, Weiner SG, Prescribing Opioids Safely in the Emergency Department (POSED) Study Investigators. Opioid prescribing in a cross section of US emergency departments. Ann Emerg Med 2015;66(3):253–259.e1. DOI: 10.1016/j.annemergmed.2015.03.026 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Jeffery MM, Hooten WM, Hess EP, et al. Opioid prescribing for opioid-naive patients in emergency departments and other settings: Characteristics of prescriptions and association with long-term use. Ann Emerg Med 2018;71(3):326–336.e19. DOI: 10.1016/j.annemergmed.2017.08.042 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Dowell D, Haegerich TM, Chou R. CDC guideline for prescribing opioids for chronic pain — United States, 2016. MMWR Recomm Rep 2016;65(No. RR-1):1–49. DOI: 10.15585/mmwr.rr6501e1 [DOI] [PubMed] [Google Scholar]
- 13.Butler MM, Ancona RM, Beauchamp GA, et al. Emergency department prescription opioids as an initial exposure preceding addiction. Ann Emerg Med 2016;68(2):202–208. DOI: 10.1016/j.annemergmed.2015.11.033 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Delgado MK, Huang Y, Meisel Z, et al. National variation in opioid prescribing and risk of prolonged use for opioid-naive patients treated in the emergency department for ankle sprains. Ann Emerg Med 2018;72(4):389–400.e1. DOI: 10.1016/j.annemergmed.2018.06.003 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Deyo RA, Smith DHM, Johnson ES, et al. Opioids for back pain patients: Primary care prescribing patterns and use of services. J Am Board Fam Med 2011;24(6):717–727. DOI: 10.3122/jabfm.2011.06.100232 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Morasco BJ, Yarborough BJ, Smith NX, et al. Higher prescription opioid dose is associated with worse patient-reported pain outcomes and more health care utilization. J Pain 2017;18(4):437–445. DOI: 10.1016/j.jpain.2016.12.004 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Liberman JS, Samuels LR, Goggins K, Kripalani S, Roumie CL, Vanderbilt Inpatient Cohort Study . Opioid prescriptions at hospital discharge are associated with more postdischarge healthcare utilization. J Am Heart Assoc 2019;8(3):e010664. DOI: 10.1161/JAHA.118.010664 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 18.The web’s free 2021 ICD-10-CM/PCS medical coding reference. ICD10data.com. Accessed June 2020. https://www.icd10data.com/
- 19.Emergency Severity Index (ESI): A triage tool for emergency departments. Agency for Healthcare Research and Quality. Accessed June 2020. https://www.ahrq.gov/professionals/systems/hospital/esi/index.html
- 20.Selby JV, Smith DH, Johnson ES, Raebel MA, Friedman GD, McFarland BH. Kaiser Permanente medical care program. In: Pharmacoepidemiology. 4th ed. Strom BL, editor. West Sussex, England: John Wiley and Sons, 2005:241–259. DOI: 10.1002/9780470059876 [DOI] [Google Scholar]
- 21.D’Hoore W, Sicotte C, Tilquin C. Risk adjustment in outcome assessment: The Charlson comorbidity index. Methods Inf Med 1993;32(5):382–387. DOI: 10.1055/s-0038-1634956 [DOI] [PubMed] [Google Scholar]
- 22.Waljee JF, Cron DC, Steiger RM, Zhong L, Englesbe MJ, Brummett CM. Effect of preoperative opioid exposure on healthcare utilization and expenditures following elective abdominal surgery. Ann Surg 2017;265(4):715–721. DOI: 10.1097/SLA.0000000000002117 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23.Rhon DI, Greenlee TA, Fritz JM. The influence of a guideline-concordant stepped care approach on downstream health care utilization in patients with spine and shoulder pain. Pain Med 2019;20(3):476–485. DOI: 10.1093/pm/pny212 [DOI] [PubMed] [Google Scholar]
- 24.Green CR, Anderson KO, Baker TA, et al. The unequal burden of pain: Confronting racial and ethnic disparities in pain. Pain Med 2003;4(3):277–294. DOI: 10.1046/j.1526-4637.2003.03034.x [DOI] [PubMed] [Google Scholar]
- 25.Pletcher MJ, Kertesz SG, Kohn MA, Gonzales R. Trends in opioid prescribing by race/ethnicity for patients seeking care in US emergency departments. JAMA 2008;299(1):70–78. DOI: 10.1001/jama.2007.64 [DOI] [PubMed] [Google Scholar]
- 26.Awsare S, Havens C, Lippi J. Facing the opioid crisis: Practical, effective actions we can take. Gastroenterology 2019;156(6):1538–1541. DOI: 10.1053/j.gastro.2018.12.035 [DOI] [PubMed] [Google Scholar]
- 27.Groenewald CB, Rabbitts JA, Hansen E, Palermo TM. Racial differences in opioid prescribing for children in the United States. Pain 2018;159(10):2050–2057. DOI: 10.1097/j.pain.0000000000001290 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ahn H, Weaver M, Lyon D, et al. Differences in clinical pain and experimental pain sensitivity between Asian Americans and Whites with knee osteoarthritis. Clin J Pain 2017;33(2):174–180. DOI: 10.1097/AJP.0000000000000378 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Heins JK, Heins A, Grammas M, Costello M, Huang K, Mishra S. Disparities in analgesia and opioid prescribing practices for patients with musculoskeletal pain in the emergency department. J Emerg Nurs 2006;32(3):219–224. DOI: 10.1016/j.jen.2006.01.010 [DOI] [PubMed] [Google Scholar]
- 30.Tamayo-Sarver JH, Hinze SW, Cydulka RK, Baker DW. Racial and ethnic disparities in emergency department analgesic prescription. Am J Public Health 2003;93(12):2067–2073. DOI: 10.2105/ajph.93.12.2067 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Singhal A, Tien Y-Y, Hsia RY. Racial–ethnic disparities in opioid prescriptions at emergency department visits for conditions commonly associated with prescription drug abuse. PloS One 2016;11(8):e0159224. DOI: 10.1371/journal.pone.0159224 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Von Korff M, Saunders K, Ray GT, et al. De facto long-term opioid therapy for noncancer pain. Clin J Pain 2008;24(6):521–527. DOI: 10.1097/AJP.0b013e318169d03b [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Boudreau D, Von Korff M, Rutter CM, et al. Trends in long-term opioid therapy for chronic non-cancer pain. Pharmacoepidemiol Drug Saf 2009;18(12):1166–1175. [DOI] [PMC free article] [PubMed] [Google Scholar]