This survey study compares the use of cannabis for medical purposes as reported in electronic health records (EHRs) with use reported in a confidential survey.
Key Points
Question
What is the prevalence of patient-reported explicit (ie, medical use) and implicit (ie, health reasons for use) medical cannabis use, and how does electronic health record documentation compare with patient report of medical use?
Findings
In this survey study, among 1688 primary care patients, 26.5% reported explicit and 35.1% reported implicit medical use of cannabis. The prevalence of medical use documented in the electronic health record was 4.8%, missing most medical cannabis use reported by patients.
Meaning
These findings suggest that asking about use of cannabis for managing pain, sleep, mood, or other health concerns may increase recognition and documentation of medical cannabis use.
Abstract
Importance
Patients who use cannabis for medical reasons may benefit from discussions with clinicians about health risks of cannabis and evidence-based treatment alternatives. However, little is known about the prevalence of medical cannabis use in primary care and how often it is documented in patient electronic health records (EHR).
Objective
To estimate the primary care prevalence of medical cannabis use according to confidential patient survey and to compare the prevalence of medical cannabis use documented in the EHR with patient report.
Design, Setting, and Participants
This study is a cross-sectional survey performed in a large health system that conducts routine cannabis screening in Washington state where medical and nonmedical cannabis use are legal. Among 108 950 patients who completed routine cannabis screening (between March 28, 2019, and September 12, 2019), 5000 were randomly selected for a confidential survey about cannabis use, using stratified random sampling for frequency of past-year use and patient race and ethnicity. Data were analyzed from November 2020 to December 2021.
Exposures
Survey measures of patient-reported past-year cannabis use, medical cannabis use (ie, explicit medical use), and any health reason(s) for use (ie, implicit medical use).
Main Outcomes and Measures
Survey data were linked to EHR data in the year before screening. EHR measures included documentation of explicit and/or implicit medical cannabis use. Analyses estimated the primary care prevalence of cannabis use and compared EHR-documented with patient-reported medical cannabis use, accounting for stratified sampling and nonresponse.
Results
Overall, 1688 patients responded to the survey (34% response rate; mean [SD] age, 50.7 [17.5] years; 861 female [56%], 1184 White [74%], 1514 non-Hispanic [97%], and 1059 commercially insured [65%]). The primary care prevalence of any past-year patient-reported cannabis use on the survey was 38.8% (95% CI, 31.9%-46.1%), whereas the prevalence of explicit and implicit medical use were 26.5% (95% CI, 21.6%-31.3%) and 35.1% (95% CI, 29.3%-40.8%), respectively. The prevalence of EHR-documented medical cannabis use was 4.8% (95% CI, 3.45%-6.2%). Compared with patient-reported explicit medical use, the sensitivity and specificity of EHR-documented medical cannabis use were 10.0% (95% CI, 4.4%-15.6%) and 97.1% (95% CI, 94.4%-99.8%), respectively.
Conclusions and Relevance
These findings suggest that medical cannabis use is common among primary care patients in a state with legal use, and most use is not documented in the EHR. Patient report of health reasons for cannabis use identifies more medical use compared with explicit questions about medical use.
Introduction
Cannabis and cannabinoid use in the US is prevalent and increasing.1,2 A majority of states have legalized medical cannabis use, and among these, 18 have legalized nonmedical use.3,4 A recent study found the prevalence of past-year cannabis use among primary care patients routinely screened for cannabis use in a state with legal nonmedical use was greater than 20%.5
Documentation of patients’ medical cannabis use in the electronic health record (EHR) can support patient-clinician discussions of the risks of cannabis use and exploration of treatment alternatives. Patients use cannabis for a variety of health conditions,6,7,8,9,10 and although evidence suggests potential benefit for neuropathic pain, appetite, nausea and vomiting, spasticity, and short-term sleep outcomes, most health conditions for which patients use cannabis have insufficient or nonexistent evidence of benefit, potential contraindications, and more effective first-line treatment options.11,12,13 Moreover, cannabis use has known risks, including increased risk of cannabis and other substance use disorders, mental health disorders, acute care utilization, and withdrawal.13,14,15,16,17,18,19,20,21
The prevalence of EHR-documented medical cannabis use may be low in comparison to self-reported prevalence.22,23 The recent study of patients routinely screened for past-year cannabis use5 also found that only 2% of patients had documentation of medical cannabis use in their EHR over a 1-year period, including documentation of explicit (ie, medical use) and implicit (ie, use to self-manage a health condition or symptom) medical use.
To understand how EHR documentation of medical use compares with patient report, we used a confidential patient survey to (1) estimate the prevalence of explicit and implicit medical cannabis use among primary care patients in a state with legal nonmedical cannabis use, and (2) compare the performance of EHR-documented medical cannabis use with patient-reported medical cannabis use on the survey as the reference standard.
Methods
Study Sample
This survey study received approval and waivers of consent (to identify eligible sample), documentation of informed consent (for survey respondents), and HIPAA (Health Insurance Portability and Accountability Act) authorization from the Kaiser Permanente Washington (KPWA) Health Research Institute institutional review board. This study follows the American Association for Public Opinion Research (AAPOR) reporting guideline for mixed-mode surveys.24
The eligible primary care sample included adult (aged ≥18 years) patients who completed a single-item cannabis screen (eg, index cannabis screen) between January 28, 2019, and September 12, 2019, during routine primary care in KPWA (Figure).25,26 KPWA is a large integrated health insurance plan and delivery system in Washington State, where nonmedical cannabis use has been legal since 2012 and can be purchased for medical use without physician authorization.27 Patients who were KPWA employees (approximately 4%), needed an interpreter (2.6%), lived outside Washington State (<1%), were recently deceased (<1%), or opted out of EHR research (<1%) were excluded. The screen, adapted from a validated alcohol screen,28,29 assessed the frequency of past-year cannabis use with the question, “How often in the past year have you used marijuana?” with response options of never, less than monthly, monthly, weekly, or daily/almost daily. More than 80% of KPWA primary care patients are screened annually for marijuana use, without reference to medical or nonmedical use.26,30
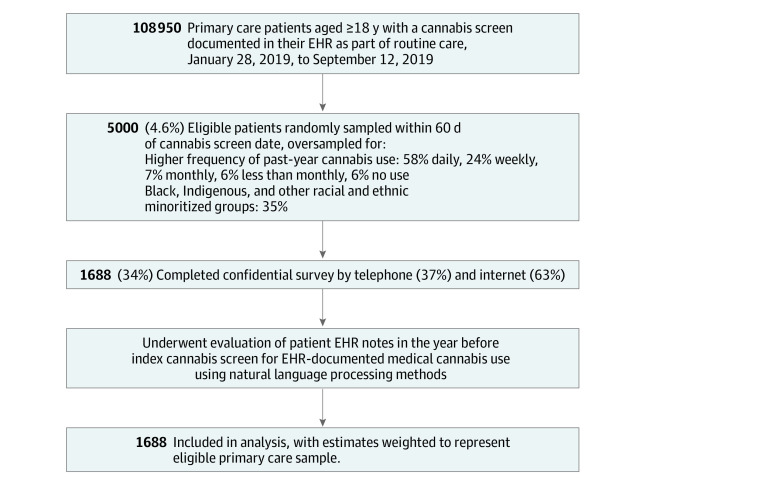
Figure. Flow Diagram of Study Sample.
Patients who were Kaiser Permanente Washington employees, needed an interpreter, lived outside Washington State, were recently deceased, or opted out of EHR research were excluded. Other racial and ethnic minoritized groups includes American Indian, Alaskan Native, Asian, Pacific Islander, Black/African American, Hispanic/Latinx, and Multiracial. EHR indicates electronic health record.
Among 108 950 primary care patients eligible from March 28, 2019, to September 12, 2019, 5000 (4.6% of eligible), including patients who reported no past-year cannabis use, were randomly sampled within 60 days of their index cannabis screen date to ensure proximity of survey to index screen (Figure). Patients were oversampled for higher frequency of past-year cannabis use and for members of racial and ethnic minoritized groups, including Hispanic/Latinx, to ensure adequate representation of racial and ethnic minoritized groups and those who use cannabis. Sampled patients received a mailed invitation, information about confidentiality, request to access patient EHR data, web-survey URL, unique study identifier, a $2 incentive, and notification of receipt of compensation ($20) for survey completion. Follow-up reminder calls offered telephone completion, prompts to complete online, and/or an offer to email the survey link. Patients acknowledged informed consent before completing the survey.
Data Collection
Data were obtained from patient’s survey responses and EHRs. The survey, developed with an expert panel of cannabis researchers (G.L.S., R.L.P., R.V., E.A.M., S.R.B., and M.A.H.) and co-investigators (U.E.G., C.H., K.C.B., I.A.B., C.I.C., A.J.S., K.A.B., and G.T.L.), was designed to assess primary care patient cannabis use, including medical use. Question selection was iterative to achieve consensus and included previously published medical use questions,22 as well as new items, including a question to assess the patient’s health reasons for use (implicit medical cannabis use). The survey was pilot tested for feasibility and acceptability with a convenience sample, including coauthors and KPWA research staff and acquaintances, before administration. The survey included 75 items (eAppendix in the Supplement) and took an average of 20 minutes. Respondents were instructed to consider a comprehensive definition of cannabis/cannabinoid use, including marijuana, cannabis concentrates, edibles, lotions, ointments, and tinctures made with cannabis, as well as CBD-only (cannabidiol) products.
Demographic data (eg, age, sex, race, ethnicity, and insurance), collected from patients by KPWA and documented in the EHR before or at the time of the index cannabis screen, were obtained for both survey respondents and nonrespondents to allow for nonresponse weighting. EHR data on free-text documentation of medical cannabis use and International Statistical Classification of Diseases and Related Health Problems, Tenth Revision (ICD-10) codes for diagnoses in the year before the index screen date were also obtained for respondents.
Measures
Patient Report of Medical Cannabis Use on a Confidential Survey
The survey first asked 2 questions about the frequency and recency of past-year cannabis use (the only 2 required for survey completion). Those with a response other than never for past-year use (ie, indicating patient report of past-year cannabis use) were asked additional questions, including 2 about past-year medical use. The primary survey measure of interest, which was used previously,22,31 asked explicitly about medical and nonmedical cannabis use (without defining medical use), as follows: “When you used marijuana/cannabis during the past year, was it: (1) for medical reasons, (2) for nonmedical reasons, or (3) both medical and nonmedical reasons?” Patients were considered to have patient report of explicit medical cannabis use if they reported any medical use (ie, both medical and nonmedical or only medical). Another question, developed as a measure of implicit medical or health reasons for cannabis use, asked patients about their reasons for use with the question, “During the past year, have you used marijuana/cannabis to help you manage any of the following? [Check all that apply]”. Response options, based on health reasons patients frequently report for using cannabis,6,7,8,9,10 included separate yes/no checkboxes for pain, muscle spasm, seizures, nausea or vomiting, sleep, stress, appetite, worry or anxiety, depression or sadness, focus or concentration, other symptoms (write-in option), and none. A binary indicator of patient report of implicit medical use was created for patient report of any of the 11 reasons, including other symptoms.
EHR-Documented Medical Cannabis Use
Patients were categorized as having EHR-documented medical cannabis use if more than 1 EHR note and/or an ICD-10 diagnosis indicated medical cannabis use. To identify medical cannabis use in respondent EHRs, a binary indicator of past-year medical cannabis use was created from EHR text records using methods described previously.5,32 Medical use was defined by clinician recommendation or characterized by clinician or patient as use to manage a health condition or symptom, explicitly (eg, medical marijuana most days) or implicitly (eg, cannabis for low back pain). Although the EHR did not prompt clinicians to document medical use, clinicians could document reasons for use in notes. In brief, all patient EHR notes, within the year before the index cannabis screen date, were evaluated using an automated machine-learned natural language processing (NLP) algorithm applied to EHR notes to (1) identify cannabis and cannabinoid terms (eg, marijuana, cannabis, THC [tetrahydrocannabinol], CBD, or pot); (2) flag nonrelevant cannabis mentions (eg, negated, historical, and hypothetical); and (3) identify relevant mentions of implicit and/or explicit medical cannabis use, according to previously defined terms.32 The automated NLP algorithm, validated specifically for medical cannabis use, achieved high specificity (94%) and limited sensitivity (67%) in a validation study32 and was augmented with NLP-assisted manual review to identify medical cannabis use mentions not captured by the algorithm.
Other Measures
Other survey measures included patient report of frequency of past-year cannabis use, marital status, and type of residence. Other EHR measures included EHR-documented frequency of past-year use (from index cannabis screen) and number of days with any free-text documentation (ie, note-days), log-transformed, to account for greater opportunity for EHR-documentation associated with greater health care use.
Statistical Analysis
All analyses were weighted to account for stratified random survey sampling and nonresponse, unless noted otherwise, so that prevalence estimates were representative of the eligible primary care sample (Figure). To account for survey sampling, weights were created for the inverse proportion of eligible patients randomly sampled within each of 10 strata resulting from 5 cannabis screen responses and the indicator for patients from racial and ethnic minoritized groups (eTable 1 in the Supplement).33,34 Inverse probability weights were estimated using logistic regression to account for differences between respondents and nonrespondents according to demographic characteristics available at sampling. The 2 weights, multiplied, were applied to survey respondent data to obtain estimates representative of the eligible primary care sample (eTable 2 in the Supplement).35
Unweighted characteristics of survey respondents and nonrespondents were compared using 2-sided χ2 tests of independence with significance set at P < .05. Demographic and clinical characteristics of the primary care sample (ie, survey respondents weighted to eligible primary care sample) were described on the basis of survey and EHR data. Main analyses estimated the weighted prevalence of medical cannabis use based on patient report and EHR documentation, with 95% CIs to convey precision of estimates.36,37 Each outcome measure was modeled using logistic regression with robust SEs38,39 adjusted for patient age, sex, race, ethnicity, and insurance, education, marital, employment, and residential status. Analyses of EHR-documented medical cannabis use were also adjusted for note-days.5 Secondary analyses repeated models for the subsample who reported any past-year cannabis use on the survey.
Patient report measures of explicit and implicit medical cannabis use were used as reference standards to evaluate the performance of EHR-documented medical cannabis use. Specifically, the weighted sensitivity, specificity, positive predictive value (PPV), and negative predictive value (NPV) of EHR-documented medical cannabis use, along with 95% CIs, were estimated with logistic regression in comparison to patient report of explicit and implicit medical cannabis use.40 Analyses were conducted using Stata statistical software version 15.1 (StataCorp).41 Data were analyzed from November 2020 to December 2021.
Results
A total of 1688 patients responded to the survey, a mean (SD) of 77 (26) days after their index cannabis screen (mean [SD] age, 50.7 [17.5] years, 861 female [56%], 1184 White [74%], 1514 non-Hispanic [97%], and 1059 commercially insured [65%]) (Table 1). Respondents differed from nonrespondents, with a greater proportion of respondents being women, aged 65 years and older, White, and Medicare-insured compared with nonrespondents (eTable 2 in the Supplement). The main study sample included 1688 survey respondents (63% online [1063 respondents], 37% by telephone [625 respondents]) and had a 34% response rate, consistent with current health survey research.42,43 Weighted results, presented hereafter, indicated that the prevalence of any past-year cannabis use reported by primary care patients on the survey was 38.8% (95% CI, 31.9%-46.1%), whereas the prevalence of past-year cannabis use documented in the EHR was 21.9% (95% CI, 18.3%-26.0%) (eTable 2 in the Supplement).
Table 1. Characteristics of the Primary Care Sample .
| Characteristic | Primary care sample (N = 1688) | |
|---|---|---|
| Patients, % (SE)a | Patients, No.b | |
| Sex | ||
| Male | 44.1 (4.1) | 827 |
| Female | 55.9 (4.1) | 861 |
| Age, y | ||
| 18-25 | 9.1 (2.4) | 246 |
| 26-35 | 17.2 (3.1) | 479 |
| 36-44 | 15.0 (3.2) | 222 |
| 45-64 | 31.0 (3.9) | 423 |
| ≥65 | 27.7 (3.4) | 318 |
| Race | ||
| American Indian/Alaskan Native | 0.1 (<1) | 13 |
| Asian/Pacific Islander | 9.1 (2.3) | 88 |
| Black/African American | 4.6 (1.7) | 135 |
| Multiracialc | 3.6 (1.5) | 109 |
| Other/unknownc | 8.4 (2.5) | 158 |
| White | 74.2 (3.7) | 1184 |
| Hispanic ethnicity | 3.3 (1.0) | 174 |
| Insurance | ||
| Medicaid/subsidized | 6.0 (1.8) | 189 |
| Medicare | 27.1 (3.4) | 323 |
| Commercial | 64.9 (3.7) | 1059 |
| Unknown | 2.0 (0.8) | 124 |
| Educationd | ||
| Less than high school | 2.8 (1.5) | 34 |
| High school graduate or GED | 9.9 (2.3) | 282 |
| Some college | 38.6 (4.0) | 665 |
| 4-y college degree | 13.4 (2.5) | 378 |
| >4-y college degree | 34.4 (4.0) | 316 |
| Missing | 0.9 (0.8) | 10 |
| Marital statusd | ||
| Married | 57.0 (4.1) | 695 |
| Widowed | 3.0 (1.3) | 43 |
| Divorced/separated | 9.2 (2.4) | 166 |
| Single/never married | 24.1 (3.5) | 505 |
| Living with partner | 5.8 (1.5) | 271 |
| Missing | 0.9 (0.8) | 8 |
| Employment statusd | ||
| Employed | ||
| Full-time | 55.4 (4.1) | 988 |
| Part-time | 12.6 (2.9) | 152 |
| School/vocational | 1.7 (1.1) | 47 |
| Retired | 22.0 (3.1) | 298 |
| Homemaker | 3.4 (1.5) | 38 |
| Unemployed | 0.8 (0.2) | 58 |
| Disabled | 2.4 (1.3) | 73 |
| Other | 0.8 (0.6) | 28 |
| Residenced | ||
| Own | 67.7 (3.8) | 883 |
| Rent | 28.9 (3.7) | 694 |
| Living with friends/family | 2.1 (1.1) | 82 |
| No permanent residence | 0.4 (0.1) | 21 |
| Missing | 0.9 (0.8) | 6 |
| Frequency of past-year cannabis use (survey)d | ||
| None | 61.2 (3.7) | 99 |
| Less than monthly | 14.6 (2.5) | 99 |
| Monthly | 5.8 (1.6) | 118 |
| Weekly | 7.3 (1.4) | 376 |
| Daily or almost daily | 11.1 (1.7) | 996 |
Percentage was calculated from survey data weighted for sampling and nonresponse rates for eligible primary care sample.
Number was calculated from unweighted survey data.
Patients are provided the option to indicate other when choosing among 1 or more race categories at appointing or check-in. Patients who indicated more than 1 race are reported as multiracial.
Indicates data from survey; all other data are from electronic health record.
The prevalence of patient report of explicit medical cannabis use was 26.5%; (95% CI, 21.6%-31.3%), including 15.5% (95% CI, 10.3%-19.8%) who reported medical use only and 10.9% (95% CI, 8.4%-13.4%) who reported both medical and nonmedical use (Table 2). Another 12.3% (95% CI, 9.0%-15.6%) reported nonmedical use only. The prevalence of patient report of implicit medical use (ie, any health reason for use) was 35.1% (95% CI, 29.3%-40.3%). The most common health reasons for cannabis use included pain (28.4%), sleep (19.0%), stress (19.0%), worry or anxiety (14.6%), and depression or sadness (9.6%). The prevalence of past-year EHR-documented medical cannabis use was 4.8% (95% CI, 3.45%-6.2%) (Table 2).
Table 2. Prevalence of Primary Care Patient Medical Cannabis Use According to Measures From a Survey and Electronic Health Record Documentation.
| Medical cannabis use measure | Patients, % (95% CI)a |
|---|---|
| Patient survey responses | |
| Use of cannabis in past year was for | |
| Nonmedical reasons | 12.3 (9.0-15.6) |
| Medical reasons | 15.5 (101.3-19.8) |
| Both medical and nonmedical reasons | 10.9 (8.4-13.4) |
| Did not use cannabis in past year | 61.2 (55.3-67.2) |
| Patient report of explicit medical cannabis useb | 26.5 (21.6-31.3) |
| Use of cannabis in past year to help manage any of the following | |
| Pain | 28.4 (23.2-33.7) |
| Sleep | 19.0 (15.1-22.9) |
| Stress | 19.0 (14.8-23.2) |
| Worry or anxiety | 14.6 (11.3-17.9) |
| Depression or sadness | 9.6 (7.2-11.9) |
| Muscle spasm | 8.2 (5.5-10.8) |
| Nausea or vomiting | 6.1 (4.1-8.2) |
| Focus or concentration | 3.6 (2.4-4.8) |
| Appetite | 3.4 (2.6-4.2) |
| Other | 3.2 (1.6-4.7) |
| Seizures | 0.1 (0.1-0.2) |
| None | 3.7 (2.0-5.4) |
| Patient report of implicit medical cannabis usec | 35.1 (29.3-40.8) |
| EHR documented measure | |
| Medical cannabis use (explicit and/or implicit)d | 4.8 (3.4-6.2) |
Abbreviation: EHR, electronic health record.
Percentage was calculated from survey data weighted for sampling and nonresponse rates to estimate eligible primary care sample, and adjusted for age, sex, race, ethnicity, insurance, education, marital, employment, and residential status, as well as note-days for the EHR-documented measure.
Includes report of medical only and both medical and nonmedical reasons for cannabis use.
Includes any above reasons for use except none.
EHR-documented medical cannabis use was assessed in year before the index cannabis screen documented in the EHR.
Among the 38.8% of patients who reported past-year cannabis use on the survey, the prevalence of patient report of explicit medical use was 68.1% (95% CI, 62.8%-73.5%); 40.1% (95% CI, 33.4%-46.8%) reported medical use only, and 28.2% (95% CI, 23.0%-33.3%) reported both medical and nonmedical use (eTable 3 in the Supplement). Nonmedical use only was reported by 31.8% (95% CI, 26.5%-37.0%). Among those who reported past year use, the prevalence of patient report of implicit medical use was 89.6% (95% CI, 85.6%-93.5%). Finally, 7.7% (95% CI, 6.2%-9.2%) of patients who reported past-year cannabis use on the survey had EHR-documented medical use (eTable 3 in the Supplement).
When compared with patient report of explicit medical cannabis use as the reference standard, EHR-documented medical cannabis use had a sensitivity of 10.0% (95% CI, 4.4%-15.6%), specificity of 97.1% (95% CI, 94.4%-99.8%), PPV of 55.4% (95% CI, 28.3%-82.6%), and NPV of 75.0% (95% CI, 68.9%-81.1%). Performance characteristics were similar when EHR-documented medical use was compared with patient report of implicit medical cannabis use (Table 3).
Table 3. Performance of EHR-Documented Medical Cannabis Use When Compared With Patient Report of Medical Use Among Primary Care Patients.
| Patient reportb | EHR-documented medical cannabis use, % (95% CI)a | |||
|---|---|---|---|---|
| Sensitivity | Specificity | PPV | NPV | |
| Explicit medical use | 10.0 (4.4-15.6) | 97.1 (94.4-99.8) | 55.4 (28.3-82.6) | 75.0 (68.9-81.1) |
| Implicit medical use | 8.4 (4.1-12.7) | 97.2 (94.1-1.00) | 61.9 (33.4-90.4) | 66.3 (59.3-73.3) |
Abbreviations: EHR, electronic health record; NPV, negative predictive value; PPV, positive predictive value.
Percentage was calculated from survey data weighted for sampling and nonresponse rates for eligible primary care sample.
Cannabis use was determined by patient report on a survey.
Discussion
Patients using cannabis for medical reasons may benefit from information on risks of use and evidence-based treatment alternatives. Yet, little is known about the prevalence of medical cannabis use among primary care populations or how often medical records reflect patient medical cannabis use. This survey study, conducted in a state with legal nonmedical cannabis use, found that medical cannabis use was common among primary care patients: 26.5% reported explicit medical cannabis use and 35.1% reported use of cannabis for health reasons—predominantly to manage pain, sleep, stress, anxiety, and depression. In contrast, the prevalence of EHR-documented medical cannabis use was 4.8% among all primary care patients. EHR-documented medical cannabis use had a low sensitivity for medical cannabis use when compared with patient report, identifying 10.0% or less of patients who reported explicit or implicit medical cannabis use.
To our knowledge, this is the first study to estimate the prevalence of medical cannabis use among primary care patients according to confidential patient report. Previous studies have estimated the prevalence of medical cannabis use in patients in specialty care settings,44,45,46,47 with specific health conditions,47,48,49,50,51 or recruited into research52,53 (range 2%-30%). This study’s survey used purposive population-based sampling, which allowed for prevalence estimates representative of primary care patients in a large health system and resulted in estimates of medical cannabis use higher than other recent surveys,22,23,54,55,56 yet comparable to estimates of cannabis use in states with legal nonmedical use.57
Asking patients about their health reasons for cannabis use may be more informative than asking explicitly about medical use. Although 26.5% of primary care patients reported medical cannabis use, 25% more patients reported a health reason for use (35.1%). These results suggest that asking patients about their use of cannabis for managing health concerns, such as pain, mood, and sleep, may identify more medical cannabis use than only asking explicitly about medical use.
This study demonstrated that most medical cannabis use is not documented in the medical record—EHR documentation missed 90% of patient self-reported cannabis use for health reasons (10.0% sensitivity equates to 90.0% of patient-reported medical use not documented). Although future exploration is needed, lack of EHR documentation may reflect absence of health system support for or prioritization of documentation, clinician priorities, and/or medical training.58,59 Lack of documentation may also reflect clinician reluctance to explore medical cannabis use with patients.60,61,62 In the study by Matson et al,5 patients with EHR documentation of medical use had a higher prevalence of health conditions with potential risks from cannabis use compared with patients with no or other past-year use, suggesting that patient comorbidity may also be associated with documentation.
Documentation of health reasons for cannabis use may help clinicians identify contraindications, drug interactions, and patient-initiated substitution of prescribed medications for cannabis.15,63,64 Moreover, documentation can support patient-centered discussions, desired by patients,65 about the limited benefits of cannabis use for some health conditions, insufficient evidence for cannabis use for other conditions (eg, depression and anxiety), the potential for cannabis to exacerbate or cause symptoms, and the availability of safer or more effective treatment options.58,59,65,66,67 Combined with cannabis screening, routinely asking about health reasons for use could improve recognition and documentation of medical cannabis use and the management of health conditions for which cannabis is being used.
Limitations
This study has important limitations. First, 34% of invited patients completed the survey. Although this rate is consistent with nationally declining response rates, higher than industry averages for telephone (18%) and online (29%) surveys, and within the range of state-level response rates for US Centers for Disease Control and Prevention annual health-risk survey (25%-60%), it is lower than desired.68,69 Second, a small number of respondents represented a large number of primary care patients who did not use cannabis according to their index screen (eTable 4 in the Supplement). However, characteristics of the weighted sample reflect those of the eligible primary care sample and KPWA patients overall,5 suggesting weights adequately compensate for sampling and survey nonresponse. Third, this study took place within a health system that routinely screens for the frequency of any past-year cannabis use. Although screening does not ask about medical use, it could have led to discussions of patient health reasons for cannabis use.70 This study could not address how often such discussions occurred but were not documented. Fourth, although time between the index screen and survey was brief, changes in cannabis use could have occurred between measures. Moreover, the survey used an inclusive definition of cannabis/cannabinoid use, which was likely associated with 25% of respondents reporting past-year use on the survey despite EHR-documentation of no past-year cannabis use. Both limitations could have influenced comparisons, with patients reporting greater use on the survey than documented in the clinical setting. Additionally, although respondents reflected the demographics of primary care patients in a single health system in 1 state, findings may not generalize to other primary care populations and settings, particularly in states where cannabis use is not legal.
Conclusions
Among primary care patients in a large integrated health system in Washington State, 35.1% of patients reported using cannabis for health reasons—predominantly pain, sleep, stress, anxiety, and depression—while 26.5% reported medical cannabis use in the past year. Only 10.0% of patients who reported medical cannabis use on the survey had medical cannabis use documented in their EHR. Asking patients about use of cannabis to manage health conditions alongside routine cannabis screening may improve recognition and documentation of medical cannabis use and the management of health conditions for which cannabis is being used.
eAppendix. Patient Survey
eTable 1. Proportion of the Eligible Primary Care Sample Who Were Randomly Sampled and Received the Survey Within Each of 10 Strata Based on EHR-Documentation of the Frequency of Past-Year Cannabis Use and Racial and Ethnic Minoritized Group Status
eTable 2. Comparison of Patient Characteristics for Each Sample Using Data Available From the EHR
eTable 3. Patient Report and EHR-Documentation of Medical Cannabis Use Among Primary Care Patients Who Reported Past Year Cannabis Use on the Survey
eTable 4. Unweighted Crosstabulation of EHR-Documented Compared With Patient Survey-Report of the Frequency of Past-Year Cannabis Use
References
- 1.Hasin D, Walsh C. Trends over time in adult cannabis use: a review of recent findings. Curr Opin Psychol. 2021;38:80-85. doi: 10.1016/j.copsyc.2021.03.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Compton WM, Han B, Jones CM, Blanco C, Hughes A. Marijuana use and use disorders in adults in the USA, 2002–14: analysis of annual cross-sectional surveys. Lancet Psychiat. 2016;3(10):954-964. doi: 10.1016/S2215-0366(16)30208-5 [DOI] [PubMed] [Google Scholar]
- 3.National Conference of State Legislatures . Cannabis overview. Updated July 6, 2021. Accessed March 12, 2021. https://www.ncsl.org/research/civil-and-criminal-justice/marijuana-overview.aspx
- 4.Hall W, Stjepanović D, Caulkins J, et al. Public health implications of legalising the production and sale of cannabis for medicinal and recreational use. Lancet. 2019;394(10208):1580-1590. doi: 10.1016/S0140-6736(19)31789-1 [DOI] [PubMed] [Google Scholar]
- 5.Matson TE, Carrell DS, Bobb JF, et al. Prevalence of medical cannabis use and associated health conditions documented in electronic health records among primary care patients in Washington State. JAMA Netw Open. 2021;4(5):e219375. doi: 10.1001/jamanetworkopen.2021.9375 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Salazar CA, Tomko RL, Akbar SA, Squeglia LM, McClure EA. Medical cannabis use among adults in the southeastern United States. Cannabis. 2019;2(1):53-65. doi: 10.26828/cannabis.2019.01.005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Ryan-Ibarra S, Induni M, Ewing D. Prevalence of medical marijuana use in California, 2012. Drug Alcohol Rev. 2015;34(2):141-146. doi: 10.1111/dar.12207 [DOI] [PubMed] [Google Scholar]
- 8.Boehnke KF, Scott JR, Litinas E, Sisley S, Williams DA, Clauw DJ. Pills to pot: observational analyses of cannabis substitution among medical cannabis users with chronic pain. J Pain. 2019;20(7):830-841. doi: 10.1016/j.jpain.2019.01.010 [DOI] [PubMed] [Google Scholar]
- 9.Nunberg H, Kilmer B, Pacula RL, Burgdorf J. An analysis of applicants presenting to a medical marijuana specialty practice in California. J Drug Policy Anal. 2011;4(1):1. doi: 10.2202/1941-2851.1017 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Reinarman C, Nunberg H, Lanthier F, Heddleston T. Who are medical marijuana patients? population characteristics from nine California assessment clinics. J Psychoactive Drugs. 2011;43(2):128-135. doi: 10.1080/02791072.2011.587700 [DOI] [PubMed] [Google Scholar]
- 11.Abrams DI. The therapeutic effects of cannabis and cannabinoids: an update from the National Academies of Sciences, Engineering and Medicine report. Eur J Intern Med. 2018;49:7-11. doi: 10.1016/j.ejim.2018.01.003 [DOI] [PubMed] [Google Scholar]
- 12.Whiting PF, Wolff RF, Deshpande S, et al. Cannabinoids for medical use: a systematic review and meta-analysis. JAMA. 2015;313(24):2456-2473. doi: 10.1001/jama.2015.6358 [DOI] [PubMed] [Google Scholar]
- 13.National Academies of Sciences Engineering and Medicine . The Health Effects of Cannabis and Cannabinoids: The Current State of Evidence and Recommendations for Research. The National Academies Press; 2017. [PubMed] [Google Scholar]
- 14.Hasin D, Walsh C. Cannabis use, cannabis use disorder, and comorbid psychiatric illness: a narrative review. J Clin Med. 2020;10(1):15. doi: 10.3390/jcm10010015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Volkow ND, Baler RD, Compton WM, Weiss SR. Adverse health effects of marijuana use. N Engl J Med. 2014;370(23):2219-2227. doi: 10.1056/NEJMra1402309 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16.Karila L, Roux P, Rolland B, et al. Acute and long-term effects of cannabis use: a review. Curr Pharm Des. 2014;20(25):4112-4118. doi: 10.2174/13816128113199990620 [DOI] [PubMed] [Google Scholar]
- 17.Hall W. What has research over the past two decades revealed about the adverse health effects of recreational cannabis use? Addiction. 2015;110(1):19-35. doi: 10.1111/add.12703 [DOI] [PubMed] [Google Scholar]
- 18.Hill KP. Cannabis use and risk for substance use disorders and mood or anxiety disorders. JAMA. 2017;317(10):1070-1071. doi: 10.1001/jama.2016.19706 [DOI] [PubMed] [Google Scholar]
- 19.Blanco C, Hasin DS, Wall MM, et al. Cannabis use and risk of psychiatric disorders: prospective evidence from a US national longitudinal study. JAMA Psychiatry. 2016;73(4):388-395. doi: 10.1001/jamapsychiatry.2015.3229 [DOI] [PubMed] [Google Scholar]
- 20.Olfson M, Wall MM, Liu SM, Blanco C. Cannabis use and risk of prescription opioid use disorder in the United States. Am J Psychiatry. 2018;175(1):47-53. doi: 10.1176/appi.ajp.2017.17040413 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Matson TE, Lapham GT, Bobb JF, et al. Cannabis use, other drug use, and risk of subsequent acute care in primary care patients. Drug Alcohol Depend. 2020;216:108227. doi: 10.1016/j.drugalcdep.2020.108227 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22.Schauer GL, King BA, Bunnell RE, Promoff G, McAfee TA. Toking, vaping, and eating for health or fun: marijuana use patterns in adults, U.S., 2014. Am J Prev Med. 2016;50(1):1-8. doi: 10.1016/j.amepre.2015.05.027 [DOI] [PubMed] [Google Scholar]
- 23.Pacula RL, Jacobson M, Maksabedian EJ. In the weeds: a baseline view of cannabis use among legalizing states and their neighbours. Addiction. 2016;111(6):973-980. doi: 10.1111/add.13282 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.The American Association for Public Opinion Research . Standard definitions: final dispositions of case codes and outcome rates for surveys. 9th ed. 2016. Accessed May 5, 2022. https://www.aapor.org/Publications-Media/AAPOR-Journals/Standard-Definitions.aspx
- 25.Lapham GT, Lee AK, Caldeiro RM, et al. Frequency of cannabis use among primary care patients in Washington state. J Am Board Fam Med. 2017;30(6):795-805. doi: 10.3122/jabfm.2017.06.170062 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Sayre M, Lapham GT, Lee AK, et al. Routine assessment of symptoms of substance use disorders in primary care: prevalence and severity of reported symptoms. J Gen Intern Med. 2020;35(4):1111-1119. doi: 10.1007/s11606-020-05650-3 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27.Klieger SB, Gutman A, Allen L, Pacula RL, Ibrahim JK, Burris S. Mapping medical marijuana: state laws regulating patients, product safety, supply chains and dispensaries, 2017. Addiction. 2017;112(12):2206-2216. doi: 10.1111/add.13910 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Babor TF, Higgins-Biddle JC, Saunders JB, Monteiro MG. AUDIT: The Alcohol Use Disorders Identification Test: guidelines for use in primary care. 2nd ed. World Health Organization; 2001. [Google Scholar]
- 29.WHO ASSIST Working Group . The Alcohol, Smoking and Substance Involvement Screening Test (ASSIST): development, reliability and feasibility. Addiction. 2002;97(9):1183-1194. doi: 10.1046/j.1360-0443.2002.00185.x [DOI] [PubMed] [Google Scholar]
- 30.Yeung K, Richards J, Goemer E, et al. Costs of using evidence-based implementation strategies for behavioral health integration in a large primary care system. Health Serv Res. 2020;55(6):913-923. doi: 10.1111/1475-6773.13592 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Centers for Disease Control and Prevention . Behavioral Risk Factor Surveillance System survey data. US Department of Health and Human Services. Accessed March 12, 2021. https://www.cdc.gov/brfss/index.html
- 32.Carrell DS, Cronkite DJ, Shea M, et al. Clinical documentation of patient-reported medical cannabis use in primary care: toward scalable extraction using natural language processing methods. Subst Abus. 2022;43(1):917-924. doi: 10.1080/08897077.2021.1986767 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Horvitz DGTD. A generalization of sampling without replacement from a finite universe. J Am Stat Assoc. 1952;47(260):633-665. doi: 10.1080/01621459.1952.10483446 [DOI] [Google Scholar]
- 34.Kish L. Survey Sampling. John Wiley & Sons, Inc.; 1965. [Google Scholar]
- 35.Brick JM, Kalton G. Handling missing data in survey research. Stat Methods Med Res. 1996;5(3):215-238. doi: 10.1177/096228029600500302 [DOI] [PubMed] [Google Scholar]
- 36.du Prel JB, Hommel G, Röhrig B, Blettner M. Confidence interval or p-value?: part 4 of a series on evaluation of scientific publications. Dtsch Arztebl Int. 2009;106(19):335-339. doi: 10.3238/arztebl.2009.0335 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Finch S, Cumming G. Putting research in context: understanding confidence intervals from one or more studies. J Pediatr Psychol. 2009;34(9):903-916. doi: 10.1093/jpepsy/jsn118 [DOI] [PubMed] [Google Scholar]
- 38.Basu A, Rathouz PJ. Estimating marginal and incremental effects on health outcomes using flexible link and variance function models. Biostatistics. 2005;6(1):93-109. doi: 10.1093/biostatistics/kxh020 [DOI] [PubMed] [Google Scholar]
- 39.Kleinman LC, Norton EC. What’s the risk? a simple approach for estimating adjusted risk measures from nonlinear models including logistic regression. Health Serv Res. 2009;44(1):288-302. doi: 10.1111/j.1475-6773.2008.00900.x [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Trevethan R. Sensitivity, specificity, and predictive values: foundations, pliabilities, and pitfalls in research and practice. Front Public Health. 2017;5:307. doi: 10.3389/fpubh.2017.00307 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41.StataCorp . Stata Statistical Software: Release 15. StataCorp LLC; 2017. [Google Scholar]
- 42.Guo Y, Kopec JA, Cibere J, Li LC, Goldsmith CH. Population survey features and response rates: a randomized experiment. Am J Public Health. 2016;106(8):1422-1426. doi: 10.2105/AJPH.2016.303198 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 43.Lallukka T, Pietiläinen O, Jäppinen S, Laaksonen M, Lahti J, Rahkonen O. Factors associated with health survey response among young employees: a register-based study using online, mailed and telephone interview data collection methods. BMC Public Health. 2020;20(1):184. doi: 10.1186/s12889-020-8241-8 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44.Ashrafioun L, Bohnert KM, Jannausch M, Ilgen MA. Characteristics of substance use disorder treatment patients using medical cannabis for pain. Addict Behav. 2015;42:185-188. doi: 10.1016/j.addbeh.2014.11.024 [DOI] [PubMed] [Google Scholar]
- 45.Nussbaum AM, Thurstone C, McGarry L, Walker B, Sabel AL. Use and diversion of medical marijuana among adults admitted to inpatient psychiatry. Am J Drug Alcohol Abuse. 2015;41(2):166-172. doi: 10.3109/00952990.2014.949727 [DOI] [PubMed] [Google Scholar]
- 46.Davis AK, Bonar EE, Ilgen MA, Walton MA, Perron BE, Chermack ST. Factors associated with having a medical marijuana card among veterans with recent substance use in VA outpatient treatment. Addict Behav. 2016;63:132-136. doi: 10.1016/j.addbeh.2016.07.006 [DOI] [PubMed] [Google Scholar]
- 47.Park JY, Wu LT. Prevalence, reasons, perceived effects, and correlates of medical marijuana use: a review. Drug Alcohol Depend. 2017;177:1-13. doi: 10.1016/j.drugalcdep.2017.03.009 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 48.Chong MS, Wolff K, Wise K, Tanton C, Winstock A, Silber E. Cannabis use in patients with multiple sclerosis. Mult Scler. 2006;12(5):646-651. doi: 10.1177/1352458506070947 [DOI] [PubMed] [Google Scholar]
- 49.Storr M, Devlin S, Kaplan GG, Panaccione R, Andrews CN. Cannabis use provides symptom relief in patients with inflammatory bowel disease but is associated with worse disease prognosis in patients with Crohn’s disease. Inflamm Bowel Dis. 2014;20(3):472-480. doi: 10.1097/01.MIB.0000440982.79036.d6 [DOI] [PubMed] [Google Scholar]
- 50.Furler MD, Einarson TR, Millson M, Walmsley S, Bendayan R. Medicinal and recreational marijuana use by patients infected with HIV. AIDS Patient Care STDS. 2004;18(4):215-228. doi: 10.1089/108729104323038892 [DOI] [PubMed] [Google Scholar]
- 51.Waissengrin B, Urban D, Leshem Y, Garty M, Wolf I. Patterns of use of medical cannabis among Israeli cancer patients: a single institution experience. J Pain Symptom Manage. 2015;49(2):223-230. doi: 10.1016/j.jpainsymman.2014.05.018 [DOI] [PubMed] [Google Scholar]
- 52.Roy-Byrne P, Maynard C, Bumgardner K, et al. Are medical marijuana users different from recreational users? The view from primary care. Am J Addict. 2015;24(7):599-606. doi: 10.1111/ajad.12270 [DOI] [PubMed] [Google Scholar]
- 53.Browne KC, Levya Y, Malte CA, Lapham GT, Tiet QQ. Prevalence of medical and non-medical cannabis use among veterans enrolled in primary care. Psychol Addict Behav. 2022;36(2):121-130. doi: 10.1037/adb0000725 [DOI] [PubMed] [Google Scholar]
- 54.Compton WM, Han B, Hughes A, Jones CM, Blanco C. Use of marijuana for medical purposes among adults in the United States. JAMA. 2017;317(2):209-211. doi: 10.1001/jama.2016.18900 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Dai H, Richter KP. A national survey of marijuana use among US adults with medical conditions, 2016-2017. JAMA Netw Open. 2019;2(9):e1911936. doi: 10.1001/jamanetworkopen.2019.11936 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 56.Han B, Compton WM, Blanco C, Jones CM. Trends in and correlates of medical marijuana use among adults in the United States. Drug Alcohol Depend. 2018;186:120-129. doi: 10.1016/j.drugalcdep.2018.01.022 [DOI] [PubMed] [Google Scholar]
- 57.Goodman S, Wadsworth E, Leos-Toro C, Hammond D; International Cannabis Policy Study team . Prevalence and forms of cannabis use in legal vs. illegal recreational cannabis markets. Int J Drug Policy. 2020;76:102658. doi: 10.1016/j.drugpo.2019.102658 [DOI] [PubMed] [Google Scholar]
- 58.Carlini BH, Garrett SB, Carter GT. Medicinal cannabis: a survey among health care providers in Washington state. Am J Hosp Palliat Care. 2017;34(1):85-91. doi: 10.1177/1049909115604669 [DOI] [PubMed] [Google Scholar]
- 59.Keerthy D, Chandan JS, Abramovaite J, et al. Associations between primary care recorded cannabis use and mental ill health in the UK: a population-based retrospective cohort study using UK primary care data. Psychol Med. 2021;1-10. doi: 10.1017/S003329172100386X [DOI] [PMC free article] [PubMed] [Google Scholar]
- 60.Ng JY, Gilotra K, Usman S, Chang Y, Busse JW. Attitudes toward medical cannabis among family physicians practising in Ontario, Canada: a qualitative research study. CMAJ Open. 2021;9(2):E342-E348. doi: 10.9778/cmajo.20200187 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Schauer GL, Njai R, Grant AM. Clinician beliefs and practices related to cannabis. Cannabis Cannabinoid Res. Published online April 26, 2021. doi: 10.1089/can.2020.0165 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Philpot LM, Ebbert JO, Hurt RT. A survey of the attitudes, beliefs and knowledge about medical cannabis among primary care providers. BMC Fam Pract. 2019;20(1):17. doi: 10.1186/s12875-019-0906-y [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Hall W, Degenhardt L. Adverse health effects of non-medical cannabis use. Lancet. 2009;374(9698):1383-1391. doi: 10.1016/S0140-6736(09)61037-0 [DOI] [PubMed] [Google Scholar]
- 64.Boehnke KF, Litinas E, Worthing B, Conine L, Kruger DJ. Communication between healthcare providers and medical cannabis patients regarding referral and medication substitution. J Cannabis Res. 2021;3(1):2. doi: 10.1186/s42238-021-00058-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Bobitt J, Qualls SH, Schuchman M, et al. Qualitative analysis of cannabis use among older adults in Colorado. Drugs & Aging. 2019;36:655-666. doi: 10.1007/s40266-019-00665-w [DOI] [PubMed] [Google Scholar]
- 66.Bahji A, Stephenson C, Tyo R, Hawken ER, Seitz DP. Prevalence of cannabis withdrawal symptoms among people with regular or dependent use of cannabinoids: a systematic review and meta-analysis. JAMA Netw Open. 2020;3(4):e202370. doi: 10.1001/jamanetworkopen.2020.2370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Fischer B, Russell C, Sabioni P, et al. Lower-risk cannabis use guidelines: a comprehensive update of evidence and recommendations. Am J Public Health. 2017;107(8):e1-e12. doi: 10.2105/AJPH.2017.303818 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Czajka JL, Beyler A. Declining response rates in federal surveys: trends and implications. 2016. Accessed March 12, 2021. https://www.mathematica.org/our-publications-and-findings/publications/ declining-response-rates-in-federal-surveys-trends-and-implications-background-paper
- 69.Behavioral Risk Factor Surveillance System . 2019 Summary of Data Quality Report. 2019. Accessed November 1, 2021. https://www.cdc.gov/brfss/annual_data/2019/pdf/2019-sdqr-508.pdf
- 70.Richards JE, Bobb JF, Lee AK, et al. Integration of screening, assessment, and treatment for cannabis and other drug use disorders in primary care: an evaluation in three pilot sites. Drug Alcohol Depend. 2019;201:134-141. doi: 10.1016/j.drugalcdep.2019.04.015 [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
eAppendix. Patient Survey
eTable 1. Proportion of the Eligible Primary Care Sample Who Were Randomly Sampled and Received the Survey Within Each of 10 Strata Based on EHR-Documentation of the Frequency of Past-Year Cannabis Use and Racial and Ethnic Minoritized Group Status
eTable 2. Comparison of Patient Characteristics for Each Sample Using Data Available From the EHR
eTable 3. Patient Report and EHR-Documentation of Medical Cannabis Use Among Primary Care Patients Who Reported Past Year Cannabis Use on the Survey
eTable 4. Unweighted Crosstabulation of EHR-Documented Compared With Patient Survey-Report of the Frequency of Past-Year Cannabis Use