Abstract
Introduction
This systematic review attempts to answer the following question – which strategies to improve clinical nursing documentation have been most effective in the acute hospital setting?
Methods
A keyword search for relevant studies was conducted in CINAHL and Medline in May 2019 and October 2020.
Studies were appraised using the Joanna Briggs Institute (JBI) critical appraisal for quasi-experimental studies. The studies were graded for level of evidence according to GRADE principles.
The data collected in each study were added to a Summary of Data (SOD) spreadsheet. Pre intervention and a post intervention percentage compliance scores were calculated for each study where possible i.e. (mean score/possible total score) × (100/1). A percentage change in compliance for each study was calculated by subtracting the pre intervention score from the post intervention score. The change in compliance score and the post intervention compliance score were both added to the SOD and used as a basis for comparison between the studies. Each study was analyzed thematically in terms of the intervention strategies used. Compliance rates and the interventions used were compared to determine if any strategies were effective in achieving a meaningful improvement in compliance.
Results
Seventy six full text articles were reviewed for this systematic review. Fifty seven of the studies were before and after studies and 66 were conducted in western countries. Publishing dates for the studies ranged from 1991 to 2020.
Eleven studies included documentation audits with personal feedback as one of the strategies used to improve nursing documentation. Ten of these studies achieved a post intervention compliance rate ≥ 70%.
Conclusion
Notwithstanding the limitations of this study, it may be that documentation audit with personal feedback, when combined with other context specific strategies, is a reliable method for gaining meaningful improvements in clinical nursing documentation. The level of evidence is very low and further research is required.
Keywords: nursing documentation, hospitals, quality improvement, systematic review
Introduction
Clinical documentation is the process of creating a written or electronic record that describes a patient's history and the care given to a patient (Blair & Smith, 2012; Wilbanks et al., 2016). It serves as an important communication tool for the exchange of information between healthcare providers and it is stored in a printed or electronic medical record (Duclos-Miller, 2016; Mishra et al., 2009). According to Wilbanks et al. (2016) good quality documentation has been defined as documentation that is correct and comprehensive, uses clear terminology, is legible and readable, timely, concise and plausible.
Poor nursing documentation in the acute care setting may have negative impacts on patient outcomes and may also result in litigation (Duclos-Miller, 2016). Therefore it is important to determine if there are any strategies that will provide meaningful improvements in the quality of nursing documentation in the acute care setting.
At the time of writing there were four systematic reviews related to nursing documentation. Three (Johnson et al., 2018; Müller-Staub et al., 2006; Saranto et al., 2014) examined the impacts of standardized nursing languages (SNL) on the quality of nursing documentation. They were narrative reviews, and include studies that were not necessarily confined to the acute sector. They demonstrated that SNL will improve the quality of nursing documentation, assist in the fulfilment of the legal requirements of documentation and facilitate the use of an electronic health record (EHR). One systematic review (McCarthy et al., 2019) examined the effects of electronic nursing documentation and found that utilizing an END system could improve the quality of nursing documentation, decrease documentation errors and increase compliance with nursing documentation guidelines.
These systematic reviews were narrative in structure and no attempt has been made to determine if the improvement in each of the studies reviewed is a clinically meaningful improvement. The aim of this systematic review is to qualitatively and quantitatively analyze the literature in an attempt to determine which strategies to improve compliance with clinical nursing documentation guidelines, and improve the quality of nursing documentation, have been most effective in the acute setting.
Methods
A systematic review of the literature was conducted following Preferred Reporting Items for Systematic Reviews and Meta-Analyzes (PRISMA) guidelines, where possible.(Page et al., 2021a, b)
Search Strategy
A keyword search for relevant studies was conducted in CINAHL and Medline in May 2019 and again October 2020, due to the time that had elapsed. The only limitations were for articles in peer reviewed journals that were written in English. An analysis of the text words contained in the titles, abstracts and index terms found in relevant articles was used to inform the search strategy. The reference lists of articles selected for inclusion were hand searched for additional articles. The full search strategy for CINAHL is found in Appendix 1.
Inclusion and exclusion criteria
Studies were included if they were quantitative research investigating strategies to improve clinical nursing documentation in acute hospitals. Where possible, the quantitative components of mixed method studies were also included. The nursing documentation components of studies that also involved allied health or medical documentation were included where possible. Studies were not excluded by intervention, we attempted to include as many studies as possible (See Table 1).
Table 1.
Inclusion and Exclusion Criteria.
| Included | Excluded | |
|---|---|---|
| Population | Clinical nursing documentation in acute hospitals – care plans, flow sheets, nursing assessment, observations, diagnosis, interventions, outcomes, discharge summaries, patient education, adverse drug reactions | Allied health, doctors, students, complimentary health, chaplains, dentists, primary care, residential care, palliative care, community care, clinical coding, trauma registers, incident reports, medication charts |
| Intervention | Strategies to improve clinical nursing documentation e.g. education, EHR, SNL, clinical governance, process improvement, audit and feedback, form modification | Nil |
| Outcome | Quantifiable changes in the quality of clinical nursing documentation | Changes in the quality of nursing documentation that are not quantifiable |
| Study type | Quantitative studies – Randomized Controlled Trials (RCT), and quasi experimental studies e.g. before and after, cross section, Plan Do Study Act (PDSA) time series analysis, randomized trials; that are published in English in a peer reviewed journal; the quantitative components of mixed method studies. | Qualitative studies, studies in a language other than English, studies not published in a peer reviewed journal. |
Study selection
Abstract and title screening from the database results lists was initially performed by the principal reviewer and citations were downloaded into EndNote X9 if they appeared relevant. The abstracts in EndNote were then screened independently by both reviewers and conflicts were resolved by discussion. Full text screening was undertaken by the principal reviewer.
Data extraction
A Summary of Data (SOD) excel spreadsheet was prepared by the principal reviewer. For each study that met the selection criteria the following data were extracted - author, year of publication, country of origin, study title, aims, study design, setting, sample size, method of randomization, interventions used, instruments used to collect data, statistical analyzes performed, outcome measures, results and conclusions.
Quality appraisal
Studies included in this systematic review were quasi-experimental studies and were appraised for risk of bias by the principal reviewer using the JBI critical appraisal for quasi-experimental studies (Tufanaru et al., 2017). The JBI Critical Appraisal Checklist for Randomized Controlled Trials (Tufanaru et al., 2017) was used for the only RCT included in the review. For before and after studies, the pre intervention group was not considered to be a control group. The statistical analyzes performed in the studies were evaluated for appropriateness with reference to the Flow chart for hypothesis tests, categorical and numerical data, found on the back inside cover of Medical Statistics at a Glance by Petrie and Sabin (2020)
Rating the certainty of the evidence was undertaken using the principles of GRADE when a meta-analysis has not been performed (Murad et al., 2017)
Analysis
The analysis was performed by the principal reviewer. Where possible each study was quantitatively analyzed such that the data collected in each study were used to calculate a pre intervention and a post intervention percentage compliance score i.e. (mean score/possible total score) × (100/1). A percentage change in compliance for each study was calculated by subtracting the pre intervention score from the post intervention score. The change in compliance score and the post intervention compliance score were both added to the SOD excel and used as a basis for comparison between the studies.
For each study, a meaningful compliance rate was defined as a post intervention compliance rate ≥ 70%, using the definition of compliance as defined within the study . This was chosen as it seems a satisfactory return on investment for the time, effort and resources that are often expended to improve nursing compliance with clinical documentation.
Each study was analyzed thematically in terms of the intervention strategies used. The themes were education alone, audit and feedback, EHR versus paper health record, SNL, EHR modifications, new forms, guidelines, and system changes. Each study was coded according to all of the intervention strategies that were applied, and the codes were recorded on the SOD spreadsheet. See Table 2 for a definition of each of the themes.
Table 2.
Definition of the Themes.
| Education alone | Training sessions, handouts, instructional emails, quizzes, prompt cards, meetings, coaching, awareness raising, elearning, simulation, workshops, champions, orientation |
| Audit and feedback | Paper or EHR documentation audits with general feedback or personal feedback to nurses |
| EHR vs paper record | Electronic health records, eDisharge applications, computer generated care plans, computerized patient assessment - compared to equivalent paper based records. |
| SNL | Standardized nursing languages – North American Nursing Diagnosis Association (NANDA) nursing diagnoses; Nursing Interventions Classification (NIC); Nursing Outcomes Classification (NOC); VIPS (an acronym for well-being, integrity, prevention and safety); Problem Etiology Signs/Symptoms (PES) |
| EHR modifications | Enhancements in the EHR, triggers, prompts, automatic suggestions, reconfigurations to reduce the number of clicks, shortcuts, forced functions, hard stops, passive visual cues, mandatory fields, ability to import notes, automatic defaults |
| New forms | New or modified paper forms and new or modified EHR templates |
| Guidelines | Documentation guidelines, standard operating procedures, policies, protocols, standards |
| System changes | Provision of equipment, cohorting of patients, ward clerks checking notes for completion, a multidisciplinary approach, avoiding duplication of nursing notes, measurement Monday, mandating compliance |
This review is as a narrative synthesis with a quantitative component. For each of the thematic strategies, the post intervention compliance scores were compared to determine if any of the strategies were effective in achieving a meaningful improvement in the quality of nursing documentation. Studies that achieved large improvements in compliance from a very low initial compliance base may not have achieved a final compliance rate of ≥ 70%, therefore good performances may have been missed in this analysis. To compensate for this, studies that achieved an improvement of ≥ 50% were also identified and analyzed in terms of strategies employed.
Ethics approval was sought and was not required.
Results
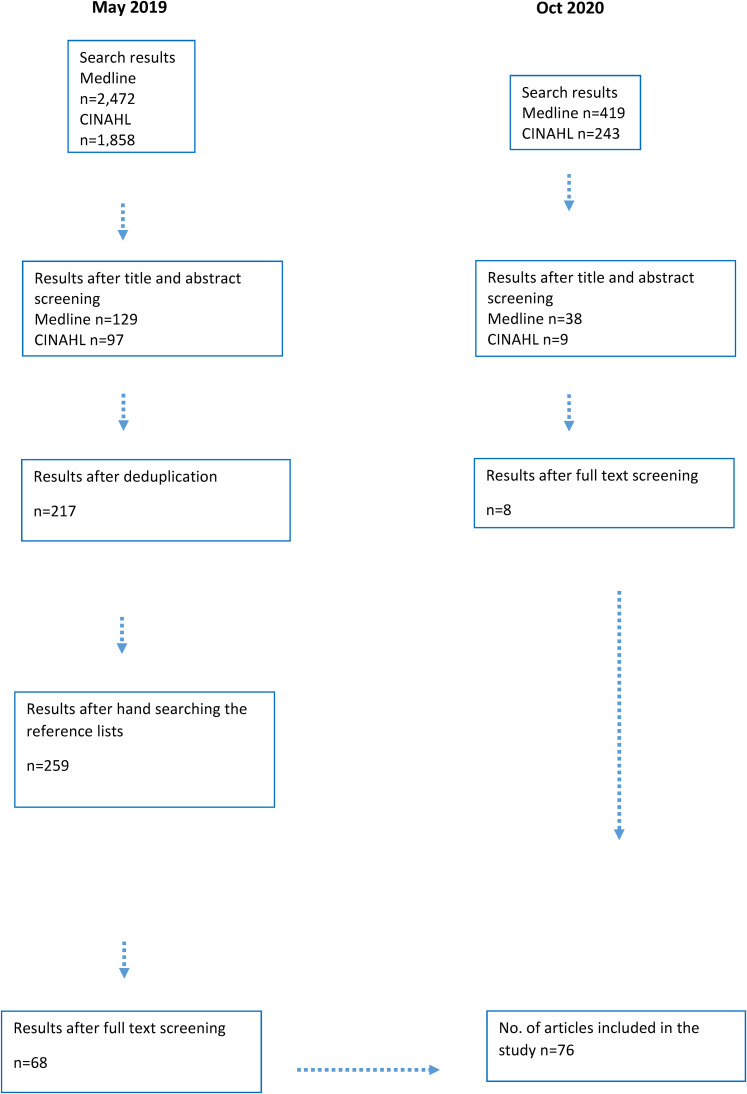
An initial search was performed in May 2019. Due to the time that had elapsed, a follow up search was performed in October 2020. See Figure 1 PRISMA Diagram below
Figure 1.
PRISMA diagram for searches conducted in 2019 and again in 2020 due to the time that had elapsed
Studies were excluded after full text review if they did not meet the inclusion criteria for this study (see Table 1).
No studies were excluded after critical appraisal, we attempted to include as many studies as possible.
Seventy six full text articles were reviewed for this study. See Appendix 2 for The Summary of Data table. You can download the data in the SOD spreadsheet from here https://osf.io/8r49s/files/
Fifty seven of the studies were before and after studies, with the remainder being cross sectional studies (six), Plan Do Study Act studies (four), non-randomized controlled studies (four), time course analyzes (two), randomized trials (two) and one randomized controlled trial. Sixty six studies were conducted in western countries including the USA, Canada, Europe, the UK and Australia. The remainder were conducted in Jordan, Kenya, Brazil, Iran and Singapore. Publishing dates for the studies ranged from 1991 to 2020, all but seven of the studies were conducted in the last 20 years.
Nine of the studies included in this review used education as their only strategy to improve nursing compliance with clinical documentation (Cone et al., 1996; Finn, 1997; Griffiths et al., 2007; Jackson, 2010; Lieow et al., 2019; Linch et al., 2017; Müller-Staub et al., 2008; Mykkänen et al., 2012; Phillips et al., 2019). Of these studies, four had a post-intervention compliance rate ≥ 70% (Jackson, 2010; Lieow et al., 2019; Müller-Staub et al., 2008; Mykkänen et al., 2012).
Twenty two studies had audit and feedback as one of the strategies used to improve compliance with nursing documentation (Azzolini et al., 2019; Bernick & Richards, 1994; Cline, 2016; Elliott, 2018; Ellis et al., 2007; Esper & Walker, 2015; Gerdtz et al., 2013; Gloger et al., 2020; Gordon et al., 2008; Goulding et al., 2015; Hayter & Schaper, 2015; Hom et al., 2019; Jacobson et al., 2016; Kamath et al., 2011; Okoyo Nyakiba et al., 2014; O’Connor et al., 2014; Porter, 1990; Stocki et al., 2018; Tejedor et al., 2013; Trad et al., 2019; Unaka et al., 2017; Wissman et al., 2020). Sixteen of these studies had a final compliance rate ≥ 70%. However if the feedback is personal, the number of studies with a compliance rate ≥ 70% improves to ten out of 11 studies (Bernick & Richards, 1994; Cline, 2016; Elliott, 2018; Esper & Walker, 2015; Gloger et al., 2020; Hayter & Schaper, 2015; Jacobson et al., 2016; Kamath et al., 2011; O’Connor et al., 2014; Unaka et al., 2017; Wissman et al., 2020). Download Table 3 Audit and personal feedback from here https://osf.io/8r49s/files/
When audit and feedback are combined with the use of a pre-existing EHR the results are also encouraging (Cline, 2016; Elliott, 2018; Esper & Walker, 2015; Gerdtz et al., 2013; Gloger et al., 2020; Hayter & Schaper, 2015; Hom et al., 2019; Jacobson et al., 2016; Kamath et al., 2011; Tejedor et al., 2013; Unaka et al., 2017). Ten of the 11 studies had a final compliance rate ≥ 70%.
Thirteen studies compared EHR with paper records as one of the strategies for increasing nursing documentation compliance (Akhu-Zaheya et al., 2018; Ammenwerth et al., 2001; Dahlstrom et al., 2011; Gunningberg et al., 2008; Gunningberg et al., 2009; Higuchi et al., 1999; Hübner et al., 2015; Larrabee et al., 2001; Mansfield et al., 2001; Rabelo-Silva et al., 2017; Rykkje, 2009; Thoroddsen et al., 2011; Tubaishat et al., 2015). Six of these studies demonstrated a final compliance rate ≥ 70% when an EHR was utilized. It should be noted that Larrabee et al. (2001) had a high compliance rate, however the improvement was 0.2%. Two studies, (Akhu-Zaheya et al., 2018; Rykkje, 2009) demonstrated a decline in compliance when comparing EHR to paper based records.
Ten studies involved the use of SNL as one of the strategies to improve nursing documentation (Björvell et al., 2002; Darmer et al., 2006; Larrabee et al., 2001; Melo et al., 2019; Müller-Staub et al., 2007; Nøst et al., 2017; Rabelo-Silva et al., 2017; Rykkje, 2009; Thoroddsen et al., 2011; Thoroddsen & Ehnfors, 2007). Four of these studies had a final compliance rate ≥ 70% (Larrabee et al., 2001; Müller-Staub et al., 2007; Thoroddsen et al., 2011; Thoroddsen & Ehnfors, 2007). It should be noted that although Larrabee et al. (2001) had a final compliance rate of 84.2%, the improvement was 0.2%.
Ten studies utilized EHR modifications as one of the strategies to improve nursing documentation (Bruylands et al., 2013; Chineke et al., 2020; Esper & Walker, 2015; Gerdtz et al., 2013; Hom et al., 2019; Jacobson et al., 2016; Kamath et al., 2011; Nielsen et al., 2014; Sandau et al., 2015; Tejedor et al., 2013). Seven of these studies had a final compliance rate ≥ 70% (Chineke et al., 2020; Esper & Walker, 2015; Hom et al., 2019; Jacobson et al., 2016; Kamath et al., 2011; Nielsen et al., 2014; Tejedor et al., 2013). Prompts were used in four of the studies (Chineke et al., 2020; Hom et al., 2019; Kamath et al., 2011; Sandau et al., 2015), and except for Sandau et al. (2015) they all had a final compliance of ≥ 80%.
Thirty two studies used new forms as one of their strategies for improving nursing documentation (Aparanji et al., 2018; Björvell et al., 2002; Bono, 1992; Cahill et al., 2011; Chineke et al., 2020; Christie, 1993; Dahlstrom et al., 2011; de Rond et al., 2000; Dehghan et al., 2015; Elliott et al., 2017; Ellis et al., 2007; Enright et al., 2015; Florin et al., 2005; Förberg et al., 2012; Gerdtz et al., 2013; Gordon et al., 2008; Hayter & Schaper, 2015; Higuchi et al., 1999; Hospodar, 2007; Hübner et al., 2015; Kamath et al., 2011; Karp et al., 2019; Khresheh & Barclay, 2008; Mansfield et al., 2001; Mitchell et al., 2010; Nomura et al., 2018; Nøst et al., 2017; O’Connor et al., 2014; Stewart et al., 2009; Stocki et al., 2018; Thoroddsen & Ehnfors, 2007; Unaka et al., 2017). Seventeen of the 32 studies had a final compliance rate ≥ 70%.
Twelve studies included changes to guidelines, procedures or policies as one of the strategies to improve nursing documentation (Considine et al., 2006; Elliott, 2018; Flores et al., 2020; Gordon et al., 2008; Gunningberg et al., 2008; Habich et al., 2012; Jacobson et al., 2016; Margonary et al., 2017; Mitchell et al., 2010; Nomura et al., 2018; Trad et al., 2019; Turner & Stephenson, 2015). Five of these studies achieved a final compliance rate ≥ 70% (Elliott, 2018; Flores et al., 2020; Gordon et al., 2008; Jacobson et al., 2016; Nomura et al., 2018). It should be noted that the results for Elliott (2018) must be used with caution as some negative results may have left out in the final calculation of compliance rates.
Ten studies included administrative or system changes as one of the strategies to improve nursing documentation (Ammenwerth et al., 2001; Dehghan et al., 2015; Enright et al., 2015; Gerdtz et al., 2013; Kamath et al., 2011; Mansfield et al., 2001; Meyer et al., 2019; Okoyo Nyakiba et al., 2014; Stewart et al., 2009; Trad et al., 2019). All of the system changes improved nursing documentation, six of them had a final compliance rate ≥70% (Ammenwerth et al., 2001; Enright et al., 2015; Kamath et al., 2011; Mansfield et al., 2001; Meyer et al., 2019; Stewart et al., 2009).
Thirty six studies achieved a meaningful compliance rate i.e. a post intervention compliance score ≥ 70%. Download Table 4 Compliance ≥ 70% from here https://osf.io/8r49s/files/
Seven of the studies had an improvement rate of ≥ 50% (Chineke et al., 2020; Gordon et al., 2008; Hayter & Schaper, 2015; Kamath et al., 2011; Müller-Staub et al., 2007; Porter, 1990; Unaka et al., 2017). The post intervention compliance rate was ≥ 80% for all of them, except Hayter and Schaper (2015), where the final compliance rate was 72%.
There are serious concerns regarding the certainty of the evidence, and the evidence has been graded as very low due to methodological limitations and issues with imprecision, inconsistency and publication bias (See Table 5)
Table 5.
Certainty of Evidence.
| GRADE domain | Judgement | Concerns about certainty domains |
|---|---|---|
| Methodological limitations of the studies | There was one RCT, the remainder were quasi experimental. There was a large variations in sample sizes (n = 3 to n = 89,521). p values were not always calculated. Instruments to measure the outcomes were not always validated or tested for reliability. Only 3 of the studies had multiple pre-intervention measures. | Very serious |
| Indirectness | The settings, populations, interventions, outcomes and comparators all provide direct evidence to the question. | Not serious |
| Imprecision | The total number of notes audited was in the tens of thousands, however only two studies reported Confidence Intervals (CI), therefore it is not possible to adequately determine imprecision. | Serious |
| Inconsistency | The direction and magnitude of effect varied across the studies from small decreases in compliance to large improvements in compliance. | Serious |
| Publication bias | There was a comprehensive search and positive and negative results were published, however some relevant studies may have been missed due to the reviewers being unable to access the full text. | Serious |
Discussion
Of the nine studies that used education alone as the strategy to improve nursing documentation, four resulted in a meaningful compliance rate. It was not possible to determine if the form of the education that was applied, e.g. lectures, simulation, case discussion or demonstrations, had any influence on the final outcome of documentation compliance. The number of studies was too small and the descriptions of the education supplied was not always adequate enough to draw any conclusions.
In terms of the hours devoted to education, one study, Müller-Staub et al. (2008), involved 22.5 h of education for a final compliance rate of 94.5%. However another study, Linch et al. (2017) had 30 h of instruction and discussion for a final compliance rate of 45%, therefore it is difficult to draw any conclusions as to whether the amount of time spent on education has any effect on documentation compliance. Bearing in mind the small number of studies that utilized education alone, it appears education alone will improve compliance, however it may not improve compliance to a meaningful extent.
When documentation auditing with personal or individual feedback was one of the strategies utilized, ten out of the 11 studies achieved a compliance rate of 70% or more (see Table 3 https://osf.io/8r49s/files/). This suggests that auditing and personal
feedback, combined with other context specific strategies such as education, new forms, new templates or EHR modifications, may be a reliable strategy for improving compliance. However the results for Elliott (2018) should be used with caution as some negative results may have been left out in the final calculation of compliance rates. When an EHR was used to conduct the audits, the improvement in compliance rate seems to be reliably high; ten out of the 11 studies that used an EHR to conduct the audits achieved a compliance rate of ≥ 70%. This may be due to the fact that the time consuming audit process is made more efficient by using an EHR for data extraction (Lieow et al., 2019).
Thirteen studies utilized an EHR as one of the strategies to improve nursing documentation, six of these achieved a meaningful compliance rate, however for one of these, Larrabee et al. (2001), the improvement was 0.2% It appears from these studies that introducing an EHR may not guarantee a meaningful improvement in nursing documentation, and it may even be counterproductive as shown by the studies Rykkje (2009) and Akhu-Zaheya et al. (2018). In nearly all of the studies the EHR system was not described or named therefore it was not possible to determine if the nature of the EHR had any effect on the results.
Standardized Nursing Language was used in ten studies, four of them achieved a compliance rate of ≥ 70%. The use of NANDA and NIC appears to be more effective than PES or VIPS for improving nursing documentation compliance. Four out of the six studies that used NANDA and NIC had a final compliance rate ≥ 80% (Larrabee et al., 2001; Müller-Staub et al., 2007; Thoroddsen et al., 2011; Thoroddsen & Ehnfors, 2007); however it should be remembered that Larrabee et al. (2001) had 0.2% improvement. Standardized Nursing Language will improve nursing documentation, however it may not improve to a meaningful extent.
Of the 10 studies that used EHR modification, seven achieved a meaningful compliance rate. For the purposes of this systematic review, new or reconfigured EHR templates, are included in the next section - New Forms. Many different EHR modifications were used across the various studies (see Table 2), and there are indications that prompts in the EHR may be useful in improving compliance, however there is no single modification that ensures meaningful compliance.
For the purposes of this systematic review new forms included new or modified paper forms and new or modified EHR templates. Thirty two of the studies included new forms as one of the strategies to improve nursing documentation, seventeen of these studies improved nursing documentation to a meaningful degree.
Of the 12 studies that used the creation of new guidelines or changes to existing guidelines as a strategy, five achieved a meaningful compliance rate. It appears that guidelines will improve nursing documentation but not always to a meaningful degree.
Ten studies utilized administrative or system changes as one of the strategies to improve compliance. The studies were too heterogeneous for any single strategy to be proven effective at providing a meaningful improvement. All of the studies that used system changes showed improved nursing documentation, six out of the ten studies demonstrated improvement to a meaningful degree.
In the future, issues with clinical nursing documentation may be dealt with by technological means, for example the use of digital scribes. Digital scribes will employ advances in speech recognition, natural language processing, artificial intelligence, machine learning and clinical decision support technologies, to translate clinical encounters into meaningful and accurate records (Coiera et al., 2018). However speech recognition systems and artificial intelligence will need to be vastly improved before the benefits outweigh the risks of using a digital scribe. Meanwhile strategies to improve nursing documentation remains a relevant topic for research.
Limitations of the Study
Full text screening and the quantitative and thematic analyzes were performed by one reviewer, this may have caused some bias in the results. There was no funding for this systematic review, therefore full text access to all of the articles that appeared in the search results was not possible, this may have resulted in some relevant research not being included in the final analysis. The research articles that were analyzed in this project were very heterogeneous in terms of design, statistical analyzes and strategies employed, meaning that traditional systematic review meta-analysis was not possible, and the percentage analysis that was undertaken was rudimentary at best. Only data that could be converted to percentages were included, therefore some data were missed in the analysis.
The studies usually combined many strategies, making it difficult to tease out the effects of any single strategy. The time that elapsed between the intervention and the post intervention audits varied between the studies and was not analyzed in this systematic review. This may have disadvantaged the studies that used a longer time interval to determine if the improvements in documentation were sustained over time. The level of certainty of the evidence is very low, (see Table 5). These limitations could be overcome by a follow up study, focusing on audit and personal feedback and utilizing more rigorous statistical analyzes.
Implications for Practice
Documentation audits with personal feedback should be considered as one of the strategies to be utilized when attempts are made to improve the quality of nursing documentation.
Conclusion
Notwithstanding the limitations of this study, it may be that documentation audit with personal feedback, when combined with other context specific strategies, is a reliable method for gaining meaningful improvements in nursing clinical documentation. Utilizing an EHR to perform the audits may be beneficial to the process, by making the audit process more efficient. The certainty in the evidence is very low, therefore using audit and personal feedback as a strategy to improve clinical nursing documentation is an area that would benefit from more research.
Appendix 1. Search strategy in CINAHL October 2020.
| Search | Search terms | Results |
|---|---|---|
| S1 Improvement | Compliance OR clinical governance OR quality improvement OR strategies OR audit OR process improvement OR Clinical Governance OR Quality Improvement | 49,843 |
| S2 Nursing documentation | electronic medical records OR electronic health records OR Documentation OR patient notes OR medical notes OR medical records OR health records OR patient records OR progress notes OR discharge summar* OR care plans OR medication charts OR charting | 13,899 |
| S3 Nursing | Nurs* | 34,956 |
| S4 Hospital | hospital | 52,337 |
| S1 AND S2 AND S3 AND S4 | 243 |
Search limiters – Peer reviewed, in English. Date range: May 2019 - Oct 2020
Appendix 2. Summary of data.
| Author/year/country/title | Study design/sample | Strategies | Outcome measures | Results |
|---|---|---|---|---|
| Forberg, U/ 2012/ Sweden. Title - Accuracy in documentation of peripheral venous catheters in pediatric care: An intervention study in electronic patient records | Before and after study. A retrospective audit of notes before intervention (n = 54), at 4 months (n = 50) and 10 months (n = 37) post intervention. | 1. Standardized EHR template 2. Education | Percentage of notes with complete recording (date, size, side, size at insertion and removal) | Before: Insertion date = 77%, side = 63%, site = 80%, size = 40%, Insertion complete = 31%, removal complete = 0%, complete recording insertion and removal = 0%, any kind = 91%. After: insertion date = 76, side = 87%, site = 93%, size = 62%, insertion complete = 49%, removal complete = 9%, complete recording insertion and removal = 9%, any kind = 93%. |
| Phillips, M/2019/USA Title - Pain assessment documentation after opioid administration at a community teaching hospital | Before and after study. A retrospective audit of notes before intervention (n = 160) and post intervention (n = 160). | 1. Mandatory education | Frequency of documentation of pain scores within appropriate time frame after opioid administration and completed documentation of vital signs after opioid administration. | Frequency of documentation of pain scores within appropriate time frame after opioid administration- pre = 622/1890 administrations (32.9%), post = 547/1,446 (37.8%); Completed documentation of vital signs after opioid administration - pre = 0/1,890(0%), post = −0/1,446(0%). BP before = 12.1%, after = 13.2%; Heart Rate (HR) before = 12.0%, after = 13.1%; Temp before = 906%, after = 9.5%; Respiratory Rate (RR) before = 33.7%, after = 44.1%, sedation level before = 33.5%, after = 44.1% |
| Turner, A/2015/ Australia Title- Documentation of chemotherapy administration by nursing staff in inpatient and outpatient oncology/hematology settings: A best practice implementation project. | Before and after study. Baseline (n = 50) and follow up (n = 50) audit of notes. | 1. Development of documentation guidelines. 2. Education | Percentage compliance with 18 best practice audit criteria | Inpatients: improvements in 12/18 criteria; 2/18 criteria remained 100%; poorer compliance in 4/18 criteria; baseline average compliance across all criteria = 52.72%; average follow up compliance across all criteria = 63.06%. Outpatients: improvements in 10/18 criteria; 3/18 criteria unchanged at 98-100%; poorer compliance in 5/18 criteria; baseline average compliance across all criteria = 71.56%; average follow up compliance across all criteria = 74.89% |
| Porter, Y/1990/USA Title- Brief: Evaluation of nursing documentation of patient teaching | Design: Non randomized controlled trial; hospital wide baseline audit; monthly audits of the control and experimental groups during the study period. N = 150 charts audited monthly during the 4 month study. | Control group 1. Pre-printed care plan 2. Monthly audits. Experimental group - 1. Pre-printed care plan 2. Education, 3. monthly audits with feedback | The average number of charts that had teaching documented. | Hospital wide baseline average = 15% of nursing charts had teaching documented. Control group improved from 15% to 53%. Experimental group improved from 15% to 90% |
| Nost, T/2017/Norway Title- Impact of an education intervention on nursing diagnoses in free-text format in electronic health records: A pretest-post-test study in a medical department in a university hospital. | Before and after study. Pre-test 1 year prior to intervention (n = 49). Post-test 1 month post intervention (n = 50) | 1. SNL nursing diagnoses in PES format 2. Education | Mean scores | Pre-test mean score for nursing diagnosis: quantity = 1.19/3, quality = 1.15/3; post-test mean score for nursing diagnosis: quantity 2.49/3, quality = 1.65/3. Pre-test 3/3 score for quantity = 6.1%, for quality = 0%; post-test 3/3 score for quantity = 62%, for quality = 4%. |
| Hospodar, M/2007/ USA Title- Sticking together! A creative approach to documenting insulin double checks | Before and after study. Baseline prior to implementation (n = 187). Re test 4 weeks into implementation (n = 230). | 1. A Sticker that can be signed and added to the chart.
2. Education |
Total insulin administrations against administrations with double check | Pre intervention 65/187 = 35%. Post intervention 167/230 = 73% |
| Florin, J/2005/Sweden Title- Quality of nursing diagnoses: Evaluation of an educational intervention. | Before and after study. Retrospective pre-test/post-test with a non-equivalent control group. Patient records were selected from a 3 month period before (n = 70) and after (n = 70) the intervention | 1. Education. 2. A new form |
Changes in quality/quantity between pre and post tests and between the intervention and control groups as measured by CAT-CH_ING and the Quality of Nursing Diagnosis scale (QOD) | Experimental- in the experimental unit nursing diagnoses were documented in 34% of records pre and 69% post intervention. QOD for experimental -mean diagnostic score improved from pre = 6.5/14 to post = 8.8/14; QOD control mean - diagnostic score was unchanged with pre = 4.3/14 to post = 4.4/14. CAT-CH-ING experimental - mean quantity and quality increased from pre = 1.5/6 to post = 3.1/6; CAT-CH_ING control - mean quantity and quality was unchanged pre = 0.0/6 to post = 0.1/6. |
| Bernick, L/1994/ Canada Title- Nursing documentation: A program to promote and sustain improvement | Before and after study. Pre-test/post-test audit of progress notes. pre-test audit n = 28, 1 month audit n = 43, 2 months n = 44, 3 months n = 27, 4 months n = 31 | 1. Education 2. Note audits with personal and group feedback. | Analysis was based on the number of criteria not met (errors per progress note) | Mean errors per notes by nursing unit - Unit A - pre = 8.50/35, 1 month = 4.39/34, 2 months = 4.00/35, 3 months = 3.00/35, 4 months = 2.80/35 Unit B - pre = 8.82/35, 1 month = 6.04/35, 2 months = 4.64/35, 3 months = 3.38/35, 4 months = 2.05/35 |
| Finn, L/1997/UK Title- Nurses’ documentation of infection control precautions: 2 | Before and after study. Pre-test/post-test with unmatched samples. Pre-test audit n = 17; post-test audit n = 50. | 1. Education | Percentage compliance with documentation for each item on the instrument. | Pre-test: infection recorded = 23.5%; hand hygiene recorded = 23.5%; protective clothing recorded = 23.5%; decontamination recorded = 11.8%. Post-test: infection recorded = 64.0%; hand hygiene = 32.0%; protective clothing = 42.0%; decontamination = 24.0%. |
| Unaka, N/2017/USA Title- Improving the readability of pediatric hospital medicine discharge instructions | Sequential Plan-Do Study-Act cycles with weekly audits of D/I. 6 months pre intervention n = 166; 11 months intervention n = 713. | 1. Education 2. Templates in the EHR 3. Audit with group and personal feedback | Percentage of D/I at or below 7th grade level, percent of discharge instructions written with a template. | The percentage of D/I written at or below 7th grade readability increased from a mean of 13% to more than 80% in 3 months; The mean was sustained above 90% for 10 months and at 98% for the last 4 months. The average reading level decreased from 10th grade to the 6th grade. The use of templates increased from 0% to 96% and was associated with the largest impact of overall improvements. |
| Tubaishat, A/ 2015/ Jordan Title- Electronic versus paper records: documentation of pressure ulcer data. | A cross-sectional, descriptive, comparative design with a retrospective review of patient records. Hospital using EHR n = 52 records reviewed; Hospital using PR n = 55 records reviewed. | 1. paper record vs electronic health record | Accuracy- congruence between skin inspection and documentation. Completeness- presence of complete documentation i.e. size, grade, location, risk assessment, prevention. | Accuracy: Electronic Health Records (EHRs) = 43/52 (83%) had Pressure Ulcer (PU) documentation; Paper Records (PRs) = 39/55 (71%) had PU documentation. Completeness: for location EHR = 91% vs PR = 82%; for grade EHR = 88% vs PR = 72%; for size EHR = 79% vs PR = 49%; for risk assessment EHR = 81% vs PR = 44%; preventive devices EHR = 72% vs PR = 54%; repositioning EHR = 93% vs PR = 87%. |
| Stocki, D/ 2018/ Northern America Title- Knowledge translation and process improvement interventions increased pain assessment documentation in a large quaternary pediatric post anesthesia unit. | Retrospective observational study, with prospective observational follow up, using the Plan-Do Study-Act (PDSA) method. Benchmark audit n = 99 consecutive Post Anaesthetic Care Unit (PACU) charts audited in the first week of July 2013. Reaudit n = 20 randomly selected charts audited at 4, 5 and 6 months after the initial audit. | 1. PACU charts modified 2. Education 3. Audit and feedback | Proportion of charts that had at least 1 pain assessment documented. | Baseline audit - 68/99 (69%) had at least 1 pain score documented, an average of 4 pain assessments were documented per patient. Pain assessment documentation increased to > 90% at 4 and 5 months, respectively and to 100% by 6 months. |
| Stewart, S/2009/USA Title- “Measurement Monday": One facility's approach to standardizing skin impairment documentation. | Before and after study. A 2 year quality improvement initiative. A Baseline chart audit in 2005 (n = 54). Post intervention chart audits in 2006 (n = 27)and 2007 (n = 27) | 1. Measurement Monday - designate day to measure wounds 2. A documentation tool 3. Education | Percentage of charts without wound measurement documentation. | Charts without wound measurement documentation declined from the baseline audit (2005) = 32/54 (59.3%); 2006 audit = 10/27 (37%); 2007 audit = 4/27 (14.8%). After 2 years the proportion of charts containing complete wound measurement documentation improved from 41% to 85%. |
| Sandau, K/2015/USA Title- Computer-assisted interventions to improve QTc documentation in patients receiving QT-prolonging drugs | Before and after study. A multi-site study with baseline measurements (n = 1517), at 3 months post intervention (n = 1,301) and at 4-6 months post intervention (n = 1,193) | 1. Computerized enhancements in the EHR (prompts and automatic calculation of the QTc) 2. Mandatory education | Whether nurses documented Corrected QT Interval (QTc) measurements in patients EHRs during the hospital stay. Relationship between hospital size and QTc documentation | Results: Percentage of patients who had appropriate QTc documentation at baseline = 263/1,517 (17.3%); at 3 months = 757/1,301 (58.2%); at 4-6 months = 741/1,193 (62.1%). The effect of the intervention was sustained at 6 months after the intervention. Inpatients in larger hospitals were considerably more likely to have QTc documentation than patients at smaller hospitals i.e. 46.4% vs 27.2% |
| Rykkje, L/ 2009/ Norway Title- Implementing Electronic Patient Record and VIPS in medical hospital ward: evaluating change in quantity and quality of nursing documentation by using the audit instrument Cat-ch-Ing. | Before and after study. Pre-test with paper records (PR) in the fall of 2003 (n = 60); post-test in fall of 2004 with EHR and VIPS (n = 60). | 1. Education 2. Electronic record 3. VIPS | Differences in mean values between PRs and EHRs | Mean sum score for PR = 33/82; Mean sum score for EHR = 29.7/82 |
| O’Connor, T./ 2014/USA Title- Improving trauma documentation in the emergency department | Before and After study. An initial retrospective analysis of all trauma charts during a randomly selected month (n = 70). Ongoing chart audits over 8 months for every chart that fit the criteria (n = 1,066). | 1. Education 2. New trauma flow chart 3. Audit and personal feedback by peer review, this was incentivised by being included in the yearly performance evaluations. | The number of charting deficiencies per month to be 15 or fewer; overall quarterly documentation compliance | Deficiencies = no. deficiencies/total no. of charts audited - Sept = 53/156(34%), Oct = 41/122(33%), Nov = 15/124(12%), Dec = 13/130(10%), Jan = 20/122 (16%), Feb = 16/113(14%), March = 21/142(15%), Apr = 19/157(12%). Compliance with vital sign charting rose from 62% to 80%; Neurological charting compliance rose from 47% to 72%. |
| Okoyo Nyakiba, J/2014/ Kenya Title- Reporting and documentation of adverse drug reactions by health care professionals at a Kenyan public hospital: a best practice implementation project. | JBI PACES, in 3 phases - 1. Audit design and a retrospective baseline audit (n = 44), 2. Best practice implementation, 3. Post-implementation audit (n = 30). | 1. Education 2. Ensure availability of reporting forms 3. Provide feedback; 4. An in-house Adverse Drug Reactions (ADR) database was developed. | Percentage compliance with each criteria | Criteria 1. Improved from 7% to 63% compliance. 2. from 0% to 29%. 3. from 45% to 83%. 4. from 9% to 94%. 5. from 2% to 20%. 6. from 5% to 50%. 7 from 5% to 37%. 8. from 2% to 3%. 9. from 0% to 100%. |
| Nomura, A/2018/Brazil Title- Quality of electronic nursing records: the impact of educational interventions during a hospital accreditation process | Before and after, retrospective study. Pre-test 1 month before the accreditation process (n = 112); post-test 1 month after the accreditation process (n = 112). | 1 Education 2. Update the EHR nursing assessment tool 3. Creating an acronyms list 4. Review of standard operating procedures. | Median compliance score (Md) and Interquartile Range (IQR). Percentage change in compliance. | Pre-test Md = 9 (IQR, 7-10); Post-test Md = 19 (IQR, 17-20). Pre-test 67.9% of records were considered compliant, Post-test 83.9% were considered compliant. 9/12 items showed a significant improvement. |
| Mykkanen, M/2012/ Finland Title- Nursing audit as a method for developing nursing care and ensuring patient safety |
Before and after study. Study 1 at the hospital level - audit in 2010 (n = 1274) and reaudit in 2011 (n = 1,366). Study 2 at the Coronary Care Unit (CCU) level - audit Spring 2010 (n = 20), intervention, re audit Autumn 2010 (n = 20) and Spring 2011 (n = 20). | Study 1 -intervention not stated Study 2 CCU - Education | A score out of 1 for each domain, for a total score out of 12. | Results: Study 1 (hospital wide) 2010 = 7.29/12; 2011 = 8.01/12, i.e. the overall level of documentation remained satisfactory. Study 2 (CCU) Spring 2010 = 7.85/12; Autumn 2010 = 11.10/12; Spring 2011 = 11.35/12 i.e. the level of document improved from satisfactory to excellent and was maintained. |
| Meyer, L/2019/USA Title- Cohorting trauma patients in a medical/surgical unit at a level 1 pediatric trauma center to enhance interdisciplinary collaboration and documentation | Before and after study. Data 2.5 years prior to and following the intervention were compared to determine the impact of the interventions on the compliance with FIM and CRAFFT screening documentation by nursing staff. Sample size not stated. | 1. Introduction of cohorting trauma patients to medical/surgical unit 2. Instituting a daily interdisciplinary trauma patient round 3. Education 4. Results from a pre intervention survey were used to improve the systems for documentation. | Percentage change in compliance with FIM and CRAFFT documentation. | 2015 Functional Independence Measure (FIM) = 72%, CRAFFT = 61%; 2016 FIM = 73%, CRAFFT = 64%; 2017 FIM = 94%, CRAFFT = 84%. |
| Margonari, H/2017/ USA Title- Quality improvement initiative on pain knowledge, assessment, and documentation skills of pediatric nurse. | Before and after study. A prospective pre and post intervention design with 3 assessment points - baseline prior to the education session (n = 153), immediately after the education session (n = 159) and follow up at one month after the education session (n = 99). | 1. A survey was conducted to identify specific knowledge deficits. 2. Education 3. Policies, procedures and a protocol were created. | Percentage improvements in pain documentation across 4 domains - 1. Pain assessment done. 2. Appropriate scales used. 3. intervention delivered. 4. Pain reassessment done. | 1. Pain assessment done- baseline = 66/153(43.1%), post = 103/159(64.8%), follow up = 67/99(67.7%). 2. Appropriate scale used- baseline = 20/153(13.1%), post = 123/159(77.4%), follow up = 81/99(81.8%). 3. Intervention delivered - baseline = 3/9(33.3%), post = 21/25(84%), follow up = 8/10(80%). 4. Pain reassessment done- baseline = 7/9(77.8%), post = 11/25(44.0%), follow up = 4/10(40%) |
| Karp, E/2019/USA Title- The changes in efficiency and quality of nursing electronic health record documentation after implementation of an admission patient history essential data set. | Before and after study, experimental pre and post nonrandomised prospective cohort design. Pre intervention data for patient admission histories was collected 30 days prior to the intervention (n = 904), post intervention data was collected over 30 days starting from 20 days post intervention (n = 805). | 1. A modified Delphi evaluation of the original Admission Patient History (APH) 2. Reduce the number of essential data elements from 215 to 58 in EHR. | The percentage of data elements captured and the number of clicks and time to complete an APH. | Results: A 6% increase in the data elements captured from pre-intervention (mean = 48%) to post-intervention (mean = 54%). The average time spent documenting decreased by 72% (6.76 min) The mean decrease in the number of clicks to document the APH was 115.6 (76%). |
| Jackson, S/2010/USA Title- The efficacy of an educational intervention on documentation of pain management for the elderly patient a hip fracture in the Emergency Department | Before and after study. A retroactive chart audit Jan through Aug 2006 (n = 151), intervention from Sept to Oct 2006, post intervention audit Jan through July 2017 (n = 151). | 1. Education | Rate of documentation compliance i.e. 1. Pain assessment within 2 min of admission. 2. First pain treatment < 60 min. 3. Pain reassessment < 60 min after pain treatment. |
1. There was 100% compliance for first pain assessment for pre and post the education intervention. 2. Time to first pain treatment < 60 min = no significant difference. 3. Pain reassessment <60 min after treatment pre = 42%, post = 70%.There was a 28% increase in documentation compliance for reassessment of pain level after treatment following the education intervention. |
| Hayter, K/2015/ USA Title- Improving pain documentation with peer chart review. | Before and after study. Retrospective quality audits of EHR records over a 9 month period. Sample size: not stated (but n = 426 taken from the graph) | 1. Education Tuesday- held weekly in Feb 2010 2. Retrospective audits with feedback, peer chart reviews with personal feedback. 3. Revision of the EHR flow sheet. 4. A quality improvement Registered Nurse Registered Nurse (RN) was assigned to each unit. | Percent of change for the median score of documentation of pain assessment and reassessment. | Results: staff completion rate for peer chart reviews was 85%. Baseline documentation was 17%; after the introduction of Tuesday education documentation decreased to 10%; when peer chart review was initiated the median score of pain documentation increased to 72%. Over 9 months the median score of pain documentation increased from 27% to 72%. |
| Hubner, U/2015/ Germany Title- Evaluating a Proof of Concept approach of the German Health telematics Infrastructure in the context of discharge management. | Randomized trial study. Discharge patients were randomly allocated to the eDischarge group or the paper discharge group. Sample size: eDischarge n = 9, paper discharge n = 3. | 1. An eDischarge application. 2. Education. 3. Two user supporters provided | Completeness measured by sum of entries and a Likert scale. | Results: eDischarges were rated better than paper discharges for completeness i.e. paper = poor to satisfying; eDischarge = sufficient to good. The average number of eDischarge entries was greater than paper discharge entries in 6/8 categories, less in 1/8 and the same in 1/8 categories. eDisharge sum of entries = 18.4, paper sum of entries = 10.7. |
| Kamath, B/2011/USA Title- Using improvement science to increase accuracy and reliability of gestational age documentation | Plan, Do, Study, Act. A prospective cohort study. A baseline audit of EHRs was conducted in Sept 2009 followed by phase I (Fall of 2009) interventions through to phase IV (May 2010) interventions. Sample size: n = 8,795 deliveries. | 1. Education 2. Nurses documenting why EHR cannot be filled 3. Ward clerk checks for completion 4. New form 5. Drs contacted if form incomplete or incorrect 6. Real time audit and personal feedback 7. Stickers for charts with incomplete EHR 8. pregnancy card for pregnant women containing GA information |
Percentage of EHR with complete Gestational Age (GA) dating. | Results: Baseline audit = 69/292 (24.6%), Oct/Nov 2010 audit = 294/361(81.4%). |
| Jacobson, T/2016/USA Title- Enhancing documentation of pressure ulcer prevention interventions: a quality improvement strategy to reduce pressure ulcers. | Before and after study. DMAIC approach - Defining the problem, Measuring performance, Analyzing the process, improving processes, controlling the process improvements. Sample size: not stated. | 1. Computer generated monthly reports 2. EHR modifications e.g. triggers, standardized language and location 3. Education 4. Guidelines 5. Personal feedback |
Documentation of turning, pressure point checks, heel elevation, rewrapping of compression bandages. Avoidable and full thickness Hospital Acquired Pressure Ulcers (HAPUs). | Results: documentation of turning increased and remained above 90%. Pressure point checks on admission improved from 86% to 93%. Documentation of daily pressure point checks rose from 70% to 99%. Documentation of twice a day pressure checks for those at risk rose from 63% to 93%. Heel prevention documentation increased by 18%. Documentation of rewrapping compression bandages improved by 6%. Reportable full thickness PUs that were deemed avoidable decreased by 67%. |
| Higuchi, K/1999/ Canada Title- Factors associated with nursing diagnosis utilization in Canada | Cross section retrospective chart audits of all patients fitting the criteria discharged from the hospital respiratory units from Sept 1992 to April 1993. Hospital A large teaching hospital (n = 40); Hospital B a large teaching hospital, used computer generated care plans, had educational programs (n = 207); Hospital C community hospital, education program, standard care plans (n = 138); Hospital D a community hospital (n = 42). | Hospital A - no education, no standard care plan Hospital B 1.education 2. Computer generated care plans Hospital C 1. Education 2. Standardized care plans Hospital D- no education, no standardized care plan | Charts with nursing diagnoses. | Hospital A 10/40(25%) Hospital B 189/207 (91%) Hospital C 75/138(54%) Hospital D 5/42(12%) |
| Griffiths, P/2007/UK Title- A comprehensive audit of nursing record keeping practice | Before and after study. In Nov 2005 and again in Nov 2006 all inpatient wards were asked to use a pro forma to audit 10 sets of notes for patients under their care at the time. Sample size: 2005 n = 64 wards, 640 patient records. 2006 n = 74 wards, 740 patient records. | 1. A nursing record group was formed 2. Education |
Percentage compliance of documentation with the 91 nursing standards. | Results: 58 wards completed the audit in both 2005 and 2006, 26 wards had a significant increase in compliance across all criteria. 10 criteria increased significantly. An average increase in compliance across all criteria of 4.3%. Traffic light coding showing percentage of standards in each category - GREEN (80-100% compliance) 2005 = 45%, 2006 = 45%; AMBER (50-79% compliance) 2005 = 32%, 2006 = 39%; RED (<50% compliance) 2005 = 23%, 2006 = 16% |
| Goulding, L/2015/UK Title- Improving critical care discharge summaries: a collaborative quality improvement project using PDSA | Plan do Study Act (PDSA). 3 PDSA cycles were undertaken with a real time audits of nursing and medical discharge summaries (D/S) for 2 weeks in each cycle. Sample size: cycle 1 = 38 D/S, cycle 2 = 34 D/S, cycle 3 = 29 D/S. | 1. Audit and feedback 2. Education 3. Financial incentive 4. Focus groups 5. Patient feedback |
Percentage of nursing D/S achieving target of good or excellent; percentage of nursing D/S not achieving target of good or excellent; percentage of nursing D/S missing. Percentage of D/S signed. | Results: Audit 1 - %of nursing D/S achieving target = 70.2; % nursing D/S not achieving target = 21.93; percentage of nursing D/S missing = 7.9; % of D/S signed = 78.9. Audit 2 - % of nursing D/S achieving target = 82.1; % of nursing D/S not achieving target = 10.26/; % of nursing D/S missing = 2.9; % of nursing signed = 82.4 Audit 3 - % of nursing D/S achieving target = 70.1; % of nursing D/S not achieving target = 12.64; % of nursing D/S missing = 17.2; % of nursing D/S signed = 69.0%. |
| Gordon, D/2008/USA Title- Improving reassessment and documentation of pain management | Design: Plan Do Check Act (PDCA). Baseline audit Nov 2005 (n = 85 open charts) Monthly compliance audits Feb, March April 2006, (n = 5 charts on each inpatient unit). Daily audits commencing May 2006, n = 100% of patient records. | 1. Task force formed 2. Policy developed 3. Flow chart modification 4. Education 5. Audit and feedback |
The number of reassessments that were documented within the specified time interval divided by the number of interventions in a 24 h time period. | Results: Baseline - 24% (94/389) of timed reassessments were made within 1 h after any intervention. With monthly audits (Feb - April 2006) this improved to 72%. With daily audits this improved to 94.9% and was sustained at > 90% for 2 years |
| Linch, G/2017/Brazil Title- An educational intervention impact on the quality of nursing records | Before and after study. Baseline audit (n = 30) and audit 5 months after the intervention (n = 30). | 1. Education | Mean values before and after intervention | There were statistically significant improvements post intervention in 20/29 items on the Q-DIO. Before = 11.8/58 (20%). After = 25.9/58 (45%) |
| Enright, K/2015/ Canada Title- Improving documentation of oral chemotherapy at a community cancer center | 3 rapid cycle improvement interventions -Plan Do Study Act (PDSA). Pre intervention assessment n = 25 (data collected Oct 14-18 2013); Second assessment n = 23 (data collected Feb 10-14 2014); Third assessment n = 20 (data collected Sept 15-19 2014). | 1. Identified the most frequently absent components of the
oral chemotherapy care plan 2. The parental flow sheet was adapted for oral chemotherapy. 3. A complete review of the Computerized Physician Order Entry (CPOE) to ensure all oral regimens were available 4. Mandating the use of CPOE for oral prescribing |
The number of components of the oral chemotherapy care plan that were documented in the medical record before the start of a new oral chemotherapy medication. | Results: Pre intervention = 8/12(68%), the improvement was sustained through PDSA 2 and 3, the degree of improvement was dampened. The most recent audit identified a mean of 91% (11/12). Use of the new flow sheet was 75% after PDSA 3. |
| Elliott, L/2018/USA Title- Standardizing documentation: a place for everything | Plan-Do-Check-Act. Pre intervention n = 30 medical records were chosen randomly from patient admissions in April - June 2014. Reaudit from May - Oct 2015 - Sample size not stated; Individual staff audits -every month documentation for one shift was reviewed for 3 patients for each staff member; unit audits of all staff members working on the unit at the time of the audits were conducted monthly during the same period; | 1. EHR flow sheets evaluated and guidelines
created 2. Mandatory education 3. Audits at a unit level 4. Individual audits and feedback. |
Adherence to new documentation standards | Results: Documentation adherence increased in all areas except in education (decreased 15%) and care plan documentation for patients designated as at risk for pressures ulcers (decreased 30%). Staff member adherence for documentation of: Daily care (RN) pre = 73%, post = 84%; daily care (CNA) pre = 67%, post = 88%; When required (PRN) pain charted pre = 80%, post = 93%; PRN pain evaluated pre = 58%, post = 78%; PRN nausea charted pre = 39%, post = 89%; PRN nausea evaluated pre = 28%, post = 71% |
| Elliott, D/2017/ Australia Title- User compliance with documenting on a track and trigger-based observation and response chart: a two-phase multi-site audit study. | Before and after 2 phase, multi-site, multi methods study. Phase 1 n = 818 patient charts were reviewed; phase 2 retrospective audit n = 522 records, prospective audit n = 536 records. | 1. New charts, each site independently selected the chart
that best aligned with their rapid response system
2. A project officer was seconded to each site 3. Education |
Compliance with chart guidelines; rate of chart completion. | Levels of compliance improved with the new chart by 4%-14% across all vital sign parameters. More completed documentation for respiratory rate = 14% increase; oxygen saturation, heart rate and temperature = 8% increase, blood pressure = 7% increase, oxygen flow = 4% increase, level of consciousness = 67%increase and pain score = 32% increase. |
| Cahill, H/2011/ Australia Title- Introduction of a new observation chart and education programme is associated with higher rates of vital-sign ascertainment in hospital wards. | A prospective before and after intervention pre-intervention n = 2,557 observations, 2 weeks post intervention n = 2,435 observations, 3 months post-intervention n = 2,250 observations. | 1. A new observation chart 2. Mandatory education |
Rates of individual vital signs as a proportion of total observation sets. | RR - pre = 47.8%, 2 weeks post = 97.8%, 3months post = 98.5%; BP- pre = 97.7%, 2 weeks post = 99.4%, 3 months post = 99.3%; SpO2 - pre = 97.0%, 2 weeks post = 98.4%, 3 months post = 98.1%; HR - pre = 99.7%, 2 weeks post = 99.7%, 3 months post = 99.9%; full set of vital signs - pre = 47.6%, 2 weeks post = 96.3%, 3 month post = 96.4%; level of consciousness - pre = no data, 2 weeks post = 93.1%, 3 months post = 92.5%. |
| Dahlstrom,M/2011/ USA Title- Improving identification and documentation of pressure ulcers at an urban academic hospital | A quality improvement project with time course analysis. Retrospective chart reviews, 2007 n = 32, 2009 n = 8, all eligible notes were audited. | 1. A Quality Improvement (QI) team and nurse champions were
formed and a Clinical Nurse Specialist (CNS) was
hired 2. Form modification 3. Education 4. Mattress replacement 5. EHR introduced with a PU specific template. |
Proportion of PUs completely documented. | Prior to implementation of the campaign 29% of PUs were completely documented by nurses; after implementation of the wound assessment form and point of care reminders this increased to 46%; with the mattress replacement and resident education there was a further increase to 55%, With the implementation of the EHR (Nov 2008) there was a decrease to 38% with a rise back to 50% in 2009. |
| Considine, J/2006/ Australia Title- Can written nursing practice standards improve documentation of initial assessments of ED patients? | Before and after study pre-test/post-test audits of the Emergency Department (ED) Observation Chart. Pre-test n = 78; post-test n = 74. | 1. Standards were developed 2. Education |
The frequency of documentation of each of the 19 parameters examined. | There were significant improvements in the frequency of documentation for - pre hospital care = 34.1%, cardiac risk factors = 25.2%, past medical history = 15.7%, respiratory effort = 52%, chest auscultation = 19.8%, capillary refill = 16.6%, conscious state = 51.4%. There was a significant decrease in the frequency of documentation of respiratory rate = 18.3% (p = 0.006). There was no significant change in the documentation of oxygen saturation, heart rate or blood pressure. Improvement in the documentation of quality of pain did not reach statistical significance. |
| Cone, K/1996/USA Title- The effect of in-service education on emergency nurses’ documentation of physical assessment | Quasi-experimental post-test design; a treatment group and a comparison group, with audits 3 months post intervention for each group. Treatment group n = 200 charts audited; Comparison group n = 200 charts audited; treatment and comparison groups were comparable on selected demographic characteristics. | 1. Education | A percentage of correctness was determined after placing a score of 1 or 0 for each criteria, mean documentation scores of those who attended the class were compared to those who didn't. | The treatment group documented 8% more cardiac and abdominal criteria than the comparison group; the treatment group documented 15% more neurologic criteria than the comparison and 3% more pulmonary criteria. |
| Cline, M/2016/USA Title- Development of a pain reassessment documentation scorecard | Before and after study. Monthly EHR audits of all pain pharmacological interventions. N = 3,000 audits per unit for the specified time period. | 1. Computer generated monthly audits 2. Personal monthly compliance feedback 3. Compliance score as part of staff annual review 4. Education 5. Friendly competition |
Percentage compliance with pain reassessment documentation. | Compliance improved from 56% to 83% from March 2014 to March 2015. |
| Bjorvell, C/2002/ Sweden Title- Long-term increase in quality of nursing documentation: effects of a comprehensive intervention. | Before and after longitudinal study, 2 hospital wards participated in a 2 year intervention and a 3rd was used for comparison. Patient records were audited before the intervention (audit 1), directly after the intervention (audit 2) and 3 years after the intervention (audit 3). Sample size n = 269 records, 30 from each ward for each audit, one record was unavailable and not used. | 1. Standardized nursing language – VIPS 2. Education 3. Change agents 4. New forms and standardized care plans |
Total mean scores. | For the intervention wards - audit 1 total mean score = 18/80, audit 2 mean = 47/80, audit 3 mean = 42/80; For audit 1 intervention mean = 18/80 vs comparison mean = 13/80; for audit 2 intervention mean = 47/80 vs comparison mean = 18/80; audit 3 intervention mean = 42/80 vs comparison mean = 29/80. The surgical ward showed the largest changes in mean scores and maintained the highest score over time, they were the only ward to develop and use new care plans. |
| Aparanji, K/2018/USA Title- Quality improvement of delirium status communication and documentation for intensive care unit patients during daily multidisciplinary rounds | 2 cycles of Plan-Do-Study-Act, with a baseline audit and audits after each cycle. Pre n = 60, post n = 160; | 1. Education 2. Confusion Assessment Method for the Intensive Care Unit (CAM-ICU) was implemented into the EHR 3. A critical care progress note template incorporating ABCDEF was implemented |
Percentage of patients with a delirium assessment documented by nurses at least once in a 12 h shift. | Results: Day shift - baseline = 40% (12/30), post cycle 1 = 69%(41/59), post cycle 2 = 93% (75/81), Night shift - baseline = 27% (8/30), post cycle 1 = 61% (36/59), post cycle 2 = 71% (56/79). After completion of the project the nurse manager performs quarterly audits and compliance with delirium screening remains consistently high. |
| Akhu-Zaheya, L/2018/ Jordan Title- Quality of nursing documentation: paper-based health records versus electronic-based health records. | Retrospective, descriptive, comparative design. N = 217 records from each of the hospitals for a total of 434 records that had been saved for at least 2 months prior to data collection. | 1. paper record vs electronic health record | Mean differences between paper based and EHRs using Cat-ch-Ing. | Name, date, signature - paper based record mean score = 8.2/13, EHRs = 12.9/13; quantity of content -for paper based record, mean score = 15.08/34 and for EHRs = 10.21/34; quality of content - for paper based record, mean score = 14/24 and for EHRs = 7.98/24; legibility- a significant difference with better EHR legibility. |
| Bruylands,M/2013/ Switzerland Title- Effect on the quality of the nursing care process through an educational program and the use of electronic nursing documentation | A quantitative comparative design comparing the quality of the documented nursing process over time - group 1 (2005) nursing diagnostics (ND) introduced with an education program that was later called GCR; group 2 (2006) GCR program refresher; group 3 (2011) introduction of the e-doc and the GCR program was suspended. Sample: n = 36 Quality of Nursing Diagnoses, Interventions and Outcomes (Q-DIO) datasets for each group. | 1. Education 2. e-doc implemented (an intelligent decision support tool that uses trigger words to automatically suggest ND, and proposes interventions and outcomes when an ND is chosen) |
The mean values of the 4 dimensions of the 29 items of the Q-DIO | The highest levels of quality of the documented nursing process were found after the second GCR training (group 2, 2006). e-doc implementation and suspension of GCR program (group 3, 2011) and introduction of ND (group 1, 2005) were almost on a par. Group 3 could not maintain the high quality level documentation of group 2. |
| Muller-Staub, M/ 2007/ Switzerland. Title- Improved quality of nursing documentation: Results of a nursing diagnoses, interventions, and outcomes implementation study (This is group 1 in the previous study). | Before and after study. A pre-test measurement 1 (n = 36), post-test measurement 2 (n = 36), 1 year after the intervention) | 1. Implementation of standardized nursing languages NANDA,
NIC and NOC (NNN) 2. Education |
Mean scores of the Q-DIO post-test compared to pre-test. | For nursing diagnoses - measurement 1 = 0.92/4, measurement 2 = 3.50/4. Nursing interventions - measurement 1 = 1.27/4, measurement 2 = 3.21/4. Nursing outcomes - measurement 1 = 0.95/4, measurement 2 = 3.02/4 |
| Mansfield, J/2001/USA Title- Linking the Orthopedic office-hospital continuum: Results before and after implementation of an automated patient health history project. | Before and after study. Pre-test n = 29, post-test n = 29. | 1. At the office based orthopedic/surgical practice the
patient assessment process was computerized and streamlined
to avoid duplication. 2. It was sent to the hospital and
this replaced the first 3 pages of the 4 page nursing
Patient Health History form required for new
admissions. |
Compliance with Joint Commission on Accreditation of Healthcare Organizations (JCAHO) documentation standards before and after implementation. | Pre implementation compliance for the 14 items ranged from 27% - 100%. Post implementation compliance was 100% for all items. |
| Mitchell, I/2010/ Australia Title- A prospective controlled trial of the effect of a multi-faceted intervention on early recognition and intervention in deteriorating hospital patients | A prospective before and after controlled trial. Control n = 427, intervention n = 320. | 1. A new ward observation chart was developed 2. Education 3. A policy for vital measurement was developed |
Average daily frequency of documentation of all the vital signs. | The average daily frequency of documentation of all vital sign measurements (BP, RR, HR, Sp02, T) significantly increased, control = 3.4 vs intervention = 4.5; respiratory rate increased from 2.3 to 4.7 |
| Christie, J/1993/UK Title- Does the use of an assessment tool in the accident and emergency department improve the quality of care? | Design: Before and after retrospective audit of nursing notes n = 40 records pre intervention, n = 40 records post intervention. | 1. A new form using the SOAPE model 2. Education |
Change in mean scores from pre to post intervention. | Post audit scores were significantly higher in 5 functions than the pre audit scores; post audit scores for 2 of the functions were not significantly higher. |
| Bono, B/1992/USA Title- Assessment and documentation of the breastfeeding couple by health care professionals | Design: Before and after chart audits i.e. baseline audit June 1990, Breastfeeding Assessment Tool (BAT) used for a month trial period, post intervention audit Oct 1990. Baseline n = charts of 36 mothers and 37 infants, post intervention n = charts of 42 mothers and 40 infants. | 1. The BAT form was developed 2. Education |
Changes in documentation compliance levels, the desired level of compliance was set at 90%. | The results ranged from a 4% improvement in documenting breast status (baseline compliance 84%; post intervention compliance 88%) to a 53% improvement in infant response (baseline 9%; post intervention 62%) |
| Darmer, M/2006/ Denmark Title- Nursing documentation audit - the effect of a VIPS implementation programme in Denmark | Before and after retrospective study across 4 sites. A baseline audit in 2002, a one year audit in 2003, a final two year audit in 2004. n = 50 patient records from each of the sites in 2002, 2003 and 2004 for a total n = 600 patient records. | I. Introduction of modified VIPS 2. Education |
Median score on Cat-ch-Ing out of a possible 76. | The nursing documentation significantly improved during the course of the study; 2002 score = 21/76; 2003 = 36/76; 2004 = 50/76. After the first year the appropriate use of key words was 2.7/3 and 2.8/3 for correct use. After the second year appropriate use of keywords was 2.5/3 and 2.4/3 for correct use of keywords. |
| Gerdtz, M/2013/ Australia Title- Evaluation of a multifaceted intervention on documentation of vital signs at triage: a before-and-after study. | Before and after study, data collection occurred over 5 cycles between March 2011 and May 2012. A comparison was made between the proportion of vital signs documented at Time 1 (T1) and Time 5 (T5). Sample T1 n = 5250, T5 n = 5,008. | 1. Vital sign field reconfigured in the computerized triage
interface 2. Audit and feedback 3. Education 4. Implementation of a tympanic thermometer |
Rates of recording of vital signs at triage. | RR at T1 = 18.5% at T5 = 69.0%, difference = 50.5%; SpO2 at T1 = 18.1% at T5 = 52.4%, difference = 34.3%; HR at T1 = 27.5%, at T5 = 76.1%, difference = 48.6%; Temp at T1 = 10.1%, at T5 = 34.8%, difference = 24.7%; Glasgow Coma Scale (GCS) at T1 = 21.9%, at T5 = 61.6%, difference = 39.6% |
| Gunninberg, L/2009/ Sweden Title- Improved quality and comprehensiveness in nursing documentation of pressure ulcers after implementing an electronic health record in hospital care | Before and after cross sectional, descriptive, comparative, with retrospective review of health records. Sample: 2002 n = 59 paper based records; 2006 n = 71 EHR. | 1. Paper record vs electronic health record. | Proportion of nursing notes with documentation of risk assessment, pressures ulcers and prevention; proportion of notes with a comprehensiveness score ≥ 4. | Ulcer - grade 2002 = 0/59, 2006 = 24/71; size 2002 = 9/59, 2006 = 27/71; location 2002 = 57/59, 2006 = 69/71; risk assessment 2002 = 14/59, 2006 = 36/71; prevention - bed equipment 2002 = 18/59, 2006 = 26/71, repositioning bed 2002 = 31/59, 2006 = 32/71; chair equipment 2002 = 4/59, 2006 = 7/71; repositioning chair 2002 = 0/59, 2006 = 2/71 Comprehensive score ≥ 4 2002 = 9/59, 2006 = 20/71. |
| Khresheh, R/2008/ Jordan Title- Implementation of a new birth record in three hospitals in Jordan: a study of health system improvement | Before and after with an action research approach; audit 1 - pre implementation baseline (n = 180), audit 2 - immediate post implementation (n = 1254), audit 3–7 months post implementation (n = 42). | 1. A new record was developed 2. Education 3. Support from managers and Clinical Directors |
Changes in completion rates of record content. | Audit 1–50% of records were incomplete with important clinical information missing. Audit 2 - more than 75% of the records were fully completed; audit 3 - sustained improvement in the completeness rate. |
| Muller-Staub, M / 2008/ Switzerland Title- Implementing nursing diagnostics effectively: cluster randomized trial. | A cluster randomized trial across 6 wards with a baseline nursing note audit (audit1) followed by another audit (audit 2) at 3-7 months post intervention. Sample: n = 37 nursing diagnoses/interventions/outcomes from each ward at baseline and post intervention for a total of 444 units of investigation. | 1. Education – 3 Intervention wards received guided clinical reasoning (GCR) versus 3 Control wards received classical case discussions | Mean scores for nursing diagnosis, interventions and outcomes for audit 1 and audit 2 for the control group and intervention group | nursing diagnosis - intervention group audit 1 = 2.69/4, audit 2 = 3.70/4; nursing diagnosis - control group audit 1 = 3.13/4, audit 2 = 2.97/4; nursing intervention - intervention group audit 1 = 2.33/4, audit 2 = 3.88/4, nursing intervention - control group audit 1 = 2.70/4, audit 2 = 2.46/4; nursing outcomes - intervention group audit 1 = 1.53/4, audit 2 = 3.77/4, nursing outcomes - control group audit 1 = 2.02/4, audit 2 = 1.94/4. |
| Melo, LS/2019/Brazil Title- Effect of an educational program on the quality of Nursing Process recording | Before and after study. Baseline data collection was for one week prior to the intervention (n = 14 charts), the post intervention audit was for one week after the intervention (n = 14 charts). | 1. Education | The quality of the nursing records evaluated through the Q-DIO. | Total mean Q-DIO score pre intervention = 8.3/58, post intervention = 18.3/58. |
| Rabelo-Silva, E/ 2017/ Brazil Title- Advanced Nursing Process quality: Comparing the International Classification for Nursing Practice (ICNP) with the NANDA-International (NANDA-I) and Nursing Interventions Classification (NIC) | A cross sectional study. Sample: n = 138 health records, 69 per facility. | Center 1 used EHR in combination with the NAND-I and NIC
with the subjective, objective, interpretation and
management format. Center 2 used handwritten nursing records based on the ICNP and the subjective, objective assessment and plan format. |
Mean total Q-DIO scores. | Results: Center 1 total mean score = 35.46/58, center 2 = 31.71/58 |
| Thoroddsen, A/2007/ Iceland Title- Putting policy into practice: pre- and post-tests of implementing standardized languages for nursing documentation. | A cross section design in 3 phases, a pretest (2002 n = 355), an intervention (2003), a post-test (2004 n = 349). | 1. Planned work groups - nursing administrators, nurse
managers, ward nurses 2. Education. 3. Standardized nursing languages 4. Standardized care plans |
Percentage changes in documentation between 2002 and 2004. | Results: The proportion of patients who had nursing assessment documented in their records for 2002 = 96.6% and for 2004 = 94.3%. The number of patients with documented nursing diagnosis for 2002 = 74.6%, for 2004 = 84.2%. The use of NANDA in 2002 = 67% and in 2004 = 84.2%. Signs and symptoms for nursing diagnosis documented in 2002 = 29.2% and in 2004 = 62.5%, etiologies documented for 2002 = 57.2% and 2004 = 76.7% Expected outcomes documented for 2002 = 20.9% of nursing records and in 2004 = 18.7%. For documented nursing interventions NIC was used in 2002 = 27.4% and in 2004 = 66.8%. Care plans documented in 2002 = 76.3% and in 2004 = 88.5%. Standardized care plans used in 2002 = 33.7% and in 2004 = 62.5%. Up to date progress notes documented in 2002 = 84.9% and in 2004 = 91.9% |
| Larrabee, J/2001/USA Title-Evaluation of documentation before and after implementation of a nursing information system in an Acute Care Hospital | Design: Before and after study with retrospective chart reviews at 1 month before implementation (n = 90), at 6 months after (n = 90) and 18 months after (n = 90) | 1. NANDA, NIC and project team generated outcome statements
2. Education 3. Introduction of computerized nursing information system (NIS) 4. 24/7 support for 1 week |
NASSESS score = ratio of the number of times nursing assessments of patient outcomes were documented to the number of times they should have been documented; NGOAL score = ratio of the number of times patient outcomes were met to the number of times patient outcomes were assessed; NQUAL score = ratio of the number of times nursing interventions were documented to the number of times they should have been documented; measurement of routine assessments = ratio of the times they were documented to the number of times they should have been documented. | NASSESS 1995 = 79.02%, 1996 = 57.63%, 1997 = 77.36%; NGOAL 1995 = 89.14%, 1996 = 77.30%, 1997 = 86.16%; NQUAL 1995 = 68.33%, 1996 = 68.55%, 1997 = 78.79%; |
| Ellis, J/2007/Canada Title- Implementing best practice pain management in a pediatric hospital | Before and after study, the pre-audit was conducted 1 month (n = 75) prior to program implementation and post-audit 1 (n = 44) and 2 (n = 50) were conducted 6 months post implementation. Post-audit 2 focused on patients with conditions associated with pain. | 1. A pain management committee was formed 2. Education 3. New forms |
The proportion of patient records where selected criteria indicating pain management were present. | Pain scale used – pre-audit = 5%, post1 = 43%, post2 = 24%; pain flow sheet on chart – pre-audit = N/A, post1 = 43%, post2 = 24%; narrative description of pain – pre-audit = 39%, post1 = 61%, post2 = 94%; Evidence of treatment effectiveness – pre-audit = 25%, post1 = 39%, post2 = 38%; opioids ordered – pre-audit = 61%, post1 = 73%, post2 = 47%, at least 1 dose of opioid given – pre-audit = 49%, post1 = 41%, post2 = 50%. |
| Habich, M/2012/USA Title- Evaluating the effectiveness of pediatric pain management guidelines | Before and after study with retrospective chart reviews at 3 study intervals - T1 = before education and implementation (n = 70), T2 = 3 months post implementation (n = 70), T3 = 6 months post implementation (n = 70). | 1. Guideline developed 2. Education |
Percentage comparison at each time interval. | Routine pain assessment - T1 = 72.9%, T2 = 98.6%, T3 = 97.1%; Appropriate pain assessment tool - T1 = 51.6%, T2 = 78.6%, T3 = 92.9%, Reassessment - T1 = 30%, T2 = 35.6%, T3 = 69.4%; Intervention appropriate - T1 = 33%, T2 = 26.3%, T3 = 24.7%; Goal achieved - T1 = 26.7%, T2 = 24.7%, T3 = 25.0%. |
| de Rond, M/2000/ Netherlands Title- A pain monitoring program for nurses: Effects on communication, assessment and documentation of patients’ pain | A quasi experimental design with a non-equivalent control group. Control group n = 350 patients, intervention group n = 341 patients. | 1. Education 2. Implementation of twice daily pain assessments using a 10 point numeric rating scale |
Mean pain documentation per patient per day, total mean documentation per patient. | Control group mean documentation score per patient per day = 1.7, intervention group = 1.9; control group total mean documentation per patient = 23.4, intervention group = 26.6. |
| Gunningberg, L/2008/ Sweden Title- Accuracy in the recording of pressure ulcers and prevention after implementing an electronic health record in hospital care | Before and after cross section comparison. All patients at the department of surgery, orthopedics, medicine and geriatrics were inspected for the presence of PUs during 1 day in 2002 and repeated in 2006 after implementation of an EHR in 2004, the corresponding patient records were audited retrospectively for the presence of documentation on PUs. Sample: 2002- paper based records n = 413, 2006- EHR n = 343. | 1. Education 2. Development of guidelines for the purchase and allocation of pressure reducing mattresses 3. Templates for risk assessment, PU grading and standard care plans to facilitate adequate documentation in the EHR |
Prevalence of PUs observed compared to PUs documented as percentages; prevalence of PU prevention observed compared to PU prevention documented | 2002 - PU observed = 119/357(33.3%), PU documented (paper based) = 59/413(14.3%) versus 2006 - PU observed = 103/343(30.3%), PU documented in EHR = 71/343(20.7%); 2002 - PU prevention observed = 99/357(27.7%), PU prevention documented (paper based) = 16/413(3.9%) versus 2006 PU prevention observed = 177/343(51.6%), PU prevention documented in EHR = 27/343(7.9%). |
| Ammenwerth, E/2001/ Germany Title- A randomized evaluation of a computer-based nursing documentation system | A randomized controlled trial conducted over 10 weeks. Patients were randomized to a paper based control group (n = 30) or an EHR based intervention group (n = 30) | 1. EHR installed 2. Education 3. Additional computers were provided |
The quality of documentation as measured by the checklist. | Amount of documentation with a complete care plan, paper = 50%, EHR = 79.3%; average number of problems stated, paper = 3.5, EHR = 5.6; average number of aims stated, paper = 3.3, EHR = 11.3; average number of tasks listed, paper = 3.8, EHR = 18.7; percentage of documentation with planned tasks actually executed, paper = 100%, EHR = 80%; percentage of documentation correctly signed, paper = 34.7% EHR = 100%; percentage of documentation where everything is legible, paper = 14.3%, EHR = 100%. Overall quality, paper = 2.3/5, ER = 2.4/5. |
| Esper, P/2015/USA Title- Improving documentation of quality measures in the electronic health record | Before and after study. A pre intervention retrospective chart audit (n = 100), then a post intervention chart audit (n = 65) 4 weeks following the intervention. | 1. Education 2. Shortcuts in EHR 3. Personal feedback on chart audits on request. |
Percentage of charts with complete documentation. | Pain assessed pre = 83%, post = 94%; pain plan pre = 60%, post = 82%; pain plan appropriate pre = 55%, post = 95%; Rx effect check pre = 57%, post = 100%; bowel eval (pre Rx) = 64%, post = 94%; bowel eval (post Rx) pre = 68%, post = 94%; emotional eval pre = 27%, post = 48%; emotional intervention pre = 20%, post = 49%. |
| Tejedor, S/2013/USA Title- Electronic documentation of central venous catheter-days: Validation is essential | Before and after study, using process improvement methods. Sample: manual validation was performed on 22 wards, on all Central Venous Catheter (CVC) patients, on a sample of days in the month. | 1. The EHR interface was redesigned 2. Education 3. Audit and feedback 4. Prioritisation and investment of resources. |
Patient level error rate was calculated by determining the number of patients with one or more errors in the EHR real time report divided by the number of patients on the ward with one or more CVCs counted manually. | At baseline the mean patient level total error rate was 0.32 errors per CVC-day. At 6 months after the start of manual validation, the patient level total error rate was 0.05. At Sep 2011 patient level total error rate was 0.14. |
| Thoroddsen, A/2011/ Iceland Title- Content and completeness of care plans after implementation of standardized nursing terminologies and computerized records | Before and after study. T1 pretest (n = 291) before a yearlong implementation program; T2 (n = 299) at 3 weeks after the implementation program was completed and T3 (n = 281) at 22 months after T2 and 8 months after the implementation of computerized care plans. | 1. Pre-printed standardized care plans 2. Care plans were updated with standardized nursing terminology - NANDA and NIC 3. Computerized nursing care plans 4. Education 5. Task force and working groups formed |
Content and completeness of nursing diagnoses, signs and symptoms, related factors and nursing interventions; sustainability of content and completeness over time. | Records with nursing care plans- T1 = 77%, T2 = 88%, T3 = 89%; mean number of nursing diagnoses (ND) per patient- T1 = 5.8, T2 = 5.8, T3 = 5.7; Nursing diagnoses were NANDA or collaborative problems- T1 = 74.9%, T2 = 91.8%, T3 = 94.9%; ND with signs and symptoms T1 = 30%, T2 = 63%, T3 = 74%; ND with related factors- T1 = 58%, T2 = 76%, T3 = 76%; use of NIC for nursing interventions- T1 = no data, (NIC not in use), T2 = 71.1%, T2 = 96.8%; mean number of nursing interventions per patient- T2 = 7.1, T3 = 10.6. |
| Nielsen, G/2014/USA Title- Essential documentation elements: quality tool for the Emergency Department nurse | Plan, Do, Study, Act (PDSA), with a baseline audit and monthly post intervention audits. Sample: Baseline data were gathered with a convenience sample of n = 30 patient records. Following the implementation of the intervention a total population sample of n = 89,521 was obtained, approximately 7,460 records per month. | 1. Education 2. Passive visual cues in the electronic HER to provide real time feedback 3. Nursing documentation software modified to remove unnecessary steps 4. Feedback from all stakeholders |
Percentile compliance. | Improvements were achieved with 7 elements, no change was noted in 5 elements, a slight decrease for 4 elements. Improvements - initial pain assessment by 4%, administration of blood components by 44%, immunization status documentation by 54%, height by 28%, the Braden scale by 78%. |
| Dehghan, D/2015/Iran Title- The quality of clinical documentation of patients admitted to an Iranian teaching hospital: A two-year impact of Clinical Governance | Before and after study. n = 165 records before and after implementation of clinical governance. | 1. The 7 axis model of clinical governance was implemented
2. Education 3. Head nurses obligated to control nursing records 4. Forms introduced - patient education and patient assessment of nursing care quality. |
Percentages and mean scores for content and structure. | Mean quality scores of nursing records - before = 1.62, after = 1.66; quality of record structure increased significantly after clinical governance; nursing record content showed no significant difference; before clinical governance 89.63% were average quality and 10.37% were good quality; after clinical governance 83% were average and 17% were good. |
| Wissman, K/2020/USA Title- Improving pain reassessment and documentation rates: A quality improvement project in a teaching hospital's emergency department | Before and after study. Pre intervention n = 260 patient encounters; post intervention n = 321 patients. | 1. Daily audits for each nurse who worked the previous day
and individual feedback via email 2. Education 3. Focus groups to identify barriers to completing pain reassessment |
The reassessment of pain (yes or no) | Pre-intervention = 94/260 (36.2%); post- intervention = 200/321(62.3%). It was determined that the overall improvement in reassessment rates was not related to individual nurses. |
| Chineke, I/2020/USA Title- Improving documentation of pain and constipation management within the cancer center of a large urban academic hospital | Before and after study. Pre- intervention n = 123, post-intervention n = 194. | 1. Education 2. Cause and effect analysis 3. A pareto chart to prioritize barriers to assessment and documentation 4. An automated assessment tool was integrated into the nursing assessment 5. The nursing assessment was imported directly into the provider's progress note 6. A mandatory section for provider documentation of pain and constipation 7. A prompt to implement a plan when indicated 8. An order panel linking frequently prescribed opioids to prescriptions for bowel regimes |
The assessment and documentation of pain and constipation before and after the interventions. | At baseline pain assessment was documented in 66.7% of patient encounters, and constipation was documented in 20.4%. Post intervention 100% of patient encounters had pain assessment and constipation assessment documentation. |
| Hom, L/2019/USA Title- Quality improvement interventions to improve critical congenital heart disease screening | A baseline audit (July to Dec 2015) followed by Plan, Do, Study, Act cycles to implement and evaluate changes (Jan 2016 to Dec 2018). At baseline n = 188 infants, during the implementation n = 1,564 infants. | 1. Formation of an interdisciplinary team 2. Monthly meetings for data review and analysis 3. Monthly reports and email feedback loop to clinical team screening 4. EHR enhancements - blocks, prompts, automatic defaults 5. Education |
The percentage of documentation errors | Base line documentation errors = 23.5%, documentation errors in the intervention period = 1.2% and was sustained during the intervention period. |
| Flores, C/2020/Australia Title- Embedding best transfusion practice and blood management in neonatal intensive care | Before and after study with Practice based Evidence for Clinical Practice Improvement (PBE-CPI). Baseline transfusion audit n = 59, post-intervention audit n = 20. | 1. Reviewed and updated current policies and
processes 2. Education |
Percentage compliance with patient blood management and the blood and blood product form (consent, appropriateness, procedure) | Baseline -consent = 65.4%, appropriateness = 83.1%, procedure = 65.6%. Post-intervention - consent = 88.3%, appropriateness = 95%, procedure = 91.4% |
| Lieow, L/2019/Singapore Title- Effectiveness of an advanced practice nurse-led delirium education and training programme | Before and after study with pre-test (May 2014) and post-test (Oct 2014, May 2015). Sample: not stated. | 1. Education | The total number of documented assessments per 24hr divided by the total minimum standard for the respective scale. | RASS overall compliance pre- intervention = 79%, 10 months post- intervention = 80%; CAM-ICU overall compliance pre-intervention = 36%, 10 months post-intervention = 61%. |
| Gloger, A/2020/USA Title- Use of tailored feedback improves accuracy of delirium documentation in the Burn ICU: results of a performance improvement initiative. | Before and after study; Pre-corrective feedback (PRE-CFB) from Sep -Dec 2017 (n = 59 RNs audited) and Post-corrective feedback (POST-CFB) from Jan 2018-Sep 2018 (n = 375 RNs audited). | 1. Education 2. Nurse educator sent an email to every nurse found to have inaccurately documented a delirium assessment; the email contained a snapshot of the documentation and an explanation of why it was incorrect 3. Nursing staff were notified that the nurse manager would be made aware if any nurse had 3 or more episodes of inaccurate documentation. |
Accuracy was documented as either correct or incorrect. | PRE-CFB - RNs passing the audit = 49.6%; POST-CFB - RNs passing the audit = 91.75% |
| Trad, W/2019/Australia Title- Nursing assessment and management of incontinence among medical and surgical adult patients in a tertiary hospital: a best practice implementation project. | Before and after study with JBI Practical Application of Clinical Evidence Systems (PACES) and Getting Research into Practice (GRiP). Baseline audit (n = 100) Aug-Oct 2016. Follow up audit (n = 100) Nov 2016- July 2017. | 1. Creation of a multidisciplinary project team 2. Creation of assessment and management guides 3. Creation of a chart of types of urinary incontinence 4. Development of a pad selection guide 5. Education 6. Sourcing of appropriate continence products 7. The follow up audit results were widely disseminated. |
Percentage compliance with the audit criteria. | Baseline audit = 25.13% compliance with audit criteria (criteria 8 and 9 not included, they are not documentation criteria). Follow up audit = 51.50% compliance. Overall compliance with audit criteria improved. |
| Azzolini, E/2019/Italy Title- Quality improvement of medical records through internal auditing: a comparative analysis | Before and after study; first evaluation June - Nov 2013 (n = 1,460), intervention Nov 2013- June 2014, second evaluation July - Dec 2015 (n = 1,402). | 1. 34 audits were performed and the results were shared with personnel. | Percentage of medical records fulfilling the quality items for each domain; number of satisfied items/total of evaluable items. | 2013 - Daily nursing progress notes = 54.7%. 2015 - Daily nursing progress notes = 86.3%. |
Footnotes
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) received no financial support for the research, authorship and/or publication of this article.
ORCID iD: Jeanette Bunting https://orcid.org/0000-0002-0828-4015
References
- Akhu-Zaheya L., Al-Maaitah R., Bany Hani S. (2018). Quality of nursing documentation: Paper-based health records versus electronic-based health records. Journal of Clinical Nursing (John Wiley & Sons, Inc.), 27(3–4), e578–e589. 10.1111/jocn.14097 [DOI] [PubMed] [Google Scholar]
- Ammenwerth E., Eichstädter R., Haux R., Pohl U., Rebel S., Ziegler S. (2001). A randomized evaluation of a computer-based nursing documentation system. Methods of Information in Medicine, 40(2), 61–68. 10.1055/s-0038-1634465 [DOI] [PubMed] [Google Scholar]
- Aparanji K., Kulkarni S., Metzke M., Schmudde Y., White P., Jaeger C. (2018). Quality improvement of delirium status communication and documentation for intensive care unit patients during daily multidisciplinary rounds. BMJ Open Quality, 7(2), e000239–e000239. 10.1136/bmjoq-2017-000239 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Azzolini E., Furia G., Cambieri A., Ricciardi W., Volpe M., Poscia A. (2019). Quality improvement of medical records through internal auditing: A comparative analysis. Journal of Preventive Medicine and Hygiene, 60(3), E250–E255. 10.15167/2421-4248/jpmh2019.60.3.1203 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Bernick L., Richards P. (1994). Nursing documentation: A program to promote and sustain improvement. Journal of Continuing Education in Nursing, 25(5), 203–208. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,athens&db=rzh&AN=107397873&site=ehost-live&scope=site [DOI] [PubMed] [Google Scholar]
- Björvell C., Wredling R., Thorell-Ekstrand I. (2002). Long-term increase in quality of nursing documentation: Effects of a comprehensive intervention. Scandinavian Journal Of Caring Sciences, 16(1), 34–42. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,athens&db=cmedm&AN=11985747&site=ehost-live&scope=site [DOI] [PubMed] [Google Scholar]
- Blair W., Smith B. (2012). Nursing documentation: Frameworks and barriers. Contemporary Nurse: A Journal for the Australian Nursing Profession, 41(2), 160–168. 10.5172/conu.2012.41.2.160 [DOI] [PubMed] [Google Scholar]
- Bono B. J. (1992). Assessment and documentation of the breastfeeding couple by health care professionals. Journal of Human Lactation, 8(1), 17–22. Retrieved from 10.1177/089033449200800119 [DOI] [PubMed] [Google Scholar]
- Bruylands M., Paans W., Hediger H., Müller-Staub M. (2013). Effects on the quality of the nursing care process through an educational program and the use of electronic nursing documentation. International Journal of Nursing Knowledge, 24(3), 163–170. 10.1111/j.2047-3095.2013.01248.x [DOI] [PubMed] [Google Scholar]
- Cahill H., Jones A., Herkes R., Cook K., Stirling A., Halbert T., Gattas D. J. (2011). Introduction of a new observation chart and education programme is associated with higher rates of vital-sign ascertainment in hospital wards. Bmj Quality & Safety, 20(9), 791–796. 10.1136/bmjqs.2010.045096 [DOI] [PubMed] [Google Scholar]
- Chineke I., Adams Curry M., Bell W., Flood D., Mishra P., Power S., Bernal-Mizrachi L. (2020). Improving documentation of pain and constipation management within the cancer center of a large urban academic hospital. JCO Oncol Pract, 16(3), e251–e256. 10.1200/jop.19.00332 [DOI] [PubMed] [Google Scholar]
- Christie J. (1993). Does the use of an assessment tool in the accident and emergency department improve the quality of care? Journal Of Advanced Nursing, 18(11), 1758–1771. Retrieved from 10.1046/j.1365-2648.1993.18111758.x [DOI] [PubMed] [Google Scholar]
- Cline M. A. (2016). Increasing RN accountability in professional practice: Development of a pain reassessment documentation scorecard. The Journal Of Nursing Administration, 46(3), 128–131. 10.1097/NNA.0000000000000311 [DOI] [PubMed] [Google Scholar]
- Coiera E., Kocaballi B., Halamka J., Laranjo L. (2018). The digital scribe. npj Digital Medicine, 1(1), 58. 10.1038/s41746-018-0066-9 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Cone K. J., Anderson M. A., Johnson J. A. (1996). The effect of in-service education on emergency nurses’ documentation of physical assessment. Journal of Emergency Nursing, 22(5), 398–402. 10.1016/s0099-1767(96)80159-0 [DOI] [PubMed] [Google Scholar]
- Considine J., Potter R., Jenkins J. (2006). Can written nursing practice standards improve documentation of initial assessment of ED patients? Australasian Emergency Nursing Journal, 9(1), 11–18. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,athens&db=rzh&AN=106352052 &site=ehost-live&scope=site [Google Scholar]
- Dahlstrom M., Best T., Baker C., Doeing D., Davis A., Doty J., Arora V. M. (2011). Improving identification and documentation of pressure ulcers at an urban academic hospital. Joint Commission Journal on Quality & Patient Safety, 37(3), 123–130. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,athens&db=rzh&AN=104846681&site=ehost-live&scope=site [DOI] [PMC free article] [PubMed] [Google Scholar]
- Darmer M. R., Ankersen L., Nielsen B. G., Landberger G., Lippert E., Egerod I. (2006). Nursing documentation audit--the effect of a VIPS implementation programme in Denmark. Journal Of Clinical Nursing, 15(5), 525–534. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,athens&db=cmedm&AN=16629961&site =ehost-live&scope=site [DOI] [PubMed] [Google Scholar]
- de Rond M. E., de Wit R., van Dam F. S., Muller M. J. (2000). A pain monitoring program for nurses: Effects on communication, assessment and documentation of patients’ pain. Journal of Pain and Symptom Management, 20(6), 424–439. 10.1016/s0885-3924(00)00209-8 [DOI] [PubMed] [Google Scholar]
- Dehghan D., Dehghan M., Sheikhrabori A. (2015). The quality of clinical documentation of patients admitted to an Iranian teaching hospital: A two-year impact of clinical governance. Asian Journal of Nursing Education and Research, 5(2), 159. 10.5958/2349-2996.2015.00033.6 [DOI] [Google Scholar]
- Duclos-Miller P. A. (2016). Improving nursing documentation and reducing risk. HCPro, a division of BLR. [Google Scholar]
- Elliott D., Allen E., McKinley S., Perry L., Duffield C., Fry M., Roche M. (2017). User compliance with documenting on a track and trigger-based observation and response chart: A two-phase multi-site audit study. Journal Of Advanced Nursing, 73(12), 2892–2902. 10.1111/jan.13302 [DOI] [PubMed] [Google Scholar]
- Elliott L. (2018). Standardizing documentation: A place for everything. MEDSURG Nursing, 27(1), 32–37. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,athens&db=rzh&AN=128049904&site=ehost-live&scope=site [Google Scholar]
- Ellis J. A., McCleary L., Blouin R., Dube K., Rowley B., MacNeil M., Cooke C. (2007). Implementing best practice pain management in a pediatric hospital. Journal for Specialists in Pediatric Nursing, 12(4), 264–277. 10.1111/j.1744-6155.2007.00121.x [DOI] [PubMed] [Google Scholar]
- Enright K., MacMillan M., Lymburner P., Sodoski C., Gollee S., Carvalho M., Almeida B. (2015). Improving documentation of oral chemotherapy at a community cancer center. Journal Of Oncology Practice, 11(3), 213–215. 10.1200/JOP.2014.003111 [DOI] [PubMed] [Google Scholar]
- Esper P., Walker S. (2015). Improving documentation of quality measures in the electronic health record. Journal of the American Association of Nurse Practitioners, 27(6), 308–312. 10.1002/2327-6924.12169 [DOI] [PubMed] [Google Scholar]
- Finn L. (1997). Clinical. Nurses’ documentation of infection control precautions: 2. British Journal of Nursing, 6(12), 678–684. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,athens&db=rzh&AN=107349953 &site=ehost-live&scope=site [DOI] [PubMed] [Google Scholar]
- Flores C. J., Lakkundi A., McIntosh J., Freeman P., Thomson A., Saxon B., Ross B. (2020). Embedding best transfusion practice and blood management in neonatal intensive care. BMJ Open Quality, 9(1), e000694. 10.1136/bmjoq-2019-000694 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Florin J., Ehrenberg A., Ehnfors M. (2005). Quality of nursing diagnoses: Evaluation of an educational intervention. International Journal of Nursing Terminologies & Classifications, 16(2), 33–43. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,athens& db=rzh&AN=106528371&site=ehost-live&scope=site [DOI] [PubMed] [Google Scholar]
- Förberg U., Johansson E., Ygge B.-M., Wallin L., Ehrenberg A. (2012). Accuracy in documentation of peripheral venous catheters in paediatric care: An intervention study in electronic patient records. Journal Of Clinical Nursing, 21(9–10), 1339–1344. 10.1111/j.1365-2702.2011.03949.x [DOI] [PubMed] [Google Scholar]
- Gerdtz M. F., Waite R., Vassiliou T., Garbutt B., Prematunga R., Virtue E. (2013). Evaluation of a multifaceted intervention on documentation of vital signs at triage: A before-and-after study. Emergency Medicine Australasia: EMA, 25(6), 580–587. 10.1111/1742-6723.12153 [DOI] [PubMed] [Google Scholar]
- Gloger A. N., Nakonezny P. A., Phelan H. A. (2020). Use of tailored feedback improves accuracy of delirium documentation in the burn ICU: Results of a performance improvement initiative. Journal of Burn Care & Research: Official Publication of the American Burn Association, 41(2), 299–305. 10.1093/jbcr/irz153 [DOI] [PubMed] [Google Scholar]
- Gordon D. B., Rees S. M., McCausland M. P., Pellino T. A., Sanford-Ring S., Smith-Helmenstine J., Danis D. M. (2008). Improving reassessment and documentation of pain management. Joint Commission Journal on Quality & Patient Safety, 34(9), 509–517. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,athens&db=rzh&AN =105550853&site=ehost-live&scope=site [DOI] [PubMed] [Google Scholar]
- Goulding L., Parke H., Maharaj R., Loveridge R., McLoone A., Hadfield S., Sandall J. (2015). Improving critical care discharge summaries: A collaborative quality improvement project using PDSA. BMJ Quality Improvement Reports, 4(1), 1-8. 10.1136/bmjquality.u203938.w3268 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Griffiths P., Debbage S., Smith A. (2007). A comprehensive audit of nursing record keeping practice. British Journal Of Nursing (Mark Allen Publishing), 16(21), 1324–1327. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,athens&db=cmedm&AN=18073669&site=ehost-live&scope=site [DOI] [PubMed] [Google Scholar]
- Gunningberg L., Dahm M. F., Ehrenberg A. (2008). Accuracy in the recording of pressure ulcers and prevention after implementing an electronic health record in hospital care. Quality & Safety in Health Care, 17(4), 281–285. 10.1136/qshc.2007.023341 [DOI] [PubMed] [Google Scholar]
- Gunningberg L., Fogelberg-Dahm M., Ehrenberg A. (2009). Improved quality and comprehensiveness in nursing documentation of pressure ulcers after implementing an electronic health record in hospital care. Journal of Clinical Nursing (Wiley-Blackwell), 18(11), 1557–1564. 10.1111/j.1365-2702.2008.02647.x [DOI] [PubMed] [Google Scholar]
- Habich M., Wilson D., Thielk D., Melles G. L., Crumlett H. S., Masterton J., McGuire J. (2012). Evaluating the effectiveness of pediatric pain management guidelines. Journal of Pediatric Nursing, 27(4), 336–345. 10.1016/j.pedn.2011.06.002 [DOI] [PubMed] [Google Scholar]
- Hayter K. L., Schaper A. M. (2015). CONTROLLING PAIN. Improving pain documentation with peer chart review. Nursing, 45(7), 58–63. 10.1097/01.NURSE.0000463673.52336.80 [DOI] [PubMed] [Google Scholar]
- Higuchi K. A., Dulberg C., Duff V. (1999). Factors associated with nursing diagnosis utilization in Canada. Nursing Diagnosis: ND: The Official Journal Of The North American Nursing Diagnosis Association, 10(4), 137–147. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,athens&db=cmedm&AN=10786554&site=ehost-live&scope=site [DOI] [PubMed] [Google Scholar]
- Hom L. A., Chan Salcedo C., Revenis M., Martin G. R. (2019). Quality improvement interventions to improve critical congenital heart disease screening. Pediatric quality & safety, 4(5), e221–e221. 10.1097/pq9.0000000000000221 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Hospodar M. (2007). Sticking together! A creative approach to documenting insulin double checks. Rehabilitation Nursing: The Official Journal Of The Association Of Rehabilitation Nurses, 32(1), 6–8. Retrieved from 10.1002/j.2048-7940.2007.tb00142.x [DOI] [PubMed] [Google Scholar]
- Hübner U., Schulte G., Sellemann B., Quade M., Rottmann T., Fenske M., Rienhoff O. (2015). Evaluating a proof-of-concept approach of the German health telematics infrastructure in the context of Discharge management (Vol. 216). Netherlands: IOS Press. https://ebooks.iospress.nl/publication/40257. [PubMed] [Google Scholar]
- Jackson S. E. (2010). The efficacy of an educational intervention on documentation of pain management for the elderly patient with a hip fracture in the emergency department. JEN: Journal of Emergency Nursing, 36(1), 10–15. 10.1016/j.jen.2008.08.022 [DOI] [PubMed] [Google Scholar]
- Jacobson T. M., Thompson S. L., Halvorson A. M., Zeitler K. (2016). Enhancing documentation of pressure ulcer prevention interventions. Journal of Nursing Care Quality, 31(3), 207–216. 10.1097/NCQ.0000000000000175 [DOI] [PubMed] [Google Scholar]
- Johnson L., Edward K.-L., Giandinoto J.-A. (2018). A systematic literature review of accuracy in nursing care plans and using standardised nursing language. Collegian, 25(3), 355–361. 10.1016/j.colegn.2017.09.006 [DOI] [Google Scholar]
- Kamath B. D., Donovan E. F., Christopher R., Brodbeck J., Slone C., Marcotte M. P. (2011). Using improvement science to increase accuracy and reliability of gestational Age documentation. American Journal of Perinatology, 28(8), 1–8. 10.1055/s-0031-1285096 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Karp E. L., Freeman R., Simpson K. N., Simpson A. N. (2019). Changes in efficiency and quality of nursing electronic health record documentation after implementation of an admission patient history essential data Set. CIN: Computers, Informatics. Nursing, 37(5), 260–265. 10.1097/CIN.0000000000000516 [DOI] [PubMed] [Google Scholar]
- Khresheh R., Barclay L. (2008). Implementation of a new birth record in three hospitals in Jordan: A study of health system improvement. Health Policy And Planning, 23(1), 76–82. Retrieved from 10.1093/heapol/czm039 [DOI] [PubMed] [Google Scholar]
- Larrabee J. H., Boldreghini S., Elder-Sorrells K., Turner Z. M., Wender R. G., Hart J. M., Lenzi P. S. (2001). Evaluation of documentation before and after implementation of a nursing information system in an acute care hospital. Computers in Nursing, 19(2), 56–68. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,athens&db=rzh&AN=107022870&site=ehost-live&scope=site [PubMed] [Google Scholar]
- Lieow J. L. M., Chen F. S. M., Song G., Tang P. S., Kowitlawakul Y., Mukhopadhyay A. (2019). Effectiveness of an advanced practice nurse-led delirium education and training programme. International Nursing Review, 66(4), 506–513. 10.1111/inr.12519 [DOI] [PubMed] [Google Scholar]
- Linch G., Lima A. A. A., Souza E. N., Nauderer T. M., Paz A. A., da Costa C. (2017). An educational intervention impact on the quality of nursing records. Revista Latino-Americana de Enfermagem, 25, e2938. 10.1590/1518-8345.1986.2938 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mansfield J. A., Dodds K. L., Mallory T. H., Lombardi A. V., Adams J. B. (2001). Linking the orthopaedic office-hospital continuum: Results before and after implementation of an automated patient health history project. Orthopedic Nursing, 20(2), 51–60. Retrieved from 10.1097/00006416-200103000-00013 [DOI] [PubMed] [Google Scholar]
- Margonary H., Hannan M. S., Schlenk E. A. (2017). Quality improvement initiative on pain knowledge, assessment, and documentation skills of pediatric nurses. Pediatric Nursing, 43(2), 65–70. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,athens&db=cmedm&AN=29394479&site=ehost-live&scope=site [PubMed] [Google Scholar]
- McCarthy B., Fitzgerald S., O’Shea M., Condon C., Savage E., Hartnett-Collins G., Bergin M. (2019). Electronic nursing documentation interventions to promote or improve patient safety and quality care: A systematic review. Journal of Nursing Management (John Wiley & Sons, Inc.), 27(3), 491–501. 10.1111/jonm.12727 [DOI] [PubMed] [Google Scholar]
- Melo L. S. d., Figueiredo L. d. S., Pereira J. d. M. V., Flores P. V. P., Cavalcanti A. C. D. (2019). Effect of an educational program on the quality of nursing process recording. Acta Paulista de Enfermagem, 32(3), 246–253. 10.1590/1982-0194201900034 [DOI] [Google Scholar]
- Meyer L. K., Nanassy A. D., Lavella H., Arthur L. G., Grewal H. (2019). Cohorting trauma patients in a medical/surgical unit at a level I pediatric trauma center to enhance interdisciplinary collaboration and documentation. Journal Of Trauma Nursing: The Official Journal Of The Society Of Trauma Nurses, 26(1), 17–25. 10.1097/JTN.0000000000000418 [DOI] [PubMed] [Google Scholar]
- Mishra A. K., Bhattarai S., Bhurtel P., Bista N. R., Shrestha P., Thakali K., Pathak S. R. (2009). Need for improvement of medical records. JNMA; Journal of the Nepal Medical Association, 48(174), 103–106. Retrieved from https://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,athens&db=cmedm&AN=20387347&site=ehost-live&scope=site [PubMed] [Google Scholar]
- Mitchell I. A., McKay H., Van Leuvan C., Berry R., McCutcheon C., Avard B., Lamberth, P. (2010). A prospective controlled trial of the effect of a multi-faceted intervention on early recognition and intervention in deteriorating hospital patients. Resuscitation, 81(6), 658–666. 10.1016/j.resuscitation.2010.03.001 [DOI] [PubMed] [Google Scholar]
- Müller-Staub M., Lavin M. A., Needham I., van Achterberg T. (2006). Nursing diagnoses, interventions and outcomes - application and impact on nursing practice: Systematic review. Journal of Advanced Nursing, 56(5), 514–531. 10.1111/j.1365-2648.2006.04012.x [DOI] [PubMed] [Google Scholar]
- Müller-Staub M., Needham I., Odenbreit M., Lavin M. A., van Achterberg T. (2007). Improved quality of nursing documentation: Results of a nursing diagnoses, interventions, and outcomes implementation study. International Journal of Nursing Terminologies & Classifications, 18(1), 5–17. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,athens&db=rzh&AN=106298993&site=ehost-live&scope=site [DOI] [PubMed] [Google Scholar]
- Müller-Staub M., Needham I., Odenbreit M., Lavin M. A., van Achterberg T. (2008). Implementing nursing diagnostics effectively: Cluster randomized trial. Journal of Advanced Nursing, 63(3), 291–301. 10.1111/j.1365-2648.2008.04700.x [DOI] [PubMed] [Google Scholar]
- Murad M. H., Mustafa R. A., Schünemann H. J., Sultan S., Santesso N. (2017). Rating the certainty in evidence in the absence of a single estimate of effect. Evidence-based Medicine, 22(3), 85–87. 10.1136/ebmed-2017-110668 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mykkänen M., Saranto K., Miettinen M. (2012). Nursing audit as a method for developing nursing care and ensuring patient safety. NI 2012 : 11th International Congress on Nursing Informatics, June 23-27, 2012, Montreal, Canada. International Congress in Nursing Informatics (11th : 2012 : Montreal, Quebec), 2012, 301–301. Retrieved from 10.1073/pnas.83.5.1532 [DOI]
- Nielsen G., Peschel L., Burgess A. (2014). Essential documentation elements: Quality tool for the emergency department nurse. Advanced Emergency Nursing Journal, 36(2), 199–205. 10.1097/TME.0000000000000020 [DOI] [PubMed] [Google Scholar]
- Nomura A. T. G., Pruinelli L., da Silva M. B., Lucena A. d. F., Almeida M. d. A. (2018). Quality of electronic nursing records: The impact of educational interventions during a hospital accreditation process. Computers, Informatics, Nursing: CIN, 36(3), 127–132. 10.1097/CIN.0000000000000390 [DOI] [PubMed] [Google Scholar]
- Nøst T. H., Frigstad S. A., André B. (2017). Impact of an education intervention on nursing diagnoses in free-text format in electronic health records: A pretest-posttest study in a medical department at a university hospital. Nordic Journal of Nursing Research, 37(2), 100–108. 10.1177/2057158516668081 [DOI] [Google Scholar]
- O’Connor T. L., Raposo E. A., Heller-Wescott T. (2014). Improving trauma documentation in the emergency department. Journal Of Trauma Nursing: The Official Journal Of The Society Of Trauma Nurses, 21(5), 238–243. 10.1097/JTN.0000000000000071 [DOI] [PubMed] [Google Scholar]
- Okoyo Nyakiba J., McMillan M., Kenyatta G. (2014). Reporting and documentation of adverse drug reactions by health care professionals at a Kenyan public hospital: A best practice implementation project. JBI Database of Systematic Reviews & Implementation Reports, 12(7), 521–533. 10.11124/jbisrir-2014-1362 [DOI] [Google Scholar]
- Page et al. (2021a). The PRISMA 2020 statement: An updated guideline for reporting systematic reviews. BMJ, 372, n71. 10.1136/bmj.n71 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Page et al. (2021b). PRISMA 2020 Explanation and elaboration: Updated guidance and exemplars for reporting systematic reviews. BMJ, 372, n160. 10.1136/bmj.n160 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Petrie A., Sabin C. (2020). Medical statistics at glance. Wiley-Blackwell. [Google Scholar]
- Phillips M. E., Gilmore R. A., Sheffield M. C., Phan S. V. (2019). Pain assessment documentation after opioid administration at a community teaching hospital. Journal Of Pharmacy Practice, 32(2), 179–185. 10.1177/0897190017751207 [DOI] [PubMed] [Google Scholar]
- Porter Y. (1990). Evaluation of nursing documentation of patient teaching. Journal of Continuing Education in Nursing, 21(3), 134–137. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,athens&db=cmedm&AN=2112175 &site=ehost-live&scope=site [DOI] [PubMed] [Google Scholar]
- Rabelo-Silva E. R., Dantas Cavalcanti A. C., Ramos Goulart Caldas M. C., Lucena A. F., Almeida M. A., Linch G. F., Müller-Staub M. (2017). Advanced nursing process quality: Comparing the international classification for nursing practice (ICNP) with the NANDA-international (NANDA-I) and nursing interventions classification (NIC). Journal of Clinical Nursing, 26(3–4), 379–387. 10.1111/jocn.13387 [DOI] [PubMed] [Google Scholar]
- Rykkje L. (2009). Implementing electronic patient record and VIPS in medical hospital wards: Evaluating change in quantity and quality of nursing documentation by using the audit instrument Cat-ch-Ing. Nordic Journal of Nursing Research & Clinical Studies / Vård i Norden, 29(2), 9–13. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,athens&db=rzh&AN=105395041&site=ehost-live&scope=site [Google Scholar]
- Sandau K. E., Sendelbach S., Fletcher L., Frederickson J., Drew B. J., Funk M. (2015). Computer-assisted interventions to improve QTc documentation in patients receiving QT-prolonging drugs. American Journal Of Critical Care: An Official Publication. American Association Of Critical-Care Nurses, 24(2), e6–e15. 10.4037/ajcc2015240 [DOI] [PubMed] [Google Scholar]
- Saranto K., Kinnunen U. M., Kivekäs E., Lappalainen A. M., Liljamo P., Rajalahti E., Hyppönen H. (2014). Impacts of structuring nursing records: A systematic review. Scandinavian Journal of Caring Sciences, 28(4), 629–647. 10.1111/scs.12094 [DOI] [PubMed] [Google Scholar]
- Stewart S., Bennett S., Blokzyl A., Bowman W., Butcher I., Chapman K., Wenzel S. (2009). ‘Measurement Monday’: One facility’s approach to standardizing skin impairment documentation. Ostomy Wound Management, 55(12), 49–53. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,athens&db=rzh&AN=105277966&site=ehost-live&scope=site [PubMed] [Google Scholar]
- Stocki D., McDonnell C., Wong G., Kotzer G., Shackell K., Campbell F. (2018). Knowledge translation and process improvement interventions increased pain assessment documentation in a large quaternary paediatric post-anaesthesia care unit. BMJ Open Quality, 7(3), e000319–e000319. 10.1136/bmjoq-2018-000319 [DOI] [PMC free article] [PubMed] [Google Scholar]
- Tejedor S. C., Garrett G., Jacob J. T., Meyer E., Reyes M. D., Robichaux C., Steinberg J. P. (2013). Electronic documentation of central venous catheter-days: Validation is essential. Infection Control and Hospital Epidemiology, 34(9), 900–907. 10.1086/671736 [DOI] [PubMed] [Google Scholar]
- Thoroddsen A., Ehnfors M. (2007). Putting policy into practice: Pre- and posttests of implementing standardized languages for nursing documentation. Journal of Clinical Nursing, 16(10), 1826–1838. 10.1111/j.1365-2702.2007.01836.x [DOI] [PubMed] [Google Scholar]
- Thoroddsen A., Ehnfors M., Ehrenberg A. (2011). Content and completeness of care plans after implementation of standardized nursing terminologies and computerized records. Computers, Informatics, Nursing: CIN, 29(10), 599–607. 10.1097/NCN.0b013e3182148c31 [DOI] [PubMed] [Google Scholar]
- Trad W., Flowers K., Caldwell J., Sousa M. S., Vigh G., Lizarondo L., Parker D. (2019). Nursing assessment and management of incontinence among medical and surgical adult patients in a tertiary hospital: A best practice implementation project. Jbi Database of Systematic Reviews and Implementation Reports, 17(12), 2578–2590. 10.11124/jbisrir-d-19-00110 [DOI] [PubMed] [Google Scholar]
- Tubaishat A., Tawalbeh L. I., Al Azzam M., AlBashtawy M., Batiha A.-M. (2015). Electronic versus paper records: Documentation of pressure ulcer data. British Journal of Nursing, 24(6), S30–S37. Retrieved from http://search.ebscohost.com/login.aspx?direct=true&AuthType=ip,athens&db=rzh&AN=103783030&site=ehost-live&scope=site [DOI] [PubMed] [Google Scholar]
- Tufanaru C., Munn Z., Aromataris E., Campbell J., Lisa H. (2017). Chapter 3: Systematic reviews of effectiveness. In Aromataris E M. Z. (Ed.). Joanna Briggs Institute Reviewer’s Manual. [Google Scholar]
- Turner A., Stephenson M. (2015). Documentation of chemotherapy administration by nursing staff in inpatient and outpatient oncology/hematology settings: A best practice implementation project. JBI Database Of Systematic Reviews And Implementation Reports, 13(10), 316–334. 10.11124/jbisrir-2015-2157 [DOI] [PubMed] [Google Scholar]
- Unaka N. I., Statile A., Jerardi K., Dahale D., Morris J., Liberio B., Brady P. (2017). Improving the readability of pediatric hospital medicine discharge instructions. Journal of Hospital Medicine, 12(7), 551–557. 10.12788/jhm.2770 [DOI] [PubMed] [Google Scholar]
- Wilbanks B. A., Geisz-Everson M., Boust R. R. (2016). The role of documentation quality in anesthesia-related closed claims: A descriptive qualitative study. Computers, informatics, nursing : CIN, 34(9), 406–412. 10.1097/CIN.0000000000000270 [DOI] [PubMed] [Google Scholar]
- Wissman K. M., Cassidy E., D’Amico F., Hoy C., Vissari T., Baumgartner M. (2020). Improving pain reassessment and documentation rates: A quality improvement project in a teaching hospital’s emergency department. Journal of Emergency Nursing, 46(4), 505–510. 10.1016/j.jen.2019.12.008 [DOI] [PubMed] [Google Scholar]