Abstract
Objective: In Australia, approximately 3 in 4 people with acute stroke use an ambulance. Few examples of merging ambulance clinical records, hospital government data, and national registry data for stroke exist. We sought to understand the advantages of using linked datasets for describing the full clinical journey of people with stroke and the possibility of investigating their long-term outcomes based on pre-hospital management of stroke. Method: Patient-level data from the Australian Stroke Clinical Registry (AuSCR) (January 2013-October 2017) were linked with Ambulance Victoria (AV) records and Victorian Emergency Minimum Dataset (VEMD). Probabilistic iterative matching on personal identifiers were used and records merged with a project specific identification number. Results: Of the 7,373 episodes in the AuSCR and 6,001 in the AV dataset; 4,569 (62%) were matched. Unmatched records that were positive for “arrival by ambulance” in the AuSCR and VEMD (no corresponding record in AV) were submitted to AV. AV were able to identify 148/435 additional records related to these episodes. The final cohort included 4,717 records (median age: 73 years, female 42%, ischemic stroke 66%). Conclusion: The results of the data linkage provides greater confidence for use of these data for future research related to pre-hospital management of stroke.
Keywords: Health services, Stroke, Ambulance records, Stroke registry, Data linkage, Emergency records
What do we already know about this topic?
Improvement in access to reperfusion therapy and reductions in treatment delays requires coordination of multiple systems and services including a well-organised and streamlined pre-hospital and hospital care.
How does your research contribute to the field?
Our knowledge of pre-hospital factors that influence timely identification of stroke and arrival to appropriate care is less well-known.
What are your research’s implications towards theory, practice, or policy?
This research will be used to identify gaps in pre-hospital processes related to improving acute stroke care and generate a strong evidence-base that will inform clinical practice and policy for pre-hospital stroke care.
Introduction
Government departments, disease registries and health-service providers collect large volumes of clinical data for monitoring service provision, costing services or for disease surveillance. 1 Combining these records through data linkage, whereby data belonging to an individual from multiple sources are merged, 2 can provide a resource for understanding health system effectiveness or population health outcomes. 3
The aims of this study were to 1) describe the feasibility of linking data from a national stroke registry with ambulance and emergency department presentation datasets; and 2) illustrate the value of the merged data in providing a greater understanding of pre-hospital care for people with suspected stroke. This body of work is the first step in determining the feasibility of a registry for pre-hospital stroke in Victoria.
Methods
Data for patients with stroke or transient ischaemic attack (TIA) admitted to Victorian hospitals participating in the Australian Stroke Clinical Registry (AuSCR) were linked with ambulance records (Ambulance Victoria, AV) and administrative data (Victorian Emergency Minimum Dataset, VEMD) collected between January 2013 and October 2017.
Data Sources
Australian Stroke Clinical Registry
The registry provided the inception cohort of confirmed case of stroke and TIA for this study. The AuSCR is a national clinical quality registry which was commenced in 2009 to enable routine collection of a minimum dataset of clinical quality of care indicators. Eligible AuSCR registrants are followed up between 90-180 days post stroke using a survey to elicit their health outcomes. 4 The AuSCR is a minimum dataset that relies on hospital clinicians for input, therefore limited data are collected on comorbidities and medical history since these can be obtained via other means using data linkage. 5 The AuSCR uses an opt-out method of consent in which patients at participating hospitals are automatically included. At hospitalisation, participants are provided with an information sheet explaining the purpose of the registry and instructions, if they wish, to exclude part or all of their information from the AuSCR. 6 The registry maintains data integrity through routine audits of data, site-level data quality reports and case-ascertainment reviews each year to assess for selection bias. In 2017, case ascertainment for the hospitals that provided ICD10-coded discharge diagnosis data (n = 46) ranged from 28% to 100%; median 81% (increasing from 77% in previous year). 7
Ambulance records
Ambulance Victoria is the sole provider of emergency medical services in the state of Victoria, covering a landmass of 227,038 square kilometres. 8 The state of Victoria is one of the smallest in terms of geographic size and is more densely populated than other states of Australia. The majority of people with suspected stroke are within a 1-hour drive time to a stroke capable hospital. 9 The ambulance service operates on a two-tiered response system consisting of advanced life support paramedics and intensive care paramedics with different scopes of practices. 10 Ambulance Victoria uses the Advanced Medical Priority Dispatch System (AMPDS; International Academies of Emergency Dispatch – IAED, Salt Lake City, United States)), a widely used commercial medical triage system that categorises cases into urgency-based triage categories. 11 A non-clinical emergency call-taker uses the triage tool to determine the location, nature and type of incident in order to categorise each call according to the patient’s chief complaint. Electronic Patient Care Records (ePCR) were implemented by AV in 2006 with complete roll-out across the state in 2008. 12 The paramedic recorded ePCR includes demographic information, case time series information, pickup location, symptoms, vital signs and pre-existing conditions, plus paramedic diagnosis and clinical management information. These data are primarily collected for provision of health service to patients and for monitoring performance and research.
Emergency department records
The Victorian Department of Health and Human Services (DHHS) collects information on emergency presentations occurring in Victoria. The Victorian Emergency Minimum Dataset (VEMD) is an emergency dataset collected according to the processes specified in the Emergency Department Care National Minimum Data Set standards. 13 It is a dataset which includes de-identified information on emergency department (ED) presentations at Victorian public hospitals. The data collected includes demographic, administrative and clinical information. These administrative data are collected to assist in service planning and case-mix funding. These data can be used to identify variations in care delivery and patient outcomes in Victoria especially when linked with disease registries such as the AuSCR.
Selection of Participants
The AuSCR diagnosis confirmed in hospital was used as the reference standard to compare to the provisional diagnoses made by ambulance personnel, classified as ‘suspected’ and ‘not suspected’ stroke. AuSCR registrants who were 18 years or older and arrived at hospital by ambulance were included. We excluded patients with an onset of stroke during their hospital admission for another condition, or if they had been transferred between hospitals. Strokes occurring before December 2014 were excluded because AV data were inconsistently collected between September and December 2014 due to paramedic industrial action.
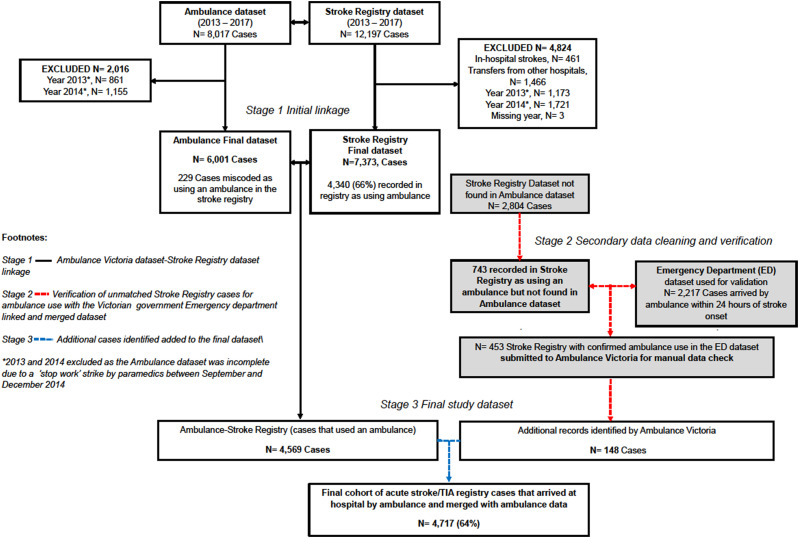
Data Linkage Procedure
In Australia we do not have a unique individual health identification number so we are reliant on matching people in different datasets based on their personal information such as name and date of birth. The linkage is undertaken by organisations with authorisation to hold personal information and a common project ID is then used to enable researchers to merge the datasets which are sent to them in a deidentified format (Supplemental Figure 1). In brief, identifiable patient information from AuSCR registrants admitted to Victorian hospitals with stroke or TIA were submitted to the DHHS and AV data linkage centres for patient matching (Supplemental Table 1). The emergency presentations dataset, that had been linked with AuSCR patients was subsequently merged to capture additional ambulance arrival episodes using a common project specific linkage key. In the AuSCR-AV dataset linkage, a probabilistic (‘fuzzy’) data linkage algorithm was employed using Stata (StataCorp, Texas, United States) and WinPure Clean and Match Enterprise (version 7.3.6.1, WinPure, New York, United States). Two stages of data linkage were performed using several different criteria in order to maximise the linkage rate. In the first stage, linkage was performed using full name (first and last), date of birth and date of arrival at ED or date of admission. The linkage was performed ‘1 to many’ such that a unique AuSCR record could be linked to many AV records based on episode of care as opposed to a patient-based match. Match scores >0.75 were assumed to be true matches, and matches <0.69 were assumed to be untrue. All patients with a match score 0.69 – 0.75 were manually reviewed for accuracy. In the second stage of the linkage, a data quality and validation review of the cases that did not match was performed. Linkage variables were the three first letters of first and last names, date of birth and the date of the call receipt (used to match to date of arrival at ED or date of admission). The fuzzy threshold for the second stage of the linkage was set at 80% to maximally capture the episodes of care that did not match. Match scores ≥80% resulted in the observations being linked together. In the final stage, additional cases identified in stage 2 were added to the merged cases in stage 1 (Figure 1). A brief overview of descriptive characteristics are provided. Categorical variables were summarised as frequencies and percentages, and continuous variables as median and interquartile range. Differences in characteristics between patients suspected of stroke and patients not suspected of stroke, and other variables were compared using Kruskal-Wallis tests for continuous variables and Pearson’s X2 tests for categorical variables. All analyses were performed using Stata/SE (version 15.0, StataCorp, Texas, United States). A P <0.05 was considered statistically significant.
Figure 1.
Merging and validation of stroke registry and ambulance data with emergency records.
Ethics
Ethics approval for this study was provided by the Monash University Human Research Ethics Committee (MUHREC 12770).
Results
Data for 12,197 patients registered in AuSCR were available for matching to 8,017 ambulance transports records (including 364 ambulance referral service records for 352 patients). Of these, we excluded strokes that occurred while the patient was in hospital for another condition (n = 461, 4%), those transferred from another hospital (n = 1,466, 13%) and for the years 2013 - 2014 or where the year was missing (n = 2,897, 28%) from the stroke registry. We excluded years 2013 - 2014 or missing year (n = 2,016, 25%) from the ambulance dataset. Overall, 7,373 case records for 6,649 patients in the AuSCR were available for linking to 6,001 records for 5,381 patients in the ambulance dataset; from which 4,569 (62%) patient records were able to be linked and merged.
Characteristics of the matched and unmatched cases are presented in Table 1. We reviewed records that merged and did not merge between datasets and verified information for overlapping variables (e.g. use of ambulance in AuSCR and the VEMD). The ambulance dataset was used as the reference standard for use of ambulance services. The first stage included a data quality assessment for cases where arrival by ambulance in the registry was recorded as positive. We subsequently found 743 cases with transport by ambulance recorded in the AuSCR with no corresponding record in the ambulance dataset. Based on information provided in the emergency department dataset, 453 of these cases had evidence of arrival to hospital by road ambulance. The 453 cases were submitted to AV for manual searching, whereby an additional 148 cases were confirmed as arriving by ambulance, and were subsequently included in the final merged dataset. The final linked cohort included 4,717 records for 4,287 patients (64%). This analysis was performed on 4,287 unique patients (denominator) with a single record in the stroke registry.
Table 1.
Characteristics of patients from merging Australian Stroke Clinical Registry (AuSCR) and Ambulance Victoria (AV) data.
| Matched (N = 4569) n (%) | AV only (N = 1432) n (%) | AuSCR only (N = 2804) n (%) | AuSCR - Arrived by ambulance (matched data, N = 3,597, 80%) n (%) | |||
|---|---|---|---|---|---|---|
| Suspected of stroke 3604 (79) | Not suspected of stroke 965 (21) | Suspected of stroke 843 (59) | Not suspected of stroke 589 (41) | |||
| Female | 1495 (41) | 436 (45) | 341 (41) | 189 (40) | 1153 (41) | 1521 (42) |
| Age (y) | ||||||
| <65 | 972 (27) | 281 (29) | 345 (41) | 323 (40) | 1105 (39) | 952 (26) |
| 65-74 | 1167 (32) | 297 (31) | 280 (33) | 192 (33) | 844 (30) | 1167 (32) |
| 75+ | 1465 (41) | 386 (40) | 218 (26) | 162 (27) | 855 (31) | 1478 (41) |
| Median age (Q1, Q3) | 72 (63, 78) | 73 (64, 79) | 68 (56, 75) | 68 (57, 75) | 69 (59, 77) | 73 (64, 79) |
| Country of birth | ||||||
| Australia | 2273 (66) | 598 (66) | Variable not collected by AV | 1783 (67) | 2290 (67) | |
| United Kingdom | 231 (7) | 68 (7) | 179 (7) | 216 (6) | ||
| Italy | 197 (6) | 59 (6) | 103 (4) | 203 (6) | ||
| Other European | 420 (12) | 111 (12) | 272 (10) | 415 (12) | ||
| Asia | 135 (4) | 37 (4) | 202 (8) | 139 (4) | ||
| Other countries | 163 (4) | 38 (5) | 142 (5) | 163 (5) | ||
| Previous stroke/TIA | 828 (26) | 187 (22) | Variable not collected by AV | 516 (21) | 873 (25) | |
| Type of stroke | ||||||
| Hemorrhagic | 367 (11) | 143 (17) | Variable not collected by AV | 191 (7) | 440 (12) | |
| Ischemic | 2190 (66) | 565 (66) | 1687 (62) | 2436 (68) | ||
| TIA | 604 (18) | 122 (14) | 793 (29) | 632 (18) | ||
| Undetermined stroke | 141 (4) | 29 (3) | 66 (2) | 85 (2) | ||
| Stroke severity | ||||||
| Able to walk on admission | 734 (41) | 716 (34) | Variable not collected by AV | 1538 (64) | 1220 (36) | |
Ability to walk on admission (proxy for stroke severity collected in AuSCR, Ambulance Victoria collects Glasgow Comma Scale); TIA = transient ischaemic attack; Q1 = 25th percentile; Q3 = 75th percentile.
Notes: 1) Of the AuSCR epidsodes that were not matched (n = 2,804) to the AV dataset, majority did not arrive by ambulance (n = 1,721, 61%); others arrived by ambulance (n = 743, 27%) and others had missing arrival status (n = 340, 12%).
Characteristics of patients suspected of stroke by paramedics in the final matched cohort are presented in Table 2. Among those matched; 42% were female and median age at stroke 73 years. Suspected diagnosis by paramedics were: stroke or TIA 69% (ischaemic 67%, intracerebral haemorrhage 12%; TIA 19% and undetermined 2%) and other conditions 31%. Patients 75 years or older were more likely to be suspected of stroke. Paramedics used the Melbourne Ambulance Stroke Screen tool and correctly identified 81% of patients as stroke/TIA. Hospital pre-notification was recorded in 56% of patients suspected of stroke/TIA compared to 16% of those not suspected of stroke/TIA by paramedics. Of those suspected of stroke by paramedics, 53% arrived to hospital within 4.5hrs. Overall, .<1% were transported using an air ambulance, 93% via an emergency ambulance and the remainder by non-emergency ambulance transport.
Table 2.
Characteristics of AuSCR confirmed stroke patients and associations with identification of stroke by paramedics.
| Suspected stroke/TIA; N = 2937 N (%) | Not suspected stroke/TIA; N = 1350 N (%) | P-value | |
|---|---|---|---|
| Female | 1208 (41) | 605 (45) | .023 |
| Age (in y) | |||
| Less than 65 | 773 (26) | 396 (29) | .030 |
| 65-74 | 921 (32) | 436 (32) | |
| 75+ | 1243 (42) | 517 (38) | |
| Median age (Q1, Q3) | 73 (64, 79) | 72 (63, 78) | <.001 |
| Born in Australia | 1819 (62) | 848 (62) | .581 |
| Identifies as aboriginal and torres strait islander | 32 (1) | 20 (1) | .278 |
| Interpreter required | 194 (7) | 102 (8) | .252 |
| Onset of symptoms <4.5 h | 1541 (53) | 460 (35) | <.001 |
| Type of stroke | |||
| Ischaemic | 1915 (67) | 831 (63) | .115 |
| Intracerebral haemorrhage | 334 (12) | 162 (12) | |
| Transient Ischaemic attack | 552 (19) | 285 (22) | |
| Undetermined | 61 (2) | 36 (3) | |
| Severe stroke (Unable to walk on admission) | 2007 (68) | 901 (67) | .299 |
| Documented previous stroke | 594 (23) | 234 (20) | .046 |
| Hospital pre-notification | 1668 (57) | 214 (16) | <.001 |
| Use of Melbourne ambulance stroke scale | 2371 (81) | 141 (11) | .000 |
| Patient’s place of residence | |||
| Metropolitan area | 1750 (60) | 827 (62) | .272 |
| Regional area | 1147 (40) | 503 (38) | |
AuSCR = Australian Stroke Clinical Registry; Ability to walk on admission (proxy for stroke severity collected in AuSCR; TIA = transient ischaemic attack; Q1 = 25th percentile; Q3 = 75th percentile; aPlace of residence defined as Accessibility and Remoteness Index of Australia.
Discussion
For the first time, ambulance and emergency presentation records and data from a stroke registry have been linked as part of a project grant funded by the Stroke Foundation. In this report we show the successful linkage and validation of information between these datasets. This innovative feasibility project establishes routine linkages and the ongoing two-way exchange of data to monitor health system issues between a state-wide ambulance service and hospitals. This data infrastructure will support other relevant research in stroke being conducted in Victoria and may be potentially scalable to other states since the same ambulance data collection is used, and the AuSCR is a national registry. Additionally, these data could also form the basis of developing robust performance indicators for the ambulance services and triage of patients with stroke.
We cross-referenced data between the different data sources to verify cases and improve the reliability and to validate our match results. For “arrival by ambulance” collected in the AuSCR, we adjudicated AV transport as reference for ambulance use. Records in the VEMD dataset were used to verify discrepancy between the AuSCR and AV. We found records that were positive for “arrival by ambulance” in the registry but had no corresponding record in the ambulance dataset. A reasonable explanation for the mis-match between the datasets may be due to the method of linkage or the accuracy and completeness of the data within each data source. 14 As Australian residents do not have a unique national health identifier, data linkage relies on common identifiers (such as names, dates of birth or Medicare number) and these may be collected with varying degrees of accuracy and completeness in prehospital and hospital settings. Our work is consistent with a new study from the United States 15 which sought to compare deterministic and probabilistic approaches for matching state emergency service records to a national stroke registry. Similar to our study, the probabilistic linkage method yielded the highest linkage rate of 67.7% compared to the deterministic method (45.5%).
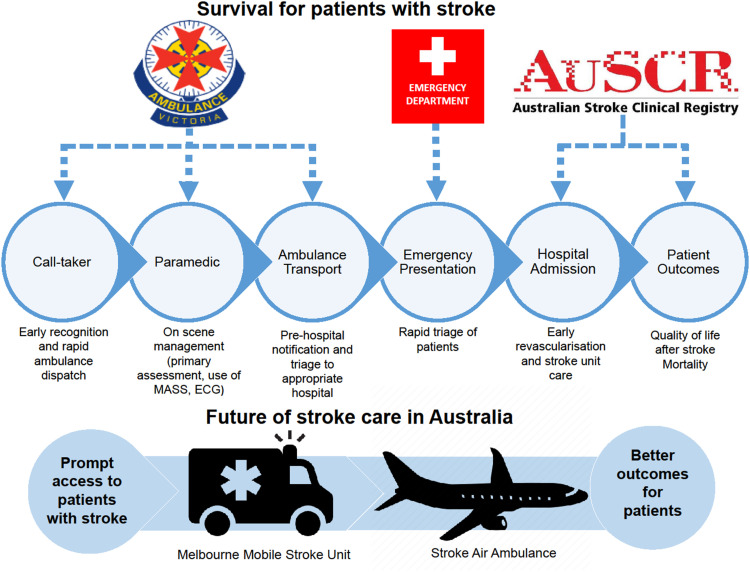
The merged data from this study will expand our potential to identify gaps in pre-hospital and hospital management processes related to improving acute stroke care and recovery (Figure 2). We can also explore factors that affect the performance of ambulance services, emergency departments and stroke units in the delivery of timely treatment. Additionally, these data will provide evidence to evaluate Ambulance policy or innovative programs such as the Melbourne Mobile Stroke Ambulance. Evidence generated from this research will be used to address the health inequity of access to stroke care between rural/remote and metropolitan communities, and for planning new operational models of stroke ambulances (road and air) in Victoria and Australia-wide.
Figure 2.
Continuum of stroke care through the Australian healthcare system.
Strengths and Limitations
There are several strengths to this study. We provide evidence for the successful linkage of ambulance records with a stroke registry for investigation of prehospital care in an Australian setting. We used AuSCR confirmed stroke diagnosis as a reference for patients with stroke unlike some studies 16 that use provisional ED discharge diagnosis. Secondly, Ambulance Victoria is the only provider of emergency ambulance services in Victoria. Therefore, linking these data with existing disease-specific registries such as the AuSCR maximises and supplements information that is not readily available in either dataset. This provides an opportunity for assessment of the continuum of care for patient with stroke through the healthcare system. In this project, we use a two-step process where data content was separated between analysts and custodians. Content data with project specific ID numbers were used to merge the non-identifiable AuSCR content data with the non-identifiable Ambulance content data by data analysts, thus preserving the privacy.
Our study has some limitations that need acknowledgement. It is possible that patients who do not recognise their stroke symptoms may choose alternate pathways to present to hospital. Authors of a study from Australia have reported that patient with less severe stroke symptoms were more likely to use other means of transport than an ambulance for transportation to hospital. 17 Secondly, not all TIAs that present to hospital are included in the AuSCR, participation is voluntary, and full coverage of all stroke cases was not possible, limiting the generalisability of the findings to Victoria. Though this is the case, at the time of this study (2017), there were 26 public hospitals supported by the Victorian government to participate in the AuSCR. Based on the Stroke Foundation organisational survey, there were 28/30 public hospitals treating patients with stroke. Therefore, 93% of Victorian hospitals admit acute stroke participate in the AuSCR.
Conclusion
We provide evidence for the feasibility of linking ambulance records to a national stroke registry in an Australian setting. The ambulance and emergency datasets supplement the information collected in the AuSCR and can be used to improve data quality and cross validate the real-world clinical data.
Supplemental Material
Supplemental Material for Linking Data From the Australian Stroke Clinical Registry With Ambulance and Emergency Administrative Data in Victoria by Amminadab L Eliakundu, Karen Smith, Monique F. Kilkenny, Joosup Kim, Kathleen L. Bagot, Emily Andrew, Shelley Cox, Christopher F. Bladin, and Dominique A. Cadilhac in The Journal of Health Care Organization, Provision, and Financing
Acknowledgments
We acknowledge members of the AuSCR Steering Committee, staff from the Florey Institute of Neuroscience and Mental Health who manage the AuSCR, and the hospital clinicians and patients who contribute data to the AuSCR. We also acknowledge the Data Linkage Units from Victoria, and the Ambulance Victoria Centre for Research and Evaluation who linked and provided access to the data used in this study.
Author Contributions: ALE was the lead author and was responsible for data analysis and writing of the manuscript. KS, MFK, JK, KLB, EA, SC, CFB, DAC contributed to the study design, interpretation of the data, and editing of the manuscript for intellectual content.
Declaration of Conflicting Interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Funding: The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This project was funded by a Stroke Foundation Seed Grant for Research (APPSeed1808).The following authors receive Research Fellowship support from the NHMRC: MFK (1109426); DAC (11542730). EA receives an NHMRC Post-Graduate Scholarship (2003449). ALE receives a Departmental Scholarship from Monash University. Other: The AuSCR was supported by grants from the National Health and Medical Research Council (NHMRC: 1034415), Monash University, Queensland Health, Victorian Department of Health and Human Services, the Stroke Foundation, Allergan Australia, Ipsen, Boehringer Ingelheim, and consumer donations.
Data Availability: The data that support the findings of this study are held by third parties and are not publicly available. Data may be available from authors upon reasonable request with permission from Ambulance Victoria, the Australian Stroke Clinical Registry and the Victorian Department of Health.
Supplemental Material: Supplemental material for this article is available online.
References
- 1.Bradley CJ, Penberthy L, Devers KJ, Holden DJ. Health services research and data linkages: issues, methods, and directions for the future. Health Serv Res. 2010;45(5 Pt 2):1468-1488. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Andrew NE, Sundararajan V, Thrift AG, et al. Addressing the challenges of cross-jurisdictional data linkage between a national clinical quality registry and government-held health data. Aust N Z J Publ Health. 2016;40(5):436-442. [DOI] [PubMed] [Google Scholar]
- 3.Jorm L. Routinely collected data as a strategic resource for research: Priorities for methods and workforce. Public health research & practice. 2015;25(4):e2541540. [DOI] [PubMed] [Google Scholar]
- 4.Cadilhac DA, Lannin NA, Anderson CS, et al. Protocol and pilot data for establishing the Australian Stroke clinical registry. Int J Stroke. 2010;5(3):217-226. [DOI] [PubMed] [Google Scholar]
- 5.Kilkenny MF, Kim J, Andrew NE, et al. Maximising data value and avoiding data waste: A validation study in stroke research. Med J Aust. 2019;210(1):27-31. [DOI] [PubMed] [Google Scholar]
- 6.Cadilhac D, Lannin N, Anderson C, et al. The Australian Stroke Clinical Registry Annual Report Victoria. Parkville, VIC: The Florey Institute of Neuroscience and Mental Health; 2014. December 2015. [Google Scholar]
- 7.Breen S, Kim J, Kilkenny M, et al. The Australian Stroke Clinical Registry Data Quality Report Victoria. Parkville, VIC: The Florey Institute of Neuroscience and Mental Health; 2017. March 2019. [Google Scholar]
- 8.Area of Australia - states and territories ACT. https://www.ga.gov.au/scientific-topics/national-location-information/dimensions/area-of-australia-states-and-territories. Accessed Febuary 3, 2020.
- 9.Bladin CF, Kim J, Bagot KL, Vu N, Moloczij S, Price C. Improving acute stroke care in regional hospitals: clinical evaluation of the Victorian Stroke Telemedicine program. Med J Aust. 2020;212(8):371-377. [DOI] [PubMed] [Google Scholar]
- 10.Eastwood K, Morgans A, Stoelwinder J, Smith K. Patient and case characteristics associated with 'no paramedic treatment' for low-acuity cases referred for emergency ambulance dispatch following a secondary telephone triage: a retrospective cohort study. Scand J Trauma Resuscitation Emerg Med. 2018;26(1):8. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eastwood K, Morgans A, Smith K, Hodgkinson A, Becker G, Stoelwinder J. A novel approach for managing the growing demand for ambulance services by low-acuity patients. Aust Health Rev. 2016;40(4):378-384. [DOI] [PubMed] [Google Scholar]
- 12.Cox S, Martin R, Somaia P, Smith K. The development of a data-matching algorithm to define the 'case patient'. Aust Health Rev. 2013;37(1):54-59. [DOI] [PubMed] [Google Scholar]
- 13.Victorian Emergency Minimum Dataset (VEMD) . User Manual 18th Edition 2013-14. Melbourne, Victoria: Department of Health and Human Services, Victorian Government; 2013. [Google Scholar]
- 14.Bohensky MA, Jolley D, Sundararajan V, et al. Data Linkage: A powerful research tool with potential problems. BMC Health Serv Res. 2010;10(1):346. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15.Oostema JA, Nickles A, Reeves MJ. A comparison of probabilistic and deterministic match strategies for linking prehospital and in-hospital stroke registry data. J Stroke Cerebrovasc Dis. 2020;29(10):105151. [DOI] [PubMed] [Google Scholar]
- 16.Williams TA, Blacker D, Arendts G, et al. Accuracy of stroke identification by paramedics in a metropolitan pre-hospital setting: A cohort study. Australasian Journal of Paramedicine. 2017;14(2). [Google Scholar]
- 17.Eliakundu AL, Cadilhac DA, Kim J, et al. Factors associated with arrival by ambulance for patients with stroke: a multicentre, national data linkage study. Australas Emerg Care. 2021. [DOI] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental Material for Linking Data From the Australian Stroke Clinical Registry With Ambulance and Emergency Administrative Data in Victoria by Amminadab L Eliakundu, Karen Smith, Monique F. Kilkenny, Joosup Kim, Kathleen L. Bagot, Emily Andrew, Shelley Cox, Christopher F. Bladin, and Dominique A. Cadilhac in The Journal of Health Care Organization, Provision, and Financing