Abstract
Objective
The impact of the coronavirus disease 2019 (COVID-19) pandemic on cancer care remains a concern. We aimed to evaluate access to diagnosis and treatment for lung cancer during the pandemic.
Methods
Times (days) from lung cancer symptom onset or referral to visit (pre-visit time), from visit to diagnosis (pre-diagnosis time), and from diagnosis to treatment (pre-treatment time) during the pandemic were compared with the times during the pre-pandemic period.
Results
The number of patients diagnosed with lung cancer was 82 and 75 during the pandemic and pre-pandemic periods, respectively. The percentage of patients with advanced-stage cancer was higher (65.9% vs. 46.7%), the percentage of patients treated with surgery was lower and the percentage treated with medication was higher (24.4% vs. 41.3% and 57.3% vs. 40.0%, respectively), the pre-visit time was longer (28.2 vs. 11.4 days), and the pre-treatment time for surgery was longer (67.3 vs. 45.6 days) during the pandemic compared with the times during the pre-pandemic period, respectively.
Conclusions
The COVID-19 pandemic resulted in delayed diagnoses, which could have led to patients being diagnosed with advanced disease. The pandemic also resulted in delayed therapy owing to the requirement for available intensive care unit beds for emergencies, including surgery.
Keywords: Coronavirus disease 2019, pandemic, delay, lung cancer, diagnosis, treatment, intensive care unit, visit, surgery
Introduction
The consequences of the coronavirus disease 2019 (COVID-19) pandemic on cancer care are a concern. Patients with thoracic malignancies are at a high risk of mortality. 1 To prevent nosocomial transmission among patients and healthcare providers, visits, examinations, and procedures were restricted during the pandemic, and many focused efforts were underway, including pre-screening for severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) using real-time reverse transcription polymerase chain reaction (RT-qPCR) before hospitalization. The increase in the number of COVID-19 patients shifted the functioning of hospitals from general practice to COVID-19 care and decreased the availability of intensive care units (ICU) for surgeries. 2 As a result, diagnostic investigations were abbreviated, and surgical treatment was replaced by radiotherapy in the United Kingdom (UK).3,4 Moreover, patients hesitated to visit hospitals because they were afraid of becoming infected in the hospital or outside their homes. 5
The period between diagnosis and treatment is associated with mortality in cancer. 6 In lung cancer, disease progression because of delayed treatment can reduce the chance of surgery. 5 The delay until treatment can be because of patient- or doctor-related reasons. The former comprises the time from the onset of symptoms or referral by primary clinics to the visit to specialized hospitals, and the latter comprises the diagnostic process and waiting time for treatment. This study aimed to assess the impact of the COVID-19 pandemic on delayed visits, examinations, and treatments for lung cancer.
Methods
Study population, follow-up time, and ethical consent
The medical charts of patients with lung cancer from the Tokyo Dental College, Ichikawa General Hospital were analyzed retrospectively. The hospital is a 570-bed healthcare facility that offers diagnostic procedures, including bronchoscopy and image-guided percutaneous biopsy; examinations for cancer staging; and treatments, namely surgery, irradiation, and medication. The hospital also offers diagnostic tests for COVID-19 using RT-qPCR and medical care for hospitalized patients with COVID-19. There were no outbreaks or transmissions in our hospital among the medical staff and patients during the study period.
This study was approved by the ethics committee of the Tokyo Dental College (reference number: I 21–27), and the study was conducted in accordance with the tenets of the Declaration of Helsinki. The requirement for informed consent was waived owing to the retrospective nature of this study.
The first case of COVID-19 in Japan was confirmed in January 2020. Since February 2020, preventive measures, such as hand washing, social distancing, and universal masking, have been implemented. The first case of COVID-19 was confirmed and admitted to our hospital in March 2020. Therefore, we defined the period affected by the COVID-19 pandemic as March 2020 to March 2021. Patients newly diagnosed with lung cancer during this period were compared with patients diagnosed during the pre-pandemic period of March 2018 to March 2019. Patients with lung cancer who were diagnosed pathologically and treated with surgery, irradiation, or anti-cancer medication were included, and those without a definitive diagnosis were excluded. Patients who received best supportive care (BSC) and no anti-cancer treatment were also excluded. The observation period of this study was up to December 2021, and the follow-up time for therapies was 9 months from the time of diagnosis.
Definitions of the evaluated time points
The pre-visit time was defined as the number of days from the date of onset of lung cancer symptoms, or from the date of referral by primary clinics or cancer screening facilities (whichever was earlier) to the date of the first visit to our hospital. The pre-diagnosis time was defined as the number of days from the date of the first visit to the date of pathological diagnosis of lung cancer. The pre-treatment time was designated from the date of diagnosis to the date of surgery, first date of irradiation, or first date of medication. Therapy was defined as the first therapy recorded in the medical charts, and the medications comprised cytotoxic drugs, immune-checkpoint inhibitors, and/or tyrosine kinase inhibitors.
Statistical analysis
Data are presented as mean ± standard deviation. The Mann–Whitney U-test was performed to assess differences between continuous variables during the pandemic and pre-pandemic periods. Subgroup analyses for non-small cell lung cancer (NSCLC) and small-cell lung cancer (SCLC), and early- (I/II/IIIA) and advanced-stage (IIIB/IIIC/IV) lung cancer were performed as the standard treatment was decided based on the histology and the stage. Categorical variables were tested using the χ2 distribution with Pearson’s correction. Statistical significance was set at p < 0.05. All data were analyzed using JMP software, version 9.0.2, for Windows (SAS Institute Japan, Tokyo, Japan).
Results
The number of patients diagnosed with lung cancer was 90 and 91 during the COVID-19 pandemic (March 2020 to March 2021) and the pre-pandemic period (March 2018 to March 2019), respectively. The number of diagnosed cases was 5 in May, 6 in June, and 12 in July in 2020, whereas this number was 8 in May, 8 in June, and 7 in July in 2018. In the other months, no noticeable differences in the numbers of patients between the pandemic and pre-pandemic periods were observed. The number of patients included in this study was 82 during the COVID-19 pandemic and 75 during the pre-pandemic period after exclusion of BSC cases (Figure 1). The characteristics of the patients with lung cancer are shown in Table 1. There were no differences in the patients’ age or sex between the pandemic and pre-pandemic periods. Although there was no difference in the number of NSCLC cases between the two periods, the number of SCLC cases was higher in the pandemic period than that in the pre-pandemic period, resulting in a higher percentage of SCLC cases in the pandemic period than that in the pre-pandemic period (p = 0.035). The percentage of patients with advanced-stage disease (IIIB/IIIC/IV) was higher during the pandemic compared with the pre-pandemic period (65.9% vs. 46.7%, respectively; p = 0.015). The percentage of patients treated with surgery was lower, and the percentage of patients treated with medication was higher, during the pandemic compared with percentages during the pre-pandemic period (24.4% vs. 41.3% and 57.3% vs. 40.0%, respectively; p = 0.027).
Figure 1.
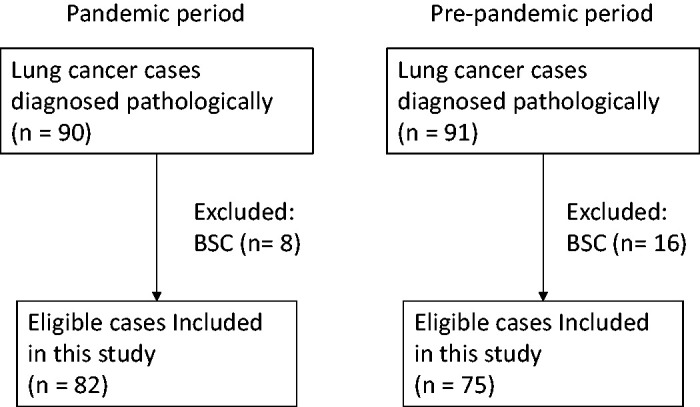
Flowchart of the cases diagnosed with lung cancer. Patients who received best supportive therapy (BSC) were excluded, and only those who received anti-cancer therapies were included, in this study.
Table 1.
Patients’ characteristics.
| Pandemic period (n = 82) | Pre-pandemic period (n = 75) | p | |
|---|---|---|---|
| Age (mean ± SD) | 71.5 ± 8.5 | 71.5 ± 8.7 | 0.98 |
| Sex | 0.56 | ||
| Male (%) | 59 (72.0) | 57 (76.0) | |
| Female (%) | 23 (28.0) | 18 (24.0) | |
| Subtype | 0.035 | ||
| NSCLC (%) | 63 (76.8) | 67 (89.3) | |
| SCLC (%) | 19 (23.2) | 8 (10.7) | |
| Stage | 0.015 | ||
| I/II/IIIA (%) | 28 (34.1) | 40 (53.3) | |
| IIIB/IIIC/IV (%) | 54 (65.9) | 35 (46.7) | |
| Therapy | 0.027 | ||
| Surgery | 20 (24.4) | 31 (41.3) | |
| Chemoradiation | 13 (15.9) | 8 (10.7) | |
| Radiation | 2 (2.4) | 6 (8.0) | |
| Medication | 47 (57.3) | 30 (40.0) | |
| Visit | 0.007 | ||
| Symptomatic | 39 (47.6) | 20 (26.7) | |
| Referral | 43 (52.4) | 55 (73.3) |
SD, standard deviation; NSCLC, non-small cell lung cancer; SCLC, small-cell lung cancer.
As shown in Table 2, the pre-visit time was longer by 17 days during the pandemic than that during the pre-pandemic period (28.2 vs 11.4 days, respectively). However, the pre-treatment time was shorter during the pandemic than that during the pre-pandemic period. Regarding surgery, the pre-treatment time of 20 patients during the pandemic was longer than that of 31 patients during the pre-pandemic period. Regarding medication, the pre-visit time was longer, and the pre-treatment time was shorter, during the pandemic compared with the times during the pre-pandemic period. The pre-visit time among both the early- (I/II/IIIA) and late-stage (IIIB/IIIC/IV) cancer patients was longer during the pandemic than that during the pre-pandemic period. The pre-visit delays (between the pandemic and pre-pandemic periods) were 7 days for early-stage (I/II/IIIA) lung cancer and 20 days for late-stage (IIIb/IIIC/IV) lung cancer. During the pandemic period, the percentage of referred cases was lower for late-stage cancer compared with that of early-stage cancer (37% vs 82%, respectively).
Table 2.
Time (days) for each process until treatment for lung cancer.
| Pandemic period | Pre-pandemic period | p | |
|---|---|---|---|
| All | n = 82 | n = 75 | |
| Pre-visit time | 28.2 ± 39.8 | 11.4 ± 22.5 | <0.0001 |
| Pre-diagnosis time | 21.5 ± 31.1 | 17.9 ± 14.5 | 0.91 |
| Pre-treatment time | 30.4 ± 25.6 | 35.8 ± 23.1 | 0.036 |
| Surgery | n= 20 | n= 31 | |
| Pre-visit time | 9.8 ± 9.8 | 9.4 ± 17.1 | 0.11 |
| Pre-diagnosis time | 42.7 ± 55.7 | 21.7 ± 15.8 | 0.52 |
| Pre-treatment time | 67.3 ± 22.6 | 45.6 ± 23.1 | 0.0022 |
| Chemoradiation | n= 13 | n= 8 | |
| Pre-visit time | 32.5 ± 46.7 | 16.0 ± 24.2 | 0.49 |
| Pre-diagnosis time | 18.8 ± 17.8 | 11.6 ± 7.0 | 0.69 |
| Pre-treatment time | 20.8 ± 12.1 | 23.5 ± 14.0 | 0.97 |
| Radiation | n= 2 | n= 6 | |
| Pre-visit time | 63.0 ± 86.3 | 19.8 ± 28.8 | 0.31 |
| Pre-diagnosis time | 13.0 ± 7.1 | 14.8 ± 12.2 | 0.87 |
| Pre-treatment time | 14.5 ± 7.8 | 19.8 ± 11.4 | 0.97 |
| Medication | n= 47 | n= 30 | |
| Pre-visit time | 33.3 ± 42.3 | 10.6 ± 26.1 | 0.0001 |
| Pre-diagnosis time | 13.6 ± 8.8 | 16.3 ± 14.6 | 0.95 |
| Pre-treatment time | 18.0 ± 10.8 | 32.1 ± 22.9 | 0.0066 |
| Stage I/II/IIIA | n = 28 | n = 40 | |
| Pre-visit time | 14.5 ± 28.8 | 7.6 ± 15.4 | 0.0106 |
| Pre-diagnosis time | 36.4 ± 48.9 | 20.9 ± 15.6 | 0.72 |
| Pre-treatment time | 53.1 ± 28.2 | 45.2 ± 24.0 | 0.27 |
| Stage IIIB/IIIC/IV | n = 54 | n = 35 | |
| Pre-visit time | 35.3 ± 43.0 | 15.4 ± 28.2 | 0.003 |
| Pre-diagnosis time | 13.7 ± 9.1 | 14.5 ± 12.5 | 0.59 |
| Pre-treatment time | 18.6 ± 13.5 | 25.0 ± 16.5 | 0.10 |
Data are presented as mean ± standard deviation.
Table 3 shows the characteristics of the patients with NSCLC. The percentage of patients with advanced-stage cancer (IIIB/IIIC/IV) was higher during the pandemic than that during the pre-pandemic period (61.9% vs. 43.3%, respectively; p = 0.033). As shown in Table 4, the pre-visit time was longer during the pandemic than that during the pre-pandemic period. Regarding surgery, the pre-treatment time of 19 patients during the pandemic was longer than that of 30 patients during the pre-pandemic period. Regarding medication, the pre-visit time was longer, and the pre-treatment time was shorter, during the pandemic than these times during the pre-pandemic period. The pre-visit time among both early-stage (I/II/IIIA) and late-stage (IIIB/IIIC/IV) lung cancer patients was longer during the pandemic compared with during the pre-pandemic period.
Table 3.
Characteristics of the patients with non-small cell lung cancer.
| Pandemic period (n = 63) | Pre-pandemic period (n = 67) | P | |
|---|---|---|---|
| Age (mean ± SD) | 71.4 ± 9.1 | 72.2 ± 8.4 | 0.84 |
| Sex | 0.83 | ||
| Male (%) | 46 (73.0) | 50 (74.6) | |
| Female (%) | 17 (27.0) | 17 (25.4) | |
| Stage | 0.033 | ||
| I/II/IIIA (%) | 24 (38.1) | 38 (56.7) | |
| IIIB/IIIC/IV (%) | 39 (61.9) | 29 (43.3) | |
| Therapy | 0.16 | ||
| Surgery (%) | 19 (30.2) | 30 (44.8) | |
| Chemoradiation (%) | 8 (12.7) | 7 (10.5) | |
| Radiation (%) | 2 (3.2) | 5 (7.5) | |
| Medication (%) | 34 (54.0) | 25 (37.3) |
SD, standard deviation.
Table 4.
Time (days) for each process until treatment for non-small cell lung cancer.
| Pandemic period | Pre-pandemic period | p | |
|---|---|---|---|
| All | n = 63 | n = 67 | |
| Pre-visit time | 29.5 ± 41.4 | 12.1 ± 23.5 | 0.0001 |
| Pre-diagnosis time | 22.7 ± 34.8 | 18.1 ± 14.3 | 0.64 |
| Pre-treatment time | 35.2 ± 26.7 | 37.8 ± 23.3 | 0.24 |
| Surgery | n = 19 | n = 30 | |
| Pre-visit time | 10.2 ± 9.9 | 9.6 ± 17.3 | 0.09 |
| Pre-diagnosis time | 44.1 ± 56.8 | 22.3 ± 15.6 | 0.61 |
| Pre-treatment time | 69.4 ± 20.1 | 46.0 ± 23.4 | 0.0011 |
| Chemoradiation | n = 8 | n = 7 | |
| Pre-visit time | 47.1 ± 55.2 | 17.7 ± 25.6 | 0.27 |
| Pre-diagnosis time | 16.4 ± 13.7 | 11.0 ± 7.3 | 0.60 |
| Pre-treatment time | 21.3 ± 14.3 | 25.1 ± 14.3 | 0.82 |
| Radiation | n = 2 | n = 5 | |
| Pre-visit time | 63.0 ± 86.3 | 23.8 ± 30.3 | 0.43 |
| Pre-diagnosis time | 13.0 ± 7.0 | 10.4 ± 6.3 | 0.56 |
| Pre-treatment time | 14.5 ± 7.8 | 17.2 ± 10.5 | 0.70 |
| Medication | n = 34 | n = 25 | |
| Pre-visit time | 34.2 ± 43.8 | 11.2 ± 28.3 | 0.0004 |
| Pre-diagnosis time | 12.7 ± 9.6 | 16.6 ± 14.0 | 0.55 |
| Pre-treatment time | 20.5 ± 9.3 | 35.8 ± 23.1 | 0.0137 |
| Stage I/II/IIIA | n = 24 | n = 38 | |
| Pre-visit time | 16.1 ± 30.9 | 8.0 ± 15.8 | 0.0182 |
| Pre-diagnosis time | 38.6 ± 51.8 | 20.9 ± 15.6 | 0.64 |
| Pre-treatment time | 57.7 ± 27.8 | 45.8 ± 24.5 | 0.08 |
| Stage IIIB/IIIC/IV | n = 39 | n = 29 | |
| Pre-visit time | 37.8 ± 45.1 | 17.6 ± 30.4 | 0.0069 |
| Pre-diagnosis time | 12.8 ± 9.6 | 14.3 ± 11.8 | 0.89 |
| Pre-treatment time | 21.3 ± 13.4 | 27.4 ± 16.8 | 0.23 |
Data are presented as mean ± standard deviation.
Table 5 shows the characteristics of the patients with SCLC. There were no differences in the stages or treatments between the pandemic and pre-pandemic periods. In addition, there were no differences in the time for each process until treatment between the pandemic and pre-pandemic periods (Table 6).
Table 5.
Characteristics of the patients with small-cell lung cancer.
| Pandemic period (n = 19) | Pre-pandemic period (n = 8) | p | |
|---|---|---|---|
| Age (mean ± SD) | 71.8 ± 6.5 | 67.8 ± 11.0 | 0.38 |
| Sex | 0.28 | ||
| Male (%) | 13 (68.4) | 7 (87.5) | |
| Female (%) | 6 (31.6) | 1 (12.5) | |
| Stage | 0.83 | ||
| I/II/IIIA (%) | 4 (21.1) | 2 (25.0) | |
| IIIB/IIIC/IV (%) | 15 (79.0) | 6 (75.0) | |
| Therapy | 0.34 | ||
| Surgery (%) | 1 (5.3) | 1 (12.5) | |
| Chemoradiation (%) | 5 (26.3) | 1 (12.5) | |
| Radiation (%) | 0 (0) | 1 (12.5) | |
| Medication (%) | 13 (68.4) | 5 (62.5) |
SD, standard deviation.
Table 6.
Time (days) for each process until treatment for small-cell lung cancer.
| Pandemic period | Pre-pandemic period | p | |
|---|---|---|---|
| All | n = 19 | n = 8 | |
| Pre-visit time | 23.8 ± 34.5 | 5.5 ± 10.0 | 0.054 |
| Pre-diagnosis time | 17.6 ± 13.0 | 16.4 ± 17.1 | 0.35 |
| Pre-treatment time | 14.5 ± 11.8 | 18.4 ± 11.8 | 0.41 |
| Medication | n = 13 | n = 5 | |
| Pre-visit time | 31.1 ± 39.6 | 7.6 ± 12.6 | 0.15 |
| Pre-diagnosis time | 15.7 ± 6.4 | 15.0 ± 19.0 | 0.21 |
| Pre-treatment time | 11.4 ± 12.1 | 13.8 ± 10.1 | 0.37 |
| Stage IIIB/IIIC/IV | n = 15 | n = 6 | |
| Pre-visit time | 28.7 ± 37.5 | 7.0 ± 11.3 | 0.15 |
| Pre-diagnosis time | 16.1 ± 7.2 | 15.2 ± 17.0 | 0.29 |
| Pre-treatment time | 11.6 ± 11.2 | 13.5 ± 9.1 | 0.46 |
Data are presented as mean ± standard deviation.
As shown in Table 1, the percentage of symptomatic patients was higher during the COVID-19 pandemic compared with the pre-pandemic period (p = 0.007). The percentage of referred cases was higher for patients who underwent surgery compared with the percentage of patients treated with medication (90% vs 63%, respectively) during the pandemic. Symptomatic cases comprised patients who visited our hospital directly and those who were referred to our hospital from clinics they had visited because of symptoms related to lung cancer. The referred cases included patients who were suspected of having lung cancer after screening examinations or with incidental findings identified through imaging performed for other purposes. Table 7 shows the time for each process in the symptomatic and referral sub-groups. In the patients referred from clinics they had visited because of symptoms, the pre-visit time was defined as the number of days from the date of the onset of symptoms to the visit to our hospital. Although this length of time was not significantly different between the pre-pandemic and pandemic periods, the pre-visit time was longer (49.0 vs 32.3 days), and the pre-treatment time was shorter, during the pandemic compared with the pre-pandemic period, respectively, for symptomatic cases. In the referred cases, the pre-visit time was longer by 5.6 days during the pandemic than that during the pre-pandemic period (p = 0.0126).
Table 7.
Time (days) for each process until treatment for the symptomatic and referral cases.
| Pandemic period | Pre-pandemic period | p | |
|---|---|---|---|
| Symptomatic | n = 39 | n = 20 | |
| Pre-visit time | 49.0 ± 47.7 | 32.3 ± 35.4 | 0.13 |
| Pre-diagnosis time | 14.5 ± 11.3 | 15.5 ± 13.9 | 0.74 |
| Pre-treatment time | 20.0 ± 18.1 | 30.8 ± 25.4 | 0.12 |
| Referral | n = 43 | n = 55 | |
| Pre-visit time | 9.3 ± 15.2 | 3.7 ± 5.3 | 0.0126 |
| Pre-diagnosis time | 27.8 ± 40.8 | 18.8 ± 14.8 | 0.79 |
| Pre-treatment time | 39.8 ± 27.8 | 37.6 ± 22.1 | 0.88 |
Data are presented as mean ± standard deviation.
Discussion
In the present study, we observed that the pre-visit time was longer during the pandemic than that during the pre-pandemic period. The percentage of patients treated with surgery was lower, and the pre-treatment time before surgery was longer, during the pandemic compared with the pre-pandemic period. Conversely, the pre-treatment time for medication was shorter during the pandemic than that during the pre-pandemic period. To our knowledge, this is the first report showing the number of days of delay, including the delay for each process, from symptom onset to treatment, during the COVID-19 pandemic.
Although we had expected fewer patients diagnosed with lung cancer during the pandemic, there was no difference in the number of patients between the pandemic and pre-pandemic periods. This finding was similar to a study from Korea showing that there were no differences in the number of patients with lung cancer before and after the COVID-19 pandemic. 5 However, a slight reduction was observed in the number of newly diagnosed lung cancer cases during the pandemic in Italy. 7 One possibility for this difference could be the differential magnitude of pandemic cases between countries. However, it was difficult to explain why the number of patients with SCLC was higher during the pandemic compared with the pre-pandemic period, in our study. No differences were observed when the analysis was limited to patients with NSCLC. To exclude the effects of SCLC, we analyzed the data for NSCLC and SCLC patients separately.
The percentage of referred cases was lower during the pandemic than the percentage of cases pre-pandemic, similar to the findings of a previous report suggesting more symptomatic cases with newly diagnosed breast cancer.8,9 The reason for the reduction may be attributed to the decline in the number of screenings. For the referred cases, the longer pre-visit time of 5.6 days during the pandemic was because of the restricted visits to the hospital. The overall pre-visit time during the pandemic was 17 days longer than that during the pre-pandemic period. A pre-visit delay was observed in patients treated with medication, but not with surgery. The reason for the lack of a pre-visit delay with surgery was attributed to the higher percentage of cases referred for surgery compared with the percentage treated with medication (90% vs 63%, respectively) during the pandemic. The pre-visit delay (between the pandemic and pre-pandemic periods) was 7 days for early-stage (I/II/IIIA) lung cancer and 20 days for late-stage (IIIB/IIIC/IV) lung cancer. The reason for the longer delay in the late-stage patients was owing to the lower percentage of referred cases (37%) compared with the percentage of referred early-stage patients (82%). It is possible that some patients were diagnosed at a more advanced stage because of disease progression during the pre-visit delay, resulting in less chances of undergoing surgery.
There are some possible reasons for the pre-visit delay identified in this study. The collateral effects of COVID-19 affected both patients and hospitals. One possibility is that the delay was caused by patients who hesitated to visit the hospital to avoid contracting COVID-19 infection. 5 Another possibility is that the delay was caused by the hospital regarding referred cases. Access to hospital services was limited during the pandemic because of the shift of functions from the care of patients with cancer to those with COVID-19. 10 The number of appointments was limited to prevent overcrowding and transmission in the hospital, which resulted in a decreased number of visits. Additionally, the shift of functions led to decreased activity in the operating rooms and ICUs, resulting in a pre-treatment delay in patients with lung cancer.2,11 Screening PCR and chest computed tomography (CT) scans prior to surgery are effective in preventing COVID-19 transmission. 12 These preventive screening tests were performed in our hospital, which may be another possible cause of the pre-treatment delay. However, the pre-treatment delay for patients with advanced stages of lung cancer was shorter during the pandemic compared with the pre-pandemic period. It is possible that the pre-visit delay led to the need for urgent medical therapy. In Canada, many patients with advanced lung cancer were forced to experience delays in chemotherapy as a direct result of the COVID-19 pandemic. 13 In contrast, the present study showed a shorter pre-treatment time, indicating that medical therapies were not influenced by the COVID-19 pandemic. One reasons for the activity in the pulmonary department not decreasing during the pandemic in our study was that there was no outbreak in our hospital.
The delay from cancer diagnosis to surgery has been reported to influence prognosis. The survival rate of patients was shorter for those who underwent treatment within 90 to 120 days from diagnosis compared with those who underwent treatment within 0 to 30 days. 6 It was unclear whether a pre-treatment delay of 69 days, as shown in our study, would induce a poor prognosis. Conversely, the time between preoperative diagnostic CT imaging and surgical treatment was reported to be associated with an increased risk of recurrence. 14 Patients who underwent surgical treatment within 12 weeks of diagnosis had better overall survival than those who underwent procedures that were delayed for more than 12 weeks. 14 The total of 123 days for pre-visit, pre-diagnosis, and pre-treatment times encountered by patients in our study undergoing surgery could increase the risk of recurrence or poor prognosis in the future.
A limitation of our study is the inclusion of a small number of patients from a single hospital. Although a study in Italy showed no significant delays from the onset of symptoms to diagnosis or treatment, 7 it was difficult to conclude whether the results of this study have implications for other areas or countries because there are substantial differences in the severity of the pandemic and in medical systems between countries. Further studies involving a larger number of patients in multiple hospitals are needed to confirm diagnostic and treatment delays resulting from the COVID-19 pandemic. Another limitation is that it is unclear how much the delay shown in our study may influence the prognosis of patients in the future. Analyses of the patients’ survival times will answer this question. Our data from the patients’ medical charts did not show the reason for the pre-visit delays we identified in this study. Analyses of the reasons are needed to improve the assessment of collateral effects of the pandemic.
In conclusion, this study showed that the COVID-19 pandemic resulted in delays in diagnosis; possibly leading to more patients being diagnosed with advanced disease. The pandemic also resulted in a delay in therapy owing to the requirement for the availability of ICU beds in case of emergencies, such as for surgery. Medical care providers need to assess the collateral effects of the COVID-19 pandemic on service delivery for patients with lung cancer.
Footnotes
Declaration of conflicting interest: The authors declare that they have no competing interests.
Funding: This research received no specific grant from any funding agency in the public, commercial, or not-for-profit sectors.
Author Contributions: TT contributed to the collection of clinical data, data analysis, and manuscript writing. AT, EI, AK, TN, and KE contributed to interpretation of the clinical data. All authors have read and approved the final manuscript.
ORCID iDs: Takeshi Terashima https://orcid.org/0000-0002-4353-7647
Aoi Kuroda https://orcid.org/0000-0002-8751-9600
Availability of data and material
All data generated or analyzed during this study are included in this published article.
References
- 1.Whisenant JG, Baena J, Cortellini A, et al. A definitive prognostication system for patients with thoracic malignancies diagnosed with COVID-19: an update from the TERAVOLT registry. J Thorac Oncol 2022; 17: 661–674. doi:10.1016/j.jtho.2021.12.015. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Wahlster S, Sharma M, Lewis AK, et al. The coronavirus disease 2019 pandemic's effect on critical care resources and health-care providers: a global survey. Chest 2021; 159: 619–633. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Spencer K, Jones CM, Girdler R, et al. The impact of the COVID-19 pandemic on radiotherapy services in England, UK: a population-based study. Lancet Oncol 2021; 22: 309–320. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4.Banfill K, Croxford W, Fornacon-Wood I, et al. Changes in the management of patients having radical radiotherapy for lung cancer during the first wave of the COVID-19 pandemic in the UK. Clin Oncol (R Coll Radiol) 2022; 34: 19–27. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Park JY, Lee YJ, Kim T, et al. Collateral effects of the coronavirus disease 2019 pandemic on lung cancer diagnosis in Korea. BMC Cancer 2020; 20: 1040. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Mayne NR, Elser HC, Darling AJ, et al. Estimating the impact of extended delay to surgery for stage I non-small-cell lung cancer on survival. Ann Surg 2021; 273: 850–857. [DOI] [PubMed] [Google Scholar]
- 7.Cantini L, Mentrasti G, Russo GL, et al. Evaluation of COVID-19 impact on DELAYing diagnostic-therapeutic pathways of lung cancer patients in Italy (COVID-DELAY study): fewer cases and higher stages from a real-world scenario. ESMO Open 2022; 7: 100406. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Knoll K, Reiser E, Leitner K, et al. The impact of COVID-19 pandemic on the rate of newly diagnosed gynecological and breast cancers: a tertiary center perspective. Arch Gynecol Obstet 2022; 305: 945–953. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Linck PA, Garnier C, Depetiteville MP, et al. Impact of the COVID-19 lockdown in France on the diagnosis and staging of breast cancers in a tertiary cancer centre. Eur Radiol 2022; 32: 1644–1651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Ranganathan P, Sengar M, Chinnaswamy G, et al. Impact of COVID-19 on cancer care in India: a cohort study. Lancet Oncol 2021; 22: 970–976. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Sokas C, Kelly M, Sheu C, et al. Cancer in the shadow of COVID: early-stage breast and prostate cancer patient perspectives on surgical delays due to COVID-19. Ann Surg Oncol 2021; 28: 8688–8696. DOI: 10.1245/s10434-021-10319-0. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Puylaert CAJ, Scheijmans JCG, Borgstein ABJ, et al. Yield of screening for COVID-19 in asymptomatic patients before elective or emergency surgery using chest CT and RT-PCR (SCOUT): multicenter study. Ann Surg 2020; 272: 919–924. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Elkrief A, Kazandjian S, Bouganim N. Changes in lung cancer treatment as a result of the coronavirus disease 2019 pandemic. JAMA Oncol 2020; 6: 1805–1806. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Heiden BT, Eaton DB, Jr, Engelhardt KE, et al. Analysis of delayed surgical treatment and oncologic outcomes in clinical stage I non-small cell lung cancer. JAMA Netw Open 2021; 4: e2111613. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Data Availability Statement
All data generated or analyzed during this study are included in this published article.


