Abstract
The authors provide the first age-standardized race/ethnicity-specific, state-specific vaccination rates for the United States. Data encompass all states reporting race/ethnicity-specific vaccinations and reflect vaccinations through mid-October 2021, just before eligibility expanded below age 12. Using indirect age standardization, the authors compare racial/ethnic state vaccination rates with national rates. The results show that white and Black state median vaccination rates are, respectively, 89 percent and 76 percent of what would be predicted on the basis of age; Hispanic and Native rates are almost identical to what would be predicted; and Asian American/Pacific Islander rates are 110 percent of what would be predicted. The authors also find that racial/ethnic vaccination rates are associated with state politics, as proxied by 2020 Trump vote share: for each percentage point increase in Trump vote share, vaccination rates decline by 1.08 percent of what would be predicted on the basis of age. This decline is sharpest for Native American vaccinations, although these are reported for relatively few states.
Keywords: COVID-19, vaccination, racial/ethnic disparities, age adjustment, Trump vote
In the United States, coronavirus disease 2019 (COVID-19) vaccination rates vary by race and by state (Ndugga et al. 2021). They also vary quite a bit by age, with 86 percent vaccination of U.S. residents aged 65 to 74 but only 53 percent vaccination of those aged 18 to 24 years, as of October 10, 2021 (see details in the Appendix). This variation in vaccination rates by age can confound racial and state vaccination patterns, because some population groups are older than others. In particular, the non-Hispanic white population is substantially older than all other populations: the median age in the United States is 43 years for the non-Hispanic white population, compared with 36 years for the non-Hispanic Asian American and Pacific Islander population, 33 years for both the non-Hispanic Black and Native populations, and just 30 years for Hispanic populations. This suggests that aggregate population vaccination rates may be relatively higher for white populations compared with others simply because the white populations have more people at older ages.
COVID-19 mortality rates are frequently presented in age-adjusted form in order to facilitate comparisons across racial/ethnic and other populations (e.g., Ahmad et al. 2021). But vaccination rates are rarely presented this way, although one analysis examined age-adjusted vaccination rates for racial/ethnic groups in cities and towns in Massachusetts (Calef and Schuster 2021). Here, we present the first age-adjusted COVID-19 vaccination rates for each racial/ethnic group in each state for which data are available. These age-adjusted rates reveal racial and state vaccination patterns net of the shared pattern that older people are more likely than younger people to be vaccinated.
Our results capture the period shortly before vaccination was opened to ages 5 to 11. We combine Kaiser Family Foundation data on state-specific shares of vaccination going to each racial/ethnic group (released on October 18, 2021) with Centers for Disease Control and Prevention data on state-level vaccination rates (released on October 21, 2021). Additionally, we incorporate subsidiary data collected by the Centers for Disease Control and Prevention and the National Center for Health Statistics (described in the Appendix).
We used a technique called “indirect age standardization” (Preston, Heuvelin, and Guillot 2001:26–28) to create race-specific, state-specific vaccination levels that adjust for each group’s unique age distribution. For each racial group in each state, these indirectly standardized rates are the ratio of the actual vaccination rate to the vaccination rate that would be predicted solely on the basis of that population’s age distribution (in conjunction with the national age pattern of COVID-19 vaccination). Thus, when this quantity exceeds 1, the group is more vaccinated than would be predicted on the basis of age; when it is less than 1, the group is less vaccinated than would be predicted. This method allows groups to be compared, revealing variation in their vaccination rates above and beyond that associated with age.
Results reveal two major patterns: (1) substantial racial variation in vaccination above and beyond the variation associated with age and (2) state-level variation, both overall and for all racial groups, that is associated with state politics.
Figure 1A shows stark variation across racial groups in vaccination rates, adjusted for age. In most states, white and Black populations are vaccinated much less than would be expected on the basis of their age distributions (with median adjusted vaccination rates across states of 89 percent and 76 percent of expectation, respectively); Hispanic and Native populations are vaccinated, on average, very similarly to what one would expect (median 100 percent and 99 percent of expectation, respectively); and Asian American and Pacific Islander populations are vaccinated much more than would be expected (median 110 percent of expectation). The tall, symmetrical shape of the Native distribution indicates vaccination rates that vary widely across states, without any clear peak range of values, though we caution that data on this population are reported by relatively few states (see Appendix).
Figure 1.
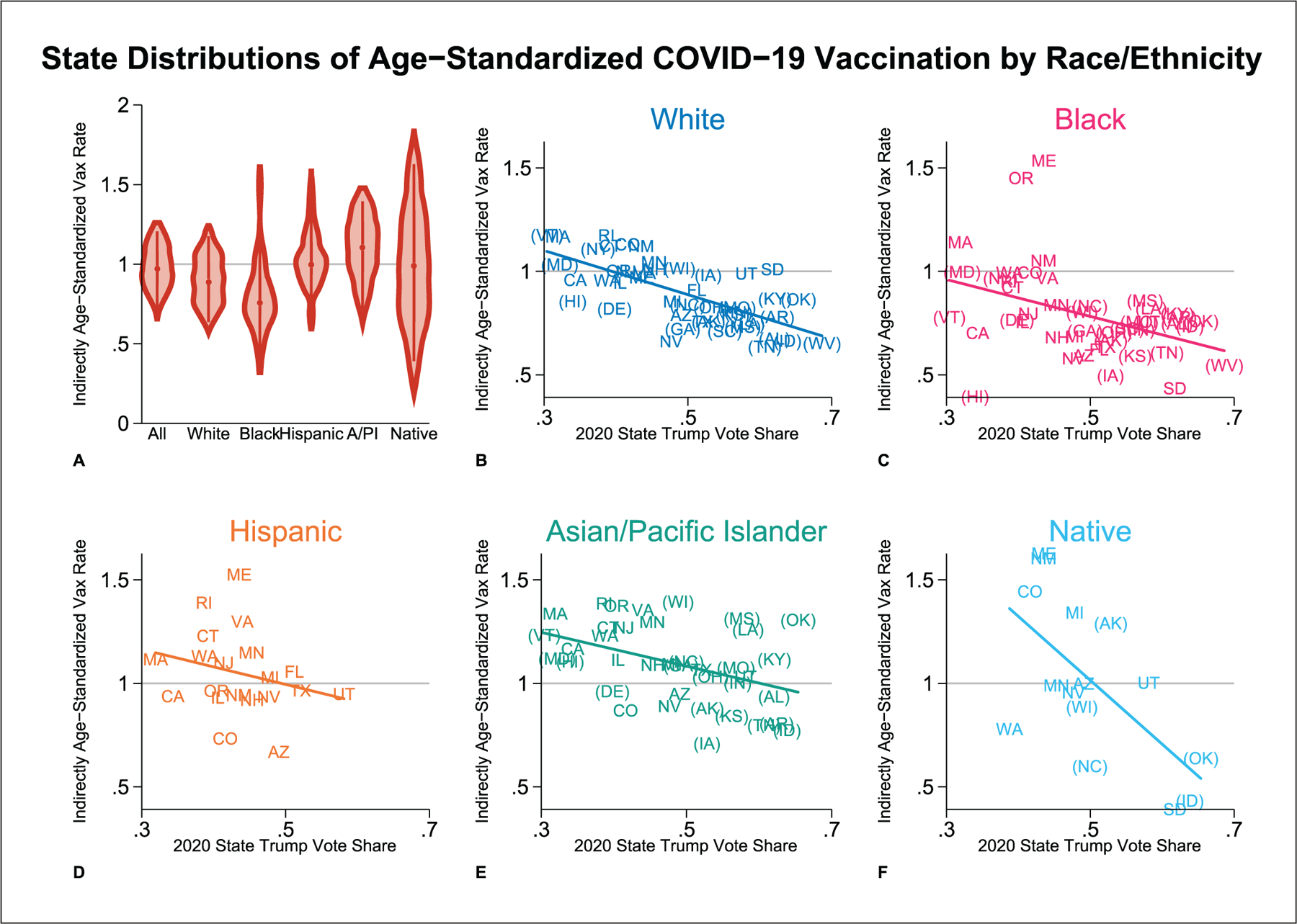
Age-standardized vaccination by race/ethnicity and state (as of October 2021).
Note: Indirectly age-standardized vaccination rates are depicted by state and race/ethnicity. When these rates exceed 1, the population displayed has vaccination rates higher than would be expected on the basis of its age distribution; when the rates are less than 1, the population has vaccination rates lower than would be expected. Panel A presents a series of violin plots showing the distribution across states of age-standardized vaccination rates for each racial/ethnic group, smoothed using the Epanechnikov kernel. In this panel, the category labels stand for state aggregate, white, Black, Hispanic, Asian/Pacific Islander, and Native, respectively. Panels B to F show the state-specific, race/ethnicity-specific age-standardized vaccination rates as a function of states’ overall Trump vote share. States differ in their handling of Hispanic populations. Some exclude Hispanic individuals from other racial groups; others include Hispanic individuals in other racial groups. The latter states are labeled in panels B to F with parentheses surrounding their state abbreviations for racial groups other than Hispanic, indicating that those racial groups include Hispanic individuals. Population denominators match states’ reported handling of Hispanic individuals in vaccination data. State-specific, race/ethnicity-specific vaccination rates are based on vaccine share data from the Kaiser Family Foundation (October 18, 2021, data release) and state-level vaccination rates from the Centers for Disease Control and Prevention (October 21, 2021, data release). Age standardization is based on national age-specific vaccination rates from the Centers for Disease Control and Prevention (October 15, 2021, data download, reflecting vaccinations through October 6, 2021) and state-specific, race/ethnicity-specific population estimates from the National Center for Health Statistics.
These vaccine distributions can also be weighted by population size, rather than treating each state equally, to better approximate national populations for each racial group rather than summarize states, although the distributions will not exactly track national populations, as not all states report racial/ethnic data. When the distributions are weighted by population size, median age-adjusted vaccination rates are very similar to the medians of the state distributions for white and Black populations (91 percent and 75 percent of expectation, respectively). However, Hispanic and, especially, Native median vaccination rates are lower than when states are weighted equally (96 percent and 89 percent of expectation, respectively), indicating that, in states reporting racial/ethnic data, Hispanic and Native people disproportionately live in states where they have low vaccination rates. The reverse is true of median Asian/Pacific Islander rates (117 percent of expectation).
The most striking pattern in Figure 1A is that only a handful of states (Maine, Massachusetts, New Mexico, and Oregon, as well as the District of Columbia) have Black populations whose vaccination rates are higher than one would predict on the basis of national vaccination rates by age. This is particularly notable given the young age distribution of most states’ Black populations. Age adjustment in a young population will tend to make it look relatively more vaccinated by partially explaining low vaccination rates as simply the consequence of age. Yet even with this adjustment, Black vaccination rates are substantially lower than vaccination rates of all other racial groups.
The undervaccination of white populations, relative to expectation, is also an important result in Figure 1A. Age adjustment highlights the extent to which, net of age, white populations are less vaccinated than most others, which is partially disguised in aggregate population rates because the white populations are so much older than all others.
State-level COVID-19 vaccination rates are also associated with state politics, as shown in Figures 1B to 1F, which use each state’s 2020 Trump vote share as a crude proxy for the state political context. Averaged across states, each additional percentage point of the state vote that went to Trump in 2020 is associated with the state’s total vaccination rate (adjusted for age) being lower by 1.08 percent of what it would be predicted to be on the basis of the state’s age distribution. (All regression results are reported in the Appendix.) These results are consistent with those of other analyses showing that COVID-19 cases and deaths are strongly associated, at the county level, with partisan political leaning (Krieger et al. 2021).
This relationship between state politics and state vaccination levels is also reproduced for each separate racial group. For Hispanic populations alone, the relationship between state Trump share and state vaccination rate is not statistically significant. Notably, these panels reveal that states with high Trump share do not report vaccination rates by Hispanic ethnicity, which also suggest that overall Hispanic vaccination distributions analyzed here may overreport vaccination. Some, but not all, states with high Trump share have very small Hispanic populations. The available data do not have sufficient statistical power to distinguish the relationship of different racial groups’ vaccination to Trump share from one another. But as a simple description, we note that the white vaccination rate varies with Trump share to almost exactly the same degree as the state aggregate vaccination rates do, while Black, Hispanic, and Asian/Pacific Islander groups vary less. The Hispanic and Black groups’ age-adjusted vaccination have the smallest relationship to Trump vote, with a loss of only 0.89 (Black) or 0.85 (Hispanic) percentage points of expected vaccination associated with each additional point of Trump share. Strikingly, the Native rate of age-adjusted vaccination varies with Trump share far more dramatically than other racial groups’ rates do, with each additional Trump point associated with a 3.1 percentage point decline in Native vaccination relative to expectation. (However, results for Native populations should be interpreted cautiously, as those vaccinations are reported in the fewest states. See further data comments in the Appendix.)
These results are qualitatively robust to data restrictions designed to overcome the differential handling of Hispanic individuals across states—particularly, to make sure that the relationship we found between race-specific vaccination and state Trump vote is not confounded by this variation in measurement. The key difference in how Hispanic individuals are counted is that 21 states exclude Hispanic individuals from all other racial categories, while 24 states allow Hispanic ethnicity to cross-cut race, so that Hispanic individuals might be counted as both Hispanic and another race. (The remaining states do not report race-specific vaccination data.) In alternative analyses, we restrict the other-than-Hispanic data to only state-race observations in which Hispanic individuals are no more than 10 percent of the group’s vaccine-eligible population. Thus, we include all Hispanic observations, all observations from states in which Hispanic ethnicity does not cross-cut race, and race-state observations for which cross-cutting Hispanic individuals are a small portion of the vaccine-eligible population; we exclude other race-state observations for which Hispanic individuals are a larger part of the vaccine-eligible population. For example, we include the Black population of North Carolina (3.5 percent are Hispanic as well as Black) but exclude the Black population of New York (22 percent are Hispanic as well as Black). In regression models run on this restricted sample (presented in the Appendix alongside the main regression results), Trump share is still associated with reduced vaccination, an association that is still significantly significant for all racial groups except Hispanic.
We do not claim that Trump voting drives these vaccination rates. Rather, Trump vote share is used as a proxy for a broad range of state political characteristics that may be related to vaccination in many different ways, including via urbanicity, beliefs about COVID-19, and longtime patterns of funding and state support for public health infrastructure. Because lack of vaccination has multiple causes, the relatively lower vaccination rates in states with higher Trump support may also have different contributing factors for different racial groups living in those states. For example, it is possible that relatively low vaccination rates in the white populations disproportionately reflect self-consciously politicized vaccine rejection, while relatively low rates in other populations may be more likely to reflect characteristics of state health infrastructures.
These age-standardized rates reveal systematic and substantial variation in vaccination levels across states, racial groups, and the intersection of the two, net of differences in population age.
Supplementary Material
Acknowledgments
We thank the Kaiser Family Foundation for answering questions about the data they have generously made available and Michelle Niemann for feedback on an article draft.
Funding
The author(s) disclosed receipt of the following financial support for the research, authorship, and/or publication of this article: This research was supported by the Eunice Kennedy Shriver National Institute of Child Health and Human Development via the Minnesota Population Center (P2C HD041023) and through a fellowship to Kaitlyn M. Berry (F31 HD107980).
Biographies
Author Biographies
Elizabeth Wrigley-Field is an assistant professor in the Department of Sociology and the Minnesota Population Center at the University of Minnesota, Twin Cities. She is a mortality demographer specializing in racial inequality, formal demographic modeling, COVID-19, and historical infectious disease.
Kaitlyn M. Berry has a master’s degree in public health from the Boston University School of Public Health and is currently completing her PhD in epidemiology at the University of Minnesota School of Public Health. As a social epidemiologist, her research focuses on how non–health care social policies shape health and well-being.
Govind Persad is an assistant professor in the University of Denver Sturm College of Law, where he specializes in health law and bioethics. During the COVID-19 pandemic, he has researched legal, ethical, and empirical issues related to vaccine distribution. He holds a PhD and JD from Stanford University.
Footnotes
Supplemental Material
Supplemental material for this article is available online.
References
- Ahmad Farida B., Cisewski Jodi A., Arialdi Miniño, and Anderson Robert N. 2021. “Provisional Mortality Data—United States, 2020.” Morbidity and Mortality Weekly Reports 70(14):519–22. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Calef Anne, and Schuster Luc. 2021. “Despite Progress, Vaccination Gaps by Race and Town Remain.” Boston Indicators Retrieved November 2, 2021. https://www.bos-tonindicators.org/reports/report-website-pages/covid_indicators-x2/2021/april/vaccinations.
- Krieger N, Chen JT, Testa C, Waterman PD, and Hanage WP 2021. “Political Lean: A Crucial Variable for monitoring COVID-19 in the United States.” Harvard Center for Population and Development Working Paper Series 21(5). [Google Scholar]
- Ndugga Nambi, Hill Latoya, Artiga Samantha, and Haldar Sweta. 2021. “Latest Data on COVID-19 Vaccinations by Race/Ethnicity” Kaiser Family Foundation. Retrieved November 18, 2021. https://www.kff.org/coronavirus-covid-19/issue-brief/latest-data-on-covid-19-vaccinations-by-race-ethnicity/ [Google Scholar]
- Preston Samuel H., Heuvelin Patrick, and Guillot Michel. 2001. Demography: Measuring and Modeling Population Processes Cambridge, MA: Wiley-Blackwell. [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


