Abstract
In most high‐resource countries with organized screening programs, the incidence and mortality of cervical cancer is decreasing. Recent statistics have also revealed a reduction in invasive cervical cancer incidence as a result of national vaccination programs. Paradoxically, cervical cancer incidence has increased in Japan, particularly amongst women of reproductive age. This study aimed to examine the trends in cervical cancer incidence and mortality for young and middle adult women in Japan, by analyzing trends in 10‐year interval age‐groups. Cervical cancer incidence for young and middle adult women (ages 20‐59 years) was obtained from high‐quality population‐based cancer registries in three prefectures from 1985 to 2015. National cancer mortality data were obtained from published vital statistics from 1985 to 2019. Trends in crude and age‐standardized rates (ASR) were analyzed using Joinpoint regression. The cervical cancer incidence trend in 20‐59‐year‐old women combined significantly increased over the observation period. Both crude and ASR increased from 1985 to 2015 with an annual percent change (APC) of +1.6% (95% confidence interval, 1.1, 2.1) and +1.7% (1.2, 2.3), respectively. Similar increases were seen in ages 20‐29, 30‐39, and 40‐49 years with higher APCs especially in 20s and 30s. Both crude and ASR mortality significantly increased after the early 1990s in ages 20‐59 years combined. Based on the recognition that current cervical cancer control strategies in Japan have not been effective in reducing the cervical cancer burden in young and middle adults, promotion of screening and vaccination should be urgently strengthened.
Keywords: cervical cancer, incidence, mortality, population surveillance, vital statistics
Trends in incidence and mortality of cervical cancer in young and middle‐aged women in Japan were analyzed by 10‐year interval age‐groups using long‐term high‐quality data. Incidence and mortality showed significant increase in young and middle adults from ages 20 to 59 years old. These results emphasize the importance of cervical cancer control in Japan.
Abbreviations
- APC
annual percent change
- ASR
age standardized rate
- CI
confidence interval
- CIN
cervical intraepithelial neoplasia
- HPV
human papillomavirus
- NOS
not otherwise specified
1. INTRODUCTION
Cervical cancer is a global public health problem, where the number of new cases is ranked 9th among all cancers with an estimated incidence of 604,127, and mortality of 341,831 in 2020 around the world. 1 Cervical cancer incidence has decreased in many high‐resource countries with organized cervical screening programs. 2 , 3 , 4 Additionally, recent analyses confirmed that well integrated HPV vaccine programs have also resulted in a reduction in cervical cancer. 5 , 6 , 7
In Japan, the Japanese government first offered financial support for cervical cancer screening in 1982. 8 Currently, the target age for population‐based screening is 20 years and older, and is recommended every 2 years. 8 The screening rate has gradually improved, from 22.6% in 2001 to 43.8% in 2019, but remains low compared to other OECD countries. 9 , 10 Public funding for HPV vaccination became available in 2010, and was included in the national immunization program for girls aged 12‐16 years, from April 2013. 11 In June 2013, proactive recommendation of the HPV vaccine program was suspended by the Ministry of Health, Labour and Welfare due to the concern of potential adverse effects reported in the media. 11 On November 12, 2021, the Counsel of Health Sciences agreed on terminating the suspension of proactive recommendation of HPV vaccines. 12
A previous analysis reported in July 2021 shows that age‐adjusted incidence and mortality rate for all ages combined is increasing in Japan, in contrast to the decreasing trend observed in many developed countries. 6 , 7 , 13 , 14 , 15
Cervical cancer is mostly known to occur in young and middle adults, and is frequently diagnosed between the ages of 35 and 55 years. 16 However, an assessment of the impact of the current system for cervical cancer in Japan for both incidence and mortality within this high‐risk age group has not yet been examined. Therefore, this study aimed to examine trends in cervical cancer incidence and mortality in young and middle adults, by analyzing trends in 10‐year interval age‐groups in order to characterize the impact of current cervical cancer control strategies in Japan.
2. MATERIALS AND METHODS
Cancer incidence data were obtained from population‐based cancer registries in three prefectures (Fukui, Nagasaki, and Yamagata) from years 1985 to 2015. These were acquired in the framework of the Monitoring of Cancer Incidence in Japan project, where data from the three prefectures were selected due to their availability of long‐term high‐quality data. 17 , 18 , 19 , 20 This dataset has been validated by usage for trend analyses and widely used in previous studies. 14 , 19 , 21 For cancer mortality, the number of annual cancer deaths and population data for the years 1985–2019 were obtained by released vital statistics. 22 The International Classification of Diseases version 10 code was used: C53 for malignant neoplasm of the cervix uteri; code D06 for CIN, grade III, with or without mention of severe dysplasia (excluding melanoma in situ and severe dysplasia of cervix) was included in the additional analysis. 23 We classified age groups by 10‐year intervals between ages 20 and 59 years to analyze trends in young and middle adults. We limited our analysis to this age range to specifically understand the trends among generations in the first peak with high prevalence of HPV infection. 24 , 25 , 26 All data analyzed in this study are publicly available (http://ganjoho.jp) with open access. No personal identifiers were recorded or used, and ethical approval was not required based on Ethics Guidelines.
A Joinpoint regression model was applied using the Joinpoint Regression Program version 4.9.0.0, developed by the US NCI. 27 In the Joinpoint regression analysis, the incidence or number of deaths was assumed to follow a Poisson distribution to estimate annual percent changes and identify any year in which a significant change in trends occurs. The maximum number of joinpoints was set at five, the minimum number of observations from a joinpoint to either end of the data was set at two, and the minimum number of observations between two joinpoints was set at three, following previous publications on overall cancer trends. 14 Crude rate was used as the dependent variable for incidence and mortality in each 10‐year age group of 20s–50s. Age standardized rate was used as the dependent variable for the pooled data for overall ages 20–59 years to adjust by age, which was standardized to the 1985 model Japanese population for cancer incidence and mortality. Annual percent change of crude rate and ASR were considered to be statistically significant when they were different from zero with a P value of <.05.
3. RESULTS
Figure 1 shows the observed crude rates in cervical cancer incidence from 1985 to 2015 by 10‐year interval age‐groups from ages 20 to 59 years in the three selected prefectures in Japan. The crude incidence was the highest among those aged 50‐59 years at 25.42 per 100,000 population at the beginning of the observation period in 1985. However, it dropped to its lowest at 10.40 in 1990 and has shown higher rates thereafter. Age group 40‐49 years had the second highest incidence in 1985 at 20.32, and increased to hit the highest rate in 2010 at 32.30. Age group 30‐39 years had a rate of 9.64 in 1985, intermittently increased and peaked at 33.69 in 2001, which is the highest among all analyzed age groups, with no steady decrease seen thereafter. As a result, the rates for 30‐ and 40‐year‐old age groups have exceeded those for 50‐year‐olds in recent years. The rate for those aged 20‐29 years was the lowest in 1985 at 0.90 and has increased since, with the highest marked in 2012 at 9.09.
FIGURE 1.
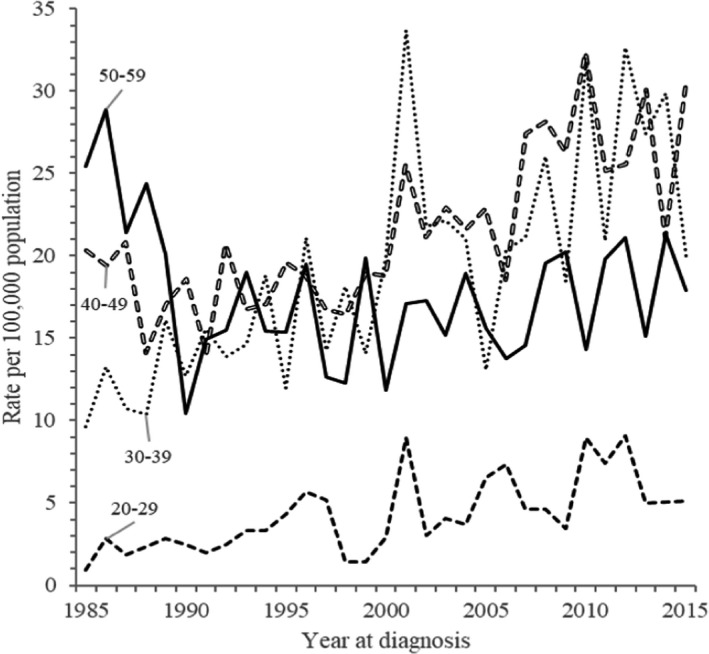
Annual trends in observed crude incidence rate in cervical cancer (1985‐2015) by age group. Data from three Japanese prefectures; Yamagata, Fukui, and Nagasaki
Figure 2 shows the modeled annual trends for cervical cancer incidence from 1985 to 2015 by 10‐year interval age‐groups from ages 20 to 59 years in the three selected prefectures in Japan. Trends by ASR among women aged 20‐59 years combined are also presented with plotted observed ASRs. Table 1 shows the results of Joinpoint regression analysis of the trends, with corresponding APC and 95% CIs. Overall trend of incidence using the ASR for ages 20‐59 years showed a significant increase throughout the whole period. Both crude and ASR sustainably increased from 1985 to 2015 with a significant APC of +1.6% (95% CI, 1.1, 2.1) and +1.7% (1.2, 2.3), respectively. Similarly, high levels of increase were seen in the 20‐, 30‐, and 40‐year‐old age groups, especially among 20s and 30s, with significant APCs of +4.0% (2.2, 5.9), +3.0% (2.1, 4.0) and +1.8% (1.2, 2.5) respectively. Among 50‐59‐year‐olds, although the incidence significantly decreased from the first year of observation until 1990 (APC, −12.3% [−19.5, −4.5]), it leveled off thereafter.
FIGURE 2.
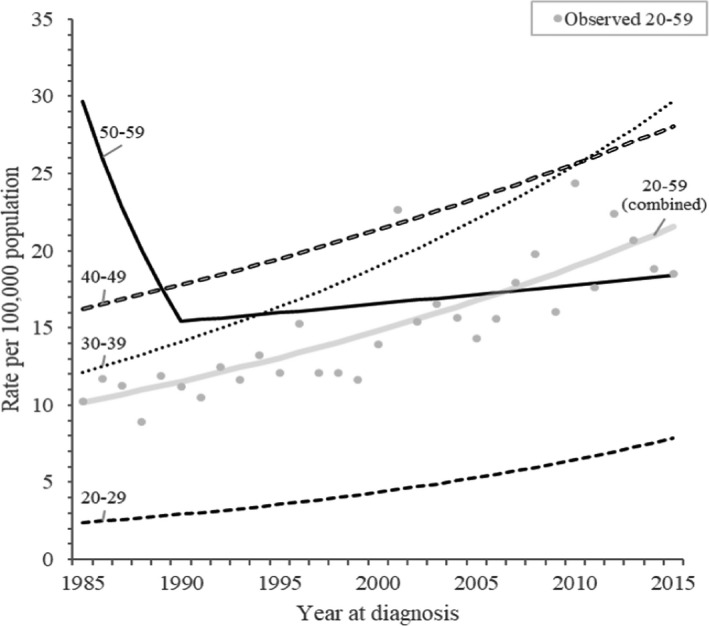
Annual trends in modelled incidence rate in cervical cancer (1985‐2015) by age group. Data from three Japanese prefectures: Yamagata, Fukui, and Nagasaki
TABLE 1.
Results of Joinpoint regression analysis on the trends in cervical cancer incidence by age group: Data from three Japanese prefectures a (1985‐2015)
| Age (y) | Number of joinpoints | Line segment | Annual % change | 95% confidence interval | ||
|---|---|---|---|---|---|---|
| Start | End | Lower | Upper | |||
| 20‐59 | ||||||
| Crude | 0 | 1985 | 2015 | 1.6 b | 1.1 | 2.1 |
| ASR | 0 | 1985 | 2015 | 1.7 b | 1.2 | 2.3 |
| 20‐29 | 0 | 1985 | 2015 | 4.0 b | 2.2 | 5.9 |
| 30‐39 | 0 | 1985 | 2015 | 3.0 b | 2.1 | 4.0 |
| 40‐49 | 0 | 1985 | 2015 | 1.8 b | 1.2 | 2.5 |
| 50‐59 | 1 | 1985 | 1990 | −12.3 b | −19.5 | −4.5 |
| 1990 | 2015 | 0.7 | −0.2 | 1.6 | ||
Abbreviation: ASR, age standardized rate.
Yamagata, Fukui, and Nagasaki prefectures.
Annual % change statistically significantly different from zero (P < .05).
Observed and modelled crude rates with CIN, grade III, with or without mention of severe dysplasia (excluding melanoma in situ and severe dysplasia of cervix) included (Figures S1, S2 and Table S1) also showed a significant rapid increase in incidence in all analyzed age groups combined until 2012. Similar to the trends without CIN, ages 30‐39 and 40‐49 years showed significant gain in APC throughout the years, and unlike the main analysis, this significant increasing trend was also seen in the 50‐59‐year‐olds from 2006 to 2015.
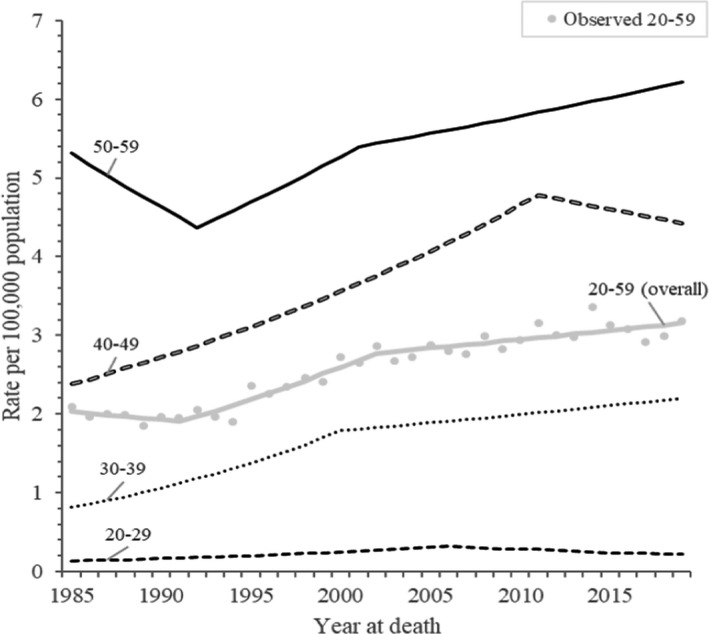
Figure 3 shows annual trends in observed crude mortality rates for cervical cancer by 10‐year interval age‐groups from age 20 to 59 years, obtained from the national data of Japan from 1985 to 2019. Observed mortality rate among age groups from highest to lowest was 50‐, 40‐, 30‐, and 20‐year‐olds at the beginning of the observation period in 1985, with rates of 5.37, 2.75, 0.85, 0.11 per 100,000 population, respectively, and the order remains the same until 2019. The lowest observed mortality was marked in 1994 for women aged 40‐49 and 50‐59 years, 1989 for those aged 30‐39 years, and 1988 for women aged 20‐29 years, and it increased thereafter in all age groups. In 2019, mortality was 6.51, 4.53, 2.29, and 0.19, respectively.
FIGURE 3.
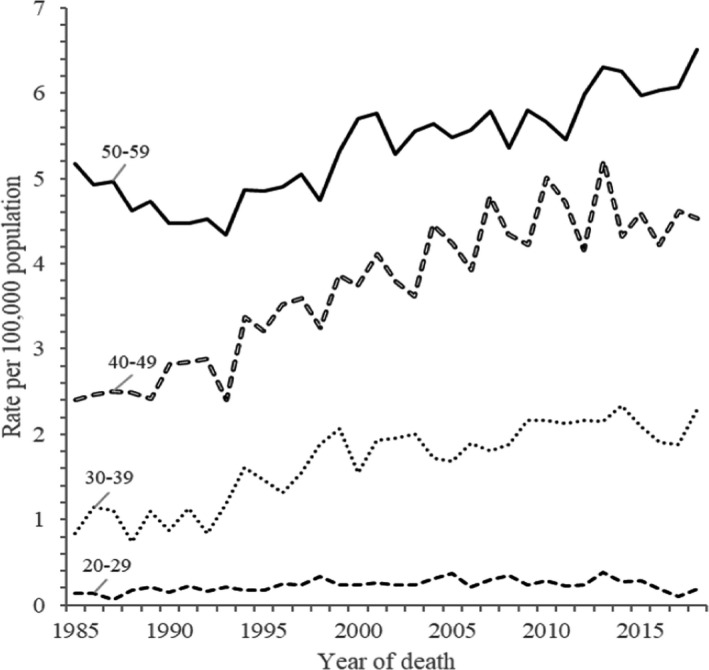
Annual trends in observed crude mortality rate in cervical cancer (1985‐2019) by age group. Data from Japanese national vital statistics
Figure 4 shows the modeled annual mortality trends from 1985 to 2019 by 10‐year interval age‐groups from 20 to 59 years old, along with the modelled and observed ASRs for ages 20‐59 years combined. Results of Joinpoint regression analysis on the trends in mortality by age group are shown in Table 2 with corresponding APC and 95% CI. For ages 20‐59 years combined, both the crude rate and ASR have significantly increased since the early 1990s. The ASR increased from 1991 with significant APCs of +3.5% (2.4, 4.6) (1991‐2002), and +0.8% (0.3, 1.2) (2002‐2019). For each individual age group, women aged 20‐29 years and 40‐49 years showed an increasing inclination until 2006 and 2011, respectively, but no significant trend was seen after those years. The 30‐39 years age group showed a significant continuous increasing trend throughout the observed periods. The greatest increase of this period was also observed in this age group; the APC was +5.4% (3.7, 7.1) from 1985 to 2000, followed by +1.1% (0.1, 2.0) from 2000 to 2019. A significant decreasing trend was observed in women aged 50‐59 years in the early period, from 1985 to 1992 (APC −2.8 [−4.3, −1.2]) but a significant increase was also seen in this age group after 1992. The APCs were +2.4% (1.1, 3.6) from 1992 to 2001, and +0.8 (0.5, 1.1) from 2001 to 2019.
FIGURE 4.
Annual trends in modelled mortality rate in cervical cancer (1985‐2019) by age group. Data from Japanese national vital statistics
TABLE 2.
Results of Joinpoint regression analysis on the trends in cervical cancer mortality by age group: Data from viral statistics (1985‐2019)
| Age (y) | Number of joinpoints | Line segment | Annual % change | 95% confidence interval | ||
|---|---|---|---|---|---|---|
| Start | End | Lower | Upper | |||
| 20‐59 | ||||||
| Crude | 2 | 1985 | 1993 | 0.1 | −1.4 | 1.6 |
| 1993 | 2000 | 4.4 a | 2.2 | 6.7 | ||
| 2000 | 2019 | 1.3 a | 0.9 | 1.6 | ||
| ASR | 2 | 1985 | 1991 | −1.1 | −3.5 | 1.5 |
| 1991 | 2002 | 3.5 a | 2.4 | 4.6 | ||
| 2002 | 2019 | 0.8 a | 0.3 | 1.2 | ||
| 20‐29 | 1 | 1985 | 2006 | 4.2 a | 2.4 | 6.1 |
| 2006 | 2019 | −3.0 | −6.6 | 0.7 | ||
| 30‐39 | 1 | 1985 | 2000 | 5.4 a | 3.7 | 7.1 |
| 2000 | 2019 | 1.1 a | 0.1 | 2.0 | ||
| 40‐49 | 1 | 1985 | 2011 | 2.7 a | 2.3 | 3.2 |
| 2011 | 2019 | −1.0 | −3.2 | 1.3 | ||
| 50‐59 | 2 | 1985 | 1992 | −2.8 a | −4.3 | −1.2 |
| 1992 | 2001 | 2.4 a | 1.1 | 3.6 | ||
| 2001 | 2019 | 0.8 a | 0.5 | 1.1 | ||
Abbreviation: ASR, age standardized rate.
Annual % change statistically significantly different from zero (P < .05).
4. DISCUSSION
This study analyzed the trend in incidence and mortality of cervical cancer in young and middle‐aged women in Japan by 10‐year interval age‐groups. The incidence of cervical cancer significantly increased throughout the observation period for ages 20‐29, 30‐39, and 40‐49 years, and overall young and middle adults from ages 20 to 59 years. Similarly, mortality also showed significant rising trends in women aged 30‐39, 50‐59, and overall 20‐59 years. Our results revealed that more women in their young and middle adult stages of life are being diagnosed and are dying of cervical cancer. The incidence and mortality due to cervical cancer among women of all ages are both increasing in Japan, and is also predicted to grow in the absence of effective prevention and intervention strategies. 13 , 14 , 28 , 29 , 30 , 31 This paper highlighted the need for further cervical cancer prevention strategies for this age group in Japan.
Contrary to this study, the incidence of cervical cancer has been decreasing in other high‐resource countries. 2 , 3 , 4 This includes other East Asian countries whose success is considered to be the result of a combination of cervical cancer control measures, particularly organized cervical screening. 4 , 32 , 33 , 34 Cervical screening with a highly sensitive and precise test has been proven to reduce the incidence and mortality of cervical cancer by increasing early detection. 35 , 36 , 37 Countries with high screening rates have been effective in lowering the incidence and mortality due to cervical cancer. 4 , 32 In Japan, cytology screening was introduced in the late 1950s, and became systematized in 1982. 38 Although the nationwide screening coverage rate has increased over the past 10 years, from 37.7% in 2010 to 43.7% in 2019 among women aged 20‐69 years, this is still low compared to other countries such as the United States (72.6%), UK (74.4%), and Korea (51.9%). 10 , 39 Therefore, in Japan, although improvement is reported in cervical screening participation, it has not been reflected in the decrease of the incidence of cervical cancer cases to date.
Evidence from many countries, including Japan, has indicated the effectiveness of the HPV vaccine; a second‐generation nonavalent HPV vaccine provides direct protection against approximately 90% of cervical cancers globally. 2 , 6 , 15 , 31 , 40 In Japan, vaccination coverage has remained below 1%. 41 This is a result of the suspension of proactive recommendation for the national immunization program for girls aged 12‐16 years due to reports in 2013 of potential adverse events following immunization. 42 It was estimated that a delay in the resumption of vaccination would likely result in as many as an additional 27,300 cases and 5,700 deaths in the near future, the impact of which has also been projected at municipal and national levels in Japan. 29 , 31 , 43 Global estimates show decreases in incidence and mortality in proportion to increasing screening and vaccination rates. 37 , 44 , 45 In 2021, after 8 years of intermission, the government of Japan has decided to end the state of withholding active recommendation for routine HPV vaccination, after confirming the safety, and strengthening the support system for the vaccine. 12 In continuation, to follow the success of long‐term reduction of cervical cancer burden in many other countries, Japan needs to increase cervical screening participation and promote coverage of the HPV vaccination program. 31 , 42
4.1. Strengths and limitations
The representativeness of the data is a major strength of this study. Incidence data were derived from three prefectures with long‐term high‐quality data, and mortality data were from a complete mandatory reporting system, based on the national vital statistics. Although incidence data were not obtained from all prefectures, past reports have confirmed its validity in terms of secular trends. 19 In addition, the data used for past reports published on cervical cancer trends in Japan are mainly based on a single city or prefecture, which also makes our population‐based study more precise. 28 , 29 , 30 , 46
Previous reports on the trends in Japanese cervical cancer mortality should be interpreted with caution because the vital statistics registry could have included the shift from cancer of the uterus, NOS. 14 However, the proportion of NOS had been stable since the late 1990s. 14 Our study limited the year range from 1985 to make the result more comparable with the incidence analysis. Therefore, it can be assumed that this will not significantly affect the results of our analysis. The age range for this study was also limited to 20 to 59 years, to explore the situation of cervical cancer in young and middle adults in Japan. Additional analyses for women aged 60 years and older are shown in the Tables S2 and S3 and Figures [Link], [Link], [Link], [Link]; where incidence rates showed decreasing or insignificant trends among these age groups. For mortality, significant increase was seen in the 60‐69 years age group. Furthermore, our analysis was only descriptive. It was also not grouped into clinically relevant subtypes, but previous reports have shown that incidence and relative survival of women did not differ between HPV‐related subtypes. 6 , 36
In summary, by examining trends of cervical cancer incidence and mortality in young and middle adults in 10‐year interval age‐groups, we observed increasing trends in incidence and mortality of cervical cancer in young and middle adults in Japan. This study revealed that current cervical cancer control strategies in Japan have not been effective in reducing the incidence and mortality due to cervical cancer in young and middle adults. Increasing participation in cervical cancer screening and implementation of a national vaccination program are urgently needed to reduce the incidence and mortality due to cervical cancer in Japan.
ACKNOWLEDGEMENTS
None.
DISCLOSURE
There are no financial or other relations that could lead to a conflict of interest regarding this study.
Supporting information
Fig S1
Fig S2
Fig S3
Fig S4
Fig S5
Fig S6
Table S1
Table S2
Table S3
Tanaka S, Palmer M, Katanoda K. Trends in cervical cancer incidence and mortality of young and middle adults in Japan. Cancer Sci. 2022;113:1801–1807. doi: 10.1111/cas.15320
REFERENCES
- 1. Sung H, Ferlay J, Siegel RL, et al. Global cancer statistics 2020: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA: Cancer J Clin. 2021;71(3):209‐249. [DOI] [PubMed] [Google Scholar]
- 2. Melnikow J, Henderson JT, Burda BU, et al. Screening for cervical cancer with high‐risk human papillomavirus testing. JAMA. 2018;320(7):687. [DOI] [PubMed] [Google Scholar]
- 3. Shim S‐H, Kim H, Sohn I‐S, et al. Nationwide cervical cancer screening in Korea: data from the national health insurance service cancer screening program and national cancer screening program, 2009–2014. J Gynecol Oncol. 2017;28(5):2009‐2014. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Vaccarella S, Franceschi S, Zaridze D, et al. Preventable fractions of cervical cancer via effective screening in six Baltic, central, and eastern European countries 2017–40: a population‐based study. Lancet Oncol. 2016;17(10):1445‐1452. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Brisson M, Kim JJ, Canfell K, et al. Impact of HPV vaccination and cervical screening on cervical cancer elimination: a comparative modelling analysis in 78 low‐income and lower‐middle‐income countries. Lancet. 2020;395(10224):575‐590. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6. Guo F, Cofie LE, Berenson AB. Cervical cancer incidence in young U.S. females after human papillomavirus vaccine introduction. Am J Prev Med. 2018;55(2):197‐204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7. Lei J, Ploner A, Elfström KM, et al. HPV vaccination and the risk of invasive cervical cancer. N Engl J Med. 2020;383(14):1340‐1348. [DOI] [PubMed] [Google Scholar]
- 8. Iwasaka T. History and current situations of cervical cancer screening. Clin Gynecol Obstets. 2009;63(9):1117‐1121. [Google Scholar]
- 9. Aoki ES, Yin R, Li K, et al. National screening programs for cervical cancer in Asian countries. J Gynecol Oncol. 2020;31(3):e55. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10. OECD Health Statistics . Health care utilisation: screening [Internet]. 2019. https://stats.oecd.org/Index.aspx?QueryId=30159. Accessed August 11, 2021.
- 11. Sekine M, Kudo R, Yamaguchi M, et al. Japan’s ongoing crisis on HPV vaccination. Vaccines. 2020;8(3):362. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12. Subcomittee of Vaccination, Side Effect Review Subcomittee, Ministry of Health Labour and Welfare . 72nd counsil for health sciences [Minutes]. 2021. https://www.mhlw.go.jp/stf/newpage_22253.html. Accessed December 26, 2021.
- 13. Utada M, Chernyavskiy P, Lee WJ, et al. Increasing risk of uterine cervical cancer among young Japanese women: comparison of incidence trends in Japan, South Korea and Japanese‐Americans between 1985 and 2012. Int J Cancer. 2019;144(9):2144‐2152. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14. Katanoda K, Hori M, Saito E, et al. Updated trends in cancer in Japan: incidence in 1985–2015 and mortality in 1958–2018—a sign of decrease in cancer incidence. J Epidemiol. 2021;31(7):426‐450. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Luostarinen T, Apter D, Dillner J, et al. Vaccination protects against invasive HPV‐associated cancers. Int J Cancer Res. 2018;142(10):2186‐2187. [DOI] [PubMed] [Google Scholar]
- 16. Matsuura Y, Yoshioka M, Nakata A, et al. Trends in uterine cervical cancer screening at physical health checkups for company employees in Japan. J Uoeh. 2019;41(3):327‐333. [DOI] [PubMed] [Google Scholar]
- 17. Center for Cancer Control and Information Services, National Cancer Center . Population files for population‐based cancer registry [internet]. 2020. https://ganjoho.jp/reg_stat/statistics/dl/statistics_p05.html. Accessed April 21, 2021.
- 18. Hori M, Matsuda T, Shibata A, et al. Cancer incidence and incidence rates in Japan in 2009: a study of 32 population‐based cancer registries for the monitoring of cancer incidence in Japan (MCIJ) project. Jpn J Clin Oncol. 2015;45(9):884‐891. [DOI] [PubMed] [Google Scholar]
- 19. Katanoda K, Ajiki W, Matsuda T, et al. Trend analysis of cancer incidence in Japan using data from selected population‐based cancer registries. Cancer Sci. 2012;103(2):360‐368. [DOI] [PubMed] [Google Scholar]
- 20. Matsuda T, Sobue T. Recent trends in population‐based cancer registries in Japan: the act on promotion of cancer registries and drastic changes in the historical registry. Int J Clin Oncol. 2015;20(1):11‐20. [DOI] [PubMed] [Google Scholar]
- 21. Katanoda K, Hori M, Matsuda T, et al. An updated report on the trends in cancer incidence and mortality in Japan, 1958–2013. Jpn J Clin Oncol. 2015;45(4):390‐401. [DOI] [PubMed] [Google Scholar]
- 22. Cancer Information Service. National Cancer Canter, Japan . Cancer registry and statistics [Internet]. https://ganjoho.jp/reg_stat/statistics/dl/index.html. Accessed April 13th, 2021.
- 23. World Health Organization . International statistical classification of diseases and related health problems, 10th revision (ICD‐10). 1992.
- 24. Sasagawa T, Maehama T, Ideta K, et al. Population‐based study for human papillomavirus (HPV) infection in young women in Japan: a multicenter study by the Japanese human papillomavirus disease education research survey group (J‐HERS). J Med Virol. 2016;88(2):324‐335. [DOI] [PubMed] [Google Scholar]
- 25. Bruni L, Diaz M, Castellsagué X, et al. Cervical human papillomavirus prevalence in 5 continents: meta‐analysis of 1 million women with normal cytological findings. J Infect. 2010;202(12):1789‐1799. [DOI] [PubMed] [Google Scholar]
- 26. Torres‐Poveda K, Ruiz‐Fraga I, Madrid‐Marina V, et al. High risk HPV infection prevalence and associated cofactors: a population‐based study in female ISSSTE beneficiaries attending the HPV screening and early detection of cervical cancer program. BMC Cancer. 2019;19(1):1205. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 27. Kim HJ, Fay MP, Feuer EJ, et al. Permutation tests for joinpoint regression with applications to cancer rates. Stat Med. 2000;19(3):335‐351. [DOI] [PubMed] [Google Scholar]
- 28. Yagi A, Ueda Y, Egawa‐Takata T, et al. Realistic fear of cervical cancer risk in Japan depending on birth year. Hum Vaccin Immunother. 2017;13(7):1700‐1704. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29. Yagi A, Ueda Y, Ikeda S, et al. Evaluation of future cervical cancer risk in Japan, based on birth year. Vaccine. 2019;37(22):2889‐2891. [DOI] [PubMed] [Google Scholar]
- 30. Yagi A, Ueda Y, Nakagawa S, et al. Potential for cervical cancer incidence and death resulting from Japan’s current policy of prolonged suspension of its governmental recommendation of the HPV vaccine. Sci Rep. 2020;10(1):15945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31. Simms KT, Hanley SJB, Smith MA, et al. Impact of HPV vaccine hesitancy on cervical cancer in Japan: a modelling study. Lancet Public Health. 2020;5(4):e223‐e234. [DOI] [PubMed] [Google Scholar]
- 32. Landy R, Sasieni PD, Mathews C, et al. Impact of screening on cervical cancer incidence: a population‐based case–control study in the United States. Int J Cancer. 2020;147(3):887‐896. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33. Lee JH, Kim H, Choi H, et al. Contributions and limitations of national cervical cancer screening program in Korea: a retrospective observational study. Asian Nurs Res. 2018;12(1):9‐16. [DOI] [PubMed] [Google Scholar]
- 34. Katanoda K, Ito Y, Sobue T. International comparison of trends in cancer mortality: Japan has fallen behind in screening‐related cancers. Jpn J Clin Oncol. 2021;51(11):1680‐1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35. Curry SJ, Krist AH, Owens DK, et al. Screening for cervical cancer: US preventive services task force recommendation statement. JAMA. 2018;320(7):674‐686. [DOI] [PubMed] [Google Scholar]
- 36. Andrae B, Andersson TML, Lambert PC, et al. Screening and cervical cancer cure: population based cohort study. BMJ. 2012;344:e900‐e900. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37. Smith M, Canfell K. Impact of the Australian national cervical screening program in women of different ages. Med J Aust. 2016;205(8):359‐364. [DOI] [PubMed] [Google Scholar]
- 38. Mori T. Advances in uterine cervical cancer screening. J Kyoto Pref Univ Med. 2014;123(5):309‐318. [in Japanese] [Google Scholar]
- 39. Cancer Information Service, National Cancer Center, Japan . Cancer registry and statistics.2007‐2019. https://ganjoho.jp/reg_stat/statistics/stat/screening/dl_screening.html. Accessed October 7, 2021.
- 40. Konno R, Yoshikawa H, Okutani M, et al. Efficacy of the human papillomavirus (HPV)‐16/18 AS04‐adjuvanted vaccine against cervical intraepithelial neoplasia and cervical infection in young Japanese women. Hum Vaccin Immunother. 2014;10(7):1781‐1794. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 41. Japanese Ministry of Health Labour and Welfare . The 23rd meeting of the vaccines adverse reactions. Review committee. 2016. https://www.mhlw.go.jp/file/05‐Shingikai‐10601000‐Daijinkanboukouseikagakuka‐Kouseikagakuka/0000147016.pdf. Accessed July 27, 2021.
- 42. Hanley SJB, Yoshioka E, Ito Y, et al. HPV vaccination crisis in Japan. Lancet. 2015;385(9987):2571. [DOI] [PubMed] [Google Scholar]
- 43. Yagi A, Ueda Y, Nakagawa S, et al. A nationwide birth year‐by‐year analysis of effectiveness of HPV vaccine in Japan. Cancer Sci. 2021;112(9):3691‐3698. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 44. Vaccarella S, Lortet‐Tieulent J, Plummer M, et al. Worldwide trends in cervical cancer incidence: impact of screening against changes in disease risk factors. Eur J Cancer. 2013;49(15):3262‐3273. [DOI] [PubMed] [Google Scholar]
- 45. Simms KT, Steinberg J, Caruana M, et al. Impact of scaled up human papillomavirus vaccination and cervical screening and the potential for global elimination of cervical cancer in 181 countries, 2020–99: a modelling study. Lancet Oncol. 2019;20(3):394‐407. [DOI] [PubMed] [Google Scholar]
- 46. Noguchi T, Zaitsu M, Oki I, et al. Recent increasing incidence of early‐stage cervical cancers of the squamous cell carcinoma subtype among young women. Int J Environ Res Public Health. 2020;17(20):7401. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Fig S1
Fig S2
Fig S3
Fig S4
Fig S5
Fig S6
Table S1
Table S2
Table S3


