Abstract
U.S. national and state population-based estimates of adults living with autism spectrum disorder (ASD) are nonexistent due to the lack of existing surveillance systems funded to address this need. Therefore, we estimated national and state prevalence of adults 18–84 years living with ASD using simulation in conjunction with Bayesian hierarchal models. In 2017, we estimated that approximately 2.21% (95% simulation interval (SI) 1.95%, 2.45%) or 5,437,988 U.S. adults aged 18 and older have ASD, with state prevalence ranging from 1.97% (95% SI 1.55%, 2.45%) in Louisiana to 2.42% (95% SI 1.93%, 2.99%) in Massachusetts. Prevalence and case estimates of adults living with ASD (diagnosed and undiagnosed) can help states estimate the need for diagnosing and providing services to those unidentified.
Keywords: Autism spectrum disorder, Developmental disabilities, Intellectual disability, Prevalence estimates, Modeling
Introduction
In the U.S. approximately 1.5 million children ages 3–17 years have been diagnosed with Autisms Spectrum Disorder (ASD), a developmental disability characterized by deficits in social communication and interaction, as well as restricted, repetitive behaviors (Kogan et al. 2018; American Psychiatric Association 2013). Prevalence estimates for adults are unknown due to a lack of existing surveillance systems to monitor the prevalence. ASD is a life-long disability that can require intensive support throughout life for some but not all with the condition (Roux et al. 2015; Croen et al 2015; Nicolaidis et al. 2014; Murphy et al. 2016). Based on data from 11 surveillance sites, 1.67% of 8-year-old children have ASD (Baio et al. 2018). As children with diagnosed ASD mature into adolescence and early adulthood, parents, service providers, and policy makers can support them by ensuring necessary services for adults with ASD are available to meet the demand.
National and state-based estimates of adults living with ASD could inform planning for programs and services; however, no U.S. estimates currently exist. Without data on ASD in adults, estimates of ASD prevalence among adults can be derived from applying existing data to models. Modeling of estimates has been done for national prevalence of congenital heart disease (Gilboa et al. 2016) and state-based prevalence of hepatitis C virus (Rosenberg et al. 2018). We estimated national and state prevalence of adults living with ASD using existing state-based data for children and adjusting for higher mortality rates among persons with ASD.
Methods
We used unpublished ASD prevalence data from NSCH (2016–2018), published ASD population mortality rates, 1999–2017 U.S. mortality rates by state, age, and sex, and 2017 population to develop an estimator of ASD prevalence and cases by state and sex, and nationally for 2017. For the unpublished ASD prevalence data, we calculated ASD prevalence for the age group 3–17 years, consistent with NSCH reports (Kogan et al 2018). In that study the age group 3–5 years had a prevalence of 1.97%, (95% CI 1.41–2.74) compared with 2.61 (95% CI 2.15–3.15) for ages 6–11 years and 2.65 (95% CI 2.27–3.10) for ages 12–17. A sensitivity analysis was run using data for ages 6–17 years to assess the effect of the choice of age group on the estimated number of adults with ASD.
Our estimator of the prevalence and cases of ASD for the ith state, jth age (year), and kth sex used the following equations and begins with the ages 3–17 prevalence estimate (see Supplemental material for derivation).
| (1) |
| (2) |
where γadj is the number of ASD cases adjusted for the survival ratio of the ASD to population, N is the population, ρ is the ASD prevalence, survival rates for the adults with ASD and population are defined by S, and ρadj is the adjusted state, sex, and age (> 17) ASD prevalence rate. National and state estimates are obtained by summing over all ASD cases for ages 18–84 and then calculating the national and state ASD prevalence estimates. Estimates went up to age 84, reflecting the availability of general population mortality data. Our ASD prevalence estimator assumes that given the age 3–17 prevalence estimate, the prevalence decreases over time as a function of the ASD-to-population survival ratio.
Inputs into the models (Eqs. 1, 2) are presented in Table 1. Inputs assumed to be known are the population and mortality rates whereas the ages 3–17 prevalence and survival ratio are estimated. Using simulation, we incorporate the uncertainty of the ages 3–17 prevalence and survival ratio estimates into the model. Our inputs include 2016–18 state-based ASD numbers by sex for children ages 3–17 years from the National Survey of Children’s Health (NSCH). NSCH is an annual, cross-sectional, complex design, address-based survey that collects information on the health and well-being of children ages 0–17 years using both web-based and paper and pencil methodologies. Children whose parents responded “yes” on two ASD questions were inCIuded: (1) “Has a doctor or other health care provider ever told you that your child has Autism or Autism Spectrum Disorder? Include diagnoses of Asperger’s Disorder or Pervasive Developmental Disorder (PDD)”; (2) “If yes, does this child currently have the condition?” We used a two-step process to estimate the ages 3–17 ASD prevalence by state and sex. First, we used the NSCH ages 3–17 data and study design weights to estimate the logistic regression model regression coefficients and standard errors (SE) by state and sex. Our second stage used the NSCH logistic regression coefficients and SE in a Bayesian hierarchical meta-analysis model to estimate the partially pooled effects for each state and sex. Partial pooling assumes each state and sex has a different prevalence, but the data for all states and sex informs the prevalence estimate of each state and sex. We used partial pooling to reduce the influence of outliers and estimates from states with small numbers of observations, resulting in more statistically robust estimates (Gelman 2013). The 2017 state populations, by sex, were obtained from the National Center for Health Statistics (US DHHS 2018a, b). We estimated ASD prevalence separately for males and females as males are known to have higher rates of ASD diagnoses than females (Kogan et al. 2018; Baio et al. 2018).
Table 1.
Data inputs used to estimate ASD prevalence among adults 18–84 years by state and sex
| Input | Data source for estimates | Link |
|---|---|---|
| 2016–2018 estimated state prevalence of male and female children ages 3–17 years with diagnosed ASD reported by a parent | National survey of children’s health, 2016–2018 | https://mchb.hrsa.gov/data/national-surveys/questionnaires-datasets-supporting-documents |
| A meta-analysis of mortality studies used to estimate male and female mortality rates among persons with diagnosed ASD |
Picket et al. (2006) All ages included among those receiving services in the California Department of Developmental Services 1/83–12/1997, 1/1998–12/2002 with autism diagnoses and died during the study time period. Comparison group adjusted for age |
PMID: 16565885 |
| Mouridsen et al. (2008) | PMID: 18,579,647 | |
| ASD was a clinical cohort, average age 43 years. Comparison group adjusted for age |
https://doi.org/10.1177/1362361308091653 | |
| Gillberg et al. (2010) | PMID: 19838782 | |
| Population-based group of persons with ASD followed up to average age of 33 years. Comparison group adjusted for age | https://doi.org/10.1007/s10803-009-0883-4 | |
| Hirvikoski et al. (2016) | PMID: 26541693 | |
| All ages included: median age of death for persons with ASD = 55 years, control population = 70 years | https://doi.org/10.1192/bjp.bp.114.160192 | |
| 2017 estimate of the state populations by sex | United States Department of Health and Human Services, Centers for Disease Control and Prevention, National Center for Health Statistics, Bridged-Race Population Estimates, United States, postcensal population estimates, released by NCHS on 6/27/2018 | https://wonder.cdc.gov/bridged-race-v2017.html |
| 1999–2017 state mortality rates | Multiple Cause of Death Files, 1999–2017, as compiled from data provided by the 57 vital statistics jurisdictions through the Vital Statistics Cooperative Program | https://wonder.cdc.gov/ucd-icd10.html |
Standardized mortality ratio (SMR) is a relative measure of excess mortality for one group compared to the general population. The SMR by sex was estimated using a meta-analysis method based on five studies (Supplement Table 1). We used a Bayesian hierarchical Poisson model with the observed mortality as the outcome and the expected mortality as the offset (Supplemental Methods) to estimate the partially pooled overall SMR by sex. We assumed that the SMR was the same across states because we had no information on state-specific mortality rates. We also assumed the SMR did not change across age groups, although the majority of the mortality studies followed persons with ASD only through middle age.
We used simulation to estimate the 2017 national and state prevalence and 95% simulation interval (SI) of men and women ages 18–84 living with ASD. First, we obtained the mortality rate by state and sex for ages 3–17, and 18–84 by year and strata (state, sex, and age). Second, we obtained the U.S. 2017 population data by state, sex, and age. Next, we estimated ages 3–17 meta-analysis prevalence and associated SE by state and sex and randomly drew 10,000 samples from a normal distribution using our estimated mean and SE meta-analysis estimates by sex for the SMRs (see Supplemental Table 1). Next, we randomly drew 10,000 prevalence samples using our meta-analysis estimates by state and sex. Lastly, we estimate the prevalence and ASD cases by state, sex, and age using Eqs. 1 and 2. Our simulation resulted in 10,000 estimates for the prevalence and ASD cases for age Class 18–84 by state and sex, and we summarize these results using the mean and 95% SI.
The male-to-female ASD prevalence ratio (PR) was calculated by state for each simulation and then summarized for all 10,000 simulations with the mean and 95% SI (see Supplement Fig. 1).
Results
In 2017, we estimated that 2.21% (95% SI 1.95%, 2.45%) or 5,437,988 (95% SI 4,798,561; 6,025,184) U.S. adults aged 18–84 years were living with ASD. State prevalence estimates ranged from 1.97% (95% SI 1.55%, 2.45%) in Louisiana to 2.42% (95% SI 1.93%, 2.99%) in Massachusetts (Table 2). The states with the greatest number of adults estimated to be living with ASD Included California (701,669 cases), Texas (449,631), New York (342,280) and Florida (329,131). No obvious geographic pattern for prevalence was found (Fig. 1).
Table 2.
State estimated autism spectrum disorder prevalence among adults ages 18–84 years, cases, and associated 95% simulation interval
| State | Cases | 95% SI | Prevalence | 95% SI |
|---|---|---|---|---|
| Alabama | 78,072 | 61,527, 96,435 | 2.12 | 1.67, 2.61 |
| Alaska | 12,000 | 9559, 14,849 | 2.19 | 1.74, 2.71 |
| Arizona | 119,924 | 95,618, 147,485 | 2.29 | 1.82, 2.81 |
| Arkansas | 45,569 | 35,644, 56,735 | 2.03 | 1.59, 2.53 |
| California | 701,669 | 563,358, 863,471 | 2.36 | 1.89, 2.90 |
| Colorado | 96,917 | 78,736, 117,790 | 2.28 | 1.85, 2.77 |
| Connecticut | 65,337 | 51,985, 81,354 | 2.37 | 1.89, 2.96 |
| Delaware | 16,683 | 13,191, 20,742 | 2.26 | 1.79, 2.81 |
| District of Columbia | 11,700 | 9281, 14,425 | 2.10 | 1.67, 2.59 |
| Florida | 329,131 | 259,573, 407,473 | 2.03 | 1.60, 2.51 |
| Georgia | 174,612 | 139,616, 213,983 | 2.25 | 1.80, 2.75 |
| Hawaii | 22,797 | 18,103, 28,324 | 2.11 | 1.67, 2.62 |
| Idaho | 27,094 | 21,741, 33,212 | 2.18 | 1.75, 2.67 |
| Illinois | 223,353 | 178,832, 274,414 | 2.32 | 1.86, 2.85 |
| Indiana | 111,067 | 88,717, 136,349 | 2.24 | 1.79, 2.75 |
| Iowa | 53,243 | 43,024, 64,598 | 2.28 | 1.84, 2.77 |
| Kansas | 46,863 | 37,387, 57,849 | 2.19 | 1.75, 2.71 |
| Kentucky | 71,791 | 56,959, 88,657 | 2.13 | 1.69, 2.64 |
| Louisiana | 68,819 | 54,071, 85,662 | 1.97 | 1.55, 2.45 |
| Maine | 23,910 | 19,244, 29,167 | 2.28 | 1.83, 2.78 |
| Maryland | 98,200 | 78,844, 118,940 | 2.14 | 1.72, 2.59 |
| Massachusetts | 129,168 | 103,105, 159,372 | 2.42 | 1.93, 2.99 |
| Michigan | 164,360 | 130,831, 201,349 | 2.17 | 1.73, 2.66 |
| Minnesota | 97,881 | 80,695, 117,401 | 2.35 | 1.94, 2.82 |
| Mississippi | 45,911 | 35,708, 57,883 | 2.07 | 1.61, 2.61 |
| Missouri | 97,377 | 77,500, 119,708 | 2.12 | 1.68, 2.60 |
| Montana | 16,969 | 13,404, 21,053 | 2.12 | 1.68, 2.63 |
| Nebraska | 31,417 | 25,045, 38,775 | 2.24 | 1.79, 2.77 |
| Nevada | 51,799 | 41,333, 63,725 | 2.28 | 1.82, 2.81 |
| New Hampshire | 23,442 | 19,085, 28,268 | 2.22 | 1.81, 2.68 |
| New Jersey | 157,245 | 127,036, 191,192 | 2.30 | 1.86, 2.80 |
| New Mexico | 31,207 | 24,166, 39,369 | 2.00 | 1.55, 2.52 |
| New York | 342,280 | 276,658, 417,725 | 2.25 | 1.82, 2.74 |
| North Carolina | 155,953 | 123,603, 192,285 | 2.00 | 1.59, 2.47 |
| North Dakota | 11,501 | 8967, 14,435 | 2.05 | 1.60, 2.57 |
| Ohio | 185,315 | 145,971, 228,939 | 2.11 | 1.66, 2.60 |
| Oklahoma | 61,672 | 49,304, 75,780 | 2.13 | 1.70, 2.61 |
| Oregon | 72,727 | 58,308, 89,294 | 2.28 | 1.83, 2.80 |
| Pennsylvania | 228,572 | 180,929, 284,166 | 2.33 | 1.85, 2.90 |
| Rhode Island | 18,472 | 15,116, 22,343 | 2.24 | 1.83, 2.71 |
| South Carolina | 75,985 | 58,887, 95,248 | 1.98 | 1.54, 2.48 |
| South Dakota | 12,830 | 9881, 16,286 | 2.02 | 1.56, 2.57 |
| Tennessee | 106,083 | 84,068, 131,132 | 2.08 | 1.65, 2.58 |
| Texas | 449,631 | 358,411, 556,627 | 2.19 | 1.74, 2.71 |
| Utah | 48,818 | 40,003, 58,452 | 2.28 | 1.87, 2.73 |
| Vermont | 10,435 | 8367, 12,764 | 2.12 | 1.70, 2.59 |
| Virginia | 155,557 | 125,110, 189,742 | 2.41 | 1.94, 2.94 |
| Washington | 119,815 | 95,514, 149,233 | 2.13 | 1.70, 2.65 |
| West Virginia | 29,083 | 22,748, 36,322 | 2.07 | 1.62, 2.58 |
| Wisconsin | 97,977 | 78,734, 119,841 | 2.23 | 1.80, 2.73 |
| Wyoming | 9758 | 7755, 12,036 | 2.26 | 1.79, 2.78 |
| Total | 5,437,988 | 4,798,561, 6,025,184 | 2.21 | 1.95, 2.45 |
Fig. 1.
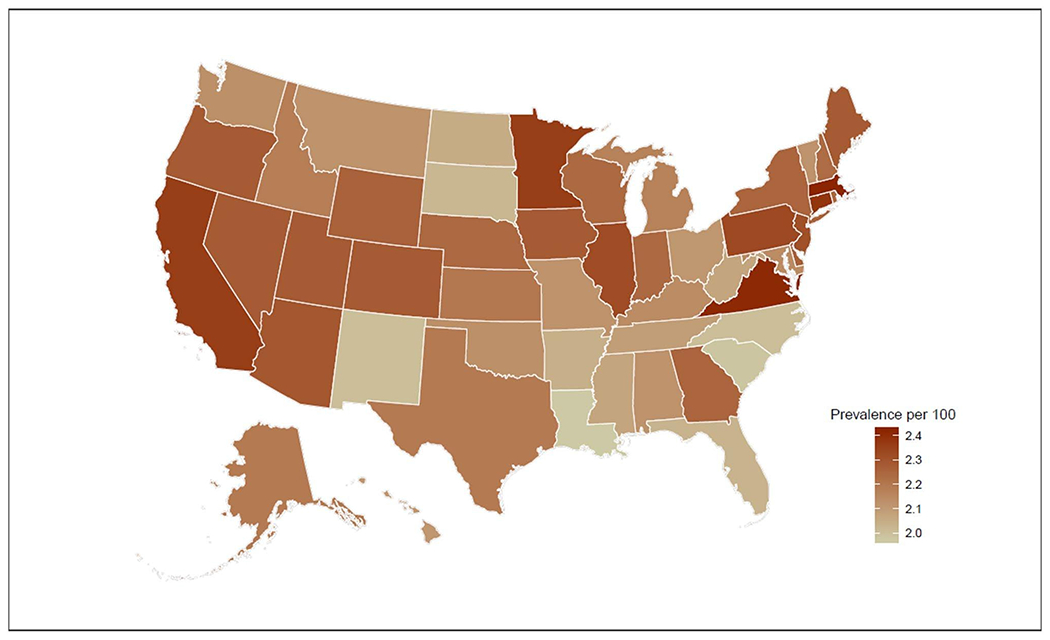
Estimated autism spectrum disorder prevalence among adults 18–84 years by state, 2017
The estimated U.S. ASD prevalence for females was 0.86% (95% SI 0.60, 1.09), and by state ranged from 0.72% (95% SI 0.41, 1.11) in Arkansas to 0.97% (95% SI 0.50, 1.45) in Virginia (Table 3, Fig. 2). The estimated U.S. ASD prevalence among adult males was higher than females, at 3.62%, (95% SI 3.14, 4.04), and state estimates ranged from 3.17% (95% SI 2.33, 4.19) in South Dakota to 4.01% (95% SI 3.07, 5.14) in Massachusetts (Table 4, Fig. 2). State PRs for males versus females estimates ranged from 3.94 (95% SI 2.29, 6.48) in South Dakota to 5.08 (95% SI 2.84, 8.78) in Arkansas (see Supplemental Table 2). The male-to-female prevalence difference ranged from 2.32% points (95% SI 1.40, 3.39) for South Dakota to 3.16% points (95% SI 2.16, 4.35) for Connecticut (see Supplemental Table 2).
Table 3.
Estimated autism spectrum disorder prevalence among females ages 18–84 years, cases, and associated 95% simulation interval
| State | Cases | 95% SI | Prevalence | 95% SI |
|---|---|---|---|---|
| Alabama | 15,072 | 8617, 22,982 | 0.79 | 0.45, 1.20 |
| Alaska | 2275 | 1399, 3291 | 0.88 | 0.54, 1.27 |
| Arizona | 22,274 | 13,559, 32,654 | 0.84 | 0.51, 1.23 |
| Arkansas | 8230 | 4690, 12,697 | 0.72 | 0.41, 1.11 |
| California | 137,645 | 89,272, 195,797 | 0.92 | 0.60, 1.31 |
| Colorado | 19,454 | 12,731, 27,303 | 0.92 | 0.60, 1.29 |
| Connecticut | 11,799 | 7494, 16,905 | 0.84 | 0.53, 1.20 |
| Delaware | 3212 | 1887, 4743 | 0.84 | 0.49, 1.24 |
| District of Columbia | 2470 | 1570, 3634 | 0.84 | 0.53, 1.23 |
| Florida | 69,038 | 40,683, 101,477 | 0.83 | 0.49, 1.22 |
| Georgia | 35,043 | 21,353, 51,568 | 0.87 | 0.53, 1.28 |
| Hawaii | 4592 | 2864, 6629 | 0.86 | 0.53, 1.24 |
| Idaho | 5241 | 3278, 7601 | 0.84 | 0.53, 1.22 |
| Illinois | 44,364 | 28,116, 63,603 | 0.90 | 0.57, 1.29 |
| Indiana | 22,492 | 13,811, 32,950 | 0.89 | 0.55, 1.30 |
| Iowa | 9822 | 6255, 14,075 | 0.84 | 0.53, 1.20 |
| Kansas | 8848 | 5478, 12,832 | 0.83 | 0.51, 1.20 |
| Kentucky | 13,109 | 7528, 19,922 | 0.77 | 0.44, 1.16 |
| Louisiana | 13,979 | 8248, 21,019 | 0.78 | 0.46, 1.17 |
| Maine | 4685 | 2909, 6775 | 0.87 | 0.54, 1.26 |
| Maryland | 21,097 | 12,870, 31,034 | 0.89 | 0.54, 1.30 |
| Massachusetts | 25,678 | 16,523, 37,094 | 0.93 | 0.60, 1.35 |
| Michigan | 32,847 | 19,687, 49,002 | 0.85 | 0.51, 1.27 |
| Minnesota | 19,328 | 12,650, 27,220 | 0.93 | 0.61, 1.30 |
| Mississippi | 8842 | 4986, 13,560 | 0.77 | 0.43, 1.18 |
| Missouri | 19,177 | 11,751, 28,060 | 0.82 | 0.50, 1.19 |
| Montana | 3430 | 1984, 5146 | 0.87 | 0.50, 1.30 |
| Nebraska | 5774 | 3615, 8476 | 0.82 | 0.52, 1.21 |
| Nevada | 9863 | 6058, 14,443 | 0.87 | 0.53, 1.27 |
| New Hampshire | 4722 | 2960, 6732 | 0.89 | 0.56, 1.27 |
| New Jersey | 30,829 | 19,381, 44,681 | 0.88 | 0.55, 1.27 |
| New Mexico | 6215 | 3548, 9505 | 0.79 | 0.45, 1.20 |
| New York | 72,438 | 46,913, 103,195 | 0.92 | 0.60, 1.31 |
| North Carolina | 33,070 | 20,403, 47,816 | 0.82 | 0.51, 1.19 |
| North Dakota | 2129 | 1308, 3177 | 0.79 | 0.48, 1.18 |
| Ohio | 37,205 | 22,486, 54,560 | 0.83 | 0.50, 1.21 |
| Oklahoma | 11,752 | 7023, 17,555 | 0.80 | 0.48, 1.20 |
| Oregon | 13,170 | 8255, 19,271 | 0.82 | 0.51, 1.20 |
| Pennsylvania | 43,191 | 26,449, 62,380 | 0.86 | 0.53, 1.25 |
| Rhode Island | 3628 | 2333, 5220 | 0.85 | 0.55, 1.23 |
| South Carolina | 16,609 | 9750, 24,644 | 0.84 | 0.49, 1.24 |
| South Dakota | 2645 | 1620, 3885 | 0.85 | 0.52, 1.24 |
| Tennessee | 20,306 | 12,014, 30,315 | 0.77 | 0.46, 1.16 |
| Texas | 90,422 | 57,760, 129,614 | 0.87 | 0.56, 1.25 |
| Utah | 9968 | 6557, 13,971 | 0.93 | 0.61, 1.31 |
| Vermont | 2087 | 1293, 3040 | 0.84 | 0.52, 1.22 |
| Virginia | 32,011 | 19,580, 47,823 | 0.97 | 0.59, 1.45 |
| Washington | 22,146 | 13,537, 33,310 | 0.79 | 0.48, 1.18 |
| West Virginia | 5910 | 3328, 9096 | 0.83 | 0.47, 1.28 |
| Wisconsin | 18,244 | 11,342, 26,895 | 0.83 | 0.52, 1.22 |
| Wyoming | 1943 | 1157, 2893 | 0.92 | 0.55, 1.37 |
| Total | 1,080,322 | 752,142, 1,359,152 | 0.86 | 0.60, 1.09 |
Fig. 2.
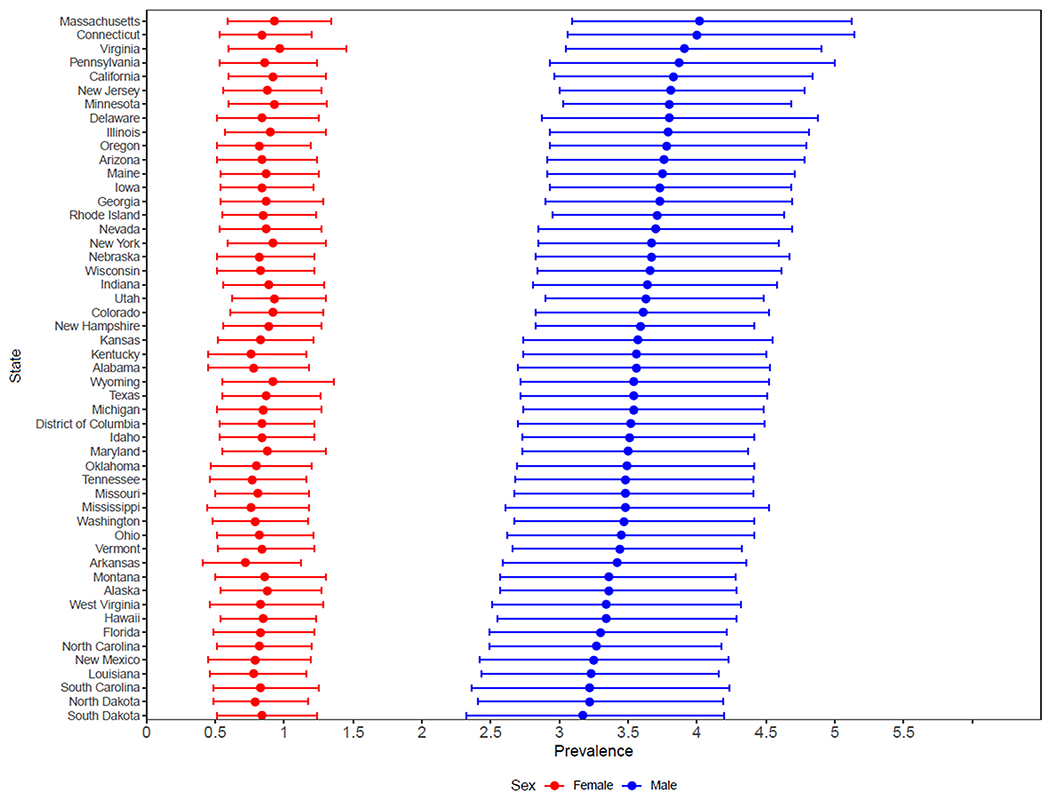
Estimated state autism spectrum disorder prevalence among adults 18–84 years by sex
Table 4.
Estimated autism spectrum disorder prevalence among males ages 18–84 years, cases, and associated 95% simulation interval
| State | Cases | 95% SI | Prevalence | 95% SI |
|---|---|---|---|---|
| Alabama | 63,000 | 48,122, 79,991 | 3.55 | 2.71, 4.51 |
| Alaska | 9725 | 7481, 12,391 | 3.36 | 2.59, 4.28 |
| Arizona | 97,650 | 75,258, 123,694 | 3.76 | 2.89, 4.76 |
| Arkansas | 37,339 | 28,428, 47,714 | 3.41 | 2.60, 4.36 |
| California | 564,024 | 436,565, 712,719 | 3.82 | 2.96, 4.83 |
| Colorado | 77,463 | 60,754, 96,994 | 3.61 | 2.83, 4.52 |
| Connecticut | 53,538 | 41,196, 69,048 | 3.99 | 3.07, 5.15 |
| Delaware | 13,471 | 10,262, 17,304 | 3.80 | 2.89, 4.88 |
| District of Columbia | 9230 | 7052, 11,767 | 3.52 | 2.69, 4.48 |
| Florida | 260,093 | 197,052, 333,489 | 3.30 | 2.50, 4.23 |
| Georgia | 139,569 | 107,666, 175,620 | 3.72 | 2.87, 4.69 |
| Hawaii | 18,205 | 13,855, 23,302 | 3.34 | 2.54, 4.28 |
| Idaho | 21,853 | 16,906, 27,494 | 3.51 | 2.71, 4.41 |
| Illinois | 178,988 | 138,499, 226,962 | 3.79 | 2.93, 4.80 |
| Indiana | 88,575 | 68,532, 111,810 | 3.63 | 2.81, 4.59 |
| Iowa | 43,421 | 33,901, 54,102 | 3.73 | 2.91, 4.65 |
| Kansas | 38,015 | 29,328, 48,321 | 3.57 | 2.75, 4.54 |
| Kentucky | 58,682 | 44,945, 74,249 | 3.56 | 2.72, 4.50 |
| Louisiana | 54,840 | 41,315, 70,670 | 3.23 | 2.43, 4.16 |
| Maine | 19,225 | 14,960, 24,183 | 3.75 | 2.91, 4.71 |
| Maryland | 77,103 | 60,286, 96,019 | 3.49 | 2.73, 4.35 |
| Massachusetts | 103,490 | 79,250, 132,425 | 4.01 | 3.07, 5.14 |
| Michigan | 131,513 | 101,753, 166,068 | 3.54 | 2.74, 4.47 |
| Minnesota | 78,554 | 62,673, 96,695 | 3.79 | 3.03, 4.67 |
| Mississippi | 37,069 | 27,818, 48,132 | 3.48 | 2.61, 4.52 |
| Missouri | 78,200 | 60,239, 98,988 | 3.48 | 2.68, 4.40 |
| Montana | 13,538 | 10,318, 17,252 | 3.36 | 2.56, 4.28 |
| Nebraska | 25,642 | 19,722, 32,701 | 3.67 | 2.82, 4.68 |
| Nevada | 41,935 | 32,438, 53,010 | 3.69 | 2.86, 4.67 |
| New Hampshire | 18,720 | 14,879, 23,148 | 3.58 | 2.85, 4.43 |
| New Jersey | 126,416 | 99,304, 158,245 | 3.81 | 2.99, 4.77 |
| New Mexico | 24,992 | 18,581, 32,421 | 3.25 | 2.41, 4.21 |
| New York | 269,842 | 210,546, 338,482 | 3.67 | 2.86, 4.60 |
| North Carolina | 122,883 | 93,683, 157,051 | 3.26 | 2.49, 4.17 |
| North Dakota | 9372 | 7026, 12,121 | 3.22 | 2.41, 4.16 |
| Ohio | 148,110 | 111,942, 188,693 | 3.45 | 2.61, 4.39 |
| Oklahoma | 49,920 | 38,731, 63,029 | 3.49 | 2.71, 4.40 |
| Oregon | 59,557 | 46,065, 75,500 | 3.78 | 2.92, 4.79 |
| Pennsylvania | 185,382 | 140,420, 238,656 | 3.87 | 2.93, 4.98 |
| Rhode Island | 14,844 | 11,772, 18,395 | 3.71 | 2.94, 4.60 |
| South Carolina | 59,376 | 43,786, 77,343 | 3.22 | 2.37, 4.19 |
| South Dakota | 10,185 | 7500, 13,455 | 3.17 | 2.33, 4.19 |
| Tennessee | 85,777 | 66,069, 108,994 | 3.48 | 2.68, 4.42 |
| Texas | 359,209 | 274,707, 459,695 | 3.53 | 2.70, 4.52 |
| Utah | 38,850 | 30,928, 47,667 | 3.63 | 2.89, 4.46 |
| Vermont | 8348 | 6457, 10,507 | 3.44 | 2.66, 4.32 |
| Virginia | 123,546 | 96,564, 154,991 | 3.91 | 3.05, 4.90 |
| Washington | 97,669 | 75,180, 125,363 | 3.47 | 2.67, 4.45 |
| West Virginia | 23,173 | 17,458, 29,832 | 3.33 | 2.51, 4.29 |
| Wisconsin | 79,733 | 62,161, 99,939 | 3.65 | 2.85, 4.58 |
| Wyoming | 7815 | 6017, 9936 | 3.53 | 2.72, 4.49 |
| Total | 4,357,667 | 3,788,037, 4,867,213 | 3.62 | 3.14, 4.04 |
We conducted a sensitivity analysis to assess the estimated number of adults with ASD using the ASD estimated prevalence for the age group 6–17 years in the model compared with the age group 3–17 years. The estimated U.S. ASD prevalence was 2.38% (95% SI 2.10, 2.64) using data for the age group 6–17 years in the model compared with 2.21% (95% SI 1.95, 2.45) using data for the age group 3–17 years in the model (see Supplement for state estimates).
Discussion
Using existing data and adjusting for elevated mortality among persons living with ASD, we estimated national and state prevalence of adults 18–84 years of age living with ASD. Our estimate of 2.21% is higher than a study estimating ASD among adults in a community in England (1.0%) (Brugha et al. 2011). Our estimate may be higher because Brugha et al. was an empirical surveillance study conducted in one community in England among adults whereas the present analysis is a modeling study based on projecting prevalence from parent-report of children diagnosed with ASD in U.S. states to adults.
National and state ASD estimates in this analysis provide a general magnitude of the population of adults living with autism, but they have some important limitations. The prevalence of ASD among children, which was used to estimate prevalence among adults in our analysis, is based on parent report, which may under- or overestimate prevalence. For example, the estimates of ASD prevalence among children ages 3–17 years does not Include children with ASD who have not been diagnosed, leading to an underestimate of prevalence. Conversely, it may overestimate prevalence, as parents may falsely report that their child was diagnosed if ASD was suspected or if the child failed a screener but did not receive a diagnosis.
Our assumption that the ASD prevalence among children ages 3–17 years during 2016–2018 (born during 1999–2015) and adults (born before 1999) is similar does not account for the possibility of environmental or gene-environment interactions associated with ASD that may have changed over time. Exposure to some risk factors may have varied among birth cohorts. However, few risk factors have consistently been associated with ASD and those that have been identified have accounted for a very small percent of increases in diagnosed ASD (Schieve et al. 2011; Quinlan et al. 2015). One study found that changes in preterm delivery, small-for-gestational age, multiple births, cesarean delivery, and assisted reproductive technology use contributed to less than 1% of the 57% increase in ASD among 8-year-old children born in 1994 compared to 1998 (Schieve et al. 2011). A study conducted among children in New York City found that changes in maternal and paternal age accounted for only 2.7% of the 143% increase in ASD among children ages 0–3 from 0.03% in 1994 to 0.43% in 2001 (Quinlan et al. 2015). The prevalence of ASD among adults may be equivalent to that among children in that at least one study by Brugha et al. 2011 showed the adult prevalence was comparable to the estimated ASD prevalence among children at the time the study was conducted.
Limited information is available on mortality among adults with ASD. However, studies have shown consistently that adults with ASD have higher mortality rates than those without (Picket et al. 2006; Mouridsen et al. 2008; Gillberg et al. 2010; Hirvikoski et al. 2016). Most of the mortality studies followed persons to an average age of 30–55 years. We assumed the SMR remained the same for ages above 50 years; however, additional mortality studies that Include older persons with ASD are needed to validate this assumption.
There was some variation in the prevalence of ASD by state, with the prevalence ranging from 1.97 to 2.42%. The prevalence estimates were estimated using a partial-pooling hierarchical model that naturally pulls the raw state prevalence estimates towards the mean U.S. estimate and pulls those with less data more towards the mean. Currently, there is no evidence that the prevalence of ASD should vary by geographic location; however, there is evidence that greater availability of screening and diagnostic services will increase the number of persons diagnosed with ASD (Rolthlz et al. 2017; Janvier et al. 2016). Male and female ASD prevalence estimates were substantially different, which is consistent with existing studies (Kogan et al. 2018; Baio et al. 2018). The reason for this difference is unknown but it may reflect, in part, differences in how ASD manifests in boys and girls leading to differential diagnosis by gender.
To date, an empirical study of adult ASD prevalence in the U.S. has not been accomplished, perhaps because any single approach to ascertain adult ASD has challenges. There are no psychometrically validated tests of ASD for adults, which leads to uncertainty for studies using tests designed for children, such as the Autism Diagnostic Observation Schedule. In addition, mixed methods are likely needed in order to reach populations living independently and in group settings. A subset of persons might only be identified through the review of service records of those being served in group settings. Individuals with ASD who live independently may be disinclined to participate in a survey if recruited via phone or in person. Adults with ASD may be more difficult to recruit because they may not be enrolled in services or may not receive services in a wide variety of settings (e.g., schools, health care providers, community-based entities) resulting in challenges to comprehensive recruitment efforts. Once a validated tool to identify adults with ASD is created, a study could incorporate information from public school classifications or publicly-funded programs that serve individuals with ASD and population-based telephone or community surveys of adults with adjustments to address greater non-response among adults with ASD.
Overall, we estimated that 1 in 45 adults (95% SI, 41, 51), ages 18–84 years, are living with ASD. While these numbers are estimates, they do provide a place for states to think about available services for adults with ASD. We used the most current data available for all states to estimate the ASD prevalence among adults. This analysis may motivate some states to explore state-based data sources that may be more informative than data available for all states, and refine the estimates based on their existing local data.
Supplementary Material
Footnotes
Electronic supplementary material The online version of this article (https://doi.org/10.1007/s10803-020-04494-4) contains supplementary material, which is available to authorized users.
Disclosure The findings and conclusions in this paper are those of the authors and do not represent the official position of the Centers of Disease Control and Prevention.
References
- American Psychiatric Association. (2013). Diagnostic and statistical manual of mental disorders (5th ed.). Washington, D.C: American Psychiatric Association. [Google Scholar]
- Baio J, Wiggins L, Christensen D, et al. (2018). Prevalence of autism spectrum disorder among children aged 8 years - autism and developmental disabilities monitoring network, 11 sites, United States, 2014. MMWR Surveillance Summaries, 67(6), 1–23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Brugha TS, McManus S, Bankart J, et al. (2011). Epidemiology of autism spectrum disorders in adults in the community in England. Archives of General Psychiatry, 68(5), 459–465. [DOI] [PubMed] [Google Scholar]
- Croen LA, Zerbo O, Qian Y, et al. (2015). The health status of adults on the autism spectrum. Autism, 19(7), 814–823. [DOI] [PubMed] [Google Scholar]
- Gelman A, Carlin JB, Stern HS, & Rubin DB (2013). Bayesian Data Analysis. New York: CRC Press. [Google Scholar]
- Gilboa SM, Devine OJ, Oster ME, et al. (2016). Congenital health defects in the United States. Estimating the magnitude of the affected population in 2010. Circulation, 134, 101–109. 10.1161/circulationaha.l15.019307. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Gillberg C, Billstedt E, Sundh V, & Gillberg IC (2010). Mortality in autism: A prospective longitudinal community-based study. Journal of Autism and Developmental Disorders, 40(3), 352–357. 10.1007/s10803-009-0883-4. [DOI] [PubMed] [Google Scholar]
- Hirvikoski T, Mittendorfer-Rutz E, Boman M, et al. (2016). Premature mortality in autism spectrum disorder. British Journal of Psychiatry, 208(3), 232–238. [DOI] [PubMed] [Google Scholar]
- Janvier YM, Harris JF, Coffield CN, et al. (2016). Screening for autism spectrum disorder in underserved communities: Early childcare providers as reporters. Autism, 20(3), 364–373. 10.1177/1362361315585055. [DOI] [PubMed] [Google Scholar]
- Kogan MD, Vladutiu CJ, Schieve LA, et al. (2018). The prevalence of parent-reported autism spectrum disorder among US children. Pediatrics, 142(6), 1–11. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Mouridsen SE, Bronnum-Hansen H, Rich B, & Isager T (2008). Mortality and causes of death in autism spectrum disorders. Autism, 12(4), 403–414. [DOI] [PubMed] [Google Scholar]
- Murphy CM, Wilson CE, Roberston DM, et al. (2016). Autism spectrum disorder in adults: diagnosis, management, and health services development. Neuropsychiatr Dis Treat, 2016(12), 1669–1686. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Nicolaidis C, Kripke CC, & Raymaker D (2014). Primary care for adults on the autism spectrum. Medical Clinics of North America, 98(5), 1169–1191. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Pickett JA, Paculdo DR, Shavelle RM, et al. (2006). 1998–2002 Update on “Causes of death in autism”. Journal of Autism and Developmental Disorders, 36(2), 287–288. [DOI] [PubMed] [Google Scholar]
- Quinlan CA, McVeigh KH, Driver CR, et al. (2015). Prental Age and autism spectrum disorders among New York City children 0–36 months of age. MCHJ, 19, 1783–1790. [DOI] [PubMed] [Google Scholar]
- Rosenberg ES, Rosenthal EM, Hall EW, et al. (2018). Prevalence of hepatitis C virus infection in US states and the District of Columbia, 2013 to 2016. JAMA Netw Open, 1(8), e186371. [DOI] [PMC free article] [PubMed] [Google Scholar]
- Rotholz DA, Kinsman AM, Lacy KK, et al. (2017). Improving early identification and intervention for children at risk for autism spectrum disorder. Pediatrics, 10.1542/peds.2016-1061. [DOI] [PubMed] [Google Scholar]
- Roux AM, Shattuck PT, Rast JE, Rava, et al. (2015). National autism indicators report: Transition into Young Adulthood. Life course Outcomes Research Program. Philadelphia, PA: A.J. Drexel Autism Institute Drexel University. [Google Scholar]
- Schieve LA, Rice C, Devine O, et al. (2011). Have secular changes in perinatal risk factors contributed to the recent autism prevalence increase? Development and application of a mathematical assessment model. Annals of Epidemiology, 21(12), 930–945. [DOI] [PMC free article] [PubMed] [Google Scholar]
- United States Department of Health and Human Services (US DHHS), Centers for Disease Control and Prevention (CDC), National Center for Health Statistics (NCHS). (2018a). Bridged-Race Population Estimates, United States July 1st resident population by state, county, age, sex, bridged-race, and Hispanic origin. Post-censal population estimates. Retrieved July 29, 2019, from https://wonder.cdc.gov/bridged-race-v2017.html.
- United States Department of Health and Human Services (US DHHS) Centers for Disease Control and Prevention, National Center for Health Statistics. (2018b). Underlying Cause of Death 1999-2017. Retrieved July 29, 2019, from https://wonder.cdc.gov/bridged-race-v2017.html.
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.


