Abstract
Purpose:
To present primary ocular manifestations in acute leukemia.
Methods:
This cross-sectional descriptive hospital-based study evaluated all newly diagnosed leukemia patients of three referral hospitals of Tehran University of Medical Sciences in 2015–2016 and Mahak Hospital in Tehran in 2017. Exclusion criteria included the patients with the previous history of chemotherapy, cases of relapsing disease, and the patients with a history of ocular disease or other systemic conditions with ophthalmic manifestations.
Results:
A total of 85 patients (170 eyes) were evaluated in our study, including 29 children (34.1%) and 43 females (50.6%). The mean patient age was 37.84 ± 11.91 years in the adult group and 6.28 ± 4.70 years in the pediatric category. Ophthalmic involvement was seen in 27 patients (31.8%), including 6 pediatric patients (20.7%) and 21 adult patients (37.5%). Two patients (2.3%) had direct infiltration by leukemic cells and 76 patients (89.41%) of patients were asymptomatic. There was a correlation between ophthalmic involvement and platelet count and hemoglobin level. In patients with ocular signs, higher mortality rates were observed.
Conclusions:
At the time of diagnosis in acute leukemia patients, complete ophthalmic evaluation including dilated fundus examination is suggested as ocular involvement in these patients is common and sometimes asymptomatic. Ophthalmic involvement in leukemic patients should be identified in a timely manner, particularly in individuals with low platelet counts and hemoglobin levels, due to the potential prognostic relevance.
Keywords: Acute leukemia, Acute lymphoblastic leukemia, Acute myeloid leukemia, Leukemia, Ocular leukemic infiltration, Ophthalmic manifestation
INTRODUCTION
Leukemia is an uncontrolled proliferation of stem cells in the bone marrow infiltrating different organs.1 Ocular and orbital involvement is common in leukemia; being the third most common site of extramedullary lesions in acute leukemia, preceded by meningeal and testicular involvement, described as a sign of poor prognosis.2
Leukemic ophthalmopathy is classified as primary infiltration of leukemic cells in different eye tissues and secondary lesions due to hyperviscosity and/or immunosuppression. Patients may be asymptomatic or complain of vision loss.3
Few studies have assessed the rate of ocular findings related to leukemia at the time of diagnosis4,5,6 and this subject has not been investigated in Iranian community. In addition, a relationship between ocular manifestations and mortality rates is yet to be established in different ethnicity groups. The current research aims to report the rate and prognostic value of various ocular involvements in acute leukemia at the time of disease diagnosis.
METHODS
This cross-sectional descriptive hospital-based study was conducted on consecutive newly diagnosed leukemia patients of three referral hospitals of Tehran University of Medical Sciences (Farabi Eye Hospital, Shariati Hospital, and Children's Hospital) from 2015 to 2016. In 2017, the patients of Mahak Hospital and Rehabilitation Complex in Tehran were also recruited. Patients with previous history of chemotherapy, cases of relapsing disease, and patients with a history of ocular disease (glaucoma, age-related macular degeneration, previous history of retinal vascular disorders and previous history of uveitis) or other systemic conditions (e.g., diabetes mellitus) with ophthalmic manifestations were excluded from study.
The local Institutional Review Board of Tehran University of Medical Sciences (IR.TUMS.REC.1394.1494) approved the current study. The study was adherent to the Declaration of Helsinki. Informed consent was obtained from all patients, parents, or guardians before enrolment.
A thorough ophthalmologic examination was performed for the patients. Examination protocol included visual acuity measurement with Snellen chart, slit-lamp examination, dilated fundoscopy, and if needed, the retinal imaging. We did not perform fundus fluorescein angiography on any patients due to safety concerns regarding performing invasive imaging on critically ill patients. In some inpatient cases, examination was done at patient's bedside using portable slit-lamp, indirect ophthalmoscope and hand-held fundus camera.
In addition to ophthalmologic examinations, demographic data, pathologic factors, biomarkers, and laboratory tests were extracted from each patient's documents. The mortality rate during the first chemotherapy session (concurrent with the ocular examination) was also recorded.
All statistical analyses were performed using SPSS software (SPSS, Inc., Chicago, IL). Univariate and multivariate binary logistic regression was used to find the predictors of ophthalmic manifestations and mortality. A receiver operating characteristic (ROC) curve analysis was used to develop a cut-off point for platelet and hemoglobin levels that predicted the likelihood of ocular involvement.
RESULTS
A total of 85 patients (170 eyes) including 29 children (age <18 years old) (34.1%) were studied in this research. Subjects comprised 43 female (50.6%) and 42 males (49.4%). Mean age of the patients was 37.84 ± 11.91 years in the adult group and 6.28 ± 4.70 years in pediatric group. Table 1 shows the demographic characteristics of the patients. The details of leukemia subtypes are summarized in Table 2.
Table 1.
Demographic data
| Total (n=85) | Adults (n=56) | Pediatrics (n=29) | |
|---|---|---|---|
| Age (years), mean±SD | 27.6±17.9 | 37.8±11.9 | 6.3±4.7 |
| Sex (% female) | 43 (50.6) | 24 (42.9) | 19 (65.5) |
| Ocular involvement (% bilateral) | 27 patients (bilateral in 70.4) | 21 patients (bilateral in 61.9) | 6 patients (bilateral in 100) |
| BCVA (logMAR) | 0.07±0.27 | 0.05±0.25 | 0.16±0.38 |
| Visual complaint (%) | 9 patients (10.6) | 8 patients (14.3) | 1 patient (3.4) |
| Mean WBC count (/ml) | 21501.9±36281.0 | 18970.9±34096.9 | 26214.8±40235.7 |
| Mean platelets count (×103/ml) | 91.9±102.6 | 66.6±79.0 | 139.1±124.5 |
| Mean Hb level (g/dl) | 8.1±2.1 | 8.2±1.5 | 7.7±2.8 |
BCVA: Best corrected visual acuity, WBC: White blood cells, Hb: hemoglobin, SD: Standard deviation
Table 2.
Distribution of the subtypes of acute leukemia
| Patients (%) | |
|---|---|
| AML | 37 (43.53) |
| M1 | 6 (16.22) |
| M2 | 3 (8.10) |
| M3 | 7 (18.92) |
| M4 | 9 (24.32) |
| M5 | 7 (18.92) |
| M6 | 1 (2.70) |
| Uncategorized | 4 (10.82) |
| ALL | 48 (56.47) |
| Pre-B cell | 26 (54.17) |
| Mature B-cell | 7 (14.58) |
| Pre-T cell | 7 (14.58) |
| Uncategorized | 8 (16.67) |
ALL: Acute lymphoblastic leukemia, AML: Acute myeloid leukemia
Since the majority of these patients were critically ill at the time of their diagnosis, an eye examination was done on 68 patients (80%) few days after their first admission to assist them stabilize. Only 20% of patients were ophthalmologically tested prior to initiation of systemic chemotherapy. The average time lag between the initiation of therapy and the ophthalmologic assessment was 4.17 ± 3.88 days. There was no significant difference in ophthalmic involvement between the two groups (P = 0.078). After a mean period of 42.13 ± 3.53 weeks, the medical records of the patients were assessed for determination of mortality rate and cause of death.
Ophthalmic involvement was seen in 27 patients (31.8%), including 6 patients in pediatric group (20.7%) and 21 patients in adult group (37.5%). However, the difference between the two groups (P = 0.115) was not statistically significant. The ocular findings were bilateral in 22.4% (19 patients) of cases (23.2% and 20.7% in adult and pediatric groups, respectively). The mean visual acuity was 0.07 ± 0.28 of logMAR in adult group. Most patients were asymptomatic and only 9 (10.6%) patients complained of vision loss; including one pediatric patient.
Ophthalmologic signs included bilateral lid edema in 1 patient (1.2%), vitreous hemorrhage in 3 eyes (1.8%), optic disc swelling in 4 eyes (2.3% [Figure 1]), Roth's spot in 19 eyes (11.2%), retinal hemorrhage (including pre, intra, and subretinal) in 31 eyes (18.2%) [Figures 2 and 3], subhyaloid hemorrhage with foveal involvement in 9 eyes (5.3%), and extrafoveal subhyaloid hemorrhage in 2 eyes (1.2%). The details of ophthalmic findings in each group and laboratory tests are shown separately in Table 3. Table 4 demonstrates the distribution of different retinal findings based on disease category (acute lymphoblastic leukemia [ALL] vs. acute myeloid leukemia [AML]). Orbital abnormalities were uncommon in our study, with the exception of one case of bilateral eyelid edema. A lumbar puncture in one of the patients with optic disc edema indicated leukemic involvement, which was treated with intrathecal chemotherapy. Two patients (2.3 %) had a potential direct invasion of leukemia cells. First patient was a 51-year-old woman with pre-B cell ALL who had no complaint of visual loss. Direct retinal infiltration was seen as grey nodules along the arcades. The patient was critically sick and toxic to be admitted to Farabi Eye Hospital and expired from septic shock 7 days after examination. The second patient was a 42-year-old man, newly diagnosed with refractory anemia with excess blasts-r without a visual loss complaint. He exhibited bilateral disc swelling with peripapillary subretinal hemorrhage in the left eye on ophthalmologic examination. Brain and orbital magnetic resonance imaging was normal. Edema persisted 3 weeks after initiation of systemic and intrathecal chemotherapy.
Figure 1.
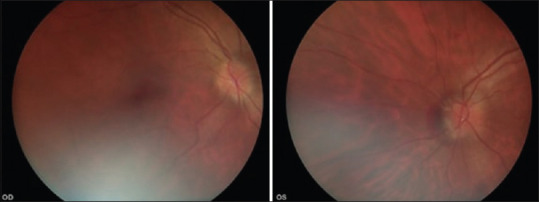
Fundus photo of a patient showing bilateral optic disc edema with peripapillary subretinal hemorrhage in the left eye
Figure 2.
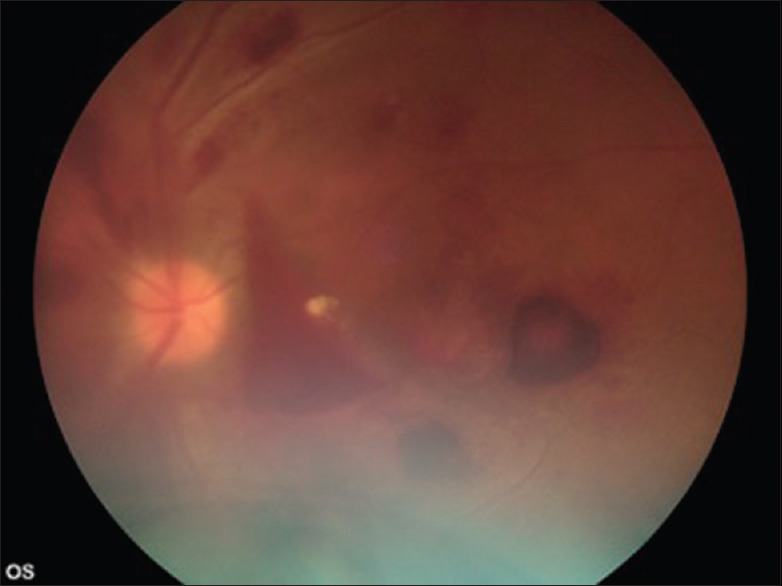
Fundus photo of the left eye of a patient with concomitant vitreous hemorrhage, Roth's spot, retinal and subhyaloid hemorrhage
Figure 3.
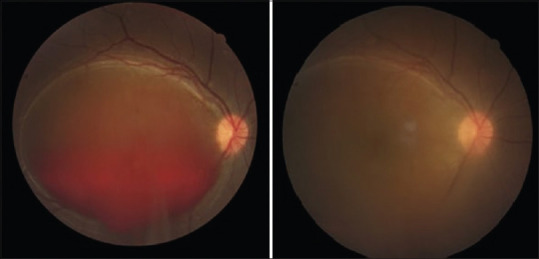
Subhyaloid hemorrhage that was treated by YAG hyaloidotomy (left image). Fundus photo of the same eye a few days later with considerable hazy media due to vitreous hemorrhage (right image)
Table 3.
Ophthalmic findings in each age group
| Eyes (%) | P* | ||
|---|---|---|---|
|
| |||
| Adult group (112 eyes) | Pediatric group (58 eyes) | ||
| Lid edema | 2 (1.8) | 0 | 0.548 |
| Vitreous hemorrhage | 2 (1.8) | 1 (1.7) | 0.227 |
| Optic disc swelling | 2 (1.8) | 2 (3.4) | 0.429 |
| Roth’s spot | 10 (8.9) | 9 (15.5) | 0.211 |
| Retinal hemorrhage | 25 (22.3) | 6 (10.3) | 0.049 |
| Subhyaloid hemorrhage | 5 (4.5) | 6 (10.3) | 0.348 |
*Pearson Chi-square or Fisher’s exact test
Table 4.
Ophthalmic finding based on subgroups of acute leukemia
| Eyes (%) | P* | ||
|---|---|---|---|
|
| |||
| ALL (96 eyes) | AML (74 eyes) | ||
| Lid edema | 2 (2.1) | 0 | 0.212 |
| Vitreous hemorrhage | 1 eye (1.0) | 2 (2.7) | 0.185 |
| Optic disc swelling | 2 (2.1) | 2 (2.7) | 0.770 |
| Roth’s spot | 10 (10.4) | 9 (12.2) | 0.673 |
| Retinal hemorrhage | 16 (16.7) | 15 (20.3) | 0.491 |
| Subhyaloid hemorrhage | 4 (4.2) | 7 (9.5) | 0.150 |
*Pearson Chi-square or Fisher’s exact test. ALL: Acute lymphoblastic leukemia, AML: Acute myeloid leukemia
In binary logistic regression, ophthalmic involvement was correlated with platelet count and hemoglobin value (P = 0.017 and P = 0.007, respectively), but not with age, white blood cell (WBC) count, or disease category. In ROC curve, a cut-off of 7.35 g/dl for hemoglobin (sensitivity: 80%, specificity: 75%) and platelet count of 23.5 (×103/μl) (sensitivity: 70%, specificity: 75%) was determined for prediction of ocular involvement [Figures 4 and 5].
Figure 4.
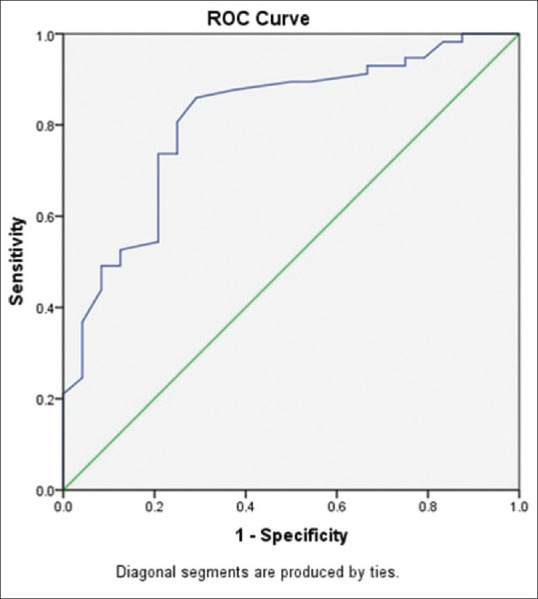
Receiver operating characteristic curve of minimum hemoglobin level with an area of 0.813 under the curve for detection retinal hemorrhage
Figure 5.
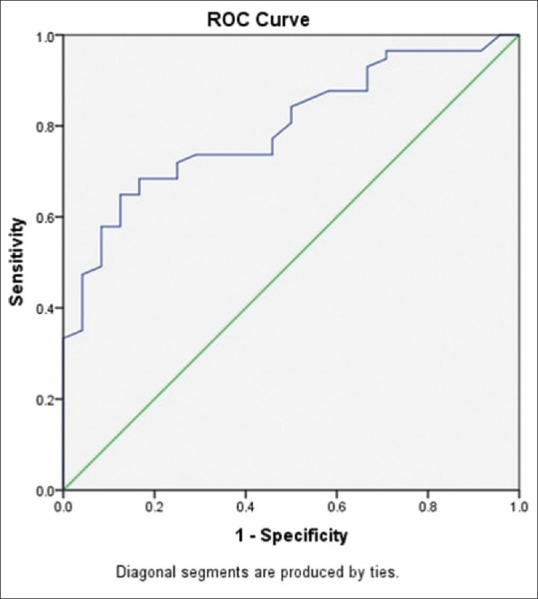
Receiver operating characteristic curve of minimum platelet number with an area of 0.813 under the curve for detection retinal hemorrhage
The total mortality rate was 21.2% (18 patients), and 77.7% (14 patients) died during their first session of admission. In the pediatric group, the total mortality rate was 24.1% (7 patients) with 42.9% of mortalities (3 patients) occurring during the first few days of the diagnosis. Overall, the causes of death included septic shock in 66.7% (12 patients), hemorrhage in 16.6% (3 patients) and resistance to chemotherapy in 16.6% (3 patients) of patients.
In the univariate analysis, ophthalmic involvement was associated with higher rates of death on the first day after diagnosis (P = 0.026, respectively). In addition, in binary logistic regression, after controlling for underlying malignancy and complete blood count findings, same session mortality rates were correlated with age, adult subgroup, and ophthalmic involvement (P = 0.000, P = 0.001 and P = 0.001, respectively).
DISCUSSION
The current study focuses on the clinical ophthalmic signs of acute leukemia at the commencement of the disease. Out of 85 individuals enrolled, 27 (31.8%) experienced ocular symptoms, the majority of which were retinal hemorrhages (88.8%). The mortality rates in the overall and first visit session were correlated with age and ophthalmic involvement.
Ocular involvement in leukemia is very common and 9% to 90% prevalence has been reported in various studies.7 The prevalence of ophthalmic involvement in this study was comparable with previous studies. A few prospective studies investigated the prevalence of leukemia ocular manifestations prior to the start of chemotherapy. Fifty-six newly diagnosed AML patients were evaluated by Karesh et al.4 and retinopathy was observed in 50% without leukemic infiltrates. Reddy examined 288 newly diagnosed leukemic patients and found ocular manifestations in 35%, although these findings were more common in adults (49%) than in children (16%).5
Schalat et al. were among the first physicians who studied the subject. In their investigation which evaluated 120 leukemia patients, the prevalence of ophthalmic involvement and direct ophthalmic infiltration was 39% and 3%, respectively.6 In a retrospective study of 185 patients with acute leukemia, Bitirgen et al.8 found 20% and 36% ocular involvement in ALL and AML patients, respectively, at the time of diagnosis. Mendonca examined 55 cases and showed 32.7% of ocular involvement.9 Hafeez et al. reported higher prevalence of ocular involvement (in 97 cases) in newly diagnosed (57.1%) cases as compared to followed patients (36.6%).10
Similar prevalence rates were found in more recent studies.11,12 The limited variation between different studies may be due to diversities in target study population and examination protocols. The higher rates shown in certain studies in Nigeria and other African nations might be attributable to resource-efficient healthcare systems, where patients are treated late during the course of the disease.11
Many studies have indicated that ocular manifestation is most commonly asymptomatic in leukemia.10,12,13,14 As with our study, among 27 patients with ocular signs, only 7 (26%) patients (including only one child) had visual complaints and others were asymptomatic despite visually significant subhyaloid hemorrhage in two of them, emphasizing the importance of ophthalmic examination even in asymptomatic patients.
While some reports indicate that ophthalmic manifestations are more prevalent in AML than in ALL,12,15 the current research did not show any major difference between the two groups, comparable to Omoti et al. study.16 This might be because our and Omoti's studies only included treatment naive individuals, whereas their studies also included relapsed instances of leukemia.12,15
As in other studies,10 anterior segment manifestations are far less prevalent than the posterior segment involvement. According to the findings of previous studies, the most prevalent posterior segment symptoms were pre and intraretinal hemorrhages, as well as Roth spots.4,5,8,10
We found significant relation between ophthalmic involvement and platelet and low hemoglobin levels. Our result is consistent with other studies.17,18,19,20 In ALL patients, low platelet count (P = 0.046) was found to be associated with intraretinal hemorrhages. Similar results were also reported by Reddy and Jackson,5 Guyer et al.,17 and Holt and Gordon-Smith.19 On the other hand, abu el-Asrar et al.21 and Suresh et al.18 noted a significant association of low Hb with intraretinal hemorrhage in ALL patients.
Soman et al. found that Hb levels are the best predictors of posterior segment manifestation of the disease and improving the Hb level from 5 to 7 g/L contributes to substantial reduction in the risk of developing subhyaloid hemorrhages. Similarly, it was found that maintaining platelet counts above 50,000 cells/mm3 significantly reduced the risk of subhyaloid hemorrhage and overall ophthalmic manifestations.22
In our study, the cut-off thresholds were 23.5 (×103/μl) for platelet count (sensitivity: 70%, specificity: 75%) and 7.35 g/dl for Hb (sensitivity: 80%, specificity: 75%) for ocular involvement. Other previous studies showed no association or positive correlation with high total leukocyte counts, low platelet counts, and low Hb levels.7,17,23 These results are important because they may lead oncologists to identify target patients that are more in need of ophthalmological evaluations. As in prior research, there was a strong relationship between ocular involvement and same-session mortality rates.24,25 In accordance with Marylin et al.,25 the significance of ophthalmological evaluation in the systematic assessment of disease status and prognosis in patients with leukemia can be inferred.
Two patients had direct leukemic infiltration, including one patient with ALL with WBC count of 97,160/ml. The other patient with optic disc edema was actually leukopenic with WBC of 2130. High WBC count has been described to be associated with higher rates of ocular leukemic infiltration, which was similarly concluded by Leonardy et al. in their study on 135 leukemic patients.26 As a result, in addition to platelet count and hemoglobin levels, WBC count may be an important aspect for ophthalmologists to consider when examining leukemic patients. This study was conducted for evaluation of ophthalmic leukemia of newly diagnosed leukemic patients. This is one of the first studies to stratify the risk of ocular involvement and offer blood transfusion recommendations to leukemia patients to prevent vision loss.
There are limitations to our study: the lack of adequate paraclinical ophthalmic investigations, including choroid assessment, due to the referral of patients to other centers and the fact that disease severity prevented the transfer of these patients to Farabi Eye Hospital for further investigation. Further studies may be planned to test subclinical choroid infiltration in patients with leukemia using ultrasound and enhanced depth imaging ocular coherence tomography and fluorescein angiography in the patients with less severe malaise.
With respect to high rates (89.41%) of asymptomatic ocular involvement, complete dilated eye examination is recommended in all cases of leukemia at the onset of disease, especially in pediatric patients and patients with low platelet count and hemoglobin levels. Prediction of ocular involvement in these patients with appropriate sensitivity and specificity can be made on the basis of a cut-off point of 7.35 g/dl and 23500/μl for hemoglobin and platelet count, respectively.
In conclusion, ophthalmic manifestations of acute leukemia may have a prognostic role in predicting the same-session mortality in patients; emphasizing the role of ophthalmologist as a member of leukemia management team.
Financial support and sponsorship
Nil.
Conflicts of interest
There are no conflicts of interest.
REFERENCES
- 1.Obasi C, Omoti C, Ukponmwan C, Omoti A. Ocular manifestations in patients with leukemia at the university of Benin teaching hospital, Benin City, Nigeria: A case control study. Ann Med Surg Pract. 2017;2:92–100. [Google Scholar]
- 2.Charif MC, Belmekki M, Hajji Z, Tahiri H, Amrani R, El Bakkali M, et al. Ophthalmic manifestations of acute leukemia. J Fr Ophtalmol. 2002;25:62–6. [PubMed] [Google Scholar]
- 3.Sharma T, Grewal J, Gupta S, Murray PI. Ophthalmic manifestations of acute leukaemias: The ophthalmologist's role. Eye (Lond) 2004;18:663–72. doi: 10.1038/sj.eye.6701308. [DOI] [PubMed] [Google Scholar]
- 4.Karesh JW, Goldman EJ, Reck K, Kelman SE, Lee EJ, Schiffer CA. A prospective ophthalmic evaluation of patients with acute myeloid leukemia: Correlation of ocular and hematologic findings. J Clin Oncol. 1989;7:1528–32. doi: 10.1200/JCO.1989.7.10.1528. [DOI] [PubMed] [Google Scholar]
- 5.Reddy SC, Jackson N, Menon BS. Ocular involvement in leukemia – A study of 288 cases. Ophthalmologica. 2003;217:441–5. doi: 10.1159/000073077. [DOI] [PubMed] [Google Scholar]
- 6.Schachat AP, Markowitz JA, Guyer DR, Burke PJ, Karp JE, Graham ML. Ophthalmic manifestations of leukemia. Arch Ophthalmol. 1989;107:697–700. doi: 10.1001/archopht.1989.01070010715033. [DOI] [PubMed] [Google Scholar]
- 7.Orhan B, Malbora B, Akça Bayar S, Avcı Z, Alioğlu B, Özbek N. Ophthalmologic findings in children with leukemia: A single-center study. Turk J Ophthalmol. 2016;46:62–7. doi: 10.4274/tjo.03880. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Bitirgen G, Belviranli S, Caliskan U, Tokgoz H, Ozkagnici A, Zengin N. Ophthalmic manifestations in recently diagnosed childhood leukemia. Eur J Ophthalmol. 2016;26:88–91. doi: 10.5301/ejo.5000647. [DOI] [PubMed] [Google Scholar]
- 9.De Queiroz Mendonca C, Freire MV, Viana SS, Silva Tavares MK, Almeida Silva WM, Cipolotti R. Ocular manifestations in acute lymphoblastic leukemia: A five-year cohort study of pediatric patients. Leuk Res. 2019;76:24–8. doi: 10.1016/j.leukres.2018.11.017. [DOI] [PubMed] [Google Scholar]
- 10.Hafeez MU, Ali MH, Najib N, Ayub MH, Shafi K, Munir M, et al. Ophthalmic manifestations of acute leukemia. Cureus. 2019;11:e3837. doi: 10.7759/cureus.3837. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Eze BI, Ibegbulam GO, Ocheni S. Ophthalmic manifestations of leukemia in a tertiary hospital population of adult Nigerian Africans. Middle East Afr J Ophthalmol. 2010;17:325–9. doi: 10.4103/0974-9233.71599. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Koshy J, John MJ, Thomas S, Kaur G, Batra N, Xavier WJ. Ophthalmic manifestations of acute and chronic leukemias presenting to a tertiary care center in India. Indian J Ophthalmol. 2015;63:659–64. doi: 10.4103/0301-4738.169789. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 13.Kochar S, Singhal Y, Manohar JM, Jain K. Ophthalmic manifestations in patients of acute leukaemia presenting to a tertiary care Centre in western Rajasthan. Delhi J Ophthalmol. 2018;28:20–4. [Google Scholar]
- 14.Khadka D, Sharma AK, Shrestha JK, Shrestha GS, Shrestha PN, Pant SR, et al. Ocular manifestations of childhood acute leukemia in a tertiiary level eye centre of Kathmandu, Nepal. Nepal J Ophthalmol. 2014;6:197–204. doi: 10.3126/nepjoph.v6i2.11678. [DOI] [PubMed] [Google Scholar]
- 15.Russo V, Scott IU, Querques G, Stella A, Barone A, Delle Noci N. Orbital and ocular manifestations of acute childhood leukemia: Clinical and statistical analysis of 180 patients. Eur J Ophthalmol. 2008;18:619–23. doi: 10.1177/112067210801800420. [DOI] [PubMed] [Google Scholar]
- 16.Omoti AE, Omoti CE, Momoh RO. Ocular disorders in adult leukemia patients in Nigeria. Middle East Afr J Ophthalmol. 2010;17:165–8. doi: 10.4103/0974-9233.63081. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Guyer DR, Schachat AP, Vitale S, Markowitz JA, Braine H, Burke PJ, et al. Leukemic retinopathy. Relationship between fundus lesions and hematologic parameters at diagnosis. Ophthalmology. 1989;96:860–4. doi: 10.1016/s0161-6420(89)32809-0. [DOI] [PubMed] [Google Scholar]
- 18.Suresh K, Sampath R. Ocular manifestations in hematological disorders. Sri Ramachandra J Med. 2011;4:1–4. [Google Scholar]
- 19.Holt JM, Gordon-Smith EC. Retinal abnormalities in diseases of the blood. Br J Ophthalmol. 1969;53:145–60. doi: 10.1136/bjo.53.3.145. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Dhasmana R, Prakash A, Gupta N, Verma SK. Ocular manifestations in leukemia and myeloproliferative disorders and their association with hematological parameters. Ann Afr Med. 2016;15:97–103. doi: 10.4103/1596-3519.188887. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Abu El-Asrar AM, Al-Momen AK, Kangave D, Harakati MS, Ajarim DS. Correlation of fundus lesions and hematologic findings in leukemic retinopathy. Eur J Ophthalmol. 1996;6:167–72. doi: 10.1177/112067219600600213. [DOI] [PubMed] [Google Scholar]
- 22.Soman S, Kasturi N, Srinivasan R, Vinod KV. Ocular manifestations in leukemias and their correlation with hematologic parameters at a tertiary care setting in South India. Ophthalmol Retina. 2018;2:17–23. doi: 10.1016/j.oret.2017.05.009. [DOI] [PubMed] [Google Scholar]
- 23.Jackson N, Reddy SC, Hishamuddin M, Low HC. Retinal findings in adult leukaemia: Correlation with leukocytosis. Clin Lab Haematol. 1996;18:105–9. doi: 10.1046/j.1365-2257.1996.d01-217.x. [DOI] [PubMed] [Google Scholar]
- 24.Ohkoshi K, Tsiaras WG. Prognostic importance of ophthalmic manifestations in childhood leukaemia. Br J Ophthalmol. 1992;76:651–5. doi: 10.1136/bjo.76.11.651. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Grishina E, Mamontov A. Ophthalmic manifestations of leukemia. Almanac of Clinical Medicine. 2016;44:587–91. [Google Scholar]
- 26.Leonardy NJ, Rupani M, Dent G, Klintworth GK. Analysis of 135 autopsy eyes for ocular involvement in leukemia. Am J Ophthalmol. 1990;109:436–44. doi: 10.1016/s0002-9394(14)74610-0. [DOI] [PubMed] [Google Scholar]


