Abstract
Background
The Open Payments Program, as designated by the Physician Payments Sunshine Act, is the single largest repository of industry payments made to licensed physicians within the United States. Though sizeable in its dataset, the database and user interface are limited in their ability to permit expansive data interpretation and summarization.
Objectives
The authors sought to comprehensively compare industry payments made to plastic surgeons with payments made to all surgeons and all physicians to elucidate industry relationships since implementation.
Methods
The Open Payments Database was queried between 2014 and 2019, and inclusion criteria were applied. These data were evaluated in aggregate and for yearly totals, payment type, and geographic distribution.
Results
A total 61,000,728 unique payments totaling $11,815,248,549 were identified over the 6-year study period; 9089 plastic surgeons, 121,151 surgeons, and 796,260 total physicians received these payments. Plastic surgeons annually received significantly less payment than all surgeons (P = 0.0005). However, plastic surgeons did not receive significantly more payment than all physicians (P = 0.0840). Cash and cash equivalents proved to be the most common form of payment; stock and stock options were least commonly transferred. Plastic surgeons in Tennessee received the most in payments between 2014 and 2019 (mean $76,420.75). California had the greatest number of plastic surgeons who received payments (1452 surgeons).
Conclusions
Plastic surgeons received more in industry payments than the average of all physicians but received less than all surgeons. The most common payment was cash transactions. Over the past 6 years, geographic trends in industry payments have remained stable.
The Open Payments Program was developed at the direction of the Affordable Care Act to promote transparency and accountability within the healthcare system.1,2 The Physician Payments Sunshine Act (PPSA) requires that medical manufacturers and group purchasing organizations who produce or negotiate any product covered by Medicare, Medicaid, or the Children’s Health Insurance Program must annually report all transfers of value greater than $10.00 paid to licensed physicians and teaching hospitals.2-4 Such payments may include consultations fees, meals, grants, donations, and ownership or investment by a physician in these medical companies.5,6
Concerns over physician financial conflicts of interest sparked such initiatives.7 Studies have shown that patients believe that their treating physician’s financial interests should be disclosed.8,9 When appropriate, working relationships between healthcare entities and medical manufacturers are often invaluable, supporting research developments and improving patient care.10 However, these advantages do not obviate the necessary boundary that exists between effective scientific collaboration and financial relationships that may unduly influence or complicate decision making in patient care.11,12 A 2007 national survey showed that 94% of all US physicians reported a financial relationship with industry.13 PPSA legislation is responsible for collecting reimbursement data from 6 consecutive years, which has been annually reported on the Open Payments database.
Despite affording the public an unprecedented level of transparency, certain aspects of physician-industry relationships remain nebulous.7 Although publicly available, the database provides limited global analytics. Because data are provided at the individual physician level, a search for specialty-specific payments and associated trends is not readily accessible. Plastic surgery is a unique medical field that focuses on creativity and innovation, but these ideas often require industry sponsorship to reach fruition. The nature and extent of our collaborations with industry may vary from other medical and surgical fields based on specialty-specific needs. Public perceptions may draw disproportionate attention from the lay media. These distinct features of plastic surgery may intensify any scrutiny of our financial conflicts, rendering self-awareness of our industry relationships critically important.
To better understand the Open Payments database and the overall impact of PPSA legislation on physician payments in plastic surgery, we analyzed data reported from 2014 to 2019 on plastic surgeons and compared their payment trends with those observed with all surgeons and all doctors in the database.
METHODS
Study Population
The CMS Open Payments database (https://www.cms.gov/OpenPayments) captures industry-related payments made to physicians. All allopathic and osteopathic physicians who held MD or DO degrees and practiced in the United States were available for inclusion in these analysis. We included payments made to physicians within the United States, including Alaska and Hawaii, but excluded those occurring in other countries or United States minor outlying islands. Payments made to physicians were sorted into 3 cohorts. The first cohort included payments made to plastic surgeons. Those practicing plastic surgery, either after completing a general surgery residency and plastic surgery fellowship or completing an integrated plastic surgery residency program, were included in this first cohort. Plastic surgeons whose primary specialty was ophthalmology or otolaryngology were excluded from the plastic surgeon’s cohort. A second cohort of the payments made to all surgeons during the study period included the specialties of general surgery (and its subspecialties), neurological surgery, oral and maxillofacial surgery, cardiothoracic surgery, transplant surgery, orthopedic surgery, otolaryngology, urology, and plastic surgery. Finally, a third cohort was sectioned, representing the payments made to all allopathic and osteopathic physicians, or all doctors, during the study window.
Dataset and Linkage
The CMS Open Payments database is publicly available and searchable, containing provider-specific data, including the field of practice; geographic location; payor company; and the nature, amount, and date of reimbursement. The database (https://www.cms.gov/OpenPayments) was accessed in August 2020 to obtain physician payment data. R.P. conducted the query, and the search results were reviewed by R.P. and J.K. At the time of this study, payment information from the years 2013 to 2019 was available. The datasets describing general payments made to healthcare workers were collated. Payment information from 2013 was incomplete and excluded. The payments made to physicians from January 1, 2014, through December 31, 2019, were extracted and analyzed.
Payment Categories and Statistical Analysis
All data collection and analysis were conducted employing R as the statistical software platform,14 utilizing dplyr,15 tidyr,16 and stringr.17
Totals per Year
The sum, mean, standard deviation (SD), and number of payments received per physician in each cohort were derived. These analyses were compared in aggregate as well as within the 3 cohort groups. Statistical analysis was conducted with 1-way analysis of variance and Tukey’s multiple comparisons testing.
Totals by Type
An investigation was further conducted into the evolution of payment types made from industry to plastic surgeons over the 6-year study period. The form of payment and the method by which value was transferred from industry affiliates to plastic surgeons were analyzed.
Totals by Region
Geographical information indicating where physicians received payments was extracted. US zip codes were extracted and utilized to geocode our database. This information was transferred onto a map to represent the amount, density, and number of payments received per region of the continental United States. Geographic data visualizations were created in Tableau Desktop (Tableau, Mountain View, CA).18 The relative amount of money transferred by each state was reported.
RESULTS
The included dataset contained payment information from 10,191,281 unique payments totaling $1,897,444,564 transferred in 2014, then 10,463,302 unique payments totaling $1,885,500,098 in 2015, followed by 10,531,779 unique payments totaling $1,941,327,891 in 2016, 10,246,921 unique payments totaling $1,931,077,892 in 2017, 9,990,536 unique payments totaling $2,011,265,921 in 2018, and 9,576,909 unique payments totaling $2,148,632,182 in 2019. In total, $11,815,248,549 from 61,000,728 payments was received by allopathic and osteopathic physicians in the United States between 2014 and 2019. Over the 6-year study period, 9089 plastic surgeons received industry-related payments. These plastic surgeons were also included in the “all surgeons” cohort (121,151 total surgeons) and “all doctors” cohort (796,260 total doctors) who were recorded receiving payments between 2014 and 2019.
Aggregate Statistics
In aggregate, the 9089 practicing plastic surgeons received 369,111 payments from 2014 to 2019, totaling $205,068,948.51. Plastic surgeons received an average of $555.58 per payment ± (SD) $28,836.70. Over these 6 years, the range of individual payments to a single plastic surgeon varied from $0.00 to $6,745,346.00. The 121,151 surgeons received 6,569,786 payments from 2014 through 2019, totaling $4,501,710,212.43. Surgeons received an average of $685.21 per payment ± $35,879.60. Over these 6 years, the range of individual payments to a single surgeon varied from $0.00 to $49,921,760.55. The 796,260 doctors, inclusive, received 61,000,728 payments from 2014 through 2019, totaling $11,815,248,548.99. All doctors received an average of $193.69 per payment ± $15,083.89. Over these 6 years, the range of individual payments to a single physician varied from $0.00 to $49,921,760.55. Average annual industry payments were calculated for each cohort based on the total number of physicians and total payments included for each 6-year cohort. On average, the 9089 plastic surgeons each received $22,562.32 from 2014 to 2019, or $3760.39 annually. On average, the 121,151 surgeons received $37,157.85 from 2014 to 2019, or $6192.97 annually. On average, the 796,260 doctors received $14,838.43 from 2014 to 2019, or $2473.07 annually.
Totals per Year
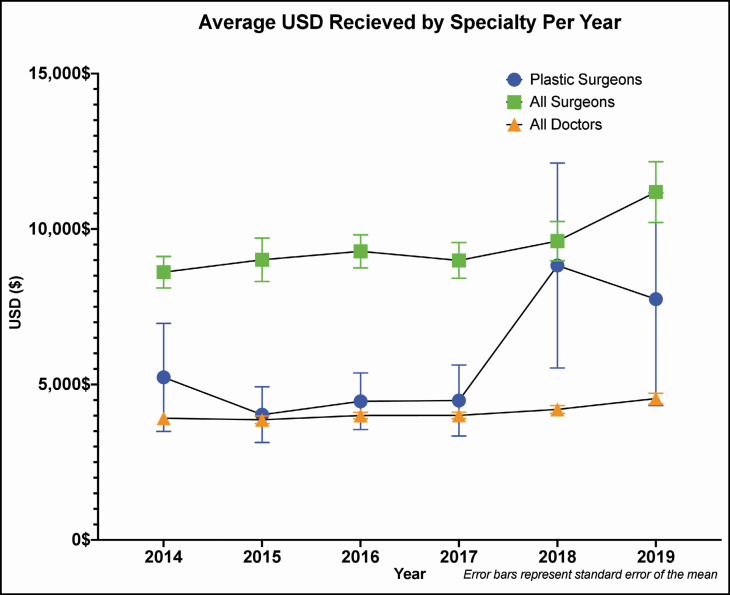
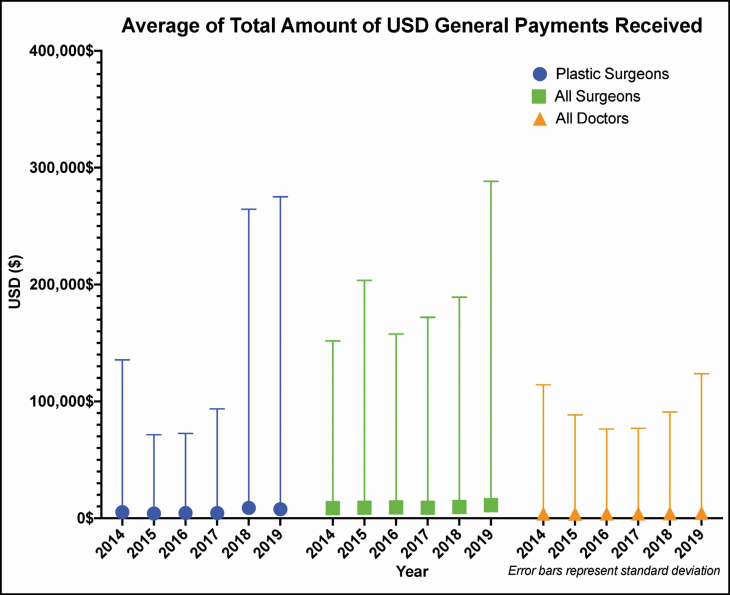
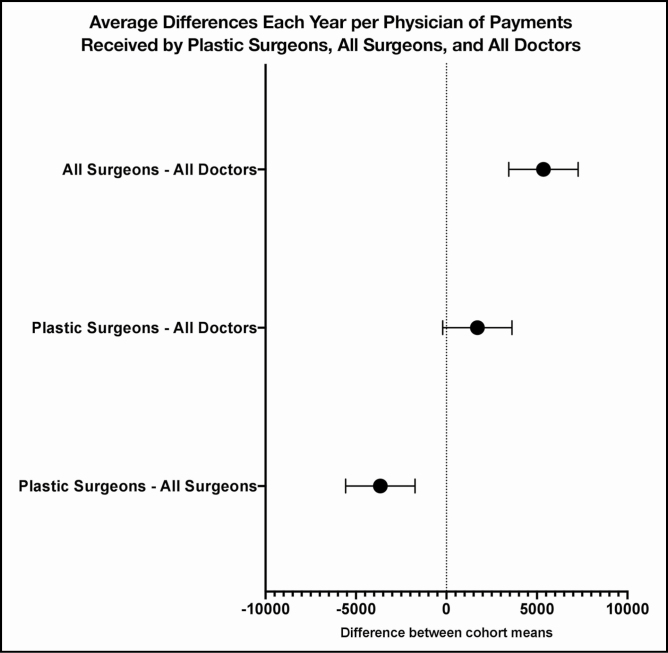
A yearly analysis was conducted for each of our 3 physician cohorts. Average payments received per cohort per year are demonstrated in Figures 1 and 2. Large SDs from the mean value were observed for each year across all cohorts. One-way analysis of variance indicated that statistically significant differences existed between the 3 cohorts (P ≤ 0.0001) (Figure 3). Tukey’s multiple comparisons test was conducted to directly compare the average amount received per physician in each cohort. Plastic surgeons received less than the all-surgeon cohort, with a mean difference of $3654 less each year per physician (P = 0.0005). All surgeons received more in industry payments than the all-doctors cohort, with a mean difference of $5361 more each year per physician (P ≤ 0.0001). The mean difference between the plastic surgery cohort and the all-doctors cohort was not significant (P = 0.0840) and is represented by an increase of $1707 received on average each year per physician in the plastic surgery cohort. In the first full 4 years after the enactment of the PPSA, average physician payments by year appeared to be stable among all surgeons and all doctors. Among plastic surgeons, there actually appeared to be a decline in payments between 2014 and 2015, after which average payments remained stable. The last 2 years of 2018 and 2019, however, appeared to witness an increase in physician payments across plastic surgery, all surgeons, and all doctors (Figure 1).
Figure 1.
Average payment received by plastic surgeons, all surgeons, and all doctors per year in US dollars. Error bars designate standard error of the mean.
Figure 2.
Average payment received by plastic surgeons, all surgeons, and all doctors by year in US dollars. Error bars designate standard deviation.
Figure 3.
Average of differences between payments received for plastic surgeons, all surgeons, and all doctors each year per physician.
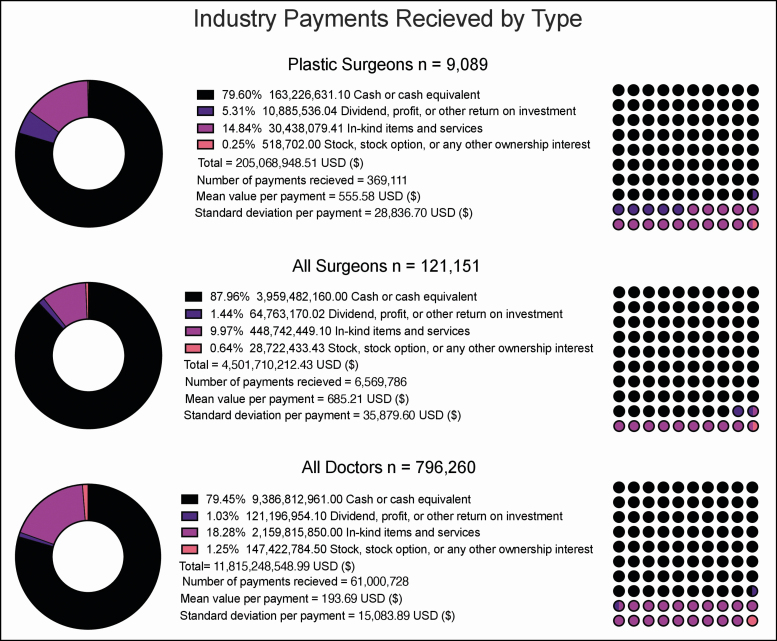
Totals by Payment Type
The CMS Open Payments database reports 4 major forms of payment. Payments made to physicians are labeled as (1) a cash or cash equivalent transfer; (2) a dividend, profit, or other return on investment; (3) in-kind items and or services; or (4) stock, stock option, or other types of ownership interest. Figure 4 and Table 1 depict industry payments made to physicians, organized based on the relative proportions of payment type. The plastic surgeons, all-surgeons, and all-doctors cohorts all received the majority payment in the form of cash or cash equivalents. Receiving payment in the form of stock or stock options was the least common for all cohorts.
Figure 4.
Industry payments made to plastic surgeons by category and by nature of transfer of value method.
Table 1.
Summary of Industry Payments Made to Surgeons, by Type and Year
| Cohort | Program year | Form of payment | Total USD received | Mean USD received per physician | Payments received, No. |
|---|---|---|---|---|---|
| Plastic surgeons | 2019 | Cash or cash equivalent | $40,766,712.52 | $3352.80 | 12,159 |
| Plastic surgeons | 2019 | In-kind items and services | $6,455,662.74 | $129.47 | 49,862 |
| Plastic surgeons | 2019 | Stock, stock option, or any other ownership interest | $173,053.00 | $34,610.60 | 5 |
| All surgeons | 2019 | Cash or cash equivalent | $797,970,217.41 | $2684.64 | 297,235 |
| All surgeons | 2019 | Dividend, profit or other return on investment | $9,793,312.65 | $89,846.91 | 109 |
| All surgeons | 2019 | In-kind items and services | $90,779,717.17 | $106.14 | 855,281 |
| All surgeons | 2019 | Stock, stock option, or any other ownership interest | $2,799,417.12 | $13,081.39 | 214 |
| All doctors | 2019 | Cash or cash equivalent | $1,746,049,535.90 | $1269.56 | 1,375,315 |
| All doctors | 2019 | Dividend, profit or other return on investment | $16,889,342.27 | $39,277.54 | 430 |
| All doctors | 2019 | In-kind items and services | $367,821,116.58 | $44.85 | 8,200,834 |
| All doctors | 2019 | Stock, stock option, or any other ownership interest | $17,872,187.74 | $54,158.14 | 330 |
| Plastic surgeons | 2018 | Cash or cash equivalent | $34,217,431.01 | $2522.48 | 13,565 |
| Plastic surgeons | 2018 | Dividend, profit or other return on investment | $10,458,768.15 | $5,229,384.08 | 2 |
| Plastic surgeons | 2018 | In-kind items and services | $8,251,494.75 | $177.74 | 46,424 |
| Plastic surgeons | 2018 | Stock, stock option, or any other ownership interest | $186,172.00 | $15,514.33 | 12 |
| All surgeons | 2018 | Cash or cash equivalent | $657,862,898.27 | $2227.42 | 295,347 |
| All surgeons | 2018 | Dividend, profit or other return on investment | $22,318,589.59 | $108,342.67 | 206 |
| All surgeons | 2018 | In-kind items and services | $94,078,528.66 | $117.36 | 801,628 |
| All surgeons | 2018 | Stock, stock option, or any other ownership interest | $3,368,118.04 | $25,908.60 | 130 |
| All doctors | 2018 | Cash or cash equivalent | $1,533,624,650.31 | $1129.76 | 1,357,475 |
| All doctors | 2018 | Dividend, profit or other return on investment | $26,550,547.88 | $94,485.94 | 281 |
| All doctors | 2018 | In-kind items and services | $422,728,601.92 | $48.97 | 8,632,539 |
| All doctors | 2018 | Stock, stock option, or any other ownership interest | $28,362,121.21 | $117,685.15 | 241 |
| Plastic surgeons | 2017 | Cash or cash equivalent | $23,206,126.92 | $1329.03 | 17,461 |
| Plastic surgeons | 2017 | Dividend, profit or other return on investment | $47.89 | $23.95 | 2 |
| Plastic surgeons | 2017 | In-kind items and services | $4,062,123.93 | $101.98 | 39,831 |
| Plastic surgeons | 2017 | Stock, stock option, or any other ownership interest | $12,907.00 | $12,907.00 | 1 |
| All surgeons | 2017 | Cash or cash equivalent | $640,446,677.28 | $2026.26 | 316,073 |
| All surgeons | 2017 | Dividend, profit or other return on investment | $5,010,348.22 | $13,802.61 | 363 |
| All surgeons | 2017 | In-kind items and services | $70,574,024.26 | $95.04 | 742,583 |
| All surgeons | 2017 | Stock, stock option, or any other ownership interest | $2,402,415.01 | $10,677.40 | 225 |
| All doctors | 2017 | Cash or cash equivalent | $1,556,254,053.06 | $1025.52 | 1,517,534 |
| All doctors | 2017 | Dividend, profit or other return on investment | $5,803,410.94 | $14,258.99 | 407 |
| All doctors | 2017 | In-kind items and services | $350,412,464.38 | $40.15 | 8,728,661 |
| All doctors | 2017 | Stock, stock option, or any other ownership interest | $18,607,963.77 | $58,332.17 | 319 |
| Plastic surgeons | 2016 | Cash or cash equivalent | $20,440,834.64 | $1584.68 | 12,899 |
| Plastic surgeons | 2016 | In-kind items and services | $4,549,418.93 | $85.50 | 53,209 |
| Plastic surgeons | 2016 | Stock, stock option, or any other ownership interest | $5300.00 | $5300.00 | 1 |
| All surgeons | 2016 | Cash or cash equivalent | $633,125,088.63 | $2096.57 | 301,981 |
| All surgeons | 2016 | Dividend, profit or other return on investment | $10,042,930.65 | $51,502.21 | 195 |
| All surgeons | 2016 | In-kind items and services | $70,730,546.44 | $90.43 | 782,165 |
| All surgeons | 2016 | Stock, stock option, or any other ownership interest | $8,718,913.56 | $47,385.40 | 184 |
| All doctors | 2016 | Cash or cash equivalent | $1,550,995,004.96 | $921.89 | 1,682,400 |
| All doctors | 2016 | Dividend, profit or other return on investment | $15,393,167.17 | $54,779.95 | 281 |
| All doctors | 2016 | In-kind items and services | $351,004,487.29 | $39.67 | 8,848,806 |
| All doctors | 2016 | Stock, stock option, or any other ownership interest | $23,935,231.75 | $81,969.97 | 292 |
| Plastic surgeons | 2015 | Cash or cash equivalent | $18,353,009.54 | $1547.86 | 11,857 |
| Plastic surgeons | 2015 | Dividend, profit or other return on investment | $426,720.00 | $213,360.00 | 2 |
| Plastic surgeons | 2015 | In-kind items and services | $4,045,222.81 | $73.20 | 55,261 |
| Plastic surgeons | 2015 | Stock, stock option, or any other ownership interest | $14,850.00 | $14,850.00 | 1 |
| All surgeons | 2015 | Cash or cash equivalent | $630,314,061.49 | $1942.15 | 324,544 |
| All surgeons | 2015 | Dividend, profit or other return on investment | $5,063,711.13 | $21,187.08 | 239 |
| All surgeons | 2015 | In-kind items and services | $61,246,286.33 | $81.44 | 752,007 |
| All surgeons | 2015 | Stock, stock option, or any other ownership interest | $2,275,456.19 | $17,238.30 | 132 |
| All doctors | 2015 | Cash or cash equivalent | $1,520,939,664.33 | $902.48 | 1,685,287 |
| All doctors | 2015 | Dividend, profit or other return on investment | $14,111,350.31 | $39,862.57 | 354 |
| All doctors | 2015 | In-kind items and services | $336,850,020.63 | $38.38 | 8,777,418 |
| All doctors | 2015 | Stock, stock option, or any other ownership interest | $13,599,062.73 | $55,963.22 | 243 |
| Plastic surgeons | 2014 | Cash or cash equivalent | $26,242,516.43 | $2023.32 | 12,970 |
| Plastic surgeons | 2014 | In-kind items and services | $3,074,156.25 | $70.53 | 43,586 |
| Plastic surgeons | 2014 | Stock, stock option, or any other ownership interest | $126,420.00 | $126,420.00 | 1 |
| All surgeons | 2014 | Cash or cash equivalent | $599,763,216.77 | $1829.97 | 327,745 |
| All surgeons | 2014 | Dividend, profit or other return on investment | $12,534,277.78 | $44,605.97 | 281 |
| All surgeons | 2014 | In-kind items and services | $61,333,346.27 | $79.57 | 770,828 |
| All surgeons | 2014 | Stock, stock option, or any other ownership interest | $9,158,113.51 | $100,638.61 | 91 |
| All doctors | 2014 | Cash or cash equivalent | $1,478,950,052.33 | $864.24 | 1,711,266 |
| All doctors | 2014 | Dividend, profit or other return on investment | $42,449,135.49 | $120,937.71 | 351 |
| All doctors | 2014 | In-kind items and services | $330,999,158.77 | $39.04 | 8,479,432 |
| All doctors | 2014 | Stock, stock option, or any other ownership interest | $45,046,217.27 | $194,164.73 | 232 |
Totals by Region
We analyzed trends in payment by geographic region. All states within the continental United States were considered. The results of this analysis are depicted in Supplemental Figure 1, which graphically represents the geographic variability in payments made to physicians across the country. The total payments received per physician per state were compiled from 2014 to 2019. We further analyzed the cohort of plastic surgeons. The summary statistics of mean, SD, and the number of plastic surgeon physicians who received payments in the state during the 6-year study are tabulated in Table 2. Tennessee received the most in industry payments per plastic surgeon physician between 2014 and 2019 (mean $76,420.75, SD $989,128.54, maximum $14,096,876.20, minimum $8.49, n = 203 physicians). Vermont received the least with a mean of $309.13 in payments per physician (SD $220.62, maximum $592.05, minimum $35.30, 5 physicians represented). California had the most plastic surgeons who received industry payments between 2014 and 2019 and who each on average received a mean of $48,153.22 ($48,153.22 per physician, SD = $1,436,839.58, maximum $54,726,972.93, minimum $2.88, n = 1452 physicians).
Table 2.
Industry Payments Made per State to Plastic Surgeons, 6-Year Averages (2014-2019)
| State | State abbreviation |
Total USD ($) received | Mean USD ($) received per physician | Standard deviation of USD ($) received per physician | Physicians, No. |
|---|---|---|---|---|---|
| Alaska | AK | $12,612.32 | $840.82 | $1493.45 | 15 |
| Alabama | AL | $428,167.75 | $3598.05 | $9906.55 | 119 |
| Arkansas | AR | $335,614.88 | $7295.98 | $21,655.08 | 46 |
| Arizona | AZ | $3,482,711.09 | $14,883.38 | $133,791.22 | 234 |
| California | CA | $69,918,477.80 | $48,153.22 | $1,436,839.58 | 1452 |
| Colorado | CO | $989,729.40 | $6468.82 | $28,222.02 | 153 |
| Connecticut | CT | $324,130.04 | $2552.21 | $11,522.72 | 127 |
| Washington DC | DC | $2,900,561.85 | $37,186.69 | $177,745.35 | 78 |
| Delaware | DE | $203,249.85 | $5645.83 | $23,087.19 | 36 |
| Florida | FL | $16,181,053.62 | $18,620.31 | $227,730.10 | 869 |
| Georgia | GA | $3,057,323.59 | $9126.34 | $40,570.74 | 335 |
| Hawaii | HI | $234,735.54 | $6018.86 | $15,115.13 | 39 |
| Iowa | IA | $153,790.57 | $2698.08 | $7843.62 | 57 |
| Idaho | ID | $123,752.96 | $3867.28 | $5679.54 | 32 |
| Illinois | IL | $9,726,309.62 | $24,255.14 | $190,756.07 | 401 |
| Indiana | IN | $969,523.27 | $5669.73 | $25,244.14 | 171 |
| Kansas | KS | $2,624,288.38 | $27,624.09 | $243,862.15 | 95 |
| Kentucky | KY | $5,766,242.34 | $33,330.88 | $262,976.89 | 173 |
| Louisiana | LA | $767,081.23 | $5113.87 | $16,767.87 | 150 |
| Massachusetts | MA | $1,993,516.55 | $6946.05 | $31,840.78 | 287 |
| Maryland | MD | $4,189,977.28 | $15,634.24 | $78,378.58 | 268 |
| Maine | ME | $55,074.38 | $1776.59 | $2915.07 | 31 |
| Michigan | MI | $4,436,205.02 | $12,602.86 | $78,909.34 | 352 |
| Minnesota | MN | $1,930,349.92 | $10,322.73 | $46,965.67 | 187 |
| Missouri | MO | $1,856,487.87 | $8002.10 | $34,127.98 | 232 |
| Mississippi | MS | $495,499.70 | $5898.81 | $19,465.80 | 84 |
| Montana | MT | $125,077.61 | $5685.35 | $11,246.83 | 22 |
| North Carolina | NC | $4,367,352.44 | $17,126.87 | $131,649.41 | 255 |
| North Dakota | ND | $94,020.83 | $3482.25 | $5775.18 | 27 |
| Nebraska | NE | $132,737.12 | $3587.49 | $6800.97 | 37 |
| New Hampshire | NH | $219,138.19 | $6261.09 | $21,985.01 | 35 |
| New Jersey | NJ | $2,200,581.07 | $6251.65 | $30,404.01 | 352 |
| New Mexico | NM | $308,907.81 | $7534.34 | $19,472.47 | 41 |
| Nevada | NV | $961,925.24 | $10,808.15 | $34,939.42 | 89 |
| New York | NY | $9,268,800.45 | $11,047.44 | $81,836.08 | 839 |
| Ohio | OH | $3,438,524.79 | $8727.22 | $48,218.01 | 394 |
| Oklahoma | OK | $1,037,041.17 | $12,646.84 | $51,279.13 | 82 |
| Oregon | OR | $460,722.64 | $4607.23 | $10,811.21 | 100 |
| Pennsylvania | PA | $5,304,475.10 | $11,005.14 | $72,172.44 | 482 |
| Rhode Island | RI | $273,141.85 | $5574.32 | $21,967.53 | 49 |
| South Carolina | SC | $490,869.06 | $3805.19 | $7625.22 | 129 |
| South Dakota | SD | $140,945.51 | $5637.82 | $7468.47 | 25 |
| Tennessee | TN | $15,513,412.32 | $76,420.75 | $989,128.54 | 203 |
| Texas | TX | $20,274,636.52 | $21,545.84 | $367,188.60 | 941 |
| Utah | UT | $422,155.22 | $3872.98 | $10,778.69 | 109 |
| Virginia | VA | $2,400,270.62 | $9126.50 | $45,359.91 | 263 |
| Vermont | VT | $1545.64 | $309.13 | $220.62 | 5 |
| Washington | WA | $2,841,528.70 | $17,432.69 | $111,073.55 | 163 |
| Wisconsin | WI | $1,149,713.61 | $7821.18 | $42,825.07 | 147 |
| West Virginia | WV | $456,854.15 | $10,152.31 | $40,286.55 | 45 |
| Wyoming | WY | $28,104.03 | $9368.01 | $8302.70 | 3 |
DISCUSSION
Transparent presentation of industry-based physician reimbursement is important in maintaining patient-centered care. Although advancing medical and surgical practices is in the best interest of improving patient care, such efforts are often inconsistently financially supported. In their review of the nuances of surgical innovation, Riskin et al stress the importance of understanding these potentially competing forces while emphasizing that when done appropriately, commercialization by means of industry-physician relationships can help foster advancements in patient care.19 A recent 2018 survey taken by members of the American Society of Plastic Surgeons confirmed that although 75% of individuals acknowledged receipt of recent gifts from industry, they in turn contend that such reimbursement has no influence on their clinical practice.20 Directly industry-sponsored research or indirect sponsorship of research investigators in specialized fields represent complex scenarios in which study results must be interpreted through the lens of potential author financial conflict.21
Equally as important as the influence industry reimbursement can have on physician decision making is how patients react to the knowledge of these financial relationships. Although data reflecting patient opinion is limited, 1 recent study concluded that among plastic surgery patients, older and educated individuals endorsed increased transparency concerning potential conflict of interest as it related to their clinical care. However, 81% of respondents were unaware of the PPSA prior to study participation.22 Although multiple survey studies have been conducted to further evaluate public opinion, Camp et al concluded that physician disclosure and systematic oversight of these relationships would positively influence the ability to maintain trusting relationships between physicians and patients.23-26,27 Doing so would ultimately still allow medical professionals to collaborate with industry to improve patient care.28 Our study evaluated the amount, form, and geographic distribution of payments made to plastic surgeons in the United States between 2014 and 2019. Overall, this study characterized and accounted for 796,260 doctors, who received 61,000,728 payments from 2014 through 2019, totaling $11,815,248,549. Of these doctors, 9089 were practicing plastic surgeons, whose payments accounted for 369,111 totaling $205,068,949. We then compared payments made to plastic surgeons with those received by all surgeons (n = 121,151) and all physicians (n = 796,260).
Previous reports have concluded that the top payors to physicians include suppliers of surgical equipment; therefore, it is not unreasonable to surmise that those specialties who rely more heavily on such devices would receive a greater share of overall reimbursement.29 On average, plastic surgeons receive $3654 less per year than all surgeons (P = 0.0005), whereas they receive $1707 more per year than all payment-receiving doctors (P = 0.0840). One could hypothesize that these payments are directly proportionate to the cost of certain medical devices, surgical instrumentation, or pharmaceutical products. Examples of successful clinical and scientific collaboration with plastic surgeons are pervasive among the mesh, injectable, and implant industries, where effective product development has benefited from mutual feedback between company research and development teams and external consultants. Venture capitalism also represents a source of support for entrepreneurial plastic surgeons in a field known for creativity.30 Of note, the average dollar amount received in each cohort had large SDs, which corroborates the large variability in payments received by each physician.
Interestingly, the trend for payments made to plastic surgeons mirrored those observed for the all-doctors cohort from 2014 to 2017, albeit with larger SDs. However, in 2018 and 2019, the mean received per plastic surgeon and the SD of these means substantially increased. Specifically, in 2017 plastic surgeons received on average $4485 ± $89,141 (n = 6083), which in 2018 increased to $8827 ± $255,657 (n = 6017). The observed increase persisted through 2019. These trends can be observed in Figure 1.
Without any evidence of causation, one can only speculate as to the reason for these changes. To the best of the authors’ knowledge, there was no major legislative or reimbursement policy changes during that time. One explanation for this observation could be related to an initial reduction in industry payments after the PPSA was enacted in 2013 over concerns of public optics; thereafter, a subsequent period of industry “relaxation” could explain the resurgence in industry payments. This finding is corroborated by the increases observed in the all-surgeons and all-doctors cohorts during this same time period. It is unclear the extent to which the trend in the all-surgeons cohort drove the same observation among the all-inclusive doctors cohort. Unfortunately, this study lacks the granularity necessary to conclude that a “relaxation” of industry compensations is associated with these observed increases, and our explanation should be regarded as speculative.
Our analysis showed that cash or cash equivalent transfers dominated as the main form of compensation. Among plastic surgeons, all surgeons, and all doctors, over 75% of industry payments were cash based. In aggregate, cash transactions totaled $9,386,812,961, or 79.5% of $11,815,248,549 over this 6-year period. This trend was observed among plastic surgeons, with cash transactions totaling $163,226,631, or 79.6% of $205,068,949. Stock holdings and partial ownership stakes in a company represented the least frequent form of payment. Payment of this form represented 0.25% of total transferred assets.
Analysis of geographic payment distribution within the United States was made difficult by the large variability in physician density in each state. To quantify these measures, the total sum of payments received in a specific state over a defined period of time was divided by the total number of physicians who received payment in that state. These “state-level averages” are depicted in Supplemental Figure 1. An interactive map that contains all state-wide data metrics can be viewed by visiting the https://public.tableau.com/profile/rowland.pettit. It is clear that state-level averages vary over time for all cohorts. Despite this variability, the overall shading of the continental United States from year to year remains consistent, demonstrating geographic consistency over time.
When looking at plastic surgeon reimbursement, one sees that California was consistently responsible for a large proportion of total physician payments. The initial explanation for this finding is that California has a disproportionally higher number of practicing plastic surgeons who received industry payments compared with other states (n = 1452). However, after adjusting for this variable by calculating the average payment received per physician, California and Tennessee plastic surgeons consistently received higher average payments during all 6 years of this study.
Previous studies of industry payments made to plastic surgeons as recorded by the PPSA have adopted differing analytic perspectives utilizing more cross-sectional data.31-33 In 2016, Chao et al captured similar data and included total compensation received by plastic surgeons, type of compensation, and a geographic sub-analysis. Although thorough, the analysis only reviewed data from 1 year (2014), making it difficult to assess payment trends over time.31 A comparable study, by Ahmed et al, looked at similar metrics to our study but captured data from a 5-month period.33 The authors found that those in private practice received greater amounts of financial reimbursement compared with those in academics. However, with academic practices, h-index, which is utilized to measure one’s academic productivity, was positively correlated with higher financial payments.33 Our study represents the only comprehensive analysis, to our knowledge, that includes all data across the time period since implementation. Other similarly structured reports, which characterize single-specialty payments, have primarily focused on orthopedic surgery.7,34 Garstka et al report a broad, 2-year analysis of payments made to all physicians, which includes surgical and non-surgical specialties.29 With over 6 years of data now available, older studies should be revised to reflect the latest trends in industry payments.
This study is not without limitations. It is federally mandated that to be in accordance with the PPSA, industry payments must be reported and recorded in the Open Payments database. However, payments that were not reported to the federal Open Payments database could not be accounted for in this analysis. There is limited pre-release vetting that occurs to validate or remove errors before the Open Payments data is nationally published, strengthening this limitation.33 Beyond geography, practice types and settings were not accessible. Although broadly informative, these limitations prevent these results from having direct actionable utility. Without physician payment data predating the Open Payment database, it is not possible to measure the short-term effect of the PPSA on financial relationships between industry and doctors. However, continued monitoring of long-term trends at the individual, specialty, and global levels should allow for internal assessment and self-regulation as needed.
CONCLUSIONS
We aimed to characterize potential changes in physician, surgeon, and plastic surgeon payments from industry during the 6 years since implementation of the PPSA. We present the first comprehensive temporal trend investigation of this information from the Open Payments database pertaining to plastic surgeons, to our knowledge, contextualized against the background of corresponding data associated with all surgeons and doctors. We found that plastic surgeons received more per year on average than all physicians but less than surgeons in general. Across all cohorts, the majority of payments were completed through cash transactions. We found that per state, related trends remained largely consistent with regard to industry payments between 2014 and 2019. Further work is warranted to more specifically compare industry-related payments outside of the field of plastic surgery, for example between plastic surgeons and each of the other surgical disciplines. Such investigation would further frame how plastic surgeons compare with other similarly performing physicians.
Supplementary Material
Disclosures
Dr Offodile reports research funding from Blue Cross Blue Shield Affordability Cures Research Consortium (Richardson, TX), University Cancer Foundation (Houston, TX), and the National Academy of Medicine (Washington, DC); all are unrelated to the submitted work. Dr Offodile is also a board member of the Patient Advocate Foundation (Hampton, VA). Dr Kumar serves as a consultant to Synthes (West Chester, PA) and is a recipient of grant funding from KLS Martin (Jacksonville, FL). He was previously a consultant for Polarity TE (Salt Lake City, UT). Mr Pettit is supported by a fellowship from the Training in Precision Environmental Health Sciences (TPEHS) Program (NIH Grant No. T32ES027801, Bethesda, MD); Mr Pettit would like to thank the Baylor Research Advocates for Student Scientists (Houston, TX) for their funding support. The remaining authors declared no potential conflicts of interest with respect to the research, authorship, and publication of this article.
Funding
The authors received no financial support for the research, authorship, and publication of this article.
REFERENCES
- 1.Agrawal S, Brown D. The Physician Payments Sunshine Act–two years of the Open Payments Program. N Engl J Med. 2016;374(10):906-909. [DOI] [PubMed] [Google Scholar]
- 2.Agrawal S, Brennan N, Budetti P. The Sunshine Act–effects on physicians. N Engl J Med. 2013;368(22):2054-2057. [DOI] [PubMed] [Google Scholar]
- 3.Saver RS. Shadows amid sunshine: regulating financial conflicts in medical research. Chest. 2014;145(2):379- 385. [DOI] [PubMed] [Google Scholar]
- 4.Bengtson BP. Shedding some light on the sunshine act. Aesthet Surg J. 2015;35(5):NP129-NP130. [DOI] [PubMed] [Google Scholar]
- 5.Kirschner NM, Sulmasy LS, Kesselheim AS. Health policy basics: the Physician Payment Sunshine Act and the Open Payments Program. Ann Intern Med. 2014;161(7):519-521. [DOI] [PubMed] [Google Scholar]
- 6.Richardson E, Brookings I. Health policy brief: The Physician Payments Sunshine Act. Health Aff. October 2, 2014. [Google Scholar]
- 7.Cvetanovich GL, Chalmers PN, Bach BR Jr. Industry financial relationships in orthopaedic surgery: analysis of the Sunshine Act Open Payments database and comparison with other surgical subspecialties. J Bone Joint Surg Am. 2015;97(15):1288-1295. [DOI] [PubMed] [Google Scholar]
- 8.Kim SY, Millard RW, Nisbet P, Cox C, Caine ED. Potential research participants’ views regarding researcher and institutional financial conflicts of interest. J Med Ethics. 2004;30(1):73-79. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Licurse A, Barber E, Joffe S, Gross C. The impact of disclosing financial ties in research and clinical care: a systematic review. Arch Intern Med. 2010;170(8):675-682. [DOI] [PubMed] [Google Scholar]
- 10.Volk AS, Kaplan J, Izaddoost SA, Reece EM, Winocour S. Advertising or education: biomedical industry and interactions with residents. Plast Reconstr Surg. 2019;144(6): 1134e-1135e. [DOI] [PubMed] [Google Scholar]
- 11.Rhee TG, Stanic T, Ross JS. Impact of US industry payment disclosure laws on payments to surgeons: a natural experiment. Res Integr Peer Rev. 2020;5:1. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 12.Fazendin JM, Corey BL, Heslin MJ, Chen H. Analysis of open payments receipts among surgical faculty at a large academic institution. J Surg Res. 2019;244:599-603. [DOI] [PubMed] [Google Scholar]
- 13.Campbell E, Gruen R, Mountford J, Miller LG, Cleary PD, Blumenthal D.. A National Survey of Physician–Industry Relationships. N Engl J Med. 2007;1742-1750. [DOI] [PubMed] [Google Scholar]
- 14.R Core Team. R: a language and environment for statistical computing. R Found Stat Comput. 2020. https://www.r-project.org/. Accessed October 26, 2020.
- 15.Wickham H, François R, Henry L, Müller K. dplyr: A Grammar of Data Manipulation. 2020. https://cran.r-project.org/package=dplyr. Accessed October 26, 2020.
- 16.Hadley W, Henry L. tidyr: Tidy Messy Data. 2020. https://cran.r-project.org/package=tidyr. Accessed October 26, 2020.
- 17.Hadley W. stringr: Simple, Consistent Wrappers for Common String Operation. 2019. https://cran.r-project.org/package=stringr. Accessed October 26, 2020.
- 18.Tableau Core Team. Tableau Software. 2020. http://www.tableausoftware.com/products/desktop/specs. Accessed October 26, 2020.
- 19.Riskin DJ, Longaker MT, Gertner M, Krummel TM. Innovation in surgery: a historical perspective. Ann Surg. 2006;244(5):686-693. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Purvis TE, Lopez J, Milton J, May JW Jr, Dorafshar AH. Plastic surgeons’ perceptions of financial conflicts of interest and the sunshine act. Plast Reconstr Surg Glob Open. 2018;6(4):e1733. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21.Lopez J, Samaha G, Purvis TE, et al. The accuracy of conflict-of-interest disclosures reported by plastic surgeons and industry. Plast Reconstr Surg. 2018;141(6):1592-1599. [DOI] [PubMed] [Google Scholar]
- 22.Lopez J, Naved BA, Pradeep T, et al. What do plastic surgery patients think of financial conflicts of interest and the sunshine act? Ann Plast Surg. 2019;82(6):597-603. [DOI] [PubMed] [Google Scholar]
- 23.Volk AS, Kaplan J, Reece EM, Winocour S. Are surgical consents an ideal platform for disclosing conflicts of interests to patients? Plast Reconstr Surg. 2019;144(5):954e. [DOI] [PubMed] [Google Scholar]
- 24.Camp MW, Mattingly DA, Gross AE, Nousiainen MT, Alman BA, McKneally MF. Patients’ views on surgeons’ financial conflicts of interest. J Bone Joint Surg Am. 2013;95(2):e91-e98. [DOI] [PubMed] [Google Scholar]
- 25.Khan MH, Lee JY, Rihn JA, et al. The surgeon as a consultant for medical device manufacturers: what do our patients think? Spine (Phila Pa 1976). 2007;32(23):2616-2618; discussion 2619. [DOI] [PubMed] [Google Scholar]
- 26.DiPaola CP, Dea N, Noonan VK, Bailey CS, Dvorak MF, Fisher CG. Surgeon-industry conflict of interest: survey of North Americans’ opinions regarding surgeons consulting with industry. Spine J. 2014;14(4):584-591. [DOI] [PubMed] [Google Scholar]
- 27.Camp MW, Mattingly DA, Gross AE, Nousiainen MT, Alman BA, McKneally MF. Patients’ views on surgeons’ financial conflicts of interest. J Bone Joint Surg Am. 2013;95(2):e9 1-e9 8. [DOI] [PubMed] [Google Scholar]
- 28.Camp MW, Gross AE, McKneally MF. Patient views on financial relationships between surgeons and surgical device manufacturers. Can J Surg. 2015;58(5):323-329. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 29.Garstka ME, Monlezun D, DuCoin C, Killackey M, Kandil E. The Sunshine Act and surgeons: a nation-wide analysis of industry payments to physicians. J Surg Res. 2019;233:41-49. [DOI] [PubMed] [Google Scholar]
- 30.Jalalabadi F, Grome L, Shahrestani N, Izaddoost SA, Reece EM. Entrepreneurial strategies to seek venture capital funding. Semin Plast Surg. 2018;32(4):179-181. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Chao AH, Gangopadhyay N. Industry financial relationships in plastic surgery: analysis of the sunshine act open payments database. Plast Reconstr Surg. 2016;138(2):341e-348e. [DOI] [PubMed] [Google Scholar]
- 32.Luce EA. Financial conflicts of interest in plastic surgery: background, potential for bias, disclosure, and transparency. Plast Reconstr Surg. 2015;135(4):1149-1155. [DOI] [PubMed] [Google Scholar]
- 33.Ahmed R, Lopez J, Bae S, et al. The dawn of transparency: insights from the Physician Payment Sunshine Act in plastic surgery. Ann Plast Surg. 2017;78(3):315-323. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 34.Samuel AM, Webb ML, Lukasiewicz AM, et al. Orthopaedic surgeons receive the most industry payments to physicians but large disparities are seen in Sunshine Act data. Clin Orthop Relat Res. 2015;473(10):3297-3306. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.