Number of working hours, work-related psychological demands, and use of lumbar support moderate the beneficial effects of preventive interventions for neck and low back pain.
Keywords: Active break, Postural shift, Moderator, Neck pain, Low back pain, Sedentary worker
Abstract
Introduction:
Neck and low back pain are significant health problem in sedentary office workers. Active break and postural shift interventions has been proved to reduce the incidence of new onset of both neck and low back pain.
Objectives:
To identify variables that moderate the effects of active breaks and postural shift interventions on the development of neck and low back pain in office workers.
Methods:
Using data from a 3-arm (active break, postural shift, and control group) cluster randomized controlled trial (N = 193), we evaluated the moderating effects of age, job position, education level, sex, perceived psychological work demands, number of working hours, and using a chair with lumbar support on the benefits of 2 interventions designed to prevent the development of neck and low back pain in office workers. Moderation analyses were conducted using the Hayes PROCESS macro, with post hoc Johnson–Neyman techniques and logistic regressions.
Results:
Significant interactions between intervention groups and 3 moderators assessed at baseline emerged. For the prevention of neck pain, the effect of the active break intervention was moderated by the number of working hours and the effect of the postural shift intervention was moderated by the level of perceived psychological work demands and the number of working hours. For the prevention of low back pain, the effect of postural shift intervention was moderated by having or not having a chair with lumbar support.
Conclusions:
The study findings can be used to help determine who might benefit the most from 2 treatments that can reduce the risk of developing neck and low back pain in sedentary workers and may also help us to understand the mechanisms underlying the benefits of these interventions.
1. Introduction
Neck and low back pain are common in sedentary office workers. One-year prevalence rates for neck and low back pain among office workers have been shown to range from 42% to 69%1,16 and 31% to 51%,2,39 respectively. Although improvement of neck and low back symptoms can occur,22,28 the 1-year recurrence rate of neck and low back pain has been shown to range from 23% to 69%.9,12 Moreover, 17% and 27% of office workers who report a new onset of neck and low back pain report that these pain problems become chronic, respectively.38 Given that chronic pain represents a leading cause of disability worldwide17 and continues to be a major economic burden to society,10 identifying effective strategies to prevent neck and low back pain is of high importance. Moreover, identifying the individuals who would benefit the most from preventive treatments could improve the effectiveness and efficiency of treatment because this information could be used to inform better individual-treatment matching.
There is evidence supporting the effectiveness of exercise programs for reducing the risk of new episodes of neck pain13 and that exercise combined with education reduces the risk of subsequent episodes of low back pain.41 Research has also found that an intervention to increase daily walking steps reduced onset neck pain in high-risk office workers.40 Recently, we found that 2 interventions—one an active break and the second a postural shift intervention—reduced the incidence of new onset of both neck and low back pain.45 Both interventions were delivered by a custom-designed apparatus and were aimed to minimize seat discomfort by providing (1) recommendations for taking breaks (active break intervention) or (2) making postural shifts during prolonged sitting (postural shift intervention). However, in the primary outcome article, we did not conduct analyses to identify the moderators of treatment effects. Such research is important for being able to determine who might benefit the most from these interventions.
A systematic review found that the variables with strong evidence for moderating response to low back pain treatments (including cognitive-behavioral therapy, acupuncture, and manipulation combined with exercise) were age (younger participants may gain more benefits), employment status (those who were employed benefited more), occupation type (those in sedentary occupations benefited more), back pain severity (those who have worse initial back pain status benefited more), opioid medication use (those reporting less opioid use benefited more), treatment expectation (those with a greater positive expectations benefited more), and education level (those with greater than 10 years of schooling benefited more).18 Potential moderators with weaker evidence included sex, baseline psychological distress, baseline pain intensity, and baseline disability level.18 Another study reported that individuals with low back pain with high levels of fear avoidance were more likely to benefit from an educational booklet and an exercise program than were those with lower baseline levels of fear avoidance.25
To the best of our knowledge, no research has sought to identify the moderators of strategies to prevent neck and low back pain in office workers. To address this knowledge gap, here we used data from a completed randomized clinical trial45 to evaluate the moderation effects of different variables on the impact of the active break and postural shift interventions on the development of neck and low back pain. Given previous research and theory, we hypothesized that an active break intervention and postural shift approach would be more likely to reduce the risk of developing neck and low back pain in (1) younger participants than older participants, (2) general office workers than office managers, (3) participants with higher than a bachelor's degree than a bachelor's degree or lower, (4) female than male workers, and (5) those endorsing more psychological work demands than those endorsing fewer psychological work demands. In exploratory analyses, we also evaluated the potential moderating effects of a number of variables that have not yet been examined in previous research. Based on the available evidence regarding the predictors of neck or low back pain, we included baseline measures of chair height adjustability and the number of working hours as potential moderators of onset of neck pain7,34 and baseline measures of years of work experience, whether or not the participant engages in continuous standing for >2 hours/d, having a job that requires frequent trunk forward bending, and whether or not the worker's chair has lumbar support23 as potential moderators for the effects of the active treatments on the development of low back pain.
2. Materials and methods
2.1. Participants and procedures
The data for the analyses presented here came from a trial comparing the effects of active break and postural shift interventions designed to reduce the incidence of neck and low back pain, relative to no treatment, in office workers.45 Both the active break and postural shift interventions used a custom-designed apparatus, which consisted of 3 components: (1) a seat pad, (2) a processor, and (3) a smartphone application. The seat pad collected sitting behavior data, including the duration of any sitting breaks and the number of postural shifts. Data were stored in the processor and were used to compute recommended break durations and the number of postural shifts for each individual. For those in the active break intervention, instructions to take breaks were sent from the processor to the smartphone application. For those in the postural shift intervention, recommended postural shifts were induced by the apparatus gradually pumping air into various parts of the seat pad placed underneath a participant's buttocks. Commands to operate the seat pad were sent from the processor to the seat pad through a cord that connected them.
The study was a 3-arm, parallel group, cluster randomized controlled trial conducted using a convenience sample of 193 office workers who were at risk of developing nonspecific neck or low back pain. Details about the trial are available in the previous publication.45 The protocol was registered with the Thai Clinical Trials Registry (https://www.thaiclinicaltrials.org) (TCTR20190111002) and approved by the Chulalongkorn University Human Ethics Committee. Two eligibility criteria were adjusted subsequent to trial registration: (1) age (from 23–45 to 23–55 years) and (2) time needed to be pain free (from 12 to 6 months).
2.2. Descriptive variables
Baseline descriptive data were collected using a questionnaire assessing age, sex, height and weight (from which BMI was computed), education level, frequency of exercise, and smoking status. Work-related characteristics included job position, number of working hours, years of work experience, time per day spent using a computer, average number of hours/day of continuous standing and continuous sitting, whether work involved frequently engaging in 5 specific activities (ie, head extensions, head flexions, head rotations, trunk bending, and trunk rotations), and having or not having regular rest breaks. The questionnaire also asked participants to note different aspects of the ergonomics of their workstations and their work environments (ie, whether the desk height, computer screen level, position of a keyboard and mouse were suitable and whether or not the office had a comfortable air temperature, level of light brightness, and was well-ventilated).
Baseline neck and low back discomforts were assessed using the Borg CR-10 scale, which asked participants to rate the amount of perceived discomfort they felt in the past year in their neck and low back on 0 to 10 scales, with 0 = “no discomfort” and 10 = “extreme discomfort.”4 Discomfort was defined as the nonpainful but still uncomfortable feelings and sensations, such as tension, fatigue, or tremors,19 assessed using a body chart based on the modified Nordic questionnaire.27
2.3. Criterion variables: development of neck or low back pain
The 2 criterion variables in the current secondary analyses were new onset of nonspecific neck or low back pain, with or without radiation and without a disease identified as the underlying cause of the complaints at the first episode of pain during the 12-month follow-up period using a monthly diary.5,26 To assess this, the participants answered the question, “Have you experienced any neck or low back pain lasting >24 hours during the past month?” If they answered “yes,” a follow-up question about pain intensity measured using a visual analogue scale was asked, and the presence of weakness or numbness in the upper or lower limb was assessed. Those who (1) answered “yes” to the first question,14 (2) reported pain intensity >30 mm on a100-mm visual analogue scale,42 and (3) had no weakness or numbness in the upper or lower limbs (ie, to exclude symptoms more likely to be due to a serious medical conditions of neck or low back pain) were identified as cases.
2.4. Potential moderators
The potential moderators were classified into confirmatory or exploratory moderator variables. Moderators included in the confirmatory analyses were those for which we had a specific a priori hypothesis, based on previous evidence. Moderators classified as exploratory were those that have not yet been evaluated or for which a specific theory or mechanism is lacking.
The Descriptive Variables section above described the 4 confirmatory moderators (age, sex, job position, and education level). The fifth confirmatory variable was the level of psychological work demands. This variable was assessed using the 12-item Psychological Work Demands subscale of the Thai version of the Job Content Questionnaire.35 The internal consistency of this scale in the current sample was adequate (Cronbach alpha = 0.69).
Exploratory moderators of the neck pain onset included chair adjustability and number of working hours.7,34 Exploratory moderators of the low back pain onset included years of work experience and whether or not the participant (1) engages in continuous standing for >2 hours/day vs ≤2 hours/day, (2) describes themselves as needing to bend their trunk forward often during the work day, and (3) has a chair with lumbar support.23
2.5. Statistical analysis
Descriptive statistics were computed to describe the sample. All analyses followed an intention-to-treat approach (ie, last observation carried forward method). To estimate the associations between the potential moderators and the subsequent onset of nonspecific neck and low back pain in a cohort of office workers, analyses included the Hayes PROCESS 4.0 macro (model 1) in SPSS version 25 with 5000 bootstrapped samples (IBM SPSS; Preacher & Hayes, 2008). The analyses examined the interactions between the proposed moderators (ie, age, sex, job position, education level, and level of psychological work demands) and the treatment groups (active break, postural shift, and control) on the onset of neck and low back pain criterion variables (dichotomous). During March 2020, the COVID-19 outbreak occurred in Thailand. At the time, a majority of the study participants (68%) were required to work from home and did not bring the custom-designed apparatus or placebo foam pad home with them. Thus, status of working from home (yes/no) during the study was included as a covariate. Moreover, we controlled for the preintervention discomfort level on the dependent variables by using them as covariates to account for individual response tendencies and within-person variability. Treatment condition (ie, intervention groups and control group) was entered as 2 dummy coded variables. Potential moderators were also entered (1 per model tested), as was the Group × Moderator interaction.
To describe any significant moderations found, post hoc analysis was used including pairwise comparisons (ie, active break vs control group, postural shift vs control group, and active break vs postural shift) through PROCESS model 1 with the Johnson–Neyman technique and logistic regression analysis (an alpha level of 0.05). All statistical analyses were performed using SPSS for Windows version 25.0 (SPSS Inc, Chicago, IL). The regression models were constructed using the PROCESS macro version 4.0 (Andrew F. Hayes) for SPSS. Statistical significance was set at the 5% level and 95% CI.
3. Results
3.1. Sample description and general results of the moderator analyses
The trial spanned June 2019 to November 2020. The final sample included 193 office workers with a mean age of 33.8 (SD = 6.3) years. Most of the office workers were women (76%). Additional details regarding the demographic characteristics of the study participants are presented in Table 1.
Table 1.
Descriptive characteristics of the study participants.
| Characteristic | Active break (n = 47) | Postural shift (n = 46) | Control (n = 100) | P |
|---|---|---|---|---|
| Demographic characteristics | ||||
| Age (y) | 31.6 (6.1) | 35.0 (7.7) | 34.1 (5.3) | 0.008* |
| Sex: Female (%) | 33 (70.2) | 35 (74.5) | 79 (79.0) | NS |
| BMI | 21.3 (2.3) | 22.3 (2.3) | 21.0 (2.0) | 0.002* |
| Education: higher than a bachelor's degree (%) | 44 (95.7) | 45 (95.7) | 95 (95) | NS |
| Smoking status: No (%) | 38 (80.9) | 42 (91.3) | 91 (91) | NS |
| Exercise frequency in the past 12 mo: Regularly (%) | 7 (14.9) | 10 (21.8) | 22 (22.0 | NS |
| Job position: Manager level (%) | 45 (95.7) | 44 (95.7) | 95 (95) | NS |
| Baseline neck discomfort measured by the Borg CR-10 scale | 1.5 (1.2) | 1.3 (1.1) | 1.9 (1.6) | NS |
| Baseline low back discomfort measured by the Borg CR-10 scale | 2.9 (2.2) | 2.2 (2.2) | 3.7 (2.4) | 0.001* |
| Work-related characteristics | ||||
| Number of working hours (per day) | 8.0 (1.3) | 8.7 (1.3) | 7.8 (0.8) | NS |
| Year of work experience (y) | 6.9 (4.3) | 10.8 (5.3) | 9.1 (4.8) | <0.001* |
| Chair adjustability: Yes (%) | 46 (97.9) | 43 (93.5) | 64 (64) | <0.0001* |
| Continuous standing > 2 hours: No (%) | 43 (91.5) | 45 (97.8) | 94 (94) | NS |
| Having or not having lumbar support: Yes (%) | 20 (54.1) | 16 (39.0) | 43 (43) | NS |
| Often bending trunk forward: No (%) | 36 (76.6) | 37 (80.4) | 78 (78) | NS |
| Psychosocial characteristics | ||||
| Psychological job demands | 30.8 (4.4) | 32.5 (4.2) | 33.2 (4.4) | 0.009* |
P < 0.05.
Three moderators, 1 from the list of confirmatory moderators and 2 from the list of exploratory moderators, emerged as significant. Table 2 presents the results of all tests of confirmatory and exploratory moderations.
Table 2.
Results of analysis of preventive treatment (ie, active break and postural shift) effects.
| Moderator | Onset of neck pain | Onset of low back pain | ||||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Estimate | SE | Effect size (f2) | 95% CI | P | Estimate | SE | Effect size (f2) | 95% CI | P | |
| Active break vs postural shift vs control (n = 193) | ||||||||||
| Confirmatory moderators | ||||||||||
| Age | 0.07 | 0.04 | 0.11 | −0.01 to 0.16 | 0.096 | 0.01 | 0.05 | 0.05 | −0.78 to 0.1 | 0.840 |
| Sex | −0.38 | 0.64 | 0.11 | −1.13 to 1.23 | 0.929 | 14.43 | 711.13 | 0.06 | −1379.3 to 1408.2 | 0.984 |
| Job position | −0.87 | 0.59 | 0.11 | −2.04 to 0.31 | 0.147 | 1.05 | 0.70 | 0.05 | −0.32 to 2.41 | 0.136 |
| Education | −0.55 | 0.96 | 0.10 | −2.44 to 1.34 | 0.568 | 14.81 | 633.57 | 0.04 | −1226.9 to 1256.6 | 0.981 |
| Level of work psychological demands | −0.12 | 0.06 | 0.14 | -0.25 to −0.05 | 0.048* | -0.00 | 0.63 | 0.07 | −0.13 to 0.12 | 0.650 |
| Exploratory moderators for neck pain | ||||||||||
| Chair adjustability | 1.16 | 0.74 | 0.11 | −0.29 to 2.61 | 0.119 | |||||
| Number of working hours | −0.69 | 0.34 | 0.17 | −1.35 to −0.03 | 0.040* | |||||
| Exploratory moderators for low back pain | ||||||||||
| Years of work experience | 0.05 | 0.05 | 0.06 | −0.44 to 0.13 | 0.323 | |||||
| Continuous standing | -0.76 | 1.29 | 0.04 | −3.29 to 1.76 | 0.554 | |||||
| Not having lumbar support | −1.97 | 0.66 | 0.09 | −3.27 to −0.67 | 0.003* | |||||
| Often bending trunk forward | -0.38 | 0.65 | 0.04 | −1.65 to 0.89 | 0.556 | |||||
| Active break vs control (n = 147) | ||||||||||
| Level of work psychological demands | −0.73 | 0.11 | 0.14 | −0.29 to 0.14 | 0.051 | 0.05 | 0.15 | 0.09 | −0.23 to 0.34 | 0.703 |
| Number of working hours | −1.39 | 0.55 | 0.26 | −2.47 to −0.32 | 0.010* | |||||
| Not having lumbar support | -0.64 | 1.45 | 0.19 | −3.48 to 2.21 | 0.635 | |||||
| Postural shift vs control (n = 146) | ||||||||||
| Level of work psychological demands | −0.146 | 0.07 | 0.14 | −0.28 to −0.01 | 0.030* | -0.03 | 0.06 | 0.05 | −0.14 to 0.08 | 0.650 |
| Number of working hours | −0.69 | 0.32 | 0.11 | −1.33 to −0.05 | 0.033* | |||||
| Not having lumbar support | −2.09 | 0.69 | 0.11 | −3.44 to −0.74 | 0.003* | |||||
| Active break vs postural shift (n = 93) | ||||||||||
| Level of work psychological demands | −1.69 | 0.14 | 0.05 | −0.45 to 0.11 | 0.241 | -0.11 | 0.17 | 0.02 | −0.44 to 0.23 | 0.532 |
| Number of working hours | 0.12 | 0.53 | 0.09 | −0.93 to 1.17 | 0.820 | |||||
| Not having lumbar support | −3.14 | 1.81 | 0.00 | −6.69 to 0.41 | 0.095 | |||||
P < 0.05.
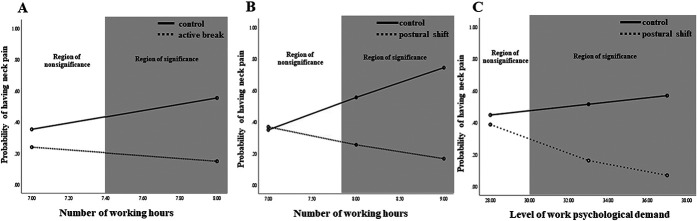
3.2. Number of working hours/day as a moderator
The analysis for the onset of neck pain revealed a significant Treatment Group X Number of Working Hours/Day interaction (B = −0.69, SE =0.34, R2 = 0.33, P =0.040; Fig. 1). Post hoc comparisons indicated a difference between the active break vs control group (B = −0.39, SE = 0.55, R2 = 0.44, P = 0.010) and postural shift vs control group (B = −0.69, SE = 0.32, R2 = 0.37, P = 0.033); participants who reported working more hours/day at baseline gained more benefits from both interventions, compared with those in the control group. Johnson–Neyman results indicated that participants in the active break group who reported working >7.4 hours/day, and participants in the postural shift group who reported working >7.8 hours/day, were more likely to benefit from the interventions to prevent the onset of neck pain in comparison to the control group, who also worked these hours at baseline (Fig. 2A and B). Logistic regressions analyzing within-treatment conditions indicated that the number of hours of work per day was a significant predictor of neck pain for the active break (B = −0.6, SE = 0.28, OR = 0.55, 95% CI 0.32–0.95, R2 = 0.18, P = 0.032) and control groups (B = 0.81, SE = 0.31, OR = 2.26, 95% CI 1.23–4.23, R2 = 0.12, P = 0.008; Table 3), indicating that more hours of work per day were associated with increased neck pain.
Figure 1.
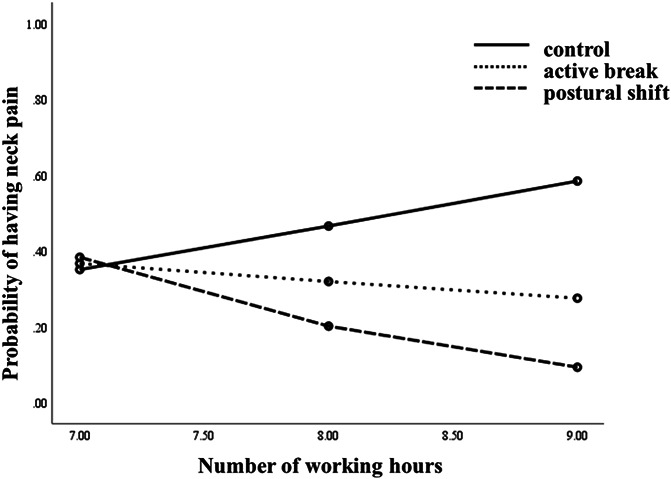
Illustration of the Group × Working Hours moderation effect on the probability of having neck pain.
Figure 2.
Significant moderations of the differences in the treatment effect and region of significance difference in (A) active break vs control groups and (B and C) postural shift vs control groups on the onset of neck pain.
Table 3.
Within-group simple slopes for significant tests of moderation (ie, simple effects).
| Moderator | Active break (n = 47) | Postural shift (n = 46) | Control (n = 100) | |||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| B | SE | β | P | B | SE | β | P | B | SE | β | P | |
| Nonspecific neck pain | ||||||||||||
| Level of work psychological demands | 0.03 | 0.89 | 0.97 | 0.784 | −0.09 | −0.89 | 0.91 | 0.297 | 0.11 | 0.05 | 1.12 | 0.022* |
| Number of working hours | −0.60 | 0.28 | 0.55 | 0.032* | −0.49 | 0.39 | 0.62 | 0.220 | 0.81 | 0.31 | 2.26 | 0.008* |
| Nonspecific low back pain | ||||||||||||
| Not having lumbar support | 0.93 | 1.27 | 2.53 | 0.465 | −1.09 | 0.87 | 0.34 | 0.290 | 1.86 | 0.47 | 6.39 | < 0.001* |
P < 0.05.
3.3. Psychological work demands as a moderator
The moderation analysis for the onset of neck pain revealed a significant Treatment Group X Psychological Work Demands interaction (B = −0.12, SE = 0.06, R2 = 0.32, P = 0.048; Fig. 3). Post hoc pairwise comparisons indicate a significant difference between the postural shift and control group (B = −0.15, SE = 0.07, R2 = 0.37, P = 0.030); participants who endorsed higher levels of psychological work demands at baseline and who were assigned to the postural shift group were less likely to develop neck pain than those randomized to the control group. Johnson–Neyman results indicated that participants with a level of work psychological demands >30.6 were less likely to develop neck pain with the postural shift condition compared with those in the control condition with this same level of perceived work demands (Fig. 2C).
Figure 3.
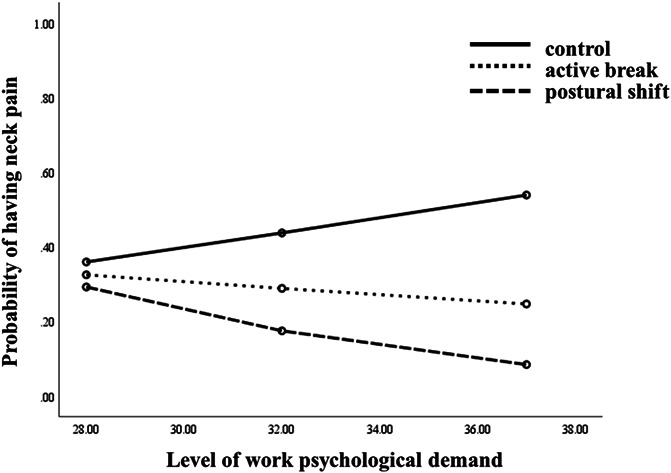
Significant moderations of the differences in group condition effects (ie, active break, postural shift, and control groups) on neck pain.
The perceived level of psychological work demands evidenced a nonsignificant trend to be a moderator (B = −0.73, SE = 0.11, R2 = 0.38, P = 0.051) for the active break vs control group and active break vs postural shift group (B = −1.69, SE = 0.14, R2 = 0.22, P = 0.241) with respect to the development of neck pain. Logistic regressions suggested that the level of work psychological demands was a significant predictor of neck pain only for the control condition (B = 0.11, SE = 0.05, OR = 1.12 95% CI 1.01–1.24, R2 = 0.08, P = 0.022; Table 3), in which more psychological demands were associated with increased neck pain.
3.4. Having or not having lumbar support as a moderator
The analysis for the onset of low back pain revealed a significant Treatment Group X Lumbar Support interaction (B = −1.97, SE = 0.66, R2 = 0.37, P = 0.003; Fig. 4). Post hoc comparisons indicated a significant difference between the postural shift and control group (B = −2.09, SE = 0.69, R2 = 0.42, P = 0.003); participants who reported not having lumbar support gained more benefits from the postural shift intervention than those in the control group. However, having or not having lumbar support was not found to predict any benefit for the active break vs control group (B = −0.64, SE = 1.45, R2 = 0.42, P = 0.635) or active break vs postural shift group (B = −3.14, SE = 1.81, R2 = 0.15, P = 0.095). Logistic regressions suggested that having or not having lumbar support was a significant predictor of low back pain for the control condition (B = 1.86, SE = 0.47, OR = 6.39, 95% CI 2.52–16.20, R2 = 0.23, P < 0.001; Table 3); not having lumbar support was associated with increased low back pain.
Figure 4.
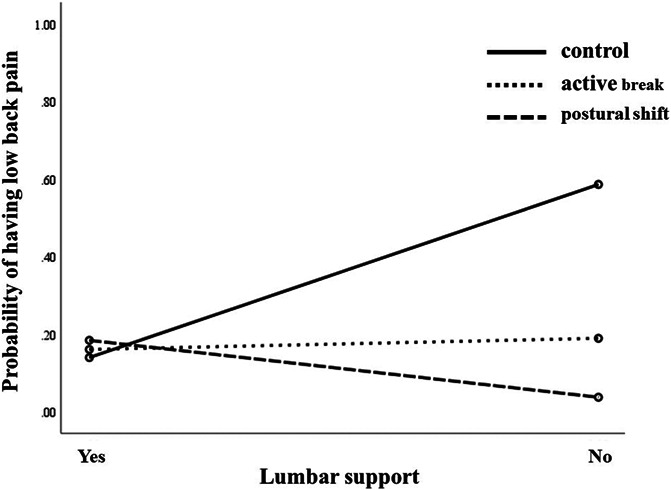
Significant moderations of the differences in group condition effects (ie, active break, postural shift, and control groups) on low back pain.
4. Discussion
This study sought to identify workers more or less likely to achieve benefits from interventions designed to reduce the risk of developing neck and low back pain. With respect to neck pain, we found that workers who worked more hours/day gained more benefits from both the active break and postural shift interventions than from the control condition and that workers who endorsed higher levels of psychological work demands gained more benefits from the postural shift intervention. The only moderator found with respect to preventing low back pain was that workers who had no lumbar support gained more benefits from the postural shift intervention than those in the control group. These findings have important implications for understanding who might benefit the most from these treatments, as well as for understanding the potential mechanisms underlying those benefits.
4.1. Moderators of prevention treatments and possible mechanisms
We found that the effects of the active break and postural shift interventions on neck pain risk were moderated by the number of working hours/day. Previous research has shown that both prolonged sitting and working time increase the risk of developing neck pain.7,36 The present findings suggest that the 2 interventions studied may mitigate the negative effects of longer working hours. Given the previous findings that increasing daily walking steps reduces the onset neck pain in office workers,40 it seems possible that the beneficial effects of taking breaks on neck pain could be mediated by increases in walking steps that could occur during those breaks. With respect to the postural shift intervention, changing sitting postures has been found to result in changes in cervicothoracic muscle activity.8 It is therefore possible that changing sitting postures may impose alternating activity in the neck and shoulder muscles, resulting in the alleviation of postural discomfort during prolonged sitting and consequently reducing the risk of developing neck pain.
We also found a significant moderation effect for the level of psychological work demands on the benefits of the postural shift intervention, and a nonsignificant trend (P = 0.051) for this same moderation effect for the active break intervention. Consistent with this finding, Gurung and colleagues18 identified psychological distress as a potential moderator of the benefits of cognitive-behavioral therapy on back pain–related disability. Other researchers have found that negative mood and emotions, cognitive functioning, and pain behavior are all related to the onset of neck pain and other musculoskeletal conditions.3,30 We can envision 2 possible mechanisms for the moderation effect we observed. First, psychological stress could induce negative physical effects (eg, muscle tension47 or postural discomfort44), which may then be mitigated by position shifts or by taking breaks. Second, taking active breaks or postural shifts might directly reduce psychological stress. Consistent with this idea, previous research has found that breaks can reduce or prevent stress and help to facilitate recovery from early symptoms of work-related mental and physical fatigue.37 However, research is needed to test psychological stress as a potential mediator of the beneficial effects of these treatments.
The moderation effect of lumbar support on the beneficial effects of the postural shift intervention for low back pain is consistent with previous research showing that lumbar support helps to prevent the development of low back pain.23 Prolonged sitting with poor posture (ie, reduced lumbar–lordotic curve) might increase strain on the back of the spine, consequently increasing the risk of hyperflexion injury to the disk and ligament.24,31 The negative effects of poor sitting posture can be minimized by using lumbar support, which contributes to maintaining the natural lordotic curvature.29 Regularly performing postural shifts while sitting may also decrease static trunk muscle activity,8 thus reducing trunk muscle fatigue and delaying the onset of low back discomfort.32,33 The concept that sitting with poor posture can contribute to exacerbations of low back symptom is controversial.6,11 Thus, the association between sitting posture and low back pain remains tenuous. Additional research to clarify the roles of sitting posture, lumbar support, and postural shifts in the development of low back pain is warranted.
4.2. Variables not showing a significant moderation effect
The hypothesized moderators that did not emerge as significant included age, job position, education level, and sex. The exploratory moderators that did not emerge as significant were having an adjustable chair, years of employment, standing for more than 2 hours in a typical work day, and needing to bend one's trunk forward frequently during work. These null findings have a number of possible explanations. First, it is possible that these factors moderate the effects of treatments that were not examined here. For example, the hypothesized moderators have been shown in previous research to moderate the effects of passive treatments such as acupuncture (ie, age and sex)46 and spinal manipulation (ie, low back pain duration and baseline pain intensity).15 By contrast, we examined the effects of active interventions, which may have different moderators. A second possible reason may be related to differences in the study samples. Hayden and colleagues described that having or not having heavy physical demands at work, using or not using medications, and BMI level moderated the effects of exercise treatment,20 and Underwood and colleagues found that age and employment status moderated the effects of a cognitive-behavioral intervention in individuals with low back pain.43 However, in the current study, the participants were office workers who were not currently reporting any neck or back pain. Additional research is needed to determine the extent to which moderators influence outcome across different samples of individuals and different types of treatment.
4.3. Implications for understanding mechanisms
The fact that the interventions studied here were moderated by 2 factors that seem to be biomechanical in nature (ie, longer work day hours and lack of lumbar support) is consistent with the idea that the interventions studied reduce the risk of developing neck and back pain by reducing biomechanical stress. This idea could be tested by including objective measures of biomechanical stress (eg, EMG activity) during treatment and then conducting mediation analyses21 to test biomechanical stress as a potential mediator. It is also possible that having more work hours could affect pain through its effects on psychosocial stress. Research to examine both types of stress as potential mediators is warranted.
4.4. Study strengths and limitations
A major strength of this study is a conservative definition of neck and low back pain (ie, pain that is moderate in intensity42 and lasts for at least 24 hours14) as our measure of pain onset. It is noteworthy that the results might have differed had we used a less conservative operational definition of pain onset.
The study has 4 primary limitations. First, we did not control for multiple testing. It is possible that some of the significant effects found emerged because of chance alone. The analyses conducted here should be repeated in other samples. Second, there are potential moderators identified in previous research that we did not evaluate here. Future research should examine these moderators. Third, the sample size for these analyses was not determined a priori because they are secondary analysis using data from a completed study. It is possible that significant moderation effects might have gone undetected. However, we did compute the effect sizes (f2) of the moderation effects tested, which may be used to determine the sample size by future researchers. Finally, the study was conducted using otherwise healthy 23 to 55 years old office workers who were pain free at the time of study enrollment. Therefore, generalization of the findings to other populations should be made with caution.
5. Conclusions
The findings provide new and important information regarding the role that several factors play as moderators of the effects of active break and postural shift interventions. We found significant moderating roles for (1) the number of working hours/day for the benefits of the active break intervention and (2) the number of working hours/day and perceived psychological work demands for the benefits of the postural shift intervention. The role of not having lumbar support was a moderator of the effect of the postural shift intervention in the development of low back pain. These findings can be used to identify those workers who are most likely to benefit from the interventions and provide preliminary findings that could inform future studies to evaluate the mechanisms that underlie the beneficial effects of these treatments.
Disclosures
The authors have no conflicts of interest to declare.
Acknowledgments
The study was approved by the Chulalongkorn University Human Ethics Committee.
This work was supported by the Thailand Research Fund through the Royal Golden Jubilee Ph.D. Program (PHD/0180/2558 and PHD/0120/2559) and Industry Division (RDG6050058). Srithai Auto Seats Industry Company Limited provided service and financial support for research projects to enhance the evidence-based knowledge for neck and low back pain in office workers for the Department of Physical Therapy of Chulalongkorn University with no interference on the concept or design, methodology, data collection, and data analysis of the study.
The authors have contributed in the following ways: N. Akkarakittichoke provided the concept or research design, data collection, data analysis, and manuscript writing. P. Waongenngarm contributed to the concept or research design and data collection. M.P. Jensen and P. Janwantanakul contributed to the concept or research design, data analysis, and manuscript writing. A.K. Newman contributed to the data analysis and manuscript writing. All authors read and approved the final manuscript.
Footnotes
Sponsorships or competing interests that may be relevant to content are disclosed at the end of this article.
Contributor Information
Nipaporn Akkarakittichoke, Email: nipaponr.pt@gmail.com.
Mark P. Jensen, Email: mjensen@uw.edu.
Andrea K. Newman, Email: anewman3@uw.edu.
Pooriput Waongenngarm, Email: pooriput.wao@cra.ac.th.
References
- [1].Areerak K, van der Beek AJ, Janwantanakul P. Recovery from nonspecific neck pain in office workers. J Back Musculoskelet Rehabil 2018;31:727–34. [DOI] [PubMed] [Google Scholar]
- [2].Ayanniyi O, Ukpai B, Adeniyi A. Differences in prevalence of self-reported musculoskeletal symptoms among computer and non-computer users in a Nigerian population: a cross-sectional study. BMC Musculoskelet Disord 2010;11:177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [3].Bongers PM, de Winter CR, Kompier MA, Hildebrandt VH. Psychosocial factors at work and musculoskeletal disease. Scand J Work Environ Health 1993;19:297–312. [DOI] [PubMed] [Google Scholar]
- [4].Borg G. Psychophysical scaling with applications in physical work and the perception of exertion. Scand J Work Environ Health 1990;16(Suppl 1):55–8. [DOI] [PubMed] [Google Scholar]
- [5].Borghouts JAJ, Koes BW, Bouter LM. The clinical course and prognostic factors of non-specific neck pain: a systematic review. PAIN 1998;77:1–13. [DOI] [PubMed] [Google Scholar]
- [6].Burnett AF, Cornelius MW, Dankaerts W, O'Sullivan PB. Spinal kinematics and trunk muscle activity in cyclists: a comparison between healthy controls and non-specific chronic low back pain subjects—a pilot investigation. Man Ther 2004;9:211–19. [DOI] [PubMed] [Google Scholar]
- [7].Cagnie B, Danneels L, Van Tiggelen D, De Loose V, Cambier D. Individual and work related risk factors for neck pain among office workers: a cross sectional study. Eru Spine J 2007;16:679–86. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [8].Caneiro JP, O'Sullivan P, Burnett A, Barach A, O'Neil D, Tveit O, Olafsdottir K. The influence of different sitting postures on head/neck posture and muscle activity. Man Ther 2010;15:54–60. [DOI] [PubMed] [Google Scholar]
- [9].Côté P, Cassidy DJ, Carroll LJ, Kristman V. The annual incidence and course of neck pain in the general population: a population-based cohort study. PAIN 2004;112:267–73. [DOI] [PubMed] [Google Scholar]
- [10].Côté P, van der Velde G, Cassidy JD, Carroll LJ, Hogg-Johnson S, Holm LW, Carragee EJ, Haldeman S, Nordin M, Hurwitz EL, Guzman J, Peloso PM. The burden and determinants of neck pain in workers: results of the bone and joint decade 2000-2010 task force on neck pain and its associated disorders. J Manipulative Physiol Ther 2009;32:S70–86. [DOI] [PubMed] [Google Scholar]
- [11].Dankaerts W, O'Sullivan P, Burnett A, Straker L. Differences in sitting postures are associated with nonspecific chronic low back pain disorders when patients are subclassified. Spine 2006;31:698–704. [DOI] [PubMed] [Google Scholar]
- [12].da Silva T, Mills K, Brown BT, Natasha Pocovi N, de Campos T, Maher C, Hancock MJ. Recurrence of low back pain is common: a prospective inception cohort study. J Physiother 2019;65:159–65. [DOI] [PubMed] [Google Scholar]
- [13].de Campos TF, Maher CG, Steffens D, Fuller JT, Hancock MJ. Exercise programs may be effective in preventing a new episode of neck pain: a systematic review and meta-analysis. J Physiother 2018;64:159–65. [DOI] [PubMed] [Google Scholar]
- [14].de Vet HCW, Heymans MW, Dunn KM, Pope DP, van der Beek AJ, Macfarlane GJ, Bouter LM, Croft PR. Episodes of low back pain: a proposal for uniform definitions to be used in research. Spine 2002;27:2409–16. [DOI] [PubMed] [Google Scholar]
- [15].de Zoete A, de Boer MR, Rubinstein SM, van Tulder MW, Underwood M, Hayden JA, Buffart LM, Ostelo R; International IPD-SMT group. Moderators of the effect of spinal manipulative therapy on pain relief and function in patients with chronic low back pain: an individual participant data Meta-analysis. Spine 2021;46:E505–e17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [16].Ehsani F, Mosallanezhad Z, Vahedi G. The Prevalence, risk factors and consequences of neck pain in office employees. Middle East J Rehab Health Stud 2017;4:e42031. [Google Scholar]
- [17].GBD 2015 Disease and Injury Incidence and Prevalence Collaborators. Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries: a systematic analysis for the Global Burden of Disease Study 2015. Lancet 2016;388:1545–602. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [18].Gurung T, Ellard DR, Mistry D, Patel S, Underwood M. Identifying potential moderators for response to treatment in low back pain: a systematic review. Physiotherapy 2015;101:243–51. [DOI] [PubMed] [Google Scholar]
- [19].Hamberg-van Reenen HH, van der Beek AJ, Blatter BM, van der Grinten MP, van Mechelen W, Bongers PM. Does musculoskeletal discomfort at work predict future musculoskeletal pain? Ergonomics 2008;51:637–48. [DOI] [PubMed] [Google Scholar]
- [20].Hayden JA, Wilson MN, Stewart S, Cartwright JL, Smith AO, Riley RD, van Tulder M, Bendix T, Cecchi F, Costa L, Dufour N, Ferreira ML, Foster NE, Gudavalli MR, Hartvigsen J, Helmhout P, Kool J, Koumantakis GA, Kovacs FM, Kuukkanen T, Long A, Macedo LG, Machado L, Maher CG, Mehling W, Morone G, Peterson T, Rasmussen-Barr E, Ryan CG, Sjögren T, Smeets R, Staal JB, Unsgaard-Tøndel M, Wajswelner H, Yeung EWe. Exercise treatment effect modifiers in persistent low back pain: an individual participant data meta-analysis of 3514 participants from 27 randomised controlled trials. Br J Sports Med 2020;54:1277–78. [DOI] [PubMed] [Google Scholar]
- [21].Hayes AF, Rockwood NJ. Regression-based statistical mediation and moderation analysis in clinical research: observations, recommendations, and implementation. Behav Res Ther 2017;98:39–57. [DOI] [PubMed] [Google Scholar]
- [22].Henschke N, Maher CG, Refshauge KM, Herbert RD, Cumming RG, Bleasel J, York J, Das A, McAuley JH. Prognosis in patients with recent onset low back pain in Australian primary care: inception cohort study. BMJ 2008;337:a171–a71. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [23].Janwantanakul P, Pensri P, Moolkay P, Jiamjarasrangsi W. Development of a risk score for low back pain in office workers-a cross-sectional study. BMC Musculoskelet Disord 2011;12:23. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [24].Jung KS, Jung JH, In TS, Cho HY. Effects of prolonged sitting with slumped posture on trunk muscular fatigue in adolescents with and without chronic lower back pain. Medicina 2020;57:3. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [25].Klaber Moffett JA, Carr J, Howarth E. High fear-avoiders of physical activity benefit from an exercise program for patients with back pain. Spine 2004;29:1167–73. [DOI] [PubMed] [Google Scholar]
- [26].Krismer M, van Tulder M. Strategies for prevention and management of musculoskeletal conditions. Low back pain (non-specific). Best Pract Res Clin Rheumatol 2007;21:77–91. [DOI] [PubMed] [Google Scholar]
- [27].Kuorinka I, Jonsson B, Kilbom A, Vinterberg H, Biering-Sorensen F, Andersson G, Jorgensen K. Standardised Nordic questionnaires for the analysis of musculoskeletal symptoms. Appl Ergon 1987;18:233–37. [DOI] [PubMed] [Google Scholar]
- [28].Leaver AM, Maher CG, McAuley JH, Jull G, Latimer J, Refshauge KM. People seeking treatment for a new episode of neck pain typically have rapid improvement in symptoms: an observational study. J Physiother 2013;59:31–7. [DOI] [PubMed] [Google Scholar]
- [29].Makhsous M, Lin F, Hendrix RW, Hepler M, Zhang LQ. Sitting with adjustable ischial and back supports: biomechanical changes. Spine 2003;28:1113–21. [DOI] [PubMed] [Google Scholar]
- [30].Mayerl H, Stolz E, Großschädl F, Rásky É, Freidl W. The moderating role of personal resources in the relationship between psychosocial job demands and health: a cross-sectional study. J BMJ Open 2017;7:e015710. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [31].McGill SM, Brown S. Creep response of the lumbar spine to prolonged full flexion. Clin Biomech 1992;7:43–6. [DOI] [PubMed] [Google Scholar]
- [32].O'Sullivan K, O'Keeffe M, O'Sullivan L, O'Sullivan P, Dankaerts W. The effect of dynamic sitting on the prevention and management of low back pain and low back discomfort: a systematic review. Ergonomics 2012;55:898–908. [DOI] [PubMed] [Google Scholar]
- [33].O'Sullivan K, O'Sullivan P, O'Keeffe M, O'Sullivan L, Dankaerts W. The effect of dynamic sitting on trunk muscle activation: a systematic review. Appl Ergon 2013;44:628–35. [DOI] [PubMed] [Google Scholar]
- [34].Paksaichol A, Lawsirirat C, Janwantanakul P. Contribution of biopsychosocial risk factors 0to nonspecific neck pain in office workers: a path analysis model. J Occup Health 2015;57:100–9. [DOI] [PubMed] [Google Scholar]
- [35].Phakthongsuk P. Construct validity of the Thai version of the job content questionnaire in a large population of heterogeneous occupations. J Med Assoc Thai 2009;92:564–72. [PubMed] [Google Scholar]
- [36].Shenbagasundaram S, Balasuburamaniam A. Risk factor analysis in sedentary office workers with low back pain. J Chalmeda Anandrao Inst Med Sci 2017;3:15–18. [Google Scholar]
- [37].Sianoja M, Kinnunen U, de Bloom J, Korpela K, Geurts S. Recovery during lunch breaks: testing long-term relations with energy levels at work. Eur J Work Organ Psychol 2016;1:9. [Google Scholar]
- [38].Sihawong R, Sitthipornvorakul E, Paksaichol A, Janwantanakul P. Predictors for chronic neck and low back pain in office workers: a 1-year prospective cohort study. J Occup Health 2016;58:16–24. [DOI] [PubMed] [Google Scholar]
- [39].Sitthipornvorakul E, Janwantanakul P, Lohsoonthorn V. The effect of daily walking steps on preventing neck and low back pain in sedentary workers: a 1-year prospective cohort study. Eur Spine J 2015;24:417–24. [DOI] [PubMed] [Google Scholar]
- [40].Sitthipornvorakul E, Sihawong R, Waongenngarm P, Janwantanakul P. The effects of walking intervention on preventing neck pain in office workers: a randomized controlled trial. J Occup Health 2020;62:e12106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [41].Steffens D, Maher CG, Pereira LS, Stevens ML, Oliveira VC, Chapple M, Teixeira-Salmela LF, Hancock MJ. Prevention of low back pain: a systematic review and meta-analysis. JAMA Intern Med 2016;176:199–208. [DOI] [PubMed] [Google Scholar]
- [42].Tsauo JY, Jang Y, Du CL, Liang HW. Incidence and risk factors of neck discomfort: a 6-month sedentary-worker cohort study. J Occup Rehabill 2007;17:171–9. [DOI] [PubMed] [Google Scholar]
- [43].Underwood MR, Morton V, Farrin A. Do baseline characteristics predict response to treatment for low back pain? Secondary analysis of the UK BEAM dataset [ISRCTN32683578]. Rheumatology 2007;46:1297–302. [DOI] [PubMed] [Google Scholar]
- [44].Wahlström J. Ergonomics, musculoskeletal disorders and computer work. Occup Med 2005;55:168–76. [DOI] [PubMed] [Google Scholar]
- [45].Waongenngarm P, van der Beek AJ, Akkarakittichoke N, Janwantanakul P. Effects of an active break and postural shift intervention on preventing neck and low-back pain among high-risk office workers: a 3-arm cluster-randomized controlled trial. Scand J Work Environ Health 2021;47:306–17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- [46].Witt CM, Schützler L, Lüdtke R, Wegscheider K, Willich SN. Patient characteristics and variation in treatment outcomes: which patients benefit most from acupuncture for chronic pain? Clin J Pain 2011;27:550–5. [DOI] [PubMed] [Google Scholar]
- [47].Yaribeygi HPY, Sahraei H, Johnston TP, Sahebkar A. The impact of stress on body function: a review. Excli J 2017;16:1057–72. [DOI] [PMC free article] [PubMed] [Google Scholar]