The novel coronavirus SARS-CoV-2/COVID-19 is rapidly and dramatically spreading throughout the world. We describe the clinical and histopathological features of 3 Italian patients with different cutaneous presentations of COVID-19 infection, observed and followed at the University of Milan.
CASE REPORTS
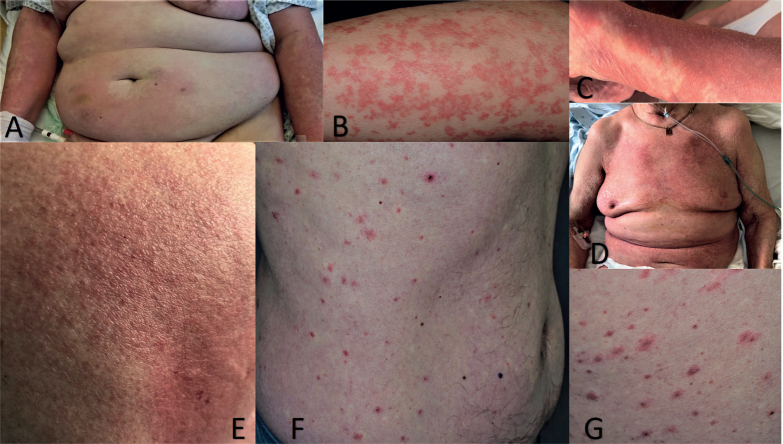
Case 1. A 59-year-old woman was admitted to the intensive care unit (ICU) at the University of Milan with bilateral interstitial pneumonia. Three days after admission, she developed widespread erythematous macules on arms, trunk and lower limbs (Fig. 1 A-C) that spontaneously improved within 5 days. C-reactive protein was 12 mg/l. Reverse transcriptase (RT)-PCR for COVID-19 virus was positive. Treatment was started with lopinavir-ritonavir, heparin and levofloxacin. She is currently recovering.
Fig. 1.
Case 1 (A). Erythema on the abdomen. (B). Erythematous macules on a leg. (C). Diffuse erythematous macules on a forearm. Case 2 (D). Erythema on the chest and abdomen. (E). Close up image demonstrating erythematous plaques made up of tiny papules. Case 3 (F, G). Widespread erythematous crusted papules; some of them are erosive.
Case 2. An 89-year-old woman was suffering from fever and cough of one-week duration. An exanthem on the trunk and arms was observed on admission at ICU (Fig. 1 D,E). Laboratory tests revealed mild increase in fibrinogen and transaminases. RT-PCR was positive for COVID-19 virus. Ceftriaxone and azithromycin were started. The exanthem improved spontaneously 8 days later. Case 3. A 57-year-old man in good general health acutely developed a widespread pruritic eruption of erythematous macules and papules (Fig. 1 F,G), followed two days later by fever, headache, cough and arthralgias. RT-PCR for COVID-19 virus was positive. Treatment with levofloxacin and hydroxychloroquine was started. It was suggested that the patient go home for quarantine. Ten days after the appearance of the rash, skin lesions reduced in number and severity without therapy.
Histopathological examinations
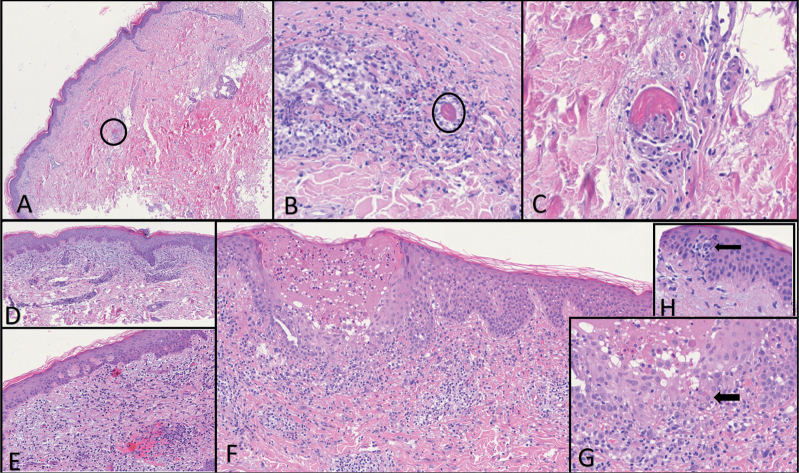
Histopathology of the leg in Case 1 showed a superficial perivascular dermatitis with slight lymphocytic exocytosis. In the mid dermis a small thrombus in a vessel was present. Swollen thrombosed vessels with neutrophils, eosinophils and nuclear debris were patchy distributed in the dermis (Fig. 2 A-C).
Fig. 2.
Case 1. (A) Superficial perivascular dermatitis with mild spongiosis and a small thrombus in the mid dermis (encircled). (B) Vasculitis with nuclear debris and a small thrombus (encircled). (C) High magnification of a small thrombized vessel. Case 2: (D) Superficial perivascular dermatitis with lymphocytic vasculitis in mid dermis. (E) Extravasated red blood cells due to endothelial damage. Case 3: (F) Superficial perivascular and vesicular dermatitis with patchy band-like infiltration. (G) Dyskeratotic, ballooning and necrotic keratinocytes with lymphocytic exocytosis. (H) Nest of Langerhans cells within the epidermis.
Histopathology of the back in Case 2 showed a superficial and deep perivascular dermatitis with cuffs of lymphocytes surrounding blood vessels in a vasculitic pattern (Fig. 2D). In the mid dermis extravasated red blood cells from damaged vessels were visible (Fig. 2E).
Histopathology of the back in Case 3 showed a superficial perivascular vesicular dermatitis. Focal acantholytic suprabasal clefts, dyskeratotic and ballooning herpes-like keratinocytes were observed. A patchy band-like infiltration with occasional necrotic keratinocytes and minimal lymphocytic satellitosis were present. In the dermis the vessels were swollen, with dense lymphocyte infiltration, mixed with rare eosinophils. Within the epidermis a nest of Langerhans cells were also observed (Fig. 2 F-H).
DISCUSSION
There are limited reports about cutaneous manifestations associated with COVID-19 virus infection. One report documented cutaneous rash in 20% of patients, most commonly as “erythematous rash” (1). Other cutaneous manifestations include urticaria (1), papules and vesicles (1) and a “dengue-like” rash (2).
The clinical and histopathological differential diagnosis of an exanthematous eruption most commonly includes drug eruptions and viral infections. Positive COVID-19 virus RT-PCRs in all our patients strongly suggests an exanthem associated with a viral infection. The histopathological picture observed in Cases 1 and 2 is consistent with that of a viral exanthem. However, the finding of early microthrombi in Case 1 is significant, as autopsy reports from COVID-19-infected patients have shown hyaline thrombi in microvessels of the lungs (3). Furthermore, one of us (RG) had the opportunity to study a second case of disseminated intravascular coagulationlike lesions in a COVID-19-positive patient (in press). Very recently, a paper (currently in press), reported severe thrombosis of the cutaneous vascular plexus in 5 patients with superimposable histopathological features of our Case 1 (4).
Skin specimen from Case 2 did not show thrombi in small vessels, but features present in a lymphocytic vasculitis that are similar to those observed in thrombophilic arteritis induced by blood immune complexes that activate cytokines recruiting eosinophils and cytotoxic T cells (5).
The histopathology observed in Case 3 has features reminiscent of transient acantholytic dermatosis (Grover’s disease), with ballooning multinucleated cells. We do not think it is a fortuitous concomitant disease because two of us (RG and SV) observed a second case of Grover’s disease in a COVID-19-positive patient (in press). These overlapping features, mimicking a herpes infection, have already been described in patients with simultaneous Grover’s and Kaposi’s varicelliform eruption (6). An interface dermatitis with necrotic keratinocytes surrounded by lymphocytes may suggest that the virus induces a cytokine cascade activation of cytotoxic and NK lymphocytes which in turn damage keratinocytes. Finally, nests of Langerhans cells are well known to be present in other viral-induced skin dermatitis, such as pityriasis rosea (7).
We think that the finding of viral particles present in the cutaneous blood vessels in patients with COVID-19 infection (4) could implicate a possible viral interaction also with the keratinocytes, inducing a spectrum of different clinical manifestations.
Footnotes
The authors have no conflicts of interest to declare.
REFERENCES
- 1.Recalcati S. Cutaneous manifestations in COVID-19: a first perspective. J Eur Acad Dermatol Venereol 2020. Mar 26. [Epub ahead of print]. [DOI] [PubMed] [Google Scholar]
- 2.Joob B, Wiwanitkit V. COVID-19 can present with a rash and be mistaken for dengue. J Am Acad Dermatol 2020; 82: e177. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Yao XH, Li TY, He ZC, Ping YF, Liu HW, Yu SC, et al. A pathological report of three COVID-19 cases by minimally invasive autopsies. Zhonghua Bing Li Xue Za Zhi 2020; 49: E009. [DOI] [PubMed] [Google Scholar]
- 4.Magro C, Mulvey JJ, Berlin D, Nuovo G, Salvatore S, Harp J, et al. Complement associated microvascular injury and thrombosis in the pathogenesis of severe COVID-19 infection: A report of five cases. Transl Res 2020 Apr 15. pii: S1931-5244(20)30070-0. [Epub ahead of print]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Lee JS, Kossard S, McGrath MA. Lymphocytic thrombophilic arteritis: a newly described medium-sized vessel arteritis of the skin, Arch Dermatol 2008; 144: 1175–1182. [DOI] [PubMed] [Google Scholar]
- 6.Kosann MK, Fogelman JP, Stern RL. Kaposi’s varicelliform eruption in a patient with Grover’s disease. J Am Acad Dermatol 2003; 49: 914–915. [DOI] [PubMed] [Google Scholar]
- 7.Broccolo F, Ciccarese G, Oggioni M, Rebora A, Parodi A, Drago F. The saliva quantitative PCR assay is inadequate to detect and monitor human herpesvirus-7 and -6 reactivation in patients with pityriasis rosea. J Clin Virol 2014; 61: 615–616. [DOI] [PubMed] [Google Scholar]