Abstract
Ocular surface disorders such as Lid Wiper Epitheliopathy (LWE), Superior Epithelial Arcuate Lesion (SEAL), and contact lens-induced Limbal Stem Cell Deficiency (LSCD) as well as Superior Limbic Keratoconjunctivitis (SLK) affect one's quality of life. Hence, it is imperative to investigate the underlying causes of these ocular surface disorders. During blink, the undersurface of the eyelid tends to interact with the cornea and the conjunctiva. The presence of a contact lens can add to the biomechanical frictional changes on these surfaces. To estimate these changes with and without a contact lens, a finite element model (FEM) of the eyelid wiper, eyeball, and contact lens was developed using COMSOL Multiphysics. Biomechanical properties such as von Mises stress (VMS) and displacement were calculated. Our study concluded that (a) maximum VMS was observed in the lid wiper in the absence of contact lens in the eye and (b) maximum VMS was observed in the superior 1.3 mm of the cornea in the presence of the contact lens in the eye. Thus, the development of friction-induced ocular surface disorders such as LWE, SLK, SEAL, and LSCD could be attributed to increased VMS. FEA is a useful simulation tool that helps us to understand the effect of blink on a normal eye with and without CL.
1. Introduction
It is estimated that currently there are more than 140 million contact lens (CL) wearers worldwide [1]. Existing literature states that about 21%–64% of these CL wearers tend to discontinue CL use [2–4] as a result of contact lens discomfort (CLD). CLD is a condition characterized by “episodic or persistent adverse ocular sensations due to CL wear, either with or without visual disturbance. It arises from a reduced compatibility between the CL and the ocular environment and thus accounts for 50% of patients' experiencing a reduced CL-wearing time and/or discontinuation of CL use” [5]. Factors contributing to CLD include CL material, design, lens care, fit, and tear film stability [6]. Apart from CLD, dry eye (19.9%) [7], ocular redness (6.8%) [7], cost of CL (6.8%) [7], and handling issues (6.3%) [7] can also lead to CL dropouts. Conditions such as age; gender; systemic diseases like autoimmune diseases; CL solution and care regimen; and design, material, and modality of the CL account for a smaller percentage of CL dropouts [1, 8].
During the blink reflex, the undersurface of the eyelid interacts with the cornea and the conjunctiva [9]. This setup of the human eye can be considered as a complex tribological system consisting of two sliding surfaces (eyelid and corneo-conjunctival complex) moving relative to each other, with the tear film as a lubricant [10]. Deficiency of tear fluid or excessive evaporation of tears may lead to dry eye disease [11] which in turn may harm the ocular surface due to friction [12]. Having a CL in situ results in two sets of sliding surfaces. While in the anterior aspect, the sliding surfaces are is formed by the palpebral conjunctiva (which lines the inner surface of the eyelid) and anterior surface of the contact lens, in the posterior aspect, it is formed by the posterior surface of contact lens, anterior surface of the cornea, and bulbar conjunctiva [13]. This tribological system is also highly influenced by various tear film characteristics that may result from the presence of dry eye disease in CL wearers.
The cornea and the lid wiper (a portion of the lid margin of the upper eyelid that wipes the ocular surface during blinking) [14] are more prone to frictional damage than the bulbar conjunctiva [15]. Frictional damage to the ocular surface causes ocular surface disorders such as Lid Wiper Epitheliopathy (LWE), Superior Limbic Keratoconjunctivitis (SLK) [16], Superior Epithelial Arcuate Lesion (SEAL) [17], and Limbal Stem Cell Deficiency (LSCD) [18]. These conditions cause a variety of symptoms such as foreign-body sensation during blink, discomfort, and visual loss, thereby decreasing the quality of life [16].
Friction is usually quantified using Coefficient of Friction (CoF) which is the ratio between the frictional force and the normal force. The most commonly used in vitro methods to measure CoF are through the use of an instrument called micro tribometer [19, 20] and atomic force microscopy [21, 22]. In case of CL, CoF can vary depending on its material properties, thickness, and modulus of elasticity. However, in general, a CL having low CoF reduces friction and improves comfort [10, 20, 23–25]. The CoF values range from 0.011 to 0.562 across various studies [19, 20, 26]. This wide variation noted is due to the difference in the material used to measure the CoF. For example, instead of cornea and eyelid, studies have used borosilicate glass slab [20] and mucin coated glass slab [19] where only the curvature is considered. The exact material properties such as modulus, Poisson's ratio, and density of the ocular structures were not considered. An in vivo experiment done on animal models using micro tribometer has led to epithelial damage because of the rubbing of the cantilever against the cornea while estimating CoF [27].
Since in vitro studies are not producing reliable results and performing in vivo experiments could lead to tissue damage, Finite Element Analysis (FEA) has been used in this study as a tool to analyze the biomechanical changes [16]. FEA is the simulation of any given physical phenomenon using the numerical technique called Finite Element Method (FEM). Using FEA, Kataoka et al. have estimated the deformation and shearing stress between the eyelid and the corneo-conjunctival complex, while considering the ocular surface to be a flat surface [16].
When compared to in vitro studies done using micro tribometer, atomic force microscope, etc., FEA is a superior technique for understanding the biomechanical changes (deformation, displacement, and stress) which take place during the blink reflex. However, there are very limited studies [16] that estimate the biomechanical parameters during blinking while considering the actual anatomy and material properties of the eye.
Hence, our study aims to develop a finite element model (FEM) consisting of the lid wiper, eyeball, and contact lens, in order to estimate the biomechanical changes in the cornea and the lid wiper, during a blink, in the presence as well as absence of CL.
2. Methods
FEA is a popular method to analyze complex systems. The benefit of using an FEA on complex problems is that geometry can be precisely defined [28]. It is very sensitive such that it can measure even a subtle change in geometry, which is otherwise difficult to pick up with the current instruments such as Optical Coherence Tomography (OCT) and Anterior Segment OCT [29]. Since FEA uses the static equilibrium and theories of elasticity, it is possible to assess a physical system subjected to multiple external forces with regard to stresses, deformation, and strain [30]. Hence, FEA is chosen as the analytical tool.
A computer with 2.80 GHz CPU and 8 GB RAM is used for this experimental study. COMSOL Multiphysics, an FEA tool, is used for the construction and analysis of the human eye model. The COMSOL Multiphysics is used for the FEA because of its ability to provide accurate FE simulation results. The flow of procedure for the FEA includes the following:
Modeling the geometry.
Assigning the material properties.
Meshing.
Setting boundary conditions.
Parametric sweep analysis.
Postprocessing the results.
Ocular parameters of various structures and their material properties were obtained from previous works of literature done on Indian eyes. Linear static analysis was carried out ignoring gravity.
2.1. Modeling
It is unrealistic to consider a single eye geometry since the dimensions of the human eye vary from person to person. Here, we have used the average value of each of the ocular parameters of the Indian eyes obtained through a thorough literature search.
The Indian eye model, which closely resembles the dimensions of the actual human eye, is constructed in 2D (Figure 1(a)) and is converted into a solid 3D model (Figure 1(b)). For simplicity, the human eye is assumed to be rotationally symmetrical along the optic axis. The eye model comprises the following structures: lid wiper, cornea, anterior chamber, vitreous cavity, sclera, optic nerve, and optic nerve head. The anteroposterior (transverse) diameter of the eye model is approximately 24 mm, and the vertical (sagittal) diameter is approximately 23 mm [31].
Figure 1.
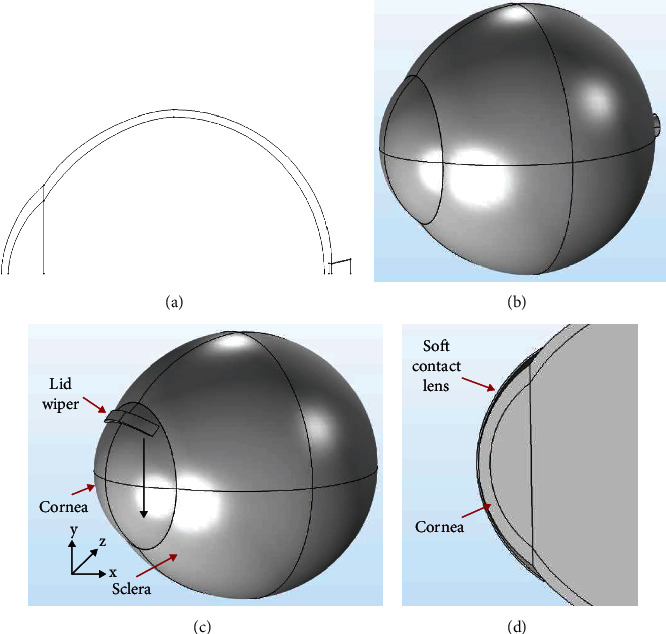
Two-dimensional (a) and three-dimensional model of the eyeball (b). Three-dimensional model of the eyeball with lid wiper (black arrow represents the direction of movement of the lid wiper on the cornea) (c). Cross section of the eyeball with soft contact lens (d). The model was constructed using COMSOL Multiphysics v5.2 (https://www.comsol.com) and the collage of the exported images was made using Microsoft PowerPoint 2019 (https://www.microsoft.com/en-in/microsoft-365/get-started-with-office-2019).
The asymmetrical nature of the optic nerve is ignored. The dimensions used in the construction of each structure of the human eye are as shown in Table 1.
Table 1.
Dimensions of ocular structures and contact lens used in the finite element modeling.
| Part of the eye | Value (mm) |
|---|---|
| Lid wiper thickness [32] | 0.8 |
| Corneal thickness [33] | 0.5 |
| Corneal diameter [34] | 12 |
| Anterior corneal curvature [34] | 7.8 |
| Posterior corneal curvature [34] | 6.5 |
| Scleral thickness [35] | 0.5 |
| Scleral radius [36] | 11.5 |
| Diameter of the contact lens chosen | 15 |
| Base curve of the contact lens chosen | 8.6 |
| Thickness of the contact lens chosen | 0.08 |
The prolate nature of the cornea is not considered. A cornea of uniform thickness is assumed for the construction. For the ease of modeling, the scleral thickness and corneal diameter are considered to be uniform throughout the respective structures.
Since eyelid conforms to the curvature of the ocular surface while blinking, we have assumed the curvature of the inner lid wiper to be the curvature of the anterior cornea. The thickness of the lid wiper (y-direction, Figure 1(c)) is considered to be 0.8 mm with reference to the literature [32]. The contact width between the lid wiper and cornea (the width of the lid wiper which was in contact with the cornea in the x-direction) is 1 mm [37]. The entire simulated model consisting of the eyeball and the lid wiper can be seen in Figure 1(c).
Different soft CL geometries have been explored in previous research [38–40]. CL parameters such as center thickness, base curve, and diameter are available in the literature [41]. In general, a CL is thicker at the center than in the periphery, and this ranges from 0.05 to 0.9 mm. The radius of curvature of the back surface of the lens, i.e., the base curve, generally ranges from 7 to 9 mm, and also the diameter of the CL ranges from 13.00 to 14.50 mm.
In this study, based on the eye geometry, the contact lens of 15 mm diameter (2-3 mm greater than corneal diameter) and 8.6 mm base curve (0.8–1.0 mm flatter than corneal curvature) is fitted in the eye (Figure 1(d)). The peripheral curve radius of soft contact lens (radius of the curve which connects the front and back surface of contact lens) is not available in the literature. Hence, in this study, it is assumed to be 0.5 mm. Contact lens parameters used in this study can be found in Table 1.
Young's modulus, Poisson's ratio, and density are the important material properties considered. Human ocular tissues are generally viscoelastic and exhibit nonlinear material properties [42]. This nonlinear material property of the human eye ranges widely due to its complex nature. These viscoelastic properties of the structures of the eyeball are not yet investigated properly. Hence, the material properties are assumed to be homogenous, isotropic, and linearly elastic. As shown in Table 2, the material properties of the ocular structures are obtained from the previous works of literature. Young's modulus of the human eyelid has not yet been investigated [43]. Hence, a value of 0.42 MPa, which is Young's modulus of the human skin, is assumed [43, 44]. Poisson's ratio of the aqueous humor, vitreous humor, retina, zonules, and optic nerve has not yet been investigated. Since soft biological tissues hold more amount of moisture, Poisson's ratio is set to be less than 0.5 for these ocular structures [42, 45].
Table 2.
Material properties of the ocular structures and contact lens used in the finite element modeling.
| Part of the eye | Young's modulus (MPa) | Poisson's ratio | Density (kg/m3) |
|---|---|---|---|
| Lid wiper [44, 46] | 0.42 | 0.49 | 999 |
| Cornea [30, 47, 48] | 0.4 | 0.42 | 1400 |
| Aqueous humor [30, 49] | 0.037 | 0.49 | 999 |
| Vitreous humor [30, 49] | 0.042 | 0.49 | 999 |
| Retina [45, 50–52] | 0.03 | 0.49 | 999 |
| Optic nerve [45, 51, 53] | 0.03 | 0.49 | 999 |
| Comfilcon A contact lens [29, 54] | 0.82 | 0.49 | 1040 |
The material properties used for the CL are as shown in Table 2. CL is a rubbery polymer, and it is highly hydrated. Hence, a Poisson's ratio of 0.49 was set, which makes it incompressible. Density of the contact lenses is not directly available in the literature. However, specific gravity is available for the contact lenses. Hence, using the following formula, we have calculated the density of these contact lenses.
| (1) |
where density of the water at 4°C = 999.97 [55] and specific gravity of the contact lens = 1.04 [56].
2.2. Mesh Convergence Study
Mesh convergence study was carried out to analyze the proper number of finite elements. Figure 2 shows the result when a body load of 0.03 N is applied on the surface of the lid wiper. It can be found that the VMS barely changes when the length of a side of the finite element is 0.259 mm or more. Hence, the value of 0.259 mm is used as the length of a side of the element during Finite Element Analysis.
Figure 2.
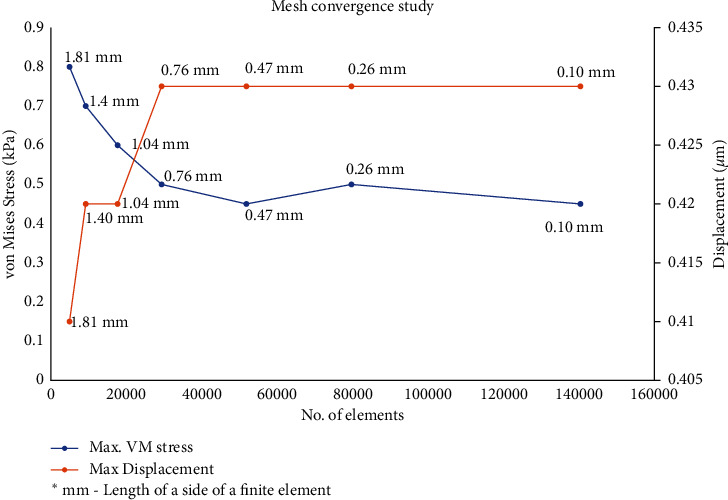
Mesh convergence study: proper number of finite elements. Graph drawn with Microsoft Excel 2019 (https://www.microsoft.com/en-in/microsoft-365/get-started-with-office-2019).
Sensitivity analysis has been carried out to study the effect of material properties (Young's modulus, Poisson's ratio, and density) of the cornea and lid wiper on the outcome parameters (VMS and displacement). Each material property was studied individually by keeping the other two material properties constant. For example, when Young's modulus of the lid wiper was varied between 0.45 and 0.85 MPa, by keeping Poisson's ratio (0.49) and density (999 kg/m3) of lid wiper constant, the corresponding change in VMS in the lid wiper was found to be between 17.1 and 20.9 kPa. Our sensitivity analysis results (Figure 3) showed that there was no significant variation in the outcome parameters when the material properties of the cornea and lid wiper were changed. However, there was a slight variation noted in the VMS when Young's modulus of the lid wiper was changed. This is due to the huge variation in Young's modulus of the lid wiper (0.45 MPa to 0.85 MPa). Since Young's modulus of the lid wiper is not available in the literature, the current study has assumed Young's modulus of skin to be Young's modulus of lid wiper. Young's modulus of the skin varies widely across different studies, which explains why there is a slight variation in the VMS in the lid wiper. Since conjunctiva is more flexible than cornea, Kataoka et al. have assumed Young's modulus of eyelid to be half that of the cornea. In a similar assumption, we have also considered Young's modulus of lid wiper to be between 0.10 and 0.20 MPa (half of the cornea), and we have found the corresponding VMS to be between 16.8 and 16.9 kPa. Overall, our sensitivity analysis has shown that the VMS and displacement were not varying significantly based on a single value of the material properties. The detailed values of sensitivity analysis of the material properties of the cornea and lid wiper in terms of von Mises stress and displacement are included in Supplementary Tables 1Sa and 1Sb.
Figure 3.

Sensitivity analysis of the material properties of the cornea and lid wiper. Change in Young's modulus of cornea does not have any effect on the VMS of the cornea whereas VMS increases slightly with the increase in Young's modulus of the lid wiper (a). Change in Poisson's ratio of cornea does not have any effect on the VMS of the cornea whereas VMS decreases slightly with the increase in Poisson's ratio of the lid wiper (b). Change in density does not have any effect on VMS of the cornea and lid wiper (c). Change in Young's modulus, Poisson's ratio, and density does not have any effect on displacement of the cornea (d–f). Graph drawn with Microsoft Excel 2019 (https://www.microsoft.com/en-in/microsoft-365/get-started-with-office-2019).
All components of the FEM are meshed with the physics-controlled settings in the COMSOL Multiphysics. The predefined size of each element is set as “fine.” Figure 4 shows the mesh-divided model of the eyeball with lid wiper (Figure 4(a)) and the contact lens (Figure 4(b)).
Figure 4.
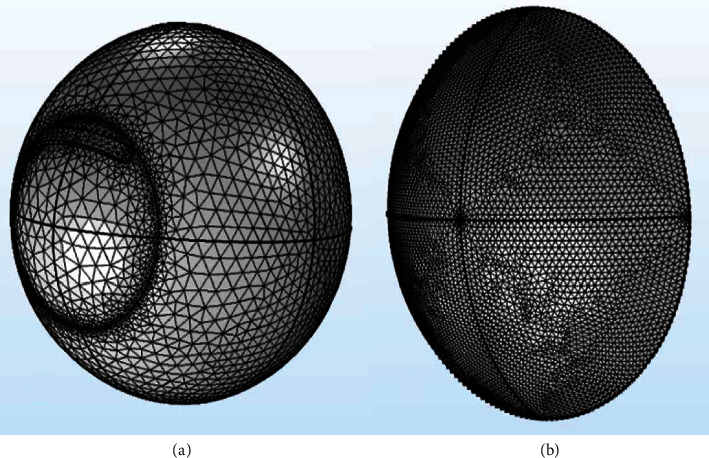
Meshing of the eye (a) and contact lens (b). The model was constructed using COMSOL Multiphysics v5.2 (https://www.comsol.com), and the collage of the exported images was made using Microsoft PowerPoint 2019 (https://www.microsoft.com/en-in/microsoft-365/get-started-with-office-2019).
2.3. Analysis
The outer surface of the sclera is fixed completely. During blink, the lid wiper is in contact with the cornea. Hence, a contact pair was created between these two surfaces. The dynamic friction coefficient of the contact surface between the cornea and the lid wiper was set to 0.1 with reference to the previous literature [57]. The eyelid itself exerts some amount of force over the cornea during blink [10]. Hence, a body load of 0.03 N was applied at the surface of the lid wiper [43]. In order to account for the effect of intraocular pressure (IOP), a boundary load of 15 mmHg (normal IOP of human eye ranges between 10 and 21 mmHg) was applied at the inner boundary of the aqueous humor.
Blink is simulated by making the lid wiper move over the cornea (Figure 1(c)). Parametric sweep analysis is carried out by displacing the lid wiper for every 10°, i.e., from the superior to the inferior portion of the cornea. Linear static analysis dealing with the contact problem was carried out. The whole analysis along with the parametric sweep required approximately 12 hours to complete. VMS and displacement were obtained as a result of FEA. VMS is a scalar value which determines whether a given material will yield (deform plastically) or fracture when a load is applied. In this study, the stress experienced by the cornea as a result of the force exerted by the lid wiper was estimated. Hence, VMS was chosen. In humans, stress represents the feeling of pain. Displacement is the distance at which one object has moved from its original location when an external force is applied. In this study, the displacement indicated how much cornea has moved from its original position as a result of force produced by the lid wiper during blink. This indicates the amount of biomechanical response in human tissues [58]. Surface plots were used to display the results of the analysis.
3. Results
The three-dimensional model of the eyeball (Figure 5) was created using the COMSOL Multiphysics (v5.2, COMSOL AB, Stockholm, Sweden) tool.
Figure 5.
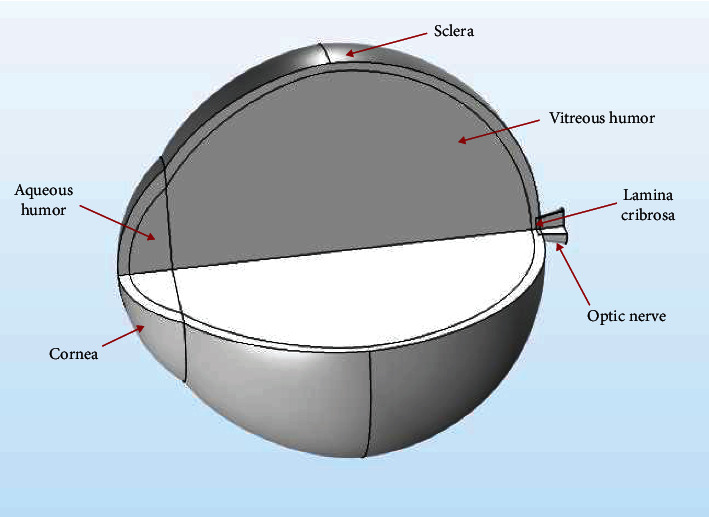
Three-dimensional model of the eyeball depicting the different ocular structures. The model was constructed using COMSOL Multiphysics v5.2 (https://www.comsol.com).
The biomechanical changes due to the blink were simulated using the FEM, and the results were obtained as von Mises stress (VMS) and displacement. Initially, the blink was simulated by displacing the lid wiper for every 10° (1.3 mm) using the parametric sweep. All the von Mises stress and displacement values are provided in Supplementary Table 2S.
3.1. Without Contact Lens
Figure 6 shows the VMS (kPa) of the lid wiper and cornea at different positions of lid wiper during blink without CL. Lid wiper underwent maximum VMS (32 kPa) when it interacted with the superior 1.3 mm of the cornea (Figure 7(a)). The maximum VMS was seen in the central 1.3 mm of the cornea (23 kPa) compared to the rest of the peripheral cornea during blink (Figure 8(a)). The maximum VMS was noted in the lid wiper (32 kPa) when compared to the cornea (23 kPa) during the interaction between them (Figure 6).
Figure 6.
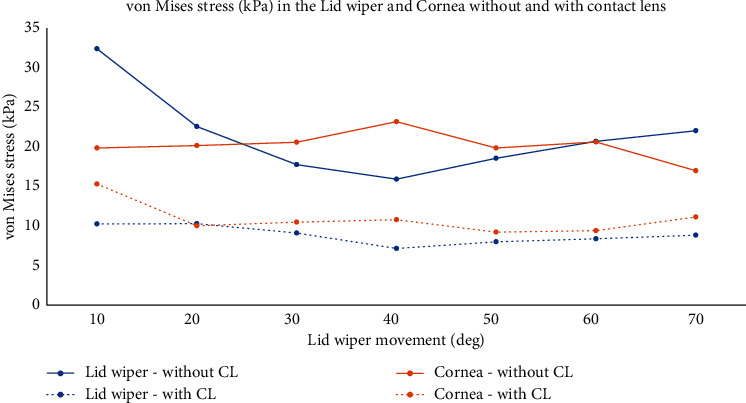
Von Mises stress (kPa) in the lid wiper and cornea during blink without and with CL when the lid wiper is moved at different positions from superior (10°) to inferior cornea (70°) (value of the data labels shows von Mises stress; unit: kPa). Graph drawn with Microsoft Excel 2019 (https://www.microsoft.com/en-in/microsoft-365/get-started-with-office-2019).
Figure 7.
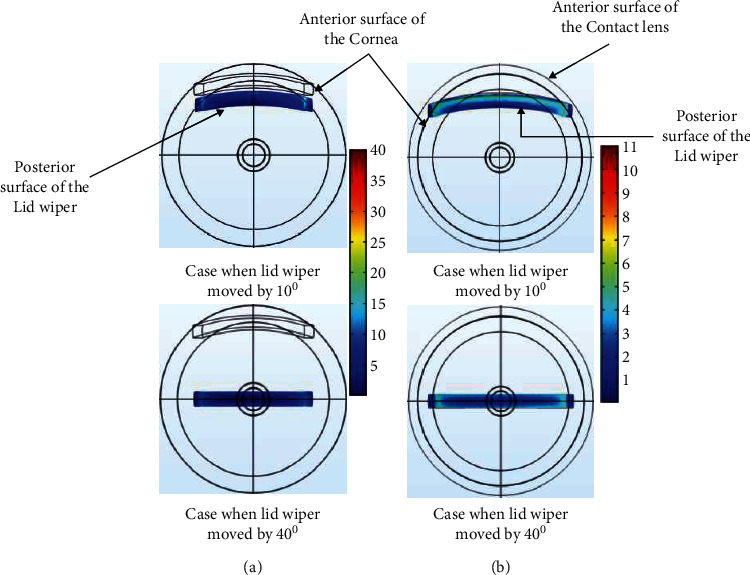
Contour plot of the von Mises stress in the lid wiper during blink without CL (a) and with CL (b) when the lid wiper is moved at superior (10°) and central position (40°) of the cornea (value of the legend shows von Mises stress; unit: kPa). The plots were exported as images from COMSOL Multiphysics v5.2 (https://www.comsol.com), and image collage was made using Microsoft PowerPoint 2019 (https://www.microsoft.com/en-in/microsoft-365/get-started-with-office-2019).
Figure 8.
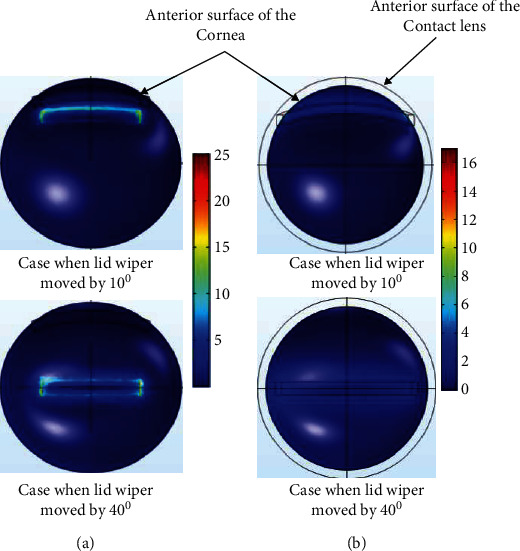
Contour plot of the von Mises stress in the cornea during blink without CL (a) and with CL (b) when the lid wiper is moved at superior (10°) and central position (40°) of the cornea (value of the legend shows von Mises stress; unit: kPa). The plots were exported as images from COMSOL Multiphysics v5.2 (https://www.comsol.com), and image collage was made using Microsoft PowerPoint 2019 (https://www.microsoft.com/en-in/microsoft-365/get-started-with-office-2019).
The displacement of the lid wiper was maximum when the lid wiper interacted with the central cornea. Displacement caused by the lid wiper on the cornea during blink is shown in Figure 9(a). It can be seen clearly that the central 1.3 mm of the cornea (120 µm) has been displaced more than the peripheral 2.6 mm of the cornea during blink (Figure 10).
Figure 9.
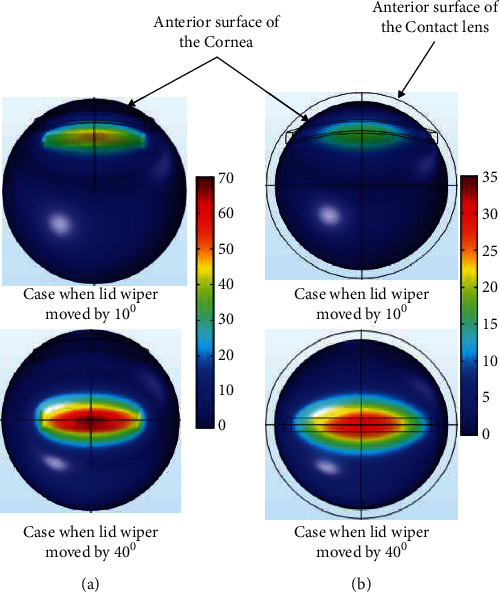
Contour plot of the displacement in the cornea during blink without CL (a) and with CL (b) when the lid wiper is moved at superior (10°) and central position (40°) of the cornea (value of the legend shows displacement; unit: µm). The plots were exported as images from COMSOL Multiphysics v5.2 (https://www.comsol.com), and image collage was made using Microsoft PowerPoint 2019 (https://www.microsoft.com/en-in/microsoft-365/get-started-with-office-2019).
Figure 10.
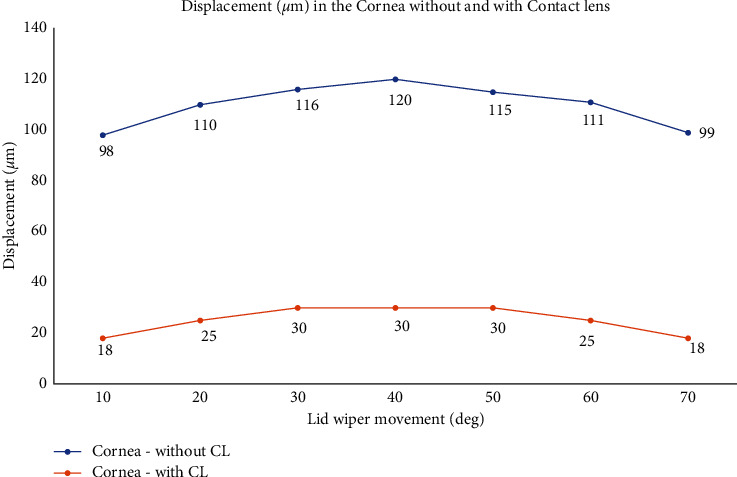
Displacement (µm) in the cornea during blink without and with CL when the lid wiper is moved at different positions from superior (10°) to inferior cornea (70°) (value of the data labels shows displacement; unit: µm). Graph drawn with Microsoft Excel 2019 (https://www.microsoft.com/en-in/microsoft-365/get-started-with-office-2019).
3.2. With Contact Lens
Figure 6 shows the VMS (kPa) of the lid wiper and cornea at different position of lid wiper during blink with CL. Lid wiper underwent maximum VMS (10 kPa) when it interacted with the superior 1.3 mm of the cornea (Figure 7(b)). The maximum VMS was seen in the superior 1.3 mm of the cornea (15 kPa) compared to the central 1.3 mm of the cornea (11 kPa) during blink (Figure 8(b)). Maximum VMS was noted in the cornea (15 kPa) compared to the lid wiper (10 kPa) during the interaction between them when CL was in situ (Figure 6).
The displacement of the lid wiper was maximum when the lid wiper interacted with the central 1.3 mm of the cornea. Displacement caused by the lid wiper on the cornea during blink is shown in Figure 9(b). It can be seen clearly that the central cornea (30 µm) has been displaced more than the peripheral cornea during blink (Figure 10).
4. Discussion
A three-dimensional model of the eyeball was created. The construction of the three-dimensional model of the eyeball used retrospective data from FEA studies [42, 59–62].
4.1. von Mises Stress and Displacement: Without Contact Lens
The current study aimed at quantifying the biomechanical changes such as VMS and displacement in the eye during blink. In this study, the VMS was found to be higher in the lid wiper than in the cornea. This large VMS on the lid wiper could be the reason for LWE seen in many patients with ocular dryness and discomfort [10, 14, 16, 63]. This also suggests that the lid wiper would be the first structure to get affected in any ocular surface disorder, even before a change is noticed in the cornea [14, 63]. Hence, the VMS developed during the rubbing could be the reason behind the formation of LWE especially in patients with dry eye disease [10, 64].
VMS was found to be larger in the central 1.3 mm of the cornea than in the peripheral cornea which makes it susceptible to injury by the lid wiper [16]. This is in accordance with the study done by Ousler et al. where they have reported that the ocular surface discomfort is more severe in patients with central corneal damage [65].
Maximum displacement is observed in the central 1.3 mm of the cornea than the peripheral cornea. This suggests that the force produced by the eyelid because of its body load (load that acts throughout the volume of the body) displaces the cornea by 120 µm posteriorly. This finding is in good accordance with the study by Masterton and Ahearne in which they have found out that during blink, the lid wiper pushes the cornea backwards, thereby causing thinning of the tear film, under this compressed area [66]. During blink, the rubbing of lid wiper may cause shear forces on the cornea. This combination of shear forces and displacement caused by the eyelid on the cornea can harm the health of the cornea [66].
One of the most accepted theories proposed by Wright is that the primary factor which causes the development of SLK is constant friction caused by the lid wiper on the conjunctiva and cornea due to excessive laxity of the lid wiper [67]. This has also been proven by one more study where they have found out that in cases of SLK there is upregulation of transforming growth factor-beta 2 (TGF-β2) and tenascin 13. These are the factors that are induced by mechanical trauma, thereby proving that mechanical trauma is one of the crucial factors in the development of SLK [52]. Thus, we can attribute the formation of SLK to the large amount of friction caused by the lid wiper on the superior 1.3 mm of the cornea during blink [68].
4.2. von Mises Stress and Displacement: With Contact Lens
Studies [10, 66] have proven that the introduction of contact lenses in the eye may disrupt the tear film, thereby dividing the tear film into pre- and post-lens tear film [69]. In some cases, the long-term use of the contact lens can result in the meibomian gland blockage and reduced tear film thickness, thereby causing more friction [70, 71]. This may also lead to the damage of the ocular surface, in some patients [10, 43]. The current study has found that the VMS is larger in the superior 1.3 mm of the cornea than in the central cornea when the CL is in situ. Thus, we can attribute the formation of contact lens-induced SEAL and LSCD to the friction caused by the lid wiper on the superior cornea during blink. In some cases, the inadequate lens flexure creates an area of misalignment in the superior epithelial cornea where pressure from the lid forces the lens against the cornea [72–73]. This produces greater frictional forces on the cornea in the superior region [17, 75]. This is how SEAL occurs in the cornea due to the friction caused by the CL wear [17]. It is reported that about 15.3% of the total LSCD cases are due to CL wear [76]. Mechanical trauma caused by the rubbing of the CL plays a central role in the etiology of CL-induced LSCD [18, 77, 78]. This rubbing is induced by the movement of the soft CL during blink [79]. LSCD due to CL wear is often asymptomatic [80] which makes it is necessary to suspect LSCD in CL wearers.
This study explores the possible mechanism behind the occurrence of certain ocular surface disorders such as SLK, LWE, SEAL, and LSCD in lens wearers and non-lens wearers using FEA. However, there are few limitations in our study. Since the cornea and bulbar conjunctiva follow different curvature, it is difficult to simulate complete blink. Hence, the effect of blink on the bulbar conjunctiva was not considered in this study. Biological systems are quite complex to model and simulate. With the current computing power and modeling and simulation tools available, there are limitations on the exact replication of biological systems, more so when they involve complex tribological aspects. During blink, the pressure exerted by the eyelid on the corneo-conjunctival complex varies depending upon the downward or upward motion of the eyelid. In this study, only the downward motion of the blink process was studied considering challenges with computational resources. Studying the upward phase of the eyelid would give a complete picture of the blinking process. Various theories have been proposed by researchers with regard to the tribological behavior of the human eye with and without contact lens [81]. Researchers say that the behavior is hydrodynamic when a thick tear film is present, and when there is no tear film, the lubrication behavior could be from boundary to mixed regime. Even when there is a tear film present, the tribological behavior could be in the elasto-hydrodynamic regime. In this study, the various regimes of lubrication are not considered, except maybe boundary, wherein there is almost no tear present. In future, studies involving the effect of the tear film and bulbar conjunctiva could give us further insights into the effect of the blink on the ocular surface.
5. Conclusion
In this study, we have found that, during blink, the lid wiper has displaced the cornea posteriorly by 30 µm. With the CL in situ, during blink, the lid wiper pushes the CL against the ocular surface, which effectively moves the tears away, causing the surface to dry, thereby creating friction [17]. Hence during blink, the CL slides over the high-pressure areas, i.e., the superior cornea and superior limbus. On long-term use of CL, this can induce significant trauma to the ocular surface [18, 78, 82–85]. We also noted in our study that, during the blink reflex, the lid wiper pressure is less as it approaches the inferior cornea. This is why the CL induces less mechanical trauma at the inferior cornea and limbus [18]. Hence, the occurrence of CL-induced LSCD is also uncommon in the inferior areas. Overall, FEA is a useful simulation tool that helps us to understand the effect of blink on a normal eye with and without CL. This can be extended to other wider areas of research including simulation of surgery and trauma.
Data Availability
Previously reported normative data used to support this study are cited at relevant places within the text as references [29–51, 53–56]. The data supporting the conclusion of this study are included within the article and in its supplementary information file.
Disclosure
The manuscript has been presented as a preprint in Research Square [86].
Conflicts of Interest
The authors declare that they have no conflicts of interest.
Authors' Contributions
S Meenatchi Sundaram and Ramesh S Ve conceptualized the study; S Meenatchi Sundaram, Ramesh S Ve, Rinu Thomas, and Vivek Suganthan Ramasubramanian formulated the methodology; Vivek Suganthan Ramasubramanian, S Meenatchi Sundaram, and Rakshath G Poojary constructed the model; Vivek Suganthan Ramasubramanian, S Meenatchi Sundaram, and Vernon Seth Crasto performed the analysis; Vivek Suganthan Ramasubramanian prepared the original draft of the manuscript; S Meenatchi Sundaram, Rinu Thomas, Ramesh S Ve, Raghuvir Pai B, Manali Hazarika, Shah Mohammed Abdul Khader, and Girish H revised and edited the manuscript; and S Meenatchi Sundaram, Rinu Thomas, Ramesh S Ve, Raghuvir Pai B, Manali Hazarika, and Shah Mohammed Abdul Khader supervised the work. All the authors have read and agreed to the published version of the manuscript.
Supplementary Materials
Table 1S: von Mises stress (kPa) and displacement (μm) in the lid wiper and cornea during blink without and with CL when the lid wiper is moved at different positions from superior (100) to inferior cornea (700). Table 2Sa: sensitivity analysis of the material properties of the cornea and lid wiper (von Mises stress). Table 2Sb: sensitivity analysis of the material properties of the cornea and lid wiper (displacement).
References
- 1.Nichols J. J., Willcox M. D., Bron A. J., et al. The TFOS international workshop on contact lens discomfort: executive summary. Investigative Ophthalmology & Visual Science . 2013;54:TFOS7–TFOS13. doi: 10.1167/iovs.13-13212. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 2.Pucker A. D., Jones-jordan L. A., Marx S. Clinical factors associated with contact lens dropout. Contact Lens and Anterior Eye . 2018;42:318–324. doi: 10.1016/j.clae.2018.12.002. [DOI] [PubMed] [Google Scholar]
- 3.Young G., Veys J., Pritchard N., Coleman S. A multi-centre study of lapsed contact lens wearers. Ophthalmic and Physiological Optics . 2002;22(6):516–527. doi: 10.1046/j.1475-1313.2002.00066.x. [DOI] [PubMed] [Google Scholar]
- 4.Sulley A., Young G., Hunt C. Factors in the success of new contact lens wearers. Contact Lens and Anterior Eye . 2017;40(1):15–24. doi: 10.1016/j.clae.2016.10.002. [DOI] [PubMed] [Google Scholar]
- 5.Dumbleton K., Caffery B., Dogru M., et al. The TFOS international workshop on contact lens discomfort: report of the subcommittee on epidemiology. Investigative Ophthalmology & Visual Science . 2013;54:TFOS20–TFOS36. doi: 10.1167/iovs.13-13125. [DOI] [PubMed] [Google Scholar]
- 6.Nichols K. K., Redfern R. L., Jacob J. T., et al. The TFOS international workshop on contact lens discomfort: report of the definition and classification subcommittee. Investigative Ophthalmology & Visual Science . 2013;54:TFOS14–TFOS19. doi: 10.1167/iovs.13-13074. [DOI] [PubMed] [Google Scholar]
- 7.Pucker A. D., Tichenor A. A. A review of contact lens dropout. Clinical Optometry . 2020;12:85–94. doi: 10.2147/opto.s198637. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Fonn D. Targeting contact lens induced dryness and discomfort: what properties will make lenses more comfortable. Optometry and Vision Science . 2007;84(4):279–285. doi: 10.1097/opx.0b013e31804636af. [DOI] [PubMed] [Google Scholar]
- 9.Subbaraman L. N., Pruitt J., Jones L. Measuring contact lens friction with multiple measurement variables and testing methods, is standardization possible? Contact Lens Spectrum . 2016;31:40–43. [Google Scholar]
- 10.Pult H., Tosatti S. G. P., Spencer N. D., Asfour J.-M., Ebenhoch M., Murphy P. J. Spontaneous blinking from a tribological viewpoint. Ocular Surface . 2015;13(3):236–249. doi: 10.1016/j.jtos.2014.12.004. [DOI] [PubMed] [Google Scholar]
- 11.Craig J. P., Nichols K. K., Akpek E. K., et al. TFOS DEWS II definition and classification report. Ocular Surface . 2017;15(3):276–283. doi: 10.1016/j.jtos.2017.05.008. [DOI] [PubMed] [Google Scholar]
- 12.Berry M., Pult H., Purslow C., Murphy P. J. Mucins and ocular signs in symptomatic and asymptomatic contact lens wear. Optometry and Vision Science: Official Publication of the American Academy of Optometry . 2008;85:E930–E938. doi: 10.1097/OPX.0b013e318188896b. [DOI] [PubMed] [Google Scholar]
- 13.Mang T. Encyclopedia of Lubricants and Lubrication . Berlin, Germany: Springer; 2014. [Google Scholar]
- 14.Korb D. R., Herman J. P., Greiner J. V., et al. Lid wiper epitheliopathy and dry eye symptoms. Eye and Contact Lens: Science and Clinical Practice . 2005;31:2–8. doi: 10.1097/01.icl.0000140910.03095.fa. [DOI] [PubMed] [Google Scholar]
- 15.Franzco I. C. Blink-related microtrauma: when the ocular surface harms itself. Clinical and Experimental Ophthalmology . 2003;31:183–190. doi: 10.1046/j.1442-9071.2003.00633.x. [DOI] [PubMed] [Google Scholar]
- 16.Kataoka R., Okamoto S., Lee J. H. Finite element analysis on friction developing on contact surfaces between eyeball and eyelid during blink. Lecture Notes in Engineering and Computer Science . 2018;2:751–755. [Google Scholar]
- 17.Holden B., Stephenson A., Stretton S. Superior epithelial arcuate lesions with soft contact lens wear. Optometry and Vision Science . 2001;78:9–12. doi: 10.1097/00006324-200101010-00008. [DOI] [PubMed] [Google Scholar]
- 18.Rossen J., Amram A., Milani B., et al. Contact lens-induced limbal stem cell deficiency. Ocular Surface . 2016;14:419–434. doi: 10.1016/j.jtos.2016.06.003. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Rennie A. C., Dickrell P. L., Sawyer W. G. Friction coefficient of soft contact lenses: measurements and modeling. Tribology Letters . 2005;18:499–504. doi: 10.1007/s11249-005-3610-0. [DOI] [Google Scholar]
- 20.Roba M., Duncan E. G., Hill G. A., Spencer N. D., Tosatti G. P. Friction measurements on contact lenses in their operating environment. Tribology Letters . 2011;44:387–397. doi: 10.1007/s11249-011-9856-9. [DOI] [Google Scholar]
- 21.Kim S. H., Opdahl A., Marmo C., Somorjai G. A. AFM and SFG studies of pHEMA-based hydrogel contact lens surfaces in saline solution: adhesion, friction, and the presence of non-crosslinked polymer chains at the surface. Biomaterials . 2002;23:1657–1666. doi: 10.1016/s0142-9612(01)00292-7. [DOI] [PubMed] [Google Scholar]
- 22.Kim S. H., Marmo C., Somorjai G. A. Friction studies of hydrogel contact lenses using AFM: non-crosslinked polymers of low friction at the surface. Biomaterials . 2001;22:3285–3294. doi: 10.1016/s0142-9612(01)00175-2. [DOI] [PubMed] [Google Scholar]
- 23.Papas E. B., Ciolino J. B., Jacobs D. The TFOS international workshop on contact lens discomfort: report of the management and therapy subcommittee. Investigative Ophthalmology & Visual Science . 2013;54:TFOS183–TFOS203. doi: 10.1167/iovs.13-13166. [DOI] [PubMed] [Google Scholar]
- 24.Brennan N. A. Contact lens-based correlates of soft lens wearing comfort. Optometry and Vision Science . 2009;86:8–10. [Google Scholar]
- 25.Jones L., Brennan N. A., Lally J., et al. The TFOS international workshop on contact lens discomfort: report of the contact lens materials, design, and care subcommittee. Investigative Ophthalmology & Visual Science . 2013;54:TFOS37–TFOS70. doi: 10.1167/iovs.13-13215. [DOI] [PubMed] [Google Scholar]
- 26.Hofmann G., Jubin P., Gerligand P. In-vitro method for determining corneal tissue friction and damage due to contact lens sliding. Biotriology . 2016;5:23–30. doi: 10.1016/j.biotri.2016.01.001. [DOI] [Google Scholar]
- 27.Sterner O., Aeschlimann R., Zurcher S., et al. Tribological classification of contact lenses: from coefficient of friction to sliding work. Tribology Letters . 2016;63:1–13. doi: 10.1007/s11249-016-0696-5. [DOI] [Google Scholar]
- 28.Bro-nielsen M. Finite element modeling in surgery simulation. Proceedings of the IEEE . 1998;86:490–503. doi: 10.1109/5.662874. [DOI] [Google Scholar]
- 29.Day K. D., Boyce M. C. The Mechanics of a Hydrogel Contact Lens on the Human Eye with a Lubricating Tear Layer . Cambridge, MA, USA: Massachusetts institute of Technology; 1999. [Google Scholar]
- 30.Al-Sukhun J., Lindqvist C., Kontio R. Modelling of orbital deformation using finite-element analysis. Journal of The Royal Society Interface . 2006;3:255–262. doi: 10.1098/rsif.2005.0084. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Bekerman I., Gottlieb P., Vaiman M. Variations in eyeball diameters of the healthy adults. Journal of Ophthalmology . 2014;2014:5. doi: 10.1155/2014/503645.503645 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Kiranantawat K., Suhk J. H. The asian eyelid: relevant anatomy. Seminars in Plastic Surgery . 2015;29:158–164. doi: 10.1055/s-0035-1556852. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 33.Vijaya L., George R., Arvind H. Central corneal thickness in adult south Indians: the Chennai glaucoma study. Ophthalmology . 2010;117:700–704. doi: 10.1016/j.ophtha.2009.09.025. [DOI] [PubMed] [Google Scholar]
- 34.Sridhar M. S. Anatomy of cornea and ocular surface. Indian Journal of Ophthalmology . 2018;66:190–194. doi: 10.4103/ijo.ijo_646_17. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 35.Dhakal R., Vupparaboina K. K., Verkicharla P. K. Anterior sclera undergoes thinning with increasing degree of myopia. Investigative Ophthalmology & Visual Science . 2020;61 doi: 10.1167/iovs.61.4.6. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Jesus D. A., Kedzia R., Iskander D. R. Precise measurement of scleral radius using anterior eye profilometry. Contact Lens and Anterior Eye . 2017;40:47–52. doi: 10.1016/j.clae.2016.11.003. [DOI] [PubMed] [Google Scholar]
- 37.Shaw A. J. B., Collins M. J., Davis B. A., Carney L. G. Eyelid pressure and contact with the ocular surface. Investigative Ophthalmology & Visual Science . 2010;51:1911–1917. doi: 10.1167/iovs.09-4090. [DOI] [PubMed] [Google Scholar]
- 38.Ho A., Evans S. Finite element modelling of soft contact lens flexure and aberrations. Proceedings of the SPIE—The International Society for Optical Engineering; December 2004; Denver, CO, USA. pp. 195–200. [Google Scholar]
- 39.Moore J., Lopes B. T., Eliasy A. Simulation of the effect of material properties on soft contact lens on-eye power. Bioengineering . 2019;6:1–22. doi: 10.3390/bioengineering6040094. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 40.Dan B. N., Augustin S., Mariana M. I., Doina N. O. Computer assisted design and finite element analysis of contact lenses. Romanian Journal of Ophthalmology . 2016;60:132–137. [PMC free article] [PubMed] [Google Scholar]
- 41.White P. 2018 contact lenses & solutions summary. Contact Lens Spectrum . 2018;15:7–8. [Google Scholar]
- 42.Dai P., Zhao Y., Sheng H. Simulating the effects of elevated intraocular pressure on ocular structures using a global finite element model of the human eye. Journal of Mechanics in Medicine and Biology . 2017;17:1–17. doi: 10.1142/s0219519417500385. [DOI] [Google Scholar]
- 43.Jones M. B., Fulford G. R., Please C. P. Elastohydrodynamics of the eyelid wiper. Bulletin of Mathematical Biology . 2008;70:323–343. doi: 10.1007/s11538-007-9252-7. [DOI] [PubMed] [Google Scholar]
- 44.Aache P. G., Monneur C., Leveque J. L., Rigal J. D. Mechanical properties and young’s modulus of human skin in vivo. Archives of Dermatological Research . 1980;269:221–232. doi: 10.1007/BF00406415. [DOI] [PubMed] [Google Scholar]
- 45.Sigal I. A., Flanagan J. G., Tertinegg I., Ethier C. R. Finite element modeling of optic nerve head biomechanics. Investigative Ophthalmology & Visual Science . 2005;45:4378–4387. doi: 10.1167/iovs.04-0133. [DOI] [PubMed] [Google Scholar]
- 46.Liang X., Boppart S. Biomechanical properties of in vivo human skin from dynamic optical coherence elastography. IEEE Transactions on Biomedical Engineering . 2010;57:953–959. doi: 10.1109/tbme.2009.2033464. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Hamilton K. E., Pye D. C. Young’s modulus in normal corneas and the effect on applanation tonometry. Optometry and Vision Science . 2008;85:445–450. doi: 10.1097/opx.0b013e3181783a70. [DOI] [PubMed] [Google Scholar]
- 48.Uchio E., Ohno S., Kudoh J. Simulation model of an eyeball based on finite element analysis on a supercomputer. British Journal of Ophthalmology . 1999;83:1106–1111. doi: 10.1136/bjo.83.10.1106. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 49.Power E. D., Duma S. M., West R. L. A Nonlinear Finite Element Model of the Human Eye to Investigate Ocular Injuries from Night Vision Goggles . Blacksburg, VA, USA: Virginia Polytechnic Institute and State University; 2001. [Google Scholar]
- 50.Rossi T., Boccassini B., Esposito L., et al. Primary blast injury to the eye and orbit: finite element modeling. Investigative Ophthalmology & Visual Science . 2012;53:8057–8066. doi: 10.1167/iovs.12-10591. [DOI] [PubMed] [Google Scholar]
- 51.Sigal I. A., Flanagan J. G., Ethier C. R. Factors influencing optic nerve head biomechanics. Investigative Ophthalmology & Visual Science . 2005;46:4189–4199. doi: 10.1167/iovs.05-0541. [DOI] [PubMed] [Google Scholar]
- 52.Matsuda A., Tagawa Y., Matsuda H. Cytokeratin and proliferative cell nuclear antigen expression in superior limbic keratoconjunctivitis. Current Eye Research . 1996;15:1033–1038. doi: 10.3109/02713689609017652. [DOI] [PubMed] [Google Scholar]
- 53.Roy A. S., Dupps W. J. Effects of altered corneal stiffness on native and postoperative LASIK corneal biomechanical behavior: a whole-eye finite element analysis. Journal of Refractive Surgery . 2009;25:875–887. doi: 10.3928/1081597x-20090917-09. [DOI] [PubMed] [Google Scholar]
- 54.Jones L. W., Subbaraman L., Dumbleton K. A. Surface treatment, wetting and modulus of silicone hydrogels. Optician . 2006;232:28–34. [Google Scholar]
- 55.Toolbox E. Water—Density, Specific Weight and Thermal Expansion Coefficient . New Haven, CT, USA: The Engineering ToolBox; 2003. [Google Scholar]
- 56.Coopervision. BIOFINITY® (Comfilcon A) Soft (Hydrophilic) Contact Lenses for Planned Replacement . San Ramon, CA, USA: Coopervision; 2014. [Google Scholar]
- 57.Okamoto S., Pranoto S., Ohwaki Y. Development of a physical apparatus and computational program employing a genetic algorithm and least-squares method for measuring the frictional coefficient of the human ocular surface. Proceedings of the 2nd World Congress on Electrical Engineering and Computer Systems and Science; July 2016; Budapest, Hungary. pp. 1–8. [DOI] [Google Scholar]
- 58.Eilaghi A., Flanagan J., Simmons C. A., Ethier C. R. Effects of scleral stiffness properties on optic nerve head biomechanics. Annals of Biomedical Engineering . 2010;38:1586–1592. doi: 10.1007/s10439-009-9879-7. [DOI] [PubMed] [Google Scholar]
- 59.Shukla V. FEA investigation of a human eye model subjected to intra-ocular pressure (IOP) and external pressure. Journal of Applied Mechanics . 2017;2:1–14. [Google Scholar]
- 60.Heussner N., Holl L., Shults A. Thermodynamic finite-element-method (FEM) eye model for laser safety considerations. Proceedings of the SPIE—The International Society for Optical Engineering; February 2013; Porto, Portugal. pp. 1–8. [DOI] [Google Scholar]
- 61.Liu X., Wang L., Wang C., Sun G., Liu S., Fan Y. Mechanism of traumatic retinal detachment in blunt impact: a finite element study. Journal of Biomechanics . 2013;46:1321–1327. doi: 10.1016/j.jbiomech.2013.02.006. [DOI] [PubMed] [Google Scholar]
- 62.Liu X., Wang L., Ji J., Fan Y. The protective effect of the eyelid on ocular injuries in blunt trauma. World Biomedical Engineering and Medical Physics . 2015;51:338–341. doi: 10.1007/978-3-319-19387-8_81. [DOI] [Google Scholar]
- 63.Greiner J. V., Korb D. R., Herman J. P. Dry eye signs and symptoms and lid wiper epitheliopathy. Ocular Surface . 2005;3:p. S68. doi: 10.1016/s1542-0124(12)70422-6. [DOI] [Google Scholar]
- 64.Li W., Yeh T. N., Leung T., Yuen T., Lerma M., Lin M. C. The relationship of lid wiper epitheliopathy to ocular surface signs and symptoms. Investigative Ophthalmology & Visual Science . 2018;59:1878–1887. doi: 10.1167/iovs.17-23639. [DOI] [PubMed] [Google Scholar]
- 65.Ousler G. W., Kellerman D., Durham T. A correlation between central corneal staining and dry eye symptomatology. Investigative Ophthalmology & Visual Science . 2006;47 [Google Scholar]
- 66.Masterton S., Ahearne M. Mechanobiology of the corneal epithelium. Experimental Eye Research . 2018;177:122–129. doi: 10.1016/j.exer.2018.08.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Wright P. Superior limbic keratoconjunctivitis. Transactions of the American Ophthalmological Society . 1972;92:555–560. [PubMed] [Google Scholar]
- 68.Cher I. Superior limbic keratoconjunctivitis: multifactorial mechanical pathogenesis. Clinical and Experimental Ophthalmology . 2000;28:181–184. doi: 10.1046/j.1442-9071.2000.00284.x. [DOI] [PubMed] [Google Scholar]
- 69.Muntz A., Subbaraman L. N., Sorbara L., Jones L. Tear exchange and contact lenses: a review. Journal of Optics . 2015;8:2–11. doi: 10.1016/j.optom.2014.12.001. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Siddireddy J. S., Vijay A. K., Tan J., Willcox M. The eyelids and tear film in contact lens discomfort. Contact Lens and Anterior Eye . 2018;41:144–153. doi: 10.1016/j.clae.2017.10.004. [DOI] [PubMed] [Google Scholar]
- 71.Craig J. P., Willcox M. D. P., Arg P. The TFOS international workshop on contact lens discomfort: report of the contact lens interactions with the tear film subcommittee. Investigative Ophthalmology & Visual Science . 2013;54:TFOS123–TFOS156. doi: 10.1167/iovs.13-13235. [DOI] [PubMed] [Google Scholar]
- 72.Jalbert I., Sweeney D., Holden B. Epithelial split associated with wear of a silicone hydrogel contact lens. CLAO Journal . 2001;27:231–233. [PubMed] [Google Scholar]
- 73.Carnt N., Stapleton F., Naduvilath T., Jalbert I., Sweeney D. F., Holden A. Interaction between the contact lens and the ocular surface in the etiology of superior epithelial arcuate lesions. Advances in Experimental Medicine & Biology . 2002;506:973–980. doi: 10.1007/978-1-4615-0717-8_36. [DOI] [PubMed] [Google Scholar]
- 74.Young G., Mirejovsky D. A hypothesis for the aetiology of soft contact lens-induced superior arcuate keratopathy. International Contact Lens Clinic . 1993;20:177–180. doi: 10.1016/0892-8967(93)90114-7. [DOI] [Google Scholar]
- 75.Lin M. C., Yeh T. N. Mechanical complications induced by silicone hydrogel contact lenses. Eye and Contact Lens: Science and Clinical Practice . 2013;39:115–124. doi: 10.1097/icl.0b013e31827c77fd. [DOI] [PubMed] [Google Scholar]
- 76.Donisi P. M., Rama P., Fasolo A., Ponzin D. Analysis of limbal stem cell deficiency by corneal impression cytology. Cornea . 2003;22:533–538. doi: 10.1097/00003226-200308000-00009. [DOI] [PubMed] [Google Scholar]
- 77.Ahmad S. Concise review: limbal stem cell deficiency, dysfunction, and distress. STEM CELLS Translational Medicine . 2012;1:110–115. doi: 10.5966/sctm.2011-0037. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 78.Lee S. C., Hyon J. Y., Jeon H. S. Contact lens induced limbal stem cell deficiency: clinical features in Korean patients. Korean Journal of Ophthalmology . 2019;33:500–505. doi: 10.3341/kjo.2019.0095. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 79.Truon T., Graham A., Lin M. Factors in contact lens symptoms: evidence from a multistudy database. Optometry and Vision Science . 2014;91:133–141. doi: 10.1097/opx.0000000000000138. [DOI] [PubMed] [Google Scholar]
- 80.Chan C. C., Holland E. J. Severe limbal stem cell deficiency from contact lens wear: patient clinical features. American Journal of Ophthalmology . 2013;155:544.e2–549.e2. doi: 10.1016/j.ajo.2012.09.013. [DOI] [PubMed] [Google Scholar]
- 81.Dunn A. C., Tichy J. A., Uruenã J. M., Sawyer W. G. Lubrication regimes in contact lens wear during a blink. Tribology International . 2013;63:45–50. doi: 10.1016/j.triboint.2013.01.008. [DOI] [Google Scholar]
- 82.Bhatia R. P., Srivastava R., Ghosh A. Limbal stem cell study in contact lens wearers. Annals of Ophthalmology . 2009;41:87–92. [PubMed] [Google Scholar]
- 83.Bloomfield S. E., Jakobiec F. A., Theodore F. H. Contact lens-induced keratopathy: a severe complication extending the spectrum of keratoconjunctivitis in contact lens wearers. Ophthalmology . 1984;91:290–294. doi: 10.1016/s0161-6420(84)34308-1. [DOI] [PubMed] [Google Scholar]
- 84.Jeng B. H., Halfpenny C. P., Meisler D. M., Stock E. L. Management of focal limbal stem cell deficiency associated with soft contact lens wear. Cornea . 2011;30:18–23. doi: 10.1097/ico.0b013e3181e2d0f5. [DOI] [PubMed] [Google Scholar]
- 85.Kim B. Y., Riaz K. M., Bakhtiari P., et al. Medically reversible limbal stem cell disease: clinical features and management strategies. Ophthalmology . 2014;121:2053–2058. doi: 10.1016/j.ophtha.2014.04.025. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Vivek R. V. S., Sundaram S. M., Thomas R., et al. Finite element analysis of cornea and lid wiper during blink with and without contact lens. 2020. [DOI] [PMC free article] [PubMed]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Table 1S: von Mises stress (kPa) and displacement (μm) in the lid wiper and cornea during blink without and with CL when the lid wiper is moved at different positions from superior (100) to inferior cornea (700). Table 2Sa: sensitivity analysis of the material properties of the cornea and lid wiper (von Mises stress). Table 2Sb: sensitivity analysis of the material properties of the cornea and lid wiper (displacement).
Data Availability Statement
Previously reported normative data used to support this study are cited at relevant places within the text as references [29–51, 53–56]. The data supporting the conclusion of this study are included within the article and in its supplementary information file.


