Abstract
In oral endoscopy, linked color imaging (LCI) detects atrophic border and gastric mucosal diseases better than white light imaging (WLI), but its usefulness in transnasal endoscopy has not been fully investigated. Here, we retrospectively compared WLI and LCI using the L*a*b* color space in images from 57 patients aged ≥20 years who had undergone transnasal endoscopy as part of a health check-up from May 2016 to January 2017. We measured color differences at the atrophic/non-atrophic and fundic/pyloric mucosal borders. Gastritis severity scored using the Kyoto classification of gastritis was similar between the two techniques. However, in patients with current and with past Helicobacter pylori infection, color difference at the atrophic border was greater with LCI (21.58 ± 6.97 and 27.34 ± 10.32, respectively) than with WLI [14.42 ± 5.95 (p = 0.004) and 17.9 ± 8.48 (p<0.001)]; in those never infected with Helicobacter pylori, color difference at the fundic/pyloric mucosal border was greater with LCI than with WLI (p<0.001). Because of its enhancement of atrophic border detection, we recommend linked color imaging as the method of choice for transnasal endoscopy in health check-ups, particularly for identifying people at high risk of gastric cancer.
Keywords: linked color imaging, transnasal endoscopy, atrophic border, Helicobacter pylori, Kyoto classification of gastritis
Introduction
The World Health Organization declared in 1994 that infection with Helicobacter pylori (H. pylori) is an important risk factor for gastric cancer.(1) At present, infection with H. pylori is broadly recognized as the most important risk factor for the development of gastric cancer. An observational study in Japan showed that 99.34% of 3,161 patients with gastric cancer were positive for H. pylori infection.(2) Gastric cancer was not detected among people negative for H. pylori infection during mean observation period of 7.8 years, whereas patients who were positive for H. pylori developed gastric cancer at a rate of 0.4% annually (differentiated: 63.4%; non-differentiated: 36.1%).(3) Moreover, many studies have demonstrated that eradication therapy of H. pylori significantly reduces the development of solitary and metachronous gastric cancers. A meta-analysis demonstrated that eradication therapy could decrease the relative risk of gastric cancer to around 0.5.(4–6) Therefore, to identify people at high risk of gastric cancer, it is important to determine the presence or absence of H. pylori.
Japan has a high prevalence of H. pylori infection, and the prevalence of gastric cancer is also high, as it is in other East Asian countries (https://www.wcrf.org/dietandcancer/stomach-cancer-statistics/).(7) To address this, health insurance coverage was approved in 2012 for eradication therapy for those positive for H. pylori infection, if endoscopy confirmed that there is H. pylori-associated gastritis and no gastric cancer.(8) However, although eradication can reduce the risk of gastric cancer, it cannot prevent it entirely. Therefore, it is important to efficiently detect patients at high risk of gastric cancer and/or to perform periodic health checks after eradication. The Kyoto classification of gastritis was proposed in 2016 to categorize the endoscopic characteristics of patients with H. pylori infection and assess the risk of gastric cancer. Five parameters including atrophy, intestinal epithelial metaplasia, mucosal fold enlargement, nodularity, and diffuse redness are scored, and the characteristics of H. pylori infection are assessed as currently infected, previously infected, or never infected, based on endoscopic findings. Characteristic endoscopic findings for never-infected patients include a regular arrangement of collecting venules (RAC) at gastric angle and fundic gland polyps. Current infection is characterized by diffuse redness, mucosal enlargement, mucosal fold enlargement, and nodularity as a result of inflammatory cell infiltration. Because some findings such as gastric mucosal atrophy, intestinal metaplasia, and xanthoma may be present after eradication, differentiation between current and past infection requires careful assessment.(9–12) Furthermore, Nishizawa et al.(13) reported that simplified Kyoto classification score was consistent with the ABC method of classification as a grading system for endoscopic gastritis. Developments in endoscopic instrumentation and image-enhancement techniques (image enhancement endoscopy: IEE) including narrow band imaging (NBI), blue laser imaging (BLI), and linked color imaging (LCI) have improved the detection rate of gastric cancer and intestinal epithelial metaplasia.(14–18) LCI uses narrow-band, short-wavelength light to increase the observed gastric mucosal color differences. Used with oral endoscopy, LCI facilitates the identification of endoscopic atrophic/non-atrophic border and is useful for the diagnosis of H. pylori infection.(12,18,19) However, transnasal endoscopy has become popular in the current medical screening environment in Japan because it is relatively pain-free for the patient; it is also recommended in the endoscopy manual for gastric cancer screening as the method causing patients the least discomfort. It has been reported that transnasal and oral endoscopy have different rates of detection of upper gastrointestinal diseases, but IEE techniques may compensate for this difference. To date, there have been no reports comparing the effectiveness of white light imaging (WLI) and LCI for objectively evaluating the risk factors for gastric cancer (e.g., atrophy, intestinal metaplasia, xanthoma, and map-like redness) using transnasal endoscopy. Because of an increase in medical health check-ups, the number of transnasal endoscopy procedures is increasing, so it is prudent to evaluate its usefulness.
To this end, we investigated whether transnasal endoscopy using LCI could improve the visibility of gastric cancer risk based on the Kyoto classification of gastritis, including endoscopic atrophy and diffuse redness, compared with WLI. In addition, we quantified the color difference at the atrophic border and compared the values obtained with LCI and WLI.
Materials and Methods
Study design and patients
This was a retrospective single-center observational study conducted at Tokyo Medical University Hospital. We examined endoscopy images from 57 patients aged ≥20 years who had undergone transnasal endoscopy using WLI and LCI as part of a health check-up between May 2016 and January 2017. Exclusion criteria were a history of gastric surgery, receiving chemotherapy, and a lack of clear images to evaluate endoscopic findings using WLI and LCI.
The study protocol was approved by the institutional review board of Tokyo Medical University (T2020-0059) and the study was performed in accordance with the ethical standards laid down in the 1964 Declaration of Helsinki and its later amendments. Because this study was a retrospective investigation and, as such, written informed consent was not obtained from each enrolled patient, a document describing an opt-out policy through which patients and/or relatives could refuse inclusion was uploaded to the Tokyo Medical University Hospital website.
Endoscopy and severity of gastritis
We used an EG-L580NW endoscope with the LASEREO system (Fujifilm Co., Tokyo, Japan), which is capable of producing light suitable for WLI and LCI. During endoscopy, the borders between atrophic and non-atrophic mucosa and between fundic and pyloric mucosa were identified and the severity of gastritis was scored according to the Kimura–Takemoto classifications and the Kyoto classifications of gastritis.(9,20) In the Kyoto classification of gastritis, the total score includes five parameters of gastritis: atrophy (Kimura–Takemoto C1 = Kyoto A0; C2–C3 = A1, and O1–O3 = A2), intestinal metaplasia (none, IM0; within antrum, IM1; up to corpus, IM2), hypertrophy of gastric folds (negative, H0; positive, H1), nodularity (negative, N0; positive, N1), and diffuse redness (negative, DR0; mild, DR1; moderate–severe, DR2).(10,21–23) The Kyoto classification risk score was calculated as the total score (0–8) of the five subscores. Two researchers (YK and MS) evaluated the quality of the findings between WLI and LCI, and the images deemed to have clearly increased visibility were classed as enhanced.
Helicobacter pylori infection
All patients were tested for H. pylori infection using the rapid urease test (Helicocheck®; Institute of Immunology Co., Ltd., Tochigi, Japan), an anti-H. pylori IgG test (antibody determination kit, E-Plate Eiken H. pylori antibody; cut-off, 10 U/ml), and the 13C-urea breath test (UBIT 100 mg tablets, Otsuka Pharmaceutical Co., Ltd.; cut-off, 2.5‰). Patients were diagnosed as H. pylori infection-positive if at least one of the three tests was positive. If all tests of H. pylori infection were negative and there was no endoscopic atrophy and intestinal metaplasia, the patient was classed as never infected with H. pylori.
Color measurement
Color differences at the borders between atrophic and non-atrophic mucosa and between fundic and pyloric mucosa were measured and compared between WLI and LCI images.(18) In each patient, we chose at random three pairs of areas at the border between atrophic and non-atrophic mucosa and between fundic and pyloric mucosa and calculated the color differences at these borders.
Color differences (ΔE) were calculated using the L*a*b* color space devised by the International Commission on Illumination (CIE) in 1976.(24,25) The L*a*b* color space is a three-dimensional model composed of a black–white axis (L*, brightness), a red–green axis (a*), and a yellow–blue axis (b*). ΔE expresses the distance between two points in the color space and is calculated using the following formula: [(ΔL*)2 + (Δa*)2 + (Δb*)2]1/2, where ΔL*, Δa*, and Δb* are, respectively, the differences in the L*, a*, and b* values between the atrophic and non-atrophic mucosa. Each ΔL*, Δa*, and Δb* value was measured by a single computer operator with no clinical information or knowledge about atrophy, using Adobe Photoshop 22.5.1 (Adobe KK, Tokyo, Japan).
Statistical analysis
Age and body mass index are expressed as the mean ± SD. Numbers of patients in the three groups (currently infected, previously infected, and never infected), and numbers of patients who underwent WLI and LCI were summarized as n (%) and compared using χ2 tests. Statistically significant differences in mean endoscopic scores using the Kyoto classification and mean ΔE between the WLI and LCI groups were determined using Student’s t test. All statistical analyses were performed using SPSS 27.0 (IBM Japan, Tokyo, Japan).
Results
Patient characteristics
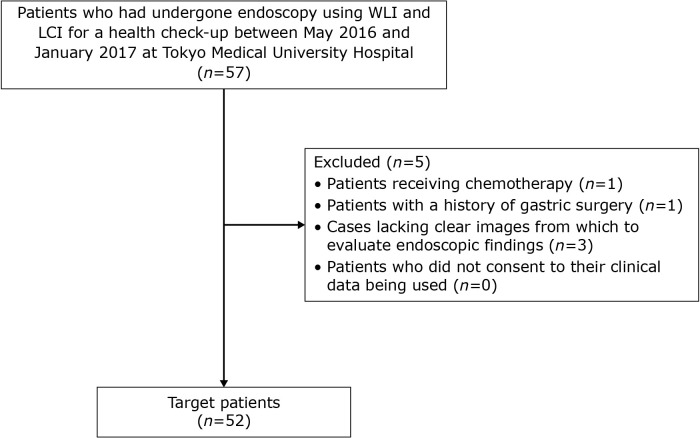
We identified a total of 57 patients who had undergone endoscopy using WLI and LCI as part of a health check-up (Fig. 1). Of these, five patients met an exclusion criterion (receiving chemotherapy, n = 1; remnant stomach, n = 1; insufficiently clear images to evaluate endoscopic findings using WLI and LCI, n = 3) (Fig. 1).
Fig. 1.
Workflow for patient enrollment to evaluate the atrophic border by transnasal endoscopy using linked color imaging.
The patient characteristics and H. pylori infection status rates are shown in Table 1. When we divided patients into three groups based on the status of H. pylori infection, the percentages of patients who were currently infected (at the time of endoscopy), previously infected, and never infected were 25.0% (13/52), 34.6% (18/52), and 40.3% (21/52), respectively.
Table 1.
Patient characteristics
| All patients (n = 52) |
Helicobacter pylori infection | p value | |||
|---|---|---|---|---|---|
| Currently infected (n = 13) |
Previously infected (n = 18) |
Never infected (n = 21) |
|||
| Demographics | |||||
| Age, years (mean ± SD) | 64.6 ± 13.8 | 62.5 ± 13.9 | 71.6 ± 12.4 | 62.8 ± 12.3 | 0.035 |
| Sex [male, n (%)] | 27 (51.9%) | 6 (46.2%) | 11 (21.2%) | 10 (47.6%) | 0.626 |
| Body mass index, kg/m2 (mean ± SD) | 22.9 ± 3.18 | 23.0 ± 2.57 | 23.7 ± 3.82 | 22.0 ± 2.69 | 0.113 |
| H. pylori infection [n (%)] | 13 (25.0%) | 13 (100%) | 0 (0%) | 0 (0%) | <0.001 |
| Diseases | |||||
| Hypertension [n (%)] | 17 (32.7%) | 3 (23.1%) | 7 (38.9%) | 7 (33.3%) | 0.649 |
| Diabetes mellitus [n (%)] | 4 (7.7%) | 1 (7.7%) | 3 (16.7%) | 0 (0%) | 0.15 |
| Heart disease [n (%)] | 17 (32.7%) | 4 (30.8%) | 8 (44.4%) | 5 (23.8%) | 0.386 |
| Cancer [n (%)] | 5 (9.6%) | 1 (7.7%) | 3 (16.7%) | 1 (4.8%) | 0.437 |
Severity of endoscopic gastritis in patients with different H. pylori infection statuses
Kyoto classification scores for gastritis were similar for WLI and LCI (Table 2 and 3). When we evaluated the quality of endoscopic findings and compared WLI and LCI images, deeming only those with clearly increased visibility as being enhanced, LCI was identified as superior to WLI for evaluating atrophy, intestinal metaplasia, and diffuse redness in 21.1% (11/52), 15.4% (8/52), and 3.8% (2/52) of patients, respectively, across all infection status groups (Table 3). Notably, LCI was endoscopically superior to WLI in 44.4% (8/18) of patients with past infection (Table 3).
Table 2.
Severity of endoscopic gastritis in patients with different Helicobacter pylori infection statuses
| All patients (n = 52) |
H. pylori infection | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Currently infected (n = 13) |
Previously infected (n = 18) |
Never infected (n = 21) |
||||||||||||||
| WLI | LCI | p value | WLI | LCI | p value | WLI | LCI | p value | WLI | LCI | p value | |||||
| Kimura–Takemoto classification | ||||||||||||||||
| Atrophy | C0 | 19 | 18 | 1 | 0 | 0 | 1 | 0 | 0 | 0.98 | 19 | 18 | 0.598 | |||
| C1 | 2 | 2 | 0 | 0 | 0 | 0 | 2 | 2 | ||||||||
| C2 | 8 | 9 | 2 | 2 | 6 | 6 | 0 | 1 | ||||||||
| C3 | 2 | 2 | 0 | 0 | 2 | 2 | 0 | 0 | ||||||||
| O1 | 7 | 7 | 4 | 4 | 3 | 3 | 0 | 0 | ||||||||
| O2 | 10 | 9 | 4 | 4 | 6 | 5 | 0 | 0 | ||||||||
| O3 | 4 | 5 | 3 | 3 | 1 | 2 | 0 | 0 | ||||||||
| Kyoto classification | ||||||||||||||||
| Atrophy | A0 | 21 | 20 | 1 | 0 | 0 | 1 | 0 | 0 | 1 | 21 | 20 | 1 | |||
| A1 | 10 | 11 | 2 | 2 | 8 | 8 | 0 | 1 | ||||||||
| A2 | 21 | 21 | 11 | 11 | 10 | 10 | 0 | 0 | ||||||||
| Intestinal metaplasia | IM0 | 36 | 34 | 0.796 | 5 | 4 | 0.856 | 10 | 9 | 0.881 | 21 | 21 | 1 | |||
| IM1 | 4 | 6 | 2 | 3 | 2 | 3 | 0 | 0 | ||||||||
| IM2 | 12 | 12 | 6 | 6 | 6 | 6 | 0 | 0 | ||||||||
| Enlarged folds | H0 | 48 | 48 | 1 | 9 | 9 | 1 | 18 | 18 | 1 | 21 | 21 | 1 | |||
| H1 | 4 | 4 | 4 | 4 | 0 | 0 | 0 | 0 | ||||||||
| Nodular gastritis | N0 | 51 | 51 | 1 | 12 | 12 | 1 | 18 | 18 | 1 | 21 | 21 | 1 | |||
| N1 | 1 | 1 | 1 | 1 | 0 | 0 | 0 | 0 | ||||||||
| Diffuse redness | DR0 | 40 | 38 | 0.86 | 4 | 3 | 0.881 | 15 | 14 | 0.674 | 21 | 21 | 1 | |||
| DR1 | 7 | 9 | 4 | 5 | 3 | 4 | 0 | 0 | ||||||||
| DR2 | 5 | 5 | 5 | 5 | 0 | 0 | 0 | 0 | ||||||||
| Xanthoma | Negative | 46 | 46 | 1 | 11 | 11 | 1 | 14 | 14 | 1 | 21 | 21 | 1 | |||
| Positive | 6 | 6 | 2 | 2 | 4 | 4 | 0 | 0 | ||||||||
LCI, linked color imaging; WLI, white light imaging.
Table 3.
Superiority of LCI vs WLI for evaluating endoscopic findings
| All patients (n = 52) |
Helicobacter pylori infection | ||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Currently infected (n = 13) |
Previously infected (n = 18) |
Never infected (n = 21) |
|||||||||||||
| WLI | Equal | LCI | WLI | Equal | LCI | WLI | Equal | LCI | WLI | Equal | LCI | ||||
| Atrophy | 0 | 41 | 11 | 0 | 10 | 3 | 0 | 10 | 8 | 0 | 20 | 1 | |||
| Intestinal metaplasia | 0 | 44 | 8 | 0 | 12 | 1 | 0 | 17 | 1 | 0 | 21 | 0 | |||
| Enlarged folds | 0 | 52 | 0 | 0 | 13 | 0 | 0 | 18 | 0 | 0 | 21 | 0 | |||
| Nodular gastritis | 0 | 52 | 0 | 0 | 13 | 0 | 0 | 18 | 0 | 0 | 21 | 0 | |||
| Diffuse redness | 0 | 50 | 2 | 0 | 12 | 1 | 0 | 17 | 1 | 0 | 21 | 0 | |||
| Xanthoma | 0 | 52 | 0 | 0 | 13 | 0 | 0 | 18 | 0 | 0 | 21 | 0 | |||
LCI, linked color imaging; WLI, white light imaging.
Color differences at the endoscopic gastric atrophic border in patients with different H. pylori infection statuses
The color differences at the atrophic border in patients with current or past infection were significantly greater using LCI than those obtained using WLI (Table 4). The color differences at the atrophic border on LCI images in patients with current or past H. pylori infection (21.58 ± 6.97 and 27.34 ± 10.32, respectively) were significantly larger than those on WLI images [14.42 ± 5.95 (p = 0.004) and 17.9 ± 8.48 (p<0.001)] (Table 4).
Table 4.
Color differences between atrophic and non-atrophic mucosa and between fundic and pyloric mucosa
| Helicobacter pylori infection | |||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Currently or previously infected (n = 31) |
Currently infected (n = 13) |
Previously infected (n = 18) |
Never infected (n = 21) |
||||||||||||
| WLI | LCI | p value | WLI | LCI | p value | WLI | LCI | p value | WLI | LCI | p value | ||||
| Border between atrophic and non-atrophic mucosa | |||||||||||||||
| Color difference (n = 31) |
16.08 ± 7.82 | 25.03 ± 9.72 | <0.001 | 14.42 ± 5.95 | 21.58 ± 6.97 | 0.004 | 17.1 ± 8.48 | 27.34 ± 10.32 | <0.001 | — | — | — | |||
| Border between fundic and pyloric mucosa | |||||||||||||||
| Color difference (n = 21) |
— | — | — | — | — | — | — | — | — | 14.04 ± 4.24 | 28.71 ± 5.92 | <0.001 | |||
LCI, linked color imaging; WLI, white light imaging.
In never-infected patients, the color difference at the endoscopic border between fundic and pyloric mucosa on LCI (28.71 ± 5.92) was significantly larger than that on WLI (14.04 ± 4.24; p<0.001) (Table 4).
Discussion
We demonstrated that the color differences at the atrophic border in transnasal endoscopy images using LCI in the L*a*b* color space were significantly larger than those on WLI images in patients with current or past infection of H. pylori. In addition, the color differences at the border between fundic and pyloric mucosa on LCI images in patients with no history of H. pylori infection were significantly larger than those on WLI images. Although there were no significant differences between WLI and LCI in gastritis severity as scored using the Kyoto classification, when we evaluated the ease of subjective endoscopic judgement, LCI was superior to WLI in evaluating atrophy. Recently, the superior efficacy of LCI over WLI was reported in the detection of atrophic borders and intestinal metaplasia using oral endoscopy; we show here that LCI also has this advantage in transnasal endoscopy.
Endoscopic detection of gastric cancer risk on LCI images
While conventional endoscopy systems use white light from a xenon light source, the LASEREO system (Fujifilm) is a new-generation endoscopy system that uses two types of blue laser light (410 nm and 450 nm), which allows visualization of the microvessels and gastric mucosal surface structure at high contrast. It also uses LCI, which emphasizes the colors of the gastrointestinal mucosa by image processing. LCI uses a white-light laser to maintain brightness, strongly reflects the influence of 410 nm short-wave narrow-band light, and rearranges the color information to detect slight color differences near the mucosal border. Thereby, LCI improves the visibility of lesions that can cause color changes such as diffuse redness, map-like redness, and/or ridge-like redness, or whitish-colored findings such as MALT lymphoma and undifferentiated gastric cancer.(14) Consequently, LCI is expected to improve the diagnostic efficiency of endoscopy for such conditions.(26,27) To efficiently perform gastric cancer screening using an endoscope, the status of infection must be accurately diagnosed by endoscopy in combination with a diagnostic test for H. pylori infection. Finally, risk factors for gastric cancer (e.g., atrophy, intestinal metaplasia, map-like redness, and xanthoma) should be detected and diagnosed in an efficient manner.
Several studies have been conducted to compare the diagnostic capability of LCI, WLI, and other IEEs in detecting gastric cancer risk factors. Gastric mucosa of currently infected H. pylori is characterized by atrophy and intestinal metaplasia, diffuse redness, mucosal enlargement, mucosal fold enlargement, and loss of RAC. However, in clinical practice, some cases are difficult to diagnose using WLI alone, such as cases with severe atrophy, cases of autoimmune gastritis, or cases that arise after H. pylori eradication.(19,28) Ono et al.(28) examined the diagnostic capability of WLI and LCI for currently infected cases of H. pylori in 127 patients and reported that the accuracy of LCI was 86.6% (sensitivity, 84.4%; specificity, 88.9%). This was significantly higher than that of WLI (79.5%: sensitivity, 84.4%; specificity, 74.6%). Diagnosis of past infection was also significantly more accurate with LCI than with WLI (78.9% vs 36.8%, respectively). This improvement was ascribed to the improved detection by LCI of diffuse redness and atrophy, which indicate the infection status of H. pylori.
A diagnosis of endoscopic atrophy is based on the disappearance and discoloration of mucosal folds and increased vascular translucency. However, in many cases, it is difficult to evaluate the atrophic border, especially when the gastric mucosa is partially regenerated and the atrophy has improved after eradication treatment.(29) Takeda et al.(12) reported that LCI produced superior visibility of the atrophy boundary to that visualized by WLI alone in 42.1% of cases. Mizukami et al.(18) also objectively evaluated the color difference of the atrophy boundary in the CIE 1976 L*a*b* color space, and reported that it was 14.79 ± 6.68 for LCI and 11.06 ± 5.44 for WLI; this difference was significant. The color difference was also significantly different between people with a current infection and those who had been previously infected. Atrophy findings differ between endoscopic and histological methods and the degree of improvement in atrophy after eradication also differs when assessed using endoscopic and histological approaches.(29) Especially after eradication, atrophy is improved, and atrophied and non-atrophied mucosa coexist, which often makes endoscopic diagnosis difficult. This divergence may disappear when endoscopy is combined with LCI. To accurately stratify the risk of gastric cancer by assessing atrophy, it is necessary to use LCI as appropriate, and to include histological assessment as recommended in the guideline on the management of epithelial precancerous conditions and lesions in the stomach (MAPS II).(31)
Intestinal metaplasia, like atrophy, is a high-risk lesion for gastric cancer that needs to be diagnosed carefully.(10) The endoscopic characteristic of intestinal metaplasia when assessed using WLI is that it looks whiter than the non-metaplastic mucosa, and the diagnostic sensitivity and specificity of WLI are, respectively, 86% and 66% in the lesser curvature of the corpus, and 95% and 69% in the lesser curvature of the vestibular region.(32) In the Kyoto classification of gastritis, intestinal metaplasia that could not normally be visualized with white light can be visualized by IEE, so IEE is recommended when evaluating intestinal metaplasia. In fact, reported characteristic endoscopic findings of intestinal metaplasia using NBI are a white opaque substance and a light blue crest, whereas using LCI, intestinal metaplasia is observed as a lavender region, which is easier to recognize than white.(33) In addition, Ono et al.(16) conducted a prospective study to histopathologically evaluate lesions identified as intestinal metaplasia using WLI and lavender regions identified using LCI, and the diagnostic accuracy against the target biopsy was 23.7% by WLI (range, 22.8–27.2%; sensitivity, 21.2%; specificity, 99.2%) and 84.2% by LCI (range, 79.0–86.9%; sensitivity, 66.7%; specificity, 96.2%). Thus, LCI demonstrated significantly better diagnostic capability. Furthermore, in a previous evaluation using the CIE 1976 L*a*b* color space, the diagnostic accuracy of LCI for intestinal metaplasia was significantly higher than that of WLI (21.1 ± 6.6 vs 9.7 ± 6.6).(34)
Despite these promising reports, there have been no reports of objective evaluations based on CIE 1976 L*a*b* color space used in transnasal endoscopy. Therefore, we examined the risk of gastric cancer according to the Kyoto classification of gastritis based on LCI observation with transnasal endoscopy. Like for oral endoscopy, the visibility of atrophy and intestinal metaplasia was improved when using LCI with transnasal endoscopy. The color difference at the atrophic border in patients with current or past infection was significantly greater with LCI than with WLI (Table 4). In particular, the difference in the red–green element (a*) of the L*a*b* color space was significantly greater with LCI, possibly due to the decrease in redness of the non-atrophic part.
Transnasal endoscopy for health check-ups
Regular endoscopic examinations increase survival rates of gastric cancer, and the importance of endoscopic evaluation has been re-confirmed all over the world.(35) The American Gastroenterological Association recommends that patients with advanced atrophic gastritis should be monitored by endoscopy every 3 years.(36) The recommendation in MAPS II is for a tailor-made approach (rather than routine surveillance) based on risk factors such as atrophy of the antrum and corpus, localization and progression of intestinal metaplasia, family history, and complications of autoimmune gastritis.(31) The Japan Gastroenterological Endoscopy Society’s guideline for the endoscopic diagnosis of early gastric cancer recommends that patients with risk factors for developing gastric cancer should undergo regular endoscopy for the long term, although a specific interval for such examinations is not specified.(37) However, in a Japanese cohort study, >95% of cases with gastric cancer detected by annual endoscopy surveillance were cured by endoscopic resection.(38) Accordingly, we consider yearly surveillance after eradication to be appropriate.
In Japan, endoscopic examination is often via the transnasal route to reduce invasiveness and distress to the patient. However, with the development of new endoscopic technologies such as IEE, it was not clear whether transnasal endoscopy used with IEE could be expected to have the same high diagnostic capability as oral endoscopy used with IEE. Adding IEE to routine endoscopy increases the workload for clinicians performing the health checks, so it is important to evaluate its usefulness. We have shown here that the color difference at the atrophic border is greater with LCI than with WLI even in transnasal endoscopy, and the subjective diagnostic capability was also excellent. In the future, as the number of people with past infection grows due to the increased use of eradication therapy, the importance of surveillance endoscopy for gastric cancer by transnasal endoscopy will likely increase. Accordingly, we consider it appropriate to use LCI with transnasal endoscopy for regular health checks.
Limitations
This study has a few limitations. First, it was a single-center retrospective study. Second, we examined only transnasal endoscopy images, so we did not directly compare oral and transnasal endoscopy in the efficacy of assessment of gastritis severity. Third, because of the small sample size, we were unable to determine conclusively whether efficacy of transnasal endoscopy using LCI in determining the severity of gastritis differed between patients with different H. pylori infection statuses.
Conclusion
The diagnostic capability of endoscopy has progressed substantially due to recent advances in endoscopic technology, and it is important to identify the most appropriate diagnostic method for gastric cancer treatment. In this study, we showed that transnasal endoscopy with LCI using the CIE 1976 (L*a*b*) color space is useful and effective for diagnosing H. pylori infection, gastric mucosal atrophy, and intestinal metaplasia. In cases where evaluation was difficult with WLI observation, IEE observation was used. The greater differences in color tone increased the diagnostic efficiency, which helped improve risk stratification for gastric cancer. A larger, multi-center prospective study is warranted to confirm these results and to understand the factors that affect them. Nevertheless, we recommend the use of LCI observation for endoscopic surveillance even in the health check-up environment.
Author Contributions
Study concept and design: YK, MS, and TK; methodology: YK, MS, and TK; software: YK, TK, and MS; investigation: YK and TK; formal analysis: YK, TK, and MS; drafting of the manuscript: YK, MS, and TK; critical revision of the manuscript: YK, MS, MH, NN, EI, RN, MF, TI, and TK; supervision: TI and TK; project administration: TK.
Acknowledgments
No specific funding was received for the present study.
Abbreviations
- CIE
International Commission on Illumination
- IEE
image enhancement endoscopy
- LCI
linked color imaging
- RAC
regular arrangement of collecting venules
- WLI
white-light imaging
Conflict of Interest
No potential conflicts of interest were disclosed.
References
- 1.Infection with Helicobacter pylori. IARC Monogr Eval Carcinog Risks Hum 1994; 61: 177–240. [PMC free article] [PubMed] [Google Scholar]
- 2.Matsuo T, Ito M, Takata S, Tanaka S, Yoshihara M, Chayama K. Low prevalence of Helicobacter pylori-negative gastric cancer among Japanese. Helicobacter 2011; 16: 415–419. [DOI] [PubMed] [Google Scholar]
- 3.Uemura N, Okamoto S, Yamamoto S, et al. Helicobacter pylori infection and the development of gastric cancer. N Engl J Med 2001; 345: 784–789. [DOI] [PubMed] [Google Scholar]
- 4.Fukase K, Kato M, Kikuchi S, et al. Effect of eradication of Helicobacter pylori on incidence of metachronous gastric carcinoma after endoscopic resection of early gastric cancer: an open-label, randomised controlled trial. Lancet 2008; 372: 392–397. [DOI] [PubMed] [Google Scholar]
- 5.Sugimoto M, Murata M, Yamaoka Y. Chemoprevention of gastric cancer development after Helicobacter pylori eradication therapy in an East Asian population: meta-analysis. World J Gastroenterol 2020; 26: 1820–1840. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Sugano K. Effect of Helicobacter pylori eradication on the incidence of gastric cancer: a systematic review and meta-analysis. Gastric Cancer 2019; 22: 435–445. [DOI] [PubMed] [Google Scholar]
- 7.Stomach cancer statistics. World Cancer Research Fund and American Institute for Cancer Research. https://www.wcrf.org/dietandcancer/stomach-cancer-statistics/. Accessed 9 Oct 2021.
- 8.Kato M, Ota H, Okuda M, et al. Guidelines for the management of Helicobacter pylori infection in Japan: 2016 Revised Edition. Helicobacter 2019; 24: e12597. [DOI] [PubMed] [Google Scholar]
- 9.Kamada T, Haruma K, Inoue K, Shiotani A. Helicobacter pylori infection and endoscopic gastritis—Kyoto classification of gastritis. Nihon Shokakibyo Gakkai Zasshi 2015; 112: 982–993. [DOI] [PubMed] [Google Scholar]
- 10.Sugimoto M, Ban H, Ichikawa H, et al. Efficacy of the Kyoto classification of gastritis in identifying patients at high risk for gastric cancer. Intern Med 2017; 56: 579–586. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Yoshii S, Mabe K, Watano K, et al. Validity of endoscopic features for the diagnosis of Helicobacter pylori infection status based on the Kyoto classification of gastritis. Dig Endosc 2020; 32: 74–83. [DOI] [PubMed] [Google Scholar]
- 12.Takeda T, Asaoka D, Nojiri S, et al. Linked color imaging and the Kyoto classification of gastritis: evaluation of visibility and inter-rater reliability. Digestion 2020; 101: 598–607. [DOI] [PubMed] [Google Scholar]
- 13.Nishizawa T, Toyoshima O, Kondo R, et al. The simplified Kyoto classification score is consistent with the ABC method of classification as a grading system for endoscopic gastritis. J Clin Biochem Nutr 2021; 68: 101–104. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 14.Dohi O, Yagi N, Naito Y, et al. Blue laser imaging-bright improves the real-time detection rate of early gastric cancer: a randomized controlled study. Gastrointest Endosc 2019; 89: 47–57. [DOI] [PubMed] [Google Scholar]
- 15.Majima A, Dohi O, Takayama S, et al. Linked color imaging identifies important risk factors associated with gastric cancer after successful eradication of Helicobacter pylori. Gastrointest Endosc 2019; 90: 763–769. [DOI] [PubMed] [Google Scholar]
- 16.Ono S, Kato M, Tsuda M, et al. Lavender color in linked color imaging enables noninvasive detection of gastric intestinal metaplasia. Digestion 2018; 98: 222–230. [DOI] [PubMed] [Google Scholar]
- 17.Ono S, Kawada K, Dohi O, et al. Linked color imaging focused on neoplasm detection in the upper gastrointestinal tract: a randomized trial. Ann Intern Med 2021; 174: 18–24. [DOI] [PubMed] [Google Scholar]
- 18.Mizukami K, Ogawa R, Okamoto K, et al. Objective endoscopic analysis with linked color imaging regarding gastric mucosal atrophy: a pilot study. Gastroenterol Res Pract 2017; 2017: 5054237. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 19.Dohi O, Yagi N, Onozawa Y, et al. Linked color imaging improves endoscopic diagnosis of active Helicobacter pylori infection. Endosc Int Open 2016; 4: E800–E805. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Kimura K, Takemoto T. An endoscopic recognition of the atrophic border and its significance in chronic gastritis. Endoscopy 1969; 1: 87–97. [Google Scholar]
- 21.Dixon MF, Genta RM, Yardley JH, Correa P. Classification and grading of gastritis. The updated Sydney System. International Workshop on the Histopathology of Gastritis, Houston 1994. Am J Surg Pathol 1996; 20: 1161–1181. [DOI] [PubMed] [Google Scholar]
- 22.Rugge M, Correa P, Di Mario F, et al. OLGA staging for gastritis: a tutorial. Dig Liver Dis 2008; 40: 650–658. [DOI] [PubMed] [Google Scholar]
- 23.Rugge M, Meggio A, Pennelli G, et al. Gastritis staging in clinical practice: the OLGA staging system. Gut 2007; 56: 631–636. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 24.Kuehni RG. Color-tolerance data and the tentative CIE 1976 L*a*b* formula. J Opt Soc Am 1976; 66: 497–500. [DOI] [PubMed] [Google Scholar]
- 25.Sato Y, Sagawa T, Hirakawa M, et al. Clinical utility of capsule endoscopy with flexible spectral imaging color enhancement for diagnosis of small bowel lesions. Endosc Int Open 2014; 2: E80–E87. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26.Fukuda H, Miura Y, Hayashi Y, et al. Linked color imaging technology facilitates early detection of flat gastric cancers. Clin J Gastroenterol 2015; 8: 385–389. [DOI] [PubMed] [Google Scholar]
- 27.Osawa H, Miura Y, Takezawa T, et al. Linked color imaging and blue laser imaging for upper gastrointestinal screening. Clin Endosc 2018; 51: 513–526. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 28.Ono S, Dohi O, Yagi N, et al. Accuracies of endoscopic diagnosis of Helicobacter pylori-gastritis: multicenter prospective study using white light imaging and linked color imaging. Digestion 2020; 101: 624–630. [DOI] [PubMed] [Google Scholar]
- 29.Kodama M, Okimoto T, Mizukami K, et al. Gastric mucosal changes, and sex differences therein, after Helicobacter pylori eradication: a long-term prospective follow-up study. J Gastroenterol Hepatol 2021; 36: 2210–2216. [DOI] [PubMed] [Google Scholar]
- 30.Kono S, Gotoda T, Yoshida S, et al. Can endoscopic atrophy predict histological atrophy? Historical study in United Kingdom and Japan. World J Gastroenterol 2015; 21: 13113–13123. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 31.Pimentel-Nunes P, Libânio D, Marcos-Pinto R, et al. Management of epithelial precancerous conditions and lesions in the stomach (MAPS II): European Society of Gastrointestinal Endoscopy (ESGE), European Helicobacter and Microbiota Study Group (EHMSG), European Society of Pathology (ESP), and Sociedade Portuguesa de Endoscopia Digestiva (SPED) guideline update 2019. Endoscopy 2019; 51: 365–388. [DOI] [PubMed] [Google Scholar]
- 32.Fukuta N, Ida K, Kato T, et al. Endoscopic diagnosis of gastric intestinal metaplasia: a prospective multicenter study. Dig Endosc 2013; 25: 526–534. [DOI] [PubMed] [Google Scholar]
- 33.Ono S, Kato M, Nakagawa S, Mabe K, Sakamoto N. Vonoprazan improves the efficacy of Helicobacter pylori eradication therapy with a regimen consisting of clarithromycin and metronidazole in patients allergic to penicillin. Helicobacter 2017; 22: 10. [DOI] [PubMed] [Google Scholar]
- 34.Ono S, Shimoda Y, Tanaka I, et al. Optical effect of spraying l-menthol on gastric intestinal metaplasia visualized by linked color imaging. Eur J Gastroenterol Hepatol 2021; 33: 358–363. [DOI] [PubMed] [Google Scholar]
- 35.Jun JK, Choi KS, Lee HY, et al. Effectiveness of the Korean National Cancer Screening Program in Reducing Gastric Cancer Mortality. Gastroenterology 2017; 152: 1319–1328.e7. [DOI] [PubMed] [Google Scholar]
- 36.Shah SC, Piazuelo MB, Kuipers EJ, Li D. AGA clinical practice update on the diagnosis and management of atrophic gastritis: expert review. Gastroenterology 2021; 161: 1325–1332.e7. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Yao X, Ghert M, Dickson BC, et al. An evidence-based guideline on the application of molecular testing in the diagnosis, prediction of prognosis, and selection of therapy in non-GIST soft tissue sarcomas. Cancer Treat Rev 2020; 85: 101987. [DOI] [PubMed] [Google Scholar]
- 38.Nakajima T, Oda I, Gotoda T, et al. Metachronous gastric cancers after endoscopic resection: how effective is annual endoscopic surveillance? Gastric Cancer 2006; 9: 93–98. [DOI] [PubMed] [Google Scholar]