Abstract
Background:
Integrated community case management (ICCM) service is provision of concurrent clinical and preventive care by trained community health workers for common childhood illnesses in the community. In Ethiopia, integrated community case management (ICCM) service utilization is low and its magnitude is unknown as well as no adequate evidence on its associated factors. This study aimed to investigate use of integrated community case management service of childhood illness and factors associated with it.
Methods:
A community-based cross-sectional study was conducted in Shashogo district. A total of 422 mothers who have under-five children were selected using simple random sampling method. Structured interviewer administered pre-tested in 5% of the sample; questionnaire was used to collect data. Descriptive statistics, binary and multivariable logistic regression analyses were used.
Results:
The proportion of integrated community case management (ICCM) service utilization among sick under-five children in past six months at Shashogo district was found was 199(47.2%, with 95%CI:(43.2, 51.2)). Receiving training on health extension packages as model family AOR = 2.07(1.05, 4.08), experiencing frequent childhood illness AOR = 1.92(1.11, 3.33), having information about ICCM service AOR = 3.73(1.42, 9.76), and having a postnatal care visit in recent child AOR = 13(7.37, 23.06) were associated with utilization of integrated community case management service.
Conclusion:
ICCM service was not used as planned though there is offer of free of charge service nearby. ICCM service is affected by maternal and child health utilization. Hence, collaborative activities of information, education, and communication activities are needed.
Keywords: Integrated community, case management, under-five children, Shashogo district
Introduction
Integrated community case management (ICCM) is a strategy to train, support, and supply community health workers (CHW) to provide diagnostics and treatment for multiple illnesses specifically pneumonia, diarrhea, and malaria for sick children of families with difficult access to case management at health facilities. ICCM relies on evidence-based and one of the most cost-effective child survival interventions—proven to save the lives of newborns and children under five, at a price that is affordable in developing countries.1–3
ICCM program targets the main causes of child morbidity and mortality, namely pneumonia, diarrheal, malaria, and malnutrition.1–4 Decentralizing preventive, promotive and basic curative child health and nutrition services through the policy of the health extension program has significantly contributed to the reduction of under-five mortality. 5
Globally, 5.6 million under-five children died in 2016, and sub-Saharan Africa remains the region with the highest under-five mortality rate in the world. In 2016, sub-Saharan Africa has an average under-five mortality rate of 79 deaths per 1,000 live births.6–10 The patterns of child morbidity and mortality varied slightly by region.11,12
Despite the increased implementation of ICCM program focus and intention increases with time, utilization remains low 12 and its factors are not well known for children less than five years in Ethiopia; the main barriers to care-seeking at health posts were socio-cultural, religious, lack of information on availability of ICCM service at health post, low health care-seeking behavior among families.12,13 Under-five children morbidity was stable after ICCM introduction in 2014. Currently, ICCM service is being given nationally but magnitude of ICCM service utilization at Oromia region of Agerfa district was found to be 10.5%. 13 This shows that utilization of ICCM service for the common killer childhood illness using effective interventions is fairly low.
Most previous studies focused on ICCM program implementation strength and quality of service provision on provider side and implementation systems of ICCM. Previous studies collected data from registration book of health post and counting cases reported without considering the denominator and studies were also descriptive only.13–16 Hence, this study assessed the magnitude of ICCM service utilization and associated factors by considering predisposing, enabling and need factors by adapting Andersen and Ronald Framework of healthcare utilization. 17
Methods and materials
The study was conducted from March 15/2018 to April 30/2018 in Shashogo district of Hadiya zone, SNNPR, whose capital is Bonosha which is located at a distance of 52 km away from the zonal capital of Hossana town and 117 km away from Hawassa capital of SNNPR, 224 km from Addis Ababa, capital of Ethiopia.
A community-based cross-sectional study design was triangulated with qualitative method was employed. Qualitative study was conducted parallel to the quantitative study to validate and credible the findings. The study population was mothers who have under-five children and history of illness within six months residing in the selected kebeles for quantitative study. Health extension supporters from woreda health office, leaders (community, clans, and kebele), and male parents were selected for the qualitative study. All mothers who have children whose age less than five years and have history of illness within six months before actual data collection from rural kebeles were included. Mothers who were permanent residents of the study area and who lived for more than six months during actual data collection time were included for qualitative study, but critically sick under-five children during actual data collection were excluded from study and advised parents to take health institutions.
Sample size and sampling techniques of quantitative study
Sample size was determined by using single population proportion formula for magnitude of ICCM utilization by considering the following assumptions, 95% confidence level = 1.96, Margin of error (d) 5% = 0.05, proportion of mothers who have under-five children who utilize ICCM service in Bale zone Agerfa woreda(P) = (10.5%). 13
where n = required sample size since using
For factors associated with ICCM, sample size calculated using predictor variables of integrated community case management service utilization from previous different studies using EPI-INFO version 7.1.1 by considering AOR, 95%CI and power (80%) for association with dependent variable (See Table 1).
Table 1.
Sample size determination for second objective using predictor variables of ICCM service utilization from previous studies.
| S. No. | Variables associated with ICCM service utilization | Reference | Expected frequency % | AOR | Sample size | 10% nonresponse added sample size |
|---|---|---|---|---|---|---|
| 1 | Educational status of secondary education | Gorfu 13 | 81 | 3.1 | 237 | 261 |
| 2 | Marital status other than married | Gorfu 13 | 25 | 4.28 | 288 | 317 |
| 3 | Information source of ICCM service:HEWs | Gorfu 13 | 50.1 | 0.19 | 384 | 422 |
| 4 | Awareness of child health service availability at HP | Yansaneh et al. 18 | 48.6 | 2.52 | 341 | 376 |
| 5 | Previously use of ICCM service | Yansaneh et al. 18 | 31.1 | 6.57 | 329 | 362 |
Then, calculated sample size for magnitude of ICCM utilization was 145 and 384 for factors associated with ICCM, which is the largest sample size of predictor variable (ICCM service information from HEWs). Therefore, the larger one, that is, sample size for factors associated with ICCM was taken.
Finally, adding nonresponse rate of 10% on accepted larger sample size and final sample size could be 422.
The woreda has 36 kebeles in the Shashogo district of which 2 are urban kebeles. From total of 34 kebeles, 11 (30%) kebeles were selected by computer generating methods on SPSS and Census was conducted to identify eligible children. To choose the final sample, each kebele’s population to size allocation procedures were used. Eligible mothers who have children for the study were marked using chalk with respective kebeles, village, and house number (consecutive numbers given each households) by health extension workers. The identified eligible sick children also recorded. Then, from the identified eligible sick children list, children who included in the study were chosen by lottery method from each kebele
Sample size determination and sampling procedure for qualitative study
The purposive sampling technique was used. Health extension Program supporters, male parents, and leaders (religious, clan, and kebele) were selected purposively for focus group discussion, and six FGD sessions were conducted with a total of forty-two FG Discussants.
Variables
Dependent variable
Utilization of ICCM service
Independent variables
Predisposing factors
Age
Sex
Cultural beliefs and practices
Family size
Head of household
Child age
Child sex
Birth order
Education
Marital status
Occupation
Religion
Experienced time of child illness
Number of under-five children
Need factors
Knowledge and attitude toward ICCM service
Attitude toward HEWs
Information for ICCM service
Source of information
Perceived susceptibility and severity of childhood illness
Enabling factors
ANC visit in recent child
PNC visit in recent child
Received health extension package training
Health extension workers presence
Distance to health post
Distance to nearest health facility other than health post
Means of transportation
Data collection techniques and measuring instrument of quantitative study
The final version of the English questionnaire was developed after reviewing of different relevant literature.13,19,20 Then, the questionnaire was translated into local language.
A face-to-face interview of mothers/caregivers of children was interviewed using structured, semistructured pre-tested questionnaire.
Open-ended non-directive focus group discussion (FGD) guide was designed. Accordingly, six FGDs were conducted in a group such as two FDGs with program supporters, two FDGs with husbands, and the last two with leaders. The point of saturation of idea reached was used to stop. We declared point of saturation when repeated ideas were raised and assumed that no additional data could be obtained.
The data collection process and supervision
Five data collectors who have diploma nurse qualification and could speak Hadiyisa were selected. For supervision, two degree nurses from the health center hired. To assure quality, two days of training was given for data collectors and supervisors. Pretest was conducted in 5% of the sample. For the qualitative study, the principal investigator and three male staffs of woreda health office with BSC holders moderate the discussion of the each group. Group discussions with their respective members were conducted in a quiet hall in District health office. Every conversation was recorded. Finally, the principal investigator transcribed the recorded and taken notes so as not to miss any of the discussed issues. Data were tape recorded and notes collected from each part, which was then translated and interpreted.
Every day questionnaires were reviewed and checked for completeness. Participants were not compensated for their time. The duration of discussion is according to guideline.
Statistical analysis
The data on each coded questionnaire were entered into Epi data version 3.1. Then, data were exported to SPSS version 20.0 for analysis. Bivariate and multivariable logistic regression models were used to measure the strength of association. Candidate variable selection with P-value less than 0.25 used in bivariate analysis. Adjusted odds ratio with 95% confidence interval was considered to declare statistically significant variables. Multico-linearity was tested. Goodness-of-fit with Hosmer and Lemeshow test has p-value = 0.70. After the interview, Hadiyisa audio recorded qualitative data were translated word by word into the English language and then transcribed into an English language in text form. Finally, results of the qualitative study were triangulated with the quantitative results.
Ethical clearance
Prior to data collection, ethical clearance was obtained from the ethical review board of the Jimma University Institute of Health. An official letter was written from the Institute of health science of Jimma University to administrative body of Hadiya zone. A formal letter of permission was received from administrative bodies of the Hadiya zone to Shashogo district Health office. Finally, verbal consent was requested from every participant during data collection time for both quantitative and qualitative data collection methods. Confidentiality was assured for the information provided.
Result
Among 422 mothers planned to be interviewed, 415 caregivers interviewed with response rate of 98.3%
This research findings revealed that 188 (44.8%) respondents were age group between 25 and 34 years with mean age of 34.1 (SD ± 7.66). Regarding under-five children’s age, 129 (30.6%) children were at age group between 24 and 35 months with mean age of 26 months (SD ± 14). About 396 (93.8%) were married caregivers. Hadiya were dominant ethnic group accounting for 353 (83.6%) of the respondents, and majority of respondents were protestant religion followers accounting for 216 (51.2%). Two hundred eighty-nine (68.1%) had completed secondary level of education (See Table 2).
Table 2.
Socio-demographic characteristics of mothers/caregivers and children age less than five years Shashogo district, 2018 (n = 422).
| Variables | Frequency | % |
|---|---|---|
| Sex of caregiver | ||
| male | 134 | 31.7 |
| Female | 280 | 66.4 |
| Sex of child | ||
| Male | 189 | 44.7 |
| Female | 225 | 53.3 |
| Age of respondent | ||
| 18–24 | 29 | 6.8 |
| 25–34 | 188 | 44.8 |
| 35–44 | 161 | 38.2 |
| 45–55 | 34 | 8 |
| Age of children | ||
| < 2mo | 2 | 1.1 |
| 2–11mo | 69 | 16.4 |
| 12–23 | 95 | 22.5 |
| 24–35 | 129 | 30.6 |
| 36–47 | 66 | 15.6 |
| 48–59 | 56 | 13.2 |
| Marital status | ||
| Single | 10 | 2.3 |
| Married | 396 | 93.8 |
| Widowed | 9 | 2.1 |
| Educational level | ||
| No Formal education | 70 | 16.5 |
| 1–8 | 289 | 68.4 |
| 9–12 | 52 | 12.3 |
| Collage or above | 4 | 0.9 |
| Occupational status | ||
| Housewife | 227 | 53.8 |
| Private business | 37 | 8.8 |
| Farmer | 130 | 30.8 |
| Ethnicity | ||
| Hadiyya | 353 | 83.6 |
| Kambata | 41 | 9.7 |
| Family size | ||
| < 6 | 255 | 60.4 |
| >= 6 | 160 | 37.9 |
| Religion of caregiver | ||
| Protestant | 216 | 51.2 |
| Muslim | 197 | 46.7 |
| Head of HH | ||
| Male | 396 | 93.8 |
| Number of < 5 child | ||
| 1 child | 201 | 47.6 |
| >= 2 child | 214 | 50.7 |
| Birth order of child | ||
| 1 | 34 | 8.1 |
| 2 | 62 | 14.6 |
| 3 | 85 | 20.1 |
| >= 4 | 234 | 55.5 |
Need factors
Two hundred twenty-nine (54.3%) of the respondents had good knowledge toward ICCM services. Most of the study participants, 412 (97.6%) had a positive attitude toward health extension workers. Three hundred thirty-eight (80.1%) of the respondents had information to ICCM services (See Table 3).
Table 3.
Need factors of integrated community case management service utilization, 2018.
| Variable | Categories | Frequency | Percent |
|---|---|---|---|
| Knowledge toward ICCM | Good knowledge | 229 | 54.3 |
| Poor knowledge | 186 | 44 | |
| Attitude toward ICCM services | Positive attitude | 403 | 95.5 |
| Negative attitude | 12 | 2.8 | |
| Attitude toward HEWs | Positive attitude | 412 | 97.6 |
| Negative attitude | 3 | 0.7 | |
| Information for ICCM | Yes | 338 | 80.1 |
| No | 77 | 18.2 | |
| Source of ICCM information | HEWS | 181 | 52.0 |
| VCHWS | 150 | 35.5 | |
| Radio | 8 | 1.8 | |
| Perceived susceptibility of childhood illness | low perception | 49 | 11.6 |
| high perception | 368 | 87.2 | |
| Perceived severity of child hood illness | low perception | 23 | 5.5 |
| high perception | 392 | 92.8 |
This finding was also supported by qualitative result: “. . . I came Health post more than one times and learnt about childhood illness and management service. . .”
(35-year-old women league of kebele)
Enabling factors
A significant number of 374 ( 88.6%) interviewed caregivers went to child health care other than health post with a distance of greater than an hour. Two hundred fifty-five (60.4%) of respondents were not getting health extension workers at the time of visiting health post. It was 299 (70.9%) caregivers who have trained on health extension packages as a model family (See Table 4).
Table 4.
Enabling factors of integrated community case management service utilization, 2018.
| Variables | Category | Frequency | Percentage |
|---|---|---|---|
| Distance to child care other than HP by minute | >= 60 minute | 374 | 88.6 |
| < 60 minute | 48 | 11.4 | |
| HEWS presence at the time of visiting | No | 255 | 60.4 |
| Yes | 167 | 39.6 | |
| Distance from HP to their Home by minute | < 15 | 5 | 1.2 |
| >= 15 | 417 | 98.8 | |
| Received health extension package training as model family | No | 123 | 29.1 |
| Yes | 299 | 70.9 | |
| Means of transportation | Foot | 317 | 75.3 |
| Motor | 96 | 22.8 | |
| Car | 6 | 1.4 |
Integrated community case management service utilization
Of the total respondents, only, 199 (47.2%, with 95% CI: (43.2,51.2)) utilized ICCM service among sick under-five children caregivers in the past six months at Shashogo district.
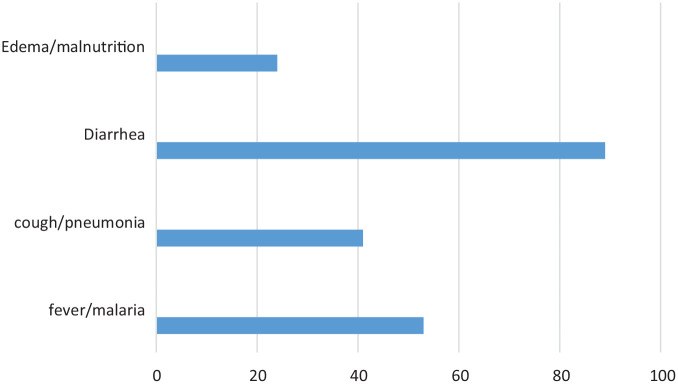
Among ICCM service users, majority 89(43.0%) of the caregivers reported diarrhea as most common childhood illness followed by fever/malaria 53(25.6%) (See Figure 1).
Figure 1.
Type of ICCM service children received from health post, Shashogo woreda, Hadiya zone, south Ethiopia, 2018.
Different reasons were given by the caregivers for not utilizing ICCM services within six months; lack of supply 272(81.9%) and closed health post 208 (62.7%) at visiting time were main ones.
In qualitative data analysis, three themes were generated as facilitator to use and barrier not to use ICCM service provided free of charge nearby the community.
Theme 1: Availability and accessibility of service
Theme 2: Information and knowledge
Theme 2: Providers’ skill
FGD discussants responded that; “. . . I used the service provided by health post repeatedly and better child health service was given here in health post, but many parents took their child to traditional healers for tonsillitis (pneumonia) and tooth extraction. . .” (42-year-old male, program supporter)
FGD participants mentioned that the most common reasons for not utilizing the service in the area: “two months before, I came to health post with my sick child for diarrheal disease but no improvement. Then, I went to local traditional healers and cured. . .” (30-year-old male parent)
Another discussant said that “. . .Our home is far from health post, road is inaccessible and thus difficult for us to come back carrying child. . .” (49-year-old religious leader)
Factors associated with ICCM service utilization
Fourteen independent variables were identified during bivariate binary logistic regression analyses which have p-value less than 0.25 and fourteen of them were checked for association but only four variables showed association with outcome variable.
Factors independently associated with ICCM service utilization
The result of this study showed that disease experience of two and above times was 1.92 times more likely to utilize ICCM service than those of counterpart ((AOR = 1.92 (1.11, 3.33). Concerning mothers, those having PNC visits in the recent child were 13 times more likely to utilize ICCM service than mothers who did not having PNC visit in recent child (AOR = 13(7.37, 23.06)). Caregivers that heard information for ICCM service were 3.73 times more likely to practice ICCM service when compared to caregivers did not hear (AOR = 3.73(1.42, 9.76). Care providers who received health extension package training were two times more likely than their counterparts to use ICCM services. (AOR = 2.07(1.05, 4.08)) (See Table 5).
Table 5.
Independent predictors of ICCM service utilization and associated factors among under-five children in Shashogo district, Hadiya zone south Ethiopia, 2018 (n = 422).
| Variables | Label of category | ICCM service utilization | COR (95%CI) | AOR (95% CI) | |
|---|---|---|---|---|---|
| Yes N (%) | No N (%) | ||||
| Birth order of child | First | 23 (67.6) | 11 (32.4) | 3.46 (1.60, 7.44) | 2.76 (0.92,8.33) |
| Second | 48 (75) | 16 (25) | 4.96 (2.65,9.27) | 1.09 (0.39,3.05) | |
| Third | 41 (53.9) | 35 (46.1) | 1.93 ( 1.14,3.27) | 1 (0.39,2.53) | |
| ⩾ Forth | 87 (37.7) | 144 (62.3) | 1 | 1 | |
| Disease experienced | 1 times | 98 (41.5) | 138 (58.5) | 1 | 1 |
| ⩾ 2 times | 101 (59.8) | 68 (40.2) | 2.09 (1.39,3.12) | 1.92 (1.11,3.33)* | |
| Having PNC visit in recent child | Yes | 163 (82.3) | 35 (17.7) | 22.12 (13.25, 36.92) | 13 (7.37,23.06)* |
| No | 36 (17.4) | 171 (82.6) | 1 | 1 | |
| Health extension package training | Yes | 179 (61.5) | 112 (38.5%) | 0.13 (0.07, 0.22) | 2.07 (1.05,4.08)* |
| No | 20 (17.5%) | 94 (82.5%) | 1 | 1 | |
| Heard information of ICCM service | Yes | 193 (59.6) | 131 (40.1) | 0.05 (0.02,0.12) | 3.73 (1.42,9.76)* |
| No | 6 (7.4) | 75 (92.6) | 1 | 1 | |
significant association.
Discussion
This community-based cross-sectional study was supplemented by qualitative method has used to determine prevalence and factors associated with ICCM service utilization among caregivers who had history of sick under-five children within six months. As the result, having PNC visit in recent child, heard information for ICCM service, experienced frequent times of childhood illness and received health extension package training were associated with ICCM service utilization in Shashogo district.
The magnitude of ICCM service utilization was 199 (47.2%, with 95% CI:(43.2, 51.2)) among sick under-five children caregivers in the past six months at Shashogo district.
This study depicted that almost one in two caregivers (47.2%) utilized ICCM service. This implied that more than half of illegible under-five children did not receive ICCM service. The possible reason for this low ICCM service utilization could be either health post bypass the service offered freely or not utilizing any other health care-seeking service though their child became sick. Though the reason was either of the case, the community has not been benefited. This finding is lower than the studies conducted in South Sudan (74%) 7 and Nepal (69%). 21 The probable reasons may be the difference in mode of service delivery, access of services. In contrast to this higher ICCM utilization than studies done in a study conducted in south Ethiopia, Boloso Sore Woreda (25%), 22 Southern Ethiopia, Hadiya zone (22.5%), 23 siraleone (14%), 18 Uganda (27.3%), 9 and Ghana (30%). 24 This difference might be due to access, time, place, and social context variation between this study and previous studies.
Also, this study demonstrated a remarkably higher proportion of the ICCM service utilization among sick under-five children in Shashogo district Hadiya zone, compared to study done in Ethiopia in, Oromia zone, Agerfa district 10.5% 13 . The possible explanation might be supportive supervision to health post, time variation, and eligiblity criteria. The implementation performance assessment study done in west Hararghe and Jimma zones indicates significant increment on ICCM service utilization in comparison groups. 3 All interviewed caregivers majority receive ICCM service 89(43.0%) for diarrhea as most common childhood illness followed by fever/malaria 53(25.6%). Multi-country analysis in different sub-Saharan Africa indicates that annual expected cases treated for total ICCM were 27%. 7 This multi-country’s finding is lower than this study’s finding. The reasons could be overreporting and type of data source used (register review data). Evidence from FGD also supports this idea.
The study done in Kenya depicted a significant increment of ICCM service utilization from 2% to 35%, but lower than this study. 25 This might be a difference in socio-demographic factors and health service delivery system difference.
The current study revealed that caregiver’s information affects ICCM service utilization. Caregivers who had heard about ICCM services were 3.7 times more likely to use them than those who had not heard about them. This finding was supported by a study done in the Dara District, UNICEF literature,13,26 south Ethiopia, Boloso Sore Woreda 22 , and Hadiya zone. 23
This study also identified factors that influence ICCM service utilization was receiving training of health extension program packages were more likely to practice ICCM service as compared to those did not receive training. The possible explanation might be time difference as access to information source and recent strong governmental intervention than the previous study. Another study in Jimma and west Hararghe is in agreement with this study. 27
The current study also identified that mother/ caregivers having PNC visit in recent child were 13 times more likely to utilize ICCM service than those counterparts. This contradicts a research conducted in the Agerfa district. 13 This variation could be attributed to socio-cultural differences in study areas.
This study showed under-five children who had two and more times experience of common child hood illness were more likely to utilize ICCM service than one times illness-experienced children.
Of the total interviewed caregivers or mothers’ majority 272(81.9%) responded the lack of necessary supply to health post as main barriers not utilize ICCM service. This finding is consistent with a study done in Uganda. 28
Current study revealed 208(62.7%) of closed health post at visiting time and 90(27.1%) of long waiting time not to utilize ICCM service in Shashogo district.
The strength of this study is using both quantitative community-based studies triangulated with qualitative data collected at parallel to enhance validity and credibility.
The possibility of recall bias and social desirability bias due to self-report could be limitation of this study.
Conclusion
Less than half of respondents utilized integrated community case management service in the Shashogo district. This study showed that having PNC visit in recent child, heard information for ICCM service, experienced frequent time of childhood illness and received health extension package training showed statistically significant positive association with ICCM service utilization.
The reasons not to utilize ICCM service among participants were mainly for lack of necessary supply and closed health post at visiting time.
Recommendation
To Woreda Health office, zonal health department, regional health bureau, Federal Minister of health and Non-governmental organizations working on Primary health care: Collaborative activities of information, education, and communication activities needed. Giving emphasis on model family training of health extension packages is mandatory. Strengthening the integration of ICCM service provision with maternal and child health service such as antenatal, postnatal care and EPI services.
Supplemental Material
Supplemental material, sj-docx-1-smo-10.1177_20503121221097643 for Utilization of integrated community case management service of childhood illness (ICCM) and associated factors among under-five children in Shashogo district, Hadiya zone, south Ethiopia by Endale Abera Kassa, Tilahun Beyene Handiso, Bittiya Admassu and Aderajew Nigussie in SAGE Open Medicine
Acknowledgments
We would like to thank Jimma University, data collectors, supervisors, and respondents.
Footnotes
Declaration of conflicting interests: The author(s) declared no potential conflicts of interest with respect to the research, authorship, and/or publication of this article.
Ethical approval: Prior to data collection ethical clearance was obtained from the ethical review board of the Jimma University institute of Health. Ethical committee reviewed and approved as verbal consent will be obtained before data collection.
Funding: The author(s) received no financial support for the research, authorship, and/or publication of this article.
Informed consent: Verbal Informed consent was obtained from each participants, which was initially approved by ethical review board of the Jimma University institute of Health.
ORCID iD: Tilahun Beyene Handiso  https://orcid.org/0000-0002-5113-6763
https://orcid.org/0000-0002-5113-6763
Supplemental material: Supplemental material for this article is available online.
References
- 1. Simoes EA, Desta T, Tessema T, et al. Performance of health workers after training in integrated management of childhood illness in Gondar, Ethiopia. Bull World Health Organ 1997; 75: 43–53. [PMC free article] [PubMed] [Google Scholar]
- 2. Child health: integrated community case management, 2014, https://www.mchip.net/interventions/child-health/integrated-community-case-management/
- 3. Miller NP, Amouzou A, Tafesse M, et al. Integrated community case management of childhood illness in Ethiopia: implementation strength and quality of care. Am J Trop Med Hyg 2014; 91: 424–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 4. Amouzou A, Morris S, Moulton LH, et al. Assessing the impact of integrated community case management (ICCM) programs on child mortality: review of early results and lessons learned in sub–Saharan Africa. J Glob Health 2014; 4: 020411. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5. Ghana Evidence Review Symposium Integrated community case management/ICCM/story in Ethiopia: background, 2014, https://www.childhealthtaskforce.org/sites/default/files/2019-07/iCCM%20Symposium%20Presentation_iCCM%20in%20Ethiopia%28MOH%20Ethiopia%2C%202014%29.pdf
- 6. UNICEF, Levels and trends in child mortality, 2017, https://data.unicef.org/resources/levels-trends-child-mortality-2017/
- 7. Oliphant NP, Muñiz M, Guenther T, et al. Multi–country analysis of routine data from integrated community case management (ICCM) programs in sub–Saharan Africa. J Glob Health 2014; 4: 020408. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8. Daviaud E, Besada D, Leon N, et al. Costs of implementing integrated community case management (ICCM) in six African countries: implications for sustainability. J Glob Health 2017; 7: 010403. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9. Muhumuza G, Mutesi C, Mutamba F, et al. Acceptability and utilization of community health workers after the adoption of the integrated community case management policy in Kabarole district in Uganda. Health Syst Policy Res 2015; 2: 13. [PMC free article] [PubMed] [Google Scholar]
- 10. Sinyangwe C, Graham K, Nicholas S, et al. Assessing the quality of care for pneumonia in integrated community case management: a cross-sectional mixed methods study. PLoS ONE 2016; 11: e0152204. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11. Teferi E, Teno D, Ali I, et al. Quality and use of IMNCI services at health center under-five clinics after introduction of integrated community-based case management (ICCM) in three regions of Ethiopia. Ethiop Med J 2014; 52: 91–98. [PubMed] [Google Scholar]
- 12. Yansaneh AI, Moulton LH, George AS, et al. Influence of community health volunteers on care seeking and treatment coverage for common childhood illnesses in the context of free health care in rural Sierra Leone. Trop Med Int Health 2014; 19: 1466–1476. [DOI] [PubMed] [Google Scholar]
- 13. Gorfu MB. Factors affecting utilization of integrated community case management of common childhood illnesses in Agarfa woreda, Oromiya regional state, Ethiopia, 2014, https://uir.unisa.ac.za/bitstream/handle/10500/18597/dissertation_mersha_bogale_gorfu.pdf?sequence=1&isAllowed=y
- 14. Miller NP, Amouzou A, Tafesse M, et al. Integrated community case management of childhood illness in Ethiopia: implementation strength and quality of care. Am J Trop Med Hyg 2014; 91: 424–434. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 15. Shaw B, Amouzou A, Miller NP, et al. Determinants of utilization of health extension workers in the context of scale-up of integrated community case management of childhood illnesses in Ethiopia. Am J Trop Med Hyg 2015; 93: 636–647. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 16. Amouzou A, Hazel E, Shaw B, et al. Effects of the integrated community case management of childhood illness strategy on child mortality in Ethiopia: a cluster randomized trial. Am J Trop Med Hyg 2016; 94: 596–604. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17. Andersen RM, Davidson PL, Baumeister SE. Improving access to care, 2013, https://www.scirp.org/(S(351jmbntvnsjt1aadkposzje))/reference/ReferencesPapers.aspx?ReferenceID=1354237
- 18. Yansaneh AI, George AS, Sharkey A, et al. Determinants of utilization and community experiences with community health volunteers for treatment of childhood illnesses in rural Sierra Leone. J Community Health 2016; 41: 376–386. [DOI] [PubMed] [Google Scholar]
- 19. Marsh DR, Nefdt R, Hazel E. Introduction to a special supplement: delivering integrated community case management to treat childhood illness at scale in Ethiopia. Ethiop Med J 2014; 52: 1–6. [PubMed] [Google Scholar]
- 20. Mitiku I, Assefa A. Caregivers’ perception of malaria and treatment-seeking behaviour for under five children in Mandura district, west Ethiopia: a cross-sectional study. Malar J 2017; 16: 144. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 21. Young M, Wolfheim C, Marsh DR, et al. World Health Organization/United Nations Children’s Fund joint statement on integrated community case management: an equity-focused strategy to improve access to essential treatment services for children. Am J Trop Med Hyg 2012; 87: 6–10. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 22. Samuel S, Arba A. Utilization of integrated community case management service and associated factors among mothers/caregivers who have sick eligible children in southern Ethiopia. Risk Manag Healthc Policy 2021; 14: 431–438. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 23. Yohannes S, Habtu Y, Abreham B, et al. Utilization of integrated community case management and its factors in southern Ethiopia: facility based-cross-sectional study. Adv Publ Health 2021; 2021: 8835804. [Google Scholar]
- 24. Ferrer BE, Webster J, Bruce J, et al. Integrated community case management and community-based health planning and services: a cross sectional study onthe effectiveness of the national implementation for the treatment of malaria, diarrhoea and pneumonia. Malar J 2016; 15: 340. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25. Kisia J, Nelima F, Otieno DO, et al. Factors associated with utilization of community health workers in improving access to malaria treatment among children in Kenya. Malar J 2012; 11: 248. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 26. UNICEF and PATH, Literature review on barriers to utilization of health extension services: draft report, 2016, https://www.childhealthtaskforce.org/sites/default/files/2019-05/Literature%20Review%20on%20Barriers%20to%20Utilization%20of%20Health%20Extension%20Services%20Draft%20Report%28UNICEF%2CPATH%2C2016%29.pdf
- 27. Miller NP, Amouzou A, Bryce J, et al. Assessment of iCCM implementation strength and quality of care in Oromia, Ethiopia. Baltimore, USA and Addis Ababa, Ethiopia: Institute for International Programs, Johns Hopkins Bloomberg School of Public Health, 2013. https://www.jhsph.edu/research/centers-and-institutes/institute-for-international-programs/_docs/mcnh-rapid-scale-up/Ethiopia_QoC-IS_Final_Report_16Jan2013.pdf [Google Scholar]
- 28. Mukanga D, Tibenderana JK, Peterson S, et al. Access, acceptability and utilization of community health workers using diagnostics for case management of fever in Ugandan children: a cross-sectional study. Malar J 2012; 11: 121. [DOI] [PMC free article] [PubMed] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
Supplemental material, sj-docx-1-smo-10.1177_20503121221097643 for Utilization of integrated community case management service of childhood illness (ICCM) and associated factors among under-five children in Shashogo district, Hadiya zone, south Ethiopia by Endale Abera Kassa, Tilahun Beyene Handiso, Bittiya Admassu and Aderajew Nigussie in SAGE Open Medicine