Abstract
A veterinarian presented with multiple erythematous tender nodules over his right hand and arm. One month prior to the appearance of the lesions, he had treated a cat imported from Brazil who had ulcerated pustular cutaneous lesions. Despite antibiotic treatment there had been no improvement in his symptoms.
Biopsies from the patient were sent for histology, bacterial and fungal culture. Periodic acid-Schiff (PAS) stains showed a PAS positive oval yeast-like micro-organism with surrounding necrosis. Fungal cultures resembling Sporothrix species grew after 18 days with typical appearances seen on direct microscopy; this was confirmed as Sporothrix brasiliensis on 18S PCR. The patient was treated with oral itraconazole.
This is a unique case of cutaneous S. brasiliensis acquired from an infected imported cat. S. brasiliensis is a rare pathogen in the UK. This case has clinical relevance due to its unusual aetiology and in raising awareness of rarer infections associated with importation of pets and global travel. Clinicians should be aware of sporotrichosis as a differential diagnosis for cutaneous and extracutaneous infection in patients with a high risk of exposure, as well as the use of appropriate diagnostic tests.
Keywords: Infectious diseases, Dermatology, Global Health, Tropical medicine (infectious disease)
Background
Sporotrichosis is primarily a cutaneous infection caused by dimorphic fungi from the genus Sporothrix. These fungi are widespread in the environment, most commonly found in soil and plant material. Sporotrichosis in Europe is usually associated with Sporothrix schenckii; however, there are other species which are human pathogens such as Sporothrix brasiliensis, Sporothrix globosa and Sporothrix luriei.1 S. brasiliensis is typically geographically limited to South America.
Cutaneous sporotrichosis is associated with gardening and agricultural work, but can also be acquired via cat scratches, bites or contact with exudate from cutaneous lesions.2 Cutaneous infection is caused by inoculation with infected organic material leading to the formation of an erythematous papule which later ulcerates. It can cause lymphocutaneous disease; lesions can exhibit sporotrichoid-like spread. Extracutaneous infection has been described resulting in pulmonary, ocular, bone and meningeal disease with disseminated sporotrichosis reported in severely immunocompromised patients.3
In Brazil, S. brasiliensis has emerged as a significant disease in cats with more than 12 000 cases recorded in the state of Rio de Janeiro between 2000 and 2017.4 Additionally over 5000 cases of zoonotic disease have been reported in humans between 1998 and 2015.5
Although Sporothrix species has a global distribution, infection in cats in the UK is rare. A case report in 2020 described the first case of cutaneous sporotrichosis in a cat in the UK which was confirmed to be caused by Sporothrix humicola.6 The cat in our case was diagnosed clinically with sporotrichosis infection suggesting there may be additional unrecognised cases within the UK.
Diagnosis is based on the isolation of Sporothrix species from clinical specimens. Sporothrix species is a thermally dimorphic fungus and is typically isolated after 5–7 days on Sabourard dextrose agar. At 25°C–30°C Sporothrix species colonies appear as finely wrinkled and cream in colour which then turn brown or black, whereas at 37°C colonies are creamy white with a smooth texture.2 Branched hyaline septate hyphae are seen microscopically and the conidiophore has round hyaline conidia arranged in a characteristic bouquet formation at 25°C.7
Histopathological diagnosis can also be made by demonstrating fungal structures in the tissue using periodic acid-Schiff (PAS) or Grocott’s methenamine silver stains. Species-specific PCR is also available to differentiate between Sporothrix species and can be used to detect infection from clinical specimens.8
Case presentation
A veterinarian in his late 20s who is normally fit and well presented with a 1 week history of erythematous tender swellings over his right middle finger, upper arm and elbow associated with right-sided axillary lymphadenopathy. He denied fevers and was systemically well. He was initially prescribed flucloxacillin for possible cellulitis followed by cephalexin and metronidazole, and then oral co-amoxiclav with minimal improvement in his lesions.
He subsequently presented to the emergency department 6 weeks after the initial appearance of the lesions. His lesions had increased in size and spread up the arm. On examination the patient had nodular, mildly tender lesions measuring approximately 6×4 cm over the antecubital fossa and 2×2 cm over his elbow (see figure 1). Additionally he was noted to have several pea size nodules over his forearm. The lesion on his finger was ulcerated with some desquamation seen (see figure 2). The patient denied any extracutaneous symptoms.
Figure 1.

Example of sporotrichoid spread seen over patient’s right arm.(Courtesy of patient, 2021)
Figure 2.

Ulcerated lesion seen on patient’s finger. (Courtesy of patient, 2021)
Clinical history revealed that 4 weeks prior to the appearance of the lesions, he was scratched by a pet cat at work. The cat had been imported from Brazil in 2019 and had granulomatous and ulcerated skin lesions which had been present for 6 months. The cat’s lesions were initially suspected to be inflammatory in nature but did not improve with non-steroidal treatment. The cat then had samples taken for histology which were suggestive of fungal infection with no definitive fungal organism identified.
Based on clinical history and examination in addition to the histology results from the cat, the possibility of S. brasiliensis was considered. A course of itraconazole was commenced.
Biopsies from the patient were sent for histology, bacterial and fungal culture. PAS stains showed a PAS-positive oval yeast-like micro-organism with surrounding necrosis (see figures 3 and 4). White-grey colonies appeared on Sabourard dextrose agar after 18 days of incubation (figure 5). Lactophenol cotton blue preparation of the culture demonstrated microscopic appearances consistent with Sporothrix species (figure 6). This was later confirmed as S. brasiliensis via 18S PCR. The sample was sent to the reference laboratory for susceptibility testing, and later confirmed as sensitive to itraconazole. Bacterial cultures showed no growth.
Figure 3.
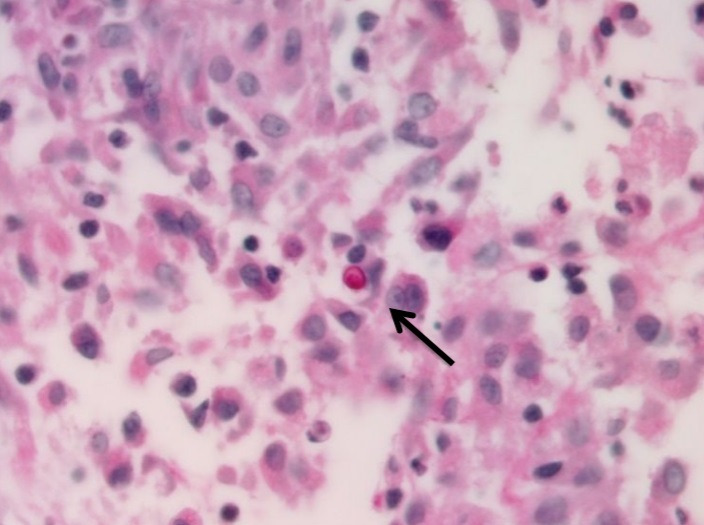
High magnification (600x) pictures of the periodic acid-Schiff stain with one micro-organism surrounded by mixed inflammatory infiltrate (Image courtesy Dr Marcin Ligaj, Consultant Histopathologist, 2021)
Figure 4.
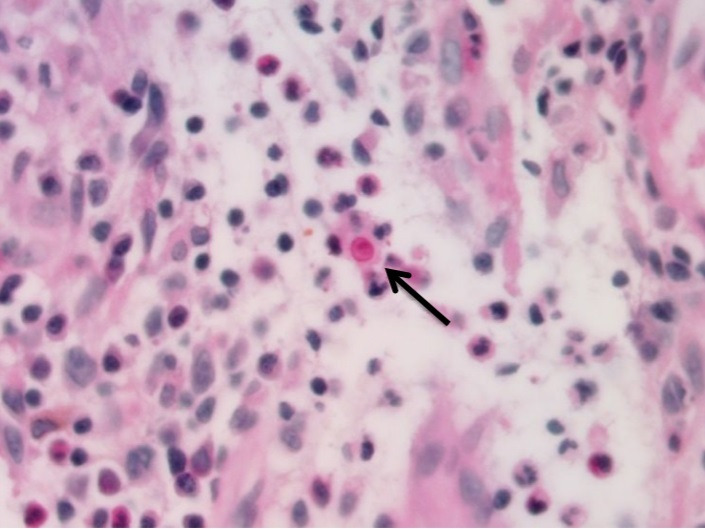
High magnification (600x) pictures of the periodic acid-Schiff stain with one micro-organism surrounded by mixed inflammatory infiltrate (Image courtesy Dr Marcin Ligaj, Consultant Histopathologist, 2021).
Figure 5.

Colony growth seen on Sabourard dextrose agar.(Courtesy of Dr Raissa Rachman, 2021)
Figure 6.
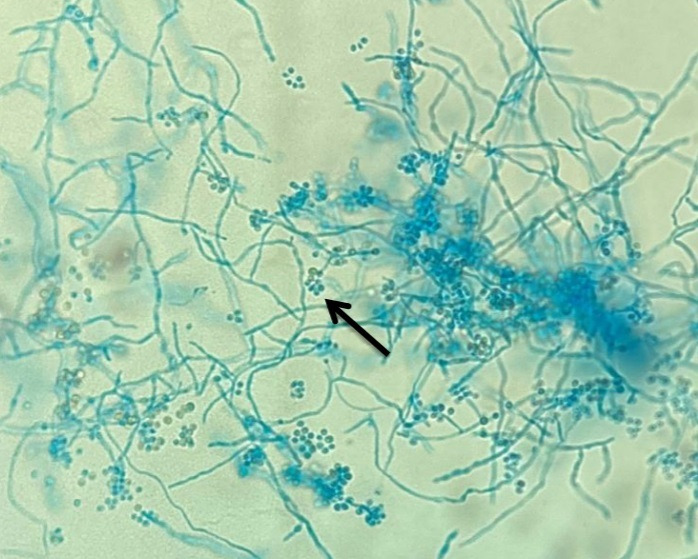
Lactophenol cotton blue stain seen at high magnification (100x) showing branching hyphae and clustered conidia typically seen in Sporothrix spp.(Courtesy of Dr Raissa Rachman, 2021)
Treatment
The patient was treated with oral itraconazole 200 mg capsules once daily as recommended in the Infectious Disease Society of America clinical practice guidelines for the treatment of sporotrichosis.9 The patient was found to have low serum itraconazole levels; therefore, his dose was increased to 200 mg two times per day. The planned treatment duration was 6 months. The patient’s liver function was monitored and remained stable during the course of treatment. The patient also independently applied over the counter topical clotrimazole ointment to the lesion.
Outcome and follow-up
At 3-month follow-up, he was systemically well, the lesions on his arm had reduced in size and the ulcer on the index finger was completely healed (see figure 7).
Figure 7.

Resolution of lesion on patient’s finger. (Courtesy of patient, 2021)
Discussion
This is the first report of zoonotic transmission of S. brasiliensis in the UK. Sporotrichosis is a very rare disease in the UK with only a few cases previously described.
S. brasiliensis was first identified among cats in 1997 and due to high transmission via bites and scratches, it is now considered endemic in cats in South America.4 Outbreaks of zoonotic S. brasiliensis have occurred in Brazil10 and further zoonotic Sporothrix species infections have been described in Malaysia, Thailand, Germany, India and Argentina.4 5 11
In humans, the cutaneous lesions caused by Sporothrix species infection can take up to 12 weeks to develop and can easily be mistaken for a bacterial infection. This can lead to delayed diagnosis and treatment; lesions can continue to spread causing significant morbidity.
The lesions usually begin on exposed or traumatised skin such has fingers and hands. The spores then spread in a lymphocutaneous distribution, classically referred to as ‘sporotrichoid spread’. Sporotrichosis should be considered as a differential in at-risk populations such as veterinarians and cat owners especially if there has been contact with imported animals.
Without early diagnosis and treatment, disseminated spread can occur causing pulmonary and musculoskeletal disease. Biopsy for fungal culture and histopathology have a pivotal role in diagnosis. Antifungal susceptibility testing is recommended due to variable activity of some azole antifungals. Notably voriconazole has been found to have low inhibitory activity in vitro so would not be recommended as a treatment.4 Antifungal treatment with oral itraconazole has a high success rate and should be used to treat lesions. Treatment should be continued for 2–4 weeks after all lesions have resolved, usually lasting for a total of 3–6 months.
Learning points.
Sporotrichosis is emerging globally as an important zoonotic infection associated with cats. Diagnosis should be considered in patients presenting with a granulomatous lesion and history of exposure to or work with cats, especially when there has been limited improvement with antibiotics.
Differential diagnosis of the skin lesions include Mycobacterium marinum infection (fish tank granuloma), cutaneous leishmaniasis and cutaneous nocardiosis.
As numbers of cats imported to the UK continue to rise there may be an associated increase in imported zoonoses, particularly Sporothrix brasiliensis in cats imported from South America.
Diagnosis of sporotrichosis can be aided by sampling of cutaneous lesions for histology, fungal culture and molecular methods such as 18S PCR.
Oral itraconazole 200 mg once daily is the recommended treatment for lymphocutaneous disease and should be continued for 2–4 weeks after resolution of lesions. Patients taking a prolonged course of itraconazole should have liver function monitored if receiving other hepatotoxic drugs, or if at risk of hepatotoxicity or liver disease.
Acknowledgments
The authors wish to thank the patient Mr Lukas Vasiliaukas for his involvement in the case report.
Footnotes
Contributors: RR wrote the case report. SC and RS-W reviewed the report. RR and ML were involved in the microbiological diagnosis. All four authors were involved in the patient's care.
Funding: The authors have not declared a specific grant for this research from any funding agency in the public, commercial or not-for-profit sectors.
Case reports provide a valuable learning resource for the scientific community and can indicate areas of interest for future research. They should not be used in isolation to guide treatment choices or public health policy.
Competing interests: None declared.
Provenance and peer review: Not commissioned; externally peer reviewed.
Ethics statements
Patient consent for publication
Obtained.
References
- 1.Chakrabarti A, Bonifaz A, Gutierrez-Galhardo MC, et al. Global epidemiology of sporotrichosis. Med Mycol 2015;53:3–14. 10.1093/mmy/myu062 [DOI] [PubMed] [Google Scholar]
- 2.Barros MBdeL, de Almeida Paes R, Schubach AO. Sporothrix schenckii and sporotrichosis. Clin Microbiol Rev 2011;24:633–54. 10.1128/CMR.00007-11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 3.Freitas DFS, de Siqueira Hoagland B, do Valle ACF, et al. Sporotrichosis in HIV-infected patients: report of 21 cases of endemic sporotrichosis in Rio de Janeiro, Brazil. Med Mycol 2012;50:170–8. 10.3109/13693786.2011.596288 [DOI] [PubMed] [Google Scholar]
- 4.Etchecopaz A, Toscanini MA, Gisbert A, et al. Sporothrix Brasiliensis: A Review of an Emerging South American Fungal Pathogen, Its Related Disease, Presentation and Spread in Argentina. J Fungi 2021;7. 10.3390/jof7030170. [Epub ahead of print: 26 Feb 2021]. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Gremião IDF, Oliveira MME, Monteiro de Miranda LH, et al. Geographic expansion of sporotrichosis, Brazil. Emerg Infect Dis 2020;26:621–4. 10.3201/eid2603.190803 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Makri N, Paterson GK, Gregge F, et al. First case report of cutaneous sporotrichosis (Sporothrix species) in a cat in the UK. JFMS Open Rep 2020;6:205511692090600. 10.1177/2055116920906001 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 7.Orofino-Costa R, Macedo PMde, Rodrigues AM, et al. Sporotrichosis: an update on epidemiology, etiopathogenesis, laboratory and clinical therapeutics. An Bras Dermatol 2017;92:606–20. 10.1590/abd1806-4841.2017279 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Rodrigues AM, de Hoog GS, de Camargo ZP. Molecular diagnosis of pathogenic Sporothrix species. PLoS Negl Trop Dis 2015;9:e0004190. 10.1371/journal.pntd.0004190 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 9.Kauffman CA, Bustamante B, Chapman SW, et al. Clinical practice guidelines for the management of sporotrichosis: 2007 update by the infectious diseases Society of America. Clin Infect Dis 2007;45:1255–65. 10.1086/522765 [DOI] [PubMed] [Google Scholar]
- 10.Rodrigues AM, de Melo Teixeira M, de Hoog GS, et al. Phylogenetic analysis reveals a high prevalence of Sporothrix brasiliensis in feline sporotrichosis outbreaks. PLoS Negl Trop Dis 2013;7:e2281. 10.1371/journal.pntd.0002281 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 11.Reinprayoon U, Jermjutitham M, Tirakunwichcha S, et al. Conjunctival sporotrichosis from cat to human: case report. Am J Ophthalmol Case Rep 2020;20:100898. 10.1016/j.ajoc.2020.100898 [DOI] [PMC free article] [PubMed] [Google Scholar]


