Abstract
Background
Virtual reality (VR) is a computer technology that immerses a user in a completely different reality. The application of VR in acute pain settings is well established. However, in chronic pain, the applications and outcome parameters influenced by VR are less clear.
Objective
This review aimed to systematically identify all outcome parameters that are reported in relation to VR in patients with chronic pain.
Methods
A total of 4 electronic databases (PubMed, Scopus, Web of Science, and Embase) were searched for relevant studies. Multilevel random-effect meta-analyses were performed, whereby the standardized mean difference was chosen as the effect size to denote the difference between measurements before and after a VR intervention.
Results
The initial database search identified 1430 studies, of which 41 (2.87%) were eventually included in the systematic review. Evidence has been found for the effects of VR on pain, functioning, mobility, functional capacity, psychological outcomes, quality of life, neuropsychological outcomes, and physical sensations. The overall effect size (a total of 194 effect sizes from 25 studies) based on a three level meta-analysis was estimated at 1.22 (95% CI 0.55-1.89; z=3.56; P<.001), in favor of improvements after a VR intervention. When categorizing effect sizes, the overall effect sizes were reported as follows: 1.60 (95% CI 0.83-2.36; z=4.09; P<.001) for the effect of VR on pain (n=31), 1.40 (95% CI 0.13-2.67; z=2.17; P=.03) for functioning (n=60), 0.49 (95% CI −0.71 to 1.68; z=0.80; P=.42) for mobility (n=24), and 0.34 (95% CI −1.52 to 2.20; z=0.36; P=.72) for functional capacity (n=21).
Conclusions
This systematic review revealed a broad range of outcome variables influenced by an intervention of VR technology, with statistically significant pain relief and improvements in functioning. These findings indicate that VR not only has applications in acute pain management but also in chronic pain settings, whereby VR might be able to become a promising first-line intervention as complementary therapy for patients with chronic pain.
Trial Registration
PROSPERO International Prospective Register of Systematic Reviews CRD42021227016; https://www.crd.york.ac.uk/prospero/display_record.php?RecordID=227016
Keywords: virtual reality, chronic pain, systematic review, multilevel meta-analysis, immersive technologies, clinical outcomes, mobile phone
Introduction
Background
After the recent revision of the definition of pain in 2020 by the International Association for the Study of Pain, chronic primary pain is defined as pain in 1 or more anatomical regions that (1) persists or recurs for >3 months and (2) is associated with significant emotional distress (eg, anxiety, anger, frustration, or depressed mood) or significant functional disability (interference in activities of daily life and participation in social roles), and (3) the symptoms are not better accounted for by another diagnosis [1]. Approximately 19% of adults complain of chronic pain [2], resulting in significant physical and mental burden as well as significant economic and social consequences [3,4]. Pain management for chronic pain conditions that are incorporated within chronic primary pain often entails a multidisciplinary or interdisciplinary pain management program relying on a biopsychosocial approach [5], mostly with a focus on functional restoration [6]. For the management of long-term pain, public opinion is currently in strong favor of self-management strategies as a first-line effective strategy to engage patients in actively managing their own health status [7-9]. The safety and cost-effectiveness of self-management programs have been proven; nevertheless, the effect sizes are small and not sustained in the long term [7,10]. In addition, the limited efficacy of pharmacotherapy in treating chronic pain and the long-term side effects of these pharmacological treatment options [11,12] have put a premium on novel nonpharmacological therapy options for chronic pain, thereby creating room for promising new pain management strategies such as virtual reality (VR) [13,14].
VR is characterized by an artificial computer-generated environment created to replace real-world sensory inputs [15]. This technology has evolved rapidly over the last 2 decades [16] and can be operationally described as simulations that use a combination of interaction devices and sensory display systems [17]. Within VR applications, an important distinction can be made between immersive and nonimmersive media, whereby they differ based on the participant’s point of view and the experience that is produced during the application (ie, difference in spatial presence [18]) [19]. With immersive technology, participants view the full panorama, which enables the creation of a high sense of presence and immersion as if the participant is essentially inside the created environment [19]. In a nonimmersive environment, virtual content is based on how the device (PC, smartphone, or tablet) is moved or rotated, and participants are only external observers [20].
In both acute and chronic pain settings, the main idea of VR is to create distraction from the painful region [21]. VR can affect pain perception through immersive virtual environments, by occupying finite attentional resources, and by blocking external stimulation associated with the real environment and painful stimuli [22]. As distraction interventions work by competing for attention otherwise directed toward painful stimuli, pain tolerance and pain thresholds have been shown to increase under VR conditions [23]. Moreover, pain intensity, anxiety, and time spent thinking about pain decreased after VR distraction [24]. VR is thought to be more effective than traditional methods of distraction (eg, pleasant imagining, rhythmic cognitive activities, external focus of attention, and neutral imagining [25]) because of its immersive property, encompassing a patient’s visual and auditory processing and even physical actions, which, in theory, demand more attention [26]. In addition to distraction as an underlying analgesic effect of VR, the long-term use of VR is expected to induce neuroplastic changes in the sensory and motor brain regions [27].
Objectives
Several systematic reviews have stressed the effectiveness of VR in the management of acute pain associated with medical procedures, wound debridement, and experimental pain [28-31]. The implementation of VR in chronic pain settings is still in its infancy compared with the widely accepted use of VR in acute pain settings [16]. Within the context of chronic pain, VR could be applied as an analgesic intervention and distraction method or could address pain-related behaviors [32]. Nevertheless, there is no consensus yet on which outcome measures VR has a positive effect in chronic pain settings. Therefore, this systematic review and meta-analysis aimed to evaluate the effect of VR on several outcome parameters related to the application of VR in patients with chronic pain.
Methods
Protocol and Registration
The study protocol was registered prospectively with PROSPERO (CRD42021227016). This systematic review and meta-analysis was conducted according to the PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) guidelines [33].
Search Strategy
A search strategy based on the PICO (Patient or Population, Intervention, Comparison, and Outcome; evidence-based search strategy focusing on patients or populations, interventions, comparisons, and outcomes) framework was developed [34]. The following research question was constructed: The effects of virtual reality (intervention) on multiple outcome measurements (outcome) in patients with chronic pain (population). The component control was not defined for this question. The final search strategy was built by combining free and Medical Subject Headings terms. Within Population, Intervention, and Outcome, search terms were combined using the Boolean term OR. The Boolean term AND was used between the complete search terms for Population, Intervention, and Outcome. The search strategy was conducted using the following databases: PubMed, Embase, Scopus, and Web of Science from their outset until December 2020. No limitations were applied to the search. The full search strategy for PubMed is outlined in Multimedia Appendix 1.
Eligibility Criteria
Studies exploring the effects of VR in patients with chronic pain were eligible for inclusion. Studies with both adults and children were eligible if the study participants experienced chronic pain. Chronic pain was defined as pain that lasted for >3 months [35], including patients with primary and secondary chronic pain conditions. Studies in which the effect of VR was explored in healthy participants or in acute pain settings were excluded. For this intervention, there were no restrictions on the VR devices, and all types of VR were permitted, including (but not limited to) studies with head-mounted displays, video games, displays with body motion sensors, Nintendo Wii consoles, Xbox, PlayStation, and computers. Studies that did not use VR to explore its effects on patients with chronic pain were excluded. There were no limitations in the outcome measurements because the goal was to explore the effects of VR on all types of outcome variables that were recorded in this setting. Studies reporting in languages other than English, Dutch, French, or German were excluded. Publications available only in abstract form, conference abstracts, expert opinions, letters to the editor, study protocols, reviews, meta-analyses, or meeting reports were considered not suitable for inclusion.
Study Selection
After deduplication using the EndNote X9 reference manager (Clarivate), 2 reviewers (JJ and VN) independently screened all retrieved articles for titles and abstracts using the Rayyan web-based software (Rayyan Systems Inc) [36]. Subsequently, the same 2 reviewers performed the full-text screening (independently). If discrepancies occurred, consensus was sought through consultation and discussion with a third independent reviewer (ADS).
Data Extraction
All relevant information concerning the possible effects of VR in patients with chronic pain was synthesized in an a priori constructed evidence table. The following items were extracted from each of the remaining articles: author, publication year, country, study design, sample size (including sex distribution), underlying pathology, VR application (including duration, type of VR, and device), and reported outcome measurements. Data extraction was performed by one reviewer (JJ) and checked for correctness by another (LG). Any discrepancies were discussed in a consensus meeting with all the reviewers.
Risk of Bias Assessment
A modified version of the Downs and Black checklist was used to assess the quality of the included studies [37]. This instrument, consisting of 27 items, was developed to evaluate the methodological quality of several study designs, including randomized trials, nonrandomized trials, and observational studies [37]. All items were categorized into 5 subscales: reporting, external validity, bias, confounding, and power. Each item was given a score of 0 (no) or 1 (yes), except for item 5, where a score of 1 meant the item was partially presented and a score of 2 if a complete description was presented. The answer option not applicable was also available. The scoring of item 27, which refers to the power of the study, had been modified in the sense that it received a score of 1 if a power calculation was performed and 0 otherwise [38,39]. After scoring each individual item, all included studies were categorized as having poor, fair, good, or excellent quality based on the total score for further data synthesis. A total score of ≤14 out of 28 was considered poor quality, 15-19 was considered fair, 20-25 was considered good, and 26-28 was considered excellent methodological quality [40].
Statistical Procedure for the Meta-analysis
The standardized mean difference was chosen as the effect size to compare the differences between measurements before and after the VR intervention, calculated as the difference in sample means after VR minus before VR, divided by the SD before VR (g gain).nOnly sample SDs of the measurements before VR, instead of pooled SDs, were used in the calculation because they are not influenced by VR effects and are therefore more likely to be consistent across studies [41]. Correlations between measurements were estimated to be 0.5. As standardized mean difference does not correct for differences in the direction of the scale, the mean values from outcomes that have a higher score when they reveal an improvement are multiplied by −1 to ensure that all the scales point in the same direction. Thus, the effect size measures are positive if the data indicate a desirable effect of VR. Several studies included more than one outcome measurement, wherefore a random-effect 3-level meta-analysis was performed [42]. Thus, a 3-level meta-analysis model was fitted with sampling variance at the first level, within-study variance at the second level, and between-study variance at the third level [42]. Meta-analyses were performed for all effect sizes combined and for effect sizes categorized according to the type of outcome measurements (ie, pain, functioning, mobility, and functional capacity). Meta-analyses were performed using R Studio (R Foundation for Statistical Computing) version 1.4.1106 (R version 4.0). P≤.05 was considered statistically significant. Figures were created based on the code provided by Fernández-Castilla et al [43] to visually present the results of meta-analyses of multiple outcomes. Only studies with sufficient data were included in this meta-analysis. If insufficient information was provided, the authors were contacted to provide more in-depth data.
Results
Study Selection
A total of 1430 articles were identified through 4 database searches (Figure 1). After removing duplicates, 687 (48.04%) articles were selected for screening. After screening titles and abstracts, 13.2% (91/687) of articles remained eligible for full-text screening. Studies were excluded based on study design or reporting (n=198), no patients with chronic pain (n=194), no VR as intervention (n=199), duplicates (n=4), or other languages (n=1). The percentage of agreement on title and abstract screening between both reviewers was 92.8%. After full-text screening, 41 articles were included in this systematic review. The primary reasons for study exclusion were no patients with chronic pain (n=10), no VR as intervention (n=13), and a different study design or reporting (n=27). The percentage agreement between both reviewers for full-text screening was 95.7%. Data from 25 studies were included in the meta-analysis.
Figure 1.
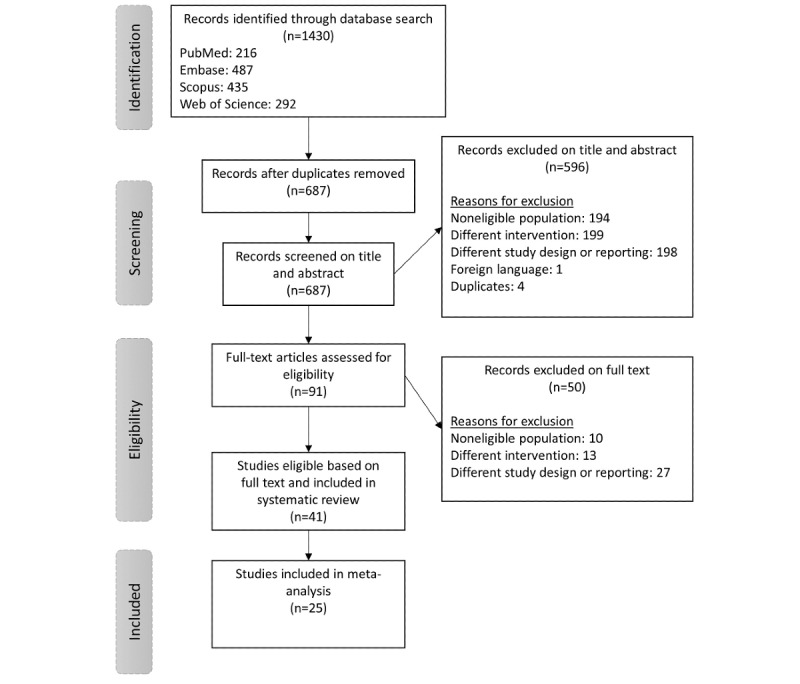
PRISMA (Preferred Reporting Items for Systematic Reviews and Meta-Analyses) flowchart.
Study Characteristics
A comprehensive overview of the characteristics of the included studies is presented in Table 1. The earliest study included in this review was published in 2008 and the most recent study, in 2020. In terms of study design, the following studies were included: 18 quasi-experimental study designs, 16 randomized controlled trials, and 7 case series.
Table 1.
Characteristics of the included studies.
| Authors | Country | Design | Participants, N (number of female participants) | Population | Duration of the intervention | VRa device and application | Type of VR | Outcome measurements |
| Alemanno et al [62] | Italy | QEb | 20 (11) | Adults with chronic low back pain | 1 hour per session for 12 sessions over 4-6 weeks | VR Rehabilitation System, Khymeia, Italy | Nonimmersive | Roland and Morris Disability Questionnaire, Repetition Index, SF-36 Short Form Health Survey, NRSc Pain, McGill Pain Questionnaire, Brief Pain Inventory, Beck Depression Inventory, and neuropsychological evaluations |
| Amin et al [44] | Canada | RCTd | 30 (13) | Adult patients with chronic pain | 2×10 minutes | Oculus Rift DK2 and a Cardboard VR to play InMind | Immersive | Present and retroactive pain intensity |
| Botella et al [55] | Spain | QE | 6 (6) | Adult patients with fibromyalgia | 7 weeks with ten 2-hour sessions: sessions 1 through 6 were delivered twice a week for 3 weeks, whereas sessions 7 through 10 were delivered weekly for 4 weeks | 2 PCs, a large projection screen, 2 projectors, a wireless pad, and a speaker system. Application used: EMMAe World | Nonimmersive | Beck Depression Inventory II, Positive and Negative Affect Schedule, Chronic Pain Coping Inventory, Fibromyalgia Impact Questionnaire, and VR Satisfaction Scale |
| Brown et al [63] | United States | RCT | 45 (27) | Adults with chronic low back pain, receiving spinal injections | One 5-minute session | VR immersive format in the Oculus GoÒ headset | Immersive | Anxiety thermometer, NRS pain, Patient-Reported Outcomes Measurement Information System, Modified Oswestry Disability Index, and VR Symptom Questionnaire |
| Chau et al [73] | United States | CSf | 8 (7) | Upper limb complex regional pain syndrome (adults and 1 adolescent) | 10 sessions (1-3 per week) with 45-60 minutes each session | HTC Vive VR System (virtual 3D kitchen environment) | Immersive | Short Form McGill Pain Questionnaire, VASg, Wong-Baker Faces Scale, and Subjective feedback |
| Collado-Mateo et al [56] | Spain | RCT | 83 (83) | Adult patients with fibromyalgia | Twice a week for 1 hour per session over 8 weeks | An exergame called VirtualEx-FM based on Microsoft Kinect | Nonimmersive | Timed up and go test, functional reach, Clinical Test of Sensory Integration of Balance, fear of falling using VAS |
| Darnall et al [81] | United States | RCT | 88 (NDh) | Adults with chronic nonmalignant low back pain or fibromyalgia | 21 days | Oculus Go VR Headset (visual biofeedback in relaxation training) | Immersive | Defense and Veterans Pain Rating Scale; pain interference on activity, mood, sleep, and stress; pain catastrophizing scale; pain self-efficacy; global impression of change; satisfaction with treatment; and motion sickness and nausea |
| Fowler et al [45] | United States | QE | 16 (3) | Veterans with chronic pain | 19-day program with 20 minutes per VR session | Oculus Rift and Samsung Oculus Gear VR | Immersive | VR feasibility, Pain Outcomes Questionnaire-VA, Fear of Daily Activities, questionnaire for kinesiophobia, Pain Catastrophizing Scale, and patient-specific functional scale |
| Garcia-Palacios et al [57] | Spain | RCT | 61 (61) | Adults with fibromyalgia | Six 2-hour group sessions delivered twice a week | 2 PC computers with an EMMA VR environment | Nonimmersive | Fibromyalgia Impact Questionnaire, Brief Pain Inventory, Chronic Pain Coping Inventory, Beck Depression Inventory II, Quality of Life Index, and acceptability and satisfaction |
| Garrett et al [46] | Canada | CS | 8 (6) | Adults with chronic pain conditions | 1 month with 12 sessions of 30 minutes each | Oculus Rift DK2 1100 field of view stereoscopic HMDi | Immersive | NRS pain, Brief Pain Inventory, Self-Administered Leeds Assessment of Neuropathic Symptoms and Signs, cybersickness, and individual interviews |
| Griffin et al [80] | United States | QE | 17 (13) | Pediatric patients with chronic pain | 1-8 sessions of 30 minutes (once a week) | HTC Vive VR system | Immersive | Presence, child daily questionnaire, and interviews |
| Gromala et al [47] | Canada | RCT | 13 (7) | Adult patients with chronic pain | 1 moment | Technology’s DeepStream VR with virtual meditative walk | Immersive | NRS pain |
| Guarino et al [48] | Italy | CS | 11 (8) | Adult patients with chronic pain | 8 VR sessions of 30 minutes, 2 times a week | VR scenarios were run in a PC, and the environments were visualized on a monitor | Nonimmersive | McGill Pain Questionnaire, Brief Pain Inventory Severity and Interference, State trait Anxiety Inventory, Beck Depression Inventory, VAS, and subjective units of distress scales |
| Harvie et al [68] | Australia | CS | 12 (3) | Adults with chronic neck pain | 36-70 days with 10 minutes of VR twice a day | Samsung Gear VR system with Motor Offset Visual Illusion | Immersive | Pain threshold and NRS pain |
| Herrero et al [58] | Spain | QE | 40 (40) | Adults with fibromyalgia | 3 sessions of 20 minutes each | 2 PC computers, a 3.4-m screen made of reflective material, 2 projectors, and a Dolby 7.1 surround sound audio system with EMMA | Nonimmersive | Mood State, NRS pain, NRS fatigue, NRS motivation, NRS self-efficacy, and NRS of several emotions (joy, sadness, anger, surprise, anxiety, calmness, and vigor/energy) |
| House et al [82] | United States | QE | 12 (12) | Adults with persistent pain in shoulder and arm following postsurgical breast cancer | 20-50 minutes twice week for 8 weeks | BrightArm Duo technology with 3D custom integrative rehabilitation games | Nonimmersive | NRS pain, upper limb range of motion, Beck Depression Inventory II, Neurophysiological Assessment Battery, Revised Hopkins Verbal Learning Test, Revised Brief Visuospatial Memory Test, and Trail Making Test |
| Jin et al [49] | Canada | RCT | 20 (16) | Adults with chronic pain | 1 moment, 35-45 minutes per participant with 10-minute VR | Oculus Rift DK2 with Cryoslide game | Immersive | Pain intensity (VAS) and distraction |
| Jones et al [50] | United States | QE | 30 (20) | Adults with chronic pain conditions | Single 5-minute exposure to VR | Oculus rift DK2 and Deepstream VR with cool! | Immersive | NRS pain, engagement, and side effects |
| Matamala-Gomez et al [74] | Spain | QE | 19 (14) | Adults with neuropathic chronic pain in the upper limb | Single session of 55 minutes | HMD rift development kit 2, Oculus | Immersive | Ownership, agency, mental representation, NRS pain, and VR questionnaire |
| Matheve et al [64] | Belgium | RCT | 84 (54) | Adults with chronic low back pain | 2×2 minutes with 30 seconds of rest in between | Valedo Pro, Hocom | Nonimmersive | NRS pain, Roland and Morris Disability Questionnaire, Pain Catastrophizing Scale, Tampa Scale for Kinesiophobia, pain intensity, time spent thinking about pain, and pelvic tilts |
| Monteiro et al [65] | Portugal | RCT | 34 (34) | Adults with chronic low back pain | 8 weeks with sessions 3 times a week for 90 minutes | Nintendo Wii motion and Wii balance board | Nonimmersive | NRS pain, balance, sit-to-stand test, and profile of mood states |
| Mortensen et al [59] | Denmark | QE | 15 (15) | Adults with fibromyalgia | 15 sessions of 30 minutes | Motion-controlled video games, Wii, Ps3, and Xbox Kinect | Nonimmersive | Pain VAS, Brief Fatigue Inventory, Activities of Daily Life Questionnaire, test of playfulness, and interviews |
| Mouraux et al [76] | United States and Belgium | QE | 22 (12) | Adults with chronic neuropathic pain in unilateral upper extremity | 5 sessions of 20 minutes over 1 week | 3D augmented reality system with a 3D display (Kit Nvidia 3D Vision) and 3D camera (Xbox 360 Kinect) | Nonimmersive | Pain VAS, McGill Pain Questionnaire, and Douleur Neuropathique 4 Questions |
| Ortiz-Catalan et al [77] | Sweden and Slovenia | QE | 14 (ND) | Adults with chronic intractable phantom limb pain | Twice per week, 12 sessions of 2 hours each | Neuromotus and Integrum AB | Nonimmersive | NRS intensity, frequency, duration, and quality of phantom limb pain; Pain Rating Index Scale; Short form of McGill questionnaire; and interviews |
| Pamment and Aspell [51] | United Kingdom | QE | 18 (12) | Adults with chronic pain | 4 conditions, each lasting 2 minutes | HMD (WRAP 1200, Vuzix) connected to a video camera | Immersive | McGill Pain Questionnaire and illusion and control questions |
| Phoon Nguyen et al [83] | Australia | QE | 9 (7) | Adults with burning mouth syndrome | 1 session of 3 experimental conditions of 1 minute each | MIRAGE-mediated reality system; computer screen displaying live digitally manipulated video feed of their own face | Nonimmersive | Pain VAS, Wong-Baker Faces Pain Rating Scale, and VAS burning pain/sensation |
| Rezaei et al [69] | Iran | RCT | 44 (ND) | Adults with chronic neck pain | 8 training sessions over 4 weeks with 21 minutes each | Cervigame head mouse extreme | Nonimmersive | Pain VAS, Neck Disability Index, and Y-balance test |
| Rutledge et al [78] | United States | QE | 14 (1) | Adults with phantom limb pain | 57 treatment sessions with 40-60 minutes per session | VR treatment based on mirror therapy with an Oculus Rift Headset | Immersive | Phantom Limb Pain Questionnaire, Trinity Amputation and Prosthetic Experience Scale-Short Form-12, Patient Health Questionnaire-9, Posttraumatic Stress Disorder Checklist-Military version, and Present Questionnaire |
| Sarig-Bahat et al [70] | Australia | RCT | 32 (22) | Adults with chronic neck pain | 4-6 supervised intervention sessions for 30 minutes each over a period of 5 weeks+home training sessions of 30 minutes for at least three times a week | HMD with a Wrap 1200VR by Vuzix | Immersive | VAS pain, Neck Disability Index, Tampa Scale for Kinesiophobia, static and functional balance, satisfaction, global perceived effect, and range of motion |
| Sarig-Bahat et al [71] | Australia and Israel | RCT | 90 (63) | Adults with chronic neck pain | 5 minutes, 4 times a day, 4 days per week, for 4 weeks | Oculus Rift DK1 HMD with 3D motion tracking | Immersive | Neck disability Index, global perceived effect, VAS pain, self-rated health status in the European life quality questionnaire, velocity, Tampa scale for kinesiophobia |
| Sato et al [75] | Japan | CS | 5 (4) | Adults with complex regional pain syndrome | 5-8 weeks with 1 session each week | FASTRAK and cyberglove, PC desktop with a CyberGlove as hand input, FASTRAK as real-time position and motion tracker, and computer screen | Nonimmersive | VAS pain and range of motion |
| Shahrbanian et al [52] | Canada | QE | 12 (5) | Adult stroke patients with chronic pain | 1 moment with 3-5 minutes of each VR condition | HMD Kaiser Optical System with Nvidia Quadro FX 4500 graphics card | Immersive | Pain threshold, engagement, VAS mood, and NRS pain |
| Solca et al [84] | Switzerland | QE | 15 (5) | Adults with chronic leg pain with a spinal cord implant | 1 moment | Oculus Rift CV1 with RealiSM software | Immersive | Analgesia and embodiment |
| Tejera et al [72] | Spain | RCT | 44 (23) | Adults with nonspecific chronic neck pain | 2 sessions per week for 4 weeks | VR Vox Play glasses used with an HMD clamping system | Immersive | VAS pain, pain pressure threshold, temporal summation, range of motion, neck disability index, pain catastrophizing scale, Tampa scale for kinesiophobia, fear-avoidance beliefs questionnaire, and Pain Anxiety Symptoms Scale |
| Thomas et al [66] | United States | RCT | 53 (ND) | Adults with chronic low back pain | 3 consecutive days | Samsung 3D shutter glasses with Vizard software | Nonimmersive | Changes in lumbar spine flexion, VAS expectations of pain and harm, and game experience survey |
| Tong et al [79] | China | CS | 5 (0) | Adults with phantom limb pain | 10 sessions over 6 weeks | Immersive room-scale VR system and HMD from HTC Vive with Unity 3D | Immersive | Short Form McGill Pain Questionnaire, VAS pain, NRS embodiment, NRS ownership, and hospital anxiety and depression scale |
| Trujillo et al [67] | United States | CS | 2 (0) | Adults with chronic low back pain | 7 sessions with 2 sessions per week of 30-45 minutes each | Virtual embodiment training with Virtual Embodiment Training (KVET); HTC Vive with a VR HMD | Immersive | Simulator Sickness Questionnaire; VAS pain and Pain Catastrophizing Scale |
| Villafaina et al [60] | Spain | RCT | 55 (55) | Adults with fibromyalgia | 2 sessions of 1 hour per week for 24 weeks | VirtualEx-FM | Nonimmersive | Chair-stand test, 10-step stair test, 6-minute walk test, Fibromyalgia impact questionnaire, and International Physical Activity Questionnaire |
| Villafaina et al [61] | Spain | RCT | 55 (55) | Adults with fibromyalgia | 2 sessions of 1 hour per week for 24 weeks | VirtualEx-FM | Nonimmersive | Electroencephalography |
| Wiederhold et al [53] | United States | QE | 31 (ND) | Adults with chronic pain | 5-minute pain focus session followed by a 20-minute intervention session | Mobile phone VR therapy and an HMD | Immersive | Simple Descriptive Pain Intensity Scale, Numerical Pain Intensity Scale, VAS pain, and physiological measures (heart rate, peripheral skin temperature, respiration, and skin conductance) |
| Wiederhold et al [54] | Belgium and United States | QE | 40 (ND) | Adults with chronic pain | 15-minute exposure session | VR exposure while wearing HMD | Immersive | Pain reduction, pain focus, and skin temperature |
aVR: virtual reality.
bQE: quasi-experimental.
cNRS: Numeric Rating Scale.
dRCT: randomized controlled trial.
eEMMA: Engaging Media for Mental Health Applications.
fCS: case series.
gVAS: visual analog scale.
hND: not displayed.
iHMD: head-mounted display.
In terms of population, most studies (n=11) investigated adults with chronic pain without further specification of the specific type of chronic pain [44-54]. A total of 7 studies evaluated the effect of VR in patients with fibromyalgia [55-61], 6 studied patients with chronic low back pain [62-67], 5 studied patients with chronic neck pain [68-72], 4 studies evaluated VR in patients with (upper limb) complex regional pain syndrome [73-76], and 3 studied patients with phantom limb pain [77-79]. In addition, 1 study investigated pediatric patients with chronic pain [80], and 1 study investigated both adults and adolescents [73]. A total of 1232 patients were enrolled in 41 studies, of which 784 (63.64%) were women.
With regard to the VR application, the duration of the sessions ranged from 2×2 minutes with 30 seconds rest between sessions [64] up to sessions of 1 hour [60]. The frequency varied from 1 session [64] to 2 sessions per week for 24 weeks [60].
Risk of Bias
The range of the total scores on the Downs and Black checklist varied between 8 out of 28 and 25 out of 28. Overall, 5 (12%) of the 41 included studies scored poor on the risk of bias assessment (total score ≤14), 17 (42%) had a fair score (total score between 15 and 19), and 19 (46%) had good quality (total score between 20 and 25). The total scores on the risk of bias assessment are presented in Table 2. Multimedia Appendix 2 presents the full results of the risk of bias assessment.
Table 2.
Total score on the risk of bias assessment.
| Studya | Total score (out of 28) | Category |
| Alemanno et al [62] | 22 | Good |
| Amin et al [44] | 19 | Fair |
| Botella et al [55] | 16 | Fair |
| Brown et al [63] | 24 | Good |
| Chau et al [73] | 16 | Fair |
| Collado-Mateo et al [56] | 24 | Good |
| Darnall et al [81] | 25 | Good |
| Fowler et al [45] | 21 | Good |
| Garcia-Palacios et al [57] | 23 | Good |
| Garrett et al [46] | 18 | Fair |
| Griffin et al [80] | 20 | Good |
| Gromala et al [47] | 18 | Fair |
| Guarino et al [48] | 10 | Poor |
| Harvie et al [68] | 20 | Good |
| Herrero et al [58] | 18 | Fair |
| House et al [82] | 19 | Fair |
| Jin et al [49] | 18 | Fair |
| Jones et al [50] | 16 | Fair |
| Matamala-Gomez et al [74] | 19 | Fair |
| Matheve et al [64] | 24 | Good |
| Monteiro et al [65] | 21 | Good |
| Mortensen et al [59] | 18 | Fair |
| Mouraux et al [76] | 14 | Poor |
| Ortiz-Catalan et al [77] | 18 | Fair |
| Pamment and Aspell [51] | 20 | Good |
| Phoon Nguyen et al [83] | 21 | Good |
| Rezaei et al [69] | 25 | Good |
| Rutledge et al [78] | 18 | Fair |
| Sarig-Bahat et al [70] | 23 | Good |
| Sarig-Bahat et al [71] | 21 | Good |
| Sato et al [75] | 12 | Poor |
| Shahrbanian et al [52] | 17 | Fair |
| Solca et al [84] | 19 | Fair |
| Tejera et al [72] | 23 | Good |
| Thomas et al [66] | 25 | Good |
| Tong et al [79] | 16 | Fair |
| Trujillo et al [67] | 17 | Fair |
| Villafaina et al [60] | 23 | Good |
| Villafaina et al [61] | 22 | Good |
| Wiederhold et al [53] | 11 | Poor |
| Wiederhold et al [54] | 8 | Poor |
aEach study was scored on all 27 items of the modified Downs and Black checklist. On the basis of the total score, all included studies were categorized as presenting poor, fair, good, or excellent quality. A total score of ≤14 out of 28 was considered poor quality, 15-19 was considered fair, 20-25 was considered good, and 26-28 was considered excellent methodological quality.
In the 18 studies with a quasi-experimental design, low scores were found for the external validity subscale. Only 6 (33%) of the 18 studies had an accurate score on the item of whether patients were representative of the entire population from which they were recruited, and the item concerning representativeness of staff, places, and facilities where the patients were treated was only considered representative of the treatment most patients received in 7 (39%) of 18 studies. Several items that evaluated internal validity performed poorly, including the attempt to blind study participants, which was only evaluated efficiently in 1 (6%) of the 18 studies. No study has attempted to blind outcome assessors. Recruiting patients over the same period was only scored satisfactory in 3 (17%) studies, no studies randomized patients, and adjustments for confounding were only performed in 6 (33%) of 18 studies.
In the 16 randomized controlled trials, several items evaluating internal validity received low scores. Of the 16 studies, only 1 (6%) study provided information on attempts to blind study participants, whereas 5 (31%) studies provided information on attempts to blind outcome assessors. Information regarding adjustments for confounding was provided in only 7 (44%) studies.
A total of 7 case series were included; only 2 (29%) studies reported the estimates of random variability. For the 3 items evaluating external validity, most studies performed poorly with representativeness ranging from 14% (1/7) to 43% (3/7). Of the 7 studies, on the subscale for internal validity (bias), only 1 (14%) study attempted to blind the study participants, and none attempted to blind the outcome assessor. Patients were not recruited in the same period within a study, and only 1 (14%) of 7 studies used randomization (no concealed randomization). Adjustments for confounding were explored in 2 (29%) studies, and a power calculation was reported in 3 (43%) of the 7 studies.
Interventions
A total of 23 studies used immersive VR techniques, and 18 used non-immersive techniques. Within the category of immersive techniques, VR games (7/23, 30%), mindfulness-based interventions (6/23, 28%), practical exercises (6/23, 28%), and visual illusions (4/23, 17%) were used. In the category of nonimmersive techniques, of the 18 studies, 6 (33%) used exergames, 3 (17%) used an avatar or exoskeleton, and 9 (50%) studies used a television or PC screen. A more detailed description of immersive techniques is provided in further sections, followed by an in-depth explanation of nonimmersive VR techniques.
When VR was applied as a game, a broad range of VR games were used, including shooter games [44], a game of grasping where participants had to stomp fruit [80], a game with sliding in an icy cave during which participants should hit creatures with snowballs [49], a game in which the user travels through a landscape with interaction [50], a game with a visualization of a red airplane that could be controlled by head motion and the user could hit targets [70,71], and a game of pushing a ball of the table and shooting a basketball [79].
When VR was used in the context of mindfulness-based or relaxation treatments, several applications were used, including a 5-minute relaxation video [63], sessions to support patients in learning self-management skills based on cognitive behavior therapy principles in which the VR headset was used for visual biofeedback in relaxation training [81], exploratory environments [46,47], interaction with simulation graphics and exploration of virtual worlds [53], and relaxing environments and sounds [54].
In addition, immersive VR was also used to practice exercises in a kitchen environment in which participants had to perform tasks representative of daily activities [73]. In addition, minimal exercises such as neck and head movements and larger exercises such as torso and upper extremity movements were provided [45,68]. Participants could bicycle on a pedaller through VR environments [78], practice neck exercises through the illusion of diving with sounds of the sea [72], and perform exercises based on the principles of graded motor imagery to relearn associations to pain and improve their function [67].
Finally, other possibilities of immersive VR were seeing an illusion of the affected body part through an avatar [74], a visualization of their own back and synchronously or asynchronously tapping with a wooden stick [51], experiencing hot and cold stimuli through a snow world environment and a canyon environment, respectively [52], and a visual illumination of a circumscribed skin region in the VR corresponding with Spinal Cord Stimulation [84].
In contrast to immersive applications, several studies have used nonimmersive VR techniques. The studies (n=6) that made use of exergames consisted of a variety of exercises, such as aerobic sessions; postural control and coordination; exercises to improve mobility skills, fitness, ability, and balance [56,60,61]; Wii Fit Plus workouts [65]; a sports game package [59]; and an exercise in which a real-time 3D image of the individual’s moving, nonaffected body part was presented, and participants played a game to touch a few targets with the hand or fingers of the virtual affected upper extremity [76].
An avatar or exoskeleton was used in 3 studies as virtual rehabilitation and could help to teach patients to execute correct movements with the painful body parts to regain a correct body image [62] or with games for unimanual and bimanual motor, emotive, and cognitive training [82] or with pelvic tilt exercises where the VR was used as a game [64].
A television or PC screen was used in the following situations (n=9): support of a group cognitive behavior therapy containing specific content for developing relaxation and mindfulness skills, as an adjunct to the activity pacing component, with education, activity management, and relapse prevention, to induce positive emotions and promote motivation, self-efficacy, and behavior activation [48,55,57,58]. Other authors used a television or PC screen to practice motor execution by games, such as racing cars using phantom movements and matched random target postures of a virtual arm [66,77], a rabbit attempting to reach carrots and avoid obstacles [69], or a target-oriented motor control task where hand exercises consisted of reaching out, grasping, transferring, and placing [75]. In another study, patients with burning mouth syndrome watched their tongues on a computer screen with illusions and performed tongue movements [83].
Instruments of Outcome Measurements
Multimedia Appendix 3 provides a complete summary of the measurement instruments used to evaluate these outcomes. Of the 41 included studies, 35 (85%) evaluated pain-related outcomes [44-54,57-59,62-73,75-81,83,84]. Psychological outcomes, such as kinesiophobia and fear, mood, satisfaction, expectations of pain, pain focus, time spent thinking about pain, self-efficacy, emotions, motivation, stress, catastrophizing, acceptability, global impression of change, ownership, and agency, were measured in 19 studies [45,48,52,55-59,62-65,67,70-72,74,81,82]. Functional outcomes, including disability, physical comfort, strength, fitness, and sleep, were measured in 15 studies [45,55-57,59,60,62,64,65,69-72,77,82]. Functional capacity (evaluated by measuring balance, repetition index, step test, and composite value) was measured in 5 studies [56,62,65,69,70]. Mobility (range of motion) was measured in 4 studies [45,62,71,72]. Neuropsychological functions were measured in 2 studies [61,82] using resting brain dynamics with electroencephalography, Brief Visuospatial Memory Test-Revised, Neurophysiological Assessment Battery, Revised Hopkins Verbal Learning Test, Trail Making Test, and other neuropsychological evaluations. Quality of life was measured in 3 studies [57,62,71]. Other sensations were measured in 5 studies [52,54,68,72,78]. The experience of VR technology, such as presence, simulator sickness, physical comfort, feasibility, safety, effort put in the game, and satisfaction, was measured in 18 of the included studies [45,46,50-52,55,57,59,63,66,67,70,74,78-81,84] using the VR Satisfaction Scale, VR Symptom Questionnaire, satisfaction with treatment (numeric rating scale), motion and nausea (numeric rating scale), test of playfulness, illusion and control questions, questionnaire of embodiment, and a game experience survey.
Meta-analysis of Outcome Measurements
In most (21/25, 84%) studies, more than one outcome measurement was used to evaluate the effect of VR in patients with chronic pain, resulting in 194 effect sizes from 25 studies. Figure 2 [45,49,52,55-60,62-65,69-73,75-79,82,84] presents the summary forest plots, where each line represents all the outcomes from a particular study. If 0 was included in the CI, the reported effect size was not statistically significant at the 5% level. The overall effect size based on the 3‐level meta‐analysis was estimated at 1.22, with an SE of 0.34 and a 95% CI of 0.55-1.89 (z=3.56; P<.001). This indicates that VR intervention in patients with chronic pain had a positive effect on the outcome measurements used. Caterpillar plots are visualized in Figure 3 to provide a general view of the distribution of all effect sizes (Figure 3A) and study effect sizes (Figure 3B). Funnel plots are scatter plots in which effect sizes are plotted against the SE with small SEs at the top of the graph. Funnel plots for this meta-analysis are displayed in Figure 4, demonstrating an asymmetrical plot, which might be interpreted as an indication of publication bias.
Figure 2.
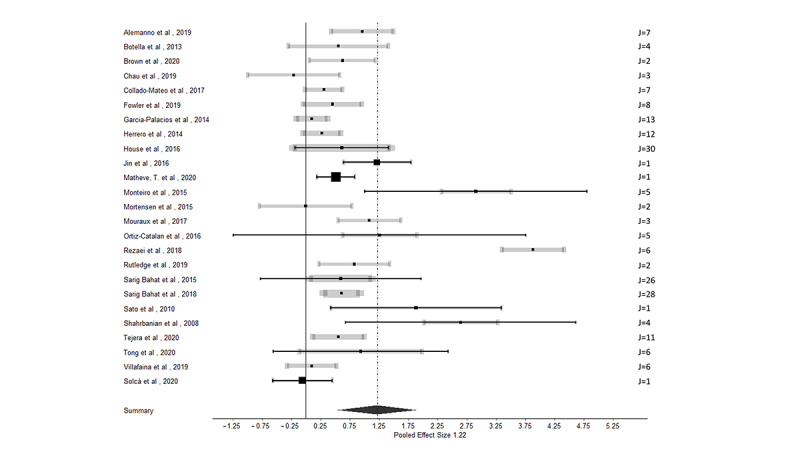
Summary forest plot for the effect of virtual reality on all outcome measurements in patients with chronic pain. Each line presents the results of 1 study (potentially including multiple effect sizes). The meta-analytic mean, with the corresponding 95% CI, is presented with a black dot and black line. This black 95% CI represents the total study precision. The additional CI in gray is based on the sampling variance of individual observed effect sizes of the study to obtain a visual contribution of the study sample size on the total study precision. The thickness of the gray CI is proportional to the number of effect sizes within studies. The number of effect sizes per study is presented as "J" on the right side of the figure [45,49,52,55-60,62-65,69-73,75-79,82,83].
Figure 3.
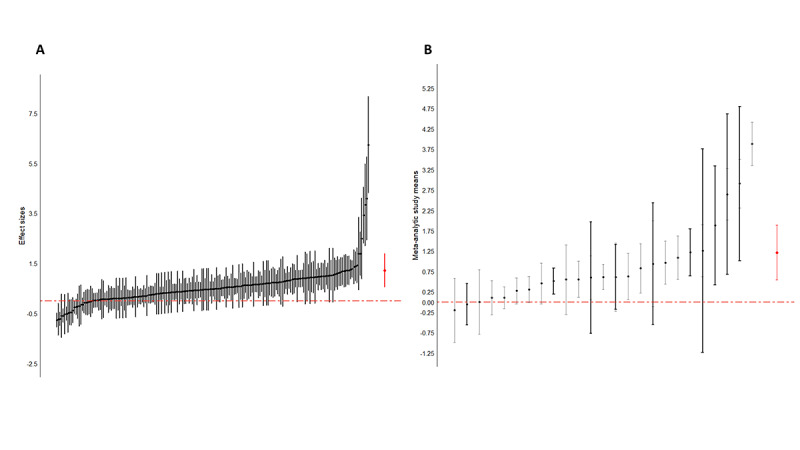
Caterpillar plots with all effect sizes (A) and study effect sizes (B). The overall effect size is presented in red.
Figure 4.

A funnel plot of all effect sizes (A) and a study funnel plot (B).
The type of VR intervention (binary factor: immersive vs nonimmersive) was included as an additional covariate in the analysis; however, the type of VR intervention was not statistically significant (F1,192=0.88; P=.35). Given these results, it can be concluded that the overall effect of VR on several outcome measurements is not moderated by the type of VR intervention. In addition, the type of pain (primary or secondary) and the objective of VR (exercise, virtual illusion, distraction, or cognitive therapy) were added as potential moderators to the analyses, whereby the omnibus test for the moderator analysis was not statistically significant for the type of pain (F1,180=0.03; P=.86), nor for the objective of VR (F1,190=0.59; P=.62).
When specifically focusing on effect sizes that measure the effect of VR on pain (n=31), an overall effect size of 1.60 (SE 0.39, 95% CI 0.83-2.36) was revealed, favoring VR interventions to decrease pain (z=4.09; P<.001; Figure 5A). For functioning (n=60), an effect size of 1.40 (SE 0.65, 95% CI 0.13-2.67) was calculated (z=2.17; P=.03; Figure 5B). For mobility (n=24; Figure 5C) and functional capacity (n=21; Figure 5D), effect sizes of 0.49 (SE 0.61, 95% CI −0.71 to 1.68; z=0.80, P=.42) and 0.34 (SE 0.95, 95% CI −1.52 to 2.20; z=0.36; P=.72) were revealed, respectively.
Figure 5.

Reported effect sizes from the studies exploring (A) pain, (B) functioning, (C) mobility, and (D) functional capacity. Significant effects were found for pain and functioning outcome variables. Effect sizes from individual studies are presented in black, and the overall effect size is shown in red.
Discussion
Principal Findings
The main aim of this systematic review was to systematically identify all outcome parameters that are reported in relation to VR in the context of chronic pain management. This review revealed a broad range of outcome variables that are influenced by an intervention of VR technology, with statistically significant results on pain relief and improvements in functioning. These findings indicate that VR not only has applications in acute pain management but also in chronic pain. Over the last decade, medicine has shifted toward the use of innovative tools such as VR. The use of VR technology has expanded from the entertainment industry to clinical medicine and has proven to be cost-effective and efficient [14]. The effects of VR technology have been explored in different settings in medicine, ranging from surgical education to pain management [14]. The use of VR technology in surgical training has become an essential prerequisite for junior physicians before they can actively participate in real surgical operations [85]. Compared with VR technology, trainees who have received conventional surgical training have been found to perform surgery substantially slower and are more likely to cause injury, damage tissue, or fail to progress with surgery [86].
Comparison With Existing Literature
The management of pain in acute care settings often relies on pharmacological treatments to decrease pathophysiological responses [87]. However, the emergence of VR technology has brought another path for the management of acute pain and has been investigated for the management of burn-induced injuries [14]. As a result, VR technology provides analgesia with minimal side effects [88] and minimal impact on the physical hospital environment [88]. Another approach to the use of VR technology is to augment hypnosis, where patients report lower levels of pain and anxiety [89,90]. In addition to the use of morphine for pain reduction, VR for relaxation has shown to be very effective [91]. In addition, in chronic pain management, the applications of VR technology are very broad, including distraction, cognitive therapy, exercise, and enabling virtual limb movements [32].
Within the field of VR, one of the major classifications is based on the applied materials to induce a virtual experience. Both studies with 3D settings with a computer-generated simulation of 3D environment that makes use of a head-mounted display to entirely replace the real world and computer-generated simulations of 2D environment viewed on a computer or a wall-mounted screen were included [32]. A systematic review concluded that immersive VR technology is more likely to generate pain than nonimmersive (2D) VR technology [30]. As the price of immersive VR equipment continues to decrease, this approach is becoming very affordable and could potentially become a self-management tool for pain relief used by patients in ambulatory and home settings [14]. In this meta-analysis, the type of VR (immersive vs nonimmersive) was not a statistically significant confounder, indicating that VR in general has a beneficial effect on the reported outcome measurements. Further studies are required to confirm these results in chronic pain settings.
Patients affected by chronic pain aim to increase participation in daily living, ranging from work duties and family commitments to social activities and leisure time [92]. Therefore, a complete view of the patient’s functioning and health-related quality of life is needed rather than exclusively assessing the degree of pain relief [93]. A possible framework for organizing and documenting information on functioning and disability is the International Classification of Functioning, Disability, and Health (ICF), which is a classification of health and health-related outcomes [94]. The model conceptualizes functioning as a dynamic interaction between a person’s health condition, personal factors, and environmental factors, as the functioning and disability of an individual occur in this context [95]. Therefore, the ICF provides a multi-perspective, biopsychosocial approach, which is reflected in the multidimensional model [95]. Multiple factors of the ICF model have been found in the reported outcome measurements of this systematic review, whereby mainly bodily functions and structures (eg, pain intensity and sleep), functional disability (eg, walking and balance control), and psychological distress (eg, depression, anxiety, and catastrophizing) were represented. The meta-analyses revealed a statistically significant positive effect of VR on pain-related (95% CI 0.83-2.36; z=4.09; P<.001) and functioning-related (95% CI 0.13-2.67; z=2.17; P=.03) outcome measurements. These results are in line with the decrease in pain intensity and disability by VR compared with proprioceptive training and lumbar stabilization exercises in patients with chronic neck pain and chronic low back pain, respectively, as observed in a recent meta-analysis [96]. No statistically significant results were found for functional capacity and mobility, whereby a number of effect sizes were indicative of no effect of VR on these outcome measurements. However, this finding does not exclude the potential added value of VR with another rehabilitation strategy to work on these concepts. Recently, it was suggested that manual therapy in combination with VR could define an entire mind-body intervention that relies on psychological, interoceptive, and exteroceptive stimulations for rebalancing sensorimotor integration and distorted perceptions, including visual and body images [97], denoting the complementary action of several conservative treatments.
Strengths and Limitations
The main strength of this literature review was the addition of a 3-level meta-analysis to consider the dependency between effect sizes. In the case of dependency, effect sizes are correlated, which inevitably leads to inflation of information and overconfidence in the results of a standard meta-analysis [42]. To avoid this inflation, several approaches have been used, among which the selection of only one effect size per study, relying on an average effect size for dependent effect sizes, or dependency could simply be ignored, and the analysis was performed as if the effect sizes were independent [98]. As the aim of this review was to evaluate the effect of VR on all outcome measurements in relation to chronic pain, the authors did not find the stated methods well suited, wherefore a multilevel approach was found to be the most appropriate. Furthermore, this systematic review has certain strengths that secure a minimal risk of potential bias: double-blind screening of the literature, including consensus meetings when needed, and consultation with several databases with the aim of fully representing the existing literature.
Certain limitations should be taken into account as well when interpreting the results of this study. None of the included studies qualified for excellent methodological quality. Of the 41 studies, most of the studies were scored as good on the risk of bias assessment (n=19, 46%), 17 (41%) scored as fair, and only 5 (12%) studies scored as poor. In many of the included studies, the authors mainly focused on the primary outcome variables; in this systematic review, all outcome variables were taken into account (primary and secondary outcome measurements); hence, the results were not always described in full detail for secondary outcomes. Finally, much heterogeneity is present in studies with VR, especially in terms of study design, underlying chronic pain etiologies, VR materials, and VR applications.
Conclusions
This systematic review explored the outcome measurements that are influenced by VR in patients with chronic pain. A broad range of outcome variables was revealed, whereby an intervention using VR technology can induce pain relief and improvements in functioning. These findings indicate that VR not only has applications in acute pain management but also in chronic pain settings, whereby VR technology might be able to become a promising first-line intervention as a complementary therapy for patients with chronic pain.
Abbreviations
- ICF
International Classification of Functioning, Disability, and Health
- PICO
Patient or Population, Intervention, Comparison, and Outcome
- PRISMA
Preferred Reporting Items for Systematic Reviews and Meta-Analyses
- VR
virtual reality
The full search strategy for PubMed.
Risk of bias table based on the modified version of the Downs and Black Checklist.
Overview of the effects of virtual reality on several outcome measurements for each study.
Footnotes
Conflicts of Interest: MM received speaker fees from Medtronic Nevro, and Saluda outside of the submitted work. LG is a postdoctoral research fellow funded by the Research Foundation Flanders, Belgium (project number: 12ZF622N). STIMULUS (Research and Teaching Neuromodulation Universitair Ziekenhuis Brussel/Vrije Universiteit Brussel) has received research grants from Medtronic.
References
- 1.Nicholas M, Vlaeyen JW, Rief W, Barke A, Aziz Q, Benoliel R, Cohen M, Evers S, Giamberardino MA, Goebel A, Korwisi B, Perrot S, Svensson P, Wang SJ, Treede RD, IASP Taskforce for the Classification of Chronic Pain The IASP classification of chronic pain for ICD-11: chronic primary pain. Pain. 2019 Jan;160(1):28–37. doi: 10.1097/j.pain.0000000000001390.00006396-201901000-00004 [DOI] [PubMed] [Google Scholar]
- 2.Breivik H, Collett B, Ventafridda V, Cohen R, Gallacher D. Survey of chronic pain in Europe: prevalence, impact on daily life, and treatment. Eur J Pain. 2006 May;10(4):287–333. doi: 10.1016/j.ejpain.2005.06.009.S1090-3801(05)00086-8 [DOI] [PubMed] [Google Scholar]
- 3.Suso-Ribera C, Yakobov E, Carriere JS, García-Palacios A. The impact of chronic pain on patients and spouses: consequences on occupational status, distribution of household chores and care-giving burden. Eur J Pain. 2020 Oct;24(9):1730–40. doi: 10.1002/ejp.1616. [DOI] [PubMed] [Google Scholar]
- 4.Naiditch N, Billot M, Moens M, Goudman L, Cornet P, Le Breton D, Roulaud M, Ounajim A, Page P, Lorgeoux B, Nivole K, Pries P, Swennen C, Teyssedou S, Charrier E, de Montgazon GB, Descoins PF, Roy-Moreau B, Grimaud N, David R, Vendeuvre T, Rigoard P. Persistent spinal pain syndrome type 2 (PSPS-T2), a social pain? Advocacy for a social gradient of health approach to chronic pain. J Clin Med. 2021 Jun 25;10(13):2817. doi: 10.3390/jcm10132817. https://www.mdpi.com/resolver?pii=jcm10132817 .jcm10132817 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 5.Wippert PM, Drießlein D, Beck H, Schneider C, Puschmann AK, Banzer W, Schiltenwolf M. The feasibility and effectiveness of a new practical multidisciplinary treatment for low-back pain: a randomized controlled trial. J Clin Med. 2019 Dec 31;9(1):115. doi: 10.3390/jcm9010115. https://www.mdpi.com/resolver?pii=jcm9010115 .jcm9010115 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 6.Gatchel RJ, Okifuji A. Evidence-based scientific data documenting the treatment and cost-effectiveness of comprehensive pain programs for chronic nonmalignant pain. J Pain. 2006 Nov;7(11):779–93. doi: 10.1016/j.jpain.2006.08.005.S1526-5900(06)01024-8 [DOI] [PubMed] [Google Scholar]
- 7.Elbers S, Wittink H, Pool JJ, Smeets RJ. The effectiveness of generic self-management interventions for patients with chronic musculoskeletal pain on physical function, self-efficacy, pain intensity and physical activity: a systematic review and meta-analysis. Eur J Pain. 2018 Oct;22(9):1577–96. doi: 10.1002/ejp.1253. http://europepmc.org/abstract/MED/29845678 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 8.Damush TM, Kroenke K, Bair MJ, Wu J, Tu W, Krebs EE, Poleshuck E. Pain self-management training increases self-efficacy, self-management behaviours and pain and depression outcomes. Eur J Pain. 2016 Aug;20(7):1070–8. doi: 10.1002/ejp.830. [DOI] [PubMed] [Google Scholar]
- 9.Billot M, Daycard M, Rigoard P. Self-Reiki, consideration of a potential option for managing chronic pain during pandemic COVID-19 period. Medicina (Kaunas) 2021 Aug 25;57(9):867. doi: 10.3390/medicina57090867. https://www.mdpi.com/resolver?pii=medicina57090867 .medicina57090867 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 10.Du S, Hu L, Dong J, Xu G, Chen X, Jin S, Zhang H, Yin H. Self-management program for chronic low back pain: a systematic review and meta-analysis. Patient Educ Couns. 2017 Jan;100(1):37–49. doi: 10.1016/j.pec.2016.07.029.S0738-3991(16)30324-X [DOI] [PubMed] [Google Scholar]
- 11.Teater D. The psychological and physical side effects of pain medication. National Safety Council. 2015. [2021-10-10]. https://www.nsc.org/getmedia/0113f259-d2c5-4a3e-abca-f05299f65ec2/adv-rx-side-effects-wp.pdf .
- 12.Cheatle MD. Prescription opioid misuse, abuse, morbidity, and mortality: balancing effective pain management and safety. Pain Med. 2015 Oct;16 Suppl 1:S3–8. doi: 10.1111/pme.12904. [DOI] [PubMed] [Google Scholar]
- 13.Gupta A, Scott K, Dukewich M. Innovative technology using virtual reality in the treatment of pain: does it reduce pain via distraction, or is there more to it? Pain Med. 2018 Jan 01;19(1):151–9. doi: 10.1093/pm/pnx109.4100671 [DOI] [PubMed] [Google Scholar]
- 14.Li L, Yu F, Shi D, Shi J, Tian Z, Yang J, Wang X, Jiang Q. Application of virtual reality technology in clinical medicine. Am J Transl Res. 2017 Sep 15;9(9):3867–80. http://europepmc.org/abstract/MED/28979666 . [PMC free article] [PubMed] [Google Scholar]
- 15.Chuan A, Zhou JJ, Hou RM, Stevens CJ, Bogdanovych A. Virtual reality for acute and chronic pain management in adult patients: a narrative review. Anaesthesia. 2021 May;76(5):695–704. doi: 10.1111/anae.15202. [DOI] [PubMed] [Google Scholar]
- 16.Keefe FJ, Huling DA, Coggins MJ, Keefe DF, Rosenthal ZM, Herr NR, Hoffman HG. Virtual reality for persistent pain: a new direction for behavioral pain management. Pain. 2012 Nov;153(11):2163–6. doi: 10.1016/j.pain.2012.05.030. http://europepmc.org/abstract/MED/22770840 .00006396-201211000-00005 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 17.Trost Z, Zielke M, Guck A, Nowlin L, Zakhidov D, France CR, Keefe F. The promise and challenge of virtual gaming technologies for chronic pain: the case of graded exposure for low back pain. Pain Manag. 2015;5(3):197–206. doi: 10.2217/pmt.15.6. [DOI] [PubMed] [Google Scholar]
- 18.Kober SE, Kurzmann J, Neuper C. Cortical correlate of spatial presence in 2D and 3D interactive virtual reality: an EEG study. Int J Psychophysiol. 2012 Mar;83(3):365–74. doi: 10.1016/j.ijpsycho.2011.12.003.S0167-8760(11)00382-5 [DOI] [PubMed] [Google Scholar]
- 19.Ventura S, Brivio E, Riva G, Baños RM. Immersive versus non-immersive experience: exploring the feasibility of memory assessment through 360° technology. Front Psychol. 2019 Nov 14;10:2509. doi: 10.3389/fpsyg.2019.02509. doi: 10.3389/fpsyg.2019.02509. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 20.Repetto C, Germagnoli S, Triberti S, Riva G. Learning into the wild: a protocol for the use of 360° video for foreign language learning. In: Cipresso P, Serino S, Ostrovsky Y, Baker JT, editors. Pervasive Computing Paradigms for Mental Health. Cham, Switzerland: Springer; 2018. pp. 56–63. [Google Scholar]
- 21.Abiodun AO, Adesina MA. Virtual reality: a breakthrough in pain management? World News Nat Sci. 2019;23:24–33. [Google Scholar]
- 22.Wismeijer AA, Vingerhoets AJ. The use of virtual reality and audiovisual eyeglass systems as adjunct analgesic techniques: a review of the literature. Ann Behav Med. 2005 Dec;30(3):268–78. doi: 10.1207/s15324796abm3003_11. [DOI] [PubMed] [Google Scholar]
- 23.Hoffman HG, Patterson DR, Carrougher GJ, Nakamura D, Moore M, Garcia-Palacios A, Furness III TA. The effectiveness of virtual reality pain control with multiple treatments of longer durations: a case study. Int J Hum Comput Interact. 2001 Mar 21;13(1):1–12. doi: 10.1207/S15327590ijhc1301_1. [DOI] [Google Scholar]
- 24.Rutter CE, Dahlquist LM, Weiss KE. Sustained efficacy of virtual reality distraction. J Pain. 2009 Apr;10(4):391–7. doi: 10.1016/j.jpain.2008.09.016. http://europepmc.org/abstract/MED/19231295 .S1526-5900(08)00800-6 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 25.Johnson MH. How does distraction work in the management of pain? Curr Pain Headache Rep. 2005 Apr;9(2):90–5. doi: 10.1007/s11916-005-0044-1. [DOI] [PubMed] [Google Scholar]
- 26.Mahrer NE, Gold JI. The use of virtual reality for pain control: a review. Curr Pain Headache Rep. 2009 Apr;13(2):100–9. doi: 10.1007/s11916-009-0019-8. [DOI] [PubMed] [Google Scholar]
- 27.Cheung KL, Tunik E, Adamovich SV, Boyd LA. Neuroplasticity and virtual reality. In: Weiss PL, Keshner EA, Levin MF, editors. Virtual Reality for Physical and Motor Rehabilitation. New York, NY, USA: Springer; 2014. pp. 5–24. [Google Scholar]
- 28.Garrett B, Taverner T, Masinde W, Gromala D, Shaw C, Negraeff M. A rapid evidence assessment of immersive virtual reality as an adjunct therapy in acute pain management in clinical practice. Clin J Pain. 2014 Dec;30(12):1089–98. doi: 10.1097/AJP.0000000000000064. [DOI] [PubMed] [Google Scholar]
- 29.Shahrbanian S, Ma X, Korner-Bitensky N, Simmonds MJ. Scientific evidence for the effectiveness of virtual reality for pain reduction in adults with acute or chronic pain. Stud Health Technol Inform. 2009;144:40–3. [PubMed] [Google Scholar]
- 30.Malloy KM, Milling LS. The effectiveness of virtual reality distraction for pain reduction: a systematic review. Clin Psychol Rev. 2010 Dec;30(8):1011–8. doi: 10.1016/j.cpr.2010.07.001.S0272-7358(10)00109-1 [DOI] [PubMed] [Google Scholar]
- 31.Chan E, Foster S, Sambell R, Leong P. Clinical efficacy of virtual reality for acute procedural pain management: a systematic review and meta-analysis. PLoS One. 2018 Jul 27;13(7):e0200987. doi: 10.1371/journal.pone.0200987. https://dx.plos.org/10.1371/journal.pone.0200987 .PONE-D-18-00506 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 32.Austin PD. The analgesic effects of virtual reality for people with chronic pain: a scoping review. Pain Med. 2022 Jan 03;23(1):105–21. doi: 10.1093/pm/pnab217.6321464 [DOI] [PubMed] [Google Scholar]
- 33.Page MJ, McKenzie JE, Bossuyt PM, Boutron I, Hoffmann TC, Mulrow CD, Shamseer L, Tetzlaff JM, Akl EA, Brennan SE, Chou R, Glanville J, Grimshaw JM, Hróbjartsson A, Lalu MM, Li T, Loder EW, Mayo-Wilson E, McDonald S, McGuinness LA, Stewart LA, Thomas J, Tricco AC, Welch VA, Whiting P, Moher D. The PRISMA 2020 statement: an updated guideline for reporting systematic reviews. Int J Surg. 2021 Apr;88:105906. doi: 10.1016/j.ijsu.2021.105906.S1743-9191(21)00040-6 [DOI] [PubMed] [Google Scholar]
- 34.O'Sullivan D, Wilk S, Michalowski W, Farion K. Using PICO to align medical evidence with MDs decision making models. Stud Health Technol Inform. 2013;192:1057. [PubMed] [Google Scholar]
- 35.Treede RD, Rief W, Barke A, Aziz Q, Bennett MI, Benoliel R, Cohen M, Evers S, Finnerup NB, First MB, Giamberardino MA, Kaasa S, Kosek E, Lavand'homme P, Nicholas M, Perrot S, Scholz J, Schug S, Smith BH, Svensson P, Vlaeyen JW, Wang SJ. A classification of chronic pain for ICD-11. Pain. 2015 Jun;156(6):1003–7. doi: 10.1097/j.pain.0000000000000160. http://europepmc.org/abstract/MED/25844555 .00006396-201506000-00006 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 36.Ouzzani M, Hammady H, Fedorowicz Z, Elmagarmid A. Rayyan-a web and mobile app for systematic reviews. Syst Rev. 2016 Dec 05;5(1):210. doi: 10.1186/s13643-016-0384-4. https://systematicreviewsjournal.biomedcentral.com/articles/10.1186/s13643-016-0384-4 .10.1186/s13643-016-0384-4 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 37.Downs SH, Black N. The feasibility of creating a checklist for the assessment of the methodological quality both of randomised and non-randomised studies of health care interventions. J Epidemiol Community Health. 1998 Jun;52(6):377–84. doi: 10.1136/jech.52.6.377. https://jech.bmj.com/lookup/pmidlookup?view=long&pmid=9764259 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 38.Trac MH, McArthur E, Jandoc R, Dixon SN, Nash DM, Hackam DG, Garg AX. Macrolide antibiotics and the risk of ventricular arrhythmia in older adults. CMAJ. 2016 Apr 19;188(7):E120–9. doi: 10.1503/cmaj.150901. http://www.cmaj.ca/cgi/pmidlookup?view=long&pmid=26903359 .cmaj.150901 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 39.Korakakis V, Whiteley R, Tzavara A, Malliaropoulos N. The effectiveness of extracorporeal shockwave therapy in common lower limb conditions: a systematic review including quantification of patient-rated pain reduction. Br J Sports Med. 2018 Mar;52(6):387–407. doi: 10.1136/bjsports-2016-097347.bjsports-2016-097347 [DOI] [PubMed] [Google Scholar]
- 40.Hooper P, Jutai JW, Strong G, Russell-Minda E. Age-related macular degeneration and low-vision rehabilitation: a systematic review. Can J Ophthalmol. 2008 Apr;43(2):180–7. doi: 10.3129/i08-001.S0008-4182(08)80140-8 [DOI] [PubMed] [Google Scholar]
- 41.Becker BJ. Synthesizing standardized mean-change measures. Br J Math Stat Psychol. 1988 Nov;41(2):257–78. doi: 10.1111/j.2044-8317.1988.tb00901.x. [DOI] [Google Scholar]
- 42.Van den Noortgate W, López-López JA, Marín-Martínez F, Sánchez-Meca J. Three-level meta-analysis of dependent effect sizes. Behav Res Methods. 2013 Jun;45(2):576–94. doi: 10.3758/s13428-012-0261-6. [DOI] [PubMed] [Google Scholar]
- 43.Fernández-Castilla B, Declercq L, Jamshidi L, Beretvas SN, Onghena P, Van den Noortgate W. Visual representations of meta-analyses of multiple outcomes: extensions to forest plots, funnel plots, and caterpillar plots. Methodology. 2020 Dec 22;16(4):299–315. doi: 10.5964/meth.4013. [DOI] [Google Scholar]
- 44.Amin AM, Tong X, Gromala D, Shaw CD. Cardboard mobile virtual reality as an approach for pain distraction in clinical settings: comparison, exploration and evaluation with oculus rift. Proceedings of the 2017 CHI Conference Extended Abstracts on Human Factors in Computing Systems; CHI EA '17; May 6-11, 2017; Denver, CO, USA. 2017. pp. 2345–51. [DOI] [Google Scholar]
- 45.Fowler CA, Ballistrea LM, Mazzone KE, Martin AM, Kaplan H, Kip KE, Ralston K, Murphy JL, Winkler SL. Virtual reality as a therapy adjunct for fear of movement in veterans with chronic pain: single-arm feasibility study. JMIR Form Res. 2019 Oct 30;3(4):e11266. doi: 10.2196/11266. https://formative.jmir.org/2019/4/e11266/ v3i4e11266 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 46.Garrett B, Taverner T, McDade P. Virtual reality as an adjunct home therapy in chronic pain management: an exploratory study. JMIR Med Inform. 2017 May 11;5(2):e11. doi: 10.2196/medinform.7271. https://medinform.jmir.org/2017/2/e11/ v5i2e11 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 47.Gromala D, Tong X, Choo A, Karamnejad M, Shaw CD. The virtual meditative walk: virtual reality therapy for chronic pain management. Proceedings of the 33rd Annual ACM Conference on Human Factors in Computing Systems; CHI '15; April 18-23, 2015; Seoul, Republic of Korea. 2015. pp. 521–4. [DOI] [Google Scholar]
- 48.Guarino D, La Paglia F, Daino M, Maiorca V, Zichichi S, Guccione F, Pintabona A, Wiederhold MD, Riva G, La Barbera D. Chronic pain treatment through virtual reality. Annu Rev CyberTherapy Telemed. 2017 Dec;15:181–4. [Google Scholar]
- 49.Jin W, Choo A, Gromala D, Shaw C, Squire P. A virtual reality game for chronic pain management: a randomized, controlled clinical study. Stud Health Technol Inform. 2016;220:154–60. [PubMed] [Google Scholar]
- 50.Jones T, Moore T, Choo J. The impact of virtual reality on chronic pain. PLoS One. 2016 Dec 20;11(12):e0167523. doi: 10.1371/journal.pone.0167523. https://dx.plos.org/10.1371/journal.pone.0167523 .PONE-D-16-26747 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 51.Pamment J, Aspell JE. Putting pain out of mind with an 'out of body' illusion. Eur J Pain. 2017 Feb;21(2):334–42. doi: 10.1002/ejp.927. [DOI] [PubMed] [Google Scholar]
- 52.Shahrbanian S, Simmonds MJ. Effects of different virtual reality environments on experimental pain rating in post-stroke individuals with and without pain in comparison to pain free healthy individuals. Annu Rev CyberTher Telemed. 2008 Jul;:653–9. [Google Scholar]
- 53.Wiederhold BK, Gao K, Kong L, Wiederhold MD. Mobile devices as adjunctive pain management tools. Cyberpsychol Behav Soc Netw. 2014 Jun;17(6):385–9. doi: 10.1089/cyber.2014.0202. http://europepmc.org/abstract/MED/24892202 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 54.Wiederhold BK, Gao K, Sulea C, Wiederhold MD. Virtual reality as a distraction technique in chronic pain patients. Cyberpsychol Behav Soc Netw. 2014 Jun;17(6):346–52. doi: 10.1089/cyber.2014.0207. http://europepmc.org/abstract/MED/24892196 . [DOI] [PMC free article] [PubMed] [Google Scholar]
- 55.Botella C, Garcia-Palacios A, Vizcaíno Y, Herrero R, Baños RM, Belmonte MA. Virtual reality in the treatment of fibromyalgia: a pilot study. Cyberpsychol Behav Soc Netw. 2013 Mar;16(3):215–23. doi: 10.1089/cyber.2012.1572. [DOI] [PubMed] [Google Scholar]
- 56.Collado-Mateo D, Dominguez-Muñoz FJ, Adsuar JC, Merellano-Navarro E, Gusi N. Exergames for women with fibromyalgia: a randomised controlled trial to evaluate the effects on mobility skills, balance and fear of falling. PeerJ. 2017 Apr 20;5:e3211. doi: 10.7717/peerj.3211. doi: 10.7717/peerj.3211.3211 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 57.Garcia-Palacios A, Herrero R, Vizcaíno Y, Belmonte MA, Castilla D, Molinari G, Baños RM, Botella C. Integrating virtual reality with activity management for the treatment of fibromyalgia: acceptability and preliminary efficacy. Clin J Pain. 2015 Jun;31(6):564–72. doi: 10.1097/AJP.0000000000000196. [DOI] [PubMed] [Google Scholar]
- 58.Herrero R, García-Palacios A, Castilla D, Molinari G, Botella C. Virtual reality for the induction of positive emotions in the treatment of fibromyalgia: a pilot study over acceptability, satisfaction, and the effect of virtual reality on mood. Cyberpsychol Behav Soc Netw. 2014 Jun;17(6):379–84. doi: 10.1089/cyber.2014.0052. [DOI] [PubMed] [Google Scholar]
- 59.Mortensen J, Kristensen LQ, Brooks EP, Brooks AL. Women with fibromyalgia's experience with three motion-controlled video game consoles and indicators of symptom severity and performance of activities of daily living. Disabil Rehabil Assist Technol. 2015 Jan;10(1):61–6. doi: 10.3109/17483107.2013.836687. [DOI] [PubMed] [Google Scholar]
- 60.Villafaina S, Borrega-Mouquinho Y, Fuentes-García JP, Collado-Mateo D, Gusi N. Effect of exergame training and detraining on lower-body strength, agility, and cardiorespiratory fitness in women with fibromyalgia: single-blinded randomized controlled trial. Int J Environ Res Public Health. 2019 Dec 24;17(1):161. doi: 10.3390/ijerph17010161. https://www.mdpi.com/resolver?pii=ijerph17010161 .ijerph17010161 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 61.Villafaina S, Collado-Mateo D, Fuentes JP, Rohlfs-Domínguez P, Gusi N. Effects of exergames on brain dynamics in women with fibromyalgia: a randomized controlled trial. J Clin Med. 2019 Jul 11;8(7):1015. doi: 10.3390/jcm8071015. https://www.mdpi.com/resolver?pii=jcm8071015 .jcm8071015 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 62.Alemanno F, Houdayer E, Emedoli D, Locatelli M, Mortini P, Mandelli C, Raggi A, Iannaccone S. Efficacy of virtual reality to reduce chronic low back pain: proof-of-concept of a non-pharmacological approach on pain, quality of life, neuropsychological and functional outcome. PLoS One. 2019 May 23;14(5):e0216858. doi: 10.1371/journal.pone.0216858. https://dx.plos.org/10.1371/journal.pone.0216858 .PONE-D-18-22962 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 63.Brown L, Chen ET, Binder DS. The use of virtual reality for Peri-procedural pain and anxiety at an outpatient spine clinic injection visit: an exploratory controlled randomized trial. Am J Transl Res. 2020 Sep 15;12(9):5818–26. http://europepmc.org/abstract/MED/33042461 . [PMC free article] [PubMed] [Google Scholar]
- 64.Matheve T, Bogaerts K, Timmermans A. Virtual reality distraction induces hypoalgesia in patients with chronic low back pain: a randomized controlled trial. J Neuroeng Rehabil. 2020 Apr 22;17(1):55. doi: 10.1186/s12984-020-00688-0. https://jneuroengrehab.biomedcentral.com/articles/10.1186/s12984-020-00688-0 .10.1186/s12984-020-00688-0 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 65.Monteiro-Junior RS, de Souza CP, Lattari E, Rocha NB, Mura G, Machado S, da Silva EB. Wii-workouts on chronic pain, physical capabilities and mood of older women: a randomized controlled double blind trial. CNS Neurol Disord Drug Targets. 2015;14(9):1157–64. doi: 10.2174/1871527315666151111120131.CNSNDDT-EPUB-71722 [DOI] [PubMed] [Google Scholar]
- 66.Thomas JS, France CR, Applegate ME, Leitkam ST, Walkowski S. Feasibility and safety of a virtual reality dodgeball intervention for chronic low back pain: a randomized clinical trial. J Pain. 2016 Dec;17(12):1302–17. doi: 10.1016/j.jpain.2016.08.011. http://europepmc.org/abstract/MED/27616607 .S1526-5900(16)30206-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 67.Trujillo MS, Alvarez AF, Nguyen L, Petros J. Embodiment in virtual reality for the treatment of chronic low back pain: a case series. J Pain Res. 2020 Nov 25;13:3131–7. doi: 10.2147/JPR.S275312. doi: 10.2147/JPR.S275312.275312 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 68.Harvie DS, Smith RT, Moseley GL, Meulders A, Michiels B, Sterling M. Illusion-enhanced virtual reality exercise for neck pain: a replicated single case series. Clin J Pain. 2020 Feb;36(2):101–9. doi: 10.1097/AJP.0000000000000780.00002508-202002000-00006 [DOI] [PubMed] [Google Scholar]
- 69.Rezaei I, Razeghi M, Ebrahimi S, Kayedi S, Rezaeian Zadeh A. A novel virtual reality technique (Cervigame®) compared to conventional proprioceptive training to treat neck pain: a randomized controlled trial. J Biomed Phys Eng. 2018 Nov 18;9(3):355–66. doi: 10.31661/jbpe.v0i0.556. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 70.Sarig Bahat H, Takasaki H, Chen X, Bet-Or Y, Treleaven J. Cervical kinematic training with and without interactive VR training for chronic neck pain - a randomized clinical trial. Man Ther. 2015 Feb;20(1):68–78. doi: 10.1016/j.math.2014.06.008.S1356-689X(14)00126-X [DOI] [PubMed] [Google Scholar]
- 71.Sarig Bahat H, Croft K, Carter C, Hoddinott A, Sprecher E, Treleaven J. Remote kinematic training for patients with chronic neck pain: a randomised controlled trial. Eur Spine J. 2018 Jun;27(6):1309–23. doi: 10.1007/s00586-017-5323-0.10.1007/s00586-017-5323-0 [DOI] [PubMed] [Google Scholar]
- 72.Tejera DM, Beltran-Alacreu H, Cano-de-la-Cuerda R, Leon Hernández JV, Martín-Pintado-Zugasti A, Calvo-Lobo C, Gil-Martínez A, Fernández-Carnero J. Effects of virtual reality versus exercise on pain, functional, somatosensory and psychosocial outcomes in patients with non-specific chronic neck pain: a randomized clinical trial. Int J Environ Res Public Health. 2020 Aug 16;17(16):5950. doi: 10.3390/ijerph17165950. https://www.mdpi.com/resolver?pii=ijerph17165950 .ijerph17165950 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 73.Chau B, Phelan I, Ta P, Chi B, Loyola K, Yeo E, Dunn J, Humbert S, Hata J, Haglund R, Luna L, Kampmeier G, McCowan B. Immersive virtual reality for pain relief in upper limb complex regional pain syndrome: a pilot study. Innov Clin Neurosci. 2020 Apr 01;17(4-6):47–52. http://europepmc.org/abstract/MED/32802594 . [PMC free article] [PubMed] [Google Scholar]
- 74.Matamala-Gomez M, Diaz Gonzalez AM, Slater M, Sanchez-Vives MV. Decreasing pain ratings in chronic arm pain through changing a virtual body: different strategies for different pain types. J Pain. 2019 Jun;20(6):685–97. doi: 10.1016/j.jpain.2018.12.001.S1526-5900(18)30994-5 [DOI] [PubMed] [Google Scholar]
- 75.Sato K, Fukumori S, Matsusaki T, Maruo T, Ishikawa S, Nishie H, Takata K, Mizuhara H, Mizobuchi S, Nakatsuka H, Matsumi M, Gofuku A, Yokoyama M, Morita K. Nonimmersive virtual reality mirror visual feedback therapy and its application for the treatment of complex regional pain syndrome: an open-label pilot study. Pain Med. 2010 Apr;11(4):622–9. doi: 10.1111/j.1526-4637.2010.00819.x.PME819 [DOI] [PubMed] [Google Scholar]
- 76.Mouraux D, Brassinne E, Sobczak S, Nonclercq A, Warzée N, Sizer PS, Tuna T, Penelle B. 3D augmented reality mirror visual feedback therapy applied to the treatment of persistent, unilateral upper extremity neuropathic pain: a preliminary study. J Man Manip Ther. 2017 Jul;25(3):137–43. doi: 10.1080/10669817.2016.1176726. http://europepmc.org/abstract/MED/28694676 .yjmt-25-137 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 77.Ortiz-Catalan M, Guðmundsdóttir RA, Kristoffersen MB, Zepeda-Echavarria A, Caine-Winterberger K, Kulbacka-Ortiz K, Widehammar C, Eriksson K, Stockselius A, Ragnö C, Pihlar Z, Burger H, Hermansson L. Phantom motor execution facilitated by machine learning and augmented reality as treatment for phantom limb pain: a single group, clinical trial in patients with chronic intractable phantom limb pain. Lancet. 2016 Dec 10;388(10062):2885–94. doi: 10.1016/S0140-6736(16)31598-7.S0140-6736(16)31598-7 [DOI] [PubMed] [Google Scholar]
- 78.Rutledge T, Velez D, Depp C, McQuaid JR, Wong G, Jones RC, Atkinson JH, Giap B, Quan A, Giap H. A virtual reality intervention for the treatment of phantom limb pain: development and feasibility results. Pain Med. 2019 Oct 01;20(10):2051–9. doi: 10.1093/pm/pnz121.5511535 [DOI] [PubMed] [Google Scholar]
- 79.Tong X, Wang X, Cai Y, Gromala D, Williamson O, Fan B, Wei K. "I dreamed of my hands and arms moving again": a case series investigating the effect of immersive virtual reality on phantom limb pain alleviation. Front Neurol. 2020;11:876. doi: 10.3389/fneur.2020.00876. doi: 10.3389/fneur.2020.00876. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 80.Griffin A, Wilson L, Feinstein AB, Bortz A, Heirich MS, Gilkerson R, Wagner JF, Menendez M, Caruso TJ, Rodriguez S, Naidu S, Golianu B, Simons LE. Virtual reality in pain rehabilitation for youth with chronic pain: pilot feasibility study. JMIR Rehabil Assist Technol. 2020 Nov 23;7(2):e22620. doi: 10.2196/22620. https://rehab.jmir.org/2020/2/e22620/ v7i2e22620 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 81.Darnall BD, Krishnamurthy P, Tsuei J, Minor JD. Self-administered skills-based virtual reality intervention for chronic pain: randomized controlled pilot study. JMIR Form Res. 2020 Jul 07;4(7):e17293. doi: 10.2196/17293. https://formative.jmir.org/2020/7/e17293/ v4i7e17293 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 82.House G, Burdea G, Grampurohit N, Polistico K, Roll D, Damiani F, Hundal J, Demesmin D. A feasibility study to determine the benefits of upper extremity virtual rehabilitation therapy for coping with chronic pain post-cancer surgery. Br J Pain. 2016 Nov;10(4):186–97. doi: 10.1177/2049463716664370. http://europepmc.org/abstract/MED/27867508 .10.1177_2049463716664370 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 83.Phoon Nguyen AH, Balasubramaniam R, Bellan V, Newport RN, Stanton TR. The effect of multisensory illusions on pain and perceived burning sensations in patients with Burning Mouth Syndrome: a proof-of-concept study. J Oral Pathol Med. 2020 Jul;49(6):505–13. doi: 10.1111/jop.13065. [DOI] [PubMed] [Google Scholar]
- 84.Solcà M, Krishna V, Young N, Deogaonkar M, Herbelin B, Orepic P, Mange R, Rognini G, Serino A, Rezai A, Blanke O. Enhancing analgesic spinal cord stimulation for chronic pain with personalized immersive virtual reality. Pain. 2021 Jun 01;162(6):1641–9. doi: 10.1097/j.pain.0000000000002160.00006396-202106000-00008 [DOI] [PubMed] [Google Scholar]
- 85.Stirling ER, Lewis TL, Ferran NA. Surgical skills simulation in trauma and orthopaedic training. J Orthop Surg Res. 2014 Dec 19;9:126. doi: 10.1186/s13018-014-0126-z. https://josr-online.biomedcentral.com/articles/10.1186/s13018-014-0126-z .s13018-014-0126-z [DOI] [PMC free article] [PubMed] [Google Scholar]
- 86.Seymour NE, Gallagher AG, Roman SA, O'Brien MK, Bansal VK, Andersen DK, Satava RM. Virtual reality training improves operating room performance: results of a randomized, double-blinded study. Ann Surg. 2002 Oct;236(4):458–64. doi: 10.1097/00000658-200210000-00008. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 87.Kehlet H, Holte K. Effect of postoperative analgesia on surgical outcome. Br J Anaesth. 2001 Jul;87(1):62–72. doi: 10.1093/bja/87.1.62. https://linkinghub.elsevier.com/retrieve/pii/S0007-0912(17)36344-4 .S0007-0912(17)36344-4 [DOI] [PubMed] [Google Scholar]
- 88.Das DA, Grimmer KA, Sparnon AL, McRae SE, Thomas BH. The efficacy of playing a virtual reality game in modulating pain for children with acute burn injuries: a randomized controlled trial [ISRCTN87413556] BMC Pediatr. 2005 Mar 03;5(1):1. doi: 10.1186/1471-2431-5-1. https://bmcpediatr.biomedcentral.com/articles/10.1186/1471-2431-5-1 .1471-2431-5-1 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 89.Patterson DR, Hoffman HG, Palacios AG, Jensen MJ. Analgesic effects of posthypnotic suggestions and virtual reality distraction on thermal pain. J Abnorm Psychol. 2006 Nov;115(4):834–41. doi: 10.1037/0021-843X.115.4.834.2006-20696-019 [DOI] [PubMed] [Google Scholar]
- 90.Rousseaux F, Bicego A, Ledoux D, Massion P, Nyssen AS, Faymonville ME, Laureys S, Vanhaudenhuyse A. Hypnosis associated with 3D immersive virtual reality technology in the management of pain: a review of the literature. J Pain Res. 2020 May 21;13:1129–38. doi: 10.2147/JPR.S231737. doi: 10.2147/JPR.S231737.231737 [DOI] [PMC free article] [PubMed] [Google Scholar]
- 91.Konstantatos AH, Angliss M, Costello V, Cleland H, Stafrace S. Predicting the effectiveness of virtual reality relaxation on pain and anxiety when added to PCA morphine in patients having burns dressings changes. Burns. 2009 Jun;35(4):491–9. doi: 10.1016/j.burns.2008.08.017.S0305-4179(08)00271-4 [DOI] [PubMed] [Google Scholar]
- 92.Goudman L, De Smedt A, Linderoth B, Eldabe S, Witkam R, Henssen D, Moens M. Identifying goals in patients with chronic pain: a European survey. Eur J Pain. 2021 Oct;25(9):1959–70. doi: 10.1002/ejp.1814. [DOI] [PubMed] [Google Scholar]
- 93.Fehrmann E, Kotulla S, Fischer L, Kienbacher T, Tuechler K, Mair P, Ebenbichler G, Paul B. The impact of age and gender on the ICF-based assessment of chronic low back pain. Disabil Rehabil. 2019 May;41(10):1190–9. doi: 10.1080/09638288.2018.1424950. [DOI] [PubMed] [Google Scholar]
- 94.The International Classification of Functioning, Disability and Health (ICF) World Health Organization. 2001. [2021-09-29]. http://www.who.int/classifications/icf/en/
- 95.How to use the ICF: a practical manual for using the International Classification of Functioning, Disability and Health (ICF) - Exposure draft for comment. World Health Organization. 2013. [2021-08-12]. https://www.medbox.org/pdf/5e148832db60a2044c2d4d88 .
- 96.Ahern MM, Dean LV, Stoddard CC, Agrawal A, Kim K, Cook CE, Narciso Garcia A. The effectiveness of virtual reality in patients with spinal pain: a systematic review and meta-analysis. Pain Pract. 2020 Jul;20(6):656–75. doi: 10.1111/papr.12885. [DOI] [PubMed] [Google Scholar]
- 97.Cerritelli F, Chiera M, Abbro M, Megale V, Esteves J, Gallace A, Manzotti A. The challenges and perspectives of the integration between virtual and augmented reality and manual therapies. Front Neurol. 2021 Jun 30;12:700211. doi: 10.3389/fneur.2021.700211. doi: 10.3389/fneur.2021.700211. [DOI] [PMC free article] [PubMed] [Google Scholar]
- 98.Assink M, Wibbelink CJ. Fitting three-level meta-analytic models in R: a step-by-step tutorial. Quant Meth Psych. 2016 Oct 01;12(3):154–74. doi: 10.20982/tqmp.12.3.p154. [DOI] [Google Scholar]
Associated Data
This section collects any data citations, data availability statements, or supplementary materials included in this article.
Supplementary Materials
The full search strategy for PubMed.
Risk of bias table based on the modified version of the Downs and Black Checklist.
Overview of the effects of virtual reality on several outcome measurements for each study.


